Abstract
Background
US physicians are at risk for high rates of occupational stress and burnout, which the COVID-19 pandemic has intensified. As approaches targeting physicians’ individual resilience have fallen short, researchers are increasingly calling for studies that investigate organizational drivers of stress and burnout.
Objective
To understand the multi-dimensional systems factors shaping hospital physicians’ occupational stress during the pandemic.
Design
Qualitative, semi-structured interviews conducted in February–October 2021.
Setting
Hospitals in New York City and New Orleans.
Participants
A purposive snowball sample of attending physicians and fellows in hospital medicine, emergency medicine, pulmonary critical care, and palliative care who spent at least 4 weeks providing inpatient COVID-19 care beginning in March 2020 was selected. The sample included 40 physicians from 14 hospitals in New York City and 39 physicians from nine hospitals in New Orleans.
Approach
Descriptive analysis of participants’ self-reported perceptions of occupational stress.
Key Results
Participants identified multiple factors shaping their occupational stress including individual-level factors such as age, work experience, and life stage; institutional-level factors such as resource disparities, institutional type and size, and policies; professional-level factors such as informal rationing and medical uncertainty; and societal-level factors such as the federal response, COVID politics, and social inequalities. Stressors within and across these four levels worked in combination to shape physicians’ perceptions of occupational stress at the individual level.
Conclusions
This article contributes to an emergent literature on systems-based approaches to occupational stress and burnout among physicians by demonstrating the intersections among societal conditions, professional cultures, institutional work environments, and individual stress. Findings from semi-structured interviews suggest that interventions to reduce physician stress and burnout may be more effective if they target systems factors and stressors at multiple levels.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07848-z.
KEY WORDS: Physicians, Occupational stress, Burnout, COVID-19, Qualitative research, United States
US physicians are at high risk for occupational stress and burnout,1 a phenomenon resulting from chronic workplace stress characterized by (1) fatigue or exhaustion, (2) negativity toward one’s job, and (3) reduced professional efficacy.2 A 2019 National Academies of Medicine (NAM) report estimated that 40–54% of physicians are burnt out, making burnout more prevalent in physicians than in other professionals with similar educational attainment.3 The COVID-19 pandemic has intensified stress and burnout4,5: 76% of US healthcare workers reported burnout in September 2020, up from 54% in 2019.6 Additionally, physicians globally have reported increased levels of depression,7–10 anxiety,8–13 and posttraumatic stress disorder.14
Interventions targeting physicians’ individual resilience have consistently fallen short of addressing burnout effectively.15,16 Consequently, experts are increasingly calling for studies that prioritize systems-based interventions and investigate organizational drivers of burnout.3,17–22 Such factors include workload and scheduling,23–25 administrative burden,19,26 electronic medical record usage,27 organizational culture,19,25,26 and team dynamics.26 During the COVID-19 pandemic, inadequate personal protective equipment (PPE),9,28–30 nursing staffing shortages,30 lack of support at work,31 and poor leadership28,30,32 have also contributed to occupational stress and burnout.
This study adds to the growing body of research on systems approaches to burnout by qualitatively examining physicians’ perceptions of occupational stress while working during the COVID-19 pandemic. We focus on occupational stress because it is pervasive and can lead to burnout if not mitigated. Most studies of physicians during COVID-19 have focused on psychiatric morbidity, highlighting individual predictors of poor mental health like gender,9,33–36 age,8,9,34–37 social isolation,34,38 and fears about viral exposure.13,34,39,40 Only a few studies have used qualitative methods to investigate physicians’ pandemic experiences,41–43 and none has focused on physicians’ perceptions of the root causes of their stress, including systems-based drivers. In this study, we sought to characterize the multi-dimensional systems factors—at the individual, institutional, professional, and societal levels—that shaped frontline physicians’ perceptions of stress during the pandemic. To address this objective, we conducted semi-structured interviews with physicians in New York City and New Orleans who cared for hospitalized COVID-19 patients during and beyond the initial surge.
Methods
Study Design and Rationale
Our study design was guided by a conceptual model from the National Academies of Medicine report on clinician burnout, which explicitly called for more research on systems factors affecting clinician wellbeing.3 We adapted the model to include attention to professional-level factors, such as professional norms (see Fig. 1). Semi-structured interviews were selected because they are uniquely suited to producing nuanced accounts of complex phenomena.44 To assess how differences in state and local public health responses and organizational factors shape how individual physicians responded to COVID-19, we used a comparative design, sampling physicians from various hospital types in two cities. New York City (NYC) was initially selected because it was the epicenter of the US outbreak beginning in March 2020. New Orleans (NOLA) provided an apt comparison because it experienced initial surge conditions at roughly the same time; both cities peaked in early to mid-April. We hypothesized that it would be analytically generative to compare cities that experienced surge conditions contemporaneously, with similar knowledge and resource constraints, but with different social and political contexts. The study was deemed exempt by the UNC-Chapel Hill Institutional Review Board.
Fig. 1.
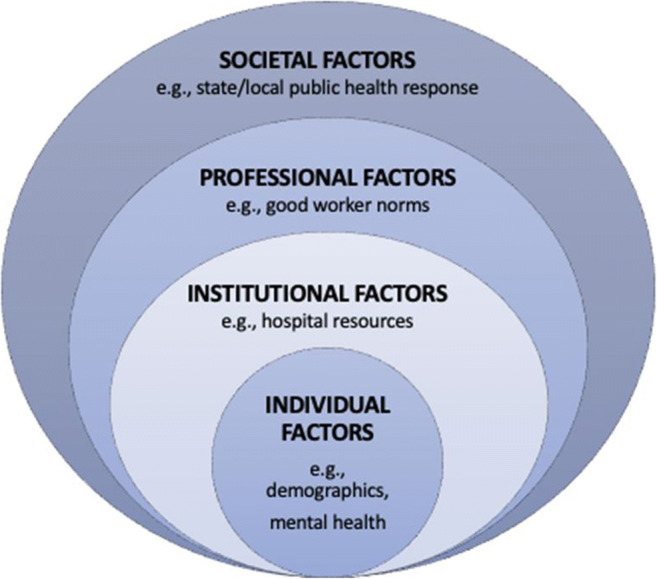
Conceptual model
Data Collection
Participants were recruited with assistance from local consultants, using direct email solicitations and snowball sampling. Eligible participants were hospital-based attending physicians and fellows who spent at least 4 weeks caring for COVID-19 patients as of March 2020. We recruited a purposive sample of physicians from a balanced range of institutional types and sizes, specialties, career stages, and demographic backgrounds.
