Abstract
Objective
Immigrant health discussions often focus on acculturation and omit discussions on historical events that may underlie health differences among immigrant older adults. This paper provides a historical overview of immigration policy and flows to the U.S. and examines insurance access and health difficulties by sending country.
Methods
We analyzed the “Immigrants Admitted to the United States, Fiscal Years 1972–2000” and 2015–2019 American Community Survey datasets to examine the number of admitted immigrants, sociodemographic profiles for current immigrant older adults, and the predicted probabilities of health insurance access and health difficulties.
Results
Our results highlight alignment of immigration flows with immigration legislation and vast heterogeneity in migration, health, and healthcare access of immigrants by sending country.
Discussion/Implications
Public health practitioners must consider how historical events and social factors contribute to the healthcare access and health of immigrant populations, as demographic shifts will require interventions that promote equitable healthy aging.
Keywords: immigration, life course, health insurance, health difficulties, older adults
Introduction
Accounting for an estimated 45 million people in 2018, the immigrant population in the United States (U.S.) is expected to double to 105 million by 2065 (Budiman, 2020). Related to this trend, the population of those 65 years and older is expected to grow from 56.1 million to 94.7 million by 2060, to be 23% of the U.S. population (Vespa et al., 2018). The older adult population in the U.S. is also rapidly diversifying and the share of racial/ethnic minority adults is expected to be a “majority” by 2060 (Alba, 2018; Vespa et al., 2018).
Given these demographic shifts, recent scholarship has called to expand research examining the experiences of older immigrant adults (Flores Morales, 2021; Ma et al., 2021). For Latino immigrant older adults, research has highlighted immigrant health advantages in depressive symptoms (Bowen & Ruch, 2015), health and disability (Downer et al., 2016), and life satisfaction (Calvo et al., 2017) relative to White adults. The health of immigrant older adults are further heterogeneous when examining differences by disaggregated racial/ethnic groups (i.e., examining health by Cuban and Dominican ethnicity vs. the broad Hispanic/Latinx group). Hooker et al. (2018) found that Mexican, Puerto Rican, and Cuban older adults had higher depressive symptoms compared to their non-Hispanic White counterparts. Filipino, Asian Indian, and Native Hawaiian and Pacific Islander (NH/PI) older adults also had higher depressive symptoms relative to older White adults. These data would have otherwise been masked if they were examined by the aggregate racial/ethnic groups. Similarly, Đoàn et al. (2021) found vast differences in cardiovascular disease (CVD) outcomes among older adults, where NH/PI older adults had the greatest risk of reporting worst CVD outcomes relative to Asian American ethnic groups and White adults. There are also racial/ethnic disparities observed in health insurance and health services utilization where older adults of color have greater prevalence of uninsurance and underutilization of healthcare services compared to White adults (Gandhi et al., 2018).
Immigration and the Life Course Perspective
Considering known health disparities and social determinants of health among the aging populations and older adult immigrants, there remains little discussion on immigration experiences. Older adults’ immigration experiences are often discussed in the context of acculturation (i.e., the adoption of U.S. culture and diminishing influence of one’s sending country culture) and immigrant integration (i.e., the process where immigrants and native-born individuals become more like each other). Acculturation and integration are typically measured using nativity status, time in the U.S. or English proficiency (Bacong & Menjívar, 2021; Bacong & Sohn, 2021; Bowen & Ruch, 2015; National Academies of Sciences et al., 2016).
Although it is important to focus on the current health and health status of older adults, it is equally important to consider the historical and migration circumstances of immigrants that underlie current and existing health inequities. The life course perspective offers an important framework to examine the social, economic, and political contexts that positively or negatively impact health outcomes and well-being over different life stages. Elder (1994) highlights the importance of considering historical and cultural events when examining biological age, to emphasize the importance of human development and aging. Prior research that has focused on the intersections between immigration and the life course have centered upon the migration experience (Gong et al., 2011; Torres & Young, 2016) as well as age and aging (Brown, 2018; Guo et al., 2021). For example, Gong et al. (2011) examined “age effects” of immigration, noting that those who immigrated to the U.S. as adolescents without clear migration goals had worse psychological distress compared to those who immigrated as children. Moreover, adult immigrants who migrated with clear goals and prepared beforehand had less psychological distress compared to those who migrated as children or adolescents. Guo et al. (2021) also note the importance of one’s age during migration, finding that those who migrated after the age of 50 years old had worse cognitive health compared to younger migrants. Brown (2018) provides a nuanced perspective of examining aging of older adult immigrants, noting that White immigrants maintain health advantage while they age while Black and Mexican immigrants’ health disadvantage intensifies with age.
Historical context is another important aspect to consider in the life course perspective. We focus on the historical context of the experiences of older adult immigrants. For example, major historical or social events, such as World War II and the Vietnam War, established temporal cohorts of adults (e.g., Baby Boomers), who had differential experiences and responses to biological and social exposures, which then impact their health and well-being.
We use the life course perspective to examine immigration-related factors like immigrant legal status, country of origin, or the historical context of migration, that affect health advantages and disadvantages that shape health inequalities and healthcare needs and utilization among immigrant older adults. The life course perspective guides our work on migration as we consider how the dynamic and cumulative effects of biological and social exposures’ impact and structure individual-level opportunities and disadvantages. Considering immigrants’ country of origin is especially important, given that immigration legislation may facilitate entry of immigrants from certain countries while restricting immigrants of other countries. Examining immigration with a life course lens can improve our understanding of how major world events and policies have impacted the health trajectories of the aging populations, particularly among immigrant older adults and given the dramatic changes in U.S. immigration policies over the last 60 years.
This paper examines how the social and political systems individuals exit (i.e., country of origin) and enter (i.e., U.S.) impact the immigrant experience and have potential ripple effects on health across the entire life course (Torres & Young, 2016). First, we use historical visa records to 1) describe immigration flows and identify immigration policies that would affect immigrants who immigrated between 1971 and 2000 and would be 65–85 years old in 2019; and 2) characterize the sociodemographic profiles of these older adult immigrants. Finally, we use nationally representative survey data to provide plausible health insurance access and health profiles of this group of older adult immigrants by country of origin. We aim for this paper to provide a foundation to understand the long-term effects of immigration legislation on health, healthcare access, and well-being.
Methods
Data
We conducted separate analyses of the Inter-university Consortium for Political and Social Research (ICSPR) “Immigrants Admitted to the United States, Fiscal Years 1972–2000 (ICPSR 37688)” (Kossoudji, 2020) and 2015–2019 American Community Survey (ACS) 5-year estimates (Ruggles et al., 2021). In our first analysis, we use the ICPSR data to provide the historical context to understanding older adult immigrant experiences. The ICPSR dataset contains federal administrative data on all immigrants who were admitted to the U.S. from fiscal years 1971–1972 to 2000–2001. This dataset provides comprehensive immigration data and has detailed information on the time to immigrant admission, visa status, and port of entry.
In our second analysis, we examined the 2015–2019 ACS 5-year estimates to provide plausible socioeconomic and health profiles of the immigrants who arrived in the US during 1971–2000 and would currently be 65–85 years in 2019. The ACS is an annual survey conducted by the Census Bureau of over 3.5 million households and captures social, housing, economic, and demographic characteristics of the US population. We used the 5-year estimates (Ruggles et al., 2021) because it provides the largest sample size and most reliable estimates compared to ACS 1-year and 3-year estimates. At the time of writing, ACS data up to 2019 were available.
To allow for comparisons between both datasets, we restrict the ICPSR and ACS dataset to individuals who would be ages 65–85 years old in the year 2019. We also restrict the ACS data to people who had immigrated between 1971 and 2000. The final analytic sample was 4,702,568 individuals for the ICPSR data and 152,441 individuals for the ACS dataset.
Measures
We examined immigration and demographic variables in the ICPSR dataset. Immigration variables included immigrant’s age of migration, year of migration (1971–1979, 1980–1989, 1990–2000), U.S. presidential administration during migration (from Richard Nixon to Bill Clinton), time for immigrants to obtain lawful permanent residence (LPR), immigration visa category and if they were a principal or derivative visa holder. Time for immigrants to obtain LPR was categorized as: arrived in the U.S. as LPR, 1 year, 2 years, 3–5 years, 6–10 years, 11 years, or more. Immigration visa categories were classified into the following nine groups: Immediate Relative Visa, Family Sponsored Visa, Employment Sponsored Visa, Refugee or Lautenberg Visa, Asylum Seeker or Nicaraguan Adjustment and Central American Relief Act (NACARA) recipient, Other Cuban Visa, Diversity Visa, Born Abroad to U.S. Parents or Amerasian Visa, and Other Visa. “Other Cuban Visa” was kept as a separate category for analysis given its historical significance to U.S. immigration policy. Definitions on each immigration visa category are provided in Table 1. Demographic variables included gender and marital status.
Table 1.
