Abstract
Background:
Despite evidence-based guidelines advocating for the provision of oral health care throughout pregnancy, dentists remain hesitant to provide dental treatment for pregnant women. However, little is known about attitudes toward treating pregnant women among dental school faculty, who may transmit their attitudes and treatment preferences to their students.
Methods:
We collected cross-sectional survey data at the New York University College of Dentistry, which produces 10% of all US dentists and is the largest US dental school, to understand faculty attitudes and knowledge regarding providing dental treatment to pregnant women. This study was part of an educational effort to improve dental care access by pregnant women and to examine what factors influence willingness to treat pregnant patients among dental faculty members.
Results:
We found that concerns about professional liability outweighed inadequate knowledge regarding treatment of pregnant patients in determining dental faculty’s willingness to treat pregnant women.
Conclusions:
Educational interventions delivered to dental faculty regarding current dental treatment guidelines for pregnant women may not be sufficient to increase faculty’s provision of dental care to women during pregnancy. Future work to design effective interventions to increase dental treatment of pregnant women among dental faculty should address liability concerns.
Knowledge Transfer Statement
Interventions addressing dental clinician and faculty knowledge about dental treatment for pregnant women may be insufficient to increase dental treatment among pregnant women. Instead, policy makers should consider designing, implementing, and evaluating interventions addressing malpractice and liability concerns.
Keywords: prenatal care, oral health, evidence-based medicine, knowledge, attitude, malpractice
Introduction
During pregnancy, women are at an increased risk of oral disease (Azofeifa et al. 2016). Despite evidence-based guidelines designed to improve oral health during pregnancy (Oral Health Care During Pregnancy Expert Workgroup 2012), dental care during pregnancy remains underutilized, especially among low-income and racial/ethnic minority women, who are especially vulnerable to oral disease (Gaffield et al. 2001; Eke et al. 2005; Dooley et al. 2010; Hwang et al. 2011; Singhal et al. 2014; Hayes et al. 2015). Importantly, for these women, pregnancy and the postpartum period may be the only time when they have access to dental care via the Medicaid program (National Health Law 2013; Hartnett et al. 2016; Stohl and Chen 2018), which covers dental care in many states, including New York State. The reason is that Medicaid programs are not required to provide adult dental services but must cover pregnancy-related dental services (National Health Law 2013). The cost of private dental care coverage and its out-of-pocket cost without coverage are otherwise prohibitive among the low-income population (Yarbrough et al. 2014).
Dental providers may be reluctant to treat pregnant women due to concerns about cost and/or reimbursement (Huebner et al. 2009; Lee et al. 2010), a lack of knowledge of current evidence-based guidelines for oral care during pregnancy, and a lack of adoption of these evidence-based guidelines (Lee et al. 2010). Low-income women covered by Medicaid may have difficulty finding dentists accepting Medicaid as payment for treatment (Russell and Mayberry 2008). Although insurers may provide reimbursement for dentists to provide dental care to pregnant patients, the perceived time and economic costs of treating pregnant patients have been found to be significant barriers for dentists (Lee et al. 2010). In a survey of an Oregon dental care organization, concerns about litigation related to complications after dental treatment were the greatest barrier for dentists in treating pregnant patients (Kloetzel et al. 2012). Hence, understanding and addressing barriers to dental care for pregnant women from dental providers are likely key in improving access to dental care and improving the oral health of pregnant women.
Though prior studies have examined determinants in dental providers’ choices to treat or not treat pregnant women (Huebner et al. 2009; Lee et al. 2010; Vieira et al. 2015), no studies to date have examined attitudes and determinants in treating pregnant women among dental school faculty. Because dental faculty instruct students in class and clinical settings, attitudes expressed by dental faculty may affect whether students are taught and exposed to opportunities to provide clinical dental treatment for pregnant women, which may lead to choice heuristics about treating pregnant women unaligned with evidence-based guidelines.
