Abstract
Purpose: To provide pharmacy leaders and clinicians with the basic principles of a training method called job instruction (JI) and its application within pharmacy as a strategy to teach routine pharmacy work. Summary: Job instruction is a reliable way to teach a person to quickly learn how to perform a work standard correctly, safely, and efficiently. Job instruction is a proven and successful technique for improving time to train, productivity, employee turnover and quality of work. In healthcare, JI training is not well-known or widely utilized. Job Instruction was the strategy of choice to stabilize the variable training practices within The University of Kansas Health System pharmacy enterprise, and a prospective, single center, multi-cohort study was conducted to study its impact. Conclusion: The preliminary results of this study provide initial insight into the applicability of job instruction in pharmacy. The study indicated the benefits of JI training within different teams to standardize training practices, decrease error and safety event rates, and increase satisfaction of team members with on-the-job training. The results of this study will be used to further analyze and optimize training practices in The University of Kansas Health System pharmacy enterprise.
Keywords: staff development, pharmacy administration, education, pharmacy, teaching, pharmacy service, hospital, quality Improvement
Introduction
The field of healthcare is rapidly growing and changing, and with this change comes the increased use of continuous improvement methods. Healthcare institutions are moving toward methods that help minimize waste with ongoing process improvement along with finding opportunities for generating and sustaining value-added processes. Training Within Industry (TWI) principles is one avenue to achieve this. Training Within Industry is a precursor model to Lean that aligns with common organizational goals at all levels such as retaining skilled staff, increasing patient safety, improving caregiver training, increasing the quality of care, reducing waste, and establishing best practices.1 -3 It was a program developed in the United States during World War II to support the increase in production needs by the Allied forces. The purpose of TWI can be summarized by how it was advertised in 1943, essentially to assist war production industries by training each worker to make the fullest use of their skill to enable production to keep pace with war demands. 4 By helping to establish methods to create work standards and effective training processes, TWI principles create a skilled and engaged workforce. During this time, TWI methodologies were also applied in healthcare facilities, due to the shortage of hospital workers during the war. 5
The foundation of TWI principles contains 4 components: job instruction (JI), job methods, job relations, and program development.6 -8Job instruction is the core component of TWI principles that focuses on the development and training of standard job practices. The focus of JI is a way to quickly teach a person a standard way to perform the work. As the front line is engaged in the development of those standards, JI is also a training tool that promotes the engagement, continuous improvement, and problem solving of existing team members.7,8 The identification of work elements, key points, and the reasons why a particular key point is “key” are the elements behind how a task can be methodically broken down to be done the “one best way” which is called a job breakdown. 8 The training process is essentially simplified and broken down into vital functions, and is based around the premise of “learning-by-doing.”2,3 Job breakdown sheets and the 4-step instruction method are the foundation on which JI training is built on. 8 The 4-step method is illustrated in Figure 1. Participants who go through the formal JI training process are taught to teach the current accepted standard and not deviate from steps listed on the job breakdown form. 2 This standardization of the job eliminates practice variation, reduces errors, and increases productivity. An example template of a job breakdown form is illustrated in Figure 2.
Figure 1.
The 4-step Method of Job Instruction. 7
Figure 2.
TUKHS Job Breakdown Sheet Example.
In healthcare, job instruction can help bridge the gap in providing more effective training for new staff while also continually updating best practices for veteran staff. 5 For example, Virginia Mason Medical Center (VMMC), a 336-bed hospital, employed JI methodologies to train staff on hand hygiene job breakdowns. Baseline audits prior to JI at VMMC showed that only 83.5% of staff were washing their hands properly and on a consistent basis. After piloting JI training in 467 nurses at VMMC, the reliability of hand hygiene in this pilot population went above 98%.
The University of Kansas Health System (TUKHS) saw an opportunity to incorporate JI in its training processes to address variability, increase efficiency and productivity, and decrease on the job errors. Integration of JI methodologies into the pharmacy staff training model was the focus of this pilot study. The goal of this study is not intended to teach readers how to structure and implement JI training. The intent is to report an example of JI implementation that will help pharmacy health system leaders and clinicians understand how applying JI concepts to routine clinical and operational tasks within a pharmacy department can lead to positive impacts of change such as reduction in error rates and increase in training satisfaction of staff.
