Abstract
Purpose:
The purpose of this study is to characterize the communication needs of older adults in group care environments and understand the factors that foster engaged communication.
Method:
This mixed methods study provides an in-depth analysis of communication and engagement for older adults at two Program for All-inclusive Care for the Elderly (PACE) sites. Seventy-two PACE participants (Mage = 74 years) completed a hearing test, cognitive screener (MOST™), the Institute of Medicine (IOM) Measures of Social and Behavioral Determinants of Health Questionnaire, and the UCLA Loneliness Scale. Using maximum variation sampling based on hearing status and UCLA Loneliness scores, 19 participants were invited to do (and 11 participants completed) one-on-one semi-structured interviews. In addition, 35 staff members participated in 5 focus groups. Field observations were interspersed throughout the data collection period.
Results:
Results suggest that communication challenges such as hearing loss, cognitive decline, and social isolation are highly prevalent in this convenience sample. Sixty-seven percent have at least a mild hearing loss in the better hearing ear. Eighty-two percent scored in the “very” or “most isolated” range of the IOM Measures of Social and Behavioral Determinants of Health questionnaire. The mean score on the MOST™ cognitive screener was 17.6, which is below the dementia screening cutoff score of 18 points. A thematic analysis of the qualitative data suggests that the PACE programs support socialization and engagement. A conceptual framework was developed by integrating quantitative and qualitative findings to recognize what contributes to meaningful interactions or engaged communication.
Conclusion:
Identifying communication challenges can enhance the benefits individuals can experience at care facilities and lessen the burden of the staff members trying to provide safe and effective care. In order to maximize the potential benefit of attending group-based day centers, the communication challenges and motivations of older adults need to be addressed.
Keywords: Aging, Hearing loss, Aural rehabilitation
Introduction
Age-related hearing loss is highly prevalent and almost always untreated (Chien & Lin, 2012; Lin, Niparko, et al., 2011; NASEM, 2016). In the past decade, many epidemiological studies have suggested that age-related hearing loss is associated with a host of poor aging outcomes—increased rates of cognitive decline, increased incidence of dementia, increased falls, increased rates of depression, and increased social isolation and loneliness (Gopinath et al., 2016; Lawrence et al., 2020; Lin, Metter, et al., 2011; Lin et al., 2013; Loughrey et al., 2018; Mick et al., 2014; Mick et al., 2018; Viljanen et al., 2009). While these studies establish associations, the underlying mechanisms of the relationships are unknown. Classic frameworks to explain these associations include the common cause hypothesis, the sensory deprivation hypothesis, and the information degradation hypothesis (Baltes & Lindenberger, 1997; CHABA, 1988; Wayne & Johnsrude, 2015). Baltes and Lindenberger (1997) favored the common cause hypothesis that age-related changes in brain structure and function are responsible for both the sensory and cognitive declines (Anderson & Craik, 2017). That said, the cascade hypotheses (i.e., sensory deprivation and information degradation) are more the focus of the recent research on the impact of age-related hearing loss. A meta-analysis by Louhrey and colleagues (2018) argued that the temporal pattern of findings in prospective studies is consistent with a causal relationship between age-related hearing loss and cognitive decline; whilst emphasizing the need for randomized control trials to confirm this relationship. If the hearing loss is indeed causing downstream mental and physical health effects, then treating hearing loss might mitigate those poor health outcomes (Jayakody et al., 2018; Uchida et al., 2019).
Lin and Albert (2014) proposed three potential mechanistic pathways that might result in age-related hearing loss being responsible for negative mental and physical health outcomes: increased cognitive load, changes in brain volume and structure, and increased social isolation. In this cascade hypothesis, the hearing loss causes the increased cognitive load, the changes to brain structure and function, and increased social isolation, leading to accelerated cognitive declines and a feedback loop of increased decline (Lin & Albert, 2014; Uchida et al., 2019). The current study focuses on the important relationship between age-related hearing loss and social isolation, and the downstream impact of those issues on mental and physical health.
Social isolation and loneliness, while different constructs, are often mentioned hand-in-hand and have been associated with hearing loss in older adults. Social isolation refers to the objective number of persons in one’s social network and loneliness refers to the subjective percept of social isolation (Wenger et al., 1996). A recent systematic review highlighted 14 manuscripts addressing the association between social isolation and/or loneliness in adults with hearing loss (Shukla et al., 2020). The studies reviewed ranged from small, clinic- or community-based samples to population-based surveys. Social isolation was a more consistent association, which may be attributed to reduced activity participation due to hearing loss. On the other hand, reduced activity participation does not necessarily create the emotional percept of loneliness because a person may be able to maintain close relationships despite the hearing loss. While the association with reported loneliness was less consistent, it was still significant in 7 of 11 reviewed manuscripts that measured hearing loss and loneliness.
The emotional percept of loneliness may be a difficult outcome target when treating hearing loss, however, reduced social isolation may be an attainable goal. Activity participation and engagement, which are key to healthy aging (Lu et al., 2019), can be difficult to maintain for all older adults, especially those with functional impairments, such as, untreated hearing loss (Mick et al., 2018). Rather than assuming increased activity participation will be a byproduct of treating hearing loss, perhaps it could be an intentional target that clinicians work to support in an interdisciplinary team approach to person-centered care for older adults. This could be achieved through integrated care teams or provider-community partnerships that incorporate hearing and communication supports (and other sensory impairment treatments) into the broader system of care accessed by older adults.
One such integrated care opportunity could be enhanced communication at Adult Day Centers. The models of care that offer day centers for older adults vary widely, but in general, they all offer the opportunity to have programmed activities and socialization for older adults living in the community. There are notable benefits to older adults and family caregivers, and health care system burden is reduced when Adult Day Centers provide safe and engaging care solutions (Gaugler et al., 2021; Orellana et al., 2020; Schmitt et al., 2010; Zarit et al., 1998). Nevertheless, there remains a substantial problem of under-identified and undertreated hearing loss in these care environments, which may limit the benefits an individual can experience in such a group care setting (Mamo et al., 2019; Mamo & Wheeler, 2021). Since these services go to great lengths to provide activity participation and social engagement opportunities for older adults in order to help people age more safely at home for longer, it is important to optimize the environment and provide communication supports to achieve these goals.
The mixed methods case study presented here provides an in-depth exploration of a unique model of comprehensive and integrated care for older adults, the Program for All-Inclusive Care for the Elderly (PACE), with a focus on the Day Health Center that supports activity participation and social engagement. A mixed methods case study differs from a clinical practice case study in that the “case” can be defined more broadly, including individuals, sites, events, or policies (Crowe et al., 2011). In order to explore hearing and communication in a group care environment for older adults, a mixed methods case study design was undertaken, with the PACE organization as the “case”. A convergent mixed methods model of quantitative and qualitative data allows for contextualizing how the organization contributes to social engagement for the older adults who attend PACE.
The PACE program focuses on holistic, comprehensive care for older adults that includes addressing physical, social, mental, and spiritual health (Mui, 2001). The program is built on a mission to help adults age safely in place. There is a shared mission, eligibility, and core structure across the 141 programs in the United States. Participants in the PACE program must be 55 years or older, deemed nursing home eligible by the state, and live within the service area of a given program (NPA, 2021). The program itself is a Medicare/Medicaid beneficiary program that operates as a capitated health system for all of its enrollees (Wieland et al., 2013). Primary care and rehabilitation services are available at the Day Health Center (DHC). Specialty services are coordinated by the PACE organization. In addition, transportation to the DHC and all other appointments is facilitated by PACE. Finally, enrollees attend the DHC for meals, activities, exercise, and social engagement 1–5 days per week depending on their Individual Care Plan.
In addition to the comprehensiveness of the services provided or coordinated by PACE, all care planning is performed via an interdisciplinary team that extends beyond the medical staff to the rehabilitation providers, the medical technicians, the recreation team, the social workers, the home health team, and the transportation team (Mukamel et al., 2007; Mukamel et al., 2006). The mission and organization of PACE emphasizes the value of each team member’s contributions. PACE provides an exemplary holistic model and approach to providing care to older individuals which makes their facilities unique and worthy of discussion.
The following mixed methods case study explores communication and engagement for older adults in an exemplary comprehensive care program. Our approach has employed a range of methods and measures to afford an in-depth analysis of the PACE program through combining data from two organizations. The purpose of this study is to characterize the communication needs of older adults in group care environments and understand the factors that foster engaged communication. This mixed methods case study describes the characteristics of PACE and examines the factors that contribute to social engagement among PACE participants. The lessons learned through this in-depth analysis will provide transferable knowledge to enhance communication and engagement at other group care settings for older adults.
As an audiology research team, we have approached this exploration through the lens of hearing loss and its effect on communication and wellbeing. We developed our research plan by posing a series of research questions about what creates an environment that fosters meaningful interactions. We argue that the goal of treating hearing loss should not simply be to restore the ‘ability to hear’, but to provide the necessary tools to have meaningful exchanges. This mixed methods case study examines the following research questions:
What do older adults value in terms of social interactions or conversations?
What can be learned at PACE about fostering activity/communication/engagement?
What can the field learn about supporting communication in a group care setting?
Methods
A mixed methods case study provides an in-depth description of a real-life complex situation through a mix of quantitative and qualitative data and an integrated analysis approach (Creswell & Plano Clark, 2018; Crowe et al., 2011). The current case is a study of PACE through a series exploration of two organizations. The two organizations are unique, and yet, they share characteristics with PACE programs nationwide. Specifically, all PACE programs share a mission and enrollment criteria, use an interdisciplinary team care approach, and center their services around the DHC.