The New York University College of Dentistry (NYU COD; 2020) trains nearly 10% of the dentists in the United States. Hence, knowledge and attitudes among dental faculty at NYU COD toward the clinical treatment of pregnant women may have an outsized impact on dental treatment norms in the United States more broadly. At the NYU COD, we are currently collaborating with Bellevue Hospital via the Prenatal Oral Health Program (POHP) to provide dental care to pregnant women who are disproportionately low income and/or insured by Medicaid. To address barriers to care at various levels, the POHP provides training for medical and dental providers and staff on how to safely, expeditiously, and effectively provide dental care for pregnant women. The educational component of our POHP at the NYU COD targets dental students and dental faculty through lectures on providing dental care during pregnancy as part of the dental curriculum and through continuing education (CE) lectures on providing dental care during pregnancy for dental faculty. As a part of our POHP at the NYU COD, we surveyed dental faculty regarding knowledge and attitudes that may affect dental faculty’s willingness to provide dental treatment during pregnancies. The purpose of this study is to report on the knowledge and attitudes of dental faculty regarding the treatment of pregnant women and the determinants of dental faculty’s willingness to treat pregnant women.
Methods
Questionnaire Design
We designed a questionnaire to evaluate knowledge and attitudes regarding provision of dental care to pregnant women and to assess dental faculty’s willingness to provide dental treatment during pregnancy. We created our questionnaire based on those described in published studies (Huebner et al. 2009; Lee et al. 2010) and pilot-tested it with a small sample of dental faculty (n = 6) for understandability, readability, and face validity.
Questionnaire and Variables
Our questionnaire comprised 14 questions designed to elicit dental faculty members’ knowledge (10 items), attitudes (2 items), and willingness (2 items) to treat pregnant patients. We used Donabedian’s (1988) conceptual model of the medical care process and Eisenberg’s (1979) reviews of physician decision making to hypothesize what attitudinal, knowledge, and demographic factors might influence dental faculty’s willingness to treat pregnant women. Responses to each statement were based on a 7-point Likert scale (very strongly agree, strongly agree, mildly agree, neutral, mildly disagree, strongly disagree, and very strongly disagree). We also included questions asking about demographic characteristics and dental school training potentially influencing a clinician’s practice style. We did not include questions eliciting the perceived cost and reimbursement from providing dental care to pregnant patients, due to potential concerns about survey anonymity and privacy. We purposefully placed sociodemographic and work-related variables at the end of the survey (see Appendix B), so concerns about privacy would not inhibit faculty from responding (at least in part) to the survey.
We did not directly include any attitude statements for the costs of providing care for pregnant women at NYU COD, since the dental faculty providing clinical care there are paid by salary. Hence, concerns about the profitability of treating pregnant women within NYU COD may not significantly affect dental faculty practice behavior. Instead, decisions about profitability are made at the institutional level, and NYU COD had issued a statement to the faculty and clinical practice community at NYU COD on its support for the treatment of pregnant women.
Study Setting and Data Collection
All full- and part-time NYU COD faculty and staff (paid and volunteer) were invited to attend a CE lecture on the appropriate provision of dental care during pregnancy according to evidence-based guidelines (Oral Health Care During Pregnancy Expert Workgroup 2012) via an email blast and posted announcements at the NYU COD. Since many clinical faculty are present at the NYU COD 1 or 2 d/wk, we presented the same lecture 5 times on different weekdays (Monday to Friday) to provide an opportunity for as many faculty as possible to attend (lecture slides are in Appendix C). We provided these 5 lectures over an approximately 1-mo period in March/April 2018. Lectures occurred during the lunchtime hour. As attendees are routinely provided lunch, there is typically robust attendance at these sessions. We distributed anonymous pen-and-paper questionnaires prior to each CE lecture to all attending participants. While participants were urged to complete the questionnaire, completion was not a requirement to receive CE credit. We advised respondents that survey responses could not be linked to individuals and only aggregate data from the questionnaires would be reported. The 3 faculty members conducting the research were excluded from participation. This study was deemed exempt by the NYU Institutional Review Board.