Job Instruction Evaluation at The University of Kansas Health System
The impact of JI training at TUKHS was evaluated as a prospective, single center, multi- cohort study within the inpatient and outpatient pharmacy departments. The University of Kansas hospital in Kansas City where this study took place is an academic medical center that staffs over 900 inpatient beds. The study period was from May 1st, 2020 to June 1st, 2021. There was a formal review by the Institutional Review Board and this study was granted exemption status. Training Within Industry training was launched by interested pharmacy areas to train current staff on JI methodology; training consisted of a 9-week cohort course with a targeted 1-week JI certification training for pharmacy leadership and frontline trainers per cohort. Job Instruction fundamentals of job breakdown sheets and the 4-step instruction method were utilized during a dedicated JI training week. Table 1 showcases the schedule of the 9-week cohort course, included the 1-week JI certification training embedded within module 3 of the course. The course was taught by a master trainer, which was a pharmacy department staff position specifically created at TUKHS to develop and implement TWI-based training and education. Pharmacy staff members who finished the 9-week cohort course would be deemed certified JI trainers and go on to train pharmacy staff members, in their respective pharmacy departments, on various job breakdowns.
Table 1.
TUKHS Pharmacy Training Modules Adapted from the Toyota Talent Development Process. 8
| Module | Target Participants | Duration | Time Commitment |
|---|---|---|---|
| Module 1: Developing Talent | LeadershipTWI Master Trainer | Complete Prior to Module 2 | • 60 min meeting |
| • 120 min training session | |||
| Module 2: Identify Critical Knowledge | Leadership | 2 Weeks | • Two 120 min training sessions |
| TWI Master Trainer | |||
| Module 3: Transfer Knowledge to Others | Leadership | 3 Weeks | • 60 min meeting |
| TWI Master Trainer | • 20 to 30 min tasks (variable) | ||
| Training Team– (Training Week only) | • Weeklong training session (8 hours × 5 days) | ||
| Module 4: Verify Learning and Success | Leadership | 4 Weeks | • One 120 min training session |
| TWI Master Trainer | • Minimum of three 90-120 min meetings |
Abbreviations: TUKHS, The University of Kansas Health System; TWI, Training Within Industry.
The primary objective was to evaluate if applying JI training would impact 3 key areas of interest: the reduction of error rates, increase in applied learning skills from training, and increase in job satisfaction of staff. Data was obtained from conducted audits, survey responses, automatic dispensing cabinet stockout reports, and an institutional safety incident reporting portal. The Kirkpatrick evaluation model was used to analyze the results of JI training on pharmacy department staff (see Table 2). This evaluation methodology is a 4 level evaluation tool that it utilized to create, deliver, measure and validate training standards. 9 Levels 1, 2, and 3 focus on the impact of learning on the participants; these levels assess whether participants engaged with the content and acquired the intended knowledge and skill. In this study, level 1 and 2 results were assessed independently by the master trainer (and not included within the scope of this study) and level 3 results were assessed by a survey questionnaire that was distributed to pharmacy staff prior to JI training and post-JI training. Level 4 is dedicated to measuring the direct results of the intended training (key performance indicators), which are established prior to the training being initiated. One focus of this pilot study was to track and report pre-specified key performance indicators for each job breakdown to see what impact a standardized approach to training had on these job functions.
Table 2.
The 4 Levels of the Kirkpatrick Evaluation Model. 9
| Level 1: Reaction | The degree to which participants find the training favorable, engaging, and relevant to their jobs |
| Level 2: Learning | The degree to which participants acquire the intended knowledge, skills, attitude, confidence, and commitment based on their participation in the training |
| Level 3: Behavior | The degree to which participants apply what they learned during training when they are back on the job |
| Level 4: Results | The degree to which target outcomes occur as a result of the training |
Overall Cohort Results
Since the initiation of TWI cohorts and JI training within the TUKHS pharmacy enterprise, there have been 8 total cohorts that have completed their the 9-week training modules. A total number of 67 pharmacy team members completed JI certification since initiation of the program through the duration of this study, which included pharmacists, pharmacy residents, and pharmacy technicians (see Table 3). The fundamental skills of creating job breakdowns are taught to JI trainers during the cohort process, and cohorts will continue to write, validate, and train to different job breakdowns as time goes on.
Table 3.