Immigrant Visa Classifications.
| Visa or Immigrant Type | Example Visa Category (if Applicable) | Number of Visas Allotted per Year | Notes |
|---|---|---|---|
| Immediate relative (IR) visa | IR1, IR2, IR3, IH1, IR4, IH4, IR5 CR1, CR2, VI5, IW | Unlimited* | • Spouse, parent, or child (under 18 years old) of current U.S. citizen (U.S. Department of State - Bureau of Consular Affairs, 2022) |
| Family sponsored (F) visa | F1, F2A, F2B, F3, F4 | 226,000 (minimum) | • Children, parents, or siblings of U.S. citizens or lawful permanent residents (U.S. Department of State - Bureau of Consular Affairs, 2022) |
| Employment sponsored visa | E1, E2, E3, E3, E4, E5 | 140,000 | • Permanent immigrants sponsored by employers in the U.S. (U.S. Department of State - Bureau of Consular Affairs, 2022) |
| Refugee visa or Lautenberg visa | Various | Various | • Refugees are individuals who fleeing
their country due to persecution or harm related on the
basis of race, religion, nationality, or affiliation
with a political opinion or social group. • Must apply for “refugee status” prior to arrival in the U.S. • Lautenberg visa-holders represented a special case of refugees who were religious minorities in the former Soviet Union, Estonia, Latvia, or Lithuania (U.S. Citizenship and Immigration Services, 2017) |
| Asylum seeker or NACARA | Various | Not applicable | • Asylum seekers are individuals who
request protection to enter the U.S., but did not apply
in their country of origin • NACARA represents a special case for immigrants and asylum seekers from Guatemala, El Salvador, as well as the former Soviet Union and its holdings (e.g., East Germany, Poland, Yugoslavia) |
| Other Cuban visa | Various | Not applicable | • Former H1 nurses in Cuba and their family |
| Diversity visa | DV | 50,000 | • Immigration visas allotted to individuals from countries with low immigration to the U.S.; typically done via a lottery. (U.S. Department of State—Bureau of Consular Affairs, 2022) |
| Born abroad to U.S. Parents or Amerasian visa | AM1, AM2, AM3 | Not applicable | • Children who were born outside of the
U.S. to U.S. citizens • Amerasian visas represent special case of children who were fathered by U.S. servicemen and Asian nationals during the Korean and Vietnam wars (U.S. Citizenship and Immigration Services, 2022) |
Note. *A total of 480,000 family reunification visas are allotted between IR and F visas. However, visas are allocated to IR visas first, followed by F visa-holders. Asylum seekers do not arrive to the U.S. with a visa, but instead apply to obtain refugee status. NACARA = Nicaraguan Adjustment and Central American Relief Act. “Visa Category” provided is not an exhaustive list of all possible visas.
We focused analysis of the ICPSR data on the top 10 immigrant sending countries to the U.S. in 2016: Mexico, China, India, the Philippines, El Salvador, Vietnam, Cuba, the Dominican Republic, South Korea, and Guatemala (Budiman, 2020). Countries not listed in the top 10 sending countries were grouped as “Other Country” and was the reference category to allow comparisons of the top 10 countries to the general population of immigrants. We expect that countries included in the “Other Country” category are not subject to the same immigration limitations (e.g., long visa processing times) that the top 10 immigrant sending countries experience (e.g., “oversubscribed” countries) (Obinna, 2014, 2020).
In the ACS, we examined immigration, health insurance and access, health difficulties, and sociodemographic variables. Immigration variables included citizenship status (naturalized, non-citizen), English language proficiency, age of migration, year of migration, presidential administration during migration, and country of origin. We examined health insurance coverage (yes, no) and type (private insurance, Medicare, Medicaid, Medicare/Medicaid). We examined each of insurance type separately because participants could have more than one type of insurance, with the exception of individuals with have both Medicare and Medicaid because this population often has additional social and medical needs compared to those with either Medicare or Medicaid (McBride et al., 2020). Medicare is available to all U.S. citizens’ aged 65 years and older and lawful permanent residents who have fulfilled certain residency requirements (Hoffman et al., 2000). Medicaid is available to those who all individuals who are experiencing poverty (Hoffman et al., 2000). We examined seven health difficulties: cognitive, physical, independent living, ability to care for oneself, sensory, sight, and hearing, and if respondents had “any difficulty” based on the seven difficulties. Sociodemographic covariates included age, sex, marital status, educational attainment, and income, as important factors related to health insurance and health difficulties.
Analysis Plan
Using the ICPSR data, we examined the total number of admitted immigrants from 1971 to 2000 and calculated univariate and bivariate distributions of immigration and demographic variables, by the immigrant sending country. Using the ACS data, we provide the univariate distribution of the immigration, health insurance access, health difficulties, and sociodemographic variables, and bivariate associations by country of origin. We conduct multivariable logistic regression to model the associations between country of origin and health insurance access and health difficulties, accounting for immigration and sociodemographic factors. We provide predicted probabilities and applied ACS survey weights to reflect a nationally representative sample of older adult immigrants in 2019. Data analyses were completed using Stata MP Version 17.0 (StataCorp, 2021).
Results
Immigration Legislation and Admitted Immigrants from 1971 to 2000
Table 2 highlights the landscape of select immigration legislation between 1965 and 2014, starting with the 1965 Immigration and Nationality Act that removed country-specific quotas for immigration and expanded immigration from Asia and Latin America to the U.S. U.S. immigration policies have fluctuated between openness for certain immigrant groups (e.g., refugees, skilled workers) and restrictions for other groups (e.g., undocumented immigrants). The 1996 Personal Responsibility and Work Reconciliation Act (PWORA) is especially noteworthy because it created limits on social services and access to healthcare for undocumented immigrants and immigrants with temporary visas (e.g., student and work visas).
Table 2.
Landscape of Immigration-related Legislation and Executive Orders.
| Year, President | Name of Legislation or Executive Order | Policy Description and Impacts on Healthcare Access and Health |
|---|---|---|
| 1965, Lydon B. Johnson (D) | Immigration and Nationality Act (Hart-Cellar Act) | • Both restrictive and inclusive
policy • Replaced the National Origins Formula immigration quota system with a seven-category preference system; prioritized visas based on family preferences (e.g., individuals who had relatives who were US citizens, legal permanent residents) and skill-based preferences |
| 1975, Gerald Ford (R) | Indochina Migration and Refugee Assistance Act | • Inclusive immigration policy • Allowed refugees from Cambodia and Vietnam to enter the US at the end of the Vietnam War; amended in 1976 to allow refugees from Laos to enter the US |
| 1976, Gerald Ford (R) | Immigration and National Act Amendments of 1976 | • Both restrictive and inclusive
policy • Extended the visas ceiling to 20,000 immigrants per country for North and South American and modified the preference system; specifically impacted Mexico with the 20,000-visa cap |
| 1978, Jimmy Carter (D) | Immigration and National Act Amendments of 1978 | • Inclusive immigration policy • Increased the annual visas ceiling to 290,000 immigrants and implemented uniform preference system for all countries |
| 1980, Jimmy Carter (D) | Refugee Act of 1980 | • Inclusive immigration policy • Created general policy for refugees; refugees were removed from the immigration preference system which increased the number of refugees entering the US; created the Federal Refugee Resettlement Program to assist with refugee resettlement and economic |
| 1986, Ronald Reagan (R) | Immigration Reform and Control Act (Simpson-Mazzoli Act or IRCA) | • Both restrictive and inclusive
policy • Created a pathway to permanent residency to unauthorized immigrant workers (e.g., agriculture industries); created new visa categories for temporary agricultural workers (H-2A) and temporary non-agricultural workers (H-2B); criminalized hiring of undocumented workers |
| 1990, George H. W. Bush (R) | Immigration Act of 1990 | • Inclusive immigration policy • Increased the annual visas ceiling; revised visa limits on certain visa categories (e.g., H-1B visas for temporary skilled workers) |
| 1996, Bill Clinton (D) | Personal Responsibility and Work Reconciliation Act of 1996 (PRWORA or “welfare reform”) | • Restrictive immigration policy • Set limits on access to federally funded health insurance, food assistance, and cash assistance for two group of immigrants (qualified and non-qualified), based on immigration status, age, year of entry to the US and residency in the US or income (Gelatt & Koball, 2014) • Non-qualified immigrants include undocumented/unauthorized immigrants, persons with Temporary Protected Status (TPS), and other lawfully present immigrants such as those with temporary student and work visas • Made it harder for low-income, lawfully present immigrants to qualify for all federally funded public assistance benefits by requiring them to claim their sponsors’ income as their own income until they naturalize or complete 10 years of qualifying employment |
| 1996, Bill Clinton (D) | Illegal Immigration Reform and Immigrant Responsibility Act (IIRAIRA) | • Restrictive immigration policy • Increased enforcement of immigration restrictions like border policing and verification of employment credentials • Restricted immigrant eligibility for public benefits (e.g., people lost Medicaid coverage due to restrictions on non-citizen eligibility) or eligible immigrants voluntarily withdrew from Medicaid (Hagan et al., 2003) |
| 2000, Bill Clinton (D) | Legal Immigration Family Equity (LIFE) and LIFE Act Amendments | • Both restrictive and inclusive
policy • Allowed families to stay together during the immigration process; created K-3 (e.g., spouses of US citizens) and K-4 (e.g., unmarried minor children of US citizens) visas |
| 2002, George W. Bush (R) | Enhanced Border Security and Visa Entry Reform Act | • Restrictive immigration policy • Expanded immigration enforcement infrastructure after the September 11, 2001 attacks |
| 2002, George W. Bush (R) | Homeland Security Act | • Restrictive immigration policy • Created the US Department of Homeland Security and Secretary of Homeland Security position after the September 11, 2001 attacks |
| 2005, George W. Bush (R) | Real ID Act | • Restrictive immigration policy • Increased requirements and procedures for receiving state drivers licenses |
| 2006, George W. Bush (R) | Secure Fence Act | • Restrictive immigration policy • Increased border surveillance by building a fence along the Mexican border |
| 2010, Barack Obama (D) | Development, Relief, and Education for Alien Minors (DREAM) Act | • Inclusive immigration policy • Protects certain immigrants who came to the US as children; provided certain immigrants a pathway to US citizenship • Increased eligibility for public health benefits and assistance |
| 2012, Barack Obama (D) | Deferred Action for Childhood Arrivals (DACA) | • Both restrictive and inclusive
policy • Allows certain immigrants who came to the US as children to receive a two-year period of deferred action from deportation that is renewable; eligibility for a work permit in the US • No pathway to citizenship and unauthorized parents can still be deported • Increased public insurance uptake and eligibility for insurance coverage and improved health outcomes (Giuntella & Lonsky, 2018) |
| 2014, Barack Obama (D) | Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and DACA Program Expanded | • Both restrictive and inclusive
policy • Allowed deferred action for deportation to certain immigrants who have lived in the US since 2010 and have children who are US citizens or lawful permanent residents |
Note. “D” = Democratic Party, “R” = Republican Party.
