Abstract
Cord entanglement and conjoined twins are unique complications of monoamniotic monochorionic pregnancy. This case report describes a case of monoamniotic twins' intrauterine demise due to lethal cord entanglement. A 26-year-old unbooked primigravida was reported in the emergency labor room at 32 weeks with the complaint of loss of fetal movements since the previous day. On obstetric examination, the uterus appeared enlarged and discordant with the gestational age, multiple fetal parts were felt on palpation, and the pelvic grip was empty. Doppler could not detect any fetal heartbeat. The emergency obstetric sonography scan showed twins, the first in breech and the second in vertex presentation. Fetal heart sound was not found for either of the twins. The patient was counseled, and the decision was taken to terminate the pregnancy by lower-segment cesarean section. During the cesarean to deliver the babies, monochorionic and monoamniotic pregnancy was confirmed.
Keywords: antenatal care, twin pregnancy, umbilical cord entanglement, monochorionic monoamniotic twins, monoamniotic twins
Introduction
Monochorionic monoamniotic gestation is known as the least common type of twin pregnancy. In a monoamniotic twin pregnancy, the twins share a single placenta, amnion, and chorion. The zygote division after fertilization decides the chorionicity and amniotic status of the pregnancy. Division on days 8-12 leads to monochorionic monoamniotic placentation. Factors affecting the time of division are not yet apparent. In vitro fertilization seems to play a role as it increases the frequency of monozygotic twinning [1-3]. Monoamniotic twin gestations are found in approximately 5% of monochorionic and 1% of twin pregnancies. Around one in 10,000 spontaneously conceived pregnancies involves monoamniotic twins [4-6]. Cord entanglement and conjoined twins are some complications unique to monoamniotic monochorionic pregnancy. This case report describes a case of monoamniotic twins' intrauterine demise due to lethal cord entanglement.
Case presentation
A 26-year-old unbooked primigravida reported in the emergency labor room at 32 weeks with the complaint of loss of fetal movements since the previous day. She was sure of her last menstrual period. She had acknowledged her pregnancy when a urine pregnancy test showed a positive result two days after she missed her period, and this was a spontaneous conception after one year of marriage. She had three antenatal visits at the local health care center before reporting to our emergency labor room. She had complained of excessive nausea and vomiting during the first trimester; otherwise, her antenatal period had been uneventful. She had two ultrasound scan reports for fetal well-being; the earliest scan was at 12 weeks and the latest was at 28 weeks. Twin pregnancy with adequate amniotic liquor and a fundal-anterior placenta was mentioned in the reports. There were no comments on chorionicity.
On general examination, she had mild pallor, bipedal edema, a pulse rate of 98 beats per minute, and a blood pressure of 150/90 mmHg. On obstetric examination, the uterus appeared enlarged and discordant with the gestational age, multiple fetal parts were felt on palpation, and the pelvic grip was empty. Doppler could not detect any fetal heartbeat. A vaginal examination revealed that the os was closed, and the cervix was posterior.
The emergency obstetric sonography scan showed twins, the first in the breech and the second in vertex presentation. Fetal heart sound was not found in either of the twins. The patient was counseled, and the decision was taken to terminate the pregnancy by lower-segment cesarean section.