Interviews were conducted confidentially over Zoom by MB and TJ, PhD-trained social scientists with expertise in qualitative methods, and AB, a PhD student whom they trained and supervised. The semi-structured interview guide covered five domains: personal background; crisis onset; institutional practices and policies; working during the pandemic, including stressors encountered; and personal wellbeing. (See eTable 1.) Interviews lasted approximately 60–90 min; no video was collected. Audio-recordings were professionally transcribed and deidentified by a team member. Interviews were completed between February and July 2021 for NYC and May and October 2021 for NOLA.
Qualitative Analysis
Transcripts were coded using a qualitative descriptive approach.45 A structured coding dictionary was developed using an iterative process and a combination of a priori and inductively generated themes. (See eTable 2.) MB created an initial draft of the coding dictionary using codes derived from the interview guide and emergent themes from an initial review of transcripts. The coding dictionary was refined iteratively with team member suggesting additional codes once coding began.
Using Dedoose qualitative data analysis software,46 we assigned codes to “chunks” (clusters of phrases or sentences) of text that matched the code definition. During an initial training period, the first 10 transcripts (9%) were coded by at least two coders from the coding team. Discrepancies were discussed in team meetings to ensure that understandings of concepts and codes were uniform, and all conflicts were resolved through consensus. The coding dictionary was revised repeatedly to ensure shared understanding of code definitions. The remaining transcripts were coded by one of five coders, following a set of procedures developed to maintain consistency across coders and ensure analytic rigor. (See eTable 3.) A portion of these transcripts (7/69, 10%) were reviewed by a second coder for accuracy. Instances of uncertainty were discussed with the full team until a decision was reached.
Following coding, we examined coding reports to identify patterns and relationships between themes. We also undertook a qualitative content analysis47 of responses to a single interview question, “What have been some of the most challenging stressors you experienced while working during the pandemic?” and associated code (“challenges”). Participants’ responses were organized into thematic categories by two members of the team according to our conceptual model. Frequencies for each category were tabulated.
Data analysis took place between October 2021 and February 2022. Our presentation of findings follows the consolidated criteria for reporting qualitative research (COREQ) guidelines.48
Results
The final sample included 46 women (58%) and 33 men (42%). Most participants were under 50 years old (n=67, 85%), white (n=62, 79%), and non-Hispanic (n=75, 95%). Participants specialized in hospital medicine (n=29, 37%), emergency medicine (n=19, 24%), pulmonary/critical care (n=18, 23%), palliative care (n=5, 6%), and other specialties redeployed for COVID-19 care (n=8, 10%), with an average of 9.8 years practicing medicine. (See Table 1.) Approximately one-fourth (n=19) of participants held a leadership position at the time of the interview. Participants worked at a total of 14 hospitals in NYC and 9 in NOLA. Roughly half (n=42) of participants worked in academic hospitals, with the remainder split between public (n=21, 27%) and community (n=17, 22%) hospitals; 30 participants (38%) worked in safety net hospitals. (See Table 2.)
Table 1.
Demographic characteristics
| Participant characteristics (n = 79) | n (%) |
|---|---|
| Age (%) | |
| 30–39 | 34 (43.0) |
| 40–49 | 33 (41.8) |
| 50–64 | 11 (13.9) |
| 65+ | 1 (1.3) |
| Gender (%) | |
| Female | 46 (58.2) |
| Male | 33 (41.8) |
| Race (%) | |
| White | 62 (78.5) |
| Black or African American | 2 (2.5) |
| Asian | 15 (19.0) |
| Ethnicity (%) | |
| Non-Hispanic | 75 (94.9) |
| Hispanic | 4 (5.1) |
| Medical specialty (%) | |
| Internal medicine/hospital medicine | 29 (36.7) |
| Emergency medicine | 19 (24.1) |
| Pulmonary/critical care | 18 (22.8) |
| Palliative care | 5 (6.3) |
| Other (redeployed) | 8 (10.1) |
| Mean years practicing medicine post-residency | 9.8 |
Table 2.
Characteristics of participants’ primary hospital workplaces
| New York City (n=40) n (%) | New Orleans (n=39) n (%) | Total n (%) | |
|---|---|---|---|
| Hospital type* | |||
| Academic | 18 (45.0) | 23 (5.0) | 41 (51.9) |
| Community | 7 (17.5) | 10 (25.6) | 17 (21.5) |
| Public | 15 (37.5) | 6 (15.4) | 21 (26.6) |
| Hospital funding structure† | |||
| Voluntary nonprofit | 25 (62.5) | 19 (48.7) | 44 (55.7) |
| Proprietary | 0 (0) | 13 (33.3) | 13 (16.5) |
| Governmental (city, federal) | 15 (37.5) | 7 (18.0) | 22 (27.9) |
| Safety net status‡ | 20 (50.0) | 10 (25.6) | 30 (38.0) |
| Hospital bed count | |||
| 0–200 | 2 (5.0) | 12 (30.8) | 14 (17.7) |
| 201–700 | 9 (22.5) | 17 (43.6) | 26 (32.9) |
| 701–1000 | 23(57.5) | 10 (25.6) | 33 (41.8) |
| 1001+ | 6 (15.0) | 0 (0) | 6 (7.6) |
*Academic hospitals are research hospitals affiliated with medical schools that operate as the primary hospital site for graduate medical education; community hospitals may or may not be affiliated with medical schools, and offer minimal-to-no graduate medical education; public hospitals are publicly funded institutions supported by federal, state, and local governments
†Voluntary nonprofit hospitals are owned and operated by nonprofit associations, such as churches and universities; proprietary hospitals are privately owned for-profit hospitals owned by corporations; governmental hospitals are those that are solely funded by federal, state, and local governments
‡Safety net hospitals are obligated to provide care to patients regardless of patients’ insurance status or ability to pay
Forty-five percent (n=35) of respondents reported some form of mental distress during the pandemic. More women (n=27) than men (n=8) reported mental distress; this difference was statistically significant, according to a chi-square test (p=.0007).