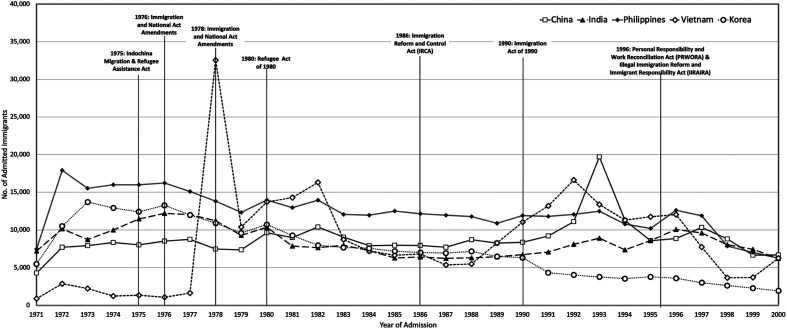
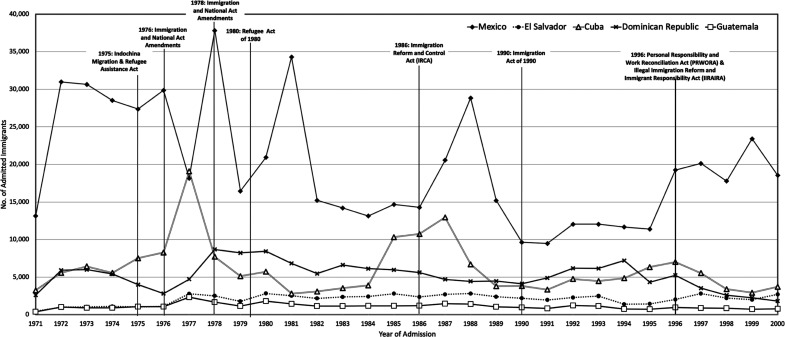
Figures 1 and 2 illustrate the number of immigrants admitted who would currently be 65–85 years old in 2019 for the top 10 immigrant sending countries and shows distinct peaks in immigration flows over time. For example, there are peaks in admission of immigrations from Vietnam in 1972, 1982, and 1992 (Figure 2) while immigrants admitted peaked in 1977 and 1987 for Cuba (Figure 1). Other countries like Mexico (Figure 1) experienced fluctuations in the number of admitted immigrants between 1971 and 2000, with decreases in 1976 and the 1990s.
Figure 1.
Number of admitted immigrants by Asian country and year of admission, among immigrants would be 65–85 years old in 2019. Note. IRCA = Immigration Reform and Control Act; IIRAIRA = Illegal Immigrant Reform and Immigrant Responsibility Act; PWORA= Personal Responsibility and Work Opportunity Reconciliation Act.
Figure 2.
Number of admitted immigrants by Central and South American country and year of admission, among immigrants would be 65–85 years old in 2019. Note. IRCA = Immigration Reform and Control Act; IIRAIRA = Illegal Immigrant Reform and Immigrant Responsibility Act; PWORA= Personal Responsibility and Work Opportunity Reconciliation Act.
Immigrant Profiles from 1971 to 2000
Table 3 shows demographic characteristics of admitted immigrants between 1971 and 2000, by top 10 and other immigrant sending countries. Most immigrants arrived in the U.S. at 25–44 years and during the Reagan Administration (1981–1988). There are distinct differences in the year of migration, mirroring Figure 1 and Figure 2. For example, most immigrants from Mexico were admitted in the 1970s while immigrants from El Salvador were admitted in the 1980s.
Table 3.
Immigration Characteristics of Older Adult Immigrants (65–85 Years Old in 2019), Immigrants Admitted to the United States, Fiscal Years 1972–2000 (ICPSR 37688) (n = 4,702,568).
| Full Sample (n = 4,702,568) | All Other Countries (n = 2,379,486) | Mexico (n = 579,116) | China (n = 28,646) | India (n = 248,764) | Philippines (n = 361,882) | El Salvador (n = 60,462) | Vietnam (n = 235,895) | Cuba (n = 179,302) | Dominican Republic (n = 152,616) | Korea (n = 213,752 | Guatemala (n = 32,647 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | % | % | % | % | % | |
| Age of migration | ||||||||||||
| 0–17 Years old | <0.1 | 0.1 | 0.2 | <0.1 | <0.1 | 0.1 | <0.1 | <0.1 | 0.1 | 0.1 | <0.1 | 0.1 |
| 18–24 Years old | 7.3 | 7.4 | 10.4 | 5.0 | 6.1 | 7.3 | 3.7 | 3.1 | 5.1 | 7.3 | 9.4 | 6.4 |
| 25–34 Years old | 32.7 | 33.5 | 35.2 | 24.5 | 36.0 | 33.6 | 28.2 | 25.9 | 20.2 | 32.3 | 39.5 | 35.4 |
| 35–44 Years old | 31.8 | 32.8 | 26.7 | 32.3 | 24.9 | 29.4 | 34.1 | 33.4 | 43.8 | 33.6 | 31.4 | 32.8 |
| 45–54 Years old | 20.6 | 19.6 | 17.9 | 27.5 | 22.5 | 20.6 | 21.6 | 28.2 | 24.1 | 20.4 | 16.7 | 18.9 |
| 55–64 Years old | 7.4 | 6.4 | 9.1 | 10.2 | 10.2 | 8.9 | 11.8 | 9.2 | 6.6 | 6.2 | 3.0 | 6.3 |
| 65 Years and older | 0.2 | 0.2 | 0.4 | 0.3 | 0.2 | 0.2 | 0.5 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 |
| Year of immigration | ||||||||||||
| 1971–1979 | 35.1 | 35.2 | 40.2 | 26.3 | 37.0 | 25.9 | 21.2 | 21.6 | 38.1 | 31.6 | 47.0 | 32.1 |
| 1980–1989 | 33.5 | 34.1 | 31.8 | 31.6 | 27.8 | 32.6 | 40.7 | 33.4 | 34.6 | 36.9 | 34.8 | 38.3 |
| 1990–2000 | 31.4 | 30.6 | 28.0 | 42.1 | 35.2 | 31.5 | 38.2 | 45.0 | 27.3 | 31.5 | 18.2 | 29.6 |
| Presidential administration during immigration | ||||||||||||
| Nixon (R) | 10.4 | 10.8 | 12.9 | 7.7 | 10.5 | 11.3 | 4.1 | 2.6 | 8.5 | 9.5 | 13.9 | 7.1 |
| Ford (R) | 11.5 | 11.1 | 14.8 | 9.6 | 13.5 | 13.3 | 5.4 | 1.6 | 11.9 | 8.0 | 18 | 9.4 |
| Carter (D) | 16.6 | 16.8 | 15.5 | 11.9 | 16.3 | 14.4 | 15.6 | 19.8 | 20.4 | 18.7 | 19.2 | 20.3 |
| Reagan (R) | 27.3 | 27.8 | 26.2 | 25.5 | 21.9 | 26.5 | 32.7 | 27.6 | 29.8 | 29.4 | 27.7 | 30.5 |
| Bush (R) | 12.3 | 12.8 | 8.0 | 14.2 | 11.4 | 12.9 | 14.6 | 20.7 | 8.7 | 12.9 | 9.9 | 12.5 |
| Clinton (D) | 22.0 | 20.7 | 22.7 | 31.0 | 26.4 | 21.7 | 27.6 | 27.8 | 20.7 | 21.5 | 11.3 | 20.3 |
| Time in U.S. Before becoming LPR (category) | ||||||||||||
| Arrived in US as LPR | 66.2 | 61.8 | 83.8 | 75.8 | 78.8 | 77.2 | 85.3 | 28.5 | 14.6 | 88.6 | 83.2 | 81.8 |
| 1 Year | 9.6 | 12.6 | 2.7 | 4.7 | 5.4 | 4.6 | 2.0 | 27.5 | 6.7 | 3.0 | 4.9 | 2.6 |
| 2 Years | 7.3 | 9.2 | 1.4 | 4.2 | 4.6 | 3.3 | 1.5 | 20.3 | 12.5 | 2.2 | 3.0 | 1.8 |
| 3–5 Years | 9.9 | 10.0 | 2.9 | 98 | 8.2 | 7.1 | 3.6 | 21.6 | 37.0 | 3.6 | 5.4 | 4.2 |
| 6–10 Years | 5.2 | 5.1 | 3.3 | 4.7 | 2.7 | 5.6 | 5.0 | 1.9 | 24.7 | 1.9 | 2.9 | 5.5 |
| 11 Years or more | 1.9 | 1.4 | 6.0 | 0.7 | 0.3 | 2.2 | 2.6 | 0.2 | 2.6 | 0.7 | 0.6 | 4.2 |
| Female sex | 52.9 | 51.3 | 53.6 | 51.8 | 47.9 | 62.2 | 62.1 | 52.5 | 49.2 | 52.8 | 58.9 | 58.3 |
| Marital status | ||||||||||||
| Single | 14.3 | 13.7 | 9.9 | 13.0 | 12.9 | 23 | 18.8 | 17.8 | 16.2 | 25.1 | 11.6 | 14.2 |
| Married | 81.4 | 81.9 | 85.8 | 83.2 | 84.2 | 73.4 | 75.1 | 77.7 | 73.3 | 71.1 | 84.7 | 80.6 |
| Widowed | 1.7 | 1.5 | 3.0 | 1.5 | 2.3 | 2.3 | 2.5 | 2.9 | 1.2 | 0.9 | 1.3 | 1.6 |
| Divorced | 2.4 | 2.7 | 1.2 | 2.2 | 0.5 | 1.2 | 3.4 | 1.4 | 9.2 | 3.0 | 2.4 | 3.3 |
| Separated | 0.2 | 0.2 | 0.2 | 0.1 | <0.1 | 0.1 | 0.2 | 0.3 | 0.1 | <0.1 | <0.1 | 0.3 |
| Visa type | ||||||||||||
| Immediate relative visa | 29.5 | 31.0 | 44.0 | 17.2 | 17.7 | 39.6 | 32.8 | 11.8 | 2.9 | 33.6 | 23.6 | 32.0 |
| Family sponsored visa | 31.6 | 29.0 | 20.6 | 55.5 | 52.6 | 39.8 | 29.7 | 11.0 | 10.6 | 49.8 | 52.5 | 29.4 |
| Employment sponsored visa | 12.6 | 14.7 | 2.2 | 20.4 | 19.7 | 19.3 | 17.8 | 0.7 | 0.3 | 1.0 | 19.0 | 13.3 |
| Refugee visa or Lautenberg visa | 9.5 | 11.0 | <0.1 | 3.5 | <0.1 | <0.1 | <0.1 | 67.0 | 10.3 | <0.1 | <0.1 | <0.1 |
| Asylum seeker or NACARA | 0.8 | 1.5 | <0.1 | 0.6 | 0.2 | <0.1 | 1.7 | <0.1 | 1.1 | <0.1 | <0.1 | 0.8 |
| Other Cuban visa | 3.4 | 0.9 | <0.1 | 0.1 | <0.1 | <0.1 | 0.1 | 3.4 | 72.1 | 0.1 | <0.1 | 0.3 |
| Diversity visa | 1.2 | 2.3 | <0.1 | <0.1 | 0.1 | <0.1 | 0 | <0.1 | 0.3 | <0.1 | <0.1 | 0.2 |
| Born abroad to U.S. Parents or Amerasian visa | 0.3 | <0.1 | 0 | <0.1 | 0 | <0.1 | 0 | 5.8 | 0 | 0 | <0.1 | 0 |
| Other visa | 11.0 | 9.7 | 33.2 | 2.7 | 9.8 | 1.3 | 17.9 | 0.2 | 2.6 | 15.6 | 4.8 | 23.9 |
| Arrived as a derivative of immigrant visa holder | 14.7 | 15.4 | 5.9 | 23.9 | 22.7 | 14 | 10.4 | 20.9 | 4.0 | 4.7 | 22.4 | 9.0 |
Note. “0” represents a true zero percentage while “<0.1” represents a small cell, but non-zero percentage. “D” = Democratic Party; “R” = Republican Party.
