Abstract
Introduction
Complications secondary to spilled gallstones can be classified in the category of disease of medical progress because prior to advent of laparoscopic cholecystectomy very few reports published on the topic. The aim of the present study was to investigate the predisposing factors and the complication rate of spilled gallstones during laparoscopic cholecystectomy over the past 21 years.
Methods
Embase, Pubmed, Medline, Google scholar and Cochrane library were systematically searched for pertinent literature.
Results
Seventy five out of 181 articles were selected including 85 patients; of those 38% were men and 62% women. The median age of the cohort was 64 years old and ranged between 33 and 87 years. Only 23(27%) of the authors reported the incident of spillage of the gallstones during the operation. Time of onset of symptoms varied widely from the second postoperative day to 15 years later. Ten of 85 patients were asymptomatic and diagnosed with spilled gallstones incidentally. The rest of the patients presented with complications of severe morbidity and almost, 87% of the patients needed to be treated with surgical intervention and 12% with US ± CT scan guidance drainage. Only one perioperative death reported.
Conclusions
Symptomatic patients with lost gallstones present with severe morbidity complications and required mostly major surgical procedures. Therefore, standardisation of the management of spilled gallstones is needed urgently. Hospitals need to review their policy with audits and recommendations and clinical guidelines are needed urgently.
Keywords: Spilled, Lost, Gallstones, Laparoscopic cholecystectomy, Systematic review
Introduction
Since 1992, laparoscopic cholecystectomy accepted as a treatment of choice for symptomatic cholelithiasis by consensus statement from the National Institute of health conference [1]. It has been reported that the incidence rate of perforation of gallbladder during laparoscopic cholecystectomy (LC) ranges from 6 to 40% [2, 3]. The incidence rate of spillage of gallstones secondary to perforation reported 16% [4]. In addition, 16 to 50% of spilled stones remained un-retrieved [4, 5]. They may migrate in different regions and the reported complication rate varies from 0.08 to 0.3% [6]. However, most recent evidence reported that the incidence rate of complications of spilled gallstones may ranges from 0.04 to 19% [7]. The management of the spilled gallstones varies widely. Notably, studies which analyse complications of the LCs did not mention perforation of the gallbladder and spillage of stones as complication [8]. In addition, a study from the UK reported that only one fifth of the surgeons document spillage of the gallstones as a potential complication in the consent form. Moreover, only half of them in case of spillage and un-retrieved stones inform the patient. They are reluctant to do that because this may lead to unnecessary stress and repeated examinations for presumed complications of low risk [9]. However, most recent evidence demonstrated that gallbladder perforation and spillage of stones may lead to complications of severe morbidity. In particular, acute cases, older age, male sex, number of spilled stones more than 15 with diameter > 1.5 cm, pigment stones and perihepatic localisation are predicting factors for developing severe complications [3].
Because of lack of consensus recommendations and guidelines the management of spilled gallstones vary widely between institutions and individual surgeons. Therefore, the need for further evaluation of the accumulated evidence is needed urgently.
The aim of the present study was to evaluate the evidence of the complications rate of the spilled gallstones overtime by conducting a systematic review.
Methods
Literature search strategy
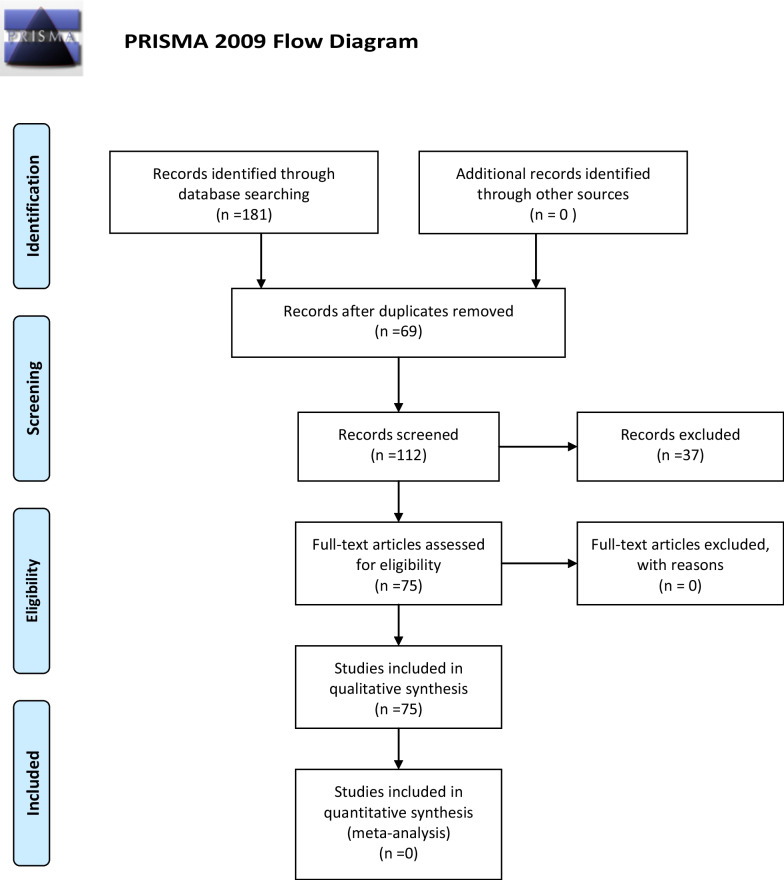
From 2000 until today a literature search was performed in Embase, Medline (Pubmed), Cochrane library, Google scholar, and National Institute for Health and clinical Excellence (NICE) databases using free and MeSH terms (spilled, lost gallstones, complications during laparoscopic cholecystectomy, late complications after laparoscopic cholecystectomy, intraabdominal abscess, retroperitoneal abscess, flank abscess, pigment gallstones, cholesterol gallstones). The search strategy was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [10].
Study, selection, and inclusion and exclusion criteria
Publications evaluating the complications of spilled gallstones during laparoscopic cholecystectomy were included. Studies referred to open cholecystectomy and editorials without original data were excluded.
Data extraction and outcomes
Two reviewers (PG and NDA) independently extracted the following data from the included studies: name of authors, country, year of publication, age, gender, indication for laparoscopic cholecystectomy, reference to spilled gallstones, type of lost stones, number of stones spilled, size of lost stones, location of lost stones, presenting symptoms, time of onset of symptoms after the laparoscopic cholecystectomy, complications caused by lost stones and location found, type of reintervention, 90-day perioperative mortality.
