Introduction
Although the majority of patients with obsessive compulsive disorder (OCD) show at least some symptom reduction with first-line treatment interventions, a small proportion of patients with greater severity show little to no benefit and often present a challenge (Jenike, 2004). Ruscio et al. (2010) examined the epidemiology of OCD, and found severe OCD accounts for a large proportion of the public health burden attributable to patients with OCD overall (rates of receiving treatment were 93% for severe OCD, compared to 26% for moderate OCD). Growing evidence now supports intensive residential treatment (IRT) as an effective treatment for patients with severe OCD (e.g., Bjorgvinsson et al., 2013; Boschen et al., 2008; Stewart et al., 2005; Veale et al., 2016). However, due to the substantial emotional and financial commitment required for IRT as well as the limited number of IRT programs (e.g., Brennan et al., 2014), it is critical that the IRT approach be continually refined and optimized in order to enhance efficacy and efficiency.
Examination of both pre-treatment predictors of response and trajectories of symptom reduction may provide valuable information on how best to optimize IRT for OCD patients. While a few studies have examined predictors of outcome in IRT settings for adults with OCD, results are mixed, limiting the potential for meaningful clinical advances. Greater baseline OCD severity has predicted better outcomes in IRT (Brennan et al., 2014), whereas lower baseline severity predicted better outcome in other studies of IRT (Bjorgvinsson et al., 2013; Stewart et al., 2006). Additionally, OCD symptom subtype was found to not predict outcome in an IRT program examined by Chase and colleagues (2015), nor was insight in an IRT program by Stewart et al. (2006). Regarding psychiatric comorbidity, depression has also had mixed findings, Stewart and colleagues (2006) found it was not predictive of outcome, whereas it was predictive of improved response in a different IRT program (Bjorgvinsson et al., 2013). Additionally, alcohol use has been associated with poorer outcome in two different IRT settings (Brennan et al., 2014; Veale et al., 2016). Psychosocial functioning has had mixed associations with outcome in IRT settings; in Stewart and colleagues (2006), it predicted lower OCD symptoms at discharge, whereas Brennan and colleagues (2014) found it did not predict outcome. Finally, demographic variables are an important area to study as predictive of outcome as well; marital status/cohabitation has been found to be a predictor of improved outcomes in a review of IRT studies (Veale et al., 2016).
One potential explanation for these equivocal findings is that distinct groups of individuals may respond differently to the same treatment. Therefore, an important next step towards individualizing and optimizing outcome is to identify trajectories of symptom reduction and predictors of differential response. Growth mixture modeling (GMM) enables detection of subgroups of participants with similar response patterns, while allowing for variability among individuals (Nagin, 2005). The use of this approach is useful in identifying groups of patients who differentially respond to treatment, which is critical in the development of more personalized treatment approaches.
To our knowledge, no studies have used GMM to examine trajectories in OCD in IRT or outpatient settings. Therefore, we sought to expand prior work examining predictors of outcome and treatment course in IRT for OCD in our treatment program (Brennan et al., 2014; Stewart et al., 2006) by investigating whether there are distinct trajectories of response in IRT. In our program, we have observed that there is a sub-group of patients who do not have a linear trajectory of improvement.
Second, we aimed to examine differential predictors of any trajectory membership. As outlined previously, demographic and clinical variables such as comorbidity and marital status/cohabitation have previously been predictive of differential response rates in IRT programs. In outpatient samples, additional clinical variables have been found to be predictive of differential response rates such as OCD subtypes, comorbid personality disorders, (e.g., Abramowitz et al., 2003; Fricke et al., 2006; Pinto et al., 2011; Williams et al., 2013). Given these prior findings in the literature in IRT and outpatient settings, along with our clinical observations, we hypothesized that age, gender, education level, income, relationship status, having children, psychiatric comorbidity, level of depressive symptoms, quality of life, alcohol use, level of insight, OCD symptom subtype, and previous ERP treatment would differentiate trajectories.
Material and Methods
Participants
Participants were adults with primary OCD (N = 305) at McLean Hospital’s OCD Institute, an IRT program for OCD and related disorders (OCRDs) with an average length of stay of six to eight weeks. In this treatment program, all participants received individual and group therapy, which included four hours of ERP daily and multiple symptom-specific groups, and regular meetings with their behavior therapists (doctoral-level and master’s level clinicians), family therapists (master’s level clinicians), and psychiatrists. Participants who were admitted during 2014-2016 were included in the study. Eight participants had been admitted more than once during this time period; only their first admission was included. Seven were excluded due to missing data. Mean age was 30.2 years (SD = 12.9), 89% identified as White, 54% as male. At baseline, the mean Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) score was 25.3 (SD = 5.7), with 5% in the Mild range of severity, 29% Moderate, 54%, and 12% Extreme. Throughout the timeframe examined in this study (admission through week 8 of the treatment program), the percentage of Y-BOCS reduction for the sample was 30.4%. Among the overall sample, 85% were diagnosed with one comorbid axis I diagnosis and 29% with at least one comorbid axis II diagnosis. The most common secondary diagnoses were major depressive disorder (44%), social phobia (9%), and generalized anxiety disorder (8%). See Table 1 for more detailed demographic and clinical information.