Most immigrants arrived in the U.S. as LPR but this varied by sending country. About 84% of immigrants from Mexico arrived as LPR compared to 29% from Vietnam and 15% from Cuba; Vietnamese and Cuban immigrants took three or more years to obtain LPR status.
Overall, most immigrants arrived in the U.S. through family sponsored (F) or immediate relative (IR) visas. Most immigrants from Mexico arrived as IR visa-holders while over half of immigrants from China, India, Dominican Republic, and Korea arrived as F visa-holders. Immigrants from the Philippines were evenly distributed between IR and F visas and about one in five individuals came on employment visas. Similarly, one in five Chinese immigrants arrived on employment visas. Most Vietnamese and Cuban immigrants arrived as refugees or asylees through specialized visas.
Health Insurance Access for Older Adult Immigrants in 2019
Table 4 displays the theoretical weighted univariate and bivariate distribution of health insurance access for older immigrant adults aged 65–85 years in the U.S. Almost 98% of older immigrant adults had health insurance, with distinct differences by country of origin. Nearly 99% of immigrants from India and the Philippines had some type of health insurance while only 92.8% of immigrants from Mexico, 94% of immigrants from Guatemala, and 95.5% of immigrants from El Salvador had health insurance.
Table 4.
Weighted Sample Characteristics by Country of Origin, 2019 American Community Survey (n = 152,441).
| Full Sample (n = 152,441) | All Other Countries (n = 71.920) | Mexico (n =23,165) | China (n = 8939) | India (n = 7821) | Philippines (n = 12,567) | El Salvador (n = 2943) | Vietnam (n = 9090) | Cuba (n = 5211) | Dominican Republic (n = 2683) | Korea (n =6626) | Guatemala (n = 1476) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % | M (SD) or % |
| Health insurance type | ||||||||||||
| Any health insurance | 97.5 | 98.2 | 92.8 | 99.0 | 99.0 | 98.9 | 95.5 | 99.2 | 99.1 | 97.5 | 98.9 | 94.4 |
| Private insurance | 48.3 | 42.3 | 20.5 | 28.6 | 46.5 | 53.7 | 23.4 | 29.2 | 14.9 | 20.1 | 34.4 | 26.3 |
| Medicaid | 29.6 | 23.6 | 37.7 | 38.9 | 18.2 | 19.5 | 39.3 | 39.3 | 48.9 | 57.6 | 28.5 | 38.6 |
| Medicare | 31.1 | 90.8 | 87.1 | 94.1 | 91.5 | 92.0 | 88.0 | 94.9 | 96.7 | 93.5 | 95.2 | 86.6 |
| Medicare and Medicaid | 29.6 | 23.6 | 37.7 | 38.9 | 18.2 | 19.5 | 39.3 | 39.3 | 48.9 | 57.6 | 28.5 | 38.6 |
| Health difficulties | ||||||||||||
| Any difficulty | 27.1 | 25.4 | 32.2 | 25.2 | 22.4 | 26.6 | 32.1 | 31.1 | 31.2 | 35.0 | 20.4 | 25.7 |
| Cognitive difficulty | 7.8 | 7.2 | 8.9 | 7.2 | 5.1 | 6.4 | 8.2 | 11.5 | 12.1 | 11.4 | 5.0 | 8.2 |
| Physical difficulty | 17.6 | 16.4 | 21.5 | 15.4 | 14.5 | 17.1 | 21.2 | 19.5 | 20.7 | 24.1 | 12.6 | 17.8 |
| Independent living difficulty | 13.1 | 12.2 | 14.8 | 13.4 | 10.8 | 12.8 | 13.5 | 17.2 | 14.4 | 17.0 | 10.0 | 11.1 |
| Care difficulty | 7.3 | 7.1 | 8.6 | 6.7 | 5.5 | 5.3 | 7.3 | 9.3 | 9.2 | 11.1 | 4.5 | 6.4 |
| Sensory difficulty | 11.3 | 10.2 | 15.2 | 10.4 | 9.3 | 11.1 | 13.3 | 13.1 | 11.6 | 13.6 | 9.0 | 8.7 |
| Sight difficulty | 5.6 | 4.9 | 8.7 | 4.2 | 3.2 | 4.1 | 8.9 | 5.9 | 7.0 | 9.3 | 3.8 | 5.3 |
| Hearing difficulty | 7.7 | 6.8 | 10.0 | 7.9 | 7.3 | 8.4 | 7.5 | 9.7 | 7.0 | 7.3 | 6.3 | 5.3 |
| Demographic characteristics | ||||||||||||
| Age | 71.63 (.02) | 71.50 (.03) | 71.13 (.05) | 72.78 (.09) | 71.52 (.08) | 71.71 (.07) | 70.61 (.12) | 72.05 (.08) | 73.32 (.10) | 71.27 (.13) | 72.30 (.09) | 70.51 (.17) |
| Female sex | 55.2 | 55.0 | 53.6 | 52.9 | 48.2 | 63.2 | 61.2 | 54.6 | 50.2 | 58.4 | 60.7 | 53.8 |
| Marital status | ||||||||||||
| Married, spouse present | 28.2 | 58.0 | 56.2 | 66.8 | 72.8 | 59.6 | 41.7 | 59.9 | 46.9 | 39.4 | 65.5 | 46.9 |
| Married, spouse absent | 3.7 | 3.1 | 4.4 | 4.5 | 4.0 | 4.0 | 4.9 | 5.0 | 2.5 | 5.2 | 3.1 | 6.0 |
| Separated | 3.0 | 2.8 | 4.4 | 1.3 | 1.0 | 1.9 | 5.4 | 2.2 | 4.1 | 8.8 | 1.8 | 5.9 |
| Divorced | 11.1 | 13.2 | 7.9 | 7.0 | 4.6 | 8.8 | 13.0 | 8.4 | 19.4 | 20.5 | 9.3 | 13.2 |
| Widowed | 18.1 | 17.3 | 20.3 | 17.7 | 16.1 | 19.5 | 17.4 | 18.6 | 19.5 | 16.4 | 18.8 | 17.2 |
| Never married/Single | 5.8 | 5.6 | 6.9 | 2.9 | 1.7 | 6.2 | 17.7 | 5.8 | 7.7 | 9.8 | 1.6 | 10.9 |
| Immigration variables | ||||||||||||
| Age at migration | ||||||||||||
| 18–24 years old | 12.1 | 12.1 | 12.2 | 16.3 | 13.4 | 10.8 | 8.4 | 10.8 | 15.8 | 13.1 | 7.4 | 9.2 |
| 25–34 years old | 29.6 | 29.8 | 26.2 | 38.1 | 24.6 | 29.2 | 26.3 | 38.5 | 27.2 | 38.6 | 23.5 | 29.7 |
| 35–44 years old | 40.8 | 40.5 | 40.0 | 33.6 | 40.5 | 38.5 | 53.9 | 45.6 | 41.2 | 38.9 | 47.5 | 44.6 |
| 45–54 years old | 17.5 | 17.7 | 21.6 | 12.0 | 21.5 | 21.5 | 11.3 | 5.1 | 15.9 | 9.5 | 21.6 | 16.6 |
| Year of immigration | ||||||||||||
| 1971–1979 | 38.7 | 28.7 | 45.2 | 26.1 | 45.2 | 41.7 | 34.4 | 31.0 | 24.5 | 26.4 | 48.1 | 38.5 |
| 1980–1989 | 34.9 | 24.8 | 31.5 | 40.3 | 29.8 | 34.7 | 47.3 | 30.4 | 43.7 | 40.6 | 35.4 | 42.0 |
| 1990–2000 | 26.4 | 26.5 | 23.3 | 33.6 | 24.9 | 23.7 | 18.3 | 38.6 | 31.8 | 32.9 | 16.4 | 19.5 |
| Presidential administration during immigration | ||||||||||||
| Nixon (R) | 13.4 | 13.6 | 16.5 | 9.2 | 16.5 | 16.4 | 8.2 | 3.9 | 12.7 | 7.4 | 15.7 | 12.8 |
| Ford (R) | 13.1 | 12.0 | 15.5 | 8.4 | 16.2 | 14.6 | 11.4 | 18 | 5.6 | 7.5 | 18.8 | 14.4 |
| Carter (D) | 19.6 | 19.6 | 20.9 | 13.6 | 17.4 | 16.0 | 26.7 | 17.2 | 31.7 | 18.6 | 20.4 | 19.2 |
| Reagan (R) | 24.2 | 24.7 | 21.1 | 30.5 | 22.2 | 26.2 | 32.8 | 19.8 | 15.6 | 29.6 | 25.8 | 30.6 |
| Bush (R) | 12.8 | 13.2 | 10.5 | 16.4 | 9.8 | 11.8 | 10.0 | 20.7 | 11.7 | 16.3 | 9.6 | 10.4 |
| Clinton (D) | 16.9 | 17.0 | 15.6 | 21.8 | 18.0 | 15.0 | 10.8 | 20.4 | 22.7 | 20.6 | 9.7 | 12.6 |
| Years in the U.S. | 34.01 (.03) | 33.94 (.04) | 34.93 (.09) | 31.74 (.12) | 34.70 (.14) | 34.60 (.10) | 34.57 (.17) | 32.38 (.12) | 32.94 (.16) | 32.17 (.19) | 35.91 (.13) | 34.77 (.29) |
| Citizenship status | ||||||||||||
| Naturalized citizen | 79.2 | 82.3 | 53.1 | 87.3 | 90.3 | 90.6 | 68.1 | 94.1 | 84.1 | 78.0 | 86.9 | 68.6 |
| Non-citizen | 20.8 | 17.7 | 46.9 | 12.7 | 9.7 | 9.4 | 31.9 | 5.9 | 15.9 | 22.0 | 13.1 | 31.4 |
| English Proficiency | ||||||||||||
| Does not speak English | 14.3 | 5.7 | 35.2 | 26.2 | 5.5 | 1.0 | 26.2 | 15.8 | 29.8 | 36.1 | 9.1 | 17.4 |
| Speaks English poorly | 25.2 | 18.6 | 33.5 | 36.1 | 12.9 | 9.7 | 40.1 | 43.8 | 33.8 | 37.1 | 40.6 | 39.9 |
| Speaks English well/Very well | 44.1 | 46.4 | 26.8 | 33.2 | 72.3 | 81.9 | 29.8 | 36.1 | 31.7 | 22.5 | 43.3 | 38.3 |
| Only speaks English | 16.4 | 29.3 | 4.5 | 4.5 | 9.4 | 7.6 | 3.9 | 4.3 | 4.8 | 4.3 | 7.0 | 4.4 |
| Socioeconomic attainment | ||||||||||||
| Educational attainment | ||||||||||||
| No school | 9.2 | 6.0 | 19.3 | 12.1 | 4.6 | 2.1 | 17.5 | 17.2 | 5.4 | 10.6 | 4.6 | 14.1 |
