Abstract
Introduction
Adverse events (AE) are an inevitable reality in healthcare, with an incidence of 7.5–14.1% worldwide. AEs are recognised to cause psychological and emotional distress in healthcare workers, with surgeons being particularly susceptible. We report the first data on the emotional impact in relation to adverse events in surgeons in the Republic of Ireland (ROI).
Methods
We distributed a web-based survey to all urology trainees in the ROI. The questionnaire focused on trainees’ personal account of AEs, their emotional response, perceived contributing factors and perceived benefit of support systems. The primary care PTSD screen (PC-PTSD-V) assessed for PTSD.
Results
A total of 16 responses were received from 12 (75%) registrars and 4 (25%) SHOs. Of the AEs reported, 12 (75%) were ≥ Clavien-Dindo 3b. Contributing factors identified included lapse of judgement (n = 6, 37.5%), risk of procedure (n = 7, 43%), lack of experience (n = 4, 25%). Anxiety (n = 8, 50%), guilt (n = 7, 44%) and sleep problems (n = 4, 25%) were the most reported emotional responses. Physical symptoms were reported in 2 (12%) trainees. A PC-PTSD-V score ≥ 3 was reported in 2 (12%) trainees. Most trainees (n = 13, 81%) reported talking to someone following the event with most (n = 12, 93%) talking to a consultant or NCHD colleague. Most respondents (n = 14, 87%) agreed that their training could better prepare them for the personal impact of AEs.
Conclusion
Surgical trainees report negative psychological and emotional responses that are consistent with second victim symptoms. Those surveyed felt that their training could better prepare them for the personal impact of such events.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11845-022-03202-8.
Keywords: Adverse events, Human factors, Psychological safety
Introduction
It is extremely important that the public, patients, media, hospital management systems and relevant regulatory bodies recognise that access to healthcare and hospital admission carries an inevitable risk of adverse events (AEs) or complications. The Irish National Adverse Events Survey (INAES) reports an incidence of AEs of 12.2% in Irish hospital admissions [1]. International figures range from 7.5–14.1% [2–4].
When an AE does occur, the primary burden is with the patient and by extension their family. The consequences of an AE can be further reaching such as the economic impact on the healthcare system, a breakdown in relationship between doctor and patient and a negative psychological impact on healthcare workers caring for that patient. Further research, and increasing recognition and analysis of the depth of the psychological impact that an AE can have upon the relevant healthcare professionals led Wu to describe that response as ‘second victim syndrome’ in 2000 [5].
More than two decades later the ‘second victim syndrome’ has been described by healthcare workers across a wide breadth of specialties and levels, with the 2021 SeViD-I survey recording that 59% of doctors surveyed had experienced ‘second victim impacts’ [6]. Looking at surgery in particular, The BISA study reported 84% of surgeons suffered an emotional toll subsequent to an AE they had been involved with [7]. While no specific clinical criteria define the ‘second victim’ symptoms, they include emotional elements such as guilt, anger, irritability and fear, and may be accompanied by physical symptoms such as tachycardia, fatigue or concentration difficulties. The extent and duration of symptoms can be variable, with reported cases of suicide, and long-term mental health impacts. The emotional impact on the physician has been shown to have a knock-on effect on other patients and the wider health system with absenteeism, repeated errors, loss of empathy or alterations in how the worker goes about their practice [8–11].
Surgeons are at a particular risk of second victim symptoms due to the invasive nature of their work combined with a frequent requirement for emergency procedures. They may take personal responsibility for events as they can observe a direct correlation between adverse outcomes and specific interventions [7, 12, 13]. Several studies have assessed surgeon’s emotional responses to AEs; however, until recently, studies of urologists were lacking [7, 14]. A recent publication by Turner et al. had responses from 80 urologists (20% of respondents) and represents the largest study of emotional responses to AEs and complications in surgeons in the United Kingdom (UK), with nearly half of respondents reporting increased anxiety in the aftermath [15]. This study was the first to differentiate between AEs and complications, with errors appearing to affect surgeons more than complications with higher rates of PTSD symptomatology.