Table 1.
Descriptives Table
| Overall Sample N (%) |
Class 1 (Linear Response) n (%) |
Class 2 (U-Shaped) n (%) |
|
|---|---|---|---|
| Gender | |||
| Male | 166 (54.4) | 159 (54.5) | 7 (53.8) |
| Female | 139 (45.6) | 133 (45.5) | 6 (46.2) |
| Race | |||
| African American | 2 (0.7) | 2 (0.7) | -- |
| Asian | 10 (3.3) | 10 (3.4) | -- |
| Caribbean Islander | 1 (0.3) | 1 (0.3) | -- |
| White | 270 (88.5) | 259 (88.7) | 11 (84.6) |
| Latino/Latina | 4 (1.3) | 3 (1.0) | 1 (7.7) |
| Multiracial | 8 (2.6) | 8 (2.7) | -- |
| Education | |||
| < High school Degree | 15 (4.9) | 13 (4.5) | 2 (15.4) |
| Graduated high school and/or started college | 148 (48.5) | 144 (49.3) | 4 (30.8) |
| Bachelors or Associates Degree | 91 (29.8) | 87 (29.8) | 4 (30.8) |
| Graduate or Professional Degree | 51 (16.7) | 48 (16.4) | 3 (23.1) |
| Relationship Status | |||
| Single | 227 (74.4) | 220 (75.3) | 7 (53.8) |
| Married/Partnered | 78 (25.6) | 72 (24.7) | 6 (46.2) |
| Children | |||
| No Children | 252 (82.6) | 244 (83.6) | 8 (61.5) |
| At least 1 child | 53 (17.4) | 48 (16.4) | 5 (38.5) |
| Previous treatment | |||
| No previous treatment | 98 (32.1) | 93 (31.8) | 5 (38.5) |
| Had previous treatment | 207 (67.9) | 199 (68.2) | 8 (61.5) |
| Previous admissions to the OCD Institute | |||
| No previous admissions | 266 (87.2) | 254 (87.0) | 12 (92.3) |
| 1 previous admission | 30 (9.8) | 29 (9.9) | 1 (7.7) |
| 2 previous admissions | 8 (2.6) | 8 (2.7) | -- |
| 3 previous admissions | 1 (0.3) | 1 (0.3) | -- |
| Concurrent Psychiatric Medication | 289 (94.7) | 277 (94.2) | 12 (92.3) |
| At least 1 Comorbid Axis I disorder | 260 (85.2) | 249 (85.3) | 11 (84.6) |
| At least 1 Comorbid Axis II disorder | 87 (28.5) | 85 (29.1) | 2 (15.4) |
| Median Household Income | $75,000 | $75,000 | $85,000 |
| M (SD) | |||
| Age | 30.17 (12.9) | 30.14 (12.9) | 30.69 (13.1) |
| Age of onset | 12.99 (7.3) | 12.97 (7.2) | 13.55 (10.9) |
| Y-BOCS at Admission | 25.3 (5.8) | 25.3 (5.7) | 25.2 (7.6) |
All participants received individual and group therapy, including four hours of ERP daily, and weekly meetings with therapists (individual and family) and psychiatrists. The treatment most resembled “open CBT” (cf. Franklin et al., 1998) - while clinicians did not follow a structured treatment manual, the task of all individual therapists (psychologists or highly experienced masters-level clinicians) was to assess and conceptualize OCD presentation and develop a targeted exposure-based treatment plan. In keeping with this, participants would initially receive psychoeducation about OCD and be provided the rationale for treatment, with emphasis placed on the importance of resisting rituals in the service of new learning. Following this, clinicians would commence with developing and implementing the treatment plan, consisting of exposure tasks that participants were expected to complete daily. This treatment plan was communicated to the programs’ mental health workers and advanced graduate students (i.e., ‘exposure coaches’; all of whom are trained and supervised in ERP) whom implemented the plan during pre-designated ERP treatment blocks (two hours in the morning and two in the afternoon). Approximately two of those four hours of ERP were completed with an exposure coach, while the others were completed in a self-directed manner. Additional exposures took place during meeting with individual therapists, however these meetings were also used to address other clinical variables that contributed to impairment (e.g., co-morbidity, willingness/motivation issues, low insight).