| Less than high school | 23.4 | 13.8 | 54.7 | 24.1 | 90.0 | 7.7 | 49.0 | 19.1 | 33.6 | 49.7 | 12.9 | 43.3 |
| High school or GED | 27.7 | 32.3 | 17.2 | 25 | 17.8 | 21.2 | 20.7 | 34.1 | 35.6 | 24.3 | 36 | 26.9 |
| Some college | 12.6 | 15.7 | 5.0 | 9.9 | 9.8 | 17.8 | 7.7 | 14.6 | 10.6 | 7.2 | 12.5 | 8.1 |
| College degree or more | 27.1 | 32.2 | 3.9 | 28.9 | 58.8 | 51.2 | 5.2 | 15.1 | 14.8 | 8.2 | 34.1 | 7.6 |
| Income | ||||||||||||
| < $25,000 | 24.7 | 23.2 | 29.5 | 30.5 | 9.6 | 1.9 | 23.4 | 25.0 | 41.1 | 43.5 | 32 | 23.5 |
| $25,000 to 34,999 | 8.6 | 8.3 | 11.0 | 8.3 | 4.3 | 6.3 | 10.2 | 7.4 | 11.4 | 10.0 | 8.8 | 12.0 |
| $35,000 to 49,999 | 11.1 | 11.4 | 12.9 | 9.3 | 8.2 | 8.6 | 13.5 | 10.4 | 11.5 | 10.6 | 10.3 | 13.4 |
| $50,000 to 74,999 | 15.1 | 15.2 | 17.7 | 12.4 | 12.8 | 14.2 | 18.2 | 15.3 | 12.5 | 12.8 | 13 | 16.0 |
| $75,000 to 99,999 | 11.0 | 11.3 | 10.8 | 9.5 | 10.0 | 13.9 | 12.5 | 11.5 | 8.0 | 8.2 | 10.4 | 10.9 |
| $100,000 to $149,999 | 13.7 | 13.8 | 11.7 | 12.8 | 17.4 | 19.2 | 13.0 | 14.7 | 9.3 | 9.3 | 11.5 | 12.7 |
| > $150,000 | 15.8 | 16.7 | 6.5 | 17.3 | 37.7 | 26.9 | 9.1 | 15.7 | 6.2 | 5.6 | 14.2 | 11.5 |
Note. “D” = Democratic Party; “R” = Republican Party.
By health insurance type, about 48% of older immigrant adults had private health insurance, followed by 31% with Medicare, 30% with Medicaid, and 30% with both Medicare and Medicaid. There were also differences in health insurance type by country of origin. About 54% of immigrants from the Philippines had private insurance, while immigrants from Cuba had the lowest rate of private insurance at 15% and 42% of immigrants from Other Countries had private insurance. For Medicaid, immigrants from the Dominican Republic had the highest rate at 57.6% compared to only 29.6% of immigrants from Other Countries; the remaining top 10 sending countries (except for India and Philippines) had higher rates of Medicaid compared to immigrants from Other Countries. For Medicare, immigrants from Cuba had the highest rate at 96.7% while immigrants from El Salvador at the lowest rate at 39.3%. For dual-eligible Medicare and Medicaid, immigrants from the Dominican Republic had the highest rate at 57.6%, followed by immigrants from Cuba (48.9%).
Health Difficulties for Older Adult Immigrants in 2019
About 27% of older immigrant adults reported having any health difficulty (Table 4). The most common health difficulty was physical difficulties (17.6%), followed by independent living difficulties (13.1%) and sensory difficulties (11.3%). Similar to health insurance access, health difficulties varied by country of origin. Immigrants from the Dominican Republic had the highest proportion of adults with any health difficulties (35.0%), followed by immigrants from Mexico (32.2%) and El Salvador (32.1%); immigrants from Korea had the smallest proportion of adults reporting any health difficulty (20.4%). Similar trends were observed across the specific difficulties such as physical difficulties.
Among immigrant adults in the U.S. who would be theoretically aged 65–85 years, they were 72 years old on average, mainly women, arrived in the U.S. when they were 25–44 years old, and immigrated during the 1970s. Immigrants resided in the U.S. about 34 years on average and nearly 90% of immigrants were naturalized citizens by 2019; there were major differences in citizenship status by country of origin. Immigrants from Mexico (53.1%), El Salvador (68.1%), Guatemala (68.6%), and Dominican Republic (78.0%) had the lowest percentage of naturalized citizens, while 82% or more of immigrants for the remaining countries were naturalized citizens.
Almost half of immigrants (44.1%) indicated that they spoke English “well/very well” and most immigrants had a high school education (28.2%) or college degree (27.6%). Immigrants were evenly distributed across income categories. Most immigrants (19.8%) indicated that an average annual income less than $25,000, followed by 17.6% reporting an annual income $150,000 or more.
Predicted Probabilities of Health Insurance Access and Health Difficulties
Table 5 displays the fully adjusted predicted probability of having any health insurance and health insurance type. Rates of having any health insurance were high among older adult immigrants, with at least a 98% insurance rate for most countries. However, rates of insurance were lowest among older adult immigrants from El Salvador, Guatemala, and Mexico. When examining specific types of insurance, most participants reported having Medicare. However, rates of Medicare insurance were lowest among older adult immigrants from El Salvador, Guatemala, and Mexico. The remaining countries had Medicare insurance rates of at least 90%. Moreover, rates of private insurance were highest among Philippine immigrants, while most other groups had private insurance rates around 30%.
Table 5.
Predicted Probabilities of Access to Health Insurance by Country of Origin, 2019 American Community Survey (n = 152,441).
| Any Health Insurance | Private Insurance | Medicaid | Medicare | Medicare and Medicaid | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country of Origin | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| All other countries | 97.9 | 97.7, 98.0 | 37.7 | 37.3, 38.2 | 27.8 | 27.3, 28.2 | 91.2 | 91.0, 91.6 | 27.8 | 27.3, 28.2 |
| Mexico | 95.9 | 95.5, 96.2 | 30.3 | 29.4, 31.2 | 29.2 | 28.4, 29.9 | 87.3 | 86.6, 87.9 | 29.2 | 28.4, 29.9 |
| China | 98.8 | 98.4, 99.1 | 34.3 | 33.1, 35.6 | 31.4 | 30.3, 32.5 | 92.9 | 92.2, 93.6 | 31.4 | 30.3, 32.5 |
| India | 98.3 | 97.8, 98.9 | 34.6 | 33.4, 35.9 | 28.6 | 27.2, 30.1 | 92.5 | 91.8, 93.2 | 28.6 | 27.2, 30.1 |
| Philippines | 98.2 | 97.7, 98.6 | 41.7 | 40.6, 42.8 | 29.9 | 28.8, 31.0 | 92.7 | 92.1, 93.3 | 29.9 | 28.8, 31.0 |
| El Salvador | 97.3 | 96.6, 98.0 | 30.2 | 29.8, 34.2 | 30.9 | 29.0, 32.7 | 88.9 | 87.3, 90.4 | 30.9 | 28.8, 31.0 |
| Vietnam | 98.8 | 98.4, 99.3 | 34.2 | 32.9, 35.5 | 32.6 | 31.4, 33.8 | 93.6 | 92.9, 94.3 | 32.6 | 31.4, 33.8 |
| Cuba | 99.2 | 98.9, 99.5 | 23.5 | 21.9, 25.2 | 34.9 | 33.4, 36.4 | 95.3 | 94.4, 96.2 | 34.9 | 33.4, 36.4 |
| Dominican Republic | 98.3 | 97.7, 98.9 | 33.3 | 30.8, 35.7 | 39.7 | 37.5, 41.8 | 92.6 | 91.3, 93.9 | 39.7 | 37.5, 41.8 |
| Korea | 98.3 | 97.8, 98.8 | 35.2 | 33.7, 36.7 | 28.5 | 27.2, 29.8 | 93.7 | 92.7, 94.6 | 28.5 | 27.2, 29.8 |
| Guatemala | 96.3 | 95.0, 97.6 | 32.3 | 29.4, 35.5 | 33.5 | 30.6, 36.4 | 87.7 | 85.5, 89.9 | 33.5 | 30.6, 36.4 |
Note. All models account for age, sex, marital status, country of origin, English proficiency, citizenship status, educational attainment, income, age of migration, year of migration, and presidential administration during migration.