Results
Seventy-five articles from a pool of 181 articles were selected including 85 patients [11–85], (Fig. 1, Table 1). The median age of the cohort was 64 years and ranged between 33 and 87 years. The percentage of males and females were of 38% and 62%, respectively. The acute cases were 26(31%). Only 23(27%) of the surgeons reported the perforation of the gallbladder and consequently, spillage of the gallstones in the operative notes. The median time of onset of symptoms was 36 months and ranged between 1 and 180 months; the mode was 24 months. The most common site of lost stones was the right subhepatic, perihepatic, retroperitoneal, right flank and pelvis. Ten (12%) out of 85 cases of lost stones discovered incidentally [18, 19, 23, 39, 47, 49, 52, 58, 71, 75]. Type of lost gallstones discovered during the re-intervention reported by 17 authors(20%), [18–20, 24, 31, 35, 39, 42, 43, 53, 54, 63, 80]; of those 7 (41%) were pigment and 8 (47%) cholesterol gallstones. Seventeen(20%) of authors reported the number of discovered gallstones [18, 25, 27–29, 31, 35, 38, 39, 44, 45, 50, 54, 57, 70, 80, 83]. The size of discovered gallstones was reported by 12(14.11%) authors [18, 19, 25, 28, 31, 35, 37, 52, 63]. The most prevalent presenting symptoms were pain, fever, nausea, vomiting, abdominal swelling, fistula formation, and loss of weight. The most prevalent complications were intrabdominal abscesses 31(36.5%), abdominal wall abscesses 9(10.6%), retroperitoneal abscesses 8(9.4%), thus abscesses in total consisted of 48(56.5%) cases. Notably, 87% of patients underwent a surgical procedure and 12% treated with US ± CT scan guidance drainage, two cases that diagnosed incidentally and were asymptomatic scheduled for regular follow-ups (Table 1). One patient died on the 11th postoperative day after lung decortication for thoracic empyema secondary to lost gallstones [15].
Fig. 1.
Diagram of the search strategy
Table 1.
Study characteristics of the publications for the complications of the spilled gallstones
| Author, country, year | Number of patients | Age | Indication for LC | Reference to the spilled stones | Presenting symptoms | Time of onset of symptoms after LC | Complications caused by Lost stones and location found | Type of reintervention |
|---|---|---|---|---|---|---|---|---|
|
Ray S India, 2021 |
1 | 48 | NR | NR | Low-grade fever and swelling on the site of the axillary port | 39 months | Tender swelling on the site of the axillary port | Surgical removal |
|
Mehmood UK, 2021 |
1 | 65 | Symptomatic cholelithiasis | Yes | Long standing dry cough, fever and painful swelling over the back in the right paraspinal area | 8 years | Large abscess in the right paraspinal region and retroperitoneal abscess | I + D |
|
Guruvaiah USA, 2021 |
1 | 61 | Acute cholecystitis | Yes | 1-year history of intermittent RUQ pain, recurrent bronchitis and pneumonia with mucopurulent cough and sputum since his LC | Recurrent pneumonia since his LC | Bronchobiliary fistula | Trans-diaphragmatic takedown of the BBF and right hepatic middle lobe wedge resection |
|
Djelassi Belgium, 2021 |
1 | 82 | Perforated necrotic cholecystitis | NR | Chronic fistula at the RUQ | 8 years | Abscess between the right internal oblique and transverses abdominis | Fistulectomy and drainage |
|
Tchercansky Argentina, 2020 |
1 | 69 | Gallbladder empyema | Yes | Loculated pleural effusion of the Right Hemithorax in posterior cost-diaphragmatic recess | 5 months | Pleural effusion | CT guided thoracic drainage initially and then Lung decortication by Video Assisted Thoracoscopy |
|
Kafadar Turkey, 2020 |
1 | 42 | NR | NR | Painful swelling in suprapubic region persistent for 3 days | 10 years | Omental granuloma | Partial omentectomy |
|
Marçal Portugal, 2020 |
1 | 79 | Symptomatic cholelithiasis | NR | Emergent admission for Right subcutaneous lumbar abscess 10 cm with no retroperitoneal extension and renal involvement | 3 years | Right subcutaneous lumbar abscess | Surgical drainage |
|
Bolat Turkey, 2020 |
1 | 62 | Acute Cholecystitis | NR | Incidental finding in the right inguinal hernial sac | 5 months | Incidental finding in the right inguinal hernial sac | Surgical excision |
|
Heywood Australia, 2019 |
1 | 70 | Emergency LC | NR | Incidental finding in the right inguinal hernial sac | 5 years | Incidental finding in the right inguinal hernial sac | Surgical excision |
|
Cummings USA, 2019 |
1 | 70 | Emphysematous cholecystitis and liver abscess | Yes | vague abdominal discomfort | 2 years | Sub hepatic | Surgical exploration + drainage |
|
Akhtar Pakistan, 2018 |
1 | 78 | NR | NR | Recurrent bouts of abdominal pain and fever for the previous 2 weeks in the RUQ | 10 years | 19 cm Right subdiaphragmatic and retroperitoneal abscess | CT-guided drainage |
|
Tyagi USA, 2018 |
1 | 70 | Acute Cholecystitis | Yes | Septic shock CT scan: two partly calcified soft tissue masses associated with the right iliopsoas and obturator internal muscles | 2 months | Iliopsoas abscess and periprosthetic hip infection | Surgical drainage |
|
Capolupo Italy, 2018 |
1 | 73 | Chronic cholecystitis | Yes | Peritoneal nodule detected during FU for kidney stones | 16 months | Peritoneum, NO complications | Laparoscopic excision |
|
Urade Japan, 2018 |
1 | 68 | Gangrenous Cholecystitis | Yes | CT findings of omental abscess and ascites around the spleen | 7 months | Omental abscess | Laparoscopic partial omentectomy |
|
Ologun 2018 |
1 | 52 | Biliary colic | NR | Occasional postpranding epigastric pain | 4 years | Calcified intraabdominal mass within the omentum detected in routine FU for Lap sleeve gastrectomy | Laparoscopic resection of the mass |
|
Stroobants Belgium, 2018 |
1 | 72 | Symptomatic cholelithiasis | NR | Intermittent complains for RUQ pain | NR | Subhepatic abscess | Open drainage |
|
Kaplan Israel, 2018 |
1 | 73 | NR | NR | Six months vague RUQ pain | 10 years | Perihepatic abscess | Lap drainage |
|
Kaplan B 2018 |
1 | 41 | NR | NR | One-month vague RUQ pain | 3 years | Perihepatic abscess | Lap drainage |
|
Koichopolos Canada, 2017 |
1 | 80 | NR | NR | Gastric outlet obstruction, 30 pounds weight loss, progressively worsening nausea, vomiting and significant gastroesophageal reflux | NR | Intramural obstruction of pylorus | Billroth II Distal gastrectomy |
|
Canna UK, 2017 |
1 | 79 | Chronic cholecystitis | NR | Painful and firm mass on the right flank | 5 years | Retroperitoneal abscess | Surgical drainage |
|
Lentz USA, 2017 |
1 | 57 | Symptomatic cholelithiasis | NR | Cough and right flank pain | 2 years | Perihepatic, pulmonary and renal abscesses | Thoracic drainage |