Most participants listed multiple stressors as “most challenging.” Altogether, participants identified 236 stressors as most challenging, with each participant identifying three stressors (on average) as most challenging. (See Table 3.) The top-cited concerns included concerns about viral exposure and/or transmission to one’s family (n=48), medical uncertainty and suboptimal care (n=30), caring for patients without family support (n=15), volume of deaths (n=14), and workload (n=14). These frequencies only reflect participants’ assessments of what was “most” challenging; the majority of participants reported most of these stressors at other points in the interview. In what follows, we present key findings at each level of the conceptual model. Exemplary quotations are reported in Table 4.
Table 3.
Responses to the question: “What have been some of the most challenging stressors you experienced while working during the pandemic?”*
| Level of conceptual model | Frequency of responses | Subthemes |
|---|---|---|
| Individual | 84 | Concerns about viral exposure and/or transmission to family (n=48) |
| Social isolation (n=12) | ||
| Balancing work and family responsibilities, including childcare and remote schooling (n=10) | ||
| Burnout and fatigue (n=4) | ||
| Discomfort of wearing PPE (n=4) | ||
| Friends not taking COVID seriously enough (n=3) | ||
| Other miscellaneous responses (n=3) | ||
| Institutional | 55 | Volume of deaths/burden of deaths (n=14) |
| Volume of patients/workload (n=14) | ||
| Resources constraints (n=8) | ||
| Constantly evolving work conditions (n=5) | ||
| Policies (e.g., quarantine, testing, PPE) (n=3) | ||
| Poor leadership (n=2) | ||
| Working in unfamiliar area (redeployment) (n=2) | ||
| Working in the ED (not set up well for COVID) (n=2) | ||
| Other miscellaneous responses (n=5) | ||
| Professional | 64 | Medical uncertainty/suboptimal care (n=30) |
| Caring for patients without family support (n=15) | ||
| Concern for healthcare worker colleagues (n=11) | ||
| Intubation decisions (n=4) | ||
| Conflict with colleagues (n=3) | ||
| Stressful patient interactions (n=1) | ||
| Societal | 33 | Mistrust toward physicians/COVID skepticism (n=11) |
| Uncertainty around course of pandemic (n=8) | ||
| Frustration with the public (n=6) | ||
| Frustration with CDC response and guidelines (n=3) | ||
| Poor federal leadership (n=2) | ||
| Other miscellaneous responses (n=3) |
*Frequencies reflect responses to this interview question and do not represent the total number of participants who endorsed each stressor during the interview. Responses total more than 79 because participants could identify more than one stressor as “most challenging”
Table 4.
Themes and exemplary quotations
| Subtheme | Exemplary quotation |
|---|---|
| Individual | |
| Age, experience, and life stage | “These are all lessons that I learned in my first eight years through H1N1, through losing young lung transplant patients with cystic fibrosis. You know, total tragedies, the patients you never forget. The … mom who’s exactly your age with a 2-year-old who dies 28 days post-transplant…You’ve kind of been through this on a smaller scale with other diseases and you apply that experience and that toughness to COVID. So I think I managed pretty well.” (0102, male, pulmonary critical care, academic hospital, NYC) |
| Institutional | |
| Resource disparities | “The grapevine word was that there’s another hospital organization in town that had a lot more money than we did, and they scooped up a lot of the resources pretty quickly, and so then it took us longer to find the resources that we needed in terms of the equipment” (0225, female hospitalist, academic hospital, NOLA) |
| “There was a dichotomy between private institutions and public institutions. For example, my institution worked with a lot of private institutions to give them ventilators that they weren’t using and all of that. They didn’t do the same thing for the public hospitals. And I think it created that ‘the tale of two cities’ that often is the reference to the way that this crisis was managed, and other crises as well. That if you’re poor, you live in certain neighborhood and all of that, you’re going to receive poor care.” (0106, male, pulmonary critical care, academic hospital, NYC) | |
| Institutional size | “During the peak, when it wasn’t just hanging out, and we did feel threatened, that lack of leadership just destroyed everybody. Yeah, I think, full-on anger looking at [how] they used shower curtains to separate the patients at one point. It was this running joke, we’re a, you know, multi-hundred-million-dollar company, a billion-dollar [company] and we got shower curtains? … It’s a very corporate institution, so I don’t think anyone felt comfortable, even you know, [saying] ‘This isn’t right.’” (0120, male, emergency medicine, academic hospital, NYC) |
| “The hospital administration was still a little removed from what was truly happening on the floors. And we could notice that in their delayed response in allocating resources and adjusting to the acute needs. Whereas I feel like the divisions within the hospital that are truly taking care of patients just rapidly came up with redesigning in how we have to manage patients and how to manage our workflows.” (0107, female, hospitalist, academic hospital, NYC) | |
| Institutional policies | “Our visitation policy right now is two people per day. And then if it’s truly end of life, four can come in, which we’ve…been negotiating against because we’ve been holding this four-person thing as, ‘Well, if you say the word comfort care, we will let more people in.’ It’s like this dangling carrot which we kind of felt like we were holding them hostage.” (0205, female, pulmonary critical care, academic hospital, NOLA |
| Professional | |
| Informal rationing | “I think that was pretty distressing, certainly for me, and probably for other clinicians, where they felt like either they were implicitly rationing care, or they weren’t providing the usual level of care that they’re accustomed to providing.” (0115, male, hospitalist, public hospital, NYC) |
| Medical uncertainty | “There is a real struggle because I wanted to provide that reassurance and because I couldn’t, I felt like I was not being a good doctor. If I provided inaccurate reassurance or concern or whatever, I think it was magnified because of the sheer amount of fear I saw on my patients’ faces and the voices or faces of their families when we called or FaceTimed them. And there was this definite erosion in my sense that…I knew what I was doing.” (0129, male, hospitalist, academic hospital, NYC) |