Separate from the survey data collection, we collected information on attendance from the sign-in sheets and linked this to internal data on faculty demographics. This was done to assess whether the faculty members participating in the CE lectures were representative of the NYU COD faculty as a whole.
Analyses
The completed questionnaires were entered into SPSS 26 (IBM). Initial data cleaning was done with SPSS, and descriptive statistics and regression analyses were conducted with Stata/MP 15.1 (StataCorp). We restricted our analysis to NYU COD faculty who answered all survey questions regarding knowledge, attitude, and willingness. We assessed reliability of the questionnaire with Cronbach’s alpha coefficient.
The small sample size (N = 86) prevented us from intensive analyses of the psychometric properties (e.g., factor analysis) of our newly developed measure. However, we plan to do so in the near future after collecting data from a larger sample, which will be overseen by a senior psychometrician on the authoring team (C.Y.). As a preliminary attempt, we ran some basic psychometric analysis at the item level and the dimension level, such as item correlation, item scale analysis, and internal consistency analysis with Cronbach’s alpha.
To test the hypothesis that attitudes and knowledge concerning dental treatment for pregnant patients influence willingness to treat pregnant patients, we conducted ordinal logit regression analysis. The dependent variable was the raw sum score of the 2 items representing the willingness to treat pregnant women during pregnancy. Given the limited sample size, we incorporated the raw sum score of the items in the knowledge domain (instead of each item individually) as an independent variable to decrease the dimensionality of the analysis. Since the attitude domain has only 2 items, we included both items separately in the analysis. Additionally, we included sociodemographic variables (gender, years as faculty) as factors that may influence the willingness to treat pregnant women during pregnancy. Due to some survey responses in the analysis sample being incomplete with regard to faculty sociodemographics, regressions including gender and years as faculty dropped observations with the missing sociodemographic variables.
We assessed whether CE participants were representative of the NYU COD clinical faculty using the linked attendance and internal faculty demographics data. This was done through chi-square tests comparing demographic distribution of CE participants to the overall NYU COD clinical faculty population. We followed STROBE guidelines for the reporting of cross-sectional studies (equator-network.org/reporting-guidelines/strobe/).
Results
A total of 102 faculty returned at least partially completed questionnaires. This represents 21.7% of the NYU COD clinical faculty (of which there are 469). Incomplete questionnaires were missing at least 1 response to the knowledge and attitude sections and were excluded from the analysis (n = 16). Of the 16 excluded questionnaires, 14 were missing a response to 1 question, and 2 were missing responses to 2 or 3 questions. This suggests that some respondents may have overlooked some of the questions by mistake.
Our analysis of the attendance data linked to the internal faculty demographic data found that CE participants were more likely to be full-time faculty and to be in private practice than the overall NYU COD clinical faculty population (Appendix A Table 1). However, CE participants were not substantially different in academic rank and full- or part-time status from the overall clinical faculty population.
Data analysis was conducted with 86 questionnaires for a response rate of 84.3% (Appendix Table 2). Respondents in the analysis sample were primarily male (57%). About one-third (33.7%) of the analysis sample reported being within the first 10 y as faculty, and 58.1% reported current work in a private practice or a clinic. Almost half (47.7%) of participants were full-time employees at the NYU COD.
Knowledge
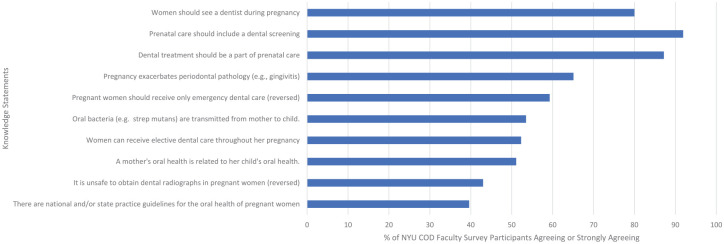
We examined the proportion of NYU COD clinical faculty respondents who reported “strongly agree” or “agree” with each knowledge question (Fig. 1). Most agreed that women should see a dentist during pregnancy (80.0%), that prenatal care should include a dental screening (91.9%), and that dental treatment should be a part of prenatal care (87.2%). Of faculty respondents 59.3% agreed that pregnant women should receive more than emergency dental care, and 43.0% agreed that it is safe to obtain dental radiographs in pregnant women. In addition, 65.1% agreed that pregnancy exacerbates periodontal pathology, and 51.1% agreed that a mother’s oral health is related to her child’s oral health. Only 39.6% of NYU COD faculty agreed that there are national and/or state practice guidelines for the oral health of pregnant women.