|
Faour Syria, 2017 |
1 | 44 | Symptomatic cholelithiasis | NR | Mass in the RUQ associated with pain, nausea and early satiety for the last 6 months | 6 years | Intra-abdominal cystic mass | Surgical excision |
|
Ragozzino Italy, 2016 |
1 | 63 | Chronic cholecystitis | NR | Intermittent vague discomfort of RUQ | 2 years | Subphrenic abscess | 3 × 3 cm mass excised |
|
Kim Korea, 2016 |
1 | 59 | NR | NR | Constant RUQ pain | 5 months | Retroperitoneal mass | 5 × 5 cm retroperitoneal mass was excised |
|
Goodman USA, 2016 |
1 | 87 | Acute Cholecystitis | NR | Right flank pain and tenderness | 4 years | Right flank soft tissue tumour | Surgical excision |
|
Moga Romania, 2016 |
1 | 66 | Acute Cholecystitis | NR | Fever and large abscess in the right lumbar region | 4 years | Right lumbar region abscess and subhepatic abscess | Lap drainage |
|
Bedell USA, 2015 |
1 | 41 | Symptomatic cholelithiasis | NR | Dysmenorrhea progressed to chronic pelvic pain unrelated to menses | 9 years | pelvic abscess | Lap drainage |
|
Binagi USA, 2015 |
1 | 58 | Symptomatic cholelithiasis | NR | Continuous but waxed and waned pain, reaching levels eight out of ten of Likert scale | 3 years | Perihepatic abscess | Lap drainage |
|
Grass Switzerland, 2015 |
1 | 75 | Acute cholecystitis | NR | Periumbilical redness and tenderness | 3 years | Abdominal wall abscess in the periumbilical port site | Drainage |
|
Noda Japan 2014 |
1 | 52 | Symptomatic cholelithiasis | NR | Incidental US finding during medical check up | 7 months | Sub hepatic abscess | Percutaneous abscess drainage |
|
Noda Japan, 2014 |
1 | 41 | Symptomatic cholelithiasis | NR | RUQ pain | 13 months | A rounded mass in the subhepatic space | Open drainage |
|
Ahmad UK, 2014 |
1 | 37 | Symptomatic cholelithiasis, incidental pT1a gallbladder cancer | Yes | Recurrent pain two year after LC | 2 years | Multiple tumour embedded gallstones on the diaphragm and lesion in segment VI of the liver | Surgical excision of diaphragmatic nodules and liver segmentectomy VI |
|
Lee Korea, 2013 |
5 | 65/55/48/72/80 | 1.recurrent ac ch/tis 2. Gangrenous Ch/tis 3. Recurrent ac ch/tis 4. Gangrenous ch/tis 5. Recurrent ac ch/tis | Yes | NR | 7/18/31/4 months 2nd post day | Subhepatic abscess/cul de sac abscess/umbilical fistula/portal fistula/peritonitis | Drainage/drainage/prolonged wound care/antibiotic administration |
|
Morris USA, 2013 |
1 | 71 | NR | Pulmonary complains of diffuse abdominal pain, associated with nausea and emesis lasted for 24 h | 15 years | Dense mesenteric cicatrix causing ileocolic torsion and cecal volvulus | Ileocecectomy | |
|
Peravali UK, 2013 |
1 | 61 | Acute Cholecystitis | Yes | 12-month history of persistent RUQ pain, 8 KG weight loss, anorexia, night sweats, intermittent pyrexical episodes | 3 years | Sub hepatic abscess | Lap drainage |
|
Peravali UK, 2013 |
1 | 86 | Acute cholecystitis | Yes | Chronically discharged right back fistula | 5 years | Subphrenic abscess with atmospheric fistula | Lap drainage |
|
Dobradin 2013 |
1 | 82 | Elective cholecystectomy | NR | RUQ pain lasting for 2 months | 8 years | Right flank abscess | I + D |
|
Chatzimavroudis Greece, 2012 |
1 | 72 | Symptomatic cholelithiasis | Yes | High fever, chills and constant pain in the Right lumbar region for 2 days | 6 months | Retroperitoneal abscess | CT-guided drainage |
|
Gorospe Spain, 2013 |
1 | 63 | Acute Cholecystitis | NR | Fever, malaise, weight loss | 6w | Fever of unknown aetiology | NR |
|
Anrique Chile, 2013 |
1 | 60 | NR | NR | Incidental finding during Lap Gynaecologic procedure | 14 years | Multiple gallstones incrusted in the Douglas’ pouch | Surgical removal |
|
Arai ColonJapan, 2013 |
1 | 65 | Symptomatic cholelithiasis | NR | Referred by GP for further investigation of an abnormal liver mass | 4 years | Subphrenic abscess | Wedge resection of the liver and diaphragm |
|
Papadopoulos Greece, 2012 |
1 | 86 | Symptomatic cholelithiasis | NR | Incidental finding during right hemicolectomy | 8 years | Gallstones embedded in the omentum | Removal during right hemicolectomy |
|
Singh USA, 2012 |
1 | 42 | NR | NR | Worsening Right-sided tenderness and pain, low grade fever, night chills | 7 years | 50 pounds weight loss over 5 months | Surgical excision of 4 × 6 cm |
|
Rammohan India, 2012 |
1 | 50 | NR | NR | Minimally painful, slow progressing mass in the RUQ for the last two years | 4 years | 10 × 5 cm organised extrahepatic mass in the sub-diaphragmatic space extending onto the soft tissues of parietal wall | Laparoscopic piecemeal excision |
|
Kayashima Japan, 2011 |
1 | 57 | Acute cholecystitis | Yes | Incidental abdominal US showed 3 liver lesions | 3 years | Inflammatory pseudotumour of the liver | Posterior segmentectomy and concomitant resection of the diaphragm |
|
Hussain Saudi Arabia, 2010 |
1 | 33 | Acute cholecystitis | Yes | Intermittent attacks of pain RUQ, nausea, vomiting for 7 months | 9 years | Discharging abdominal wall abscess extending to the retroperitoneum | I + D |
|
Pottakkat India, 2010 |
1 | Symptomatic cholelithiasis | NR | Fever, malaise | 11 years | Dumbbell abscess in the perihepatic area | Open drainage | |
|
Bouasker Tunisia, 2010 |
1 | 57 | Acute cholecystitis | NR | RIF painful swelling | 8 years | Subcutaneous collection | I + D |
|
Gooneratne New Zealand, 2010 |
1 | 54 | Acute cholecystitis | NR | Recurrent urinary tract infections | 14 years | Colovesical fistula | Surgical repair of the fistula |
|
Helme 2009 |
1 | 77 | NR | NR | Night sweets, right back pain and loin swelling for 2 weeks | 5 years | Complex subphrenic, subhepatic and subcutaneous abscesses | US-guided drainage. Patient declined operation to remove the offending gallstones |
|
Morishita Japan, 2009 |
1 | 67 | Symptomatic cholelithiasis | NR | Incidental finding during FU for aneurysm | 1 year | Granuloma | Conservative treatment |
|
Dasari UK, 2009 |
1 | 67 | Acute cholecystitis | Repeat laparoscopy for septicaemia and drainage of fluid collection | Recurrent lower abdominal pain | 2 years | Nodules mimicking peritoneal metastases | Lap excision |
|
Maempel UK, 2009 |
1 | 42 | Symptomatic cholelithiasis | NR | Strangulated recurrent paraumbilical hernia | 10 years | Abdominal wall abscess | I + D |
|
Hougård Denmark, 2008 |
1 | 64 | Acute cholecystitis | Yes | Referred for Management of abdominal fistulas | 7 years | Atmospheric fistula | Surgical excision |
|
Arishi Saudi Arabia, 2008 |
