Abstract
Background Complications after open reduction internal fixation (ORIF) for distal radius fractures (DRF) are well documented, but the impact of trainee involvement on postoperative outcomes has not been studied.
Questions Does trainee involvement affect postoperative complication rates and length of hospital stay?
Methods The American College of Surgeons National Surgical Quality Improvement Program was queried from 2006 to 2012 for patients undergoing DRF ORIF. A 1:1 propensity score matched resident/fellow involved cases to attending-only cases. Demographics, length of stay, and postoperative complications were compared between the two groups. Logistic regression was used to evaluate independent predictors of adverse events and to evaluate cases with and without trainee involvement.
Results Overall, 3,003 patients underwent DRF ORIF from 2006 to 2012. After matching, 1,150 cases (50% with resident/fellow involvement) were included. The overall rate of adverse events was 4.4% (46/1,050). There were no significant differences in the short-term complication rate in trainee-involved (2.3%) versus attending-only cases (3.9%) ( p = 0.461). For ORIF of DRF, there were no significant differences, between attending-only cases and resident/fellow-involved cases, with regard to short-term major complications ( p = 0.720) or minor complications ( p = 0.374). Length of hospital stay was similar between cohorts (1.22 vs. 0.98 days) ( p = 0.723). On multivariate analysis, trainee involvement was not an independent predictor of minor, major, or any complication after DRF fixation after controlling for multiple independent factors (all p > 0.364).
Discussion Trainee participation in DRF ORIF is not associated with increased risk of short-term (30 days) medical or surgical postoperative complications.
Level of Evidence This is a Level IV case–control study.
Keywords: NSQIP, Resident, Education, Orthopaedics, Complications, distal radius fracture, training
The objective of orthopaedic surgery training is to develop skills through the completion of core competencies and established benchmarks for common orthopaedic conditions. Orthopaedic surgery has always been regarded as a highly procedurally based specialty, and measuring competency is a challenging endeavor for program directors of accredited residencies. To develop a framework, the Accreditation Council for Graduate Medical Education launched the Next Accreditation System in 2013 and, subsequently, followed this by the implementation of “The Milestone Project.” 1 2 After the development of six core competencies, a working group of orthopaedic surgeons came together to evolve and solidify the six core competencies: technical skill, medical knowledge, patient care, professionalism, interpersonal and communication skills, systems-based practice, and practice-based learning and improvement. 3 4 The milestones span all subspecialties including hand and upper extremity surgeries. Patient care and medical knowledge of distal radius fractures (DRF) are two of the 41 milestones that trainees are expected to master by the time of independent practice.
DRF, estimated to be 17.5 to 22.2% of all fractures, represent one of the most common fractures encountered and treated by upper extremity surgeons. 5 6 In the academic training environment, orthopaedic hand surgeons are tasked with the challenge of teaching operative skills to trainees and balancing more complex surgical procedures. To add to this, operating room efficiency, length of hospital stay, decreased patient complications, cost considerations, and patient concerns contribute to increased demands for teachers of the next generation of orthopaedic surgeons. 7 The impact of resident involvement on intraoperative and postoperative morbidity and mortality has been well evaluated in the subspecialties of lower extremity trauma, spine, and joint arthroplasty. 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 However, few evaluations have been studied for hand surgery procedures. 27 28 The knowledge of the complications associated with trainee involvement for DRF fixation is important to allow surgeons to mitigate risk, to properly screen patients prior to intervention, and to dispel patient concerns about trainee involvement in their care. 7 29 30 31
Despite hand surgery having a low complication rate, patient concerns regarding hand surgery are a large part of patient education in the preoperative and postoperative periods. 32 The short-term complications after DRF open reduction internal fixation (ORIF) are reportedly low with a few known patient-specific risk factors. 33 34 35 36 37 38 We sought to use a national surgical database to answer our primary research questions: (1) does resident/fellow involvement increase short-term complication risk and surgical complications following ORIF for DRF and (2) does resident/fellow involvement have an opportunity cost with regard to the length of hospital stay? We hypothesized that major and minor adverse events and length of hospital stay would not significantly differ with the inclusion of a resident or fellow orthopaedic surgeon.
