Abstract
Aims
The aim is to evaluate associations of lung function impairment with risk of incident heart failure (HF).
Methods and results
Data were pooled across eight US population-based cohorts that enrolled participants from 1987 to 2004. Participants with self-reported baseline cardiovascular disease were excluded. Spirometry was used to define obstructive [forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) <0.70] or restrictive (FEV1/FVC ≥0.70, FVC <80%) lung physiology. The incident HF was defined as hospitalization or death caused by HF. In a sub-set, HF events were sub-classified as HF with reduced ejection fraction (HFrEF; EF <50%) or preserved EF (HFpEF; EF ≥50%). The Fine–Gray proportional sub-distribution hazards models were adjusted for sociodemographic factors, smoking, and cardiovascular risk factors. In models of incident HF sub-types, HFrEF, HFpEF, and non-HF mortality were treated as competing risks. Among 31 677 adults, there were 3344 incident HF events over a median follow-up of 21.0 years. Of 2066 classifiable HF events, 1030 were classified as HFrEF and 1036 as HFpEF. Obstructive [adjusted hazard ratio (HR) 1.17, 95% confidence interval (CI) 1.07–1.27] and restrictive physiology (adjusted HR 1.43, 95% CI 1.27–1.62) were associated with incident HF. Obstructive and restrictive ventilatory defects were associated with HFpEF but not HFrEF. The magnitude of the association between restrictive physiology and HFpEF was similar to associations with hypertension, diabetes, and smoking.
Conclusion
Lung function impairment was associated with increased risk of incident HF, and particularly incident HFpEF, independent of and to a similar extent as major known cardiovascular risk factors.
Keywords: Spirometry, Lung function, Heart failure, Prospective cohort study
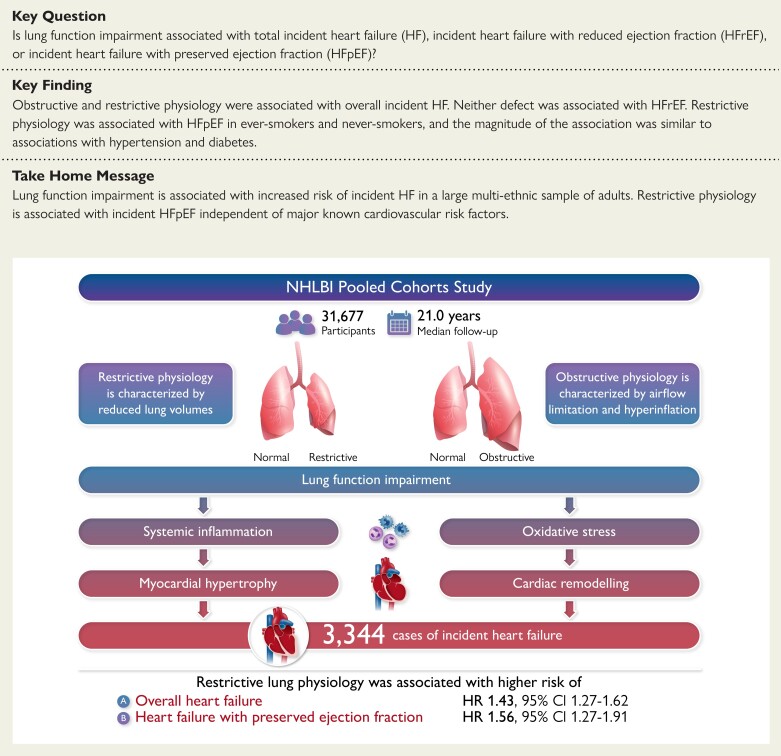
Structured Graphical Abstract
Structured Graphical Abstract.
In the NHLBI Pooled Cohorts Study, lung function impairment was associated with increased risk of incident HF, and particularly incident HFpEF, independent of and to similar extent as major known cardiovascular risk factors.
See the editorial comment for this article ‘HFp2EF: heart failure with pulmonary dysfunction and preserved ejection fraction?’, by B.A. Maron and M. Humbert, https://doi.org/10.1093/eurheartj/ehac201.
Introduction
Heart failure (HF) affects over 26 million people worldwide.1 Despite recent advances in HF treatment, HF patients require frequent hospitalization and approximately half die within 5 years of HF diagnosis.2 Identifying HF risk factors is critically important to inform HF prevention and treatment.
Lung disease may represent an important yet under-appreciated HF risk factor. The HF and chronic lung disease are frequent comorbidities, with HF affecting one in five individuals with chronic obstructive pulmonary disease (COPD).3 While this may be due in part to shared risk factors such as smoking and ageing,4 there is evidence that lung function impairment may contribute directly to HF pathogenesis. Reduced lung function is associated with increased systemic inflammation,5 which may generate endothelial inflammation in the coronary microvasculature.6 Microvascular endothelial inflammation may in turn generate cardiac hypertrophy and accelerated atherosclerosis, which contribute to HF development.7
Although prior studies have suggested associations between lung function impairment and risk of HF, the extent to which these relationships are independent of potential confounding factors such as race/ethnicity and smoking remains unclear due to the use of primarily non-Hispanic White populations, limitations in measurement of smoking exposures, and study of populations with low HF incidence rates among healthy non-smokers.8–11 In addition, there have been no large studies discriminating associations between lung function impairment and HF sub-types—namely, HF with reduced ejection fraction (HFrEF) vs. preserved EF (HFpEF)—which differ in pathogenesis and responsiveness to current HF therapies.12 The HFrEF is characterized by impaired cardiac contractility and responds to neurohormonal-blocking medications,13 while HFpEF is defined by abnormal cardiac stiffness and does not improve with neurohormonal blockade.14 We therefore aimed to define associations of lung function with total incident HF, incident HFrEF, and incident HFpEF in a large multi-ethnic sample of US adults.
Methods
Study population
The National Heart, Lung and Blood Institute (NHLBI) Pooled Cohorts Study15 harmonized data from eight prospective population-based studies that surveilled for HF events: Atherosclerosis Risk in Communities (ARIC) study;16 Coronary Artery Risk Development in Young Adults (CARDIA);17; Cardiovascular Health Study;3,18 Framingham Offspring Cohort (FHS-O);19 Health, Aging and Body Composition (Health ABC);20 Jackson Heart Study (JHS);21 Multi-Ethnic Study of Atherosclerosis (MESA);22 and Strong Heart Study.23 Design features for each cohort are described in Supplementary material online, Table S1. Participants with baseline self-reported cardiovascular disease were excluded from the analyses.
The NHLBI Pooled Cohorts Study was funded by the NHLBI. The study was approved by NHLBI as well as the institutional review boards of all collaborating institutions and complies with the Declaration of Helsinki. All participants provided written informed consent.
Spirometry
Spirometry was performed using water-seal, dry-rolling, seal, or flow-sensing spirometers in accordance with American Thoracic Society guidelines and was quality controlled using 2005 criteria.24 The spirometry methods produce comparable measurements of forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC).25 The definitions for obstructive and restrictive physiology were mutually exclusive. Obstructive physiology was defined as the presence of airflow limitation, which was operationalized as FEV1/FVC <0.70.26 Among participants without airflow limitation (FEV1/FVC ≥0.7), restrictive physiology was defined as FVC <80% predicted. The first available spirometry measurement was treated as the baseline assessment. Participants without available spirometry at the time of study enrolment were included if they had available spirometry from a subsequent visit. Follow-up was started at the first spirometry assessment and all covariates were measured at the first spirometry examination. In the six cohorts that performed multiple spirometry measurements, annual lung function decline was defined as the difference between the first and second spirometry measurements divided by years elapsed.27
Outcomes
The primary outcome was a composite of HF hospitalization or death due to HF. Participants in each cohort were contacted at regular intervals to identify deaths and hospitalizations, and HF events were adjudicated in each cohort based on a protocolized review of medical records as previously described.23,28–32 Classification criteria were similar across cohorts and are summarized in Supplementary material online, Table S2; they required a clinical HF diagnosis as well as documentation of specific signs, symptoms, and/or use of specific medications. Six cohorts reviewed records for left ventricular function assessment at the time of HF diagnosis (see Supplementary material online, Table S2). The CARDIA and JHS classified HFrEF if EF was <50% and HFpEF if EF was ≥ 50%; echocardiographic diastolic function parameters were not available to inform HFpEF ascertainment.33 To ensure standardization across cohorts, the same definitions were applied in the remaining cohorts.