1 | 45 | Symptomatic cholelithiasis | NR | Central colicky abdominal pains and swelling lasted for 6 months | 15 years | Cystic mass of the rectus abdominis | Surgical excision |
|
De Hingh the Netherlands, 2007 |
1 | 41 | Acute Cholecystitis | Yes | NR | 1 year | Rectovaginal pouch abscess | Surgical excision |
|
Stupak USA, 2007 |
1 | 72 | NR | Yes | Fever, nausea, anorexia, and pain in the RUQ lasting for 3 weeks | 11 years | Subhepatic collection | US-guided percutaneous drainage |
|
Pantamowitz USA, 2007 |
1 | 53 | Symptomatic cholelithiasis | NR | Pelvic pain | 7 years | Left overs granuloma | Surgical excision |
|
Wehbe Australia, 2007 |
1 | 80 | Symptomatic cholelithiasis | NR | Abdominal pain, nausea, diarrhoea | 10 years | Mass in the right lower quadrant | Lap excision |
|
Wittich USA, 2007 |
1 | 42 | Symptomatic cholelithiasis | NR | Severe metrorrhagia, dysmenorrhea | 13 months | Abscess in the pouch of Douglas | 16 gallstones discovered after transvaginal hysterectomy for severe dysmenorrhoea and metrorrhagia |
|
Bhati UK, 2006 A |
1 | 52 | Symptomatic cholelithiasis | NR | Upper abdominal pain | 1w | CT: cystic mass in the left lobe of the liver | Open drainage |
|
Bhati UK, 2006 B |
1 | 60 | Symptomatic cholelithiasis | NR | Fever and pain in her back | 28 months | Subdiaphragmatic abscess | Open drainage |
|
Bhati UK, 2006 C |
1 | 56 | Symptomatic cholelithiasis | NR | Fever and pain of the upper abdomen | 7 years | Subdiaphragmatic abscess | I + D |
|
Ianniti USA, 2006 |
1 | 70 | Symptomatic cholelithiasis | NR | Generalised aches and pains | 18 months | Subphrenic + pleural abscess | Open and US guided drainage, due to recurrence open removal |
|
Hand USA, 2006 |
1 | 50 | Biliary pancreatitis | NR | Pain, fever, large fluctuant mass lateral to umbilicus | 2 years | Abdominal wall cystic mass | US-guided drainage, later local exploration and excision of the abscess |
|
Viera Italy, 2006 |
1 | 72 | Symptomatic cholelithiasis | NR | Fever, general malaise and weight loss | 18 months | 3 inflammatory lesions in seg II and VII | Open excision |
|
Viera Italy, 2006 |
1 | 70 | Acute Cholecystitis | Yes | Patient asymptomatic, incidental US finding | 2 months | Asymptomatic | Watch and see approach |
|
AlSamkari USA, 2004 |
1 | 36 | Symptomatic cholelithiasis | Yes | Diffuse abdominal pain nausea, vomiting and weakness | 11 years | Necrotic transverse colon from mid-ascending to just distal the splenic flexure | Surgical excision |
|
Koç Turkey, 2004 |
1 | 75 | Symptomatic cholelithiasis | NR | NR | 6 years | Retroperitoneal abscess | Percutaneous drainage |
| Stevens, 2003 | 1 | 68 | Gallstone pancreatitis | NR | 30-pound weight loss and acholic stools | 1 year | Subhepatic abscess | Open drainage |
|
Aspelung Iceland 2003 |
1 | NR | NR | NR | Incidental finding during routine hernioplasty | days 10 | Gallstones in the hernial sac | Removal during hernia repair |
|
Papasavas Greece, 2002 |
1 | 77 | Symptomatic cholelithiasis | Yes | Fever, pain | 15 months | Right flank abscess | Surgical removal |
| Yadav, 2002 | 1 | NR | Symptomatic cholelithiasis | NR | NR | 1 year | Subphrenic abscess | Open drainage |
| Van Mierlo, 2002 | 1 | 48 | Symptomatic cholelithiasis | Yes | Pain in the RUQ, nausea, vomiting | 2 years | Subhepatic abscess | Open drainage |
| Hawasli, 2002 A | 1 | 75 | Symptomatic cholelithiasis | NR | Pain, fever | 4 years | Abdominal wall abscess | Open drainage |
| Hawasli, 2002 B | 1 | 43 | Symptomatic cholelithiasis | NR | Pain, fever | 2 months | Subdiaphragmatic and subhepatic abscesses | |
| Famulari, 2002 | 1 | NR | Symptomatic cholelithiasis | NR | Dysuria, pollakiuria, vesical tenesmus | 2 years | Urinary bladder granuloma | Partial cystectomy |
|
Werber USA, 2001 |
1 | 64 | Symptomatic cholelithiasis | Yes | Low-grade fever with chills, night sweats, weight loss, fatigue | 1 month | Sub hepatic abscess and 3 cm round mass with speculated borders in the right lower lobe of the lung | Right thoracotomy |
|
Yao China, 2001 |
1 | NR | Symptomatic cholelithiasis | NR | NR | 2 years | Periumbilical abscess | Surgical excision |
|
Battaglia Italy, 2001 |
1 | 39 | Symptomatic cholelithiasis | NR | Fever and pain | 9 years | Abdominal wall abscess | Surgical excision |
|
Ok E Turkey, 2000 |
1 | NR | Symptomatic cholelithiasis | NR | Umbilical port site hernia | 3 months | Incisional umbilical port site hernia | Surgical excision |
| Bebawi, USA. 2000 | 1 | 56 | Chronic cholecystitis | Yes | Incidental finding | 2 months | Gallstones in the hernial sac | Removed during hernia repair |
| Total | 85 cases | 64(33–87) | Acute cases 26(31%) | 23 authors (27%) |
Most prevalent Fever and pain |
36 months (1–180) |
TA: 48(56.5%) IAA:31(36.5%) RPA: 8(9.4%) AWA: 9(10.6%) IF:10(11.8%) |
Open procedure 61 (72%) Lap procedure: 13 (15%) US or CT drainage: 9(11%) 2 watch and see approach |
IAA intraabdominal abscesses, RPA retroperitoneal abscesses, AWA abdominal wall abscesses, TA total abscesses, IF incidental findings: incidental findings, Seg segment, LC laparoscopic cholecystectomy, NR nonreported
Discussion
Complications of the spilled gallstones can be described under the umbrella eponym, disease of the medical progress DOMP. There is a contrasting difference with the open cholecystectomy; because spillage of gallstones during open cholecystectomy is more easier identified and retrieved there are very few reports with the above complication [86, 87].
At the present 96% of all cholecystectomies are performed laparoscopically [88]. In general, the characteristics of the cohorts of patients who underwent laparoscopic and open cholecystectomies differ essentially. The laparoscopic cohort is consisted of younger and healthier patients whereas the open cohort tend to be older, less well, and generally the open cholecystectomy is performed in higher-risk patients [89, 90]. Another important characteristic of the laparoscopic era is the broadening of the indications and the dramatic increase in the number of LCs performed for acalculous disease [91].
Taking into account that present studies reported that older age is a predicting factor for developing complications following spillage of gallstones [3]. We can see a controversy with the above evidence that demonstrates that the LC cohort includes younger and healthier patients. Therefore, there is a strong indication for further investigation and identification of the co-factors (e. g comorbidities, type of gallstones, acute vs chronic cases) that predispose to above complication. In the present study the median age was 64 years and varied widely from 33 to 87 years (Table 1).