Figure 1.
The percentages of faculty survey participants (N = 86; New York University College of Dentistry) who agree or strongly agree with each statement in the knowledge section about treatment of pregnant women.
Attitudes
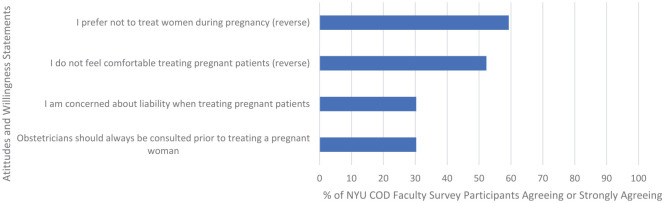
We then examined the proportion of NYU COD clinical faculty respondents who reported “strongly agree” or “agree” with each attitude question (Fig. 2). About a third of respondents (30.3%) agreed that obstetricians should always be consulted prior to treating a pregnant woman. In addition, about a third (30.3%) stated that they were concerned about liability when treating pregnant patients.
Willingness
Finally, we examined the proportion of those who indicated that they “strongly agreed” or “agreed” with each willingness question (Fig. 2). About half (52.3%) of respondents disagreed with the statement “I do not feel comfortable treating pregnant patients,” and 59.3% disagreed with the statement “I prefer not to treat women during pregnancy.”
Figure 2.
The percentages of faculty survey participants (N = 86; New York University College of Dentistry) who agree or strongly agree with each statement in the sections covering attitudes and willingness to treat pregnant women.
Cronbach’s alpha knowledge based on the original 10 items was 0.68, close to “good” (Appendix A Table 3; Kline 2015). After we removed 2 items (Q5 and Q7) with low item-test correlation (<0.3; O’Rourke and Hatcher 2013), the Cronbach’s alpha improved to 0.72 (Table 1), which is above “good.” As a result, we discarded Q5 and Q7 from the raw item score for knowledge in the regression analysis and used the remaining 8 items for the summary scores of knowledge, which ranged from 8 to 56. Higher scores represent more knowledge about treating the dental issues of pregnant women.
Table 1.
Cronbach’s Alpha for Knowledge Domain (After Excluding Items 5 and 7).
| Correlation | ||||||
|---|---|---|---|---|---|---|
| Item | Question | Sign | Item-Test | Item-Rest | Interitem | Alpha |
| 1 | Prenatal care should include a dental screening | + | 0.7304 | 0.6029 | 0.2136 | 0.6553 |
| 2 | Dental treatment should be a part of prenatal care | + | 0.7187 | 0.5872 | 0.2162 | 0.6588 |
| 3 | Women should see a dentist during pregnancy | + | 0.7597 | 0.6427 | 0.207 | 0.6464 |
| 4 | Pregnant women should receive only emergency dental care | — | 0.4316 | 0.2343 | 0.28 | 0.7313 |
| 6 | It is unsafe to obtain dental radiographs in pregnant women | — | 0.3427 | 0.1354 | 0.2997 | 0.7498 |
| 8 | Oral bacteria (e.g., strep mutans) are transmitted from mother to child. | + | 0.4842 | 0.2948 | 0.2683 | 0.7196 |
| 9 | A mother’s oral health is related to her child’s oral health. | + | 0.5998 | 0.4342 | 0.2426 | 0.6915 |
| 10 | There are national and/or state practice guidelines for the oral health of pregnant women. | + | 0.6007 | 0.4352 | 0.2424 | 0.6913 |
| Test scale | 0.2462 | 0.7232 | ||||
Analysis is based on a sample that answered all knowledge, attitude, and willingness questions (N = 86).