Measures
Structured Clinical Interview for DSM-IV Axis I and II Disorders (SCID-I/P; First et al., 1997; 2002) was used to assess for DSM-IV Axis I and II diagnoses and level of insight by trained staff, under supervision of a post-doctoral fellow and licensed clinical psychologist.
Yale-Brown Obsessive-Compulsive Scale, (Y-BOCS; Goodman et al., 1989) measures OCD severity and related impairment. Participants completed the self-report version, which has been highly correlated with the clinician-administered version (Federici et al., 2010). Scores in the Mild range are total scores of 8-15, Moderate = 16-23, Severe = 24-31, and Extreme = 32-40.
Dimensional Obsessive-Compulsive Scale (DOCS; Abramowitz et al., 2010) is a self-report measure of OCD subtypes: 1) Contamination; 2) Responsibility; 3) Unacceptable Thoughts; and 4) Symmetry. It has shown good convergent validity for associated measures and test-retest correlations (r = .55-.66) across total and subscale scores (Abramowitz et al., 2010). Within each of the four symptom dimensions, five items rated from 0 (no symptoms) to 4 (extreme symptoms) measure severity of time occupied by obsessions and compulsions, avoidance behavior, associated distress, functional interference, and difficulty disregarding the obsessions and refraining from the compulsions.
Hamilton Depression Rating Scale, six item version (HRSD-6; Bech et al., 1975).
The HRSD-6 is a six-item self-report measure of depressive symptom severity over the last 3 days. It has demonstrated acceptable psychometric properties (Bech et al., 2008). Higher scores reflected higher severity.
Alcohol Use Disorders Identification Test-Consumption Questions (AUDIT-C; Bush et al., 1998) is a brief alcohol screen that has been shown to reliably identify patients who currently have alcohol use disorders or who are hazardous drinkers.
Quality of Life Enjoyment and Satisfaction Questionnaire (Endicott, Nee, Harrison, & Blumenthal, 1993):
16-item self-report questionnaire of life satisfaction and enjoyment over the past week, and has demonstrated good reliability and validity. The total score was comprised of the sum of the first 14 items, with lower scores reflecting less life satisfaction and enjoyment.
Demographic Information and Treatment History.
This is a brief intake survey about demographic information and treatment history.
Procedures
All participants completed written informed consent, as approved by the Partners Human Research Committee. Participants were administered the SCID at admission, and self-report measures at admission, discharge, and weekly throughout treatment.
Data Analysis.
GMM was performed with Mplus 6.12 (Muthén & Muthén, 2011) to identify discrete growth trajectories based on weekly Y-BOCS scores across the first eight weeks of admission. Maximum likelihood estimation (ML) was used to account for non-normality and missing data. GMM was performed with Mplus 6.12 (Muthén & Muthén, 2011), to identify discrete growth trajectories based on weekly Y-BOCS scores across the first eight weeks of admission. Maximum likelihood estimation (ML) was used to account for non-normality and missing data. GMM is an exploratory technique for identifying classes of longitudinal change and differences in change between groups (Ram & Grimm, 2009), consisting of unconditional and conditional model analyses. Unconditional model analysis is used to determine the number of latent growth classes that best fit the data and conditional model analysis is used to test predictors of latent growth class membership.
Following procedures by Jung & Wickrama, 2008, we first conducted latent class growth analysis (LCGA) to identify a “shape” of growth in Y-BOCS scores over time and the presence or absence of distinct classes. LCGA is used initially because of faster and more likely successful model convergence during initial analyses (Jung & Wickrama, 2008). We examined three model shapes, including an intercept term and: 1) linear slope term; 2) linear and quadratic slope terms; and 3) piece-wise linear slope terms (modeling one linear slope from admission to through the third week of treatment and another for remaining weeks based on a visual examination of the raw individual data), respectively. A series of nested models (2-class, 3-class, etc.) was fit and compared to derive the number of latent growth classes that describe the heterogeneity of change in Y-BOCS scores over time. The best fitting model was determined by fit statistics, consideration of theory, and substantive meaning. The indices used to evaluate model fit were the Bayesian Information Criterion (BIC), Sample Size Adjusted BIC, Akaike’s Information Criterion, entropy, Bootstrap Likelihood Ratio Test (BLRT), and the Lo-Mendell-Rubin likelihood ratio test (LMR-LRT) test (Jung & Wickrama, 2008; Nagin & Odgers, 2010). The BIC, Sample Size Adjusted BIC, and AIC are information criterion fit statistics that compare log likelihood values of nested models where lower values represent a better fit. Entropy is a measure of classification accuracy where values close to 1 indicate high classification accuracy. A significant value of the BLRT and LMR-LRT test signifies that a model with K classes fits significantly better than a model with K-1 classes. Nylund et al. (2007) indicated the BIC is the best and most consistent fit statistic for determining the number of classes. Average posterior probabilities were also used to assess the quality of the model solution, which indicate the individual’s probabilities of being assigned to each class based on their response pattern (see Table 4). The highest probability demarcates the class to which they are assigned. Values greater than 0.80 indicate high accuracy in classification (Rost, 2006). Only classes with at least 1% of the total sample were considered.