From an Irish perspective, data on the emotional impact of AEs on doctors has not been well documented. A qualitative study of ten Irish obstetricians recognised the emotional toll of a perinatal death on the doctor, with respondents describing guilt, shock, sadness and a sense of failure [16]. More recent studies have focused on the psychological impact of the COVID-19 pandemic on healthcare workers with both reporting psychological distress in 44–45% of workers [17, 18]. All have recognised the need to provide support for healthcare workers in the aftermath of an adverse or traumatic event.
The aim of our study was to gather data on the emotional impact and potential second victim syndrome in relation to AEs with working surgeons in the Republic of Ireland. To determine what structures were in place to deal with the consequences of an AE on a surgeon, and evaluate whether there was a need to put in place some further measures.
Methods
We used a web-based questionnaire that was distributed to all urology trainees in the Republic of Ireland and asked them to participate anonymously. Respondents were asked to reflect on an AE or complication that had been part of their clinical workload within the preceding 6 months. They were requested to briefly describe it and give a Clavien-Dindo grade if applicable. The Clavien-Dindo grading system is used internationally to classify surgical complications [19].
The survey focused on physical and emotional responses to the event, potential contributing or alleviating factors and the perceived level of preparedness for the personal impact of such events (Supplementary Material).
The physical and emotional symptoms assessed were ones that are regularly described in second victim syndrome, or as those experienced in the aftermath of an AE [3, 6, 7, 11–15, 17, 18, 20–24].
The validated primary care PTSD screen (PC-PTSD-V) assessed for symptoms of post-traumatic stress disorder (PTSD). This was first described in 2016 and has been shown to be a sensitive and accurate tool to screen for symptoms of PTSD in the general population [25–27]. We used a cut-off score of 4 based on recent studies showing greater sensitivity with this cut-off [26, 27].
Data was collated and analysed using Microsoft excel.
Results
Respondent and event characteristics
A total of 16 responses were received with all levels of trainees represented (Table 1). The most representative group were specialist surgical trainees (ST) grade 5–6 (n = 7, 43.8%), the least represented were ST 3–4 (n = 1, 6%).
Table 1.
Breakdown of respondents and grades
| Grade | Number | % of total |
|---|---|---|
| ST1-2 | 4 | 25.0% |
| ST3-4 | 1 | 6.3% |
| ST5-6 | 7 | 43.8% |
| ST7-8 | 2 | 12.5% |
| Stand-alone registrar | 2 | 12.5% |
| Total | 16 | 100.0% |
Most respondents reported a Clavien-Dindo score of 3b or higher (n = 12, 75%) when reflecting on a particular AE (Fig. 1).
Fig. 1.
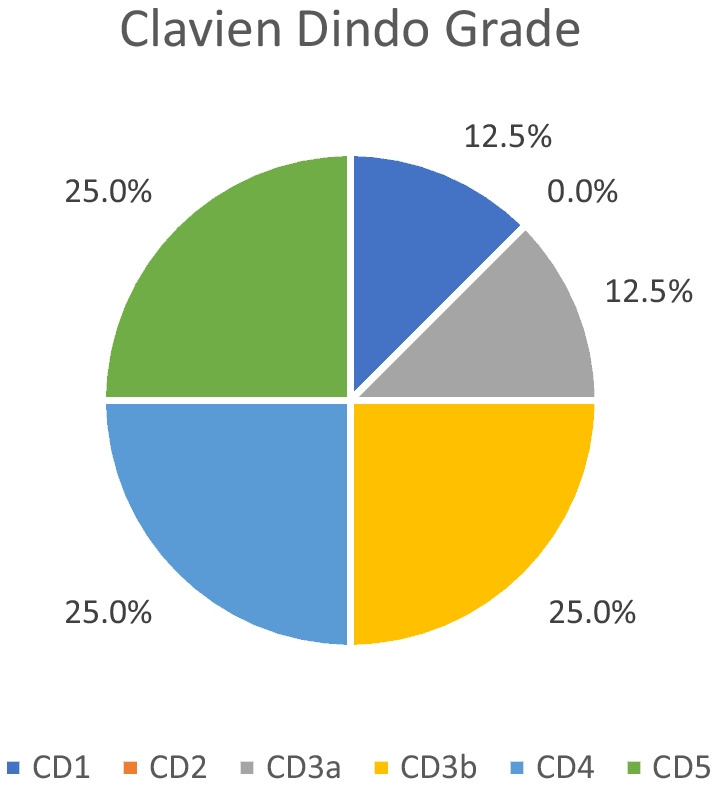
Breakdown of Responses by Clavien Dindo Grade
Physical and emotional responses
A high proportion of respondents (n = 11, 68.8%) described physical or emotional effects following the event or when reflecting on the event (Table 2). Of those who reported physical or emotional responses to the event, 7 (63%) had more than one symptom. The median PC-PTSD-V score was 0, with a range of 0–5. (Table 3). A single respondent had a PC-PTSD-V score of 4 or greater.