An analysis performed at American College of Surgeons-National Surgical Quality Improvement Program hospitals found the rates of severe morbidity of laparoscopic and open cholecystectomy to be 1.4% and 11.1%, respectively [92].
Notably, the Swiss Association of Laparoscopic and Thoracoscopic Surgeons (SALTS) database defined the rates following LC for patients only with diagnosis of acute or chronic cholecystitis for intraoperative complications at 7%, postoperative local complications at 4%, and postoperative systemic complications at 2.3% [93]. The above comparison demonstrates that when the investigation is further focused to acute vs chronic cases the incidence rate of severe morbidity of LC increases dramatically from 1.4 to 7% [92, 93]. Although, it is reported that the acute cholecystitis is predisposing factor for complications of spilled gallstones [3]; in the present study only 31% were the acute cases. Therefore, future studies need to shed further light on the above topic. Moreover, in the present study, only 23(27%) of the surgeons reported the incidence of gallbladder perforation and spillage of gallstones in the operative notes. Furthermore, Mullerat et al. reported that only one fifth of the surgeons included in the consent form spillage of the gallstones as a potential complication. In addition, if this occurred during the operation they do not report it to GPs and patient because they consider it an innocent complication; although this information is going to help colleagues to resolve future diagnostic dilemmas [9].
Although, it is reported that the number of spilled gallstones more than 15, size > 1.5 cm and pigment type gallstones are predicting factors of complications of spilled gallstones [3]; in the present study, type of lost gallstones, number, and size of discovered gallstones during the re-intervention reported at 17(20%), 17(20%), and 12(14,11%), respectively. In particular, pigmented and cholesterol gallstones consisted 41% and 47%, respectively. Therefore, future studies should be more meticulous regarding describing type, size, and number of discovered gallstones because the accumulated information will further help describing in details the predicting risk factors and furthermore, this will help in the standardisation of the management of spilled gallstones.
The median time to onset of symptoms was 36 months and ranged from 1 to 180 months. It is obvious that was ranged widely. Considering the above finding and the widely ranged follow-up, the results of the incidence rates of complications should be treated cautiously because time, follow-up, and institutions bias might have influenced the results.
Notably, vast majority of the cases of undiscovered gallstones required open intervention. In particular, 61(72%) patients underwent open surgery and 13(15%) patient laparoscopic procedure, 9(11%) treated either with US and/or CT scan guided drainage. Two cases that detected early postoperatively and were asymptomatic scheduled for regular follow-ups. These finding underlines that although the incidence rate of the complications is low when they become symptomatic the treatment of choice is surgical intervention Therefore, there is urgent need for standardisation and clinical guidelines for the management of spilled gallstones.
Limitations
The results of the present study should be treated cautiously because all the included studies were case reports. Therefore, institutional, national, underpowered sample size, learning curve, performance and follow-up bias might have influenced the results. Another topic that needs special attention is the incidence rate. Usually, the cases with most complicated presentation and with worst outcomes published as case reports. On the contrary cases with mild symptoms and better outcomes, usually are not publishable. Therefore, an international registry and audit may help to define precisely the incidence rate, and severity of complications of spilled gallstones.
Conclusions
The current evidence demonstrates that although the incidence rate of complications varies widely the majority of the patients demonstrated severe morbidity and required surgical interventions. Therefore, urgent standardisation of the management of spilled gallstones is needed. Surgeons must document all cases of spilled stones in the operative notes. Moreover, GPs and patients should be informed about the incidence, this will help to resolve diagnostic dilemmas in the future. Hospitals should review their policy by conducting audits and surgical societies should use the above information and national databases in order urgently to formulate clinical guidelines.
Acknowledgements
None to declare
Author contributions
GP: conceptualization, formal analysis, investigation, methodology, software, validation, writing-original draft, editing, supervision; CF: formal analysis, investigation, methodology, validation, editing; GdA: formal analysis, investigation, methodology, validation, editing; NdA: conceptualization, formal analysis, investigation, methodology, software, validation, writing-original draft, editing, supervision. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The authors declare that data supporting the findings of this study are available within the article.
Declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
All the authors approved the present manuscript.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gallstones and Laparoscopic Cholecystectomy. NIH Conse Statement 1992, 10:1–20. http://www.ncbi.nlm.nih.gov/pubmed/1301217 [PubMed]
- 2.Soper NJ, Dunnegan DL. Does intraoperative gallbladder perforation influence the early outcome of laparoscopic cholecystectomy? Surg Laparosc Endosc. 1991;1(3):156–161. [PubMed] [Google Scholar]
- 3.Brockmann JG, Kocher T, Senninger NJ, Schürmann GM. Complications due to gallstones lost during laparoscopic cholecystectomy. Surg Endosc. 2002;16(8):1226–1232. doi: 10.1007/s00464-001-9173-8. [DOI] [PubMed] [Google Scholar]
- 4.Diez J, Arozamena C, Gutierrez L, Bracco J, Mon A, Sanchez Almeyra R, Secchi M. Lost stones during laparoscopic cholecystectomy. HPB Surg. 1998;11(2):105–109. doi: 10.1155/1998/95874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarli L, Pietra N, Costi R, Grattarola M. Gallbladder perforation during laparoscopic cholecystectomy. World J Surg. 1999;23(11):1186–1190. doi: 10.1007/s002689900644. [DOI] [PubMed] [Google Scholar]
- 6.Sathesh-Kumar T, Saklani AP, Vinayagan R, Blackett RL. Spilled gallstones during laparoscopic cholecystectomy: a review of the literature. Postgrad Med J. 2004;80:77–79. doi: 10.1136/pmj.2003.006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabbari Nooghabi A, Hassanpour M, Jangjoo A. Consequences of lost gallstones during laparoscopic cholecystectomy: a review article. Surg Laparosc Endosc Percutan Tech. 2016;26:183–192. doi: 10.1097/SLE.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 8.Atabek U, Spence RK, Manigat Y, Barse F, Leese KH, Davies R, Vilanueva D, Camishion RC. Documentation of abdominal exploration during laparoscopic cholecystectomy. Surg Endosc. 1995;9(1):22–24. doi: 10.1007/BF00187879. [DOI] [PubMed] [Google Scholar]