Table 4:
Average Posterior Probabilities for Most Likely Latent Class Membership (Row) by Latent Class (Column)
| Assigned Class | Class 1 (Linear Response) |
Class 2 (U-Shaped Curve) |
|---|---|---|
| 1 | 0.96 | 0.04 |
| 2 | 0.25 | 0.75 |
Once the best-fitting LCGA model was identified, the comparable GMM model was evaluated and fit statistics were compared between models. Further, GMM models with the alternative “shape” and adjacent numbers of classes were examined to verify selection of the best fitting model. We chose to prioritize fit of GMM models as these specify that individuals within classes may vary, which we expected of our sample. Upon selecting the best fitting unconditional GMM model, a series of conditional GMM models were tested. Each of the conditional models included intercept and slope terms identical to the previously-selected unconditional model and added terms to regress the intercept and slope growth factors onto the time-invariant hypothesized predictor. Further, multinomial logistic regression of the class assignment on the same time-invariant predictor was included comparing class 1 to class 2.
The included time-invariant predictors were specifically: DOCS as a measure of OCD subtypes (included all four dimensional scores from baseline assessment simultaneously as continuous variables), axis I comorbidity (discrete binary variable; 0 = no comorbidity, 1 = any comorbidity in addition to OCD; no diagnosis was treated as a separate predictor but grouped together with all axis I disorders), axis II comorbidity (discrete binary variable; 0 = no comorbid personality disorder, 1 = any comorbid personality disorder), age (continuous variable), previous exposure and ritual prevention treatment (discrete binary variable; 0 = no previous exposure treatment, 1 = any previous exposure treatment), sex (discrete binary variable; 1 = male, 2 = female), educational level (ordinal variable; 1 = 8th grade or less, 2 = some high school, 3 = high school graduate/GED, 4 = some college, 5 = bachelor’s degree, 6 = associate's degree, 7 = graduate degree), household income (discrete binary variable based on a median split; 0 = less than $59,999, 1 = greater than $60,000), relationship status (discrete binary variable; 0 = single, separated, or divorced, 1 = married or partnered), children (discrete binary variable; 0 = no children, 1 = at least one child), level of insight (as an ordinal variable; 1 = absent, 2 = poor, 3 = good), level of depression symptoms (as a continuous variable), quality of life (continuous variable), and alcohol use scores (as a continuous variable).
Results
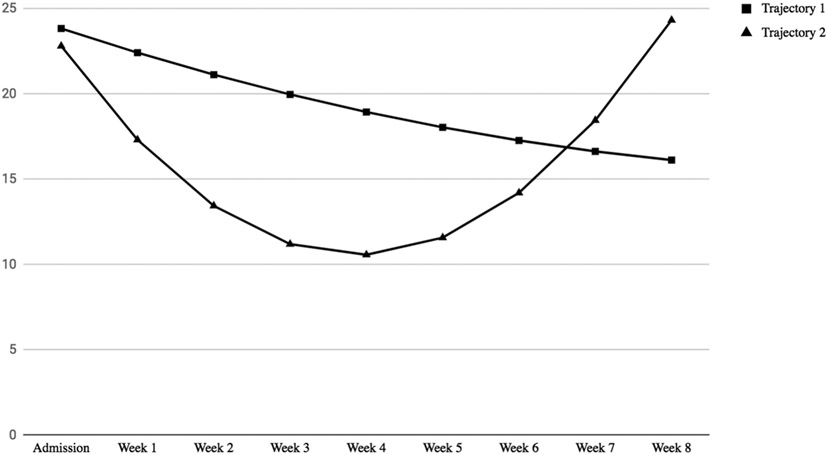
Fit statistics from the LCGA suggested the piece-wise 2-class model fit our data best. Next an unconditional GMM piece-wise 2-class model was examined; however, the latent variable covariance matrix was not positive definite, suggesting it was not a tenable model. Therefore, unconditional GMM models ranging from 1-3 latent classes were examined. Goodness of fit statistics (Table 2) suggested the quadratic 2-class model best fit our data. Overall, 96% of the sample (n = 292) belonged to a trajectory which had a linear, negative slope (i.e., linear responders). Whereas 4% (n = 13) had a trajectory exhibiting a non-significant “U-shaped curve” response pattern (i.e. the u-shaped responders; see Figure 1). The intercept parameter for the linear responders indicated group members began with moderate to severe OCD (B = 23.84, SE = 0.37, 95% CI = 23.11, 24.57, p < .001; Table 3). Linear change parameters for this trajectory revealed significant improvement in Y-BOCS scores during the first eight weeks (B = −1.48, SE = 0.35, 95% CI = −2.18, −0.79, p < .001) without a significant quadratic parameter (B = 0.07, SE =0.04, 95% CI = −0.02, 0.15, p = .13). In contrast, the intercept parameter for the u-shaped responders indicated participants began with less severe OCD (B = 22.81, SE = 2.89, 95% CI = 17.14, 28.48, p < .001) which did not change linearly during the first eight weeks (B = −6.31, SE = 3.23, 95% CI = −12.64, 0.03, p = .51), and there was not evidence of a significant quadratic effect (B = 0.81, SE = 0.65, 95% CI = −0.46, 2.08, p = .21). Examination of the growth parameters and CI’s (using the linear responders as reference group) for both trajectories revealed different intercepts, linear, and quadratic slopes; however, uneven group sizes led to larger standard errors around the estimates for the second group (see Table 3).