Setting
The first PACE organization in our study (PACE-1) is affiliated with a large medical/hospital organization and is located in a relatively rural region of New England. The average daily attendance at PACE-1 is 95 persons at the DHC. Throughout the research process, many PACE staff have facilitated the collaboration, and we have worked directly with the Executive Director, Quality Improvement Analyst, Director of Operations, Life Enrichment Coordinator, and the Office Manager/Receptionist.
The second PACE organization in our study (PACE-2) operates three separate facilities across their state. The current study investigation took place at two of the three sites. The PACE-2 site has an average daily attendance of 99 individuals total at the DHCs across all three sites. The two participating sites represent a large city setting and a small city setting. In general, the demographics of any given PACE site reflect the demographics of that service area because living within the limits of the service area is an eligibility criterion. The inclusion of PACE-2 results in a more racially, ethnically, and linguistically diverse population than the PACE-1 site in rural New England. Throughout the research process, many PACE-2 staff have facilitated this collaboration, and we have worked directly with the Chief of Clinical Services, the Education and Research Associate, and the Nurse Manager.
Recruitment and Consent
The process of partnering with the PACE organizations began with the primary investigator (SKM) directly contacting the executive directors. Contact was first made with PACE-1 in early 2017, and contact with PACE-2 began in early 2019. After gaining the support of the leadership, the PI presented information about age-related hearing loss and the plans for the research study to the full staff. Each site designated a point person to help with the logistics of the study (e.g., reserving rooms for testing) and recruitment of PACE participants and staff for study activities. The institutional review boards of the University of Massachusetts Amherst and Trinity Health of New England approved this study.
All PACE participants who participated in this study completed a capacity assessment by the researcher after reviewing the consent form with the participant.1 The capacity assessment asked questions that assessed the person’s ability to understand that they have the choice to participate or not, their ability to understand the situation and relevant information about what they would do while participating in the study, and their ability to manipulate information rationally (Wendler, 2004). Of the 45 PACE-1 participants who volunteered to participate, 4 were deemed ineligible due to lack of capacity to consent; and of the 60 potential participants at PACE-2, 3 participants were determined ineligible per the capacity assessment.2 The emphasis of the capacity assessment was on the person’s ability to state that they did not have to do anything they did not want to do and did not have to answer any questions they did not want to answer; state that they could stop participating at any time; and respond appropriately to the question: “If I ask you a question that you do not want to answer, what should you do?”
PACE Participants
All PACE programs share eligibility criteria for enrollment as described in the introduction. The variation of the demographic characteristics of enrollees in each program relates to the demographics of each given service area. In the two organizations presented in the current case study of PACE, we observe a primarily White participant population for the PACE-1 site (92%) and a 50% non-White population sample for the PACE-2 site, wherein most of the participants are from a large metro/city area (Table 1). Correspondingly, the US Census Bureau reports that the population of the city where PACE-1 is situated is 80% non-Hispanic White and the population of the city where PACE-2 is situated is 33% non-Hispanic White.
Table 1.
Demographic characteristics of a convenience sample of PACE participants (N = 72)
| Total N = 72 M (SD) |
PACE-1 n = 36 M (SD) |
PACE-2 n = 36 M (SD) |
|
|---|---|---|---|
| Age, years | 74.2 (8.2) | 75.0 (9.1) | 73.3 (7.3) |
| Better Ear PTA (dB HL) | 34.7 (14.0) | 34.5 (12.6) | 35.0 (15.3) |
| HHIE-S | 11.1 (11.0) | 11.5 (11.3) | 10.7 (10.9) |
| Loneliness Score | 42.5 (12.7) | 42.2 (12.7) | 42.9 (12.9) |
| Cognitive Score | 17.6 (5.0) | 18.7 (4.2) | 16.6 (5.5) |
| N (%) | N (%) | N (%) | |
| Race ** | |||
| White | 51 (71) | 33 (92) | 18 (50) |
| Black/AA | 6 (8) | 1 (3) | 5 (14) |
| Latinx | 11 (15) | 2 (6) | 9 (25) |
| Other | 4 (6) | 4 (11) | |
| Gender (No. female) | 41 (57) | 22 (61) | 19 (53) |
| Education * | |||
| Less than HS | 27 (38) | 7 (19) | 20 (56) |
| HS/GED | 25 (35) | 17 (47) | 8 (22) |
| More than HS | 14 (19) | 9 (25) | 5 (14) |
| Other | 6 (8) | 3 (8) | 3 (8) |
|
Hearing Status No loss Mild loss Moderate/severe loss |
24 (33) 25 (35) 23 (32) |
11 (31) 13 (36) 12 (33) |
14 (39) 11 (31) 11 (31) |
| HA Use | |||
| Yes | 7 (10) | 6 (17) | 1 (3) |
| Previous | 4 (6) | 2 (6) | 2 (6) |
| No | 58 (84) | 28 (78) | 30 (91) |
| Smoker | |||
| Never | 29 (40) | 15 (42) | 14 (39) |
| Former | 31 (43) | 18 (50) | 13 (36) |
| Current | 12 (17) | 3 (8) | 9 (25) |
|
Alcohol Usea Yes No |
7 (10) 64 (90) |
2 (6) 34 (94) |
5 (14) 30 (86) |
|
Depressionb Yes No |
25 (36) 45 (64) |
13 (37) 22 (63) |
12 (34) 23 (66) |
|
Physical Activityc Inactive Insufficiently active Sufficiently active |
11 (16) 34 (51) 22 (33) |
3 (9) 20 (59) 11 (32) |
8 (24) 14 (42) 11 (33) |
|
Financial Strain Not hard at all Somewhat hard Very hard Other |
36 (50) 23 (32) 12 (17) 1 (1) |
17 (47) 11 (31) 7 (19) 1 (3) |
19 (53) 12 (33) 5 (14) |
|
Stress Not at all A little bit Somewhat Quite a bit Very much |
22 (31) 13 (18) 14 (19) 17 (24) 6 (8) |
10 (28) 8 (22) 8 (22) 6 (17) 4 (11) |
12 (33) 5 (14) 6 (17) 11 (31) 2 (6) |
|
Social Isolation Not isolated Somewhat isolated Very isolated Most isolated |
1 (1) 12 (17) 26 (36) 33 (46) |
6 (17) 15 (42) 15 (42) |
1 (3) 6 (17) 11 (31) 18 (50) |
Note. Loneliness Score was calculated from the UCLA Loneliness Scale – Version 3; Scores range from 20–80 with higher scores indicating more loneliness. Cognitive Score was calculated from the Memory Orientation Screening Test (MOST); Scores less than 18 suggest a diagnosis of dementia. Hearing loss defined as: no loss (≤ 25 dB HL), mild loss (≥ 26–40 dB HL), and moderate/severe loss (> 40 dB HL). Not all percentages add to 100% due to rounding. PACE = Program for All-inclusive Care for the Elderly; PTA = pure-tone average; HHIE-S = Hearing Handicap Inventory for Elderly—Screening; AA = African American; HS = high school; GED = general educational development; HA = hearing aid
Missing data for alcohol use (n = 1) due to unreliable responses on the 3 questions related to alcohol use.
Missing data for depression (n = 2) because the persons opted not to answer one of the two screening questions.
Missing data for exercise (n = 5) due to lack of time estimates for their typical exercise activities.
p < .05;
p < .01
On average, the PACE participants (n = 72) were 74.2 years-old and had a mild hearing loss (Better ear PTA = 34.7 dB HL). The sample had a generally low education level with over 70% of the sample having a high school degree or less. Further description of the demographic characteristics in Table 1 are found in the Results section.
PACE Staff
Basic characteristics of the staff at both of our PACE organizations can be seen in Table 2. A notable characteristic of the PACE staff is the low turnover rate. A majority of the staff members that participated in the research study reported working with PACE for more than one year and nearly a third of those reported having worked at PACE for more than five years.
Table 2.
PACE staff demographics at both sites (N=35)
| PACE-1 (n=18) | PACE-2 (n=17) | |
|---|---|---|
| n (%) | n (%) | |
|
Race White Black/AA Latinx Other |
12 (66) 3 (22) 3 (22) |
8 (47) 1 (6) 7 (41) 1 (6) |
|
Job Title/Role Nurse Social Worker Transportation Day Center Worker Recreation team Dietician Occupational Therapy Team (OTA/OT) Administrative role |
3 2 3 3 5 1 1 |
1 2 8 1 1 2 2 |
|
Job Duration < 1 year 1–5 years > 5 years Unknown |
7 (39) 8 (44) 3 (17) |
3 (18) 8 (47) 5 (29) 1 (6) |
Note. This data only reflects PACE staff members who attended the focus groups.
Research Team
The primary investigator and lead author of this mixed methods case study is an audiology professor whose research focuses on access to hearing loss treatment for older adults. Three audiology graduate students conducted and analyzed the interviews undertaken with the PACE participants and staff focus groups. Two undergraduate communication disorders students also participated in the collection of questionnaires, hearing tests, and field observations. As a research team, we discussed all transcripts together and developed our coding and analysis process iteratively with all research team members contributing to the discussion. The third (VLPC) and fourth (CSJ) authors provided research design support as well as ongoing methodological and content feedback throughout the data gathering and analyses.