Table 2.
Reported physical and emotional responses because of the event or when thinking about the event
| Symptom | N | % of total |
|---|---|---|
| Anxiety | 8 | 50.0% |
| Guilt | 7 | 43.8% |
| Anger or Irritability | 2 | 12.5% |
| Low mood | 2 | 12.5% |
| Sleep problems | 4 | 25.0% |
| Impact on personal relationships | 1 | 6.3% |
| Impact on professional relationships | 1 | 6.3% |
| Alcohol consumption | 0 | 0.0% |
| Cardiovascular symptoms | 1 | 6.3% |
| Gastrointestinal problems | 1 | 6.3% |
| Headaches | 0 | 0.0% |
| Other | 1 | 6.3% |
Table 3.
PC-PSTD-5 score breakdown
| PC-PTSD-5 score | Number | % |
|---|---|---|
| 0 | 9 | 56.3% |
| 1 | 3 | 18.8% |
| 2 | 2 | 12.5% |
| 3 | 1 | 6.3% |
| 4 | 0 | 0.0% |
| 5 | 1 | 6.3% |
| Total | 16 | 100.0% |
Influencing factors
Contributing factors to the AE were reported by 14 (87.5%) of respondents. (Table 4) Two or more contributing factors were identified by 7 (50%) NCHDs.
Table 4.
Identified contributing factors
| Factor identified | Number | % of total |
|---|---|---|
| System outside control | 4 | 25.0% |
| Stress/burnout | 1 | 6.3% |
| Lack of knowledge/experience | 4 | 25.0% |
| Lack of resource | 1 | 6.3% |
| Lapse in judgement by you | 5 | 31.3% |
| Lapse in judgement by someone else | 6 | 37.5% |
| Poor communication | 2 | 12.5% |
| Recognised risk of procedure | 7 | 43.8% |
| Fatigue | 2 | 12.5% |
Coping strategies
Most respondents discussed the event with someone else as shown in Table 5 (n = 13, 81.3%). Of these, 12 (92.3%) respondents spoke to another work colleague with 1 (7.7%) speaking to friends or family. No respondents reported contacting local or national support services. When asked to rate the impact of discussing the event on a Likert scale from 1 (not at all helpful) to 5 (extremely helpful), 12 (92.3%) respondents scored > 3, implying it was beneficial. The median response was 4 with a range of 2–5. No respondents reported an increase in alcohol consumption associated with the event.
Table 5.
Respondents who discussed case with another person
| Who discussed with | N | % |
|---|---|---|
| Consultant colleague | 8 | 61.5% |
| NCHD colleague/other trainee | 4 | 30.8% |
| Friend family | 1 | 7.7% |
| Partner/spouse | 0 | 0.0% |
| Local/national support service | 0 | 0.0% |
| Total | 13 | 100.0% |
Preparedness for personal impact of adverse events
The respondents were asked to rate the influence of their training in preparing them for the personal impact of adverse patient outcomes with mixed results (Table 6). On a Likert scale of 1 (not at all prepared) to 5 (well prepared), the median score was 3 (range 1–5). Most respondents agreed with the statement that training should better prepare them for the management of AEs with all (n = 16, 100%) giving a score of > 3 on a Likert scale (1 = completely disagree, 5 = strongly agree). The median answer was 5 with a range of 3–5.
Table 6.