Table 2:
Goodness of Fit Statistics for Unconditional Model Solutions
| Model Type | BIC | Sample Size Adjusted BIC |
AIC | Entropy | LMR- LRT |
BLRT |
|---|---|---|---|---|---|---|
| Linear – 1 Class | 10027.360 | 9982.959 | 9975.275 | - | - | - |
| Quadratic – 1 Class | 9988.181 | 9931.093 | 9921.215 | - | - | - |
| Piece-wise – 1 Class | 9994.257 | 9937.169 | 9927.291 | - | - | - |
| Linear – 2 Class | 10039.733 | 9985.817 | 9976.488 | 0.404 | 4.52 (p=0.56) | p = .43 |
| Quadratic – 2 Class | 9995.192 | 9925.419 | 9913.345 | 0.805 | 15.21 (p = 0.65) | p < .001 |
| Piece-wise – 2 Classa | - | - | - | - | - | - |
| Linear – 3 Class | 10050.518 | 9987.088 | 9976.112 | 0.663 | 6.03 (p = .32) | p = .29 |
| Quadratic – 3 Class | 10012.066 | 9929.607 | 9915.338 | 0.611 | 5.76 (p = .10) | p = .43 |
| Piece-wise – 3 Classa | - | - | - | - | - | - |
Note. BIC = Bayesian Information Criterion. AIC = Akaike Information Criterion. LMR-LRT = Lo-Mendell-Rubin Likelihood Ratio Test. BLRT = Bootstrap Likelihood Ratio Test.
Latent variable covariance matrix is not positive definite, model is untenable.
Figure 1. Growth Trajectories (Y-BOCS Scores).
Note. Y-BOCS = Yale-Brown Obsessive Compulsive Scale.
Table 3:
Quadratic Two-Class
| B | SE | 95% CI Lower | 95% CI Upper | CI overlap | |
|---|---|---|---|---|---|
| Class 1 | |||||
| Intercept | 23.842 | 0.373 | 23.11092 | 24.57308 | No |
| Linear Slope | −1.484 | 0.353 | −2.17588 | −0.79212 | No |
| Quadratic Slope | 0.065 | 0.043 | −0.01928 | 0.14928 | No |
| Class 2 | |||||
| Intercept | 22.812 | 2.894 | 17.13976 | 28.48424 | Yes |
| Linear Slope | −6.306 | 3.232 | −12.64072 | 0.02872 | Yes |
| Quadratic Slope | 0.812 | 0.648 | −0.45808 | 2.08208 | Yes |
Predictors of Latent Class Assignment and Parameters.
Of the 14 conditional models, none of the covariates significantly predicted latent class assignment. Examination of the conditional models suggested some covariates may predict growth parameters, regardless of class assignment. Participants diagnosed with comorbid personality disorders had a higher intercept (B = 1.70, SE = 0.68, 95% CI = 0.35, 3.03, p = .01). Individuals with children had more negative linear slope (B = −1.11, SE = 0.43, 95% CI = −1.95, −0.28, p = .01) and more positive quadratic slope (B = 0.12, SE = 0.05, 95% CI = 0.03, 0.17, p = .01); suggesting that individuals with children had greater decreases in Y-BOCS scores early in treatment.
