Abstract
Data from the National Survey of Children’s Health 2016–2019 was used to examine the co-occurrence of autism and ADHD and the impact on anxiety and depression among adolescents age 12–17. Rates of anxiety and depression were up to ten-fold the prevalence of adolescents not diagnosed with autism or ADHD. Over half of autistic females (57%) and nearly half of autistic males (49%) are also diagnosed with ADHD. Autistic females with ADHD had the highest co-occurrence of anxiety at 72% followed by autistic males with ADHD at 69%. The prevalence of depression was highest among autistic adolescents with ADHD yet was consistent across genders (male/female) at 38–39%. Adolescents diagnosed with autism and/or ADHD are at heightened risk for anxiety and depression.
Keywords: Autism, Mental health, Anxiety, Depression, ADHD, Prevalence
Mental health conditions have been reported in connection to both autism (Lai et al., 2019) and attention deficit hyperactivity disorder (ADHD) (Jang et al., 2013), albeit at variable prevalence rates (Hossain et al., 2020). Autism and ADHD are noted to co-occur, however, the Diagnostic and Statistical Manual of Mental Disorders (DSM) precluded a dual Autism Spectrum Disorder (autism) and ADHD diagnosis prior to the 2013 release of the DSM-5 (APA, 2013) leading to a scarcity of research (Leitner, 2014). Since 2013, autism and ADHD have been increasingly reported together, but with emerging concern over the variability of reported rates (Hollingdale et al., 2020; Lai et al., 2014; Rong et al., 2021). School-age autistic youth and youth with ADHD are at high risk for experiencing mental health conditions including anxiety and depression (Hossain et al., 2020; Lai et al., 2019; Zablotsky et al., 2020), yet research identifying the prevalence of mental health conditions among autistic youth and youth with ADHD is limited.
Neurodiversity
The neurodiversity movement has redefined autism and other neurocognitive variations as valuable differences and cultural identities, not disorders to be remedied (e.g. Kapp, 2020; Walker, 2021). Autistic self-advocates, for example, recognize autism as a minority identity and as a disability resulting from a mismatch between autism and social contexts (e.g. den Houting, 2019; Hughes, 2016). Through a neurodiversity lens, recognizing mental health conditions as separate from autism and/or ADHD is essential to providing neurodivergent people with equitable supports provided to neurotypical people. With the recent focus on mental health needs of adolescents through the COVID-19 pandemic (Samji et al., 2022), it seems important to understand the mental health needs of our autistic school-age youth with and without ADHD. Understanding the prevalence of co-occurring autism, ADHD and mental health conditions has the potential to: (1) ensure that the mental health needs of our school-age youth do not go unnoticed or misinterpreted by healthcare providers and educators as other disability label related characteristics (Hossain et al., 2020), and (2) inform the proactive provision of holistic mental health supports, such as community-based care, counseling, and trauma-informed instruction (Gotham et al., 2020; Gunin et al., 2021).
Co-Occurrence of Autism and ADHD
Findings throughout the literature report autism and ADHD co-occurring at varying rates among school-age youth with both autism and ADHD diagnoses more common among males than females (Gargaro et al., 2011). Conducting a secondary analysis of data, Zablotsky et al. (2020) examined the 2014 National Survey of the Diagnosis and Treatment of ADHD and Tourette Syndrome (NS-DATA) and found that 10% of school-age youth aged 12–17 with an ADHD diagnosis have a co-occurring autism diagnosis. Reporting a higher co-occurrence, Hollingdale et al. (2014) conducted two meta-analyses of 22 publications and found that 21% of children and young adults with an ADHD diagnosis, both nationally and internationally, also met the criteria for an autism diagnosis.
Conversely, meta-analyses have also reported upon the prevalence of ADHD among autistic youth and adults. Hossain et al. (2020) conducted an umbrella analysis of meta-analyses on the incidence of ADHD co-occurring among autistic people of all ages nationally and internationally and reported that prevalence rates vary widely, ranging from 26 to 65%. Rong et al. (2021) conducted a meta-analysis of 56 publications (both U.S. and international) and reported the “lifetime prevalence” to be 40.2%. The considerable variation in co-occurring autism and ADHD rates is of concern as variable rates may result in a mismatch between disability specific services provided and actual service needs.
Co-Occurrence of Mental Health Conditions, Autism and ADHD
Despite the link between autism and ADHD, investigations of mental health prevalence are commonly found separate in the research literature. In a study identifying the co-occurrence of other diagnoses along with ADHD, 1.6% of school-age youth were found to have a depression diagnosis and 1.3% an anxiety disorder (Jensen & Steinhausen, 2015). In contrast, an earlier study using a cohort (n = 112) of 10- to 14-year-old children from a population-based survey (Simonoff et al., 2008), reported that 84% of children diagnosed with ADHD also had at least one co-occurring mental health condition including anxiety and depression.
In terms of autism, Lai et al. (2019) conducted a meta-analysis of co-occurring mental health diagnoses in the autistic population. The researchers reviewed 96 studies (national and international) and reported co-occurring autism and mental health conditions at the rates of: anxiety (20%), depression (11%), bipolar disorder (5%), obsessive–compulsive disorder (9%), and schizophrenia (4%). Of note, Havdahl and Bishop (2019) published concern about the data-analysis used by Lai et al. (2019) along with a conclusion that inconsistencies in the methods, conditions and reporting of autism and co-occurring diagnoses throughout the research literature have contributed to a state of variability in reported prevalence. Discussion of prevalence variability is evident throughout the synthesis literature. Hossain et al. (2020), for example, considered the co-occurrence of mental health conditions among autistic people of all ages and countries in an umbrella review and reported significant prevalence variability: eight included reviews reported on anxiety with rates ranging from 1.5% to 54%; six reviews reported on depression with rates ranging from 2.5% to 47.1%; and five reviews reported on suicidal ideation with rates ranging from 10.9% to 66% (Hossain et al., 2020).
Among the few identified studies considering mental health and co-occurring autism and ADHD diagnoses, Zablotsky et al. (2020) found that 42% of school-age youth with co-occurring autism and ADHD diagnoses also had a co-occurring anxiety disorder as reported by their parents. Additional research to understand national mental health prevalence data appears warranted and may further support the development and provision of holistic mental health supports and services for our school-age neurodivergent youth.
Sex Difference and Global Prevalence of Autism
In terms of sex differences, adolescent nonautistic females have been found to be more likely to experience depression (Pontes et al., 2020) and anxiety (Jacques & Mash, 2004). Sex differences among autistic youth in relation to mental health have been less commonly explored, however, as females are less frequently diagnosed as autistic and/or ADHD. Global estimates for autism are difficult to ascertain and compare due to the variability in the data sources and diagnostic criteria over time. Using data from a 2010 Global Study (Vos et al., 2012) and numerous other data sources—985 articles screened and 69 reviewed—Baxter and colleagues (2015) estimated the global prevalence of autism at 7.6 per 1000 persons (1/132). When the prevalence of diagnoses was measured using DSM or ICD codes, the prevalence decreased to 2.4/1000 persons (95% UI 2.3–2.6) (Baxter et al., 2015). In terms of sex differences, males had three times the diagnoses compared to females (3.6 per 1000, 95% UI 3.4–3.9 for males; 1.2 per 1000, 95% UI 1.2–1.3 for females) (Baxter et al., 2015). Data were similar over time (1990 to 2010) and regardless of location, however, it should be noted that most of the early data were from high-income countries only. Sex disparities may be in part a result of autistic females more commonly engaging in the social camouflaging of their autistic characteristics, a strategy of concern as social camouflaging has been linked to increased anxiety and depression (Tubío-Fungueiriño et al., 2020). More research is needed to understand the impact of autism, ADHD and gender on adolescent mental health.