Data Collection
Consistent with mixed methods case study procedures, the research team gathered multiple quantitative and qualitative data forms to capture the complexity of the case (Creswell & Plano Clark, 2018). The data presented in this manuscript reflects a subset of participants from a larger, on-going study with three PACE organizations. In the full study, hearing tests were administered with 160 participants (Mamo & Wheeler, 2021). The current manuscript includes data from 72 participants from two PACE organizations (n = 36 at each site) who, in addition to hearing testing, opted-in to participate in a set of questionnaires related to social determinants of health.3 A purposefully selected subset of this group (n = 11) participated in one-on-one semi-structured interviews to learn more about the daily activities of PACE enrollees. The process of data collection at each organization began with the quantitative data collection, included periodic field observations throughout, and concluded with staff focus groups and individual PACE participant interviews. At PACE-1, data was collected between February 2019 and December 2019, and at PACE-2 data was collected between September 2019 and January 2021 (with a hiatus due to COVID-19 restrictions).
Quantitative Data
Hearing Tests
Hearing tests were collected from all participants (n = 72) in the form of objective tonal responses as well as a subjective self-perceived hearing handicap questionnaire. Otoscopy was performed prior to testing as part of routine clinical care and participants were not turned away if cerumen impaction was observed. Participants were asked general hearing health-related questions regarding their hearing history and hearing aid use. Hearing testing was administered by a member of the research team using a modified automated protocol on SHOEBOX audiometers (SHOEBOX Ltd, Ottawa, ON) with RadioEar DD450 circumaural headphones (RadioEar, Denmark). SHOEBOX is a clinically validated audiometric tool for behavioral hearing threshold measurement (Thompson et al., 2015). The automated protocol is equipped with a response algorithm that notifies the tester if responses are inconsistent. Air conduction thresholds were measured at octave frequencies from 0.5–8 kHz via behavioral responses such as hand raises or verbal responses. A 4-frequency pure tone average (PTA) was calculated for each participant using the audiometric responses at 500, 1000, 2000, and 4000 Hz. Hearing loss was categorized based on the PTA of the better hearing ear. The categories of hearing loss include no loss (≤ 25 dB HL), mild loss (26–40 dB HL), and moderate/severe loss (> 40 dB HL).
Participants completed the Hearing Handicap Inventory for Elderly-Screening (HHIE-S) subjective hearing questionnaire as part of the hearing test protocol (Ventry & Weinstein, 1983).4 The HHIE-S is used to identify the perceived impact hearing loss has on an individual’s life. The HHIE-S has a high degree of reliability Pearson r = .84 (p < .0001) and a sensitivity of 72% and a specificity of 77% in a validation study of hearing-impaired older adults in a primary care setting (Lichtenstein et al., 1988). The HHIE-S is comprised of 10 questions and participants must answer yes, sometimes, or no. Each response is assigned a point value (yes = 4, sometimes = 2, no = 0); total scores range from 0–40 with a higher score indicating a higher perceived hearing handicap. A HHIE-S score between 10–24 suggests a mild-moderate perceived hearing handicap and a score of 26 or more suggests a significant hearing handicap (Lichtenstein et al., 1988).
Social and Functional Health Questionnaires
All participants (n = 72) completed questionnaires administered by a research assistant. The questionnaires were read aloud to the participant and a physical copy of the respective questionnaire was presented in size 70 font. The UCLA Loneliness Scale (Version 3)(Russell, 1996) and the Institute of Medicine (IOM) Measures of Social and Behavioral Determinants of Health (Committee on the Recommended Social Behavioral Domains Measures for Electronic Health Records Board on Population Health Public Health Practice, 2015) were completed.
The UCLA Loneliness Scale (Version 3) was used to measure the participant’s subjective feelings of loneliness and social isolation (Russell, 1996). The UCLA Loneliness Scale was developed by Russell et al. (1978) to determine the social psychological factors of loneliness. In a validation study of an older adult population that live alone, the UCLA Loneliness Scale had a Cronbach alpha of 0.95 (Velarde-Mayol et al., 2016), which suggests that the test has good internal consistency (Tavakol & Dennick, 2011). The questionnaire is comprised of 20 questions and participants are asked to indicate how often a statement is descriptive of them by responding: never, rarely, sometimes, or often. Point values were assigned to each response, and higher scores are indicative of loneliness. In a validation study of 61 older adults (age range 60–88 years), a score of 47 was one standard deviation above the mean and indicative of loneliness in older adult populations (Cutrona et al., 1986).
The IOM Measures of Social and Behavioral Determinants (SBD) of Health was used to assess the social and behavioral determinants of health (Committee on the Recommended Social Behavioral Domains Measures for Electronic Health Records Board on Population Health Public Health Practice, 2015). The IOM Measures of SBDs of Health was developed by the Commission on Social Determinants of Health to better understand how social and behavioral determinants affect health outcomes. It is a validated measure of SBDs that is comprised of 25 questions that cover a range of topics (Giuse et al., 2017). For the purpose of this study, our questionnaire included 21 questions in the domains of race/ethnicity, education, financial resource strain, stress, depression, physical activity, tobacco use, alcohol use, and social connection or isolation. The domain of intimate partner violence was excluded.
Some of the domains in the IOM Measures of SBDs generate a score from responses to multiple questions.5 The domain of depression is based on two questions regarding the past two weeks and whether or not the participant had felt bothered by little interest or pleasure in doing activities and whether or not the participant had been bothered by feelings of depression or hopelessness. Depression screener scores were calculated by summing the answers to these two questions to give a Patient Health Questionnaire (PHQ)-2 summary score (not at all = 0, several days = 1, more than half the days = 2, nearly every day = 3). A PHQ-2 score ≥ 3 suggests a positive screen for depression (Kroenke et al., 2003).
The domain of social connection or isolation was based on the answer to five questions regarding how often a participant talks on the phone with friends or family, gets together with friends or family, attends church or religious services, attends meetings of clubs or organizations, and on the basis of their marital/domestic partnership status (Pantell et al., 2013). Participants receive one point for averaging 3 or more social interactions a week based on the responses to the first two questions, one point for attending church more than 4 times per year, one point for attending meetings, and one point for being married or living in a marital-like relationship. Social isolation screener scores were categorized as most isolated (0–1 point), very isolated (2 points), somewhat isolated (3 points), and not isolated (4 points).
Cognitive Screening
The Memory Orientation Screening Test (MOST)(Clionsky & Clionsky, 2010), a general cognitive screener, was included in the questionnaire test battery. The MOST is similar to the Mini Mental State Examination (MMSE) that is used to detect the presence and severity of dementia (Folstein et al., 1975). The potential scores of the MOST range from 0–29 with higher scores indicative of higher cognitive function and a cutoff score of 18 for dementia screening (Clionsky & Clionsky, 2010). The MOST has excellent test-retest reliability Pearson r = .91 (p < .001) and in a validation study, the MOST screener has a sensitivity of 0.85 and a specificity of 0.76 for detection of dementia (Clionsky & Clionsky, 2010). The MOST includes 4 domains necessary for a cognitive test battery: memory, orientation, sequence memory, and time. The MOST was administered on an iPad by a member of the research team (Clionsky & Clionsky, 2014).
Qualitative Data
Interviews
Individual PACE participants were invited for one-on-one semi-structured interviews using maximum variation sampling based on high/low combinations of their hearing thresholds and their UCLA Loneliness scores (Palinkas et al., 2015). We wanted to explore the perceptions of individuals who did and did not follow that pattern of association between age-related hearing loss and loneliness presented in the literature. We provided our staff contact at each PACE site with a short-list of PACE participants who met our sampling criteria for interviews. Because these participants had already taken part in the first phase of the study, they were familiar with the research team, and the PACE staff member approached them directly to ask if they were interested in a one-on-one interview. At PACE-1, the offer for interviews was extended to 10 potential participants and 5 accepted and participated. At PACE-2, the opportunity for one-on-one interviews was interrupted by COVID-19; when our research study resumed, we invited 9 potential participants to interview via video-conference and 6 accepted and participated.6 An hour was allotted for each interview, and the duration of the interviews ranged from approximately 30–60 minutes.
The interview guide was designed to cover topics about their daily activities, routines, and preferences with a particular emphasis on their time spent at the DHC at their PACE site. It is worth noting that the PACE-2 interviewees were not attending the DHC at the time of their interviews due to the COVID-19 pandemic. Nevertheless, the general tone of their interviews with regard to what they value about engagement with the PACE program, while potentially nostalgic at times because of the pandemic isolation, echoed similar sentiments as the interviews that occurred in-person before the pandemic. Interviewees were also asked about their perception of hearing loss: both their own hearing and the other people with whom they interacted at PACE. In order to help the interviewee talk about social interactions and engagement, the interview guide interspersed simple, direct questions, such as “Do you sit at the same table for lunch most days? How many people sit at that table with you?”, with more abstract questions, such as, “What makes a good conversation?”. The semi-structured interview approach also afforded the opportunity for the person to go on tangents related to what was important to them.
Focus Groups
We moderated 3 focus groups at the PACE-1 site and 2 focus groups at the PACE-2 site that included a total of 35 staff members. The recruitment effort for the focus groups included flyers in the staff break rooms and an email sent to all staff from an administrative employee at the PACE sites. We invited all staff who interacted with PACE participants routinely. Multiple sessions were conducted at each site to allow for some employees to continue delivering services while others spent 1-hour participating in the focus group with the research team. The resulting sample included DHC care aides, nursing staff, rehabilitation therapists, recreation/life enrichment team members, transportation, and a few other specialties (Table 2). The focus group guide aimed to solicit conversation about communication breakdowns and solutions, overlap of hearing loss and cognitive impairment, and willingness and interest in various communication training topics.