Responses to impact of training in preparation for emotional impact of adverse events
| Likert -scale repsonse | N | % of total |
|---|---|---|
| 1 (not all prepared) | 3 | 19% |
| 2 | 4 | 25% |
| 3 | 4 | 25% |
| 4 | 3 | 19% |
| 5 (well prepared) | 2 | 13% |
Free text comments from respondents described training as ‘minimal or non-existent’ (respondent 4) with a focus on managing ‘patients who have complications…not how we deal with complications personally’ (respondent 6). Three NCHDs described the benefit of observing or discussing with senior colleagues: ‘The best surgeons…are able to reflect and critique own performance…especially when complications happen.’ (respondent 11).
Discussion
This study was designed to investigate the personal impact of patient AEs or complications on Urology trainees in the Republic of Ireland.
Respondent and event characteristics
Although we did not differentiate on gender or age, all respondents in our survey were trainees or Non Consultant Hospital Doctors, therefore relatively early in their career. A previous German study of internal medicine physicians under the age of 35 years showed a prevalence of ‘second victim traumatic episodes’ with 59% of the respondents citing involvement in an episode [6]. Other studies have shown that experienced consultant surgeons are less likely to report emotional impacts of AEs; however, this may be attributed to a historical attitude of suffering in silence [7]. It has also been identified that female gender is an independent risk factor for second victim symptoms; however, female respondents were noted to display more constructive coping strategies [6].
Comparing our study to previous studies, 75% of respondents reflected on an incident with a Clavien-Dindo score of 3 or higher. This is broadly similar to British surgical data, where 67.9% events were grade 3a or above [15]. It was noted that a higher severity of harm has been described as a risk factor for greater emotional impact [15]. Other risk factors for second victim syndrome include first patient death, death occurring in healthy individual, self-blame for event, paediatric cases and a ‘connection”’ to the patient [12].
Physical and emotional responses
A majority of our respondents (n = 11, 68.8%) describe physical or emotional symptoms, with anxiety, guilt and sleep problems being the most reported (Table 2). This reflects international data [7, 14, 15, 28]. Other reported symptoms include impact on personal or professional relationships, anger or irritation. These have been well described in international literature with varying duration.
One respondent had a score > 4 in the PC-PTSD-V; however, seven (43.8%) reported one or more PTSD symptom (Table 3). The prevalence of PTSD symptomatology shows these are not fleeting symptoms or worries but significant emotional responses. The reports of PTSD symptoms in other literature varies from 0.3 to 35.7%; however, a variety of screening tools have been reported [15, 22].
Influencing factors
Despite not feeling responsible for the event itself, and describing external influences that contributed to the event, respondents still describe symptoms of second victim syndrome (Table 4). The AEs were recognised risks of procedures in 7 (43.8%) cases; however, trainees are still reporting significant emotional symptoms associated with them. Turner demonstrates that in comparing surgeon responses to errors versus complications that both groups display significant adverse emotional impacts [15]. Although a recognised complication is more predictable than an error, the impact is perceived in a similar fashion.
Coping strategies
Previous meta-analysis showed that healthcare workers display a complex and multifactorial variety of coping mechanisms, the most frequently reported strategies were pro-active, or task orientated such as taking steps to manage the event and taking steps to improve one’s own practice [29]. The least reported strategies were avoidant with healthcare professionals instead choosing to discuss the event with colleagues, provide apologies and disclose the event [28, 29].
Medical professionals frequently opt to discuss AEs or errors with colleagues over family or friend [7, 11, 29, 30]. This is echoed in our responses, with most respondents discussing the case with a colleague, rather than a family member (Table 5). Of note, 66.6% (n = 8) of these discussed the case with a senior consultant colleague, suggesting open working relationships up the channel of command. Reflecting on such events with colleagues can be helpful as they might have been through a similar event, or experienced similar emotions in the past. Perceived support from colleagues has been shown to have a protective impact and reduce emotional impact on healthcare workers [24]. This indicates there is a role for formal peer support programmes.
It is notable that none of our respondents used local or national support systems in the period following the AE. A recent UK paper reported that similarly only 2.7% reported having access to a formal support service [15]. A formal peer support initiative, the RISE programme, in John Hopkins proved to be an effective support tool as well as a predicted annual cost savings of 1.81 million US dollars [28, 31]. Only 16% of users were physicians, and the authors report initial challenges in getting healthcare workers to seek out and use the service [28]. A surgeon developed and surgeon led peer support programme developed by El Hechi et al. has shown promising results at 1 year, users reported satisfaction with the programme and were likely to recommend it to a colleague [30].