Cronbach’s alpha was 0.37 for assessing internal consistency for attitudes and 0.87 for willingness to treat pregnant patients (Table 2). Because of the low Cronbach’s alpha for the attitude domain, we included attitude items individually into the regression analysis as separate independent variables. Due to the high Cronbach’s alpha (>0.7) for willingness to treat pregnant patients, we combined the 2 variables in the domain for the willingness to treat pregnant patients into a single raw item score for a third dependent variable.
Table 2.
Cronbach’s Alpha for Domains Covering Attitude and Willingness to Treat Pregnant Women.
| Domain: Item | Question | Scale Reliability Coefficient |
|---|---|---|
| Attitude | 0.3700 | |
| 11 | Obstetricians should always be consulted prior to treating a pregnant woman. | |
| 12 | I am concerned about liability when treating pregnant patients. | |
| Willingness to treat pregnant women | 0.8672 | |
| 13 | I do not feel comfortable treating pregnant patients. | |
| 14 | I prefer not to treat women during pregnancy. |
Analysis is based on a sample that answered all knowledge, attitude, and willingness questions (N = 86).
In our ordinal logit regression analysis, we found that faculty concerns about liability when treating pregnant patients had the strongest impact on willingness to treat them, followed by general knowledge of dental treatment for pregnant patients. We found that for a 1-unit increase in lack of concern about liability, there was a 1.633-point increase in the ordered log odds of being in a higher comfort level to treat pregnant patients, all else held constant (Table 3, column 1). In comparison, a 1-unit increase in the knowledge was correlated with a 1.170-point increase in the ordered log odds of being more comfortable providing care to pregnant patients, all else held constant. The relative size of these 2 coefficients remained fairly constant across regression specifications, even with the addition of additional sociodemographic controls.
Table 3.
Ordinal Logit Regressions Assessing Factors Influencing Willingness to Treat Pregnant Women.
| Dependent Variable: Willingness to Treat Pregnant Womena | |||
|---|---|---|---|
| Variableb | 1 | 2 | 3 |
| Knowledge about pregnant women | 1.170c (1.095 to 1.250) | 1.173c (1.097 to 1.255) | 1.147c (1.066 to 1.235) |
| Obstetricians should always be consulted prior to treating a pregnant women | 1.022 (0.800 to 1.307) | 1.027 (0.793 to 1.331) | 0.899 (0.684 to 1.180) |
| I am not concerned about liability when treating pregnant patients | 1.633d (1.197 to 2.227) | 1.604d (1.185 to 2.172) | 1.613d (1.133 to 2.296) |
| Controls for gender | × | × | |
| Controls for years as faculty | × | ||
| Observations | 86 | 83 | 77 |
Analysis is based on a sample that answered all knowledge, attitude, and willingness questions (N = 86). The drop in sample size from column 1, 2, and 3 was due to survey responses that did not include information on gender (columns 2 and 3) and/or number of years as faculty (column 3).
The dependent variable is the raw additive score across the 2 questions assessing the willingness to treat pregnant women. 95% CIs are in parentheses and were calculated with robust standard errors.
The “knowledge about pregnant women” variable is the raw additive score across all knowledge questions, excluding items 5 and 7. The other two key independent variables of interest (“Obstetricians should always be consulted prior to treating a pregnant women” and “I am not concerned about liability when treating pregnant patients”) are included individually, since these are the only 2 items in the attitude domain.
P < 0.001.
P < 0.01.