| Concern for colleagues | “We had some nurses who were terrified to take care of the patients and it was palpable. And so, to what degree do I force them to adhere to the standards that they would normally do, and to get in the patient’s room and really take care of the patient?” (0219, male, pulmonary critical care, community hospital, NOLA) |
| Specialty differences | “Most ERs throughout the country had decreased volume. And any non-academic ones are run like corporate groups, like businesses. So if you’re extra staff, they just furloughed, so the ER doctors are getting furloughed across the country. So now suddenly, everyone’s morale’s down, you’re a beaten dog, you’re at your employer’s mercy, but then you’re also were like, ‘But I have a job. So I’m just gonna, now, shut up and be happy at least I’m employed.’” (0120, male, emergency medicine, academic hospital, NYC) |
| Societal | |
| Federal response | “I feel like when we’re kids, we’re told that America is special, right? American exceptionalism. We may not have the fastest trains, but we are the greatest country. And I feel like I woke up from a dream about that.” (0116, male, emergency medicine, community hospital, NYC) |
| COVID politics | “I think social media really created a lot of stress for all of us because...say you just had the worst day of your life. And then you come home and you’re reading someone’s Facebook post about how COVID isn’t real and doctors are getting paid for COVID. … I think it was that kind of stuff that would cause stress.” (0214, female, pulmonary critical care, academic hospital, NOLA) |
| Societal inequalities | “We also have a lot of undocumented people … So I think that kind of feels sad and upsetting that my patients can’t get the same care as other people. … I think I have more feelings during the beginning when I’m worried about whether someone is gonna get really sick or not than when I’m like, oh, they’re probably not gonna make it.” (0133, female, hospitalist, public hospital, NYC) |
Individual Level
Age and years of clinical experience mattered for how physicians weathered the challenges of COVID-19, with more experienced physicians sometimes reporting that practicing medicine during earlier crises (e.g., onset of the HIV/AIDS epidemic, Hurricane Katrina in NOLA, September 11 in NYC) had prepared them for the pandemic: “I saw a lot of people die of AIDS…probably as many as I [have seen] die of COVID” (0139, female hospitalist, public hospital, NYC). In contrast, more junior physicians did not have as much experience to draw on: “I was so quick out of residency…I was still learning how to do this on my own. That was a challenging part for me, too” (0212, female hospitalist, community hospital, NOLA). Participants had varying levels of concern about viral exposure and transmission depending on who lived with them at home, with parents of young children and pregnant women reporting the most stress.
Institutional Level
Institutional factors had consequences for how individual physicians experienced stressors. Participants reported disparities in resource constraints between different hospital types, with public hospitals, particularly in NYC, facing more dire conditions: “We were a public hospital, we were already really screwed before this even started. And [that] really added to that feeling of, the public system is just not supported. And our mortality rates and how our patients do is 100% affected by the fact that we already don’t have enough nurses” (0133, female, hospitalist, public hospital, NYC). As this comment suggests, these differences mattered to patient care, which in turn had consequences for physicians’ stress levels. One physician teared up in describing how her hospital “pulled one name out of a hat every day” to decide who got convalescent plasma, whereas patients at a local academic hospital had better access (0119, female, emergency medicine, public hospital, NYC; She acknowledged that this treatment was ultimately ineffective).
Several NYC participants acknowledged that their hospitals’ location in low-income neighborhoods contributed to disparities in patient outcomes. Importantly, COVID-19 accentuated preexisting disparities between institutions. However, public hospital employees were already accustomed to working in conditions of scarcity. Participants in NOLA more frequently described sharing resources across institutions to mitigate disparities. One participant noted, “That was one of the amazing things, just the connectivity and sharing between physicians around town that I never experienced before” (0209, female, emergency medicine, public hospital, NOLA).
Hospital size also shaped the extent to which hospital leadership was perceived to be in touch with physicians’ experiences. Some physicians who worked in smaller hospitals reported that leaders were more accessible to frontline healthcare workers: “We know them [our CMO and CEO] and they’re in touch with us. And I felt like they were genuinely doing the best that they could” (0218, female, emergency medicine, public hospital with under 200 beds, NOLA). In contrast, the emphasis on public image management at larger institutions was often disjunctive with physicians’ actual experiences of patient care.
Policies regarding testing and quarantine, PPE distribution, and visitation produced stress at the institutional level. Across the sample, policies restricting hospital visitors produced the most stress. Participants also acknowledged that such policies were necessary, and in some cases were dictated by state-level policies. Overall, physicians in NOLA reported more distress due to visitation policies.
Professional Level
The professional level of our conceptual model refers to the professional norms, knowledge, and cultures that shape physician wellbeing. A major stressor at this level entailed what many described as inadequate care for patients with COVID-19, particularly early on. Many participants described feeling helpless, which undermined their sense of professional self-efficacy. The need for informal rationing cut against participants’ medical training and raised crises of professional integrity. Uncertain medical knowledge created questions about whether one had “done everything” clinically, leading to self-doubt: “It certainly [put] me sort of in a crisis of confidence in terms of being a doctor, not knowing what to do for those patients” (0209, female, emergency medicine, public hospital, NOLA). Such feelings were particularly pronounced for junior physicians: “I just graduated residency two years ago. So I’m a by-the-book doctor because I just took my Boards. And then all of a sudden, you’re telling me, ‘Okay, forget all that. You can’t do anything.’ Yeah, it’s incredibly stressful” (0210, female hospitalist, academic hospital, NOLA). Physicians with more experience working in poorly resourced hospitals reported less stress surrounding this challenge.