Aims
The present study explores the prevalence of autism, ADHD, anxiety, and depression in a national dataset of US school-age youth, aged 12–17. The Centers for Disease Control and Prevention (CDC, 2022) report anxiety and depression as primary conditions impacting the well-being of adolescents age 12–17. Specifically, the CDC reports 37% of adolescents age 12–17 experience “persistent feelings of sadness or hopelessness” (2022). In alignment with the CDC reporting and the available dataset the present analysis of data from the National Survey of Children’s Health reports upon anxiety and depression among autistic and ADHD adolescents age 12–17. A focus on prevalence rates of anxiety and depression among autistic youth and youth with ADHD may lead to understanding school-age youth experiences, to recognizing mental health needs, and to the provision of proactive holistic supports and services.
This study has four aims: (1) to examine the co-occurring prevalence of autism and ADHD among U.S. adolescents 12–17 years, along with consideration of sex, (2) to examine the prevalence of mental health conditions (e.g., anxiety and depression) co-occurring among U.S. school-age adolescents 12–17 years with neither autism nor ADHD, ADHD no autism, autism no ADHD, and both autism and ADHD, (3) to examine sex differences in the prevalence of anxiety and depression among US adolescents stratified by autism and ADHD, and (4) to estimate additive interactions between autism and ADHD on anxiety and depression separately among male and female US adolescents 12 -17 years.
Taken together, these analyses investigate the extent to which autism and ADHD co-occur among US adolescents and the extent to which autism and ADHD jointly are associated with increased anxiety and depression among US adolescents. To our knowledge there is a scarcity of research using large national data sets to examine the prevalence of co-occurring autism, ADHD, anxiety, and depression among school-age youth. An investigation of national prevalence rates can support the prioritization of understanding and resources for youth with co-occurring diagnoses.
Methods
Dataset
This research used four years of data from the National Survey of Children’s Health (NSCH) (2016–2019) (CAHMI, 2022). The NSCH is an annual cross-sectional survey that is nationally representative of US children zero to seventeen years. The survey is administered by the Census Bureau and sponsored by the Maternal and Child Health Bureau of the Health Resources and Services administration (HRSA) (US Census Bureau, 2022). The data were downloaded from the website maintained by the Children and Adolescent Health Measurement Initiative (CAHMI) (CAHMI, 2019, 2021). A concatenated dataset was prepared with data from the survey years 2016 to 2019 (n = 131,774). (Note: The number of children ages 12—17 in this dataset, n = 54,434). For this research we restricted analyses to school-age youth who were between the ages of 12 and 17 (both inclusive) whose adult household respondents completed the SCH-T3 survey.
NSCH randomly samples US households and administers surveys by mail, the telephone, or the Web. This survey oversamples children ages zero to five, and those with special health care needs. Documentation of the NSCH sampling design, data collection methodology, and variables measured are available elsewhere (CAHMI, 2022; US Census Bureau, 2022). The NSCH contains various items that measure the child’s physical and mental health, access to quality health care as well as the child’s family, neighborhood, social, and school context. The nationally representative NSCH datasets contain sampling design variables and sample weights (to adjust for nonresponse and for oversampling); these sampling design variables and sample weights need to be used for the estimation of population statistics.
Study Variables
Autism
Survey respondents who completed the SCH T3 survey (on behalf of a child 12 to 17 years old) were asked, “Has a doctor or other health care provider EVER told you that this child has Autism or Autism Spectrum Disorder (autism)? Include diagnoses of Asperger’s Disorder or Pervasive Development Disorder (PDD).” If the household respondent answered “Yes” to this question, the child was coded as “Yes” for autism. If the household respondent answered “No” to this question, the child was coded as “No” for autism.
ADHD
Survey respondents were asked, “Has a doctor or other health care provider EVER told you that this child has Attention Deficit Disorder or Attention Deficit/Hyperactivity Disorder, that is ADD or ADHD?” Responses were coded “Yes” or “No” for ADHD.
Anxiety
Survey respondents were asked, “Has a doctor or other health care provider EVER told you that this child has Anxiety Problems?” Responses were coded “Yes” or “No” for anxiety.
Depression
Survey respondents were asked, “Has a doctor or other health care provider EVER told you that this child has Depression?” Responses were coded “Yes” or “No” for depression.
The other variables used for this research include sex, age, and race/ethnicity. Sex was recorded in the dataset as binary: male or female. The race/ethnicity variable used for analyses had 4 categories, non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Other (the latter included everyone not in one of the three previous categories). Age was recorded as years. For analytic purposes, autism, ADHD, anxiety, depression, sex, age, and any two-way interactions were coded as categorical variables.
Analyses
For this research, multi-year analyses were performed as described (US Census 2021). Multivariate analyses were performed with R and the R survey package, which incorporate the sampling design variables and sampling weights and generate nationally representative weighted estimates (Lumley, 2020; R Core Team, 2020). The R survey package function, “svypredmeans,” was used to estimate average predicted marginal percentages, and the R survey package function, “svycontrast,” was used to estimate adjusted risk differences, and their respective confidence intervals as described (Bieler et al., 2010; Lumley, 2018) (Note: White = Non-Hispanic White, Black = Non-Hispanic Black, other = Non-Hispanic other).
Rationale for Estimation of Additive Interactions and Average Marginal Percentages
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines recommend that researchers always report additive interactions (Vandenbroucke et al., 2007). For example, the absence of an additive interaction between autism and ADHD on anxiety implies that the increase in anxiety (difference in the percentage of adolescents with diagnosed anxiety, autism minus no autism) does not vary if the adolescents either have or do not have ADHD. Thus, if RDA is the risk (percentage) difference for the effect of autism on anxiety among persons with ADHD and RDNoA is the risk (percentage) difference for the effect of autism on anxiety among persons without ADHD, then, if there is no additive interaction, the difference, RDA- RDNoA = 0 (Rothman, 2014; Rothman et al., 1980). A significant additive interaction implies that the 95% CI for the difference RDA– RDNoA does not include 0. This research follows STROBE guidelines and reports risk differences and additive interactions. Researchers recommend that average predicted marginal percentages (marginal percentages) be reported when researchers analyze data with binary dependent variables (Bieler et al., 2010; Leeper et al., 2018; Lumley, 2018; Norton et al., 2019). Therefore, this research also reports average predicted marginal percentages (adjusted for covariates); also referred to as adjusted percentages.
