Abstract
Objective:
Visinin-like protein 1 (VILIP-1) is a neuron-specific calcium sensor protein rapidly released into blood following mild traumatic brain injury (mTBI) and may be a suitable biomarker for identification of sports-related concussion (SRC). The objective of the study is to test if quantification of a specific post-translationally modified (ubiquitinated) form of VILIP-1 (ubVILIP-1) from a fingerstick blood sample using a point of care (POC) lateral flow device (LFD) can be used to rapidly identify athletes with SRC.
Design:
Prospective cohort study.
Setting:
Side-line blood collection at football, soccer and volleyball games/practices.
Participants:
Division I athletes with/without SRC
Main Outcome Measures:
Blood ubVILIP-1 concentrations
Results:
Data collected over two athletic seasons from non-SRC athletes (controls) show a small but statistically significant elevation of ubVILIP-1 over an individual season for male athletes (p = 0.02) dependent on sport (p = 0.014) and no significant changes in ubVILIP-1 levels between seasons. For SRC athletes, the data show ubVILIP-1 levels substantially increase above baseline as soon as 30 mins post-diagnosis with peak concentrations and times post-injury that vary based on injury severity.
Conclusion:
Results of the study suggest quantification of blood ubVILIP-1 levels measured using an LFD may provide an objective identification of athletes with SRC, setting the stage for further study with a larger number of SRC patients.
Keywords: biomarkers, ubiquitinated VILIP-1, lateral flow device, sport-related concussion, traumatic brain injury
Introduction:
According to the Centers for Disease Control (CDC), mild traumatic brain injury (mTBI) resulting from sports-related concussion (SRC) results in ~1.6–3.8 million injuries reported per year in the United States1–3 which may be an underestimate since many concussed athletes fail to seek medical care4. Currently, the most common sideline tool for SRC evaluation is the standardized Sports Concussion Assessment Tool - 5th edition (SCAT5)5. Because of the subjective nature of SRC diagnosis utilizing the SCAT5, an objective diagnostic tool to assist in SRC diagnosis is warranted.
To date, the most widely studied TBI biomarkers include the astrocytic biomarkers S100β3,6, glial fibrillary acidic protein (GFAP)7,8, and the neuronal biomarkers total tau (T-tau) [Reviewed3], and neuron-specific enolase (NSE)9 [Reviewed3]. Data to date suggest these markers may lack sufficient sensitivity and specificity for use in mTBI associated with SRC3. More importantly, the most widely studied biomarkers of mTBI use analytical platforms (ELISAs) that are not amenable for use on-field. Although Abbott Laboratories recently introduced the i-STAT GFAP test that uses a standard sandwich ELISA approach with electrochemical detection that is promoted as a point of care (POC) analytical platform delivering results from plasma in less than 15 min10 the required use of blood plasma and use of specific instrumentation limits its use for on-field evaluations. Because of the need for on-field biomarker tests for SRC we developed a POC lateral flow device (LFD) to rapidly detect a ubiquitinated form of VILIP-1 (ubVILIP-1)11 from a drop of blood from a fingerstick. Our previous animal model study showed ubVILIP-1 levels are increased 30 min post injury in a rat model of mild TBI and that levels return to baseline by 72 h post injury11. Based on our animal model data this current study was carried out to determine the potential for use of our LFD for quantification of ubVILIP-1 for on-field identification of SRC.
Method:
A prospective cohort study was conducted to determine if there are changes in blood levels of ubVILIP-1 following non-contact conditioning (running, weight lifting), during the course of the athletic season or following SRC using the LFD developed by our laboratory and previously described11. To determine if ubVILIP-1 changes due to non-contact exercise as has been shown for other biomarkers, ubVILIP-1 levels were measured on-field in blood samples from fingersticks of NCAA athletes from two Division 1 schools (82 men and 35 women) at preseason baseline and within 1 hour of completion of conditioning sessions 1 and 2 weeks after the baseline measure under University of Kentucky IRB approved protocols during the 2018–2019 season. Table 1 shows that although mean ± SEM ubVILIP-1 concentrations (pg/ml) in women decreased following conditioning compared to their baselines the differences were not statistically significant. There was no significant change in concentrations for men following conditioning.
Table 1.