Number of TUKHS Pharmacy Staff Members that are Job Instruction Trained.
| Pharmacy Department | ||||||
|---|---|---|---|---|---|---|
| Role | Acute Care Pharmacy | Cancer Care Pharmacy | Home Infusion Pharmacy | Outpatient Pharmacy | Miscellaneous | Grand Total |
| Front Line Team Member | ||||||
| Pharmacist | 8 | 1 | 0 | 2 | 0 | 11 |
| Technician | 11 | 0 | 3 | 4 | 0 | 18 |
| Leadership Team Member | ||||||
| Pharmacy Leader | 6 | 1 | 2 | 6 | 0 | 15 |
| Residents | 0 | 0 | 0 | 0 | 4 | 4 |
| Technician Leader | 6 | 4 | 3 | 6 | 0 | 19 |
| Grand Total | 31 | 6 | 8 | 18 | 4 | 67 |
Abbreviations: TUKHS, The University of Kansas Health System.
The following 3 charts (Figures 3-5) showcase results from a survey questionnaire that was distributed to pharmacy staff in the areas that completed JI training. The survey was given to participants prior to the implementation of job instruction in their area and then the same survey was given post-training to compare differences in response. There were a total of 43 individual responses collected in the pre-survey and 43 individual responses in the post-training survey. The data show that, with newly certified trainers delivering the training, there was an increase in not only applied learning skills but also staff satisfaction in their training experience post JI implementation.
Figure 3.
Survey Questionnaire Results: Worker Assessment of the Trainer.
Figure 4.
Survey Questionnaire Results: Worker Self-Assessment.
Figure 5.
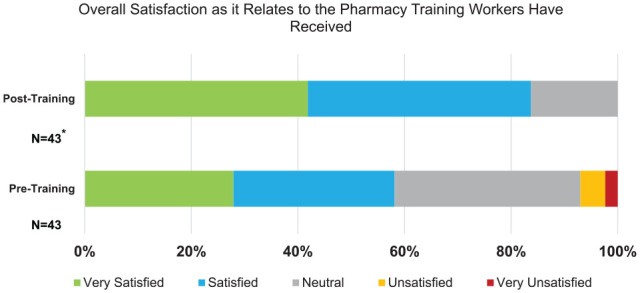
Survey Questionnaire Results: Worker Overall Satisfaction Self-Assessment.
*No unsatisfied or very unsatisfied responses were reported in the post-training survey results.
The Kirkpatrick Evaluation Model Outcome Categorization
As a relatively new concept in the healthcare space, job instruction has shown significant improvements in the way we are training our pharmacy teams and the benefits that standardized training can provide. There were many positive impacts of change seen in reduction in error rates, increase in applied learning skills from training, increase in job satisfaction of staff, and the time to train a staff member on a particular task. The following outcome results illustrate the impact of JI in various areas within TUKHS pharmacy. Post-JI training level 4 key indicator data was collected at various timepoints (up to 6 months post-JI training). Each JI cohort got to choose which key performance measures they wanted to track for each job breakdown they created. Examples of level 4 results from the Kirkpatrick evaluation model from our cohorts included:
-
Intravenous (IV) room hood set-up audits (IV room technician cohort)
80% reduction in aseptic defects in setting up a standardized IV laminar or vertical flow hood 4 months post-training of IV room staff. Defect was defined as missing any step in the IV hood set-up protocol.
-
Automated dispensing cabinet cycle count audits (inpatient floor technician cohort)
Up to 9% decrease in baseline defects of random floor automatic dispensing cabinet pocket audits 1-month post-job instruction training implementation. Average number of monthly audits were 45 random inpatient floor cabinet pockets per month. Baseline defects included: correct count in medication pocket, correct medication in pocket, and correct expiration date entered
-
Automated dispensing cabinet stockouts (inpatient floor technician cohort)
Stockouts create a delay in patient care and extra workload for hospital team members. Baseline stockout rate was 0.56 total stockouts per 100 dispenses, and post-JI training was 0.41 total stockouts per 100 dispenses.