Materials and Methods
Database and Patient Selection
This study was a retrospective review of prospectively collected data from the 2006 to 2012 American College of Surgeons—National Surgical Quality Improvement Program (ACS-NSQIP) database. Details regarding how data are collected for the database can be found on the ACS-NSQIP Web site. The database was queried using Current Procedural Terminology (CPT) codes 25607, 25608, and 25609 which represent the open treatment of DRF ranging from extraarticular to intraarticular with three or more fragments. Patients with missing data were removed from the study. The study period was limited until the year 2012 as the NSQIP did not collect reliable data regarding trainee involvement after that year. Of the cases identified in the database, 964 cases were initially excluded due to the lack of information regarding trainee involvement in the case ( Fig. 1 ). The data for this study were derived from a de-identified national surgical database; therefore, the study was exempt from Institutional Review Board (IRB) approval.
Fig. 1.
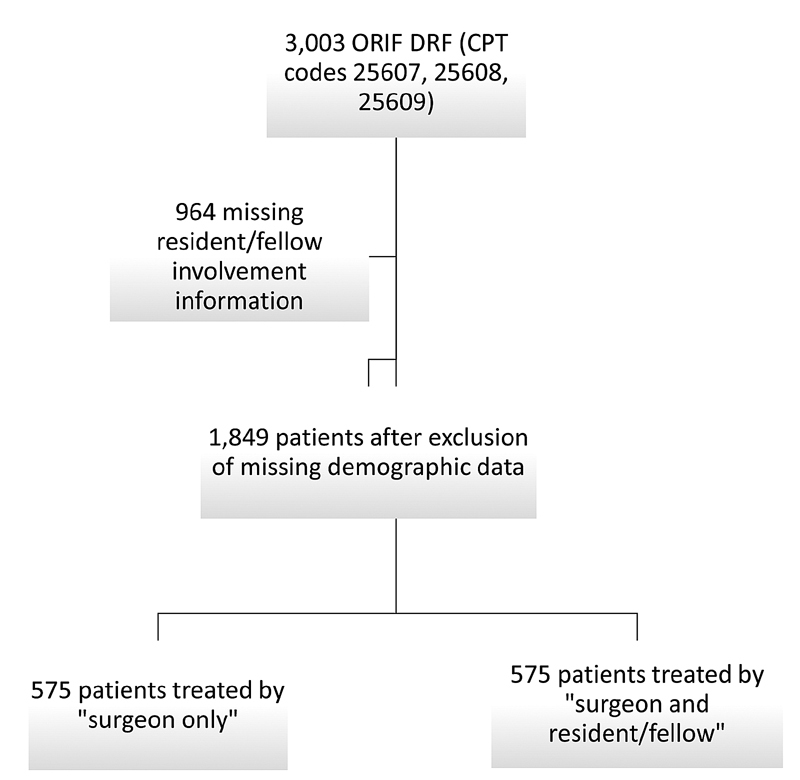
Flow chart of patients involved in study selection.
Variables and Outcomes Studied
Patient demographic variables included as part of the study were age, gender, race, body mass index (BMI; <25.0, 25.0–29.9, ≥30.0), comorbidities (diabetes mellitus, history of smoking, presence of chronic obstructive pulmonary disease [COPD], congestive heart failure, hypertension, dialysis-dependent, disseminated cancer, chronic steroid use, bleeding disorder, dyspnea, and functional health status), and American Society of Anesthesiologists (ASA) grade.
The ACS-NSQIP database includes two variables designating whether a trainee [defined by post-graduate year (PGY)] was present for the case. For the purpose of this study, we used this variable to determine resident/fellow involvement. PGY 1 and 2 were categorized as junior residents, PGY 3 to 5 were senior residents and PGY 6+ were considered fellows. Patients were excluded when the presence or absence of surgical resident/fellow involvement in the database was not recorded or if the two distinct database indicators indicating trainee involvement were discordant. Notably, the database does not indicate more granular details for the specific role of a trainee during the surgical procedure which may range anywhere from assisting, approach and dissection, hardware placement, or other involvement.