Findings
Prevalence and Co-occurrence of Autism and ADHD by Sex among US Adolescents 12–17 years
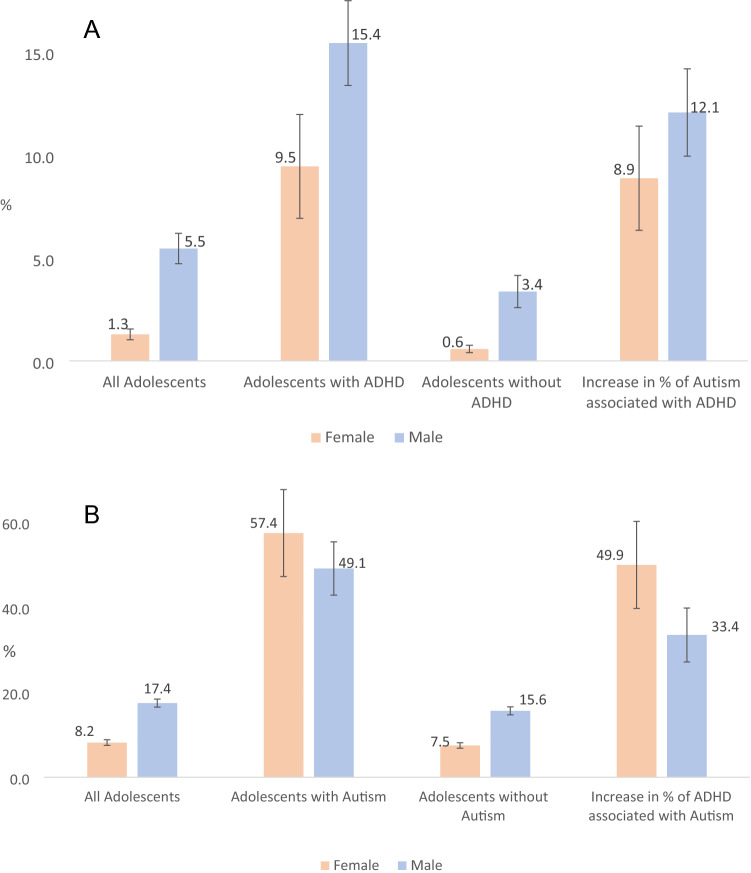
Table 1 and Fig. 1A summarize the prevalence and co-occurrence of autism by sex and ADHD among US adolescents 12–17 years. Overall, autism and ADHD are each more commonly diagnosed among US male adolescents: Among male or female adolescents, autism is significantly more commonly diagnosed among adolescents also diagnosed with ADHD. Among female adolescents the prevalence of autism is 9.5% among those with ADHD and 0.6% among those without ADHD. Among male adolescents the prevalence of autism is 15.4% among those with ADHD and 3.4% among those without ADHD. The increase in prevalence of diagnosed autism associated with ADHD is not significantly different in female adolescents (8.9%) than in male adolescents.
Table 1.
Prevalence and Co-occurrence of Autism and ADHD Among US Adolescents 12–17 Years by Sex (NSCH 2016–2019)
| Sex | Prevalence of autism – % (SE) | Percentage difference in autism prevalence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All adolescents | Adolescents with | ADHD-no ADHD | Interaction: female sex x ADHD | ||||||
| ADHD | No ADHD | RD [95% CI] | t | p | AI_RD [95% CI] | t | p | ||
| Female | 1.3 (0.13) | 9.5 (1.29) | 0.6 (0.09) | 8.9 [6.3, 11.4] | 6.88 | < .001 | −3.2 [−6.5, 0.1] | −1.91 | .057 |
| Male | 5.5 (0.38) | 15.4 (1.05) | 3.4 (0.40) | 12.1 [10.0, 14.2] | 11.17 | < .001 | |||
| Sex | Prevalence of ADHD—% (SE) | Percentage difference in ADHD prevalence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All adolescents | Adolescents with | Autism-no autism | Interaction: female sex x autism | ||||||
| Autism | No autism | RD [95% CI] | t | p | AI_RD [95% CI] | t | p | ||
| Female | 8.2 (0.34) | 57.4 (5.21) | 7.5 (0.33) | 49.9 [39.7, 60.1] | 9.56 | < .001 | 16.5 [4.5, 28.5] | 2.69 | .007 |
| Male | 17.4 (0.48) | 49.1 (3.20) | 15.6 (0.48) | 33.4 [27.1, 39.8] | 10.34 | < .001 | |||
% = average marginal predicted percentage of adolescents with autism or ADHD (Attention Deficit Hyperactivity Disorder), SE = standard error, RD = risk (percentage) difference in prevalence of ASD or ADHD, 95% CI = 95% confidence interval, t = t statistic, p = probability level (significance), AI_RD = additive interaction (RD Female – RD Male), all percentages and statistics weighted to original sample
Fig. 1.
A Average Marginal Percentage of Autism among US Adolescents 12–17 years by Sex and ADHD. B Average Marginal Percentage of ADHD among US Adolescents 12–17 years by Sex and Autism
Table 1 and Fig. 1B summarize the prevalence and co-occurrence of ADHD by sex and autism among US adolescents 12–17 years. Among male or female adolescents, ADHD is also significantly more commonly diagnosed among autistic adolescents (Table 1 and Fig. 1B). Among female autistic adolescents the prevalence of ADHD is 57.4% and among nonautistic females the prevalence of ADHD is 7.5%. Among male autistic adolescents the prevalence of ADHD is 49.1% and among nonautistic males the prevalence of ADHD is 15.6%. The increase in prevalence of diagnosed ADHD associated with autism is significantly greater in female adolescents (49.9%) than in male adolescents. See Table 1 and Fig. 1B.
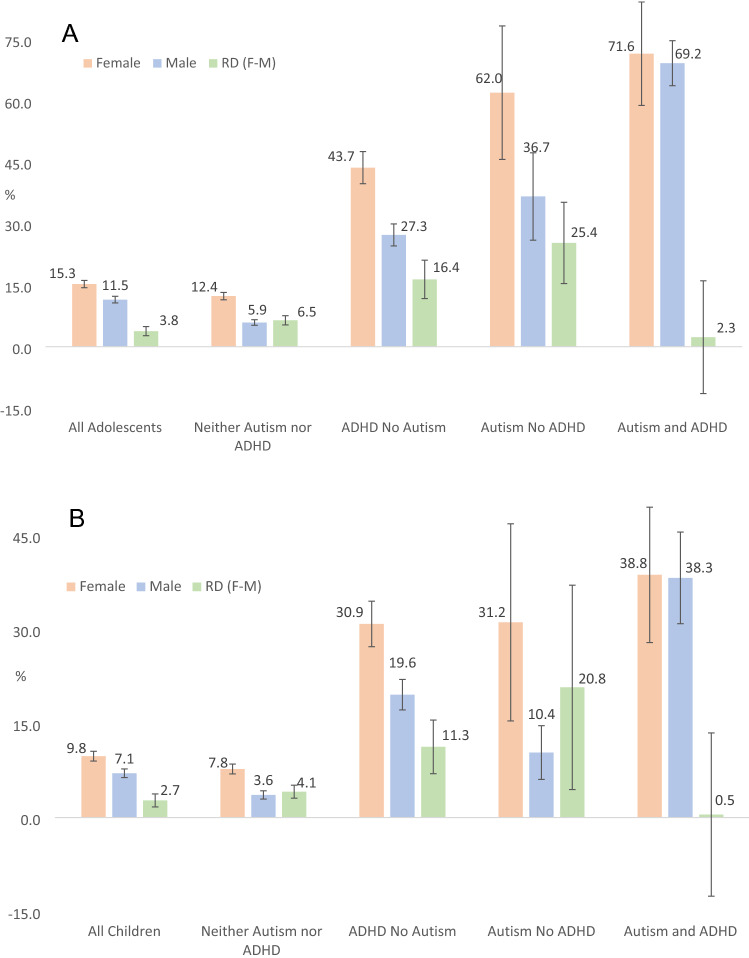
Prevalence of Anxiety by Sex, Autism and ADHD
Table 2 and Fig. 2A summarize the prevalence of anxiety by sex, autism and ADHD among US adolescents 12–17 years. Overall, anxiety was more prevalent among female adolescents (15.3%) than among male adolescents (11.5%). Anxiety was more prevalent among female adolescents than among male adolescents. This includes autistic and nonautistic adolescents with and without ADHD. There was no significant sex difference in the prevalence of anxiety among adolescents diagnosed autistic and ADHD (female = 71.6% versus male = 69.2%).