- 9.Mullerat J, Cooper K, Box B, Soin B. The case for standardisation of the management of gallstones spilled and not retrieved at laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2008;90:310–312. doi: 10.1308/003588408X285883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(6):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray S, Kumar D, Garai D, Khamrui S. Dropped gallstone-related right subhepatic and parietal wall abscess: a rare complication after laparoscopic cholecystectomy. ACG Case Rep J. 2021;8(5):e00579. doi: 10.14309/crj.0000000000000579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehmood S, Singh S, Igwe C, Obasi CO, Thomas RL. Gallstone extraction from a back abscess resulting from spilled gallstones during laparoscopic cholecystectomy: a case report. J Surg Case Rep. 2021 doi: 10.1093/jscr/rjab293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guruvaiah N, Ponnatapura J. Bronchobiliary fistula: a rare postoperative complication of spilled gallstones from laparoscopic cholecystectomy. BMJ Case Rep. 2021;14(7):e243198. doi: 10.1136/bcr-2021-243198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Djelassi S, Vandenbroucke F, Schoneveld M. A curious case of recurrent abdominal wall infections. J Belg Soc Radiol. 2021;105(1):12. doi: 10.5334/jbsr.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tchercansky AN, Fernandez Alberti J, Panzardi N, Auvieux R, Buero A. Thoracic empyema after gallstone spillage in times of Covid. Int J Surg Case Rep. 2020;76:221–226. doi: 10.1016/j.ijscr.2020.09.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kafadar MT, Çetinkaya İ, Aday U, Başol Ö, Bilge H. Acute abdomen due to spilled gallstones: a diagnostic dilemma 10 years after laparoscopic cholecystectomy. J Surg Case Rep. 2020;2020(8):rjaa275. doi: 10.1093/jscr/rjaa275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marçal A, Pereira RV, Monteiro A, Dias J, Oliveira A, Pinto-de-Sousa J. Right lumbar abscess containing a gallstone-an unexpected late complication of laparoscopic cholecystectomy. J Surg Case Rep. 2020;2020(7):rjaa248. doi: 10.1093/jscr/rjaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolat H, Teke Z. Spilled gallstones found incidentally in a direct inguinal hernia sac: report of a case. Int J Surg Case Rep. 2020;66:218–220. doi: 10.1016/j.ijscr.2019.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heywood S, Wagstaff B, Tait N. An unusual site of gallstones five years after laparoscopic cholecystectomy. Int J Surg Case Rep. 2019;56:107–109. doi: 10.1016/j.ijscr.2019.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cummings K, Khoo T, Pal T, Psevdos G. Recurrence of Citobacter koseri-associated intra-abdominal infection 2 years after spilled gallstones during laparoscopic cholecystectomy. J Global Infect Dis. 2019;11:47–49. doi: 10.4103/jgid.jgid_9_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akhtar A, Bukhari MM, Tariq U, Sheikh AB, Siddiqui FS, Sohail MS, Khan A. Spilled gallstones silent for a decade: a case report and review of literature. Cureus. 2018;10(7):e2921. doi: 10.7759/cureus.2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tyagi V, Wiznia DH, Wyllie AK, Keggi KJ. Total hip lithiasis: a rare sequelae of spilled gallstones. Case Rep Orthop. 2018;14(2018):9706065. doi: 10.1155/2018/9706065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capolupo GT, Mascianà G, Carannante F, Caricato M. Spilled gallstones simulating peritoneal carcinomatosis: a case report and literature review. Int J Surg Case Rep. 2018;48:113–121. doi: 10.1016/j.ijscr.2018.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Urade T, Sawa H, Murata K, Mii Y, Iwatani Y, Futai R, Abe S, Sanuki T, Morinaga Y, Kuroda D. Omental abscess due to a spilled gallstone after laparoscopic cholecystectomy. Clin J Gastroenterol. 2018;11(5):433–436. doi: 10.1007/s12328-018-0853-5. [DOI] [PubMed] [Google Scholar]
- 25.Ologun GO, Lovely R, Sultany M, Aman M. Retained gallstone presenting as large intra-abdominal mass four years after laparoscopic cholecystectomy. Cureus. 2018;10(1):e2030. doi: 10.7759/cureus.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stroobants E, Cools P, Somville F. Case report: an unwanted leftover after laparoscopic cholecystectomy. Acta Chir Belg. 2018;118(3):196–198. doi: 10.1080/00015458.2017.1346035. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan U, Shpoliansky G, Abu Hatoum O, Kimmel B, Kopelman D. The lost stone - laparoscopic exploration of abscess cavity and retrieval of lost gallstone post cholecystectomy: a case series and review of the literature. Int J Surg Case Rep. 2018;53:43–45. doi: 10.1016/j.ijscr.2018.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koichopolos J, Hamidi M, Cecchini M, Leslie K. Gastric outlet obstruction by a lost gallstone: case report and literature review. Int J Surg Case Rep. 2017;41:128–131. doi: 10.1016/j.ijscr.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canna A, Adaba F, Sezen E, Bissett A, Finch GJ, Ihedioha U. Para-spinal abscess following gallstones spillage during laparoscopic cholecystectomy: an unusual presentation. J Surg Case Rep. 2017 doi: 10.1093/jscr/rjx052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lentz J, Tobar MA, Canders CP. Perihepatic, pulmonary, and renal abscesses due to spilled gallstones. J Emerg Med. 2017;52(5):e183–e185. doi: 10.1016/j.jemermed.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 31.Faour R, Sultan D, Houry R, Faour M, Ghazal A. Gallstone-related abdominal cystic mass presenting 6 years after laparoscopic cholecystectomy: a case report. Int J Surg Case Rep. 2017;32:70–72. doi: 10.1016/j.ijscr.2017.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ragozzino A, Puglia M, Romano F, Imbriaco M. Intra-hepatic spillage of gallstones as a late complication of laparoscopic cholecystectomy: MR imaging findings. Pol J Radiol. 2016;10(81):322–324. doi: 10.12659/PJR.896497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim BS, Joo SH, Kim HC. Spilled gallstones mimicking a retroperitoneal sarcoma following laparoscopic cholecystectomy. World J Gastroenterol. 2016;22(17):4421–4426. doi: 10.3748/wjg.v22.i17.4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goodman LF, Bateni CP, Bishop JW, Canter RJ. Delayed phlegmon with gallstone fragments masquerading as soft tissue sarcoma. J Surg Case Rep. 2016;2016(6):rjw106. doi: 10.1093/jscr/rjw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moga D, Perişanu Ș, Popenţiu A, Sora D, Magdu H. Right retroperitoneal and subhepatic abscess late complications due to spilled stones during laparoscopic cholecystectomy - case report. Chirurgia. 2016;111(1):67–70. [PubMed] [Google Scholar]