Field observations
Four members of the research team spent time collecting field observations in the activity rooms at the PACE sites. For each site, we used a map template of the room to identify where interactions and sources of noise were located. These sessions tended to occur whenever there were downtimes in the quantitative data collection efforts. This amounted to 15 independent observation sessions lasting between 30–60 minutes. The observer was instructed to focus on interactions between participants and staff as well as between participants. They were instructed to notice physical behaviors related to hearing and listening. Observers also routinely did a count of the number of people in the room and the number of conversations occurring between two or more people. Finally, observers routinely recorded an overall background noise level using an iPad-based sound level meter (Faber Acoustical, LLC). Within 24 hours of an observation session, the observer wrote a 1-page reflection based on their field notes.
Data Analysis
Quantitative Analysis
The intent of the questionnaire data was to compare scores on the basis of hearing loss. The first quantitative analysis examined the associations between the continuous variables of hearing status (better ear PTA), perceived hearing handicap (HHIE-S score), and loneliness (UCLA Loneliness score). A second quantitative analysis analyzed cross tabulations between categories of the previously mentioned measures as well as additional demographic and social health determinant categories from the IOM Measures of SBDs (including depression and social isolation.)
Qualitative Analysis
The intent of the qualitative data was to explore the communication challenges faced by PACE participants and staff as well as understand what motivated PACE participants to participate and socially engage at the DHC. Thematic analysis was based on an iterative coding process by the research team for each of the 3 qualitative data types (interview, focus group, observation). Independent codebooks were created for each of these qualitative data sets. The process began with the interview transcripts and included five members of the research team doing independent, close reading of transcripts. The initial codebook was developed as a team process of sharing the individually assigned codes line by line for the first transcript. The codebook was then iteratively refined with two members of the research team working together to define each code, provide an example of what the code does not include, and identify an exemplar quote for each code. After the codebook was finalized, the two research team members compared their independent coding process and found their inter-coder reliability to be approximately 0.7 for each of the final three interview transcripts that were coded. Given the large number of codes (~60 codes) assigned to this open-ended text data, we found this rating to reflect substantial agreement between coders (Landis & Gary, 1977; O’Connor & Joffe, 2020). Moreover, the research team included a process of discussing and resolving discrepant codes after individually coding, which increased alignment, and resulted in a single ‘master coded’ transcript for each interview. A similar process was undertaken for the focus group transcripts and the field observations. The codes and transcripts/field notes from each of the qualitative data sets were then developed into thematic tables that categorized the main themes.
Integration
Key elements of the quantitative and qualitative data were integrated in several different ways to develop an enhanced understanding of the case and responses to the research questions (Creswell & Plano Clark, 2018; Fetters et al., 2013; Plano Clark et al., 2018). Quantitative data for the interviewees was considered within the context of the themes identified during the qualitative analysis. Specifically, thematic patterns were analyzed as a function of key demographic features. For example, we examined whether individuals with hearing loss and high loneliness scores expressed less satisfaction with their social engagement in the PACE environment than other participants. As themes emerged, they were combined with the different results from the quantitative data and interpreted in the context of each of the three study research questions.
Results
Description of Participants
All quantitative results related to participant demographics and questionnaire responses are presented in Table 1. Participant age (M = 74.2, SD = 8.2) ranged from 59 to 93 years-old. Average hearing thresholds in the better hearing ear (M = 34.7 dB HL, SD = 14.0) ranged from clinically normal hearing (14 dB HL) to severe hearing loss (73 dB HL). Overall, the categories of hearing status were 33% with no loss, 35% with a mild loss and 32% with a moderate or severe degree of hearing loss based on the average PTA in the better hearing ear. Despite nearly 70% of participants with at least a mild degree of hearing loss, only 10% were current hearing aid users.7 For all the measures reported in Table 1, only race and education were significantly different between the two sites. Using a Fisher’s exact test, PACE-1 had a more White (p = .001) and more educated (p = .01) sample population.
The UCLA Loneliness Scale can have scores between 20–80, and the range in the current sample was 20–72. Responses were checked for internal consistency and had a high Cronbach alpha (0.85), suggesting reliable responses. The MOST cognitive screener data includes 68 participants (n = 33 PACE-1; n = 35 PACE-2). The missing data from the MOST cognitive screener can be attributed to scores not being saved on the iPad (n = 2) or researcher oversight (n = 2). All four participants with missing MOST data had an indication of cognitive impairment per their medical chart review at baseline. The mean MOST score at PACE-1 was 18.7 (SD = 4.2) and was 16.6 (SD = 5.5) at PACE-2. The score range for the MOST in the full sample was 5–24, with scores below 18 suggesting possible dementia. Thirty-seven percent (n = 25) of respondents on the MOST scored below the dementia-screening cut-point.
Results from the IOM Measures of SBD of Health Questionnaire provide data as to the sample characteristics in terms of smoking and alcohol use, depression screening, physical activity, financial strain, stress, and social isolation (Table 1). Of particular interest to this manuscript is that 36% of the sample screened positive for depression and 82% of the sample fell into the ‘very’ or ‘most’ isolated categories.
Analysis per Hearing Status
The quantitative data analysis focused on hearing status, loneliness/isolation, depression and cognition because of the potential impact of age-related hearing loss on these mental health metrics. Pairwise correlations of the continuous variables (better-ear PTA, UCLA Loneliness score, HHIE-S, and MOST cognitive screener score) with Sidak correction for multiple comparisons showed significant correlations between hearing threshold (better-ear PTA) and perceived hearing handicap (HHIE-S; r = .46, p < .001) as well as between loneliness (UCLA score) and cognitive screening score (r = .33, p = .04). In a linear regression analysis, with loneliness as the independent variable and hearing status as the dependent variable defined by objective (better-ear PTA) and perceived (HHIE-S) hearing loss, there was an overall main effect of hearing status (F(2,68) = 4.11, p = 0.02)(Table 3). Within the model there was no association between UCLA Loneliness Score and better-ear PTA (CI = [−0.45, 0.02]), but there was a significant relationship between UCLA Loneliness Score and perceived hearing handicap (CI = [0.12, 0.70]). As such, hearing status was represented as the HHIE-S score in the subsequent models. When cognition is added to the model (F(2,64) = 5.46, p < .01), perceived hearing handicap is no longer significant (CI = [−0.31, 0.50]) and cognitive score is significant (CI = [0.16, 1.34]). Further, adding the demographic factors of age, gender, race, and education to the model suggests that cognitive score and age contribute to the variance in the UCLA Loneliness Score (F(6,60) = 3.49, p < .01). The pattern in the full model suggests that better cognition and younger age are associated with higher loneliness scores in this sample.
Table 3.
Regression analysis of Hearing, Cognition, and Demographics on Loneliness as measured by the UCLA Loneliness Scale, n=72
| Dependent Variables | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Hearing Threshold (Better ear PTA) | −0.22 | −0.45, 0.02 | ||||
| Perceived Hearing Handicap (HHIE-S) | 0.41 | 0.12, 0.71 | 0.23 | −0.31, 0.50 | 0.24 | −0.30, 0.52 |
| Cognitive Screening Score (MOST) | 0.75 | 0.16, 1.34 | 0.79 | 0.13, 1.45 | ||
| Demographic Factors Age Gender Race Education |
−0.49 −0.44 0.76 −1.49 |
−0.89, −0.09 −6.85, 5.97 −2.57, 4.10 −3.42, 0.44 |
||||
Note. Model 1 adjusts for hearing status by including hearing thresholds as defined by a pure tone average (PTA) calculated as the average thresholds across four octave frequencies important for hearing speech (0.5–4 kHz) and perceived hearing handicap as the score on the Hearing Handicap Inventory for the Elderly – Screening (HHIE-S); both variables are entered into the model as continuous variables. Model 2 adjusts for perceived hearing status (HHIE-S) and cognition measured as the score on a brief cognitive screener (MOST) and entered as a continuous variable in the model. Model 3 adjusts for perceived hearing status, cognitive status, and demographic factors, which includes the continuous variable of age and the categorical variables of gender, race (White, Black/AA, Latinx, or Other), and education (more than high school, high school degree, less than high school, or other).
Cross tabulations using Fisher’s exact test between the categorical factors of interest (depression and social isolation) and categorical hearing loss were calculated. Only degree of social isolation and degree of hearing loss approached significance (Fisher’s exact = .09).
Thematic Results
Perspectives of PACE Participants
The semi-structured interviews focused on what types of social interactions PACE participants had at the DHC. Through an interactive process with the research team, 8 themes were agreed upon to represent 62 defined codes based upon the interviewees’ responses (Table 4). Through the exemplar quotes in Table 4, the importance of PACE as an outlet and place for social interaction emerges. The first theme of Level of Engagement represents the participant’s involvement at PACE. The ten codes that Level of Engagement embody relate to active social participation at the DHC or via videoconference socializing with other PACE participants and staff. When asked about activities and social engagement, most interviewees participated in a variety of small group activities (e.g., cards, Bingo) and most of them chatted primarily with the others at their “assigned” table. Seating is not actually assigned per se, but all of the interviewees described routines that positioned them in the same place with the same folks most of the time. Some of the tablemates and PACE acquaintances were friendly enough that they kept in touch when the DHC shut-down during the COVID-19 pandemic:
“We get [sic] along from the first day I sat down and we get along and everything else but he’s always calling me. ‘Did you take your medicine’? I said, ‘What are you a doctor?’ He says, ‘Since when did you go to doctor school. Did you take your medicine? Did you eat your breakfast?’ Get out of here. He’s just funny with me, you know, and we get along good and everything.”
Table 4.