Discussion
The objective of this study was to empirically derive distinct trajectories of OCD symptom response during IRT, and to examine covariate predictors of these trajectories. The unconditional GMM quadratic 2-class model was the best fit to the data. The linear responders class included the majority of patients (96%) and demonstrated a linear, negative slope with steady, significant improvement during the first eight weeks, which is consistent with our observations that most patients in IRT for OCD demonstrate response. A minority of patients (4%; Class 2) showed a response pattern which resembled a “U-shaped curve” in that the patients began treatment with less severe OCD symptoms than in Class 1, had a trend for improvement, and symptoms began to increase in between weeks four and five (see Figure 1); a novel pattern of treatment response not previously documented in IRT for OCD.
These findings suggest that large changes in self-reported Y-BOCS scores are the primary difference determining class membership. In particular, the first 4-5 weeks of IRT may be a critical window for a subset of patients, although, the small size of the u-shaped responders limits confidence in the parameter estimates. Of note, there are no formal changes in the treatment program at this time point. Participants in Class 2 (U-shaped) demonstrated a faster decrease in symptoms during this window, though showed an increase in symptoms starting at week 5, whereas participants in Class 1 (Linear response) had a slower, yet steady, rate of change throughout treatment. Early gains have been documented in IRT for OCD and are worthy of further investigation (e.g., Brennan et al., 2014; Krompinger et al., 2017). Given that one of the aims of this study was to gain knowledge towards refining and optimizing IRT through the enhancement of its efficacy and efficiency, it is important for IRT programs to consider the implications of these consistent findings when developing treatment plans with patients, especially those who have logistical barriers to being able to stay in IRT beyond 4-6 weeks.
With respect to our second hypothesis, we found that none of our hypothesized predictor variables (OCD subtypes, level of insight, psychiatric comorbidities, level of depressive symptoms, quality of life, alcohol use, age, previous ERP treatment, gender, education level, income, relationship status, or having children) differentially predicted assignment to either Class 1 (Linear response) or Class 2 (U-shaped). We found this result to be surprising, as prior studies in outpatient settings have found significant predictors of OCD response patterns (e.g., comorbid axis II personality disorders; Fricke et al., 2006; Pinto et al., 2011; Steketee, Chambless & Tran, 2001), and studies of IRT although with mixed findings, have had significant predictors of outcome [i.e., alcohol use (Brennan et al., 2014; Veale et al., 2016), and baseline OCD severity (Brennan et al., 2014; Bjorgvinsson et al., 2013; Stewart et al., 2006)]. However, this is the first study to employ growth mixture modeling as an approach to studying outcome in OCD, and therefore the research question was different than in these prior studies. We sought to learn about the particular course of response among patients, and wanted to learn if predictor variables would provide additional information about the pattern of the course, not only the outcome; and we found that none of our hypothesized predictor variables provided additional information about these trajectories of response.
An interesting commonality between prior studies and the present study is that when we examined all participants in both groups, participants with comorbid axis II personality disorders had higher levels of OCD symptoms throughout treatment, which seems consistent with the general trends in the literature showing that comorbid personality disorders attenuate treatment response. However, these comorbidities did not differentially predict assignment to Class 1 or 2, therefore they did not predict a specific course of symptom change. This underscores the importance of using statistical methods such as GMM when examining predictors of treatment response in an attempt to develop personalized medicine approaches, as it enables the detection of latent classes of subgroups of participants with similar response patterns. This method gives us more information about the u-shaped responders beyond simply lack of response - here we have an example of the specific way they might respond.
The disparity in size between the two trajectory classes is striking. On one hand, this is reassuring inasmuch as it appears that IRT, generally, is effective and that most patients can expect to follow a fairly predictable, linear path through treatment (notwithstanding the phenomenon of nonlinear dynamic instability preceding change that can be detected when symptoms are assessed more frequently; e.g., Heinzel, Tominschek, & Schiepek, 2014). On the other, it illustrates the unique challenge in working in an intensive residential setting: given the severity and diagnostic complexity in these patients that would precipitate a referral to such a setting, there will exist subsets of such patients for whom established treatment approaches do not lead to typical response patterns. The current study illustrates the usefulness of the GMM approach in identifying such a patient group. Assuming that future trajectories analyses replicate this finding, such studies would benefit from deeply investigating these groups to determine phenotypic profiles that are predictive of attenuated change. It may be the case that some variables not measured here are playing a role in distinguishing this small group from the larger sample. For example, anomalies in neural mechanisms such as cognitive biases, response inhibition, and dispositional approach/avoidance may have characterized our participants who did not have a linear response. Further, it is possible that unique dynamics of moment to moment affective-behavioral interactions characterize a sample that is less responsive to IRT. For example, it may be the case that the u-shaped group participants experience more opportunities to obsess throughout a given day (e.g, “my life is an exposure”) and this data is insufficiently captured by a weekly self-reported YBOCS. Ecological momentary assessment (EMA) would be a useful tool in pursuit of uncovering such information (cf. Schiffman, Stone, & Hufford, 2008).