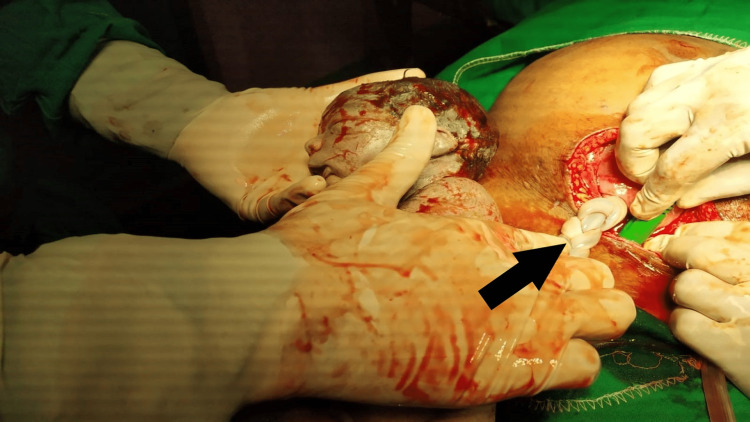
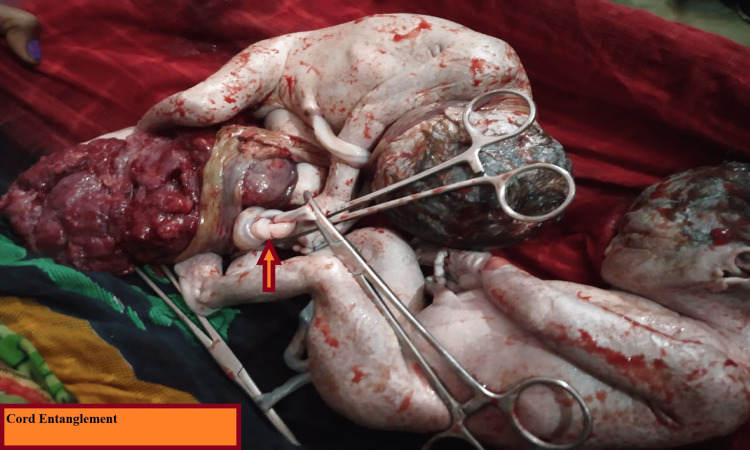
During the cesarean to deliver the babies, monochorionic and monoamniotic pregnancy was confirmed by the following features: a single placenta, where the two cords were inserted centrally within 6 cm from each other, the absence of an intertwining membrane, and same-sex babies. The entanglement of the cords, which we suspected was the cause of intrauterine death, was unique. Figures 1, 2 show intrauterine twin demise with entangled cords.
Figure 1. Intrauterine demise with thrombosed entangled cord.
Black arrow shows thrombosed cord after entanglement
Figure 2. Dead twins with cord entanglement.
Arrow shows cord entanglement
Post-cesarean, the patient was moved to the recovery ward. Milk suppression treatment was given, the patient was counseled, and her post-partum period was uneventful.
Discussion
Proper antenatal care and the timely detection of abnormality with timely intervention, which were altogether absent in this case, are critical in managing monochorionic monoamniotic pregnancies.
Monoamniotic monochorionic pregnancies can be diagnosed prenatally in the first trimester. The features include a single placenta that is not fused and no intertwining membrane between same-sex twins [7]. Fetal mortality is very high in monoamniotic gestations, around 12-23% [8-10], due to the complications unique to this gestation, such as cord entanglement and conjoined twins, and other complications associated with different types of twin pregnancies.
Cord entanglement, when found on ultrasonography, is pathognomonic for monoamniotic twins. It can be seen as early as 12-13 weeks of pregnancy and diagnosed after visualization of intertwined umbilical cords, which, upon Doppler insonation, show different fetal heart rates [5,11-13]. In the first trimester, cord entanglements may appear loose but can tighten at any time [14]. According to some studies, intermittent occlusion of umbilical blood vessels may be associated with neurological morbidity, while severe prolonged occlusion can be fatal [14,15]. Inpatient antepartum fetal monitoring and early delivery have been found to reduce the perinatal death rates in monoamniotic twin pregnancies. Monoamniotic twin pregnancies should be delivered by cesarean section between 32 and 34 weeks [16,17].