Thematic results of semi-structured interviews with PACE participants (n = 11).
| Theme | Codes | Exemplar Codes and Quotes |
|---|---|---|
| Level of Engagement | Social Friends Conversation Tablemates Privacy Food Family GrandPad Social GrandPad Games GrandPad Use |
|
| Program Satisfaction | Content Acquaintance Enjoy Outlet Satisfied Friendly Staff Preference Solo Activity GrandPad Satisfaction |
|
| General Negative Feelings | Different Opinions Avoidance Dying Burden Abuse Resistant Anxiety Disengagement Lonely Stubborn PACE Dissatisfaction |
|
| Hearing Health | Hearing Strategy Breakdown Group Activity Tablemates Mask Communication |
|
| General Health | Personal Health Other’s Health Ability Concerned Empathy Global Health |
|
| Autobiographical | Reminisce Resignation Advice Wealth Status Dignity Money Self-Reflection |
|
| Logistics | Attendance Arrival Transport Routine Living situation Remote Contact GrandPad Technical Issues COVID Guidelines |
|
| Pandemic | Quarantine Routine Quarantine Isolation Recent Events Financial Strain |
|
Other interviewees described the people they saw at PACE as acquaintances, rather than friends: “I don’t think they’re friends, they’re just people from here and we sit together.”
The theme of Program Satisfaction represents the participant’s feelings towards the PACE program, including codes related to viewing the program as an outlet, friendly staff members, and the availability of solo and group activities. That sentiment was summed up by one interviewee with the comment, “I enjoy every bit of it, you know I just love being with people, I’m always part of something in there…”
On the other hand, the theme of General Pessimistic Feelings represents any negative feelings stated during the interviews such as feeling like a burden, disengagement, loneliness, and dissatisfaction with PACE. The theme of Hearing Health encompasses any response from the participant regarding their hearing during group activities and when communicating with their tablemates or the use of amplification devices and communication strategies. Finally, the themes of General Health, Autobiographical, Logistics, and Pandemic are included in the table in order to give a full sense of the range of discussion during the semi-structured interviews, but they will not be specifically described due to their broad, general nature.
Perspectives of PACE Staff
The aim of the focus groups was to ask the staff how PACE participants with hearing loss and/or memory problems impact their workday and whether or not they have more difficulties communicating with this group of participants than others. There were 3 agreed upon themes to represent 12 defined codes that were identified based on the staff’s responses during the focus groups (Table 5). The exemplar quotes in Table 5 reflect the active, problem-solving nature of the PACE staff. The first agreed upon theme of Staff Dedication stems from four defined codes: empathy, inclusion, willing, and training. During the focus groups, it was clear that the staff has a sincere aspiration to ease the struggle of communication with this communicatively challenging group of participants. Throughout the five focus groups, the staff’s ability to pick out individuals that were withdrawn and find ways to include them in activities was apparent in each set of transcripts. The staff members were also keen on attending various trainings regarding hearing loss and communication strategies as well as distributing amplification devices in the DHC or during medical appointments.
Table 5.
Thematic results of the focus group discussions with PACE staff (n = 5 groups; 35 staff members).
| Theme | Codes | Exemplar Codes and Quotes |
|---|---|---|
| Staff Dedication | Empathy Inclusion Willing Training |
|
| Problem Solving | Adaptive Communication Strategy Communication Breakdown Support |
|
| Amplification | Experience Problems Positives Speaker system |
|
The theme of Problem Solving encompasses the codes of adaptive, communication strategy, communication breakdown and support. The staff members recalled moments of communication breakdowns that resulted due to the participant’s hearing loss and how this breakdown affects not only the staff, but also the participant. Multiple staff members mentioned communication strategies that they utilize during their workday and strategies that they have learned to incorporate into their workday, such as slowing down their speech when speaking to participants with hearing loss and/or cognitive decline. For example, one staff member explained:
“…I try not to be in a hurry, because when you’re in a hurry, you don’t look at them. You have to make sure you’re looking at them because if you’re not, they may not hear you or get it. Sometimes I talk fast, so I have to keep in mind to always look and slow down when I talk…”
Finally, the theme of Amplification represents the four codes of experience, problems, positives, and speaker system. Staff members reflected on their experiences with amplification devices of all kinds and some of the problems that they have experienced with these devices such as inconsistencies, access to devices, cost, management, and participants’ unwillingness to use these devices.
Observations
During the field observations, the researchers had a special interest in the people participating in group activities and the people withdrawn from these activities. Thematic analysis of the field observations recorded at the DHCs is shown in Table 6. The field observations at PACE provided a better understanding of the culture at PACE and the social interactions that occur. Two members of the research team compared all observations from the DHCs and agreed upon three categories comprised of nine defined codes. The first category of Physical Environment includes the codes of background noise and room details. Broad spectrum measurements of the sound levels in the rooms varied based on activity, but during the busy period of distributing lunch the noise level was between approximately 70–75 dB A. This noise level is enough to require people to speak up to be heard during conversation. On the other hand, in a side room where a small group of participants frequenty play cards, the noise level ranged from 61–66 dB A, which is a positive use of quieter space to support small group engagement. The second category of Participant Engagement is comprised of the codes group activity, solo activity, table-talk, and withdrawn. The final category of Staff Engagement includes the codes of nature, skill, and communication strategies. These codes describe the staff members’ responses to participants, their ability to recognize environments that are not conducive to the participants’ involvement in an activity, and their ability to recognize the need to repair a communication breakdown.
Table 6.
Thematic results of the field observations in the Day Health Center (15 independent sessions).
| Theme | Codes | Exemplar Codes and Quotes |
|---|---|---|
| Physical environment | Background Noise Room Details |
|
| Participant engagement | Group Activity Solo Activity Table-talk Withdrawn |
|
| Staff engagement | Nature Skill Communication Strategies |
|
Integration
Integration is the key element of mixed methods research wherein the research team tries to uncover patterns across the different data forms and respond to the study research questions (Creswell & Plano Clark, 2018). This study used a convergent mixed methods design wherein the comparisons between the quantitative and qualitative data are considered in a bi-directional, rather than explanatory, way to develop more holistic insights about the case. In sampling for the interviews, there was an effort to speak to participants with and without high scores on the loneliness scale and with and without hearing loss. Using those different characteristics to analyze the transcripts did not reveal any clear patterns. Even participants who were rated as being lonely and positive for a depression screening expressed the benefits of attending the DHC and spoke highly of the staff.
All participants were asked during the interview, “What makes a good conversation?”, which yielded three different categories: small talk, sports, and current events/politics. There were no patterns for whom preferred which topic when considered based on demographic categories of loneliness (n = 6 with high loneliness scores), depression (n = 4 with positive depression screening), hearing loss (n = 5 with at least a mild hearing loss), or cognitive status (n = 3 with low cognitive screening score). Two of the eleven interviewees did express disappointment in not being able to find others who wanted to talk about the same things as them. Both of these participants were lonely and depressed. One man had deeply held political and religious views that he wanted to discuss with others, but reported that instead he talked with others about “Mostly superficial stuff.” One woman wanted to talk about sports, but sat with a group of ladies who engaged in small talk:
Interviewer: What makes a good conversation for you?
Interviewee: Sports…Any of the Boston sports I love to talk about and a lot of people don’t and I don’t blame them for not being into football and baseball and hockey, that’s my thing but it’s not theirs…What do [the ladies I sit with] talk about? Mostly I let them talk and sometimes I listen, sometimes I don’t…
Communication Challenges
Despite comprehensive care, only one interviewee was a current hearing aid user; notably, he did not hear well during the interview with a substantial number of “huh” and “what” clarification utterances. One interviewee expressed difficulty hearing tablemates and staff members, and withdrawing from conversation due to those difficulties; but importantly, she also suggested that she was not interested in the small talk that the ladies at her table typically engaged in. Otherwise, participants (and staff) reported that activities were either led in small groups that made hearing easier or used microphones and speakers to amplify the person leading the activity (such as during a Bingo game).
Discussion
In this comprehensive mixed methods case study of the PACE Day Health Centers through the lens of communication and social engagement, we observe a high prevalence of untreated hearing loss, an enjoyed outlet for PACE participants, a kind staff and program credited with supporting the basic health and social needs of the participants, and a willingness by staff to learn new skills that aim to improve the experience of the PACE participants. In this section we interpret the mixed data presented in the results as they pertain to each of our research questions, culminating in a conceptual framework that can help speech and hearing professionals holistically support communication for older adults.
I. What do older adults value in terms of social interactions or conversations?
For PACE participants, the opportunity to get out of the house was a recurring positive noted about the DHC. Given the high rate of social isolation as measured by the IOM Measures of SBDs of Health Questionnaire and the general positive feelings about PACE as an outlet, it seems simply being with others gives a boost for most of the PACE participants. There is evidence in the literature that objective and subjective measures of social isolation have different associations with depression and psychological distress (Taylor et al., 2018). It may be the case that, despite high levels of objective social isolation as measured by the questionnaire in this study, the positive qualitative feedback about interactions at PACE suggests that attendance at the DHC reduces perceived social isolation. As noted in the integration section, the two interviewees who described not having shared interests with other attendees at PACE were positive for depression and loneliness per their questionnaire results, and congruently expressed subjective social isolation in their interviews.
II. What can be learned at PACE about fostering activity/communication/engagement?
Access to Care
Although the qualitative results with PACE participants highlighted the the quickness with which typical medical needs were addressed at the DHC, the quantitative results found that the PACE participant sample had a high prevalence of untreated hearing loss. The high prevalence of untreated hearing loss in this sample is consistent with population-based data (Bainbridge & Ramachandran, 2014; Chien & Lin, 2012); however, the comprehensive care plan of PACE creates an opportunity to more consistently address hearing loss. And yet, the capitated monetary system of PACE may make treating hearing loss expensive at a systems level. Nevertheless, the National Academies of Science, Engineering, and Medicine (2016) report on priorities for adult hearing loss has called for increased Medicaid coverage of hearing aids for adults. Further, cost anylses have shown that PACE saves Medicaid money as compared to fee-for-service long-term care systems (Wieland et al., 2013); thus, potentially creating an ideal opportunity for increased coverage of hearing aids. Perhaps, there is a policy opportunity in a model program like PACE to make hearing aids available under insurance plans for older adults.