Table 6 displays the fully adjusted predicted probability of reporting health difficulties by country of origin. Immigrants from the Philippines had the highest reports of any health difficulty (33.4%), followed by immigrants from India (29.4%) and El Salvador (28.5%), while immigrants from Korea had the lowest probability of any health difficulty (19.7%). By specific health difficulty, cognitive and physical health difficulties were highest among immigrants from the Philippines; physical and independent living difficulties was highest among immigrants from India; and physical, sensory, sight, and hearing difficulties was highest among immigrants from El Salvador.
Table 6.
Predicted Probabilities of Health Difficulty by Country of Origin, 2019 American Community Survey (n = 152,441).
| Any Difficulty | Cognitive Difficulty | Physical Difficulty | Independent Living Difficulty | Care Difficulty | Sensory Difficulty | Sight Difficulty | Hearing Difficulty | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country of Origin | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| All other countries | 27.9 | 27.4, 28.3 | 8.4 | 8.1, 8.7 | 18.1 | 17.7, 18.5 | 14.1 | 13.8, 14.5 | 8.2 | 7.9, 8.5 | 11.0 | 10.7, 11.3 | 5.4 | 5.2, 5.7 | 7.4 | 7.1, 7.6 |
| Mexico | 27.4 | 26.7, 28.1 | 6.8 | 6.4, 7.2 | 18.3 | 17.7, 19.0 | 12.1 | 11.6, 12.6 | 7.2 | 6.7, 7.6 | 13.1 | 12.5, 13.6 | 6.9 | 6.5, 7.3 | 8.9 | 8.4, 9.3 |
| China | 20.8 | 19.8, 21.8 | 5.6 | 5.0, 6.1 | 12.6 | 11.8, 13.4 | 10.0 | 9.3, 10.7 | 4.9 | 4.4, 5.4 | 8.6 | 7.9, 9.3 | 3.6 | 3.1, 4.0 | 6.4 | 5.8, 7.0 |
| India | 29.4 | 28.1, 30.7 | 8.0 | 7.1, 8.9 | 20.0 | 18.7, 21.2 | 15.1 | 14.0, 16.2 | 7.9 | 7.1, 8.8 | 11.9 | 10.9, 12.9 | 4.6 | 3.9, 5.4 | 8.9 | 8.0, 9.8 |
| Philippines | 33.4 | 32.3, 34.5 | 10.0 | 9.2, 10.8 | 22.1 | 21.1, 23.1 | 17.4 | 16.5, 18.3 | 7.5 | 6.8, 8.2 | 14.4 | 13.5, 15.3 | 5.9 | 5.3, 6.6 | 10.7 | 9.9, 11.4 |
| El Salvador | 28.5 | 26.4, 30.5 | 6.6 | 5.5, 7.7 | 18.5 | 16.8, 20.2 | 11.5 | 10.1, 12.9 | 6.4 | 5.3, 7.6 | 12.6 | 11.0, 12.7 | 7.5 | 6.3, 8.8 | 7.5 | 6.2, 8.8 |
| Vietnam | 27.5 | 26.4, 28.6 | 9.7 | 8.9, 10.5 | 16.9 | 16.0, 17.9 | 14.2 | 13.3, 15.0 | 7.5 | 6.9, 8.2 | 11.9 | 11.1, 12.7 | 5.3 | 4.7, 5.9 | 8.7 | 8.0, 9.4 |
| Cuba | 23.0 | 21.7, 24.3 | 8.1 | 7.4, 8.9 | 14.9 | 13.9, 16.0 | 9.7 | 8.9, 10.6 | 6.0 | 5.3, 6.7 | 8.4 | 7.7, 9.2 | 5.1 | 4.5, 5.7 | 4.9 | 4.4, 5.5 |
| Dominican Republic | 26.9 | 25.0, 28.8 | 7.5 | 6.4, 8.5 | 17.7 | 16.1, 19.2 | 11.9 | 10.6, 13.1 | 7.5 | 6.4, 8.6 | 10.7 | 9.4, 12.1 | 6.6 | 5.5, 7.7 | 6.0 | 5.0, 7.1 |
| Korea | 19.7 | 18.5, 20.8 | 5.0 | 4.3, 5.7 | 12.0 | 11.0, 13.0 | 9.5 | 8.6, 10.4 | 4.2 | 3.6, 4.8 | 8.8 | 8.0, 9.7 | 3.9 | 3.2, 4.5 | 6.1 | 5.4, 6.8 |
| Guatemala | 24.5 | 22.0, 27.0 | 7.5 | 6.0, 9.0 | 17.0 | 14.9, 19.1 | 10.9 | 9.2, 12.5 | 6.3 | 4.9, 7.7 | 8.6 | 7.1, 10.1 | 4.9 | 3.8, 6.1 | 5.4 | 4.2, 6.7 |
Note. All models account for age, sex, marital status, country of origin, English proficiency, citizenship status, educational attainment, income, age of migration, year of migration, and presidential administration during migration.
Discussion
This paper provides one of the first overviews of immigration flows using administrative data compiled by Kossoudji (2020). We characterize historical immigration trends by examining health insurance access and health difficulties of current older adult immigrants in the U.S. Our results highlighted close alignment of immigration flows into the U.S. with immigration legislation and the vast heterogeneity in the migration patterns, health, and healthcare access of immigrants by sending country.
As expected, peaks in immigrant admission correspond to immigration policies and historical events that shaped policies to be more or less favorable to immigrants (Table 2). For example, the number of immigrants admitted from Vietnam corresponds with the Fall of Saigon in 1975 (i.e., end of the Vietnam War), as well as passage of the 1975 Indochina Migration and Refugee Assistance Act, Refugee Act of 1980, and 1986 IRCA. We observed peaks in immigration flows from Cuba in 1977 and 1987 that are likely related to the Cuban communist revolution in 1959 and resulted in more preferential immigration policies towards Cuba. The fluctuations of immigration flow of Mexican immigrants correspond to passage of legislation like the 1976 Immigration and National Act Amendments and 1996 Illegal Immigration Reform and Immigrant Responsibility Act (IIRAIRA), that vilified Mexican immigrants as “illegal aliens.” Immigrants from the Philippines had high and steady levels of admission to the U.S. which could be related to the preferential treatment for skilled workers.
Health disparities in health and healthcare utilization are typically evaluated by differences in health based on race/ethnicity, which are socially constructed categories that may inaccurately describe individual experiences, with little or no reference to country of birth or origin or citizenship status. In this paper, we considered country of origin as an important determinant of health; other variables to better historicize health could include examination of nationality, country of origin, race/ethnicity, and ancestry. For healthcare access, we found that while most people had some form of health insurance, there were distinct deficiencies in access among those from Mexico and Latin American countries. This is surprising, especially given that most people should be eligible for at least Medicare in older age. However, the predicted probabilities of having Medicare were lowest among people from Mexico, El Salvador, and Guatemala, which may be related to potential fears of public charge (Ma et al., 2021; Perreira et al., 2018).
Moreover, in our analyses of health difficulties, the predicted probability of having any health difficulty was highest among people from the Philippines, India, and Mexico; this was quite contrasting because individuals from the Philippines and India had high predicted probabilities of having health insurance. These results invite opportunities to consider what institutional and structural factors may contribute to the poorer health among older adults from these countries. Using the Philippines as an example, potential historical and physical traumas resultant from legacies of U.S. imperialism and colonialism could contribute to both to poorer health and well-being in addition to motivation to migrate to the U.S. (Sabado-Liwag et al., 2022). Alternatively, intense work conditions that Filipinos may have experienced upon migration to the U.S. could further contribute to poorer health that could manifest in older age (de Castro et al., 2009; Fujishiro et al., 2011; Garcia & de Castro, 2017; Ma et al., 2021).
For analyses with poor quality or limited racial/ethnic data, country of origin is often used as a proxy for ethnicity. However, we encourage researchers and health professionals to reconsider country of origin as a marker of historical immigration circumstances, or an additional dimension in which to evaluate and improve health for immigrants over the life span.
It is equally important to consider what constitutes as “legal” immigration—which is highly influenced by historic events and U.S. policies that determine migration flows and visa quotas, and the economic and sociopolitical environments in which immigrants arrive. For example, the 1965 Immigration and Nationality Act established bureaucratic borders based on established familial relationships in the U.S. or potential employment and changed the demographic makeup of the U.S. by increasing immigration quotas (Bacong & Menjívar, 2021; Enchautegui & Menjívar, 2015; Obinna, 2014). Torres and Young (2016) highlight the intersections of the life course perspective with immigrant legal status and the negative long term and intergenerational effects on health for individuals with precarious legal statuses (e.g., lack of permanent residence) and their families. Policies that criminalize immigrants or decrease access to social supports can also affect immigrant experiences both before and after migration (Wallace et al., 2019; Wallace & Young, 2018; Young & Wallace, 2019).
By examining race/ethnicity in historical context, we can better understand the overall implications of immigration policies on migration flows to the U.S. as well as easing or worsening transitions into the country. For example, a significant proportion of the Vietnamese and Cuban immigrants were admitted as refugees and asylum seekers. Compared to the other immigrants, Vietnamese and Cuban immigrant older adults utilized social services (e.g., Medicaid) at higher rates. These differences could be related to the high share of Vietnamese and Cuban immigrants who have limited English proficiency, low education attainment, and lower income. This emphasizes considerations for the circumstances in which immigrants enter the US, visa types in which they are admitted, as well as environment of reception. For example, past and current refugees and asylum seekers may be fleeing their home countries due to war or persecution, and require more public resources to support their overall well-being as new immigrants. They may also experience ongoing traumas that influence their healthcare utilization and health outcomes that may persist across their lives and trickle down to impacting their families. The varied immigration trajectories highlight the need to acknowledge and develop relevant interventions that address the distinct health and social needs of immigrants.