Adjusted Mean (± SEM) ubVILIP-1 Concentration (pg/mL) following conditioning.
| Men (n = 82) | Women (n = 35) | |
|---|---|---|
|
| ||
| Baseline | 56.5 ± 5.9 | 71.2 ± 12.9 |
| Post Conditioning 1 | 53.6 ± 4.0 | 54.2 ± 4.0 |
| Post Conditioning 2 | 52.3 ± 3.9 | 45.2 ± 3.7 |
To determine if ubVILIP-1 concentrations change over the course of the season we measured ubVILIP-1 concentrations on-field from fingerstick blood samples at baseline (before beginning practice) and within 1 hour of completion of practice at the beginning of the season (Post-Practice 1), middle of the season (Post-Practice 2) and end of the season (Post-Practice 3) compared to the preseason baseline values. In addition to the 82 men and 35 women recruited during the 2018–2019 season we also recruited and evaluated an additional 66 men and 43 women during the 2019 – 2020 season for a total cohort of 229 athletes (148M (64.6%), 81W (35.4%)) aged 18–23 (mean ± SD = 20.8 ± 0.9y).
To assess changes in levels of the biomarker following SRC, blood levels of the biomarker were measured at up to 5 time points (0.5 h, 2–4 h, 24 h, 48h, and 72 h) after an athlete was clinically diagnosed as an SRC case.
Unadjusted ubVILIP1 concentration distributions were visualized with boxplots, and adjusted mean ubVILIP1 concentrations at baseline and each of the post practice time points were obtained from Generalized Estimating Equations (GEE) with a log-linear regression model. The model included main effects for study year (2018 or 2019); sport (football, soccer, volleyball); sex (male, female); study visit (Baseline, Post-Practice 1, Post-Practice 2, and Post-Practice 3); and three-way interactions among sport, sex, and study visit as well as all lower order interaction terms. For simplicity, the model assumed within-athlete correlation is constant over time. Estimated standard errors were robust sandwich estimates. The data analysis was performed in SAS 9.4® (SAS, Inc.; Cary, NC, USA), and comparisons used an α level of 0.05.
Results:
Table 2 shows the adjusted mean ± standard error of the mean (SEM) ubVILIP-1 concentrations (pg/mL) by sport, athlete sex, and athletic season. The regression results suggest that the effect of sport depended on participant sex (P = 0.020). Female soccer players had higher ubVILIP1 levels at baseline compared to male soccer players (p=0.016), and their mean ubVILIP1 levels increased to a peak at Post-Practice 2 (p=0.0013 vs. Baseline) and were then lower than Baseline at Post-Practice 3 (p=0.0079). For female volleyball players, a similar pattern was observed: the athletes had mean Baseline measures that were higher than male soccer players (p=0.0029) or football players (p=0.09). The volleyball players also had lower mean concentrations at Post-Practice 3 compared to Baseline, although this difference was not statistically different (p=0.20). These patterns were consistent from 2018 to 2019. The data for football players show a small but statistically significant increase in levels of the biomarker over the course of the season although the progression is not linear. For men’s soccer there is a trend toward increased ubVILIP-1 over the season with significantly higher levels at post-practice 3 compared to baseline.
Table 2.
Adjusted Mean (± SEM) ubVILIP-1 Concentration (pg/mL) by Sport, Sex, and Season
| Men |
Women |
||||
|---|---|---|---|---|---|
| 2018 | 2019 | 2018 | 2019 | ||
|
|
|
||||
| Football | Soccer | ||||
| Baseline | 57.0 ± 6.7 | 53.0 ± 8.1 | Baseline | 64.7 ± 7.2# | 60.2 ± 7.7# |
| Post-practice 1 | 71.8 ± 8.7 | 66.8 ± 10.7 | Post-practice 1 | 52.0 ± 9.5 | 48.4 ± 8.6 |
| Post-practice 2 | 68.5 ± 7.2 | 63.8 ± 8.4 | Post-practice 2 | 104.4±11.8* | 97.1 ± 12.8* |
| Post-practice 3 | 86.9 ±11.2* | 80.9 ± 13.6* | Post-practice 3 | 39.8 ± 5.5* | 37.0 ± 5.5* |
| Soccer | Volleyball | ||||
|
| |||||
| Baseline | 36.7 ± 7.9 | 34.2 ± 7.5 | Baseline | 77.6 ± 10.7# | 72.2 ± 11.4# |
| Post-practice 1 | 52.4 ± 7.2 | 48.7 ± 7.2 | Post-practice 1 | 56.8 ± 9.1 | 52.8 ± 8.2 |
| Post-practice 2 | 69.1 ± 7.6 | 64.3 ± 8.0 | Post-practice 2 | 66.1 ± 10.6 | 61.4 ± 9.7 |
| Post-practice 3 | 56.0 ± 8.6* | 52.1 ± 8.1* | Post-practice 3 | 57.6 ± 10.1 | 53.6 ± 8.9 |
p < 0.01 compared to baseline
p < 0.01 compared to baseline for men’s soccer.