Supporting on site Staff
While this research may have benefited from selection bias in the staff who participated in focus groups, there was a consistent willingness to engage in educational opportunities aimed at improving communication and participation. When the staff discussed communication together, they routinely generated positive adaptations to repair communication breakdowns on their own and acknowledged some poor communication behavior habits. Audiologists and SLPs (and group care organizations) should value the impact of in-service trainings on communication and hearing loss with care providers. Recently, there has been an interest in training community health workers (Sánchez et al., 2017; Suen et al., 2019; Suen et al., 2021), peer mentors (Bally & Bakke, 2007), and audiology assistants (Hamill & Andrews, 2016) to extend the provision of aural rehabilitation services. These programs could serve as models for training care staff at organizations that serve older adults. These sessions would be best if they occurred as part of an on-going relationship between the audiologist and/or SLP and the care organization (Hubbard et al., 2018).
III. What can the field learn about supporting communication in a group care setting?
The longterm interest in the series of projects that our research team has undertaken in partnership with PACE is to learn more about how addressing hearing loss at the group level might be done more affordably than custom hearing aids for each individual while acknowledging the potential for addressing hearing loss to improve the social engagement and health of the PACE participants. To that end, audiologists and SLPs should emphasize improvements to the environment that would benefit everyone without the burden of identifying individual hearing loss, which is known to be highly prevalent in the group (Mamo et al., 2019; Mamo & Wheeler, 2021). Furthermore, audiology (as a profession) and SLPs should increase their roles as the communication experts on interdisciplinary rehabilitation teams and in group care settings, similar to PACE (Johnson & Voigt, 2012). These roles are within each scope of practice, but are not at the forefront for many speech and hearing professionals (ASHA, n.d.).
Lessons Learned
As the culmination of the lessons learned through this mixed methods case study investigation we developed a conceptual framework for engaged communication (Figure 1). We define ‘engaged communication’ as ‘interaction shared between a person and one or more other people that allows the person to achieve both social and functional needs.’ By defining engaged communication this way, we advocate for a holistic approach to addressing hearing loss and supporting communication. Engaging in meaningful conversation depends on the person’s communication ability, the environment, opportunities for conversation and the interest/motivation to engage. Throughout this mixed methods case study, we have identified potential factors that contribute to engaged communication in the PACE DHC setting. If we consider each of the factors presented in the framework, we can observe how various data from this study fit into each category.
Figure 1.
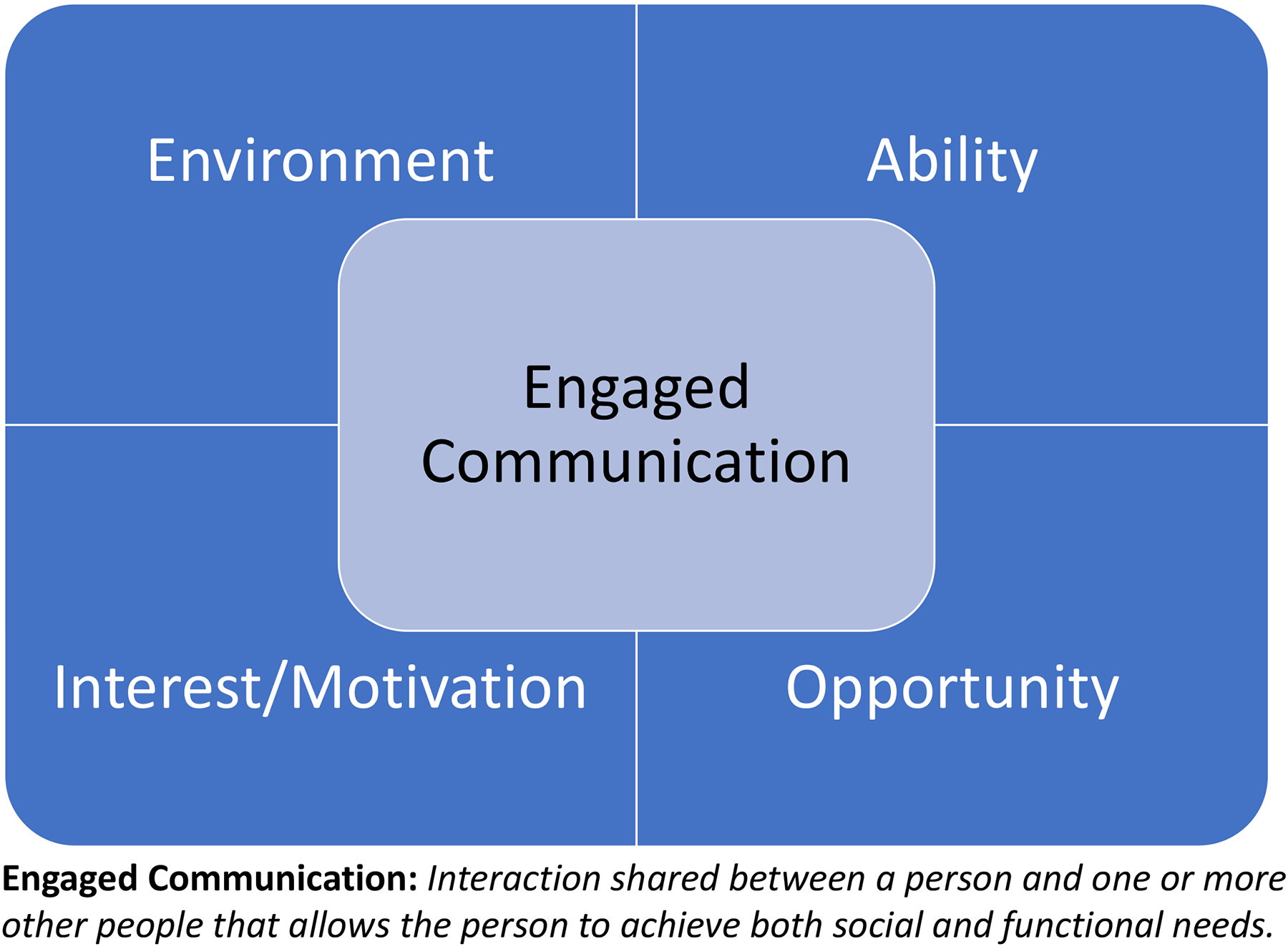
Conceptual framework defining the concept and the aspects that contribute to ‘engaged communication’ for older adults.
Environment
Regarding the “Environment”, we observed extraneous noise sources that detracted from communication in the DHCs, such as one room at lunch time that had a radio playing for the PACE participants, the sounds of a radio coming from the adjoining kitchen where staff was preparing food, and a TV in a different corner of the room playing daytime soap operas or game shows. On the other hand, staff and participants were aware of the need for less noise during activities. During group activities, staff and participants described small groups that allowed for good communication and use of microphones with activities that involved the whole room (e.g., Bingo).
Ability
For “Ability”, it is clear from the quantitative data that there is a high prevalence of untreated hearing loss. We found during focus group discussions that the staff was receptive to learning about and using personal amplifiers to support communication for people having hearing difficulties. In our current intervention research, there is a recurring interest in using amplification devices during clinic appointments; thus, highlighting a potential area were improvements can be made (NCT04659967). On the other hand, the cognitive challenge of listening with hearing loss, especially in a noisy environment, is not an aspect of communication that the staff seemed to be aware of during the focus group discussions. This is important because our quantitative data indicated that over a third of the sample participants scored below the screening cut-off for dementia on a cognitive screener. The combination of hearing loss and low cognitive processing abilities will have a negative impact on communication, especially in a noisy environment (Heinrich & Knight, 2016; Humes, 2013; Mamo & Helfer, 2021). It may be necessary for speech and hearing professionals to focus on the challenges of listening effort when preparing educational opportunities for staff.
Opportunity
“Opportunity” for engaged communication is a major highlight of the PACE program. Even interviewees who were lonely and/or depressed per the quantitative data valued being at the DHC—being with others, joining activities, having access to basic medical attention, and engaging with kind and caring staff members. The quantitative data indicated that all but one of the PACE participants scored as socially isolated on the questionnaire; thus, enrollment in a program like PACE is a key element of having the opportunity for engaged communication.
Interest/Motivation
Finally, “Interest/Motivation” seemed to be very individualized and, likely, linked more to participants’ personalities than the organization of PACE and the DHC. Audiologists and SLP team members at group care organizations can play a role in helping individuals advocate for the types of interactions that are motivating to them by including person-centered interviewing in our assessments.
The conceptual framework presented here attempts to emphasize the holistic nature of communication and the functional aspects of hearing ability in a group environment that includes both opportunities and challenges to communication and participation. Perhaps this framework could serve as a template that reminds not only audiologists and SLPs, but also OTs and Life Enrichment/Activity Coordinators, whom seem to be the de facto team members addressing the functional consequences of hearing loss, to put engaged communication at the center of their social engagement goals; thus, elevating the necessary awareness of hearing loss and environmental challenges faced by older adults in the group setting.
Limitations
This mixed methods case study is built around data collected from two PACE organizations, and there are 141 PACE organizations in the country (NPA, 2021). Nevertheless, the organizational structure of PACE yields important consistencies in their approach to and mission of care, such as the interdisciplinary nature of services and care planning, as well as the emphasis on the autonomy and care desires of their participants. In the literature, PACE is consistently described as an effective care program due to the comprehensive, interdisciplinary approach to care (Gyurmey & Kwiatkowski, 2019; Hirth et al., 2009; Mui, 2001; Wieland et al., 2013).