Covariates
Age, birth year, sex, education, race/ethnicity, smoking status, and smoking pack-years were self-reported (see Supplementary material online, Table S1). Lifetime smoking status was classified as never or ever by comparison of self-reported smoking status over all available examinations.15 Height, weight, and systolic and diastolic blood pressure were measured using standard methods. Total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), glucose, creatinine, and fibrinogen were measured in fasting blood samples. Obesity was defined as body mass index (BMI) >29.9 kg/m2. Medications were self-reported or assessed via medication inventories. Diabetes was self-reported or defined by fasting blood glucose (≥126 mg/dL) or use of relevant medications. Hypertension was defined by blood pressure (≥140/90 mmHg) or use of anti-hypertensive medications. The estimated glomerular filtration rate (eGFR) was calculated by the Chronic Kidney Disease Epidemiology Collaboration equation.34 Beyond the exclusion of participants with missing or invalid spirometry and censoring associated with loss to follow-up and non-HF mortality, 5406 participants (14.6%) were missing data for one or more covariates (see Supplementary material online, Figure S1). Additionally, 7921 (33%) participants were missing data for eGFR and 12 190 (64%) participants were missing data for fibrinogen, though these covariates were only incorporated into sensitivity analyses.
Statistical analyses
The cumulative incidence functions for incident HF were plotted for obstructive and restrictive lung physiology using preserved lung function as the referent. Associations between lung function and HF were analysed using the Fine–Gray proportional sub-distribution hazards models.35 The proportional hazards assumption was confirmed by residual plots. The linearity assumption for continuous lung function was tested using Supremum test for functional form; a non-significant P-value concludes that the linearity assumption of the continuous variable holds. Effect estimates for continuous exposures were reported per standard deviation decrement, and associations were plotted using post hoc generalized additive models.
In models of incident HF, non-HF mortality was treated as the competing risk. Time-to-event was defined as age-at-event with left truncation for age at study entry. Study cohort was treated as a stratum term to allow for different baseline hazards. Models were adjusted for a priori confounders including age/birth year (centred), sex, race/ethnicity, educational attainment, clinical site, height, weight, smoking status, smoking pack-years, systolic/diastolic blood pressure, total cholesterol, hypertension status, diabetes status, and statin use at baseline. The magnitude of confounding by each covariate was assessed by a leave-one-out approach. For analyses of lung function decline, the follow-up period started at the second spirometry assessment and models were adjusted for baseline lung function. Participants who developed HF between the first and second spirometry measurements were excluded from analyses evaluating associations of lung function decline with incident HF.
In models of incident HF sub-types with the same set of predictors, incident HF cases without EF measurements (n = 1278) were excluded, and HFrEF, HFpEF, and non-HF mortality were treated as competing risks. Non-HF deaths were defined as deaths that were not adjudicated as primarily or secondarily attributable to HF. In order to investigate the impact of missing covariate and HF sub-type data, 30 imputed data sets were generated and associations of baseline lung function with incident HF were re-evaluated using imputed data sets. Bootstrap analyses were used to perform statistical comparisons of effect estimates [log hazard ratio (HR)] for a given predictor with respect to HFrEF vs. HFpEF. Specifically, 34 bootstrap samples were generated and analysed for each of the 30 imputed data sets, and the results for all 1020 bootstrap samples were used to evaluate statistical significance of the difference between corresponding HRs predicting HFrEF vs. HFpEF. Models predicting HFrEF and HFpEF were estimated for each sample, and the difference in the coefficients of the predictor between the two models was calculated; if 995 or more of the differences had the same sign (positive vs. negative), then the effect of the predictor on HFrEF vs. HFpEF was judged to be significantly different (two-tailed P < 0.05). Because results for the complete cases were substantively the same as results for the imputed data sets, complete case analyses are presented as the main results. In order to contextualize the risk conferred by ventilatory defects, the relative magnitudes of associations between obstructive and restrictive lung physiology and incident HFrEF and HFpEF were compared with dichotomized HF risk factors [hypertension, diabetes, obesity, current smoking, and abnormal lipid profile (total cholesterol ≥200 mg/dL; HDL <40 mg/dL in men and <50 mg/dL in women36)] using sub-distribution hazards models adjusted for age, sex, race/ethnicity, site, educational attainment, smoking pack-years, and statin use. These models were not adjusted for comparative cardiovascular risk factors.
To assess potential effect measure modification, models were stratified by age, sex, race/ethnicity, BMI, and smoking status, and multiplicative two-way interaction terms were tested. In sensitivity analyses, incident HF events were censored if they were simultaneously classified as chronic lower respiratory disease (CLRD)-related events (i.e. COPD, emphysema, chronic bronchitis, or asthma),37 occurred <2 years after the baseline spirometry examination, or followed interim myocardial infarction (MI) events.
A two-tailed alpha of 0.05 was considered significant for all analyses. Analyses were completed using SAS, version 9.4 (Cary, NC, USA).
Results
Baseline characteristics
Among 31 677 participants, the mean baseline age was 54.0 ± 15.5 years, 56% were women, and 62% were non-Hispanic White (Table 1). Baseline spirometry demonstrated obstructive physiology in 20% and restrictive physiology in 7% of participants. Complete follow-up for incident HF was available for 93.9% of participants at 5 years, 80.9% at 10 years, and 63.7% at 15 years. Incomplete follow-up stemmed largely from non-HF mortality.
Table 1.