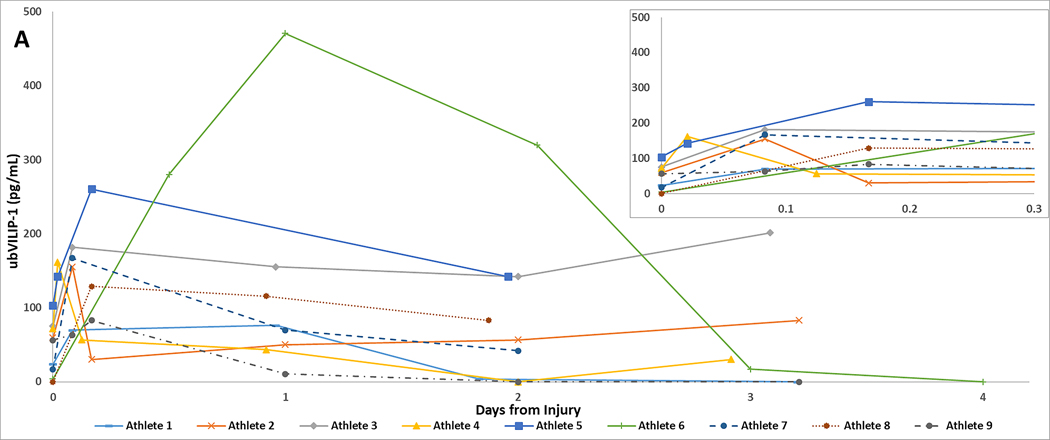
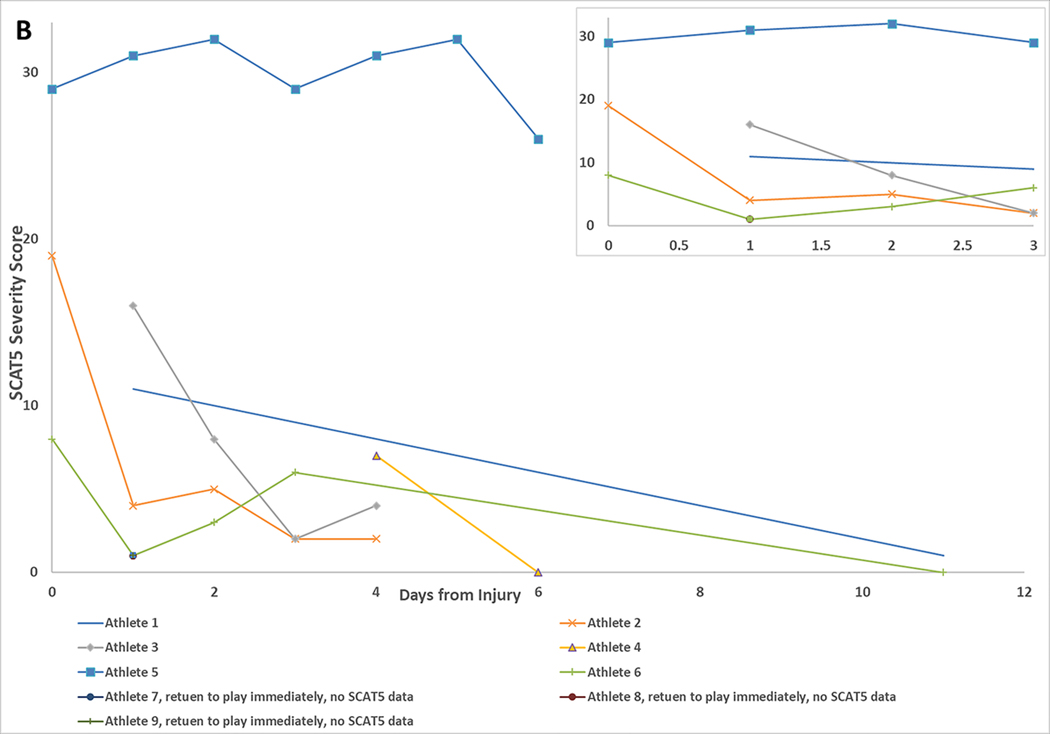
During the study, 9 consented athletes were clinically evaluated for SRC (7 M (77.8%), 2 W (22.2%)). Figure 1 (A) shows pronounced increases in blood ubVILIP-1 (pg/mL) levels above individual pre-season baseline values for the 9 athletes evaluated for SRC (insert expands early time points post diagnosis). For comparison, Figure 1 (B) shows changes in the SCAT5 severity score for 6 of the 9 athletes for whom data were available. SCAT5 metrics were not collected for 3 of the injured athletes after preliminary evaluation did not support SRC.
Figure 1A.