Another limitation to the study is that we did not test or interview anyone with moderate or severe dementia or their families. Nearly 60% of the sample population included in the larger PACE study (n = 160), of which the current study is a subset of data, had some indication of cognitive impairment in their medical chart data (Mamo & Wheeler, 2021). Three of our interview participants had a low score on the cognitive screener; these participants passed a capacity assessment to consent to the study. Otherwise, data is lacking regarding the communication needs of persons with dementia in the current analysis.
Conclusions
The PACE program is designed to support health and engagement for older adults who are nursing home eligible and living in the community (at the time of enrollment). The staff is built on a mission of interdisciplinary teamwork and demonstrates a willingness to learn new tools and techniques to support PACE participants. In this sample, the participants have a high prevalence of untreated hearing loss and high rates of loneliness and social isolation. The qualitative data suggests that the participants value the DHC, the social opportunities, the organized activities, and the kindness and support of the PACE staff. Speech and hearing professionals should consider interventions that support engaged communication by integrating hearing care services into a comprehensive care program like PACE. Future research should design low-tech hearing interventions aimed at addressing each of the factors that impact engaged communication in the conceptual framework presented in this manuscript. Designing better communication opportunities in group care settings will benefit not only those with hearing loss, but all of the older adult participants and staff working together in a busy and social environment.
Acknowledgments
Research reported in this publication was supported by the National Institute On Deafness And Other Communication Disorders of the National Institutes of Health under Award Number K23DC016855 (SKM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Drs. Mamo (trainee) and Plano Clark (mentor) were participants in the Mixed Methods Research Training Program for the Health Sciences funded by the National Institutes of Health through the Office of Behavioral and Social Science Research. The authors gratefully acknowledge Jessica Pearlman (UMass ISSR) for statistical consultations and the data collection efforts of Julia Read, Julia Serra, Frank Sigismondo, Olivia Perry, and Marcy Abong. The authors offer their sincerest thanks to the staff and participants at the PACE centers who collaborated on this project, providing support and space to do this work.
Acknowledgement of Funding Sources:
NIH/NIDCD K23DC016855
Footnotes
Conflict of Interest: There are no relevant conflicts of interest.
Due to the low-risk nature of the study, the IRB and the PACE organizations agreed to the on-site consenting of research participants with capacity assessments, rather than solicit more personal information about each participant by obtaining details and contact info regarding Legally Authorized Representatives.
Other reasons for exclusion included insufficient English understanding to provide informed consent (n = 3), opting not to complete the questionnaire portion of the study (n = 21), and inability to schedule a time to complete the questionnaires with the research team (n = 2).
The third PACE program that participated in the larger study opted not to participate in the social health questionnaire phase due to the high number of enrollees who would be unable to participate due to their English-language proficiency.
There is missing data from one participant at PACE-1, which could be due to the HHIE-S score not saving in the SHOEBOX database or due to researcher oversight/was never administered.
Physical activity score and alcohol use determination were calculated by combining answers to multiple questions; in addition to the two domains described in this methods section (Guise et al., 2017).
These participants had been provided with a GrandPad tablet for videoconferencing by the PACE-2 program to ameliorate social isolation while the DHC was closed or had reduced capacity during the pandemic.
Note: There is missing data for HA use from 3 participants. Of those participants, one had no hearing loss, one had moderate hearing loss, and one had severe hearing loss.
References
- Anderson ND, & Craik FI (2017). 50 Years of Cognitive Aging Theory. J Gerontol B Psychol Sci Soc Sci, 72(1), 1–6. 10.1093/geronb/gbw108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASHA. (n.d.). Aural Rehabilitation for Adults (Practice Portal). Retrieved 08/16/2021 from http://www.asha.org/Practice-Portal/Professional-Issues/Aural-Rehabilitation-for-Adults/
- Bainbridge KE, & Ramachandran V (2014). Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005–2006 and 2009–2010. Ear Hear, 35(3), 289–294. 10.1097/01.aud.0000441036.40169.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bally SJ, & Bakke MH (2007). A peer mentor training program for aural rehabilitation. Trends Amplif, 11(2), 125–131. 10.1177/1084713807301587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltes PB, & Lindenberger U (1997). Emergence of a powerful connection between sensory and cognitive functions across the adult life span: a new window to the study of cognitive aging? Psychol Aging, 12(1), 12–21. 10.1037//0882-7974.12.1.12 [DOI] [PubMed] [Google Scholar]
- CHABA, C. o. H., Bioacoustics, and Biomechanics). (1988). Speech understanding and aging. J Acoust Soc Am, 83, 859–895. [PubMed] [Google Scholar]
- Chien W, & Lin FR (2012). Prevalence of hearing aid use among older adults in the United States. Archives of Internal Medicine, 172(3), 292–293. 10.1001/archinternmed.2011.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clionsky M, & Clionsky E (2014). Psychometric equivalence of a paper-based and computerized (iPad) version of the Memory Orientation Screening Test (MOST®). Clin Neuropsychol, 28(5), 747–755. 10.1080/13854046.2014.913686 [DOI] [PubMed] [Google Scholar]
- Clionsky MI, & Clionsky E (2010). Development and validation of the Memory Orientation Screening Test (MOST): A better screening test for dementia. American Journal of Alzheimer’s Disease and Other Dementias, 25(8), 650–656. 10.1177/1533317510386216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on the Recommended Social Behavioral Domains Measures for Electronic Health Records Board on Population Health Public Health Practice, I. O. M. (2015). In Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. National Academies Press. 10.17226/18951 [DOI] [PubMed] [Google Scholar]
- Creswell JW, & Plano Clark VL (2018). Designing and conducting mixed methods research (Third Edition ed.). SAGE. [Google Scholar]
- Crowe S, Cresswell K, Robertson A, Huby G, Avery A, & Sheikh A (2011). The case study approach. BMC Med Res Methodol, 11, 100. 10.1186/1471-2288-11-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona C, Russell D, & Rose J (1986). Social support and adaptation to stress by the elderly. Psychol Aging, 1(1), 47–54. 10.1037//0882-7974.1.1.47 [DOI] [PubMed] [Google Scholar]
- Fetters MD, Curry LA, & Creswell JW (2013). Achieving integration in mixed methods designs-principles and practices. Health Serv Res, 48(6 Pt 2), 2134–2156. 10.1111/1475-6773.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 12(3), 189–198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Marx K, Dabelko-Schoeny H, Parker L, Anderson KA, Albers E, & Gitlin LN (2021). COVID-19 and the Need for Adult Day Services. J Am Med Dir Assoc, 22(7), 1333–1337. 10.1016/j.jamda.2021.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuse NB, Koonce TY, Kusnoor SV, Prather AA, Gottlieb LM, Huang LC, Phillips SE, Shyr Y, Adler NE, & Stead WW (2017). Institute of Medicine Measures of Social and Behavioral Determinants of Health: A Feasibility Study. American Journal of Preventive Medicine, 52(2), 199–206. 10.1016/j.amepre.2016.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinath B, McMahon CM, Burlutsky G, & Mitchell P (2016). Hearing and vision impairment and the 5-year incidence of falls in older adults. Age Ageing, 45(3), 409–414. 10.1093/ageing/afw022 [DOI] [PubMed] [Google Scholar]
- Gyurmey T, & Kwiatkowski J (2019). Program of All-Inclusive Care for the Elderly (PACE): Integrating Health and Social Care Since 1973. R I Med J (2013), 102(5), 30–32. [PubMed] [Google Scholar]
- Hamill TA, & Andrews JP (2016). Audiology Assistants in Private Practice. Semin Hear, 37(4), 348–358. 10.1055/s-0036-1593996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich A, & Knight S (2016). The Contribution of Auditory and Cognitive Factors to Intelligibility of Words and Sentences in Noise. Adv Exp Med Biol, 894, 37–45. 10.1007/978-3-319-25474-6_5 [DOI] [PubMed] [Google Scholar]
- Hirth V, Baskins J, & Dever-Bumba M (2009). Program of all-inclusive care (PACE): past, present, and future. J Am Med Dir Assoc, 10(3), 155–160. 10.1016/j.jamda.2008.12.002 [DOI] [PubMed] [Google Scholar]
- Hubbard HI, Mamo SK, & Hopper T (2018). Dementia and Hearing Loss: Interrelationships and Treatment Considerations. Semin Speech Lang, 39(3), 197–210. 10.1055/s-0038-1660779 [DOI] [PubMed] [Google Scholar]
- Humes LE (2013). Understanding the speech-understanding problems of older adults. Am J Audiol, 22(2), 303–305. 10.1044/1059-0889(2013/12-0066) [DOI] [PubMed] [Google Scholar]
- Jayakody DMP, Friedland PL, Martins RN, & Sohrabi HR (2018). Impact of Aging on the Auditory System and Related Cognitive Functions: A Narrative Review. Front Neurosci, 12, 125. 10.3389/fnins.2018.00125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson GR, & Voigt E (2012). Utilizing Interdisciplinary Treatment To Enhance Clinical Outcomes: Learning From Clinical Experience. Perspecitves of the ASHA Special Interest Groups, 17(3), 103–108. 10.1044/gero17.3.103 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care, 41(11), 1284–1292. 10.1097/01.Mlr.0000093487.78664.3c [DOI] [PubMed] [Google Scholar]