Table 2.
Prevalence of Anxiety or Depression Among US Adolescents 12–17 Years by Sex, Autism and ADHD (NSCH 2016–2019)
| Sex | All adolescents | Adolescents diagnosed with | |||
|---|---|---|---|---|---|
| Neither autism nor ADHD | ADHD No autism | Autism no ADHD | Autism and ADHD | ||
| Prevalence of anxiety | |||||
| Female—% (SE) | 15.3 (0.45) | 12.4 (0.45) | 43.7 (2.00) | 62.0 (8.32) | 71.6 (6.44) |
| Male—% (SE) | 11.5 (0.42) | 5.9 (0.35) | 27.3 (1.37) | 36.7 (5.44) | 69.2 (2.80) |
| RD [95% CI] | 3.8 [2.6, 5.0] | 6.5 [5.3, 7.6] | 16.4 [11.8, 21.1] | 25.3 [5.9, 44.8] | 2.3 [−11.4, 16.1] |
| t (p) | 6.22 (< .001) | 11.29 (< .001) | 6.88 (< .001) | 2.56 (.011) | 0.33 (.739) |
| Prevalence of depression | |||||
| Female—% (SE) | 9.9 (0.40) | 7.8 (0.40) | 30.9 (1.84) | 31.2 (8.03) | 38.8 (5.52) |
| Male—% (SE) | 7.1 (0.35) | 3.6 (0.34) | 19.5 (1.23) | 10.4 (2.19) | 38.3 (3.74) |
| RD [95% CI] | 2.7 [1.7, 3.8] | 4.2 [3.1, 5.2] | 11.4 [7.1, 15.6] | 20.8 [4.5, 37.1] | 0.5 [−12.6, 13.5] |
| t (p) | 5.15 (< .001) | 7.92 (< .001) | 5.22 (< .001) | 2.50 (.013) | 0.07 (.942) |
% = Average predicted marginal percentage of adolescents who have anxiety or depression, SE = standard error, RD = risk difference
(Female—Male), 95% CI = 95% Confidence Interval, t = t statistic, p = probability (significance level), all percentages and statistics
weighted to original sample
Fig. 2.
A Sex Differences in Average Marginal Percentage of US Adolescents with Anxiety by Autism and ADHD. B Sex Differences in Percentage of US Adolescents with Depression by Autism and ADHD
Prevalence of Depression by Sex, Autism and ADHD
Table 2 and Fig. 2B summarize the prevalence of depression by sex, autism and ADHD among US adolescents 12–17 years. Overall, depression was more prevalent among female adolescents (9.8%) than among male adolescents (2.7%). Depression was more prevalent among females than among males in autistic adolescents with and without ADHD, and nonautistic adolescents with and without ADHD. Depression was most prevalent among autistic adolescents with co-occurring ADHD, however, there was no significant sex difference in the prevalence of depression (38.3% female; 38% male).
Association Between Autism and Anxiety by ADHD Among Male and Female Adolescents
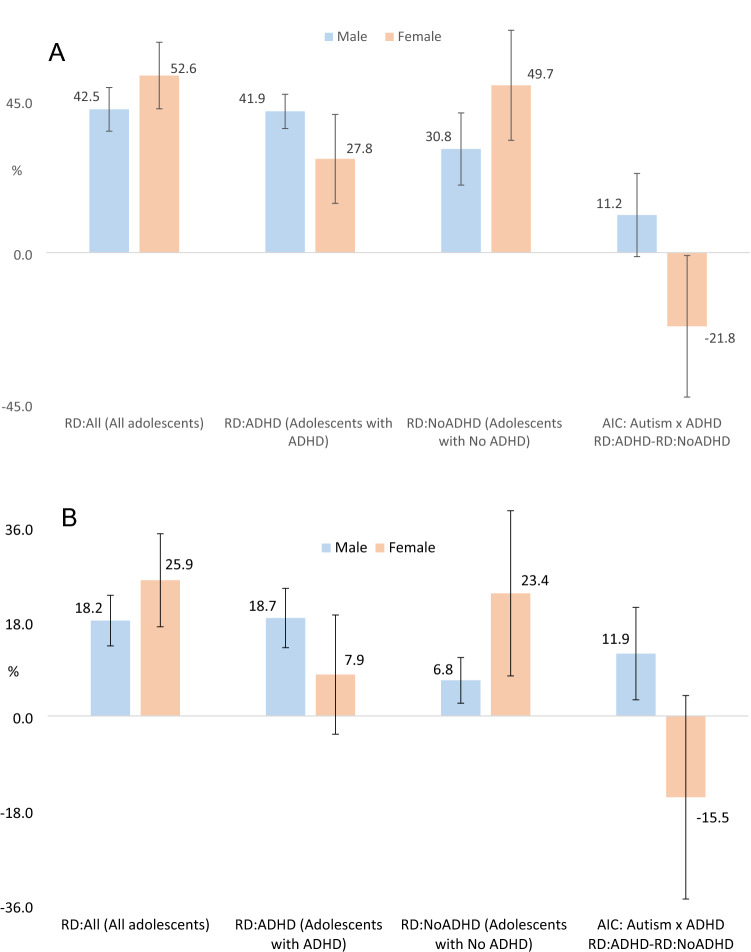
Male Adolescents
Table 3 and Fig. 3A summarize the association between autism and anxiety by ADHD and sex among US adolescents 12–17 years. Among male adolescents, there is a large and significant positive association between autism and anxiety (anxiety diagnosis: autistic males = 51.7%, nonautistic males = 9.2%. Autism is strongly associated with an increase in anxiety in male adolescents with ADHD (anxiety diagnosis: autistic and ADHD males = 69.2%, nonautistic and ADHD males = 27.3%. Autism is also strongly associated with an increase in anxiety in male adolescents without ADHD (anxiety diagnosis: autistic males without ADHD = 36.7%, nonautistic males without ADHD = 5.9%. There was no significant additive interaction between autism and ADHD among male adolescents; the risk difference (increase) in anxiety associated with autism was not significantly greater among males with ADHD (41.9%) than among males without ADHD (30.8%).
Table 3.