The ACS-NSQIP records intra- and postoperative data in a standardized fashion. The primary outcomes evaluated were surgical complications, medical complications, and length of hospital stay (days). The occurrence of postoperative adverse events was limited to 30 days. We defined a serious adverse event as the occurrence of any of the following: death, coma >24 hours, ventilator >48 hours, unplanned intubation, stroke/cerebrovascular accident, thromboembolic event (deep venous thrombosis or pulmonary embolism), cardiac arrest, myocardial infarction, acute renal failure, sepsis, septic shock, return to the operating room, deep surgical site infection, or organ/space infection. A minor adverse event was defined as superficial surgical site infection, urinary tract infection, pneumonia, progressive renal insufficiency, or wound dehiscence. Any adverse event was defined as the occurrence of any major or minor adverse event. Groups were compared in terms of any adverse event, serious adverse events, and minor adverse events.
Statistical Analysis
Bivariate analysis using Pearson chi-squared or Fisher's exact test was used to assess for significant differences in baseline demographics and associations for resident/fellow involvement in 30-day complications after ORIF for DRF. A propensity score matching algorithm was used to create similar groups for the trainee-involved and attending-only cohorts ( Fig. 1 ). In this study, a 1:1 propensity score-matching algorithm was used based on age, sex, race, BMI, smoking status, ASA classification, steroid use, and CPT code to match cases with resident/fellow involvement versus attending-only cases. The matched cohorts were compared for preoperative patient demographics, comorbidities, laboratory values, and postoperative complications using the Fisher exact test or Pearson χ 2 test for categorical variables and Student's t -test for continuous variables. All demographic variables were then entered into a logistic regression model and adjusted for each other, to identify significant independent predictors of complication. Our primary independent variable of interest was the presence of trainee involvement and whether this was an independent predictor of complication after controlling for other variables. Data were reported as odds ratios (OR) and 95% confidence intervals (CI). All statistical analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC) with statistical significance set at p < 0.05.
Results
Baseline Patient Characteristics
After propensity score matching, 1,050 cases (50% with resident/fellow involvement) were included in the study. Both matched cohorts were similar in age, sex, BMI, diabetes mellitus, smoking status, hypertension, history of COPD, steroid use, ASA classification, and CPT codes ( Table 1 ).
Table 1. Patient demographics of unmatched and matched cohorts.
| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| Resident/Fellow | Attending | p -Value | Resident/Fellow | Attending | p -Value | |
| Number of patients | 576 | 1,273 | 575 | 575 | ||
| Age (y) | 53.94 | 56.79 | 0.001 | 53.97 | 54.52 | 0.557 |
| Gender | ||||||
| Male | 188 | 360 | 0.057 | 188 | 163 | 0.109 |
| Female | 388 | 913 | 387 | 412 | ||
| Race | ||||||
| White | 395 | 1,049 | <0.001 | 395 | 413 | 0.029 |
| African American | 34 | 29 | 34 | 16 | ||
| Other | 18 | 37 | 18 | 27 | ||
| Unknown | 129 | 158 | 128 | 119 | ||
