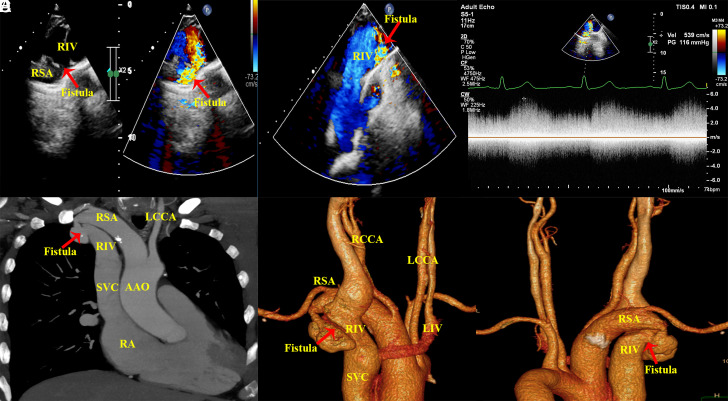
A 56-year-old man presented with intermittent chest pain for 10 years. On physical examination, a grade 3/6 continuous murmur was audible on the right sternal border at the second and third intercostal spaces. Transthoracic echocardiography showed a dilated right subclavian artery (RSA) with a 5-mm fistula to the right innominate venous (RIV), in addition to a dilated right ventricle and right atrium and mild tricuspid regurgitation (Figure 1A and 1B, Videos 1 and 2). Continuous-wave Doppler showed a flow signal at 5.4 m/s that was continuously moving from the RSA to the RIV throughout the cardiac cycle with a gradient of 116 mm Hg (Figure 1C). Maximum intensity projection (Figure 1D) and 3-dimensional reconstruction (Figure 1E, 1F) computed tomography angiography images showed an arteriovenous fistula from the RSA to the RIV associated with proximal stenosis and distal aneurysmal dilatation of the fistula vessels.
Figure 1.
(A and B) Transthoracic and color Doppler echocardiography show subclavian artery to innominate vein fistula. (C) Continuous-wave Doppler shows a flow signal at 5.4 m/s that is continuously moving from the RSA to the RIV throughout the cardiac cycle. Maximum intensity projection (D) and 3-dimensional reconstruction (E and F) show an arteriovenous fistula from the RSA to the RIV associated with proximal stenosis and distal aneurysmal dilatation of the fistula vessels. RSA, right subclavian artery; RIV; right innominate venous; LIV, left innominate venous LCCA, left common carotid artery; RCCA, right common carotid artery; AAO, ascending aorta; SVC, superior vena cava.
Congenital arteriovenous fistulas between the RSA and the RIV are uncommon in adults. They are usually acquired mostly as a consequence of an inadvertent arterial puncture during central venous catheterization, endovascular therapeutic procedures, or blunt trauma.1 The arteriovenous fistulas can actually lead to shunt-related congestive heart failure in newborns and infants.2 Depending on the degree of arteriovenous shunting, the clinical presentation of these anomalies ranges from being asymptomatic to symptoms and signs of high-output heart failure. The decision to treat or to follow up conservatively depends on the presence of symptoms and the degree of arteriovenous shunting.3 We report a rare case of an adult male associated with arteriovenous fistulas between the RSA and the RIV with proximal stenosis and distal aneurysmal dilatation of the fistula vessels, the patient has no history of trauma or previous invasive procedure, and he has asymptomatic of congestive heart failure for several years, and it is likely due to stenosis at the proximal initial site of the fistula and a little amount of left-to-right shunt, which reduces the anomalous “left-to-right” shunt from the RSA to RIV, he has been managed conservatively. Our case highlights that multimodality imaging is crucial in characterizing the arteriovenous fistulas between the RSA and the RIV and determining the treatment plan.
Footnotes
Informed Consent: The informed consent was obtained from the patient for this study.
Funding: This work is funded by the 2021 General Project Health and Family Planning Commission of Wuhan Municipality Scientific Research Project (WX21D46) and Wuhan Science and Technology Bureau (2019020701011422).
Video 2: Color Doppler echocardiography shows right subclavian artery to innominate vein fistula with dilated innominate venous.
References
- 1. Li G, Hu X, Wang Y, Chen S. Congenital subclavian-superior vena cava arteriovenous fistula with initial stenosis in an adult: a case report. BMC Cardiovasc Disord. 2020;20(1):376. 10.1186/s12872-020-01660-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dogan R, Yilmaz M, Ozkutlu S, Elsharshari H. Congenital subclavian artery to subclavian vein fistula presenting with congestive heart failure in an infant. Pediatr Cardiol. 2000;21(3):269 270. 10.1007/s002460010056) [DOI] [PubMed] [Google Scholar]
- 3. Brountzos EN, Kelekis NL, Danassi-Afentaki D, Nikolaou V, Apostolopoulou S, Kelekis DA. Congenital subclavian artery-to-subclavian vein fistula in an adult: treatment with transcatheter embolization. Cardiovasc Intervent Radiol. 2004;27(6):675 677. 10.1007/s00270-004-0027-3) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a