Association between Autism and Anxiety or Depression by ADHD Among Male and Female US Adolescents 12–17 Years
| ADHD | % (SE) | Percentage difference: autism—no autism | Interaction: autism x ADHD | |||||
|---|---|---|---|---|---|---|---|---|
| Autism | No autism | RD [95%CI] | t | p | AIC_RD [95%CI] | t | p | |
| Prevalence of Anxiety | ||||||||
| Male Adolescents | ||||||||
| All | 51.7 (3.28) | 9.2 (0.37) | 42.5 [36.1, 49.0] | 12.89 | < .001 | |||
| ADHD | 69.2 (3.74) | 27.3 (1.37) | 41.9 [35.9, 48.0] | 13.51 | < .001 | 11.1 [−1.2, 23.5] | 1.77 | .076 |
| No ADHD | 36.7 (5.44) | 5.9 (0.35) | 30.8 [20.1, 41.5] | 5.63 | < .001 | |||
| Female adolescents | ||||||||
| All | 67.3 (5.02) | 14.7 (0.45) | 52.6 [42.7, 62.4] | 10.44 | < .001 | |||
| ADHD | 71.6 (6.44) | 43.7 (2.00) | 27.8 [14.6, 41.1] | 4.13 | < .001 | −21.8 [−42.8, −0.8] | −2.04 | .042 |
| No ADHD | 62.0 (8.32) | 12.4 (0.45) | 49.7 [33.4, 66.0] | 5.97 | < .001 | |||
| Prevalence of depression | ||||||||
| Male adolescents | ||||||||
| All | 24.3 (2.43) | 6.1 (0.35) | 18.2 [13.3, 23.0] | 7.37 | < .001 | |||
| ADHD | 38.3 (3.74) | 19.6 (1.24) | 18.7 [11.0, 26.3] | 4.77 | < .001 | 11.9 [3.1, 20.7] | 2.65 | .008 |
| No ADHD | 10.4 (2.19) | 3.6 (0.34) | 6.8 [2.4, 11.1] | 3.04 | .002 | |||
| Female adolescents | ||||||||
| All | 35.3 (4.51) | 9.4 (0.40) | 25.9 [17.0, 34.8] | 5.73 | < .001 | |||
| ADHD | 38.8 (5.52) | 30.9 (1.85) | 7.9 [−3.5, 19.2] | 1.36 | .175 | −15.6 [−35.0, 3.9] | −1.57 | .116 |
| No ADHD | 31.2 (8.03) | 7.8 (0.40) | 23.4 [7.7, 39.2] | 2.91 | .004 | |||
% = Average predicted marginal percentage of male (female) adolescents who had anxiety or depression adjusted for Age, Race, and Survey Year, SE = Standard error of estimate, RD = Risk Difference (Autism—No Autism), 95% CI = 95% Confidence Interval, t = t statistic, p = probability (significance level), AIC_RD = Additive Interaction Contrast, all percentages and statistics weighted to original sample
Fig. 3.
A Association Between Autism and Anxiety Stratified by ADHD and Sex. B Association between Autism and Depression Stratified by ADHD and Sex
Female Adolescents
Among female adolescents, there is also a large and significant positive association between autism and anxiety (anxiety diagnosis: autistic females = 67.3%, nonautistic females = 14.7%. Autism is strongly associated with an increase in anxiety in female adolescents with ADHD (anxiety diagnosis: autistic females with ADHD = 71.6%, nonautistic females with ADHD = 43.7%. Autism is also strongly associated with anxiety in female adolescents without ADHD (autistic females with and without ADHD = 62.0%, nonautistic females without ADHD = 12.4%. There was a significant negative additive interaction between autism and ADHD among female adolescents; the risk difference in anxiety associated with autism was significantly smaller among females with ADHD (27.8%) than among females without ADHD (48.7%).
Association Between Autism and Depression by ADHD among Male and Female Adolescents
Male Adolescents
Table 3 and Fig. 3B summarize the association between autism and depression by ADHD and sex among US adolescents 12–17 years. Among male adolescents, there is a large and significant association between autism and depression (depression diagnosis: autistic males = 24.3%, nonautistic males = 6.1%. Autism is strongly associated with depression in male adolescents with ADHD (autistic males with ADHD = 38.3%, nonautistic males with ADHD = 19.5%. Autism is also strongly associated with depression in male adolescents without ADHD (autistic males without ADHD = 10.4%, nonautistic males without ADHD = 3.6%. There was a significant positive additive interaction between autism and ADHD among male adolescents; the risk difference in depression associated with autism was significantly greater among males with ADHD (18.7%) than among males without ADHD (6.8%).
Female Adolescents
Among female adolescents, there is also a large and significant association between autism and depression (depression diagnosis: autistic females = 35.3%, nonautistic females = 9.4%. Autism is not significantly associated with depression in female adolescents with ADHD (autistic females with ADHD = 38.8%, nonautistic females with ADHD = 30.9%. Autism, however, is significantly associated with depression in female adolescents without ADHD (autistic females without ADHD = 31.2%, nonautistic females without ADHD = 7.8%. There was no significant negative additive interaction between autism and ADHD among female adolescents; the risk difference in depression associated with autism was not significantly smaller among females with ADHD (7.9%) than among females without ADHD (23.4%).
Discussion
Key Findings
High Prevalence of Co-Occurring Autism and ADHD
Previous research by Zablotsky and colleagues (2020) estimated that 10% of adolescents aged 12–17 with ADHD have a co-occurring autism diagnosis. The present research aligns with these findings but further identifies the significant variation by sex with 9.5% of females and 15.4% of males diagnosed with ADHD and autism. Most notably, over half of autistic females (57.4%) and nearly half of autistic males (49.1%) are also diagnosed with ADHD, compared to 7.5% of nonautistic females and 15.6% of nonautistic males.
Increasing Prevalence of Co-Occuring Anxiety in either Autism or ADHD
The results of the present study suggest an increasing trend in anxiety among youth with co-occurring autism and ADHD. While Zablotsky et al. (2020) report anxiety of youth from the 2014 national survey at a concerning rate of 42%, results of the present study report anxiety of youth from the 2016–2019 national dataset even higher. Female autistic students with ADHD had the highest co-occurrence of anxiety at an alarming 72%, a six-fold increase when compared to anxiety in 12% of those without autism or ADHD diagnoses, followed by autistic females with no ADHD at 62%. Among autistic male students with ADHD, 69% experienced co-occurring anxiety, twelve-times the prevalence of anxiety when compared to 6% of nonautistic males without ADHD. Autistic males without ADHD had co-occurring anxiety at 37%.
A diagnosis of ADHD without autism was also notable in its high prevalence of co-occurring anxiety: 44% among females (compared to 12% of those with neither autism nor ADHD diagnoses); 27% among males (compared to 5.9% of those with neither autism nor ADHD diagnoses). Similarly, Zablotsky et al. (2020) report co-occurring anxiety in youth with ADHD (no autism) at 22.3%. Of note, females have higher co-occurring mental health support needs across all groups. Our results align with van Steensel and colleagues’ earlier study (2013) in which autistic youth (7–18 years) had higher rates of anxiety compared to those with ADHD.
This is the first study to our knowledge that identifies the surprisingly high prevalence of anxiety in male and female autistic adolescents with ADHD (69–72%) and in female autistic adolescents without ADHD (62%). Note that the prevalence of anxiety among autistic adolescents with ADHD does not really vary by sex (72% versus 69%). In contrast the prevalence of anxiety among nonautistic adolescents without ADHD is roughly twice as high among females than among males (12% versus 6%). This is the also the first study to our knowledge that identifies the surprisingly high prevalence of depression in male and female autistic adolescents with ADHD (38% to 39%) and in female autistic adolescents without ADHD (31%). Note that the prevalence of depression among autistic adolescents with ADHD does not really vary by sex (39% versus 38%). In contrast the prevalence of depression among non-autistic adolescents without ADHD is roughly twice as high among females than among males (8% versus 4%). Estimation of additive interaction effects enabled us to show that joint effects of autism and ADHD on anxiety or depression varied by sex.