Baseline characteristics of participants from eight population-based cohorts stratified by incidence of heart failure events
| No HF (n = 28 333) | Incident HF (n = 3344) | Total (n = 31 677) | |
|---|---|---|---|
| Total spirometry follow-up, person-years | 259 220 | 19 107 | 278 327 |
| Total HF follow-up, person-years | 554, 245 | 54 121 | 608 366 |
| Age, years, mean ± SD | 53.0 ± 15.6 | 62.2 ± 11.3 | 54.0 ± 15.5 |
| Sex, n (%) | |||
| Femalea | 15 948 (56.3) | 1827 (54.6) | 17 775 |
| Male | 12 385 (43.7) | 1517 (45.4) | 13 902 |
| BMI, kg/m2, mean ± SD | 27.3 ± 5.6 | 28.8 ± 5.8 | 27.5 ± 5.6 |
| Race/ethnicity, n (%) | |||
| European-American | 17 168 (60.6) | 2357 (70.5) | 19 525 |
| African-American | 8545 (30.2) | 786 (23.5) | 9331 |
| Asian-American | 569 (2.0) | 14 (0.4) | 583 |
| Hispanic/Latino | 793 (2.8) | 21 (0.6) | 814 |
| American-Indian | 1258 (4.4) | 166 (5.0) | 1424 |
| Education status, n (%) | |||
| Less than high school | 3046 (10.7) | 525 (15.7) | 3571 |
| High school | 7866 (27.8) | 1009 (30.2) | 8875 |
| Some college | 5097 (18.0) | 371 (11.1) | 5468 |
| College or more | 12 324 (43.5) | 1439 (43.0) | 13 763 |
| Smoking status, n (%) | |||
| Never | 13 384 (47.2) | 1309 (39.1) | 14 693 |
| Former | 8872 (31.3) | 1294 (38.7) | 10 166 |
| Current | 6077 (21.5) | 741 (22.2) | 6818 |
| Pack-years in ever-smokers, years, median (IQR) | 16.5 (5.0–34.3) | 25.3 (11.0–41.0) | 17.5 (5.6–35.3) |
| Comorbidities, n (%) | |||
| Asthmab | 1702 (6.0) | 227 (6.8) | 1929 |
| COPDc | 2176 (87.0) | 326 (13.0) | 2502 |
| Hypertensiond | 11 414 (40.3) | 2121 (63.4) | 13 535 |
| Diabetese | 3031 (7.7) | 707 (21.1) | 3738 |
| Baseline lung function, mean ± SD | |||
| FEV1 (L) | 2.8 ± 0.9 | 2.5 ± 0.8 | 2.8 ± 0.9 |
| FVC (L) | 3.7 ± 1.0 | 3.3 ± 1.0 | 3.6 ± 1.0 |
| FEV1, per cent predicted | 94.8 ± 16.9 | 89.8 ± 18.9 | 94.3 ± 17.2 |
| FVC, per cent predicted | 97.9 ± 14.7 | 93.7 ± 16.1 | 97.5 ± 14.9 |
| FEV1/FVC | 0.76 ± 0.09 | 0.73 ± 0.09 | 0.76 ± 0.09 |
| Obstructive physiology, n (%) | 5305 (18.7) | 968 (28.9) | 6273 |
| Restrictive physiology, n (%) | 1844 (6.5) | 366 (10.9) | 2210 |
| No. of spirometry examinations | 2.4 ± 1.3 | 2.0 ± 0.9 | 2.3 ± 1.3 |
| Spirometry follow-up, years | 9.1 ± 10.2 | 5.7 ± 7.1 | 8.8 ± 10.0 |
| Change in FEV1, mL/yearf | −36.8 ± 64.4 | −44.1 ± 63.1 | −37.5 ± 64.3 |
| Change in FVC, 11 937 mL/year | −39.3 ± 78.8 | −52.4 ± 80.1 | −40.7 ± 79.0 |
| Change in FEV1/FVC per year | −0.2 ± 1.2 | −0.2 ± 1.3 | −0.2 ± 1.2 |
| Cohort, n (%) | |||
| ARIC | 11 937 (42.1) | 1736 (51.9) | 13 673 |
| CARDIA | 4809 (17.0) | 70 (2.1) | 4879 |
| CHS | 1682 (5.9) | 713 (21.3) | 2395 |
| FHS offspring | 1693 (6.0) | 123 (3.7) | 1816 |
| Health ABC | 1491 (5.3) | 357 (10.7) | 1848 |
| JHS | 1777 (6.3) | 75 (2.2) | 1852 |
| MESA | 3686 (13.0) | 104 (3.1) | 3790 |
| SHS | 1258 (4.4) | 166 (5.0) | 1424 |
ARIC, Atherosclerosis Risk in Communities; BMI, body mass index; CARDIA, Coronary Artery Risk Development in Young Adults; CHS, cardiovascular health study; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FHS, Framingham Heart Study; FVC, forced vital capacity; HF, heart failure; IQR, interquartile range; JHS, Jackson Heart Study; MESA, multi-ethnic study of atherosclerosis; SHS, strong heart study; SD, standard deviation.
Column percentages reported.
Self-reported physician-diagnosed asthma.
Self-reported physician-diagnosed COPD, chronic bronchitis, or emphysema.
Self-reported hypertension or systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or use of anti-hypertensive medications.
Self-reported diabetes or fasting blood sugar level ≥ 126 mg/dL or use of hypoglycaemic agents.
Lung function decline calculated among 22 528 participants with follow-up spirometry.
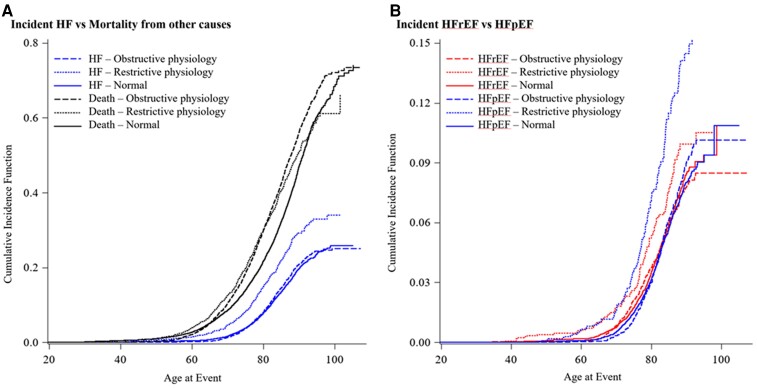
Incident heart failure
During a median follow-up of 21.0 years [interquartile range (IQR), 10.9–27.8], there were 3344 cases of incident HF (Table 2). Lower baseline FEV1 and FVC were associated with increased HF incidence (Table 2 and Supplementary material online, Figure S2). Associations were monotonic without evidence for non-linearity. Both restrictive and obstructive physiology were associated with incident HF (Table 2 and Figure 1A). The baseline FEV1/FVC was not associated with HF incidence, nor was accelerated decline in the FEV1 or the FVC (Table 2 and Supplementary material online, Figure S3). Associations of impaired lung function with incident HF persisted in multiple imputation analyses performed to account for missing covariate data (see Supplementary material online, Table S4).
Table 2.
Associations of baseline lung function and lung function decline with incident heart failure, incident heart failure with reduced ejection fraction, and incident heart failure with preserved ejection fraction
| Baseline lung functiona | Incident HFb | Incident HF sub-typesc | ||||
|---|---|---|---|---|---|---|
| Incident HFrEF | Incident HFpEF | |||||
| At risk with available baseline lung function | 31 677 | 27 455 | 27 455 | |||
| Events (cumulative incidence) | 3344 (10.6) | 1030 (3.8) | 1036 (3.8) | |||
| Incidence density rate/10 000 person-yearsd | 55.0 | 18.9 | 19.0 | |||
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Per one standard deviation decremente | ||||||
| FEV1 | 1.22 (1.15–1.30) | <0.001 | 1.13 (1.02–1.25) | 0.02 | 1.25 (1.12–1.39) | <0.001 |
| FVC | 1.32 (1.23–1.42) | <0.001 | 1.18 (1.05–1.34) | 0.007 | 1.29 (1.13–1.48) | 0.001 |
| FEV1/FVC | 1.02 (0.98–1.06) | 0.35 | 0.99 (0.92–1.06) | 0.11 | 1.05 (0.98–1.13) | 0.16 |
| Per category | ||||||
| Preserved lung function | Ref | Ref | Ref | |||
| Obstructive physiology | 1.17 (1.07–1.27) | <0.001 | 1.08 (0.92–1.26) | 0.47 | 1.30 (1.11–1.51) | <0.001 |
| Restrictive physiology | 1.43 (1.27–1.62) | <0.001 | 1.13 (0.89– 1.43) | 0.31 | 1.56 (1.27–1.91) | <0.001 |
| Lung function declinef | Incident HF | Incident HF sub-types | ||||
| Incident HFrEF | Incident HFpEF | |||||
| At risk with available lung function declineg | 22 528 | 20 564 | 20 564 | |||
| Events (cumulative incidence) | 2356 (10.5) | 739 (3.6) | 808 (3.9) | |||
| Incidence density rate/10 000 person-years | 59.9 | 19.9 | 21.8 | |||
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Per one standard deviation faster declineh | ||||||
| FEV1 decline | 1.03 (0.99–1.08) | 0.13 | 1.05 (0.98–1.13) | 0.20 | 1.01 (0.94–1.09) | 0.74 |
| FVC decline | 1.03 (0.99–1.07) | 0.14 | 1.04 (0.98–1.11) | 0.19 | 1.03 (0.96–1.11) | 0.37 |
| FEV1/FVC decline | 1.00 (0.96–1.05) | 0.84 | 1.03 (0.95–1.11) | 0.53 | 0.96 (0.89–1.04) | 0.34 |
CI, confidence interval; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HR, hazard ratio.