- 36.Bedell SL, Kho KA. Spilled gallstones after laparoscopic cholecystectomy associated with pelvic pain. Am J Obstet Gynecol. 2015;213(3):432.e1–2. doi: 10.1016/j.ajog.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 37.Binagi S, Keune J, Awad M. Immediate postoperative pain: an atypical presentation of dropped gallstones after laparoscopic cholecystectomy. Case Rep Surg. 2015;2015:930450. doi: 10.1155/2015/930450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grass F, Fournier I, Bettschart V. Abdominal wall abscess after cholecystectomy. BMC Res Notes. 2015;5(8):334. doi: 10.1186/s13104-015-1303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noda Y, Kanematsu M, Goshima S, Kondo H, Watanabe H, Kawada H, Kawai N, Tanahashi Y. Peritoneal chronic inflammatory mass formation due to gallstones lost during laparoscopic cholecystectomy. Clin Imaging. 2014;38(5):758–761. doi: 10.1016/j.clinimag.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 40.Ahmad J, Mayne AI, Zen Y, Loughrey MB, Kelly P, Taylor M. Spilled gallstones during laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2014;96(5):e18–20. doi: 10.1308/003588414X13946184900444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee W, Kwon J. Fate of lost gallstones during laparoscopic cholecystectomy. Korean J Hepato-Biliary-Pancreat Surg. 2013;17(2):66. doi: 10.14701/kjhbps.2013.17.2.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morris MW, Barker AK, Harrison JM, Anderson AJ, Vanderlan WB. Cicatrical cecal volvulus following laparoscopic cholecystectomy. JSLS. 2013;17(2):333–337. doi: 10.4293/108680813X13654754534314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peravali R, Harris A. Laparoscopic management of chronic abscess due to spilled gallstones. JSLS. 2013;17(4):657–660. doi: 10.4293/108680813X13654754535313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dobradin A, Jugmohan S, Dabul L. Gallstone-related abdominal abscess 8 years after laparoscopic cholecystectomy. JSLS. 2013;17(1):139–142. doi: 10.4293/108680812X13517013317518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chatzimavroudis G, Atmatzidis S, Papaziogas B, Galanis I, Koutelidakis I, Doulias T, Christopoulos P, Papadakis G, Atmatzidis K, Makris J. Retroperitoneal abscess formation as a result of spilled gallstones during laparoscopic cholecystectomy: an unusual case report. Case Rep Surg. 2012;2012:573092. doi: 10.1155/2012/573092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gorospe L. Intraperitoneal spilled gallstones presenting as fever of unknown origin after laparoscopic cholecystectomy: FDG PET/CT findings. Clin Nucl Med. 2012;37(8):819–820. doi: 10.1097/RLU.0b013e31824c6042. [DOI] [PubMed] [Google Scholar]
- 47.Anrique D, Kroker A, Ebert AD. “Blueberry Sign”: spilled gallstones after cholecystectomy as an uncommon finding. J Minim Invasive Gynecol. 2013;20(3):329. doi: 10.1016/j.jmig.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 48.Arai T, Ikeno T, Miyamoto H. Spilled gallstones mimicking a liver tumor. Clin Gastroenterol Hepatol. 2012;10(11):A32. doi: 10.1016/j.cgh.2012.06.026s. [DOI] [PubMed] [Google Scholar]
- 49.Papadopoulos IN, Christodoulou S, Economopoulos N. Asymptomatic omental granuloma following spillage of gallstones during laparoscopic cholecystectomy protects patients and influences surgeons' decisions: a review. Case Rep. 2012;2012(jan23 1):bcr1020114980–bcr1020114980. doi: 10.1136/bcr.10.2011.4980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh K, Wang ML, Ofori E, Widmann W, Alemi A, Nakaska M. Gallstone abscess as a result of dropped gallstones during laparoscopic cholecystectomy. Int J Surg Case Rep. 2012;3(12):611–613. doi: 10.1016/j.ijscr.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rammohan A, Srinivasan UP, Jeswanth S, Ravichandran P. Inflammatory pseudotumour secondary to spilled intra-abdominal gallstones. Int J Surg Case Rep. 2012;3(7):305–307. doi: 10.1016/j.ijscr.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kayashima H, Ikegami T, Ueo H, Tsubokawa N, Matsuura H, Okamoto D, Nakashima A, Okadome K. Inflammatory pseudotumor of the liver in association with spilled gallstones 3 years after laparoscopic cholecystectomy: report of a case. Asian J Endosc Surg. 2011;4(4):181–184. doi: 10.1111/j.1758-5910.2011.00094.x. [DOI] [PubMed] [Google Scholar]
- 53.Hussain MI, Al-Akeely MH, Alam MK, Al-Abood FM. Abdominal wall abscess following laparoscopic cholecystectomy: an unusual late complication of lost gallstones. J Coll Phys Surg Pak. 2010;20(11):763–765. [PubMed] [Google Scholar]
- 54.Pottakkat B, Sundaram M, Singh P. Abdominal wall abscess due to spilled gallstone presenting 11 years after laparoscopic cholecystectomy. Clin J Gastroenterol. 2010;3(6):324–326. doi: 10.1007/s12328-010-0180-y. [DOI] [PubMed] [Google Scholar]
- 55.Bouasker I, Zoghlami A, El Ouaer MA, Khalfallah M, Samaali I, Dziri C. Abcès pariétal fistulisé révèlant des calculs oubliés huit ans après une cholécystectomie laparoscopique [Parietal abscess revealing a lost gallstone 8 years after laparoscopic cholecystectomy] Tunis Med. 2010;88(4):277–279. [PubMed] [Google Scholar]
- 56.Gooneratne DL. A rare late complication of spilled gallstones. N Z Med J. 2010;123(1318):62–66. [PubMed] [Google Scholar]
- 57.Helme S, Samdani T, Sinha P. Complications of spilled gallstones following laparoscopic cholecystectomy: a case report and literature overview. J Med Case Rep. 2009;24(3):8626. doi: 10.4076/1752-1947-3-8626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morishita K, Otomo Y, Sasaki H, Yamashiro T, Okubo K. Multiple abdominal granuloma caused by spilled gallstones with imaging findings that mimic malignancy. Am J Surg. 2010;199(2):e23–e24. doi: 10.1016/j.amjsurg.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 59.Dasari BV, Loan W, Carey DP. Spilled gallstones mimicking peritoneal metastases. JSLS. 2009;13(1):73–76. [PMC free article] [PubMed] [Google Scholar]
- 60.Maempel J, Darmanin G, Paice A, Uzkalnis A. An unusual "hernia": losing a stone is not always a good thing! BMJ Case Rep. 2009 doi: 10.1136/bcr.12.2008.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hougård K, Bergenfeldt M. Abdominalfistel syv år efter kolecystektomi [Abdominal fistula 7 years after laparoscopic cholecystectomy] Ugeskr Laeger. 2008;170(36):2803. [PubMed] [Google Scholar]
- 62.Arishi AR, Rabie ME, Khan MS, Sumaili H, Shaabi H, Michael NT, Shekhawat BS. Spilled gallstones: the source of an enigma. JSLS. 2008;12(3):321–325. [PMC free article] [PubMed] [Google Scholar]
- 63.de Hingh IH, Gouma DJ. Diagnose in beeld (345). Een vrouw met buikpijn en vaginaal pusverlies [Diagnostic image (345). A woman with abdominal pain and purulent vaginal discharge] Ned Tijdschr Geneeskd. 2007;151(41):2271. [PubMed] [Google Scholar]