- Landis JR, & Gary GK (1977). The Measurement of Observer Agreement for Categorical Data. Biometrics, 33(1), 159–174. [PubMed] [Google Scholar]
- Lawrence BJ, Jayakody DMP, Bennett RJ, Eikelboom RH, Gasson N, & Friedland PL (2020). Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. Gerontologist, 60(3), e137–e154. 10.1093/geront/gnz009 [DOI] [PubMed] [Google Scholar]
- Lichtenstein MJ, Bess FH, & Logan SA (1988). Diagnostic performance of the hearing handicap inventory for the elderly (screening version) against differing definitions of hearing loss. Ear Hear, 9(4), 208–211. 10.1097/00003446-198808000-00006 [DOI] [PubMed] [Google Scholar]
- Lin FR, & Albert M (2014). Hearing loss and dementia - who is listening? Aging Ment Health, 18(6), 671–673. 10.1080/13607863.2014.915924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, & Ferrucci L (2011). Hearing loss and incident dementia. Arch Neurol, 68(2), 214–220. 10.1001/archneurol.2010.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Niparko JK, & Ferrucci L (2011). Hearing loss prevalence in the United States. Arch Intern Med, 171(20), 1851–1852. 10.1001/archinternmed.2011.506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, Satterfield S, Ayonayon HN, Ferrucci L, & Simonsick EM (2013). Hearing loss and cognitive decline in older adults. JAMA Intern Med, 173(4), 293–299. 10.1001/jamainternmed.2013.1868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loughrey DG, Kelly ME, Kelley GA, Brennan S, & Lawlor BA (2018). Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg, 144(2), 115–126. 10.1001/jamaoto.2017.2513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Pikhart H, & Sacker A (2019). Domains and Measurements of Healthy Aging in Epidemiological Studies: A Review. Gerontologist, 59(4), e294–e310. 10.1093/geront/gny029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamo SK, & Helfer KS (2021). Speech Understanding in Modulated Noise and Speech Maskers as a Function of Cognitive Status in Older Adults. Am J Audiol, 1–13. 10.1044/2021_aja-20-00177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamo SK, Reed NS, McNabney MK, Rund J, Oh ES, & Lin FR (2019). Age-related hearing loss and the listening environment: Communication challenges in a group care setting for older adults. Annals of Long-Term Care. 10.25270/altc.2019.09.00085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamo SK, & Wheeler KA (2021). The Combined Burden of Hearing Loss and Cognitive Impairment in a Group Care Setting for Older Adults. J Speech Lang Hear Res, 64(2), 328–336. 10.1044/2020_jslhr-20-00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mick P, Kawachi I, & Lin FR (2014). The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg, 150(3), 378–384. 10.1177/0194599813518021 [DOI] [PubMed] [Google Scholar]
- Mick P, Parfyonov M, Wittich W, Phillips N, & Kathleen Pichora-Fuller M (2018). Associations between sensory loss and social networks, participation, support, and loneliness: Analysis of the Canadian Longitudinal Study on Aging. Can Fam Physician, 64(1), e33–e41. [PMC free article] [PubMed] [Google Scholar]
- Mui AC (2001). The Program of All-Inclusive Care for the Elderly (PACE): an innovative long-term care model in the United States. J Aging Soc Policy, 13(2–3), 53–67. 10.1300/j031v13n02_05 [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Peterson DR, Temkin-Greener H, Delavan R, Gross D, Kunitz SJ, & Williams TF (2007). Program characteristics and enrollees’ outcomes in the Program of All-Inclusive Care for the Elderly (PACE). Milbank Q, 85(3), 499–531. 10.1111/j.1468-0009.2007.00497.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB, Temkin-Greener H, Delavan R, Peterson DR, Gross D, Kunitz S, & Williams TF (2006). Team performance and risk-adjusted health outcomes in the Program of All-Inclusive Care for the Elderly (PACE). Gerontologist, 46(2), 227–237. 10.1093/geront/46.2.227 [DOI] [PubMed] [Google Scholar]
- NASEM. (2016). Hearing Health Care for Adults: Priorities for Improving Access and Affordability. The National Academies Press. 10.17226/23446 [DOI] [PubMed] [Google Scholar]
- NPA. (2021). National PACE Association. Retrieved Nov 8 from https://www.npaonline.org/
- O’Connor C, & Joffe H (2020). Intercoder Reliability in Qualitative Research: Debates and Practical Guidelines. International Journal of Qualitative Methods, 19, 1–13. 10.1177/1609406919899220 [DOI] [Google Scholar]
- Orellana K, Manthorpe J, & Tinker A (2020). Day centres for older people: a systematically conducted scoping review of literature about their benefits, purposes and how they are perceived. Ageing Soc, 40(1), 73–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health, 42(5), 533–544. 10.1007/s10488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, & Adler N (2013). Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health, 103(11), 2056–2062. 10.2105/ajph.2013.301261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plano Clark VL, Foote LA, & Walton JB (2018). Intersecting mixed methods and case study research: Design possibilities and challenges. International Journal of Multiple Research Approaches, 10(1), 14–29. 10.29034/ijmra.v10n1a1 [DOI] [Google Scholar]
- Russell D, Peplau LA, & Ferguson ML (1978). Developing a measure of loneliness. J Pers Assess, 42(3), 290–294. 10.1207/s15327752jpa4203_11 [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess, 66(1), 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Sánchez D, Adamovich S, Ingram M, Harris FP, de Zapien J, Sánchez A, Colina S, & Marrone N (2017). The Potential in Preparing Community Health Workers to Address Hearing Loss. J Am Acad Audiol, 28(6), 562–574. 10.3766/jaaa.16045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt EM, Sands LP, Weiss S, Dowling G, & Covinsky K (2010). Adult day health center participation and health-related quality of life. Gerontologist, 50(4), 531–540. 10.1093/geront/gnp172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shukla A, Harper M, Pedersen E, Goman A, Suen JJ, Price C, Applebaum J, Hoyer M, Lin FR, & Reed NS (2020). Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngol Head Neck Surg, 162(5), 622–633. 10.1177/0194599820910377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen JJ, Bhatnagar K, Emmett SD, Marrone N, Kleindienst Robler S, Swanepoel W, Wong A, & Nieman CL (2019). Hearing care across the life course provided in the community. Bull World Health Organ, 97(10), 681–690. 10.2471/blt.18.227371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen JJ, Han HR, Peoples CY, Weikert M, Marrone N, Lin FR, & Nieman CL (2021). A Community Health Worker Training Program to Deliver Accessible and Affordable Hearing Care to Older Adults. J Health Care Poor Underserved, 32(1), 37–49. 10.1353/hpu.2021.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavakol M, & Dennick R (2011). Making sense of Cronbach’s alpha. Int J Med Educ, 2, 53–55. 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HO, Taylor RJ, Nguyen AW, & Chatters L (2018). Social Isolation, Depression, and Psychological Distress Among Older Adults. J Aging Health, 30(2), 229–246. 10.1177/0898264316673511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson GP, Sladen DP, Borst BJH, & Still OL (2015). Accuracy of a Tablet Audiometer for Measuring Behavioral Hearing Thresholds in a Clinical Population. Otolaryngology–Head and Neck Surgery, 153(5), 838–842. 10.1177/0194599815593737 [DOI] [PubMed] [Google Scholar]
- Uchida Y, Sugiura S, Nishita Y, Saji N, Sone M, & Ueda H (2019). Age-related hearing loss and cognitive decline - The potential mechanisms linking the two. Auris Nasus Larynx, 46(1), 1–9. 10.1016/j.anl.2018.08.010 [DOI] [PubMed] [Google Scholar]
- Velarde-Mayol C, Fragua-Gil S, & García-de-Cecilia JM (2016). [Validation of the UCLA loneliness scale in an elderly population that live alone]. Semergen, 42(3), 177–183. 10.1016/j.semerg.2015.05.017 (Validación de la escala de soledad de UCLA y perfil social en la población anciana que vive sola.) [DOI] [PubMed] [Google Scholar]
- Ventry IM, & Weinstein BE (1983). Identification of elderly people with hearing problems. Asha, 25(7), 37–42. [PubMed] [Google Scholar]
- Viljanen A, Kaprio J, Pyykko I, Sorri M, Pajala S, Kauppinen M, Koskenvuo M, & Rantanen T (2009). Hearing as a predictor of falls and postural balance in older female twins. J Gerontol A Biol Sci Med Sci, 64(2), 312–317. 10.1093/gerona/gln015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayne RV, & Johnsrude IS (2015). A review of causal mechanisms underlying the link between age-related hearing loss and cognitive decline. Ageing Res Rev, 23(Pt B), 154–166. 10.1016/j.arr.2015.06.002 [DOI] [PubMed] [Google Scholar]
- Wendler D (2004). Can we ensure that all research subjects give valid consent? Arch Intern Med, 164(20), 2201–2204. 10.1001/archinte.164.20.2201 [DOI] [PubMed] [Google Scholar]
- Wenger GC, Davies R, Shahtahmasebi S, & Scott A (1996). Social Isolation and Loneliness in Old Age: Review and Model Refinement. Ageing and Society, 16, 333–358. [Google Scholar]
- Wieland D, Kinosian B, Stallard E, & Boland R (2013). Does Medicaid pay more to a program of all-inclusive care for the elderly (PACE) than for fee-for-service long-term care? The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 68(1), 47–55. 10.1093/gerona/gls137 [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MA, Townsend A, & Greene R (1998). Stress reduction for family caregivers: effects of adult day care use. J Gerontol B Psychol Sci Soc Sci, 53(5), S267–277. 10.1093/geronb/53b.5.s267 [DOI] [PubMed] [Google Scholar]