| BMI | 27.92 | 28.57 | 0.082 | 27.93 | 28.4 | 0.248 |
| Diabetes mellitus | ||||||
| Yes | 39 | 119 | 0.066 | 39 | 51 | 0.237 |
| No | 537 | 1,154 | 536 | 524 | ||
| Current smoker | ||||||
| Yes | 122 | 269 | 0.981 | 122 | 110 | 0.378 |
| No | 454 | 1,004 | 453 | 465 | ||
| Hypertension | ||||||
| Yes | 160 | 464 | <0.001 | 160 | 182 | 0.156 |
| No | 416 | 809 | 415 | 393 | ||
| History of COPD | ||||||
| Yes | 20 | 47 | 0.815 | 20 | 17 | 0.62 |
| No | 556 | 1,226 | 555 | 558 | ||
| Steroid use | ||||||
| Yes | 19 | 25 | 0.081 | 18 | 17 | 0.864 |
| No | 557 | 1,248 | 557 | 558 | ||
| ASA class | ||||||
| 1 | 123 | 238 | 0.007 | 123 | 120 | 0.798 |
| 2 | 337 | 683 | 336 | 330 | ||
| 3 | 110 | 332 | 110 | 121 | ||
| 4 | 6 | 20 | 6 | 4 | ||
| Anesthesia technique | ||||||
| General | 415 | 1,074 | <0.001 | 414 | 485 | <0.001 |
| Monitored anesthesia care | 22 | 71 | 22 | 25 | ||
| Regional | 137 | 123 | 137 | 62 | ||
| Other | 2 | 5 | 2 | 3 | ||
| CPT code | ||||||
| 25607 | 157 | 449 | <0.001 | 156 | 156 | 1.00 |
| 25608 | 155 | 408 | 155 | 155 | ||
| 25609 | 264 | 416 | 264 | 264 | ||
Abbreviations: ASA, American Society of Anesthesiologistsl; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CPT, current procedural terminology.
Postoperative Complication Rates and Length of Hospital Stay
The overall rate of adverse events after ORIF for DRF was 4.4% (46/1,050) ( Table 2 ). The most common adverse events were return to the operating room (1.3%), death (0.67%), and unplanned intubation (0.48%).
Table 2. Short term complications comparing attending-only cases to trainee cases.
| Attending | Trainee involved | p -Value a | |
|---|---|---|---|
| Any adverse event | 29 | 17 | 0.461 |
| Any severe adverse event | 26 | 13 | 0.720 |
| Death | 6 | 1 | 0.124 |
| Coma | – | – | – |
| Ventilator >48 h | 2 | 0 | 0.500 |
| Unplanned intubation | 4 | 1 | 0.624 |
| Stroke/cerebrovascular accident | 0 | 1 | 1.000 |
| Thromboembolic event (DVT/PE) | 0 | 1 | 1.000 |
| Deep surgical site infection | 1 | 0 | 1.000 |
| Sepsis | 2 | 0 | 0.500 |
| Cardiac arrest requiring CPR | 1 | 1 | 1.000 |
| Myocardial infarction | 1 | 0 | 1.000 |
| Acute renal failure | 1 | 0 | 1.000 |
| Return to the operating room | 7 | 7 | 1.000 |
| Organ space infection | – | – | – |
| Blood transfusion | 1 | 1 | 1.000 |
| Any minor adverse event | 3 | 4 | 0.374 |
| Superficial wound infection | 0 | 2 | 0.500 |
| Wound dehiscence | – | – | – |
| Urinary tract infection | 2 | 2 | 1.000 |
| Pneumonia | 1 | 0 | 1.000 |
| Progressive renal insufficiency | – | – | – |
| Peripheral nerve injury | – | – | – |
| a Pearson chi-square or Fisher's exact test | |||
| All values are presented as the number of events | |||
Abbreviations: CPR, cardiopulmonary resuscitation; DVT, deep vein thrombosis; PE, pulmonary embolism.
Note: All values are presented as the number of events.
Pearson chi-square or Fisher's exact test
There were no significant differences in the short-term complication rate in trainee-involved (2.3%) versus attending-only cases (3.9%) ( p = 0.461) ( Table 2 ). For ORIF of DRF, there were no significant differences, between attending-only cases and resident/fellow-involved cases, with regard to short-term major complications ( p = 0.720) or minor complications (0.374). Length of hospital stay was similar between cohorts (1.22 vs. 0.98 days) ( p = 0.723) and after further stratifying by CPT code ( Table 3 ).