Concern for other healthcare workers was also a source of stress, particularly for participants with teaching and leadership responsibilities. Participants worried most frequently about nursing colleagues, who had more frequent contact with COVID-19 patients, and trainees, who were seen as especially vulnerable given their limited clinical experience and low-status in the medical hierarchy: “I also feel incredible responsibility as an attending [for] the wellbeing of residents and fellows who just don’t have the experience and just don’t have such thick skin of having seen young patients die” (0102, male critical care pulmonologist, academic hospital, NYC).
Some variation among participating specialties was identified, with emergency medicine physicians, particularly those at public and community hospitals, reporting greater resource constraints, reduced work hours, and job insecurity than physicians in other specialties.
Societal Level
Participants from both cities noted that they had access to more resources (e.g., essential medical supplies) because their cities were hit first and hard. Nevertheless, many still felt abandoned by the federal government, criticizing the confusing public health messaging and lack of federal leadership. Disillusionment was strongest among NYC physicians who worked in public hospitals: “It felt just over and over again as if we were just sort of left out to hang, like hung out to dry” (0119, female, emergency medicine, public hospital, NYC). Some NOLA participants mentioned the politicization of COVID-19 as a source of stress, explaining that interacting with families who distrusted science and disputed the reality of COVID-19 was frustrating and demoralizing: “Now I’m just angry because my job is to provide guidance and the most up-to-date information about the science and then I’m just getting yelled at about it” (0236, female, pulmonary critical care, community hospital, NOLA). One NOLA participant decided to leave the South because of the political climate around COVID-19.
Several participants expressed distress over the social inequalities that led to an uneven burden of COVID-19, particularly in NYC, where overcrowded households and neighborhood-level differences contributing to COVID-19 disparities were more palpable than in NOLA. These NYC participants recognized that they discharged patients from the hospital into suboptimal conditions for isolating from family members, “lighting the fuses for it to get worse” (0120, male, emergency medicine, academic hospital, NYC).
Relationships Across Levels
We have separated our reporting of stressors and protective factors at each level of our conceptual model for heuristic purposes, but findings reflect overlap and intersections across levels. Several NYC participants acknowledged that their hospital (institutional level) was located in a low-income neighborhood (societal level), exacerbating resource constraints and associated stressors. Insofar as inequalities at the neighborhood level shaped the hospital’s ability to respond to surge conditions, institutional and societal level stressors intersected, particularly in the hardest hit (i.e., most socioeconomically disadvantaged) areas of NYC. Hospital visitation policies (institutional level) likewise unsettled norms of patient care (professional level) that enlist family support. Communicating with families who distrusted science and thought COVID-19 was a hoax (societal level) disrupted physician norms against resenting patients (professional level). The job security of emergency medicine physicians (professional level) was particularly threatened for those working in under-resourced public hospitals (institutional level). These stressors, in turn, may contribute to physicians’ stress at the individual level. For example, one participant indicated that racial disparities in COVID-19 (societal level) were a significant source of personal distress because he is African American (individual level).
Discussion
This qualitative interview study of frontline physicians in New York City and New Orleans during the COVID-19 pandemic identified multiple factors shaping physicians’ occupational stress including individual-level factors such as age, work experience, and life stage; institutional-level factors such as resource disparities, institutional type and size, and institutional policies; professional-level factors such as informal rationing, medical uncertainty, concern for colleagues, and differences between specialties; and societal-level factors such as the federal response, COVID politics, and societal inequalities. When asked to identify which stressors had been most challenging, physicians reported a wide range of stressors at each of these levels, with the largest number of stressors falling into the individual level. Systems factors within and across the four levels worked in combination to shape physicians’ experiences of stress at the individual level.
By providing rich, descriptive information about how physicians perceived the relationships between their working conditions and individual experiences of stress during the COVID-19 pandemic, this article adds to a growing body of literature that responds to the National Academies of Medicine’s call to conceptualize occupational stress and burnout as shaped by multidimensional systems factors.3 At the individual level, this study adds nuance to quantitative evidence that burnout tends to be higher in younger and female physicians.49,50At the institutional level, it provides contextual detail regarding how clinical work environments may become drivers of job dissatisfaction and burnout.51–53 It also bolsters the importance of frequently reassessing institutional policies to eliminate those that create strain in the work environment,19 and sometimes lead to moral distress.23,54,55 At the professional level, our findings support recent calls for culture change in medicine to support clinical wellbeing by respecting work-life boundaries, prioritizing clinician self-care, and developing adaptive leadership capacity.19,51,56,57 Finally, our findings suggest that physicians are affected by upstream social and political societal stressors that have been less well explored in the clinician burnout literature. Participants appreciated the equity-oriented ethos of some institutional cultures, in which scarce medical resources were shared with neighboring hospitals, suggesting that opportunities for sharing and connection across institutions could help foster more equitable care despite societal stressors, and by extension, potentially cultivate wellbeing and decrease burnout.
This study has several limitations. The pandemic had been ongoing for between 12 and 20 months at the time of the interview; interview data may have been affected by recall bias. The qualitative data may also reflect selection bias, insofar as participants who agreed to participate in the interview study may not represent all physicians. While interviews were conducted with physicians working in a diverse range of hospitals in two large US cities in different regions, findings may not be generalizable to other areas of the USA. The categorization of participants’ “most challenging” stressors into one of four analytic levels may have been subject to coder bias. Finally, the course of the pandemic evolved throughout the data collection process. Interviews provide a snapshot of the pandemic at a particular timepoint, which varied among participants from periods of relative calm to surge conditions. Several NOLA participants were interviewed at the beginning of the Delta variant surge. This may make it challenging to compare some findings from this cross-sectional study.