Conclusions
Prenatal care is of utmost importance for monochorionic monoamniotic pregnancies. Antepartum fetal surveillance should be started early, at 24-28 weeks, and inpatient monitoring seems more beneficial. Delivery should be by cesarean section, and tertiary health care with the facility of a special newborn care unit should be available as the risk of prematurity and congenital anomalies is extremely high.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Zygotic-splitting rates after single-embryo transfers in in vitro fertilization. Blickstein I, Jones C, Keith LG. N Engl J Med. 2003;348:2366–2367. doi: 10.1056/NEJMc026724. [DOI] [PubMed] [Google Scholar]
- 2.What makes them split? Identifying risk factors that lead to monozygotic twins after in vitro fertilization. Knopman JM, Krey LC, Oh C, Lee J, McCaffrey C, Noyes N. Fertil Steril. 2014;102:82–89. doi: 10.1016/j.fertnstert.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 3.Assisted reproductive technologies and monozygous twins: implications for future study and clinical practice. Sills ES, Tucker MJ, Palermo GD. Twin Res. 2000;3:217. doi: 10.1375/136905200320565184. [DOI] [PubMed] [Google Scholar]
- 4.Monoamniotic twinning and zona manipulation: a survey of U.S. IVF centers correlating zona manipulation procedures and high-risk twinning frequency. Slotnick RN, Ortega JE. J Assist Reprod Genet. 1996;13:381–385. doi: 10.1007/BF02066168. [DOI] [PubMed] [Google Scholar]
- 5.Monoamniotic and pseudomonoamniotic twins: sonographic diagnosis, detection of cord entanglement, and obstetric management. Aisenbrey GA, Catanzarite VA, Hurley TJ, et al. Obstet Gynecol. 1995;86:218. doi: 10.1016/0029-7844(95)00130-j. [DOI] [PubMed] [Google Scholar]
- 6.Population-based study of sex proportion in monoamniotic twins. Derom C, Vlietinck R, Derom R, Van den Berghe H, Thiery M. N Engl J Med. 1988;319:119–120. doi: 10.1056/NEJM198807143190215. [DOI] [PubMed] [Google Scholar]
- 7.Sonographic detection of monoamniotic twins. Blane CE, DiPietro MA, Johnson MZ, White SJ, Louwsma GI, Hamman JE. J Clin Ultrasound. 1987;15:394–396. doi: 10.1002/jcu.1870150607. [DOI] [PubMed] [Google Scholar]
- 8.Improved perinatal survival of monoamniotic twins with intensive inpatient monitoring. Heyborne KD, Porreco RP, Garite TJ, Phair K, Abril D. Am J Obstet Gynecol. 2005;192:96–101. doi: 10.1016/j.ajog.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 9.Perinatal outcome of monoamniotic twin pregnancies. Hack KE, Derks JB, Schaap AH, et al. Obstet Gynecol. 2009;113:353–360. doi: 10.1097/AOG.0b013e318195bd57. [DOI] [PubMed] [Google Scholar]
- 10.Perinatal outcomes in monoamniotic gestations. Roqué H, Gillen-Goldstein J, Funai E, Young BK, Lockwood CJ. J Matern Fetal Neonatal Med. 2003;13:414–421. doi: 10.1080/jmf.13.6.414.421. [DOI] [PubMed] [Google Scholar]
- 11.Early prenatal diagnosis of cord entanglement in monoamniotic multiple pregnancies. Arabin B, Laurini RN, van Eyck J. Ultrasound Obstet Gynecol. 1999;13:181–186. doi: 10.1046/j.1469-0705.1999.13030181.x. [DOI] [PubMed] [Google Scholar]
- 12.First-trimester cord entanglement in monoamniotic twins. Overton TG, Denbow ML, Duncan KR, Fisk NM. Ultrasound Obstet Gynecol. 1999;13:140–142. doi: 10.1046/j.1469-0705.1999.13020140.x. [DOI] [PubMed] [Google Scholar]
- 13.The use of color flow Doppler ultrasonography to diagnose umbilical cord entanglement in monoamniotic twin gestations. Belfort MA, Moise KJ Jr, Kirshon B, Saade G. Am J Obstet Gynecol. 1993;168:601. doi: 10.1016/0002-9378(93)90502-a. [DOI] [PubMed] [Google Scholar]
- 14.Cord entanglement and perinatal outcome in monoamniotic twin pregnancies. Dias T, Mahsud-Dornan S, Bhide A, Papageorghiou AT, Thilaganathan B. Ultrasound Obstet Gynecol. 2010;35:201–204. doi: 10.1002/uog.7501. [DOI] [PubMed] [Google Scholar]
- 15.Clinical associations of prenatal ischaemic white matter injury. Gaffney G, Squier MV, Johnson A, Flavell V, Sellers S. Arch Dis Child Fetal Neonatal Ed. 1994;70:0–6. doi: 10.1136/fn.70.2.f101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prenatal management of monoamniotic twin pregnancies. Van Mieghem T, De Heus R, Lewi L, et al. Obstet Gynecol. 2014;124:498–506. doi: 10.1097/AOG.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 17.Delivery of twins. Lee YM. Semin Perinatol. 2012;36:195–200. doi: 10.1053/j.semperi.2012.02.004. [DOI] [PubMed] [Google Scholar]