Separate sub-distribution hazards regression models were used to analyse the risk of incident HF and incident HF sub-types; all models adjusted for baseline age, sex, race, educational attainment, birth year, site, height, weight, smoking status, pack-years, systolic and diastolic blood pressure, total cholesterol, hypertension status, diabetes status, and statin use.
In models of incident HF, non-HF mortality was treated as the competing risk.
In models of incident HF sub-types, which were limited to the cohorts collecting data on ejection fraction, HFrEF, HFpEF, and non-HF mortality were treated as competing risks; interaction terms for HF sub-types did not reach statistical significance.
The incidence density rates (IDR)/10 000 person-years for HFpEF and HFrEF do not add up to the IDR/10 000 per-years for HF because the size of the at-risk population differs for HF and HF sub-types based on availability of ejection fraction measurements.
One SD of FEV1 = 0.9 L; one SD of FVC = 1.1 L; one SD of FEV1/FVC = 0.09.
Time-to-event is calculated from the time of the second spirometry.
Excluded 9149 individuals who did not have follow-up spirometry.
Decline was calculated between first and second spirometry visit. One SD of decline in FEV1 = 62.4 mL; one SD of decline in FVC = 78.9 mL; one SD of decline in FEV1/FVC = 0.01.
Figure 1.
Unadjusted Fine–Gray cumulative incidence curves showing cumulative failure rates due to (A) incident heart failure and mortality and (B) incident heart failure with reduced ejection fraction and incident heart failure with preserved ejection fraction. Associations of lung function with incident heart failure were analysed using Fine–Gray proportional sub-distribution hazards models. Models were adjusted for baseline age/birth year (centred), sex, race/ethnicity, educational attainment, clinical site, height, weight, smoking status, smoking pack-years, systolic/diastolic blood pressure, total cholesterol, hypertension status, and diabetes status. In models of incident heart failure (A), non-heart failure mortality was treated as the competing risk. Restrictive and obstructive physiology were both associated with incident heart failure. In models of incident heart failure sub-types (B), heart failure with reduced ejection fraction, heart failure with preserved ejection fraction, and non-heart failure mortality were treated as competing risks. Restrictive and obstructive physiology were not associated with incident heart failure with reduced ejection fraction. In contrast, both restrictive and obstructive physiology were significantly associated with incident heart failure.
Incident heart failure with reduced ejection fraction and heart failure preserved ejection fraction
Among 27 455 participants with classifiable HF events, there were 2066 incident HF cases over a median follow-up of 22.2 years (IQR, 11.0–28.2); 1030 events were classified as HFrEF (49.9%) and 1036 were classified as HFpEF (50.1%) (see Supplementary material online, Table S3 and Figure S4). The FEV1 and FVC were associated with incident HFrEF, but obstructive and restrictive physiology were not (Table 2, Supplementary material online, Figure S2). In contrast, associations with HFpEF were of larger magnitude for FEV1 and FVC (see Supplementary material online, Figure S2) and were significant for both obstructive [HR 1.30; 95% confidence interval (CI) 1.11–1.51; P < 0.001] and restrictive physiology (HR 1.56; 95% CI 1.27–1.91; P < 0.001; Figure 1B). Associations of impaired lung function with incident HFrEF and HFpEF persisted in multiple imputation analyses performed to account for missing covariate and HF sub-type data (see Supplementary material online, Table S4). Further, when stratified by cohort, similar associations were observed in MESA, which is a contemporary cohort that started enrolling participants in 2000 with over 14 years of HF follow-up (see Supplementary material online, Figures S6–S8). Despite these consistent qualitative observations, differences between the associations with HFrEF vs. HFpEF were not statistically confirmed using the conservative bootstrap approach (P = 0.48 for obstructive physiology and 0.34 for restrictive physiology).
The association between restrictive physiology and incident HFpEF (HR 1.64; 95% CI 1.34–2.00) was similar to or greater than associations for dichotomized HF risk factors including obesity (HR 1.66; 95% CI 1.44–1.91), hypertension (HR 1.77; 95% CI 1.52–2.06), diabetes (HR 1.41; 95% CI 1.20–1.67), and current smoking (HR 1.33; 95% CI 1.08–1.64), and the CIs for restrictive physiology overlapped with intervals for established HF risk factors (Table 3).
Table 3.
Associations of baseline lung function with incident heart failure, incident heart failure with reduced ejection fraction, and incident heart failure with preserved ejection fraction compared with dichotomized established risk factors
| Incident HFa,b | Incident HF sub-typesc | |||||
|---|---|---|---|---|---|---|
| Incident HFrEF | Incident HFpEF | |||||
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Obstructive physiologyd | 1.15 (1.05–1.25) | 0.002 | 1.06 (0.90–1.24) | 0.50 | 1.25 (1.08–1.46) | 0.004 |
| Restrictive physiologye | 1.49 (1.33–1.68) | <0.001 | 1.16 (0.92–1.46) | 0.21 | 1.64 (1.34–2.00) | <0.001 |
| Current smoking | 1.33 (1.18–1.50) | <0.001 | 1.39 (1.13–1.71) | 0.002 | 1.33 (1.08–1.64) | 0.007 |
| Diabetesf | 1.43 (1.31–1.57) | <0.001 | 1.38 (1.16–1.64) | <0.001 | 1.41 (1.20–1.67) | <0.001 |
| High total cholesterolg | 0.92 (0.86–0.99) | 0.03 | 0.86 (0.75–0.98) | 0.02 | 0.98 (0.86–1.11) | 0.73 |
| Hypertensionh | 1.44 (1.33–1.57) | <0.001 | 1.32 (1.13–1.54) | 0.004 | 1.77 (1.52–2.06) | <0.001 |
| Low HDLi | 1.09 (1.01–1.17) | 0.03 | 1.09 (0.96–1.25) | 0.19 | 1.01 (0.89–1.16) | 0.87 |
| Obesityj | 1.40 (1.29–1.51) | <0.001 | 1.18 (1.02–1.36) | 0.03 | 1.66 (1.44–1.91) | <0.001 |
CI, confidence interval; HDL, high-density lipoprotein; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HR, hazard ratio.
Separate sub-distribution hazards regression models were used to analyse risk of incident HF and incident HF sub-types; models additionally adjusted for age, sex, race, birth year, site, educational attainment, smoking pack-years, and statins. Hazard ratios for obstructive and restrictive physiology differ slightly from those observed in Table 2 because we did not adjust for comparative cardiovascular risk factors evaluated in Table 3 (i.e. height, weight, systolic/diastolic blood pressure, total cholesterol, hypertension status, and diabetes status).
In models of incident HF, non-HF mortality was treated as the competing risk.
In models of incident HF sub-types, which were limited to the cohorts collecting data on ejection fraction, HFrEF, HFpEF, and non-HF mortality were treated as competing risks.
Obstructive physiology: FEV1/FVC < 70.
Restrictive physiology: FEV1/FVC ≥ 70 and per cent–predicted FVC < 80.
Self-reported diabetes or fasting blood sugar levels ≥ 126 mg/dL or use of oral hypoglycaemic agents or insulin.
High total cholesterol: total cholesterol ≥ 200 mg/dL.
Self-reported hypertension or systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or use of anti-hypertensive medications.
Low HDL: Men = HDL <40 mg/dL; Women ≤ 50 mg/dL.
Obesity: BMI > 29.9 kg/m2.