We acknowledge several limitations. First, our sample was predominantly White, limiting generalizability of our findings. Second, we used the self-reported Y-BOCS, which has the potential for response bias as there is a potential confound of patients with higher levels of comorbidities rating symptoms worse. Third, our confidence in the final model must be tempered by the inconsistent fit indices and small class prevalence of the u-shaped responder group. This model had the lowest sample-size adjusted BIC, AIC, and a significant BLRT, and the entropy measure supported the quadratic 2-class model. However, the 1-class quadratic model had lower BIC and the LMR-LRT was non-significant in the quadratic 2-class model. Fit indices tend to have difficulties in performance when the sample size is lower (Nylund et al., 2007), as it is in the current study. This required us to make a partially theory-driven selection of the quadratic 2-class model. Examination of the trajectories within this quadratic 2-class model was also consistent with clinical impressions and prior research in other samples in our IRT program (Krompinger et al., 2017), showing that there is a meaningful difference between early and later response. Fourth, the participants in this study were receiving different types of medications which limits our ability to fully evaluate the effects of medication on trajectories of response.
In conclusion, in our sample of adults with primary OCD receiving IRT, two trajectories of treatment response emerged, with assignment to these groups not differentially predicted by OCD subtypes, axis I or II comorbidities, age, previous ERP treatment, previous treatment at OCDI, alcohol use, level of depressive symptoms, quality of life, gender, education level, income, relationship status, or having children. Overall, results suggest that a sub-group of patients (“u-shaped responders”) may benefit from additional monitoring as they as they progress through treatment. It is recommended that future studies evaluate whether these findings are consistent across samples and treatment settings – particularly OCD patients receiving outpatient ERP treatment. While our current findings are only directly applicable to the IRT setting, about 40-50% of OCD outpatients receiving ERP treatment do not have adequate treatment response (Fisher & Wells, 2005), and therefore there is a critical need to make modifications to ERP treatment more generally. This study highlights the importance of monitoring the specific trajectories patients are taking while in treatment, and applying personalized treatment approaches accordingly. Further studying specific trajectories in future studies in different settings could aid in the refinement of IRT for OCD, and guide investigation into the optimal delivery of outpatient ERP treatment for OCD generally.
Acknowledgements:
We thank Sadie Cole-Monaghan, Christine Andre, and Diane Davey for their contributions to the development and ongoing support of the OCD Institute’s research program.
Funding:
BPB was partially funded by grant K23-MH092397 from the NIMH
References
- Abramowitz JS, Franklin ME, Schwartz SA, & Furr JM (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 71(6), 1049. [DOI] [PubMed] [Google Scholar]
- Abramowitz JS, Deacon BJ, Olatunji BO, Wheaton MG, Berman NC, Losardo D, … & Björgvinsson T 2010. Assessment of OC symptom dimensions: Development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psych. Ass, 22, 180. [DOI] [PubMed] [Google Scholar]
- Bech P 2008. The use of rating scales in affective disorders. European Psychiatric Review, 1, 14–18. [Google Scholar]
- Bech P, Gram LF, Dein E, Jacobsen O, Vitger J, & Bolwig TG 1975. Quantitative rating of depressive states: Correlation Between Clinical assessment, Beck's Self-Rating Scale and Hamilton's Objective Rating Scale. Acta Psychiatrica Scandinavica, 51(3), 161–170. [DOI] [PubMed] [Google Scholar]
- Björgvinsson T, Hart AJ, Wetterneck C, Barrera TL, Chasson GS, Powell DM, … & Stanley MA 2013. Outcomes of specialized residential treatment for adults with obsessive-compulsive disorder. Journal of Psychiatric Practice, 19(5), 429–437. [DOI] [PubMed] [Google Scholar]
- Boschen MJ, Drummond LM, & Pillay A (2008). Treatment of severe, treatment-refractory obsessive-compulsive disorder: a study of inpatient and community treatment. CNS spectrums, 13(12), 1056–1065. [DOI] [PubMed] [Google Scholar]
- Brennan BP, Lee C, Elias JA, Crosby JM, Mathes BM, Andre MC, … & Hudson JI 2014. Intensive residential treatment for severe OCD: Characterizing treatment course and predictors of response. Journal of Psychiatric Research, 56, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT Alcohol Consumption Questions (AUDIT-C): An effective brief screening test for problem drinking. Arch Internal Med, 3, 1789–1795. [DOI] [PubMed] [Google Scholar]