These limitations are offset by the study’s numerous strengths, including our comparative approach, which included physicians from two cities working in 23 hospitals. Most qualitative studies conducted during COVID-19 have focused on a single city or institution.42,43,58,59 Additional strengths include our attention to systems factors shaping physicians’ stress, particularly our inclusion of professional level factors, which have not been acknowledged in other socio-ecological models of physicians’ wellbeing,3,60 and the analytic generalizability of our conceptual model.61
Conclusion
This qualitative study of 79 physicians who provided care for hospitalized COVID-19 patients contributes to an emergent literature on systems-based approaches to occupational stress and burnout among physicians by demonstrating the intersections between societal conditions, professional cultures, institutional work environments, and individual stress. The study’s novel contributions include (1) its multi-sited comparative design, which identified differences among physicians practicing in different hospital types and neighborhoods, and (2) its description of how upstream, extra-institutional sociopolitical factors affect physicians’ perceptions of workplace stress. Findings from semi-structured interview suggest that interventions to reduce physician stress and burnout may be more effective if they target systems factors and stressors at multiple levels.
Supplementary information
(DOCX 23 kb)
Acknowledgements
The authors are grateful to Sara Feinstein and Laila Knio for assistance with qualitative coding, and to the members of the STEPPS expert advisory board for guidance and support throughout the study: Lilia Cervantes, Nadia Charguia, Barak Gaster, Theodore Iwashyna, Dhruv Khullar, Robert K. McLellan, Aimee Milliken, Erika Sabbath, Helene Starks, Julia Szymczak.
Funding
This study was supported by a grant from the Greenwall Foundation.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shanafelt TD, Boone S, Tan L, et al. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General US Population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Burn-out an “Occupational Phenomenon”: International Classification of Diseases. Published 2019. https://www.who.int/mental_health/evidence/burn-out/en/
- 3.National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Wellbeing. Published online 2019. 10.17226/25521 [PubMed]
- 4.Price G, Seligson R, Hollister R. 2021 Survey of America’s Physicians COVID-19 Impact Edition: A Year Later. The Physicians Foundation; 2021.
- 5.Melnikow J, Padovani A, Miller M. Frontline Physician Burnout During the COVID-19 Pandemic: National Survey Findings. BMC Health Services Research. 2022;22:365. doi: 10.1186/s12913-022-07728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NIHCM Foundation. Physician Burnout & Moral Injury: The Hidden Health Care Crisis.; 2021. Accessed March 23, 2021. https://nihcm.org/publications/physician-burnout-suicide-the-hidden-health-care-crisis?utm_source=NIHCM+Foundation&utm_campaign=feebfc4834-03222021_Physician_Burnout_Infographic&utm_medium=email&utm_term=0_6f88de9846-feebfc4834-167854680
- 7.Amin F, Sharif S, Saeed R, Durrani N, Jilani D. COVID-19 Pandemic- Knowledge, Perception, Anxiety and Depression Among Frontline Doctors of Pakistan. BMC Psychiatry. 2020;20:459. 10.1186/s12888-020-02864-x [DOI] [PMC free article] [PubMed]
- 8.AlAteeq DA, Aljhani S, Althiyabi I, Majzoub S. Mental Health Among Healthcare Providers During Coronavirus Disease (COVID-19) Outbreak in Saudi Arabia. J Infect Public Health. 2020;13(10):1432-1437. 10.1016/j.jiph.2020.08.013 [DOI] [PMC free article] [PubMed]
- 9.Thomaier L, Teoh D, Jewett P, et al. Emotional Health Concerns of Oncology Physicians in the United States: Fallout During the COVID-19 Pandemic. PLoS One. 2020;15(11):e0242767. 10.1371/journal.pone.0242767 [DOI] [PMC free article] [PubMed]
- 10.Vilovic T, Bozic J, Vilovic M, et al. Family Physicians’ Standpoint and Mental Health Assessment in the Light of COVID-19 Pandemic—A Nationwide Survey Study. Int J Environ Res Public Health. 2021;18(4):2093. doi: 10.3390/ijerph18042093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American College of Emergency Physicians. Mental Health among Emergency Physicians. Morning Consult. October 2020.