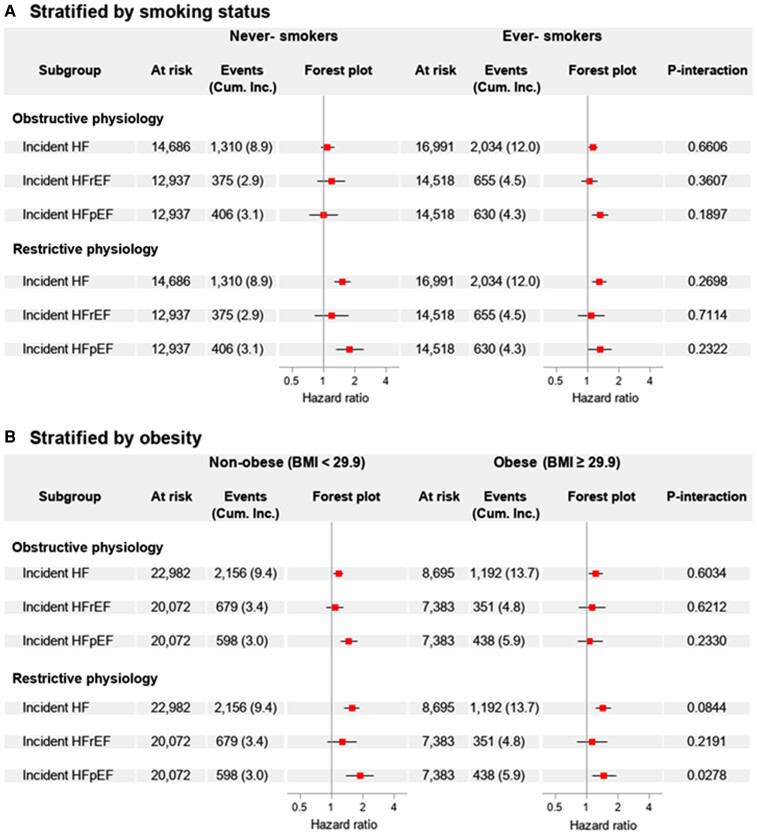
Sub-group analyses
Among the covariates included in the full model, adjustment for smoking status and weight was associated with the greatest change in effect estimates (see Supplementary material online, Figure S5). Fully stratified models by smoking status and obesity are shown in Figure 2. Among these two influential covariates, the only nominally significant interaction was for obesity with respect to the association between restrictive physiology and incident HFpEF (P-interaction, 0.03): larger associations were observed in non-obese participants, yet restrictive physiology remained strongly associated with incident HFpEF in obese participants (Figure 2B). There were no significant interactions for smoking status, although obstructive physiology was significantly associated with incident HF and HFpEF in ever-smokers but not in never-smokers (Figure 2A). In contrast, significant associations between restrictive physiology and incident HF and HFpEF were observed in both never- and ever-smokers. Among ever-smokers, the interaction term for pack-years was nominally significant for the association between restriction and incident HF (P-interaction, 0.05), with larger associations observed in participants with lesser pack-year histories (see Supplementary material online, Table S5). Nonetheless, significant associations between restrictive physiology and increased risk of HFpEF were observed across all levels of BMI and smoking status.
Figure 2.
Smoking- and obesity-stratified analyses of associations between lung function impairment and incident heart failure. To assess potential effect modification, Fine–Gray proportional sub-distribution hazards models were stratified by smoking status (A) and body mass index (B). Models were adjusted for baseline age, sex, race, educational attainment, birth year, site, height, weight, smoking status, pack-years, systolic and diastolic blood pressure, total cholesterol, hypertension status, diabetes status, and statin use. Among never-smokers, restrictive physiology was significantly associated with overall incident heart failure and incident heart failure with preserved ejection fraction, but not with incident heart failure with reduced ejection fraction. Similarly, analyses stratified by body mass index showed restrictive physiology remained strongly associated with incident heart failure preserved ejection fraction in non-obese participants. Hazard ratios are plotted on a log scale.
With respect to other covariates, effect estimates were similar when stratified by age, sex, and major comorbidities (see Supplementary material online, Table S5). Associations between impaired lung function and incident HF persisted in participants without baseline hypertension, diabetes, obesity, or smoking (see Supplementary material online, Table S5). While there was a significant interaction between restrictive physiology and race/ethnicity (P = 0.004), there were limited sample sizes in certain strata. Further, effect estimates were monotonic and similar in all levels of the covariates, which is not consistent with substantial effect measure modification.
Of importance, sub-group analyses were not adjusted for multiple comparisons and should be interpreted as exploratory.
Sensitivity analyses
Additional adjustment for renal function and fibrinogen did not alter results (see Supplementary material online, Tables S6 and S7). Results were similar when excluding incident HF events that were co-classified as CLRD-related events (see Supplementary material online, Table S8), HF events occurring within 2 years of spirometry measurement (see Supplementary material online, Table S9), and interim MI events (see Supplementary material online, Table S10). Results were also comparable in cohort-stratified analyses (see Supplementary material online, Figures S6–S8).
Discussion
Lung function impairment was associated with increased risk of incident HF in a large multi-ethnic sample of US adults. Associations varied by physiological patterns of pulmonary and cardiac impairment: restrictive physiology was more strongly associated with incident HF than obstructive physiology, and lung function impairment was more strongly associated with HFpEF compared with HFrEF. The magnitude of the association between restrictive physiology and HFpEF was similar to or greater than established HF risk factors (Structured Graphical Abstract). This suggests that the recognition and management of lung function impairment could be important for prevention and treatment of HF, and particularly HFpEF.
This is the largest study of which we are aware to define associations of lung function with incident HF. Our results are consistent with prior studies that showed associations of reduced FEV1 and FVC with incident HF risk among European men9,10 and older adults.11 The present study expands the generalizability of these findings by establishing associations of lung function impairment with HF risk in a large, multi-ethnic cohort of men and women which included middle-aged and older adults. Our results were broadly consistent in sub-group analyses according to sociodemographic, anthropometric, behavioural, and clinical factors, and persisted among participants without smoking history, obesity, or major comorbidities. Our results provide evidence that impaired lung function may provide clinicians with additional information regarding HF risk. Clinicians should consider evaluating patients with lung function impairment for comorbid HF, and may advise HF prevention strategies including regular physical activity, dietary interventions, tobacco cessation, and moderation of alcohol intake.38 Additional studies are needed to determine whether therapies that improve lung function impairment concomitantly minimize HF risk.
With regard to HF sub-types, we found that associations with lung function impairment were more consistent and of larger magnitude for HFpEF compared with HFrEF in Fine–Gray models that treated HF sub-types as competing risks. Specifically, baseline FEV1 and FVC were more strongly associated with incident HFpEF than incident HFrEF. This finding is consistent with a previous study in elderly adults in which reduced FEV1/FVC was associated with incident HFpEF but was not a significant HFrEF risk factor.8 However, our results contrast with a prior study in older adults that found similar associations of abnormal lung function with both incident HFrEF (HR 1.71) and HFpEF (HR 1.75) in Cox proportional hazards models.11 This discrepancy was not fully explained by different modelling approaches: when associations were estimated using Cox proportional hazards models in the present study, lung function impairment remained more strongly associated with HFpEF than HFrEF (results not shown). The stronger associations with HFpEF vs. HFrEF in our study may therefore be due to the larger sample size, younger mean age of participants, greater confounder adjustment, or potentially advances in the prevention of HFrEF.39
Smoking is anticipated to confound associations with incident HF, and particularly HFrEF, since it is a major known cause of accelerated lung function decline, obstructive physiology, and atherosclerotic cardiovascular disease.40 Our study confirms that adjustment for smoking status substantially attenuated associations between lung function impairment and HF, which is consistent with confounding. The ARIC study, which included a large proportion of current smokers, previously identified increased HF risk among participants with rapid declines in FEV1 and FVC.41 In contrast, the present study, which included a large proportion of never-smokers and used a substantially larger sample, did not find increased HF risk among participants with accelerated lung function decline. It is possible that incomplete control of confounding related to smoking could contribute to this discrepancy between our study and the prior report.