We found higher rates of Medicare uninsurance among immigrants from Latin American countries compared to immigrants from Asian countries. This could be the result of policy implementations in the 1990s, which criminalized border crossings and promoted ideas of immigrants being a public charge (Derose et al., 2007; Donato & Amuedo-Dorantes, 2020). The literature has demonstrated the deleterious health impacts of fear of being labeled a public charge, as well as the implications of immigration legislation like IIRAIRA, PWORA, and public charge on the health and health coverage of immigrants and their families (Castañeda et al., 2015; Perreira et al., 2018). The consequences of immigration policies are dynamic and cumulatively impact healthcare access and utilization for immigrants, as well as the development of health inequalities over the life span. Interestingly, however, Medicaid insurance rates were highest among immigrants from Guatemala, and El Salvador, despite low Medicare insurance rates. This was not the case for immigrants from Mexico. Thus, although we can consider the promotion of public charge as a deterrent for healthcare access, it may not always be the case depending on the country of origin. In summary, expanded access to health insurance and healthcare for immigrants regardless of their legal status could promote better overall well-being and healthy aging. Healthcare providers and public health professionals need to consider immigration as a social determinant of health and better address the health and social needs of older immigrant populations. Community based organizations and community health workers can provide relevant support and information to immigrant older adults to navigate and access healthcare (McBride et al., 2020).
We provide historical and contextual evidence of immigration trends for older adults with publicly available national data. Few datasets collect comprehensive individual-level historical immigration data that allow examination of how immigration systems and policies impact admission into the U.S. This paper provides a deep dive into the complex sociopolitical histories that shape health outcomes and healthcare access among the aging immigrant population. Future research should explore the migration patterns of recent immigrants to understand and contextualize the heterogeneity of the immigrant experience, as well as consider the implications of visa wait times and visa types on health status. Our paper highlights the importance of and dire need for disaggregated data collection of immigration-related factors in administrative data.
To provide a more comprehensive picture of how immigration influences health across the life course, better data are needed. We recommend the construction of already available databases (e.g., ICPRS and ACS data) that link immigration and health data, as well as new epidemiological datasets that follow diverse immigrant adults longitudinally. Future work could consider techniques like probabilistic record matching, to connect federal administrative immigration data to large population-level datasets. Doing so would allow researchers to examine issues related to the timing of when immigrants receive their visas. Longitudinal studies can also utilize probabilistic matching to examine the long-term effects of the time to obtain visa and visa types on health, which is a new and growing area of research (Bacong & Sohn, 2021; Morey et al., 2020; Obinna, 2014, 2020).
There is also a growing body of literature noting the effects of immigration policy on the health and well-being of immigrants (Novak et al., 2017; Patler et al., 2019; Venkataramani et al., 2017; Wallace et al., 2019), although the focus has been on children and young adults. Future work should consider utilizing both the ICPSR and ACS datasets to examine the effects of historical immigration policies on the health of immigrants today, as well as how anti-immigrant stigma may affect older immigrants’ health over time (Young & Wallace, 2019). For example, future work could also examine the effects of immigration policies on different temporal cohorts of immigrants to the U.S. (e.g., pre-PWORA, post-PWORA), by age cohort, and by country.
In this study, we provided an extension of the life course perspective and immigration by outlining relevant immigration legislation that were relevant to current older adults. We also looked at compositional differences based on immigrants’ time of arrival, age of arrival, and context of arrival. Overall, these results reveal the varied pathways that immigrants have taken to arrive in the U.S. Using immigrants’ country of origin allowed us to triangulate how historical events, immigration pathways, and policies could underlie disparities in health and healthcare access today. Although this work examined one aspect of the life course perspective (i.e., history), future work can be done to better contextualize the health of older adult immigrants through qualitative interviews, combining health data with immigration and policy data (Dondero & Altman, 2020; Young et al., 2019), or designing studies examining the effects of immigration policy across the life course (Nakphong et al., 2022).
Our analysis has three key limitations to note. One major limitation relates to the comparability of the ICPSR and ACS datasets. We restricted both datasets to be theoretically similar based on individuals who would be ages 65–85 years old in 2019 (i.e., the latest version of the ACS available at the time of writing). To align the ACS and ICSPR datasets since both have the similar sociodemographic variables, we restricted the data to immigrants who had arrived between 1971 and 2000. Given the exploratory nature of this study, variables to link both datasets, and data available, we provide a general population-level overview. Future studies should consider multiple imputation techniques as a possible way to combine both datasets (Capps et al., 2018; Ro & Van Hook, 2021; Van Hook et al., 2015). Second, this study only includes comparisons of the top 10 sending countries to the U.S. versus “Other Countries” and is limited to generalizability to authorized immigrants. We selected the 10 sending countries to match and be comparable to recent analyses listing the top 10 sending countries to the U.S. (Ro et al., 2016). These data are publicly available for use by the US Immigration and Naturalization Service (INS) Statistical Yearbooks but are an undercount of immigrants due to omission of unauthorized individuals in data collection. Finally, the availability of ICPSR data limited our ability to examine the immigration profiles of those who migrated after 2000. Since 2001, immigration policy has seen increased restrictiveness because of the September 11th attacks and debates of the growing population of undocumented immigrants. Thus, we cannot examine the effects of these recent policies on immigration flows. The population of older undocumented immigrants presents a new area of intervention (Flores Morales, 2021). Future work should consider expanding the research to examine immigration profiles post-2000 as data become available.
Future policies need to consider the varied circumstances of migration (e.g., family reunification, employment, refugee) in creating equitable health and social policies. For example, removing public charge restrictions for citizenship can decrease barriers to immigrants’ use of key social services. Furthermore, decreasing the cost of insurance policies and increasing the quality of Medicaid programs can better support low-income immigrant older adults. Implementing policies that can provide national health insurance coverage for all residents can further close the gap in coverage and help to reduce health disparities by country of origin. In conclusion, as we consider the growth of the older adult immigrant populations, efforts to achieve health equity must considered the varied immigration and historical circumstances that these communities face throughout the entirety of the life course.
Footnotes
Author’s Note: The authors would like to give special thanks to Dr. Lourdes Guerrero, Dr. Jacqueline Torres, and the UCLA Migration Working Group for critical feedback in previous drafts of this manuscript. We would also like to thank Dr. Steven Wallace, whom this special issue is in commemoration of, for his tireless work to address health inequities among people of color, immigrants, and older adults. Thank you for your light and your example. It has been an honor and a privilege to work with you.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: AMB is supported by the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH), Award Number F31MD015931. LÐ is supported by the NIH NIMHD Award Number U54MD000538 and NIH Resource Centers for Minority Aging Research (RCMAR) Award Number 5P30AG059302. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
ORCID iDs
Adrian M. Bacong https://orcid.org/0000-0003-0157-4754
Lan N. Đoàn https://orcid.org/0000-0003-1826-4728
References
- Alba R. (2018). What majority-minority society? A critical analysis of the Census bureau’s projections of America’s demographic future. Socius, 4, 2378023118796932. 10.1177/2378023118796932 [DOI] [Google Scholar]
- Bacong A. M., Menjívar C. (2021). Recasting the immigrant health paradox through intersections of legal status and race. Journal of Immigrant and Minority Health. 10.1007/s10903-021-01162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacong A., Sohn H. (2021). Disentangling contributions of demographic, family, and socioeconomic factors on associations of immigration status and health in the United States. Journal of Epidemiology and Community Health, 75(6), 587–592. 10.1136/jech-2020-214245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen M. E., Ruch A. (2015). Depressive symptoms and disability risk among older white and Latino adults by nativity status. Journal of Aging and Health, 27(7), 1286–1305. 10.1177/0898264315580121 [DOI] [PubMed] [Google Scholar]
- Brown T. H. (2018). Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces, 96(4), 1507–1540. 10.1093/sf/soy013 [DOI] [Google Scholar]
- Budiman A. (2020, September 21, 2020). Key findings about U.S. immigrants. Pew Research Center. Retrieved September 3, 2021 from https://www.pewresearch.org/fact-tank/2020/08/20/key-findings-about-u-s-immigrants/
- Calvo R., Carr D. C., Matz-Costa C. (2017). Another paradox? The life satisfaction of older hispanic immigrants in the United States. Journal of Aging and Health, 29(1), 3–24. 10.1177/0898264315624901 [DOI] [PubMed] [Google Scholar]
- Capps R., Bachmeier J. D., Van Hook J. (2018). Estimating the characteristics of unauthorized immigrants using U.S. Census data: Combined sample multiple imputation. The ANNALS of the American Academy of Political and Social Science, 677(1), 165–179. 10.1177/0002716218767383 [DOI] [Google Scholar]
- Castañeda H., Holmes S. M., Madrigal D. S., Young M.-E. D., Beyeler N., Quesada J. (2015). Immigration as a social determinant of health. Annual Review of Public Health, 36(1), 375–392. 10.1146/annurev-publhealth-032013-182419 [DOI] [PubMed] [Google Scholar]