Discussion
Evidence-based guidelines advocating for the delivery of dental care throughout pregnancy were first published in New York in 2006 (Kumar and Samelson 2006) and nationally in 2012 (Oral Health Care During Pregnancy Expert Workgroup 2012), but awareness among dental faculty of the presence of these guidelines remains low. Perhaps as a result, knowledge among NYU COD faculty regarding the appropriateness of dental treatment for pregnant women is highly variable. Traditionally, dental students were taught that routine dental care during pregnancy should be limited to the second trimester to avoid interfering with fetal development during the first trimester and putting undue stress on the mother during the third trimester. Given the evidence from multiple randomized controlled trials that provision of dental care during pregnancy is effective and safe (Michalowicz et al. 2006; Michalowicz et al. 2008; George et al. 2011) and the presence of published evidence-based guidelines, treatment paradigms regarding the provision of dental care during pregnancy have changed. Such changes should allow for more women to access dental health care during pregnancy to achieve better oral health for themselves and ultimately their children.
Our results suggest that addressing knowledge gaps among dental faculty may only partially address barriers to dental treatment of pregnant women. We found that higher levels of concern about liability were more strongly correlated with lower willingness to treat pregnant women, as compared with the correlation between higher levels of knowledge and higher willingness to treat pregnant women. This finding is consistent with prior literature that has examined attitudes and knowledge of dental care during pregnancy among dental practitioners more globally. Malpractice concerns are a factor in willingness to treat pregnant women even among faculty at a dental school, presumably with greater incentives to provide care for this more vulnerable population who may have access to dental care only during pregnancy and immediately postpartum.
Therefore, interventions seeking to increase treatment of pregnant women should consider addressing concerns about liability and not just the gaps in knowledge in the appropriateness of dental treatment of pregnant women. Future work uncovering determinants of beliefs about liability issues may be an important factor in designing interventions to overcome barriers to the provision of dental treatment for pregnant women.
Limitations
Although we found a statistically significant correlation between the knowledge held by dental faculty about the treatment of pregnant women and willingness to treat them, it is unclear to what extent changes in knowledge would actually result in an increased willingness to treat. In this study we did not assess the following: whether the single CE course on dental treatment for pregnant women caused dental faculty to update their knowledge, whether this knowledge was retained, whether updated knowledge affected their long-term willingness to treat pregnant women, and whether updated knowledge had a perceivable impact on the actual probability of treating pregnant women and/or the number of pregnant women treated by dental faculty. We did not include a postcourse survey to assess knowledge change, primarily due to concerns about whether such a survey would have a sufficiently high response rate, given the lack of incentives to complete the precourse survey. Additionally, we would have ideally wanted pre- and postcourse survey data to be linkable at the individual level, but this would have compromised the anonymity of the survey and potentially the response rate to the precourse survey. Moreover, such a postcourse survey would not address the question of whether the course actually changed practice behavior and student instruction. We anticipate addressing the issue of how to measure changes in the treatment of pregnant women among dental faculty in future work.
Similarly, it is unclear whether informing dental faculty about the likelihood of being faced with liability issues when treating pregnant women will affect their willingness to treat and their actual treatment behavior. Future work may examine what factors influence beliefs about liability, whether beliefs about liability can be shifted by specific policy or educational instruments, and whether changes in liability beliefs will affect actual behavior.
Another limitation of our work is the limited sample size. As in any survey study, respondents may not be representative of the entire population of interest. In this study, those who chose to attend and respond to a survey may be more likely than the overall faculty population to express a willingness to treat pregnant patients. However, it is likely that such self-selection into seminar and survey participation biases our coefficient estimates toward zero. Given that our coefficient estimates are substantive in size and statistically significant, future work replicating our analysis on a larger, more representative sample is likely to find similar results. In addition, the limited sample size of this study likely resulted in a lack of power to detect differences in groups. Despite our working hypothesis, the present study was largely exploratory; therefore, we did not undertake a power analysis prior to the start of this study. We anticipate attempting to increase our sample size and participation among dental faculty in our future work.
Finally, the low internal consistency reliability, as measured by Cronbach’s alpha of the attitude domain (0.37), is surprising. This indicates that the 2 items within the attitude domain do not correlate well. We plan in follow-up work to develop more items through qualitative and quantitative methods (i.e., focus group studies and psychometric analyses) to generate a valid and reliable measure for the attitude domain.