Our study did not find strong evidence for effect measure modification by smoking, although effect estimates varied in strata of smoking status. For example, obstructive physiology was associated with incident HFpEF among smokers but not among never-smokers. This finding is consistent with a study in men that found that obstructive physiology was associated with HF hospitalizations in smokers only.9 However, despite the uniquely large sample size in the present study, no statistically significant interaction by smoking status was shown. Yet another prior study in African-Americans found obstructive physiology was more strongly associated with incident HF than restriction.42 In contrast, in our study, restrictive physiology was strongly associated with HF and HFpEF regardless of smoking status, which is suggestive of independent mechanisms. Generally, our results in never-smokers, which are non-significantly different than results in smokers, are unlikely to be confounded by unregistered smoking exposures.
Impaired lung function may contribute directly to HF pathogenesis via several biological mechanisms. Lung function impairment generates systemic oxidative stress,43 which has been shown to induce myocardial hypertrophy and impair cardiac contractility.44 Reduced total lung capacity, which is a defining feature of restrictive physiology, has been shown to generate systemic inflammation.45 Systemic inflammation may in turn lead to endothelial inflammation in the coronary microvasculture.6 Coronary microvascular endothelial inflammation alters protein homeostasis in adjacent cardiomyocytes and generates cardiac remodelling and hypertrophy characteristic of HFpEF.46 Abnormal respiratory mechanics, which may occur with obesity,47 additionally impair left ventricular filling, reduce cardiac output, and generate haemodynamic changes.48 Indeed, BMI was found to confound and modify associations of restrictive physiology with incident HFpEF in our study, although associations were consistent across strata of BMI categories. Unfortunately, circulating markers of systemic inflammation were not available in all cohorts, so the aforementioned pathways connecting lung function impairment with incident HF are speculative. Nonetheless, our results suggest that lung function impairment, and potentially secondary systemic inflammation and oxidative stress, could represent promising targets for HFpEF prevention and treatment.
Strengths of the current work include the large, multi-ethnic population-based sample; consideration of a large number of potential confounding factors; extensive follow-up; and examination of quality-controlled physiologic and clinical endpoints. Nonetheless, the study has several limitations. First, HF is a clinical diagnosis, and HF ascertainment in cohort studies remains challenging. Defining HFpEF events is particularly challenging, as echocardiographic diastolic function parameters were not available to inform HFpEF ascertainment beyond EF ≥50%. Nevertheless, incident HF and HF sub-types were classified and adjudicated using standardized methods.49 Potential misclassification of respiratory exacerbations as incident HF events was considered, yet analyses that excluded events coded with a concomitant CLRD diagnosis yielded similar results. Second, 4222 (13.3%) participants did not have available EF measurements at the time of HF diagnosis. However, associations of impaired lung function with incident HF sub-types persisted in multiple imputation analyses that imputed missing EF data. Third, it is possible that a sub-set of the cohort had sub-clinical HF at baseline. Because HF can lower both FEV1 through peribronchial oedema and FVC through cardiac enlargement,50 impaired lung function may serve as a marker of preclinical HF. Unfortunately, biomarkers of decompensated HF including N-terminal pro B-type natriuretic peptide (NT-proBNP) were not available. However, occult baseline HF is unlikely to fully explain our results, as associations were robust both to censoring HF events occurring within 2 years of spirometry measurements and to adjusting for renal dysfunction, which can herald underlying cardiac impairment.51 Further, prior studies have demonstrated that associations of lung function impairment with incident HF persisted after adjusting for cardiac biomarkers including NT-proBNP.10 Fourth, observed associations between reduced lung function and incident HF events could be confounded by cardiovascular risk factors including genetic factors, which were not measured. However, associations between impaired lung function and incident HF persisted in participants without hypertension, diabetes, obesity, or current smoking at the baseline assessment. Fifth, data that could elucidate the aetiology of restrictive physiology (i.e. lung volumes, muscle pressures, and computed tomography imaging) were unavailable. Obesity can generate a restrictive pattern on spirometry,52 and residual confounding due to weight-related restriction may have impacted observed associations between restriction and incident HF. However, models stratified by obesity showed persistent associations in non-obese participants. Sixth, post-bronchodilator spirometry is required for defining obstructive lung physiology but was not available in these cohorts. However, prior studies have shown that pre- and post-bronchodilator measurements are highly correlated.53 Seventh, the findings are largely restricted to African-American, European-American, and American-Indian individuals, as incident HF events were relatively low among Asian-American and Hispanic/Latino participants. Eighth, it is possible that in cohorts with advanced age at enrolment, participants with impaired lung function and subsequent HF were less likely to be enrolled, which may have contributed to an under-estimation of associations between lung function impairment and incident HF.54 However, the observed associations persisted in cohorts that enrolled young adults. Finally, impaired lung function is associated with increased mortality, and comorbid HF further increases mortality in patients with respiratory diseases.55 It is possible that a selective survival bias contributed to under-estimation of associations between reduced lung function and incident HF. To mitigate this issue, we treated all-cause mortality as a competing risk in all analyses. However, the nominal interaction by pack-years identified in our study, in which persons with greater pack-years demonstrated smaller associations between restrictive physiology and incident HFpEF, may be due to incomplete accounting for competing risks despite the use of a competing risks modelling approach.
In conclusion, lung function impairment was associated with increased risk of incident HF in a large, US general population-based cohort. Reduced lung function, particularly restrictive physiology, was associated with incident HFpEF independent of and to similar extent as major known cardiovascular risk factors. Recognition of lung function impairment could be important for prevention, early diagnosis, and prognostication of HF and especially HFpEF, for which effective therapies remain limited.
Supplementary material
Supplementary material is available at European Heart Journal online.
Supplementary Material
Contributor Information
Christina M Eckhardt, Department of Medicine, Columbia University College of Physicians and Surgeons, 630 West 168th Street, Presbyterian Hospital 9th Floor, Suite 105, New York, NY 10032, USA.
Pallavi P Balte, Department of Medicine, Columbia University College of Physicians and Surgeons, 630 West 168th Street, Presbyterian Hospital 9th Floor, Suite 105, New York, NY 10032, USA.
Robert Graham Barr, Department of Medicine, Columbia University College of Physicians and Surgeons, 630 West 168th Street, Presbyterian Hospital 9th Floor, Suite 105, New York, NY 10032, USA.
Alain G Bertoni, Division of Public Health Sciences, Wake Forest University School of Medicine, Winston-Salem, NC, USA.
Surya P Bhatt, Division of Pulmonary, University of Alabama at Birmingham, Allergy and Critical Care Medicine, Birmingham, AL, USA.
Michael Cuttica, Department of Medicine, Northwestern University, Chicago, IL, USA.
Patricia A Cassano, Division of Nutritional Sciences, Cornell University, College of Human Ecology, Cornell, NY, USA.
Paolo Chaves, Department of Health and Society, Florida International University, Miami, FL, USA.
David Couper, Department of Biostatistics, University of North Carolina, Chapel Hill, NC, USA.
David R Jacobs, Division of Epidemiology and Community Health, University of Minnesota, School of Public Health, Minneapolis, MN, USA.
Ravi Kalhan, Department of Medicine, Northwestern University, Chicago, IL, USA.
Richard Kronmal, Department of Statistics, University of Washington, School of Public Health, Seattle, WA, USA.
Leslie Lange, Department of Medicine, University of Colorado, Denver, CO, USA.
Laura Loehr, Department of Medicine, University of North Carolina, Chapel Hill, NC, USA.
Stephanie J London, National Institute of Environmental Health Sciences, National Institutes of Health, Department of Health and Human Services, Research Triangle Park, NC, USA.
George T O’Connor, Department of Medicine, Boston University, Boston, MA, USA.
Wayne Rosamond, Department of Medicine, University of North Carolina, Chapel Hill, NC, USA.
Jason Sanders, Division of Pulmonary Medicine, Brigham and Women’s Hospital, Boston, MA, USA.