- 12.Dolev T, Zubedat S, Brand Z, et al. Physiological Parameters of Mental Health Predict the Emergence of Post-Traumatic Stress Symptoms in Physicians Treating COVID-19 patients. Transl Psychiatry. 2021;11:169. 10.1038/s41398-021-01299-6 [DOI] [PMC free article] [PubMed]
- 13.Ferreira LC, Amorim RS, Melo Campos FM, Cipolotti R. Mental Health and Illness of Medical Students and Newly Graduated Doctors During the Pandemic of SARS-Cov-2/COVID-19. PLoS One. 2021;16(5):e0251525. 10.1371/journal.pone.0251525 [DOI] [PMC free article] [PubMed]
- 14.Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental Health of Staff Working in Intensive Care During COVID-19. Occup Med (Lond). Published online January 13, 2021:kqaa220. 10.1093/occmed/kqaa220 [DOI] [PMC free article] [PubMed]
- 15.West CP, Dyrbye LN, Sinsky C, et al. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Network Open. 2020;3(7):e209385. doi: 10.1001/jamanetworkopen.2020.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Panagioti M, Panagopoulou E, Bower P, et al. Controlled Interventions to Reduce Burnout in Physicians A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177(2):195-205. 10.1001/jamainternmed.2016.7674 [DOI] [PubMed]
- 17.Goroll AH. Addressing Burnout—Focus on Systems, Not Resilience. JAMA Netw Open. 2020;3(7):e209514. doi: 10.1001/jamanetworkopen.2020.9514. [DOI] [PubMed] [Google Scholar]
- 18.Carayon P, Cassel C, Dzau VJ. Improving the System to Support Clinician Well-being and Provide Better Patient Care. JAMA. 2019;322(22):2165–2166. doi: 10.1001/jama.2019.17406. [DOI] [PubMed] [Google Scholar]
- 19.Sinsky CA, Biddison LD, Mallick A, et al. Organizational Evidence-Based and Promising Practices for Improving Clinician Well-Being. NAM Perspect. Published online 2020:10.31478/202011a. [DOI] [PMC free article] [PubMed]
- 20.Vercio C, Loo LK, Green M, Kim DI, Beck Dallaghan GL. Shifting Focus from Burnout and Wellness toward Individual and Organizational Resilience. Teaching and Learning in Medicine. 2021;33(5):568–576. doi: 10.1080/10401334.2021.1879651. [DOI] [PubMed] [Google Scholar]
- 21.Shapiro DE, Duquette C, Abbott LM, Babineau T, Pearl A, Haidet P. Beyond Burnout: A Physician Wellness Hierarchy Designed to Prioritize Interventions at the Systems Level. Am J Med. 2019;132(5):556-563. 10.1016/j.amjmed.2018.11.028 [DOI] [PubMed]
- 22.De Simone S, Vargas M, Servillo G. Organizational Strategies to Reduce Physician Burnout: A Systematic Review and Meta-Analysis. Aging Clinical and Experimental Research. 2021;33:883-894. [DOI] [PubMed]
- 23.Hlubocky FJ, Symington BE, McFarland DC, et al. Impact of the COVID-19 Pandemic on Oncologist Burnout, Emotional Well-Being, and Moral Distress: Considerations for the Cancer Organization’s Response for Readiness, Mitigation, and Resilience. JCO Oncol Pract. 2021;17(7):365–374. doi: 10.1200/OP.20.00937. [DOI] [PubMed] [Google Scholar]
- 24.Tebes JK, Awad MN, Connors EH, et al. The Stress and Resilience Town Hall: A Systems Response to Support the Health Workforce During COVID-19 and Beyond. General Hospital Psychiatry. 2022;77:80-87. 10.1016/j.genhosppsych.2022.04.009 [DOI] [PMC free article] [PubMed]
- 25.Dillon EC, Tai-Seale M, Meehan A, et al. Frontline Perspectives on Physician Burnout and Strategies to Improve Well-Being: Interviews with Physicians and Health System Leaders. J Gen Intern Med. 2020;35(1):261-267. [DOI] [PMC free article] [PubMed]
- 26.Mehta A, Lockhart S, Reed K, et al. Drivers of Burnout Among Critical Care Providers: A Multicenter Mixed-Methods Study. Chest. 2021;161(5):1263-1274. [DOI] [PMC free article] [PubMed]
- 27.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship Between Clerical Burden and Characteristics of the Electronic Environment With Physician Burnout and Professional Satisfaction. Mayo Clinic Proceedings. 2016;91(7):836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 28.Sonis J, Pathman DE, Read S, et al. Effects of Healthcare Organization Actions and Policies Related to COVID-19 on Perceived Organizational Support Among U.S. Internists: A National Study. Journal of Healthcare Management. 2022;67(3):192–205. doi: 10.1097/JHM-D-21-00208. [DOI] [PubMed] [Google Scholar]
- 29.Vindrola-Padros C, Andrews L, Dowrick A, et al. Perceptions and Experiences of Healthcare Workers During the COVID-19 Pandemic in the UK. BMJ Open. 2020;10(11):e040503. 10.1136/bmjopen-2020-040503 [DOI] [PMC free article] [PubMed]
- 30.Wahlster S, Sharma M, Lewis AK, et al. The Coronavirus Disease 2019 Pandemic’s Effect on Critical Care Resources and Health-Care Providers. Chest. 2021;159(2):619–633. doi: 10.1016/j.chest.2020.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Afonso AM, Cadwell JB, Staffa SJ, Zurakowski D, Vinson AE. Burnout Rate and Risk Factors among Anesthesiologists in the United States. Anesthesiology. 2021;134(5):683–696. doi: 10.1097/ALN.0000000000003722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Ghunaim TA, Johnson J, Biyani CS, O’Connor D. Psychological and Occupational Impact of the COVID-19 Pandemic on UK Surgeons: A Qualitative Investigation. BMJ Open. 2021;11(4):e045699. 10.1136/bmjopen-2020-045699 [DOI] [PMC free article] [PubMed]
- 33.Uyaroğlu OA, Başaran NÇ, Ozisik L, et al. Evaluation of the Effect of COVID-19 Pandemic on Anxiety Severity of Physicians Working in the Internal Medicine Department of a Tertiary Care Hospital: A Cross-Sectional Survey. Intern Med J. 2020;50(11):1350-1358 [DOI] [PMC free article] [PubMed]
- 34.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, Prevention, and Management of the Psychological Effects of Emerging Virus Outbreaks on Healthcare Workers: Rapid Review and Meta-Analysis. BMJ. 2020;369:m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed]
- 35.Kang L, Ma S, Chen M, et al. Impact on Mental Health and Perceptions of Psychological Care Among Medical and Nursing Staff in Wuhan During the 2019 Novel Coronavirus Disease Outbreak: A Cross-Sectional Study. Brain Behav Immun. 2020;87:11-17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed]