Conclusions
Despite multiple evidence-based guidelines for dental treatment for women during pregnancy, awareness of these guidelines remains low among dental faculty at the NYU COD. Yet, educational interventions to increase dental faculty’s knowledge about guidelines for dental treatment of pregnant women may not be sufficient—concerns about liability are likely a significant barrier in dentists’ willingness to provide treatment for pregnant women.
This study’s findings have potentially large ramifications for the dental profession as a whole, especially for future cohorts of dentists, since NYU COD (2020) trains a large proportion of all US dentists (10%). Even if students are taught how to treat patients during pregnancy according to current guidelines, dental faculty may be unwilling to supervise the treatment of pregnant patients and could transmit their own beliefs and attitudes to students despite countervailing evidence. Thus, outdated attitudes and beliefs toward the dental treatment of pregnant women may be propagated in later generations of dentists despite existing guidelines and interventions.
As a result, further work is warranted to untangle the causal determinants of willingness to treat pregnant women for dental faculty and to design effective interventions to increase the dental treatment of pregnant women among faculty.
Author Contributions
S.S. Huang, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript; C. Yang, contributed to design, data analysis, and interpretation, critically revised the manuscript; V. Cohen, contributed to data analysis, critically revised the manuscript; S.L. Russell, contributed to conception, design, and data acquisition, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, sj-docx-1-jct-10.1177_23800844211028132 for What Factors Influence Dental Faculty’s Willingness to Treat Pregnant Women? by S.S. Huang, C. Yang, V. Cohen and S.L. Russell in JDR Clinical & Translational Research
Footnotes
A supplemental appendix to this article is available online.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: S.L. Russell is funded by the New York State Health Foundation (NYSHF 18-06007, $154,000; November 1, 2018, to February 28, 2019).
References
- Azofeifa A, Yeung LF, Alverson C, Beltrán-Aguilar E. 2016. Dental caries and periodontal disease among US pregnant women and nonpregnant women of reproductive age, National Health and Nutrition Examination Survey, 1999–2004. J Public Health Dent. 76(4):320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. 1988. The quality of care: how can it be assessed? JAMA. 260(12):1743–1748. [DOI] [PubMed] [Google Scholar]
- Dooley S, Lincoln A, Smith M, O’Neil M, Ahluwalia I, D’Angelo D, Morrow B. 2010. Perceived health needs and receipt of services during pregnancy—Oklahoma and South Carolina, 2004–2007. MMWR Morb Mortal Wkly Rep. 59(23):710–714. [PubMed] [Google Scholar]
- Eisenberg JM. 1979. Sociologic influences on decision-making by clinicians. Ann Intern Med. 90(6):957–964. [DOI] [PubMed] [Google Scholar]
- Eke PI, Timothé P, Presson SM, Malvitz DM. 2005. Dental care use among pregnant women in the United States reported in 1999 and 2002. Prev Chronic Dis. 2(1):A10. [PMC free article] [PubMed] [Google Scholar]
- Gaffield ML, Gilbert B, Malvitz D, Romaguera R. 2001. Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc. 132(7):1009–1016. [DOI] [PubMed] [Google Scholar]
- George A, Shamim S, Johnson M, Ajwani S, Bhole S, Blinkhorn A, Ellis S, Andrews K. 2011. Periodontal treatment during pregnancy and birth outcomes: a meta-analysis of randomised trials. Int J Evid Based Healthc. 9(2):122–147. [DOI] [PubMed] [Google Scholar]
- Hartnett E, Haber J, Krainovich-Miller B, Bella A, Vasilyeva A, Kessler JL. 2016. Oral health in pregnancy. J Obstet Gynecol Neonatal Nurs. 45(4):565–573. [DOI] [PubMed] [Google Scholar]