High Prevalence of Depression Among Youth with both Autism and ADHD
Male and female adolescents with co-occurring autism and ADHD both had a high prevalence of depression with no significant difference by sex (Males = 38.3%; Females = 38.8%). Notably, autistic males with ADHD had ten-fold the increased prevalence in depression compared to depressed nonautistic males without ADHD (38.3% compared to 3.6%). Autistic females with ADHD had nearly five-fold the increased prevalence in depression compared to nonautistic females without ADHD (38.8% compared to 7.8%). To our knowledge this is addressing an important gap in the literature representing the stark differences in depression diagnosis in those with co-occurring autism and ADHD compared to those without. Additionally, findings address an important gap in the literature representing the stark differences overall and by sex in depression diagnosis in those with co-occurring autism and ADHD compared to those without.
Implications for Practice
The increasing prevalence of anxiety and depression among school-age autistic youth with and without ADHD identified in the present study has implications for healthcare providers, parents and educators. Specifically, findings align with the need identified by Hossain et al. (2020) to proactively identify mental health needs of our autistic and ADHD youth at the onset and not to misinterpret symptoms of anxiety and depression as other disability related characteristics. Findings support a need to educate health-care providers, parents and educators about identifying mental health needs and providing holistic supports. Examples of holistic mental health supports recommended for autistic youth with and without ADHD in the research literature include community-based care, trauma-informed instruction (Gotham et al., 2020; Gunin et al., 2021), exercise (Spratt et al., 2018), counseling, cognitive behavior therapy, emotional support animals, mentoring programs, online resources, and support groups provided with consideration of service delivery modalities preferred by the individual (Kuder et al., 2021).
Given the high co-occurrence of mental health conditions with autism and ADHD and the potential negative impact on social and daily living, a high index of suspicion for anxiety and depression is important for every child diagnosed with autism or ADHD. Broader mental health screening practices for children diagnosed with autism to identify co-occurring ADHD is justified (Antshel et al., 2019; Antshel & Russo, 2016). Identifying and treating anxiety and depression early may result in better outcomes, for example related to social functioning (Hillman, 2020; McGillivray, 2014) or in the area of academic performance also found to be impacted by mental health conditions (Kuder et al., 2021).
Death by suicide as the second leading cause of death among adolescents (Hedegaard et al., 2021) identifies the importance of early identification of anxiety and depression in autistic adolescents with ADHD as even more important. Furthermore, recent findings from a Danish national study estimated that autistic individuals have a higher rate of both suicide attempts and death by suicide, and this rate further increases if a person had a psychiatric co-morbidity (Adjusted Incident Rate Ratio [aIRR] of 1.33 compared to 9.27) (Kolves et. al., 2021). Similarly, college medical students (N = 5693) in China found those with self-reported ADHD had higher rates of suicidal ideation (27.5%) and attempts (14.8%) compared to those without ADHD (Shen et al., 2021). In contrast to the Kolves et al. study (2021), the suicide attempt risk was independent of other risk factors such as depression and anxiety (Shen et al., 2021).
Autistic youth and young adults report being stigmatized by their diagnoses, report bias, discrimination and a lack of social inclusion leading to the need to mask or camouflage their autism, all of which impacts their mental health (Kuder et al., 2021). Findings call for educators and health care providers to support school-aged youth within education and health-care systems that focus on the strengths of autism, disability as diversity, and self-advocacy skills.
Future Research
This research highlights the importance of positioning autism and ADHD as overlapping yet distinct valuable neurodevelopmental differences that share common co-occurring mental health conditions such as anxiety and depression. Further research is needed to explore this intersection of diagnoses, to identify best practices for screening and to identify holistic supports and services. Due to the heterogeneity of these diagnoses, identifying mental health conditions and providing supports proactively for autistic youth with and without ADHD is complex, compounding the need for participatory research methods recommended by neurodiversity scholars as essential (Fletcher-Watson, 2019).
In the present analysis, sex differences were significant and autistic females experienced increased anxiety and depression. This finding warrants further exploration of associations among autism, mental health and gender especially given that research focused on trans identity reports gender variance as more common among autistics and people with ADHD (Strang et al., 2014) as well as heightened depression and anxiety among autistic people with gender variance (Murphy et al., 2020). While the present study was limited by the available NSCH data categories of male and female, a need emerges for future surveys to expand gender categories and for research around mental health, autism and ADHD to routinely consider intersecting gender identities.
Future research should also explore underlying factors that impact the health outcomes of this population. For example, adolescents with and without autism and ADHD are vulnerable to various forms of victimization such as school bullying, which impacts mental health, including suicidal behaviors (Montes & Halterman, 2007; Pontes et al., 2018). Suicide prevention in this population is a critical area for future research to identify best practices in the clinical, educational and community settings to mitigate this risk factor and improve sense of well-being for adolescents who have been victimized. Future research is warranted to identify best trauma-informed approaches within this population (Langenfeld, 2021).
Future research to explore if factors that impact mental health are exacerbated for autistic individuals and individuals with ADHD is also warranted, including sleep problems (Green et al., 2016; Thomas et al., 2018), lack of physical activity (Must et al., 2014), use of excessive screen time (Dong et al., 2021), social isolation and loneliness (Erzen & Çikrikci, 2018), and poor nutrition (Råstam, 2013).
Maddox and colleagues (2020) found that healthcare workers declined seeing autistic clients for mental health conditions due to misconceptions around supporting autistic people. Findings of the present study strengthen and expand the recommendation of Maddox et al. (2020) for future research to focus on training healthcare workers and educators in how to recognize mental health conditions of autistic youth with and without ADHD and in providing related individualized proactive and holistic supports.
Limitations
This research using the National Survey of Children’s Health has several limitations. As a secondary data analysis, it is limited by the ability to alter, add, or drop questions. The participants in the survey are parents of school-age youth and are not self-reports of the youth, which may risk under-reporting from memory errors or social desirability bias. Furthermore, reporting on anxiety and depression is based on a clinical diagnosis, which may underreport true prevalence of anxiety and depression, especially among those who have lower socioeconomic status or access to health care services. Davidsson et al. (2017) in a small clinical study of adolescents (N = 65) estimated one-third of the adolescents had mental health symptoms not recognized by the parents, especially among males. There is the potential that incorrect diagnoses provided by parents may have inflated or underestimated rates of anxiety, depression, autism and ADHD. In addition, diagnoses of autism, ADHD, anxiety and depression may have been influenced by access to healthcare which is influenced by family income and parental education.
Conclusions
The present study identified heightened rates of anxiety and depression among autistic youth and/or youth with ADHD via a large, nationally representative and generalizable data set.
Most notably, youth with both autism and ADHD have higher levels of anxiety and depression compared to those with autism or ADHD, but not both, which highlights the importance of identifying co-occurring ADHD in autistic adolescence. A major contribution of this paper is the use of additive interactions—recommended by STROBE guidelines—to examine additive impacts of co-occurring autism and ADHD on anxiety and depression among male and female youth. Using this approach, we identified significant differences in these effects in males compared to females. Future research should use statistical measures such as additive interactions to further test these relationships, and identify disparities by sex, race and other determinants of health. This research also strengthens a need to build awareness of co-occurring mental health conditions in neurodivergent school-age youth and to develop ways to educate the healthcare, education and wider community to recognize and support these needs. Research, development and implementation of systems and practices that recognize anxiety, depression and other mental health conditions as separate from autism and/or ADHD, that screen for mental conditions and that provide autistic people with and without ADHD with proactive and holistic mental health supports is recommended.
Author Contributions
AA, NP and MP all contributed to the study conception and design and made substantial contributions to the work. AA and NP prepared the introductions, results and discussion. MP prepared the methods and conducted the data analysis. All authors approved the final manuscript to be published.