Table 3. Comparison of trainee involvement and length of hospital stay.
| CPT 25607 | p -Value a | CPT 25608 | p -Value a | CPT 25609 | p -Value a | All CPTs | p -Value a | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attending only | With any trainee | Attending only | With any trainee | Attending only | With any trainee | Attending only | With any trainee | |||||
| Length of hospital stay (d) | 3.06 (29.26) | 1.66 (11.98) | 0.582 | 0.36 (0.97) | 0.35 (0.80) | 0.949 | 0.65 (1.64) | 0.94 (1.89) | 0.056 | 1.22 (15.30) | 0.98 (6.39) | 0.723 |
Abbreviation: CPT, current procedural terminology.
Note: Values are mean and standard deviation
Student's t -test comparing attending only and attending + trainee
Predictors of Complication after ORIF for DRF
On multivariate analysis, trainee involvement was not a significant predictor of any complication, minor complication, or major complication after ORIF for DRF ( Table 4 ). With respect to independent predictors of any complication after surgery, we found that African American race was associated with increased odds of complication (OR 4.48; 95% CI 1.43–14.03; p = 0.010]. ASA Class 4 (OR 13.74; 95% CI 1.30–144.72; p = 0.029) and African American race (OR 4.38; 95% CI 1.25–15.42; p = 0.021) were associated with increased odds of major complication.
Table 4. Multivariate logistic regression of factors associated with complication after distal radius fracture open reduction and internal fixation.
| Predictors of Any Complication | Adjusted OR (95% CI) a | p -Value |
|---|---|---|
| Trainee involvement | ||
| No | Ref. | |
| Yes | 0.995 (0.45–2.20) | 0.991 |
| Gender | ||
| Male | Ref. | – |
| Female | 0.54 (0.22–1.31) | 0.171 |
| COPD | ||
| No | Ref. | |
| Yes | 2.79 (0.73–10.68) | 0.133 |
| ASA class | ||
| 1 | Ref. | |
| 2 | 0.62 (0.16–2.32) | 0.475 |
| 3 | 0.89 (0.19–4.26) | 0.882 |
| 4 | 6.61 (0.84–52.12) | 0.073 |
| Race | ||
| White | Ref. | |
| Black | 4.48 (1.43–14.03) | 0.01 |
| Unknown | 1.13 (0.35–3.62) | 0.84 |
| Other | 0.00 (0.00–) | 0.998 |
| Predictors of major complication | Adjusted OR (95% CI) | p -Value |
| Trainee involvement | ||
| No | Ref. | |
| Yes | 0.76 (0.31–1.83) | 0.539 |
| Gender | ||
| Male | Ref. | – |
| Female | 0.42 (0.16–1.12) | 0.081 |
| ASA class | ||
| 1 | Ref. | |
| 2 | 1.14 (0.21–6.18) | 0.881 |
| 3 | 1.4 (0.20–9.67) | 0.731 |
| 4 | 13.74 (1.30–144.72) | 0.029 |
| Race | ||
| White | Ref. | |
| Black | 4.38 (1.25–15.42) | 0.021 |
| Unknown | 0.67 (0.14–3.10) | 0.603 |
| Other | 0.00 (0.00–) | 0.998 |
| Predictors of minor complication | Adjusted OR (95% CI) | p -Value |
| Trainee involvement | ||
| No | Ref. | |
| Yes | 2.51 (0.34–18.30) | 0.364 |
| COPD | ||
| No | Ref. | – |
| Yes | 11.56 (0.89–149.45) | 0.061 |
| ASA class | ||
| 1 | Ref. | |
| 2 | 0.11 (0.01–1.87) | 0.127 |
| 3 | 0.21 (0.01–6.66) | 0.374 |
| 4 | 1.77 (0.02–166.03) | 0.805 |
| Race | ||
| White | Ref. | |
| Black | 9.12 (0.49–168.76) | 0.138 |
| Unknown | 5.06 (0.51–50.20) | 0.166 |
| Other | 0.00 (0.00–) | 0.998 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CPT, current procedural terminology; OR, odds ratio.