- 36.Song X, Fu W, Liu X, et al. Mental Health Status of Medical Staff in Emergency Departments During the Coronavirus Disease 2019 Epidemic in China. Brain Behav Immun. 2020;88:60-65. 10.1016/j.bbi.2020.06.002 [DOI] [PMC free article] [PubMed]
- 37.Khatun F, Parvin F, Rashid M, et al. Mental Health of Physicians During COVID-19 Outbreak in Bangladesh: A Web-Based Cross-Sectional Survey. Front Public Health. 2021;9:592058. 10.3389/fpubh.2021.592058 [DOI] [PMC free article] [PubMed]
- 38.Sanghavi PB, Au Yeung K, Sosa CE, Veesenmeyer AF, Limon JA, Vijayan V. Effect of the Coronavirus Disease 2019 (COVID-19) Pandemic on Pediatric Resident Well-Being. J Med Educ Curric Dev. 2020;7:2382120520947062. doi: 10.1177/2382120520947062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Portoghese I, Meloni F, Galletta M, et al. Concerns, Perceived Impact, Preparedness in Coronavirus Disease (COVID-19) Pandemic and Health Outcomes among Italian Physicians: A Cross-Sectional Study. J Prim Care Community Health. 2021;12:21501327211000244. doi: 10.1177/21501327211000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shahbaz S, Ashraf MZ, Zakar R, Fischer F. Psychosocial, Emotional and Professional Challenges Faced by Gemale Healthcare Professionals During the COVID-19 Outbreak in Lahore, Pakistan: A Qualitative Study. BMC Womens Health. 2021;21:197. 10.1186/s12905-021-01344-y [DOI] [PMC free article] [PubMed]
- 41.Butler CR, Wong SPY, Vig EK, Neely CS, O’Hare AM. Professional Roles and Relationships During the COVID-19 Pandemic: A Qualitative Study among US Clinicians. BMJ Open. 2021;11:e047782. [DOI] [PMC free article] [PubMed]
- 42.Rao H, Mancini D, Tong A, et al. Frontline Interdisciplinary Clinician Perspectives on Caring for Patients with COVID-19: A Qualitative Study. BMJ Open. 2021;11(5):e048712. 10.1136/bmjopen-2021-048712 [DOI] [PMC free article] [PubMed]
- 43.Norful AA, Rosenfeld A, Schroeder K, Travers JL, Aliyu S. Primary Drivers and Psychological Manifestations of Stress in Frontline Healthcare Workforce During the Initial COVID-19 Outbreak in the United States. General Hospital Psychiatry. 2021;69:20-26. 10.1016/j.genhosppsych.2021.01.001 [DOI] [PMC free article] [PubMed]
- 44.Sofaer S. Qualitative Methods: What Are They and Why Use Them? Health Serv Res. 1999;34(5 Pt 2):1101-1118. [PMC free article] [PubMed]
- 45.Sandelowski M. Whatever Happened to Qualitative Description? Research in Nursing and Health. 2000;23:334-340. [DOI] [PubMed]
- 46.SocioCultural Research Consultants, LLC. Dedoose Version 8.0.35, web application for managing, analyzing, and presenting qualitative and mixed method research data. Published online 2018.
- 47.Morgan DL. Qualitative Content analysis: A Guide to Paths Not Taken. Qualitative Health Research. 1993;3:112-121. [DOI] [PubMed]
- 48.Tong A, Sainsbury P, Craig J, Tong A, Sainsbury P, Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed]
- 49.Hoff T, Lee D. Burnout and Physician Gender: What Do We Know? Medical Care. 2021;59(8):711–720. doi: 10.1097/MLR.0000000000001584. [DOI] [PubMed] [Google Scholar]
- 50.West CP, Dyrbye LN, Shanafelt TD. Physician Burnout: Contributors, Consequences and Solutions. J Intern Med. 2018;283(6):516-529. 10.1111/joim.12752 [DOI] [PubMed]
- 51.Linzer M, Levine R, Meltzer D, Poplau S, Warde C, West CP. 10 Bold Steps to Prevent Burnout in General Internal Medicine. J Gen Intern Med. 2014;29(1):18-20. 10.1007/s11606-013-2597-8 [DOI] [PMC free article] [PubMed]
- 52.Linzer M, Poplau S, Grossman E, et al. A Cluster Randomized Trial of Interventions to Improve Work Conditions and Clinician Burnout in Primary Care: Results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30(8):1105-1111. 10.1007/s11606-015-3235-4 [DOI] [PMC free article] [PubMed]
- 53.Linzer M, Sinsky C, Poplau S, Brown R, Williams E. Joy In Medical Practice: Clinician Satisfaction In The Healthy Work Place Trial. Health Aff. 2017;36(10):1808-1814. [DOI] [PubMed]
- 54.Daubman BR, Black L, Goodman A. Recognizing Moral Distress in the COVID-19 Pandemic: Lessons From Global Disaster Response. J Hosp Med. 2020;15(11):696–698. doi: 10.12788/jhm.3499. [DOI] [PubMed] [Google Scholar]
- 55.Hines SE, Chin KH, Glick DR, Wickwire EM. Trends in Moral Injury, Distress, and Resilience Factors among Healthcare Workers at the Beginning of the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18(2):E488. doi: 10.3390/ijerph18020488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sinskey JL, Margolis RD, Vinson AE. The Wicked Problem of Physician Well-Being. Anesthesiology Clinics. 2022;40(2):213–223. doi: 10.1016/j.anclin.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McQueen SA, Mobilio MH, Moulton CA. Pulling Our Lens Backwards to Move Forward: An Integrated Approach to Physician Distress. Medical Humanities. Published online August 19, 2021. 10.1136/medhum-2020-012100 [DOI] [PubMed]
- 58.Cubitt LJ, Im YR, Scott CJ, Jeynes LC, Molyneux PD. Beyond PPE: A Mixed Qualitative–Quantitative Study Capturing the Wider Issues Affecting Doctors’ Well-being During the COVID-19 Pandemic. BMJ Open. 2021;11(3):e050223. 10.1136/bmjopen-2021-050223 [DOI] [PMC free article] [PubMed]
- 59.Liu Q, Luo D, Haase JE, et al. The Experiences of Health-care Providers During the COVID-19 Crisis in China: A Qualitative Study. The Lancet Global Health. 2020;8(6):e790-e798. 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed]
- 60.Schwartz R, Sinskey JL, Anand U, Margolis RD. Addressing Postpandemic Clinician Mental Health : A Narrative Review and Conceptual Framework. Ann Intern Med. 2020;173(12):981–988. doi: 10.7326/M20-4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yin R. Qualitative Research from Start to Finish. The Guilford Press; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 23 kb)