Preparedness for event
This study suggests that surgical trainees in Ireland do not feel ready to manage the emotional impact of AEs or complications and that their training could prepare them more effectively. This has been mirrored in international surveys with recommendations that healthcare organisations and training bodies take steps to introduce support systems and training for healthcare workers [6, 11, 12, 29, 32].
There has been a push to broaden surgical training with the successful introduction of human factors training in Ireland, the commencement of Schwartz rounds in some centres suggests a shift in culture [33]. Despite this, our respondents still have symptoms suggestive of emotional distress and felt unprepared to manage it. Potential solutions include confidential peer support programmes as described above, emotional first aid, prompt debriefing and the opportunity for a break from professional activities [6, 11, 12, 21, 28, 29, 32]. There will also be a requirement for a larger cultural shift to a ‘no blame’ open culture, and normalisation of engagement with support services [15, 28].
Study limitations
Limitations to our pilot study include the small numbers limiting in depth statistical analysis and the lack of a validated tool to assess for ‘second victim’ symptoms. Such a tool is undergoing development and validation; however, the symptoms we assessed for our well-reported across international literature in this setting [24]. Larger studies in the Irish and urology setting are needed to allow for statistical analysis and to provide data that would assist in the formation of support programmes and structures.
Conclusion
We have presented the results of the first survey In Irish healthcare workers and the first in Irish urologists about the emotional response to AEs in a patient. Doctors are human, and error is an inevitable risk even within modern healthcare systems. As a result of this ‘humanity’, we experience emotional as well as mental responses to these mistakes or outcomes. We have demonstrated that these responses occur in Irish urology trainees. Healthcare organisations have taken steps to develop standardised procedures to investigate and report these AEs and develop mandatory open disclosure policies to protect patients. However, there would seem to be a lack of support structures available to doctors and perhaps a lack of willingness to seek these supports. More research is needed in the Irish context, and in the wider urology sphere, and steps need to be taken by healthcare management and supervising bodies to ensure these supports are developed in conjunction with the relevant stakeholders. As Wu first said in 2000, ‘Physicians will always make mistakes. The decisive factor will be how we handle them’ [5].
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by S. O’Meara. The first draft of the manuscript was written by S. O’Meara, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Ethics approval
This study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All participants volunteered to partake, gave informed consent and all data collected was anonymous and stored in compliance with national data protection legislation.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rafter N, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals—a retrospective record review study. BMJ Qual Saf. 2017;26(2):111. doi: 10.1136/bmjqs-2015-004828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Vries EN, et al. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17(3):216–223. doi: 10.1136/qshc.2007.023622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker GR, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–1686. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halfon P, Staines A, Burnand B. Adverse events related to hospital care: a retrospective medical records review in a Swiss hospital. Int J Qual Health Care. 2017;29(4):527–533. doi: 10.1093/intqhc/mzx061. [DOI] [PubMed] [Google Scholar]
- 5.Wu AW (2000) Medical error: the second victim: the doctor who makes the mistake needs help too. British Medical Journal Publishing Group p. 726–727 [DOI] [PMC free article] [PubMed]
- 6.Strametz R, et al. Prevalence of second victims, risk factors and support strategies among young German physicians in internal medicine (SeViD-I survey) J Occup Med Toxicol. 2021;16(1):11. doi: 10.1186/s12995-021-00300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han K et al (2017) The surgeon as the second victim? Results of the Boston Intraoperative Adverse Events Surgeons' Attitude (BISA) study. J Am Coll Surg 224(6) [DOI] [PubMed]
- 8.Pratt SD, Jachna BR. Care of the clinician after an adverse event. Int J Obstet Anesth. 2015;24(1):54–63. doi: 10.1016/j.ijoa.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Scott SD, et al. Caring for our own: deploying a systemwide second victim rapid response team. The Joint Commission Journal on Quality and Patient Safety. 2010;36(5):233–240. doi: 10.1016/S1553-7250(10)36038-7. [DOI] [PubMed] [Google Scholar]