- Chase T, Wetterneck CT, Bartsch R. a., Leonard RC, & Riemann BC 2015. Investigating treatment outcomes across OCD symptom dimensions in a clinical sample of OCD patients. Cognitive Behaviour Therapy, 6073, 1–12. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, & Blumenthal R (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: A New Measure. Psychopharmacology Bulletin, 321–326. [PubMed] [Google Scholar]
- Federici A, Summerfeldt LJ, Harrington JL, McCabe RE, Purdon CL, Rowa K, & Antony MM 2010. Consistency between self-report and clinician-administered versions of the Yale-Brown Obsessive–Compulsive Scale. J.Anx.Disorders, 24, 729–733. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, & Benjamin LS, 1997. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington D.C.: American Psychiatric Press, Inc. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders. NY: Biometrics Research, NYSPI. [Google Scholar]
- Franklin ME, Kozak MJ, Cashman LA, Coles ME, Rheingold AA, & Foa EB (1998). Cognitive-behavioral treatment of pediatric obsessive-compulsive disorder: an open clinical trial. Journal of the American Academy of Child & Adolescent Psychiatry, 37(4), 412–419. [DOI] [PubMed] [Google Scholar]
- Fricke S, Moritz S, Andresen B, Jacobsen D, Kloss M, Rufer M, & Hand I 2006. Do personality disorders predict negative treatment outcome in obsessive–compulsive disorders? A prospective 6-month follow-up study. European Psychiatry, 21(5), 319–324. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, … & Charney DS 1989. The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Archives of General Psychiatry, 46(11), 1006–1011. [DOI] [PubMed] [Google Scholar]
- Heinzel S, Tominschek I, & Schiepek G 2014. Dynamic patterns in psychotherapy-discontinuous changes and critical instabilities during the treatment of obsessive compulsive disorder. Nonlinear dynamics, psychology, and life sciences, 18(2), 155–176. [PubMed] [Google Scholar]
- Jenike MA 2004. Obsessive–compulsive disorder. New England J. of Med, 350(3), 259–265. [DOI] [PubMed] [Google Scholar]
- Jung T, & Wickrama KAS 2008. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. [Google Scholar]
- Krompinger JW, Monaghan SC, Gironda CM, Garner LE, Crosby JM, Brennan BP, & Elias JA 2017. Early response is predictive of outcome in intensive behavioral treatment for OCD. Journal of Obsessive-Compulsive and Related Disorders, 15, 57–63. [Google Scholar]
- Muthén LK, & Muthén BO 2011. Mplus user’s guide (6th ed.). Los Angeles: CA. [Google Scholar]
- Nagin DS, 2005. Group-based modeling of development. Harvard University Press. [Google Scholar]
- Nagin DS, & Odgers CL (2010). Group-based trajectory modeling in clinical research. Annual review of clinical psychology, 6., 109–138. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO 2007. Deciding on the number of classes in LCA and GMM: A Monte Carlo simulation study. Structural Eq. Modeling, 14, 535–69. [Google Scholar]
- Pinto A, Liebowitz MR, Foa EB, & Simpson HB 2011. OCPD as a predictor of exposure and ritual prevention outcome for OCD. Behaviour Research and Therapy, 49, 453–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram N, & Grimm KJ (2009). Methods and measures: Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International journal of behavioral development, 33(6), 565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rost J (2006). Latent-class-analyse. In Handbuch der Psychologischen Diagnostik (pp. 275–287). Göttingen, Germany: Hogrefe. [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, & Kessler RC 2010. The epidemiology of OCD in the National Comorbidity Survey Replication. Molecular Psychiatry, 15(1), 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR 2008. Ecological momentary assessment. Annu. Rev. Clin. Psychol, 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Steketee G, Chambless DL, & Tran GQ (2001). Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry, 42(1), 76–86. [DOI] [PubMed] [Google Scholar]
- Stewart SE, Stack DE, Farrell C, Pauls DL, & Jenike MA (2005). Effectiveness of intensive residential treatment (IRT) for severe, refractory obsessive-compulsive disorder. Journal of psychiatric research, 39(6), 603–609. [DOI] [PubMed] [Google Scholar]
- Stewart SE, Yen CH, Stack DE, & Jenike MA 2006. Outcome predictors for severe OCD patients in intensive residential treatment. J. Psych.Res, 40, 511–519. [DOI] [PubMed] [Google Scholar]
- Veale D, Naismith I, Miles S, Gledhill LJ, Stewart G, & Hodsoll J (2016). Outcomes for residential or inpatient intensive treatment of obsessive–compulsive disorder: a systematic review and meta-analysis. Journal of Obsessive-Compulsive and Related Disorders, 8, 38–49. [Google Scholar]
- Williams MT, Mugno B, Franklin M, & Faber S (2013). Symptom dimensions in obsessive-compulsive disorder: phenomenology and treatment outcomes with exposure and ritual prevention. Psychopathology, 46(6), 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]