- de Castro A. B., Cabrera S. L., Gee G. C., Fujishiro K., Tagalog E. A. (2009). Occupational health and safety issues among nurses in the Philippines. AAOHN Journal, 57(4), 149–157. 10.1177/216507990905700405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derose K. P., Escarce J. J., Lurie N. (2007). Immigrants and health care: Sources of vulnerability. Health Affairs, 26(5), 1258–1268. 10.1377/hlthaff.26.5.1258 [DOI] [PubMed] [Google Scholar]
- Đoàn L. N., Takata Y., Hooker K., Mendez-Luck C., Irvin V. L. (2021). Trends in cardiovascular disease by asian American, native Hawaiian, and pacific islander ethnicity, Medicare health outcomes survey 2011–2015. The Journals of Gerontology: Series A, 77(2), 299–309. 10.1093/gerona/glab262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donato K. M., Amuedo-Dorantes C. (2020). The legal landscape of U.S. Immigration: An introduction. RSF: The Russell Sage Foundation Journal of the Social Sciences, 6(3), 1–16. 10.7758/rsf.2020.6.3.01 [DOI] [Google Scholar]
- Dondero M., Altman C. E. (2020). Immigrant policies as health policies: State immigrant policy climates and health provider visits among U.S. immigrants. SSM - Population Health, 10, 100559. 10.1016/j.ssmph.2020.100559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downer B., Chen N.-W., Wong R., Markides K. S. (2016). Self-reported health and functional characteristics of Mexican and Mexican American adults aged 80 and over. Journal of Aging and Health, 28(7), 1239–1255. 10.1177/0898264316656508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder G. H. (1994). Time, human agency, and social change: Perspectives on the life course. Social Psychology Quarterly, 57(1), 4–15. 10.2307/2786971 [DOI] [Google Scholar]
- Enchautegui M. E., Menjívar C. (2015). Paradoxes of family immigration policy: Separation, reorganization, and reunification of families under current immigration laws. Law & Policy, 37(1–2), 32–60. 10.1111/lapo.12030 [DOI] [Google Scholar]
- Flores Morales J. (2021). Aging and undocumented: The sociology of aging meets immigration status. Sociology Compass, 15(4), e12859. 10.1111/soc4.12859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujishiro K., Gee G. C., Castro A. B. d. (2011). Associations of workplace aggression with work-related well-being among nurses in the Philippines. American Journal of Public Health, 101(5), 861–867. 10.2105/ajph.2009.188144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi K., Lim E., Davis J., Chen J. J. (2018). Racial disparities in health service utilization among Medicare fee-for-service beneficiaries adjusting for multiple chronic conditions. Journal of Aging and Health, 30(8), 1224–1243. 10.1177/0898264317714143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia G. M., de Castro B. (2017). Working conditions, occupational injuries, and health among Filipino fish processing workers in Dutch harbor, Alaska. Workplace Health & Safety, 65(5), 219–226. 10.1177/2165079916665396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelatt J., Koball H. (2014). Immigrant Access to Health and Human Services. Immigrants and Immigration, Issue https://www.urban.org/sites/default/files/publication/33551/2000012-Immigrant-Access-to-Health-and-Human-Services.pdf
- Giuntella O., Lonsky J. (2018). The Effects of DACA on Health Insurance, Access to Care, and Health Outcomes. Discussion Paper Series, Issue https://docs.iza.org/dp11469.pdf
- Gong F., Xu J., Fujishiro K., Takeuchi D. T. (2011). A life course perspective on migration and mental health among Asian immigrants: The role of human agency. Social Science & Medicine, 73(11), 1618–1626. 10.1016/j.socscimed.2011.09.014 [DOI] [PubMed] [Google Scholar]
- Guo M., Li M., Xu H., Stensland M., Wu B., Dong X. (2021). Age at migration and cognitive health among Chinese older immigrants in the United States. Journal of Aging and Health, 33(9), 709–720. 10.1177/08982643211006612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan J., Rodriguez N., Capps R., Kabiri N. (2003). The effects of recent welfare and immigration reforms on immigrants' access to health care. The International Migration Review, 37(2), 444–463. http://www.jstor.org/stable/30037845 [Google Scholar]
- Hoffman E. D., Jr., Klees B. S., Curtis C. A. (2000). Overview of the Medicare and Medicaid programs. Health Care Financing Review, 22(1), 175–193. https://pubmed.ncbi.nlm.nih.gov/25372783 [PMC free article] [PubMed] [Google Scholar]
- Hooker K., Phibbs S., Irvin V. L., Mendez-Luck C. A., Doan L. N., Li T., Turner S., Choun S. (2018). Depression among older adults in the United States by disaggregated race and ethnicity. The Gerontologist, 59(5), 886–891. 10.1093/geront/gny159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossoudji S. (2020). Immigrants Admitted to the United States, Federal Fiscal Years 1972-2000 Inter-university Consortium for Political and Social Research [distributor]. 10.3886/ICPSR37688.v2 [DOI]
- Ma K. P. K., Bacong A. M., Kwon S. C., Yi S. S., Ðoàn L. N. (2021). The impact of structural inequities on older asian Americans during COVID-19 [perspective]. Frontiers in Public Health, 9(1183). 10.3389/fpubh.2021.690014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride K., Bacong A. M., Reynoso A., Benjamin A. E., Wallace S. P., Kietzman K. G. (2020). Healthcare decision-making among dual-eligible immigrants: Implications from a study of an integrated medicare-medicaid demonstration program in California. Journal of Immigrant and Minority Health, 22(3), 494–502. 10.1007/s10903-019-00922-5 [DOI] [PubMed] [Google Scholar]
- Morey B. N., Bacong A. M., Hing A. K., de Castro A. B., Gee G. C. (2020). Heterogeneity in migrant health selection: The role of immigrant visas. Journal of Health and Social Behavior, 61(3), 359–376. 10.1177/0022146520942896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakphong M. K., De Trinidad Young M.-E., Morales B., Guzman-Ruiz I. Y., Chen L., Kietzman K. G. (2022). Social exclusion at the intersections of immigration, employment, and healthcare policy: A qualitative study of Mexican and Chinese immigrants in California. Social Science & Medicine, 298, 114833. 10.1016/j.socscimed.2022.114833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of SciencesE., MedicinePopulation, C. o. (2016). The integration of immigrants into American society. National Academies Press [Google Scholar]
- Novak N. L., Geronimus A. T., Martinez-Cardoso A. M. (2017). Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology, 46(3), 839–849. 10.1093/ije/dyw346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obinna D. N. (2014). The challenges of American legal permanent residency for family- and employment-based petitioners. Migration and Development, 3(2), 272–284. 10.1080/21632324.2014.914689 [DOI] [Google Scholar]
- Obinna D. N. (2020). Wait-times, visa queues and uncertainty: The barriers to American legal migration. Migration and Development, 9(3), 390–410. 10.1080/21632324.2020.1797456 [DOI] [Google Scholar]
- Patler C., Hamilton E. R., Meagher K., Savinar R. (2019). Uncertainty about DACA may undermine its positive impact on health for recipients and their children. Health Affairs, 38(5), 738–745. 10.1377/hlthaff.2018.05495 [DOI] [PubMed] [Google Scholar]
- Perreira K. M., Yoshikawa H., Oberlander J. (2018). A new threat to immigrants’ health—the public-charge rule. The New England Journal of Medicine, 379(10), 901–903. 10.1056/nejmp1808020 [DOI] [PubMed] [Google Scholar]
- Ro A., Fleischer N. L., Blebu B. (2016). An examination of health selection among U.S. immigrants using multi-national data. Social Science & Medicine, 158, 114–121. 10.1016/j.socscimed.2016.04.023 [DOI] [PubMed] [Google Scholar]
- Ro A., Van Hook J. (2021). Comparing immigration status and health patterns between Latinos and asians: Evidence from the survey of income and program participation. Plos One, 16(2), e0246239. 10.1371/journal.pone.0246239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggles S., Flood S., Foster S., Goeken R., Pacas J., Schouweiler M., Sobek M. (2021). IPUMS USA. (Version 11.0) IPUMS 10.18128/D010.V11.0 [DOI]
- Sabado-Liwag M. D., Manalo-Pedro E., Taggueg R., Bacong A. M., Adia A. C., Demanarig D., Sumibcay J. R., Valderama-Wallace C., Oronce C. I. A., Bonus R., Ponce N. A. (2022). Addressing the interlocking impact of colonialism and racism on filipinx/a/o American health inequities. Health Affairs, 41(2), 289–295. 10.1377/hlthaff.2021.01418 [DOI] [PubMed] [Google Scholar]
- StataCorp (2021). Stata statistical software: Release 17. StataCorp LLC. [Google Scholar]
- Torres J. M., Young M.-E. D. (2016). A life-course perspective on legal status stratification and health. SSM - Population Health, 2, 141–148. 10.1016/j.ssmph.2016.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Citizenship and Immigration Services . (2017, November, 27, 2017). Green Card for Lautenberg Parolee. U.S. Department of Homeland Security. Retrieved May 3, 2022 from https://www.uscis.gov/green-card/green-card-eligibility/green-card-for-a-lautenberg-parolee
- U.S. Citizenship and Immigration Services . (2022, April 27, 2022). Chapter 9 - Amerasian Immigrants. U.S. Department of Homeland Security. Retrieved May 3, 2022 from https://www.uscis.gov/policy-manual/volume-7-part-p-chapter-9
- U.S. Department of State - Bureau of Consular Affairs . (2022, May 3, 2022). Directory of Visa Categories. U.S. Department of State. Retrieved May 3, 2022 from https://travel.state.gov/content/travel/en/us-visas/visa-information-resources/all-visa-categories.html
- Van Hook J., Bachmeier J. D., Coffman D. L., Harel O. (2015). Can we spin straw into gold? An evaluation of immigrant legal status imputation approaches. Demography, 52(1), 329–354. 10.1007/s13524-014-0358-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkataramani A. S., Shah S. J., O'Brien R., Kawachi I., Tsai A. C. (2017). Health consequences of the US deferred action for childhood arrivals (DACA) immigration programme: A quasi-experimental study. The Lancet Public Health, 2(4), e175–e181. 10.1016/S2468-2667(17)30047-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vespa J., Medina L., Armstrong D. M. (2018). Demographic Turning Points for the United States: Population Projects for 2020 to 2060. Current Population Reports, Issue. U. S. C. Bureau https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf
- Wallace S. P., Young M. E. d. T. (2018). Immigration versus immigrant: The cycle of anti-immigrant policies. American Journal of Public Health, 108(4), 436–437. 10.2105/AJPH.2018.304328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace S. P., Young M.-E. D. T., Rodríguez M. A., Brindis C. D. (2019). A social determinants framework identifying state-level immigrant policies and their influence on health. SSM - Population Health, 7, 100316. 10.1016/j.ssmph.2018.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young M.-E. D. T., Leon-Perez G., Wells C. R., Wallace S. P. (2019). Inclusive state immigrant policies and health insurance among Latino, Asian/Pacific Islander, Black, and White noncitizens in the United States. Ethnicity & Health, 24(8), 960–972. 10.1080/13557858.2017.1390074 [DOI] [PubMed] [Google Scholar]
- Young M.-E. D. T., Wallace S. P. (2019). Included, but deportable: A new public health approach to policies that criminalize and integrate immigrants. American Journal of Public Health, 109(9), 1171–1176. 10.2105/ajph.2019.305171 [DOI] [PMC free article] [PubMed] [Google Scholar]