- 64.Stupak D, Cohen S, Kasmin F, Lee Y, Siegel JH. Intra-abdominal actinomycosis 11 years after spilled gallstones at the time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2007;17(6):542–544. doi: 10.1097/SLE.0b013e3181469069. [DOI] [PubMed] [Google Scholar]
- 65.Pantanowitz L, Prefontaine M, Hunt JP. Cholelithiasis of the ovary after laparoscopic cholecystectomy: a case report. J Reprod Med. 2007;52(10):968–970. [PubMed] [Google Scholar]
- 66.Wehbe E, Voboril RJ, Brumfield EJ. A spilled gallstone. Med J Aust. 2007;187(7):397. doi: 10.5694/j.1326-5377.2007.tb01310.x. [DOI] [PubMed] [Google Scholar]
- 67.Wittich AC. Spilt gallstones removed after one year through a colpotomy incision: report of a case. Int Surg. 2007;92(1):17–19. [PubMed] [Google Scholar]
- 68.Bhati CS, Tamijmarane A, Bramhall SR. A tale of three spilled gall stones: one liver mass and two abscesses. Dig Surg. 2006;23(3):198–200. doi: 10.1159/000094739. [DOI] [PubMed] [Google Scholar]
- 69.Ianniti DA, Zaydfudim VK, McKee J. Subphrenic and pleural abscess due to spilled gallstones. JSLS. 2006;10:101–104. [PMC free article] [PubMed] [Google Scholar]
- 70.Hand AA, Self ML, Dunn E. Abdominal wall abscess formation two years after laparoscopic cholecystectomy. JSLS. 2006;10(1):105–107. [PMC free article] [PubMed] [Google Scholar]
- 71.Viera FT, Armellini E, Rosa L, Ravetta V, Alessiani M, Dionigi P, Rossi S. Abdominal spilled stones: ultrasound findings. Abdom Imaging. 2006;31(5):564–567. doi: 10.1007/s00261-005-0241-8. [DOI] [PubMed] [Google Scholar]
- 72.AlSamkari R, Hassan M. Middle colic artery thrombosis as a result of retained intraperitoneal gallstone after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2004;14(2):85–86. doi: 10.1097/00129689-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 73.Koç E, Suher M, Oztuğut SU, Ensari C, Karakurt M, Ozlem N. Retroperitoneal abscess as a late complication following laparoscopic cholecystectomy. Med Sci Monit. 2004;10(6):CS27. [PubMed] [Google Scholar]
- 74.Stevens S, Rivas H, Cacchione RN, O'Rourke NA, Allen JW. Jaundice due to extrabiliary gallstones. JSLS. 2003;7(3):277–279. [PMC free article] [PubMed] [Google Scholar]
- 75.Aspelund G, Halldórsdóttir BA, Isaksson HJ, Möller PH. Gallstone in a hernia sac. Surg Endosc. 2003;17(4):657. doi: 10.1007/s00464-002-4257-7. [DOI] [PubMed] [Google Scholar]
- 76.Papasavas PK, Caushaj PF, Gagné DJ. Spilled gallstones after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2002;12(5):383–386. doi: 10.1089/109264202320884144. [DOI] [PubMed] [Google Scholar]
- 77.Yadav RK, Yadav VS, Garg P, Yadav SP, Goel V. Gallstone expectoration following laparoscopic cholecystectomy. Indian J Chest Dis Allied Sci. 2002;44(2):133–135. [PubMed] [Google Scholar]
- 78.Van Mierlo PJ, De Boer SY, Van Dissel JT, Arend SM. Recurrent staphylococcal bacteraemia and subhepatic abscess associated with gallstones spilled during laparoscopic cholecystectomy two years earlier. Neth J Med. 2002;60(4):177–180. [PubMed] [Google Scholar]
- 79.Hawasli A, Schroder D, Rizzo J, Thusay M, Takach TJ, Thao U, Goncharova I. Remote complications of spilled gallstones during laparoscopic cholecystectomy: causes, prevention, and management. J Laparoendosc Adv Surg Tech A. 2002;12(2):123–128. doi: 10.1089/10926420252939664. [DOI] [PubMed] [Google Scholar]
- 80.Famulari C, Pirrone G, Macrì A, Crescenti F, Scuderi G, De Caridi G, Giuseppe AL. The vesical granuloma: rare and late complication of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11(6):368–371. doi: 10.1097/00129689-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 81.Werber YB, Wright CD. Massive hemoptysis from a lung abscess due to retained gallstones. Ann Thorac Surg. 2001;72(1):278–279. doi: 10.1016/S0003-4975(00)02563-7. [DOI] [PubMed] [Google Scholar]
- 82.Yao CC, Wong HH, Yang CC, Lin CS. Abdominal wall abscess secondary to spilled gallstones: late complication of laparoscopic cholecystectomy and preventive measures. J Laparoendosc Adv Surg Tech A. 2001;11(1):47–51. doi: 10.1089/10926420150502959. [DOI] [PubMed] [Google Scholar]
- 83.Battaglia DM, Fornasier VL, Mamazza J. Gallstone in abdominal wall–a complication of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11(1):50–52. doi: 10.1097/00129689-200102000-00014. [DOI] [PubMed] [Google Scholar]
- 84.Ok E, Sözüer E. Intra-abdominal gallstone spillage detected during umbilical trocar site hernia repair after laparoscopic cholecystectomy: report of a case. Surg Today. 2000;30(11):1046–1048. doi: 10.1007/s005950070032. [DOI] [PubMed] [Google Scholar]
- 85.Bebawi M, Wassef S, Ramcharan A, Bapat K. Incarcerated indirect inguinal hernia: a complication of spilled gallstones. JSLS. 2000;4(3):267–269. [PMC free article] [PubMed] [Google Scholar]
- 86.Jacob H, Rubin KP, Cohen MC, Kahn IJ, Kan P. Gallstones in a retroperitoneal abscess: a late complication of perforation of the gallbladder. Dig Dis Sci. 1979;24:964–966. doi: 10.1007/BF01311955. [DOI] [PubMed] [Google Scholar]
- 87.Rothlin MA, et al. Stones spilled during cholecystectomy. A long-term liability for the patient. Surg Laparosc Endosc. 1997;7:432–434. doi: 10.1097/00019509-199710000-00016. [DOI] [PubMed] [Google Scholar]
- 88.Tsui C, Klein R, Garabrant M. Minimal Invasive surgery: national trends in adoption and future directions for hospital strategy. Surg Endosc. 2013;27:2253–2257. doi: 10.1007/s00464-013-2973-9. [DOI] [PubMed] [Google Scholar]
- 89.Shea JA, Berlin JA, Bachwich DR, Staroscik RN, Malet PF, McGuckin M, et al. Indications and outcomes of cholecystectomy: a comparison of the pre and postlaparoscopic eras. Ann Surg. 1998;227:343–350. doi: 10.1097/00000658-199803000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Khan MH, Howard TJ, Fogel EL, Sherman S, McHernyn L, Watkins JL, et al. Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: experience at a large tertiary center. Gastrointest Endosc. 2007;65:247–252. doi: 10.1016/j.gie.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 91.Johanning JM, Gruenberg JC. The changing face of cholecystectomy. Am Surg. 1998;64:643–647. [PubMed] [Google Scholar]
- 92.Ingraham AM, Cohen ME, Ko CY, Hall BL. A current profile and assessment of north American cholecystectomy: results from the American college of surgeons national surgical quality improvement program. J Am Coll Surg. 2010;211:176–186. doi: 10.1016/j.jamcollsurg.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 93.Giger UF, Michel JM, Opitz I, Inderbitzin D, Kocher T, Krähenbühl L. Swiss Association of Laparoscopic and Thoracoscopic Surgery (SALTS) study: Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22953 consecutive cases from Swiss Association of Laparoscopic and Thoracoscopic surgery databases. J Am Coll Surg. 2006;203:723–728. doi: 10.1016/j.jamcollsurg.2006.07.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors declare that data supporting the findings of this study are available within the article.