Joseph E Schwartz, National Institute of Environmental Health Sciences, National Institutes of Health, Department of Health and Human Services, Research Triangle Park, NC, USA.
Amil Shah, Division of Cardiovascular Medicine, Brigham and Women’s Hospital, Boston, MA, USA.
Sanjiv J Shah, Department of Medicine, Northwestern University, Chicago, IL, USA.
Lewis Smith, Department of Medicine, Northwestern University, Chicago, IL, USA.
Wendy White, Undergraduate Training and Education Center, Tougaloo College, Jackson Heart Study, Jackson, MS, USA.
Sachin Yende, Department of Critical Care Medicine, Veterans Affairs Pittsburgh Healthcare System and University of Pittsburgh, Pittsburgh, PA, USA.
Elizabeth C Oelsner, Department of Medicine, Columbia University College of Physicians and Surgeons, 630 West 168th Street, Presbyterian Hospital 9th Floor, Suite 105, New York, NY 10032, USA.
Funding
This work was supported by The National Heart, Lung, and Blood Institute Pooled Cohorts Study that has been funded with federal funds from the National Heart, Lung, and Blood Institute and National Institutes of Health (R21-HL121457, R21-HL-129924, and K23-HL-130627). Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, and Department of Health and Human Services (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, and HHSN268201700004I). The authors thank the staff and participants of the ARIC study for their important contributions. Funding for laboratory testing and biospecimen collection at ARIC Visit 6 was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (R01DK089174). The authors thank the staff and participants of the ARIC study for their important contributions. The CARDIA (Coronary Artery Risk Development in Young Adults) Study: CARDIA is supported by contracts HHSN268201800003I, HHSN268201800004I, HHSN268201800005I, HHSN268201800006I, and HHSN268201800007I from the National Heart, Lung, and Blood Institute. CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging and an intra-agency agreement between National Institute on Aging and the National Heart, Lung, and Blood Institute (AG0005), as well as a National Heart, Lung, and Blood Institute grant (R01 HL122477 to R.K.). This manuscript has been reviewed by CARDIA for scientific content. Cardiovascular Health Study3 has been funded in whole or in part by contracts (HHSN268201200036C, HHSN268200800007C, HHSN268201800001C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, and N01HC85086) and grants (U01HL080295 and U01HL130114) from the National Heart, Lung, and Blood Institute, as well as grants (R01-HL093081 and R01-HL077612) with additional contribution from the National Institute of Neurological Disorders and Stroke. Additional support was provided by the National Institute on Aging (R01AG023629). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org. The FHS (Framingham Heart Study): From the Framingham Heart Study of the National Heart, Lung, and Blood Institute of the National Institutes of Health and Boston University School of Medicine. This work was supported by the National Heart, Lung, and Blood Institute’s Framingham Heart Study (N01-HC-25195 and HHSN268201500001I). Health ABC (Health Aging and Body Composition) Study: This research was supported by National Institute on Aging contracts (N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106) and grants (R01-AG028050), and by National Institute of Nursing Research (R01-NR012459). The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I), and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I, and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities. The authors also thank the staffs and participants of the JHS. The MESA (Multi-Ethnic Study of Atherosclerosis): MESA has been funded in whole or in part by The National Heart, Lung, and Blood Institute and the National Institutes of Health (R01-HL-077612, R01-HL-093081, RC1-HL-100543, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169). The Strong Heart Study has been funded in whole or in part with federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services (75N92019D00027, 75N92019D00028, 75N92019D00029, and 75N92019D00030). The study was previously supported by research grants (R01HL109315, R01HL109301, R01HL109284, R01HL109282, and R01HL109319) and by cooperative agreements (U01HL41642, U01HL41652, U01HL41654, U01HL65520, and U01HL65521). This work was supported by a clinical and translational science awards grant (TL1TR001875 to C.M.E.]. This work was supported by additional federal funds from the US National Heart, Lung, and Blood Institute (U54 HL160273 R01 HL107577, R01 HL140731, and R01 HL149423 to S.J.S.). At the time of publication, J.S. was employed by Vertex Pharmaceuticals. S.J.L. is supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services.
Conflict of interest The authors declare there are no conflicts of interest, beyond grant funding by the National Institutes of Health, with the following exceptions. A.S. receives funding from Novartis and Philips Ultrasound, for which he serves on an Advisory Board. L.S. participates on data safety monitoring boards from clinical trials by TORAY/Covance and Clinipace/Puretech. P.A.C. is a Field Advisory Board Member for Cochrane Nutrition. R.K. receives consulting fees and/or honoraria from CVS Health, AstraZeneca, GlaxoSmithKline, and Omron. S.P.B. receives royalties or licenses from Springer Humana; consulting fees from Boehringer Ingelheim, Sanovi/Regeneron, and Sunovion; payment or honoraria from GlaxoSmithKline; and holds stock or stock options from Vigor Medical Systems. At the time of manuscript resubmission, J.S. was employed by Vertex Pharmaceuticals; however, his participation in this project pre-dated and is independent of his employment at Vertex. S.J.S. has received research grants from Actelion, AstraZeneca, Corvia, Novartis, and Pfizer, and consulting fees from Abbott, Actelion, AstraZeneca, Amgen, Aria CV, Axon Therapies, Bayer, Boehringer-Ingelheim, Boston Scientific, Bristol-Myers Squibb, Cardiora, Coridea, CVRx, Cyclerion, Cytokinetics, Edwards Lifesciences, Eidos, Eisai, Imara, Impulse Dynamics, Intellia, Ionis, Ironwood, Lilly, Merck, MyoKardia, Novartis, Novo Nordisk, Pfizer, Prothena, Regeneron, Rivus, Sanofi, Shifamed, Tenax, Tenaya, and United Therapeutics.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol 2011;8:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KKL, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med 2002;347:1397–1402. [DOI] [PubMed] [Google Scholar]
- 3. Rutten FH, Cramer MJM, Grobbee DE, Sachs APE, Kirkels JH, Lammers JWJ, et al. Unrecognized heart failure in elderly patients with stable chronic obstructive pulmonary disease. Eur Heart J 2005;26:1887–1894. [DOI] [PubMed] [Google Scholar]
- 4. Guder G, Rutten FH. Comorbidity of heart failure and chronic obstructive pulmonary disease: more than coincidence. Curr Heart Fail Rep 2014;11:337–346. [DOI] [PubMed] [Google Scholar]
- 5. Gan WQ, Man SFP, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004;59:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paulus WJ, Tschope C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 2013;62:263–271. [DOI] [PubMed] [Google Scholar]
- 7. Corbi G, Bianco A, Turchiarelli V, Cellurale M, Fatica F, Daniele A, et al. Potential mechanisms linking atherosclerosis and increased cardiovascular risk in COPD: focus on Sirtuins. Int J Mol Sci 2013;14:12696–12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lam CSP, Lyass A, Kraigher-Krainer E, Massaro JM, Lee DS, Ho JE, et al. Cardiac dysfunction and noncardiac dysfunction as precursors of heart failure with reduced and preserved ejection fraction in the community. Circulation 2011;124:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Engstrom G, Melander O, Hedblad B. Population-based study of lung function and incidence of heart failure hospitalisations. Thorax 2010;65:633–638. [DOI] [PubMed] [Google Scholar]
- 10. Wannamethee SG, Shaper AG, Papacosta O, Lennon L, Welsh P, Whincup PH. Lung function and airway obstruction: associations with circulating markers of cardiac function and incident heart failure in older men—the British Regional Heart Study. Thorax 2016;71:526–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Georgiopoulou VV, Kalogeropoulos AP, Psaty BM, Rodondi N, Bauer DC, Butler AB, et al. Lung function and risk for heart failure among older adults: the Health ABC Study. Am J Med 2011;124:334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 13. Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN, SOLVD Investigator . Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293–302. [DOI] [PubMed] [Google Scholar]