Blood ubVILIP-1 levels following SRC in 9 athletes are substantially elevated compared to individual baselines soon after clinical diagnosis of SRC.
Figure 1B.
(B) SCAT5 symptom severity scores following SRC in 6 athletes for whom SCAT5 metrics were collected.
Discussion:
Our data show several key observations. First, blood ubVILIP-1 levels are not significantly different following non-contact practice in contrast to other markers that have been shown to increase following exercise6–8. The data also show that ubVILIP-1 levels have a small but statistically significant increase over the season for male athletes (P = 0.02) (likely driven by football players) whereas females did not have a significant change over the season. Comparison of ubVILIP-1 levels by season showed there were no significant differences between data collected between the 2018–2019 and 2019–2020 seasons (P = 0.47) (Table 2). Over the 2018–2020 seasons, 9 validated SRC cases were reported (5 cases in 2018–2019 season, 4 cases in 2019–2020 season). Figure 1A shows blood ubVILIP-1 levels in 9 athletes evaluated for SRC up to ~72 hrs. post-diagnosis and demonstrates that biomarker levels are elevated above pre-season baselines as soon as 30 minutes post-diagnosis and levels peaked at different times. Overall, these preliminary data demonstrate the potential for POC LFD detection of ubVILIP-1 following SRC and that might be used for objective on-field identification of athletes with SRC without the need for laboratory instrumentation. The study is limited by a small number of SRCs in the study population and a lack of SCAT5 in subjects that were not subsequently diagnosed with concussion. Current data collection is underway to increase the number of SRCs evaluated.
Acknowledgments:
The authors would like to thank the institutions’ athletic trainers, sports medicine staff, and all the athletes who participated in this study.
Funding:
This study was supported by the National Institutes of Health grant NINDS-R01NS104289.
Footnotes
Declaration of interest: Dr. Mark Lovell holds an equity interest in Fawkes Diagnostics LLC., which has licensed the use of the LFD for detection of ubVILIP-1 (US Patent 9,482,675, Issued 11/1/16). There are no other conflicts of interest.
References:
- 1.Kawata K, Liu CY, Merkel SF, Ramirez SH, Tierney RT, Langford D. Blood biomarkers for brain injury: What are we measuring? Neurosci Biobehav Rev. 2016;68:460–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zuckerman SL, Kerr ZY, Yengo-Kahn A, Wasserman E, Covassin T, Solomon GS. Epidemiology of Sports-Related Concussion in NCAA Athletes From 2009–2010 to 2013–2014: Incidence, Recurrence, and Mechanisms. Am J Sports Med. 2015;43(11):2654–2662. [DOI] [PubMed] [Google Scholar]
- 3.Papa L, Ramia MM, Edwards D, Johnson BD, Slobounov SM. Systematic review of clinical studies examining biomarkers of brain injury in athletes after sports-related concussion. J Neurotrauma. 2015;32(10):661–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30(1):1-17, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Echemendia RJ, Meeuwisse W, McCrory P, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. Br J Sports Med. 2017;51(11):848–850. [DOI] [PubMed] [Google Scholar]
- 6.Lee JY, Lee CY, Kim HR, Lee CH, Kim HW, Kim JH. A Role of Serum-Based Neuronal and Glial Markers as Potential Predictors for Distinguishing Severity and Related Outcomes in Traumatic Brain Injury. J Korean Neurosurg Soc. 2015;58(2):93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neselius S, Brisby H, Marcusson J, Zetterberg H, Blennow K, Karlsson T. Neurological assessment and its relationship to CSF biomarkers in amateur boxers. PLoS One. 2014;9(6):e99870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papa L, Lewis LM, Falk JL, et al. Elevated levels of serum glial fibrillary acidic protein breakdown products in mild and moderate traumatic brain injury are associated with intracranial lesions and neurosurgical intervention. Ann Emerg Med. 2012;59(6):471–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma R, Laskowitz DT. Biomarkers in traumatic brain injury. Current neurology and neuroscience reports. 2012;12(5):560–569. [DOI] [PubMed] [Google Scholar]
- 10.Biberthaler P, Musaelyan K, Krieg S, et al. Evaluation of Acute Glial Fibrillary Acidic Protein and Ubiquitin C-Terminal Hydrolase-L1 Plasma Levels in Traumatic Brain Injury Patients with and without Intracranial Lesions. Neurotrauma Rep. 2021;2(1):617–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradley-Whitman MA, Roberts KN, Abner EL, Scheff SW, Lynn BC, Lovell MA. A novel method for the rapid detection of post-translationally modified visinin-like protein 1 in rat models of brain injury. Brain Inj. 2018;32(3):363–380. [DOI] [PubMed] [Google Scholar]