- Hayes DK, Turnure M, Mattheus DJ, Shannon MT. 2015. Predictors of dental cleaning over a two-year time period around pregnancy among Asian and Native Hawaiian or other Pacific Islander race subgroups in Hawai’i, 2009–2011. Hawaii J Med Public Health. 74(10):328–333. [PMC free article] [PubMed] [Google Scholar]
- Huebner CE, Milgrom P, Conrad D, Lee RSY. 2009. Providing dental care to pregnant patients: a survey of Oregon general dentists. J Am Dent Assoc. 140(2):211–222. [DOI] [PubMed] [Google Scholar]
- Hwang SS, Smith VC, McCormick MC, Barfield WD. 2011. Racial/ethnic disparities in maternal oral health experiences in 10 states, pregnancy risk assessment monitoring system, 2004–2006. Matern Child Health J. 15(6):722–729. [DOI] [PubMed] [Google Scholar]
- Kline RB. 2015. Principles and practice of structural equation modeling. New York (NY): Guilford Publications. [Google Scholar]
- Kloetzel MK, Huebner CE, Milgrom P, Littell CT, Eggertsson H. 2012. Oral health in pregnancy: educational needs of dental professionals and office staff. J Public Health Dent. 72(4):279–286. [DOI] [PubMed] [Google Scholar]
- Kumar J, Samelson R. 2006. Oral health care during pregnancy and early childhood: practice guidelines. New York (NY): New York State Department of Health. [Google Scholar]
- Lee RS-Y, Milgrom P, Huebner CE, Conrad DA. 2010. Dentists’ perceptions of barriers to providing dental care to pregnant women. Womens Health Issues. 20(5):359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalowicz BS, DiAngelis AJ, Novak MJ, Buchanan W, Papapanou PN, Mitchell DA, Curran AE, Lupo VR, Ferguson JE, Bofill J. 2008. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc. 139(6):685–695. [DOI] [PubMed] [Google Scholar]
- Michalowicz BS, Hodges JS, DiAngelis AJ, Lupo VR, Novak MJ, Ferguson JE, Buchanan W, Bofill J, Papapanou PN, Mitchell DA. 2006. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 355(18):1885–1894. [DOI] [PubMed] [Google Scholar]
- National Health Law. 2013. Dental coverage for low-income pregnant women [accessed 2020 Nov 25]. https://healthlaw.org/resource/dental-coverage-for-low-income-pregnant-women/#.VjjiuLerTct
- New York University College of Dentistry. 2020. About us [accessed 2020 Sep 28]. https://dental.nyu.edu/aboutus.html
- O’Rourke N, Hatcher L. 2013. A step-by-step approach to using SAS for factor analysis and structural equation modeling. Cary (NC): SAS Institute Inc. [Google Scholar]
- Oral Health Care During Pregnancy Expert Workgroup. 2012. Oral health during pregnancy: a national consensus statement. Washington (DC): National Maternal and Child Oral Health Resource Center. [Google Scholar]
- Russell SL, Mayberry LJ. 2008. Pregnancy and oral health: a review and recommendations to reduce gaps in practice and research. MCN Am J Matern Child Nurs. 33(1):32–37. [DOI] [PubMed] [Google Scholar]
- Singhal A, Chattopadhyay A, Garcia AI, Adams AB, Cheng D. 2014. Disparities in unmet dental need and dental care received by pregnant women in Maryland. Matern Child Health J. 18(7):1658–1666. [DOI] [PubMed] [Google Scholar]
- Stohl HE, Chen A. 2018. Oral health coverage options for pregnant adults and adolescents. Matern Child Health J. 22(1):24–31. [DOI] [PubMed] [Google Scholar]
- Vieira D, de Oliveira A, Lopes FF, Lopes e Maia MF. 2015. Dentists’ knowledge of oral health during pregnancy: a review of the last 10 years’ publications. Community Dent Health. 32(2):77–82. [PubMed] [Google Scholar]
- Yarbrough C, Nasseh K, Vujicic M. 2014. Why adults forgo dental care: evidence from a new national survey. American Dental Association Health Policy Institute Research Brief [accessed 2021 Jun 9]. https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1114_1.ashx
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jct-10.1177_23800844211028132 for What Factors Influence Dental Faculty’s Willingness to Treat Pregnant Women? by S.S. Huang, C. Yang, V. Cohen and S.L. Russell in JDR Clinical & Translational Research