- 14. Kitzman DW, Hundley WG, Brubaker PH, Morgan TM, Moore JB, Stewart KP, et al. A randomized double-blind trial of enalapril in older patients with heart failure and preserved ejection fraction: effects on exercise tolerance and arterial distensibility. Circ Heart Fail 2010;3:477–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oelsner EC, Balte PP, Cassano PA, Couper D, Enright PL, Folsom AR, et al. Harmonization of respiratory data from 9 US population-based cohorts: the NHLBI pooled cohorts study. Am J Epidemiol 2018;187:2265–2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosamond WD, Folsom AR, Chambless LE, Wang CH, ARIC Investigators, Atherosclerosis Risk in Communities . Coronary heart disease trends in four United States communities. The Atherosclerosis Risk in Communities (ARIC) study 1987-1996. Int J Epidemiol 2001;30:S17–S22. [DOI] [PubMed] [Google Scholar]
- 17. Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs D, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–1116. [DOI] [PubMed] [Google Scholar]
- 18. Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 19. Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design and preliminary data. Prev Med 1975;4:518–525. [DOI] [PubMed] [Google Scholar]
- 20. Goodpaster BH, Carlson CL, Visser M, Kelley DE, Scherzinger A, Harris TB, et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol 2001;90:2157–2165. [DOI] [PubMed] [Google Scholar]
- 21. Sempos CT, Bild DE, Manolio TA. Overview of the Jackson Heart Study: a study of cardiovascular diseases in African American men and women. Am J Med Sci 1999;317:142–146. [DOI] [PubMed] [Google Scholar]
- 22. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–881. [DOI] [PubMed] [Google Scholar]
- 23. Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, et al. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol 1990;132:1141–1155. [DOI] [PubMed] [Google Scholar]
- 24. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–338. [DOI] [PubMed] [Google Scholar]
- 25. Wever AM, Britton MG, Hughes DT, Van der Plas KH, Wever-Hess J. Clinical evaluation of five spirometers. Monaghan M403, Pneumoscreen, Spirotron, Vicatest and Vitalograph. Eur J Respir Dis 1981;62:127–137. [PubMed] [Google Scholar]
- 26. Bhatt SP, Balte PP, Schwartz JE, Cassano PA, Couper D, Jacobs DR, et al. Discriminative accuracy of FEV1:FVC thresholds for COPD-related hospitalization and mortality. JAMA 2019;321:2438–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas ET, Guppy M, Straus SE, Bell KJL, Glasziou P. Rate of normal lung function decline in ageing adults: a systematic review of prospective cohort studies. BMJ Open 2019;9:e028150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Butler J, Kalogeropoulos AP, Georgiopoulou VV, Bibbins-Domingo K, Najjar SS, Sutton-Tyrrell KC, et al. Systolic blood pressure and incident heart failure in the elderly. The Cardiovascular Health Study and the Health, Ageing and Body Composition Study. Heart 2011;97:1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gilkes A, Ashworth M, Schofield P, Harries TH, Durbaba S, Weston C, et al. Does COPD risk vary by ethnicity? A retrospective cross-sectional study. Int J Chron Obstruct Pulmon Dis 2016;11:739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Keku E, Rosamond W, Taylor HA Jr, Garrison R, Wyatt SB, Richard M, et al. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis 2005;15:S62–S70. [PubMed] [Google Scholar]
- 31. Reis JP, Allen N, Gunderson EP, Lee JM, Lewis CE, Loria CM, et al. Excess body mass index- and waist circumference-years and incident cardiovascular disease: the CARDIA study. Obesity (Silver Spring) 2015;23:879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, et al. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail 2012;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zacharias M, Joffe S, Konadu E, Meyer T, Kiernan M, Lessard D, et al. Clinical epidemiology of heart failure with preserved ejection fraction (HFpEF) in comparatively young hospitalized patients. Int J Cardiol 2016;202:918–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 36. Haffner SM, American Diabetes Association . Dyslipidemia management in adults with diabetes. Diabetes Care 2004;27:S68–S71. [DOI] [PubMed] [Google Scholar]
- 37. Oelsner EC, Loehr LR, Henderson AG, Donohue KM, Enright PL, Kalhan R, et al. Classifying chronic lower respiratory disease events in epidemiologic cohort studies. Ann Am Thorac Soc 2016;13:1057–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Horwich TB, Fonarow GC. Prevention of heart failure. JAMA Cardiol 2017;2:116. [DOI] [PubMed] [Google Scholar]
- 39. Raj L, Adhyaru B. An evidence-based review of recent advances in therapy for heart failure with reduced ejection fraction (HFrEF). Postgrad Med J 2016;92:726–734. [DOI] [PubMed] [Google Scholar]
- 40. Ockene IS, Miller NH. Cigarette smoking, cardiovascular disease, and stroke: a statement for healthcare professionals from the American Heart Association. American Heart Association Task Force on Risk Reduction. Circulation 1997;96:3243–3247. [DOI] [PubMed] [Google Scholar]
- 41. Silvestre OM, Nadruz W, Querejeta Roca G, Claggett B, Solomon SD, Mirabelli MC, et al. Declining lung function and cardiovascular risk: the ARIC study. J Am Coll Cardiol 2018;72:1109–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jankowich M, Elston B, Liu Q, Abbasi S, Wu WC, Blackshear C, et al. Restrictive spirometry pattern, cardiac structure and function, and incident heart failure in African Americans. The Jackson Heart Study. Ann Am Thorac Soc 2018;15:1186–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rahman I, Morrison D, Donaldson K, MacNee W. Systemic oxidative stress in asthma, COPD, and smokers. Am J Respir Crit Care Med 1996;154:1055–1060. [DOI] [PubMed] [Google Scholar]
- 44. Dhalla AK, Hill MF, Singal PK. Role of oxidative stress in transition of hypertrophy to heart failure. J Am Coll Cardiol 1996;28:506–514. [DOI] [PubMed] [Google Scholar]
- 45. Hancox RJ, Gray AR, Sears MR, Poulton R. Systemic inflammation and lung function: a longitudinal analysis. Respir Med 2016;111:54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Oeing CU, Mishra S, Dunkerly-Eyring BL, Ranek MJ. Targeting protein kinase G to treat cardiac proteotoxicity. Front Physiol 2020;11:858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cornelius T, Schwartz JE, Balte P, Bhatt SP, Cassano PA, Currow D, et al. A Dyadic growth modeling approach for examining associations between weight gain and lung function decline. Am J Epidemiol 2020;189:1173–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Barr RG, Bluemke DA, Ahmed FS, Carr JJ, Enright PL, Hoffman EA, et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med 2010;362:217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pfeffer MA, Shah AM, Borlaug BA. Heart failure with preserved ejection fraction in perspective. Circ Res 2019;124:1598–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Olson TP, Beck KC, Johnson BD. Pulmonary function changes associated with cardiomegaly in chronic heart failure. J Card Fail 2007;13:100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Uduman J. Epidemiology of cardiorenal syndrome. Adv Chronic Kidney Dis 2018;25:391–399. [DOI] [PubMed] [Google Scholar]
- 52. Zammit C, Liddicoat H, Moonsie I, Makker H. Obesity and respiratory diseases. Int J Gen Med 2010;3:335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kato B, Gulsvik A, Vollmer W, Janson C, Studnika M, Buist S, et al. Can spirometric norms be set using pre- or post- bronchodilator test results in older people? Respir Res 2012;13:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Schisterman EF, Cole SR, Ye A, Platt RW. Accuracy loss due to selection bias in cohort studies with left truncation. Paediatr Perinat Epidemiol 2013;27:491–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kaszuba E, Odeberg H, Rastam L, Halling A. Impact of heart failure and other comorbidities on mortality in patients with chronic obstructive pulmonary disease: a register-based, prospective cohort study. BMC Fam Pract 2018;19:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.