- 10.Burlison JD, et al. The Effects of the second victim phenomenon on work-related outcomes: connecting self-reported caregiver distress to turnover intentions and absenteeism. J Patient Saf. 2021;17(3):195–199. doi: 10.1097/PTS.0000000000000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.West CP, et al. Association of perceived medical errors with resident distress and empathya prospective longitudinal study. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 12.Marmon LM, Heiss K. Improving surgeon wellness: the second victim syndrome and quality of care. Semin Pediatr Surg. 2015;24(6):315–318. doi: 10.1053/j.sempedsurg.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Luu S, et al. Waking up the next morning: surgeons’ emotional reactions to adverse events. Med Educ. 2012;46(12):1179–1188. doi: 10.1111/medu.12058. [DOI] [PubMed] [Google Scholar]
- 14.Biggs S, Waggett HB, Shabbir J. Impact of surgical complications on the operating surgeon. Colorectal Dis. 2020;22(9):1169–1174. doi: 10.1111/codi.15021. [DOI] [PubMed] [Google Scholar]
- 15.Turner K, et al. Impact of adverse events on surgeons. Br J Surg. 2022;109(4):308–310. doi: 10.1093/bjs/znab447. [DOI] [PubMed] [Google Scholar]
- 16.McNamara K, Meaney S, O'Donoghue K. Intrapartum fetal death and doctors: a qualitative exploration. Acta Obstet Gynecol Scand. 2018;97(7):890–898. doi: 10.1111/aogs.13354. [DOI] [PubMed] [Google Scholar]
- 17.Ali S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. BMJ Open. 2020;10(12):e042930. doi: 10.1136/bmjopen-2020-042930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts T, et al. Psychological distress and trauma in doctors providing frontline care during the COVID-19 pandemic in the United Kingdom and Ireland: a prospective longitudinal survey cohort study. BMJ Open. 2021;11(7):e049680. doi: 10.1136/bmjopen-2021-049680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clavien PA, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 20.Abd Elwahab S, Doherty E (2014) What about doctors? The impact of medical errors. The Surgeon 12(6):297–300 [DOI] [PubMed]
- 21.Seys D, et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof. 2012;36(2):135–162. doi: 10.1177/0163278712458918. [DOI] [PubMed] [Google Scholar]
- 22.Sligter LM, et al. Mental-health, coping and support following adverse events on the work-floor : a cross-sectional study among Dutch orthopaedic surgeons. Acta Orthop Belg. 2020;86(3):349–362. [PubMed] [Google Scholar]
- 23.Ullström S, et al. Suffering in silence: a qualitative study of second victims of adverse events. BMJ Qual Saf. 2014;23(4):325–331. doi: 10.1136/bmjqs-2013-002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Winning AM, et al. Validation of the second victim experience and support tool-revised in the neonatal intensive care unit. J Patient Saf. 2021;17(8):531–540. doi: 10.1097/PTS.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 25.Prins A, et al. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31(10):1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williamson MLC et al (2022) Diagnostic accuracy of the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) within a civilian primary care sample. J Clin Psychol [DOI] [PubMed]
- 27.Bovin MJ et al (2021) Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the diagnostic and statistical manual of mental disorders (Fifth Edition) among US veterans. JAMA Netw Open 4(2):e2036733 [DOI] [PMC free article] [PubMed]
- 28.Edrees H, et al. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6(9):e011708. doi: 10.1136/bmjopen-2016-011708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Busch IM, et al. Dealing with adverse events: a meta-analysis on second victims’ coping strategies. J Patient Saf. 2020;16(2):e51–e60. doi: 10.1097/PTS.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 30.El Hechi MW, et al. Design and impact of a novel surgery-specific second victim peer support program. J Am Coll Surg. 2020;230(6):926–933. doi: 10.1016/j.jamcollsurg.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 31.Moran D, et al. Cost-benefit analysis of a support program for nursing staff. J Patient Saf. 2020;16(4):e250–e254. doi: 10.1097/PTS.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 32.Koyle MA, et al. The second victim requires more than Medice Cura Te Ipsum. Can Urol Assoc J. 2021;15(6 Suppl 1):S40–s42. doi: 10.5489/cuaj.7229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doherty E, O'Keeffe D, Traynor O. Developing a human factors and patient safety programme at the Royal College of Surgeons in Ireland. Surgeon. 2011;9(Suppl 1):S38–S39. doi: 10.1016/j.surge.2010.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