-
Increase in job satisfaction of staff (all cohorts; Figure 5)
There were no “Unsatisfied” or “Very Unsatisfied” responses in the post-training survey given to staff that assessed overall satisfaction as it related to the pharmacy training they had received at TUKHS. One component of this could be attributed to the efficiency of the training process utilizing job breakdowns. Average time to train a staff member on one job breakdown is about 20 to 30 minutes
An example of Level 3 results from the Kirkpatrick Evaluation Model from our cohorts included:
There was an increase in applied learning for both the trainer and the worker in 3 of the 4 steps of the 4-step method, excluding step number 4, as assessed by the self-reported surveys given to those who were trained on a job breakdown by a certified JI trainer. Step 4 was the follow-up step, and included encouraging the worker to ask questions, connecting the worker with someone who would support them if they needed help once they started to do the task independently, and periodically checking back in on them. This highlights an opportunity for TUKHS to focus in on this critical step of the process as we move forward. Examples of level 2 results from the Kirkpatrick evaluation model from our cohorts included:
-
Creation of job breakdowns during the TWI cohort process
The fundamental skills of creating job breakdowns are taught to JI trainers during the cohort process, and cohorts will continue to write, validate, and train to different job breakdowns as time goes on. For example: the IV room technician cohort has created 13 job breakdowns that have gone through the validation phase and are now part of the training plans of IV room pharmacy technicians.
Conclusion
The preliminary results of this study provide initial insight into the applicability of job instruction training in pharmacy. The pharmacy enterprise at TUKHS has and will continue to benefit from TWI principles and JI training within different teams to standardize training practices, decrease error and safety event rates, and increase satisfaction of team members with on-the-job training. The results of this study will be used to further analyze and optimize training practices within the pharmacy enterprise, and we hope these results encourage other institutions to adopt TWI and JI methodologies. Having a dedicated TWI master trainer staff position was necessary at TUKHS to implement TWI training methodologies. The master trainer took certified TWI coursework to become knowledgeable in this area and worked closely with the TUKHS pharmacy leadership team to set-up and implement JI training in different pharmacy departments within this initial pilot. With the initiation of the JI training program, the goal is to eventually have 100% of pharmacy staff supported by a 1:8 ratio of certified JI trainers, which would equate to 15 to 20% of pharmacy staff being JI trainer certified. These certified JI trainers would then be able to continue to train new and veteran employees on various job breakdowns as time went on.
It is important to note that many of the TUKHS pilot cohorts were conducted during the start of the COVID-19 pandemic. This led to prolonged training timelines due to a multitude of reasons. One main reason was the shortage of JI certified trainers for on-the-job training due to staffing needs. There was also decreased engagement and accountability of cohort leadership due to increased needs of daily operational problem-solving. Some training sessions and touchbases were also conducted via virtual sessions instead of originally planned in-person sessions, which could have decreased training impact and engagement.
Future program direction includes a continued emphasis on increased accountability of all levels of management involved in training. This will be done through increased stakeholder engagement and understanding of TWI and JI training prior to cohort implementation. Cohort specific metrics will also continue to be tracked to showcase the impact of standardized training practices and increased employee engagement.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Faria Munir  https://orcid.org/0000-0001-6642-498X
https://orcid.org/0000-0001-6642-498X
References
- 1. What is training within industry (TWI)? TWI Institute. Accessed May 31, 2022. https://www.twi-institute.com/twi-training/ [Google Scholar]
- 2. Pascual AA. Training Within Industry in the Emergency Department: Team Development to Improve Patient Care and Alleviate Staff Burnout. ProQuest Dissertations Publishing, 2017. [Google Scholar]
- 3. Donald D. Training Within Industry: The Foundation of Lean. Productivity Press; 2005. [Google Scholar]
- 4. Labor Division. War Production Board. Training Within Industry Service. The Training Within Industry Program, Bulletin No. 1. U.S. Government Printing Office; 1943. [Google Scholar]
- 5. Graupp P. Getting to Standard Work in Health Care: Using TWI to Create a Foundation for Quality Care. CRC Press; 2017. [Google Scholar]
- 6. Bianchi N, Giorcelli M. The dynamics and spillovers of management interventions: Evidence from the training within industry program. J Polit Econ. 2022;130(6):1630-1675. doi: 10.1086/719277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huntzinger J. The roots of lean: Training within industry: The origin of Japanese management and kaizen. Target. 2002, 18(1). https://www.lean.org/downloads/105.pdf [Google Scholar]
- 8. Liker JK, Meier D. Toyota Talent: Developing Your People the Toyota Way. McGraw-Hill; 2007:35-256. [Google Scholar]
- 9. Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick’s Four Levels of Training Evaluation. Atd Press; 2016. [Google Scholar]