Declarations
Conflict of interest
They authors declare they have no conflict of interest. No financial support was given for this research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amy L. Accardo, Email: Accardo@rowan.edu
Nancy M. H. Pontes, Email: Pontesnh@camden.rutgers.edu
Manuel C. F. Pontes, Email: Pontes@rowan.edu
References
- American Psychiatric Association (APA). (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). 10.1176/appi.books.9780890425596.
- Antshel KM, Russo N. Autism spectrum disorders and ADHD: Overlapping phenomenology, diagnostic issues, and treatment considerations. Current Psychiatry Reports. 2019;21(5):1–11. doi: 10.1007/s11920-019-1020-5. [DOI] [PubMed] [Google Scholar]
- Antshel KM, Zhang-James Y, Wagner KE, Ledesma A, Faraone SV. An update on the comorbidity of ADHD and ASD: A focus on clinical management. Expert Review of Neurotherapeutics. 2016;16(3):279–293. doi: 10.1586/14737175.2016.1146591. [DOI] [PubMed] [Google Scholar]
- Baxter A, Brugha T, Erskine H, Scheurer R, Vos T, Scott J. The epidemiology and global burden of autism spectrum disorders. Psychological Medicine. 2015;45(3):601–613. doi: 10.1017/S003329171400172x. [DOI] [PubMed] [Google Scholar]
- Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. American Journal of Epidemiology. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- CAHMI. (2019). 2016–17 Child and Adolescent Health Measurement Initiative (CAHMI). Dataset Downloads. https://www.childhealthdata.org/dataset/download?rq=10048
- CAHMI. (2021). 2018–19 Child and Adolescent Health Measurement Initiative (CAHMI). Dataset Downloads. https://www.childhealthdata.org/dataset/download?rq=10048
- CAHMI. (2022). About the National Survey of Children’s Health (NSCH). https://www.childhealthdata.org/learn-about-the-nsch/NSCH
- Centers for Disease Control and Prevention. Data and statistics on children’s mental health. (June 2022). https://www.cdc.gov/childrensmentalhealth/index.html
- Davidsson M, Hult N, Gillberg C, Särneö C, Gillberg C, Billstedt E. Anxiety and depression in adolescents with ADHD and autism spectrum disorders: Correlation between parent- and self-reports and with attention and adaptive functioning. Nordic Journal of Psychiatry. 2017;71(8):614–620. doi: 10.1080/08039488.2017.1367840. [DOI] [PubMed] [Google Scholar]
- den Houting J. Neurodiversity: An insider’s perspective. Autism. 2019;23(2):271–273. doi: 10.1177/1362361318820762. [DOI] [PubMed] [Google Scholar]
- Dong H-U, Wang B, Li H-H, Yue X-J, Jia F-Y. Correlation between screen time and autistic symptoms as well as development quotients in children with autism spectrum disorder. Frontiers in Psychiatry. 2021;12:619994–619994. doi: 10.3389/fpsyt.2021.619994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzen E, Çikrikci Ö. The effect of loneliness on depression: A meta-analysis. International Journal of Social Psychiatry. 2018;64(5):427–435. doi: 10.1177/0020764018776349. [DOI] [PubMed] [Google Scholar]
- Fletcher-Watson S, Adams J, Brook K, Charman T, Crane L, Cusack J, Pellicano E. Making the future together: Shaping autism research through meaningful participation. Autism. 2019;23(4):943–953. doi: 10.1177/1362361318786721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargaro BA, Rinehart NJ, Bradshaw JL, Tonge BJ, Sheppard DM. Autism and ADHD: How far have we come in the comorbidity debate? Neuroscience & Biobehavioral Reviews. 2011;35(5):1081–1088. doi: 10.1016/j.neubiorev.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Gotham K, Cassidy S, Weiss J. Mental health across the lifespan. Autism. 2020;24(4):805–808. doi: 10.1177/1362361320912132. [DOI] [PubMed] [Google Scholar]
- Green JL, Sciberras E, Anderson V, Efron D, Rinehart N. Association between autism symptoms and functioning in children with ADHD. Archives of Disease in Childhood. 2016;101(10):922–928. doi: 10.1136/archdischild-2015-310257. [DOI] [PubMed] [Google Scholar]
- Gunin GB, Gravino A, Bal., V. H. Advancing mental health supports for autistic postsecondary students: A call for research. Autism in Adulthood. 2021;3(1):30–36. doi: 10.1089/aut.2020.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havdahl A, Bishop S. Heterogeneity in prevalence of co-occurring psychiatric conditions in autism. The Lancet Psychiatry. 2019;6(10):794–795. doi: 10.1016/S2215-0366(19)30326-8. [DOI] [PubMed] [Google Scholar]
- Hedegaard, H. Curtin, S. C., & Warner, M. 2021. NCHS Data Brief: Suicide mortality in the United States, 1999-2019. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db398-H.pdf
- Hillman K, Dix K, Ahmed K, Lietz P, Trevitt J, O’Grady E, Uljarević M, Vivanti G, Hedley D. Interventions for anxiety in mainstream school-aged children with autism spectrum disorder: Asystematic review. Campbell Systematic Review. 2020 doi: 10.1002/cl2.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingdale J, Woodhouse E, Young S, Fridman A, Mandy W. Autistic spectrum disorder symptoms in children and adolescents with attention-deficit/hyperactivity disorder: a meta-analytical review. Psychological Medicine. 2020;50(13):2240–2253. doi: 10.1017/S0033291719002368. [DOI] [PubMed] [Google Scholar]
- Hossain MM, Khan N, Sultana A, Ma P, McKyer ELJ, Ahmed HU, Purohit N. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: An umbrella review of systematic reviews and meta-analyses. Psychiatry Research. 2020;287:112922. doi: 10.1016/j.psychres.2020.112922. [DOI] [PubMed] [Google Scholar]
- Hughes JM. Increasing neurodiversity in disability and social justice advocacy groups. Autistic Self Advocacy Network; 2016. [Google Scholar]
- Jacques HA, Mash EJ. A test of the tripartite model of anxiety and depression in elementary and high school boys and girls. Journal of Abnormal Child Psychology. 2004;32(1):13–25. doi: 10.1023/B:JACP.0000007577.38802.18. [DOI] [PubMed] [Google Scholar]
- Jang J, Matson JL, Williams LW, Tureck K, Goldin RL, Cervantes PE. Rates of comorbid symptoms in children with ASD, ADHD, and comorbid ASD and ADHD. Research in Developmental Disabilities. 2013;34(8):2369–2378. doi: 10.1016/j.ridd.2013.04.021. [DOI] [PubMed] [Google Scholar]
- Jensen CM, Steinhausen HC. Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders. 2015;7(1):27–38. doi: 10.1007/s12402-014-0142-1. [DOI] [PubMed] [Google Scholar]
- Kapp SK, editor. Autistic community and the neurodiversity movement: Stories from the frontline. Springer Nature; 2020. [Google Scholar]
- Kolves K, Fitzgerald C, Nordentoft M, Wood SJ, Erlangsen A. Assessment of suicidal behaviors among individuals with autism spectrum disorder in Denmark. JAMA Network Open. 2021;4(1):e2033565. doi: 10.1001/jamanetworkopen.2020.33565. [DOI] [PubMed] [Google Scholar]
- Kuder SJ, Accardo AL, Woodruff J. College Success for students on the autism spectrum: A neurodiversity perspective. Stylus; 2021. [Google Scholar]
- Lai MC, Kassee C, Besney R, Bonato S, Hull L, Mandy W, Szatmari P, Ameis SH. Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. The Lancet Psychiatry. 2019;6(10):819–829. doi: 10.1016/S2215-0366(19)30289-5. [DOI] [PubMed] [Google Scholar]
- Lai M-C, Lombardo MV, Baron-Cohen S. Autism. Lancet. 2014;383:896–910. doi: 10.1016/S0140-6736(13)61539-1. [DOI] [PubMed] [Google Scholar]
- Langenfeld A, Kroupina M, Palmer A, Gustafson K, Augustyn M. Importance of trauma-informed practice in evaluation of children diagnosed with autism spectrum disorder. Journal of Developmental and Behavioral Pediatrics. 2021;42(8):690–693. doi: 10.1097/DBP.0000000000000999. [DOI] [PubMed] [Google Scholar]
- Leeper, T. J., Arnold, J., & Arel-Bundock, V. (2018). Margins: marginal effects for model objects. R Package Version 0.3, 23.
- Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children–what do we know? Frontiers in Neuroscience. 2014 doi: 10.3389/fnhum.2014.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley, T. S. (2018). Predictive margins like SUDAAN does them. GitHubGist. https://gist.github.com/tslumley/2e74cd0ac12a671d2724
- Lumley, T. S. (2020). survey: Analysis of complex survey samples. R package (R package version 4.0) [R]. https://CRAN.R-project.org/package=survey
- Maddox BB, Crabbe S, Beidas RS, Brookman-Frazee L, Cannuscio CC, Miller JS, Nicolaidis C, Mandell DS. "I wouldn't know where to start": Perspectives from clinicians, agency leaders, and autistic adults on improving community mental health services for autistic adults. Autism. 2020;24(4):919–930. doi: 10.1177/1362361319882227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGillivray JA, Evert HT. Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Autism and Developmental Disorders. 2014;44(8):2041–2051. doi: 10.1007/s10803-014-2087-9. [DOI] [PubMed] [Google Scholar]
- Montes G, Halterman JS. Bullying among children with autism and the influence of comorbidity with ADHD: A population-based study. Ambulatory Pediatrics. 2007;7(3):253–257. doi: 10.1016/j.ambp.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Murphy J, Prentice F, Walsh R, Catmur C, Bird G. Autism and transgender identity: Implications for depression and anxiety. Research in Autism Spectrum Disorders. 2020;69:101466. doi: 10.1016/j.rasd.2019.101466. [DOI] [Google Scholar]
- Must A, Phillips SM, Curtin C, Anderson SE, Maslin M, Lividini K, Bandini LG. Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism. 2014;18(4):376–384. doi: 10.1177/1362361313479039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton EC, Dowd BE, Maciejewski ML. Marginal effects—quantifying the effect of changes in risk factors in logistic regression models. JAMA. 2019;321(13):1304–1305. doi: 10.1001/jama.2019.1954. [DOI] [PubMed] [Google Scholar]
- Pontes NM, Ayres CG, Pontes MCF. Additive interactions between gender and bullying victimization on depressive symptoms and suicidality: Youth risk behavior survey 2011–2015. Nursing Research. 2018 doi: 10.1097/NNR.0000000000000310. [DOI] [PubMed] [Google Scholar]
- Pontes NM, Ayres CG, Pontes MC. Trends in depressive symptoms and suicidality: Youth risk behavior survey 2009–2017. Nursing Research. 2020;69(3):176–185. doi: 10.1097/NNR.0000000000000424. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing (4.0) [Mac OSX]. R Foundation for Statistical Computing. https://www.R-project.org/
- Råstam M, Täljemark J, Tajnia A, Lundström S, Gustafsson P, Lichtenstein P, Gillberg C, Anckarsäter H, Kerekes N. Eating problems and overlap with ADHD and autism spectrum disorders in a nationwide twin study of 9- and 12-year-old children. The Scientific World. 2013 doi: 10.1155/2013/315429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rong Y, Yang CJ, Jin Y, Wang Y. Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: A meta-analysis. Research in Autism Spectrum Disorders. 2021;83:101759. doi: 10.1016/j.rasd.2021.101759. [DOI] [Google Scholar]
- Rothman KJ. Six persistent research misconceptions. Journal of General Internal Medicine. 2014;29(7):1060–1064. doi: 10.1007/s11606-013-2755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Walker AM. Concepts of interaction. American Journal of Epidemiology. 1980;112(4):467–470. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, Snell G. Mental health impacts of the COVID-19 pandemic on children and youth–a systematic review. Child and Adolescent Mental Health. 2022;27(2):173–189. doi: 10.1111/camh.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y, Chan BM, Huang C, Cui X, Liu J, Lu J, Pate M, Verrico CD, Luo X, Zhang XY. Suicidal behaviors and attention deficit hyperactivity disorder (ADHD): A cross-sectional study among Chinese medical college students. BMC Psychiatry. 2021;21:258. doi: 10.1186/s12888-021-03247-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Spratt, E., Mercer, M. A., Grimes, A., Papa, C., Norton, J., Serpe, A., & Newton, J. (2018). Translating benefits of exercise on depression for youth with autism spectrum disorder and neurodevelopmental disorders. Journal of Psychology and Psychiatry, 2, 109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602550/ [PMC free article] [PubMed]
- Strang JF, Kenworthy L, Dominska A, Sokoloff J, Kenealy LE, Berl M, Wallace GL. Increased gender variance in autism spectrum disorders and attention deficit hyperactivity disorder. Archives of Sexual Behavior. 2014;43(8):1525–1533. doi: 10.1007/s10508-014-0285-310.1007/s10508-014-0285-3. [DOI] [PubMed] [Google Scholar]
- Thomas S, Lycett K, Papadopoulos N, Sciberras E, Rinehart N. Exploring behavioral sleep problems in children with ADHD and comorbid autism spectrum disorder. Journal of Attention Disorders. 2018;22(10):947–958. doi: 10.1177/1087054715613439. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. (2021, August 30). National Survey of Children’s Health: Guide to Multi-Year Analysis. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/NSCH-Guide-to-Multi-Year-Estimates.pdf
- US Census Bureau. (2022, May 22). National Survey of Children’s Health (NSCH). Census.Gov. https://www.census.gov/nsch
- van Steensel FJA, Bögels S, de Bruin E. Psychiatric comorbidity in children with autism spectrum disorders: A comparison with children with ADHD. Journal of Child and Family Studies. 2013;22(3):368–376. doi: 10.1007/s10826-012-9587-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, STROBE Initiative Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. PLOS Medicine. 2007;4(10):e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T, Naghavi M, Michaud C, Ali MK, Anderson LM, Atkinson C, Baddour LM, Baxter A, Bennett D, Bhalla K, Bhandari B, Black JA, Blore JD, Bourne R, Brayne C, Brooker S, Buchbinder R, Calabria B, Canter CE, Coffeng LE. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the global burden of disease study 2010. The Lancet (british Edition) 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, N. (2021). Neuroqueer heresies: Notes on the neurodiversity paradigm, autistic empowerment, and postnormal possibilities. Autonomous Press, LLC. https://neuroqueer.com/neuroqueer-heresies/
- Zablotsky B, Bramlett MD, Blumberg SJ. The co-occurrence of autism spectrum disorder in children with ADHD. Journal of Attention Disorders. 2020;24(1):94–103. doi: 10.1177/1087054717713638. [DOI] [PMC free article] [PubMed] [Google Scholar]