Note: Bold values are statistically significant.
Multivariate logistic regression is adjusted for age, sex, race, BMI, smoking status, diabetes, hypertension, COPD, steroid use, ASA class, and CPT code. The values are reported as OR, with the 95% CI in parentheses. p < 0.05 is considered significant
Discussion
With limited literature specifically analyzing the impact of trainee involvement during hand surgery, the current study is the first to identify rates and predictors of complication after ORIF for DRF utilizing a matched cohort. Patient attitudes toward resident and fellow participation during orthopaedic surgery have rarely been studied, which warrants further reporting on this topic. 7 Despite claiming nearly 95% of patients feel that residents and fellows should perform surgeries as part of their education, 40% of patients did not feel a second-year resident assisting in their own surgery was satisfactory. 7 Even with programs emphasizing graduated autonomy and milestones in place, the current study is a step toward providing objective data for a patient population that appears to not be fully comfortable with trainee involvement in their own surgery. Using a nationwide surgical database, we found that that resident and fellow involvement in ORIF for DRF procedures does not significantly alter major or minor short-term adverse events or length of hospital stay. The overall complication rate in the current study was low (4.4%) and similar between the two cohorts. The results of this study can be utilized during the preoperative counseling period to address any patient concerns regarding the assistance of residents/fellows during ORIF for DRF.
There are a few limitations to the study that should be considered. Notably, the database does not indicate the specific role of the resident/fellow during the surgical procedure but rather specifies if they were scrubbed and present as an assistant in some capacity during the procedure. The duration of involvement intraoperatively and more granular details such as level of assistance, approach and dissection, hardware placement, or other involvement are not specified. As a result, the clinical outcome of patients postoperatively may not be directly attributed to trainee involvement. In addition, the database lacks granular clinical information, such as post-operative pain and functional scores, as well as socioeconomic data, which would be useful to evaluate between the two cohorts. Additional clinical outcomes specific to DRF fixation such as paresthesias, swelling, postoperative range of motion, radiographic alignment, subsidence, tendon complications, malunion and nonunion, and symptomatic hardware are not included in the NSQIP database. Complications and reoperation evaluation was limited to 30 days postoperatively which may not capture patients who presented to the hospital after that time period. The data utilized in this study were from academic teaching hospitals which may not be generalizable to alternative practicing environments. Additionally, we were unable to match propensity score based on case complexity as only general CPT codes are documented in the database. The surgical technique and approach are also not available which would be valuable for further evaluation. Despite these limitations, this is the first study to evaluate resident/fellow involvement for ORIF of DRF and may be helpful during the preoperative counseling period to ease any patient concerns.
The low short-term complication rate noted in the current study is similar to prior evaluations after ORIF for DRF. 33 34 35 36 37 38 Using the NSQIP database, Jiang et al reported a complication rate of 2% and reoperation rate of 1.1% after DRF fixation. 35 Other studies have evaluated more patient-specific risk factors including age, smoking status, BMI, and frailty to understand the importance of these factors affecting the complication rate. 33 34 35 36 37 38 Hand surgery is generally regarded as low risk; however, the involvement of trainees during these procedures is unknown. The findings from this study show that resident/fellow involvement is not a risk factor for complications. Further evaluation with regard to other hand-specific procedures should be done to confirm similar findings. Our results in this study mimic prior NSQIP evaluations which demonstrated no increased risk of complications when comparing surgeries involving trainees versus attending-only cases within the subspecialties of trauma, spine, sports medicine, and joint arthroplasty. We did find that certain patient demographics including African American race and higher ASA class were associated with increased odds of major complication after DRF fixation when controlling for other variables. In the context of prior studies, ASA class was shown to be a predictor of complication in those studies as well. 36 38 The higher ASA class is likely an indication for increased comorbidity burden which would explain the increased chance for complication. African American race being associated with increased odds of complication after ORIF for DRF warrants further study involving both medical and patient-reported complications.
The comparison of length of hospital stay between attending-only cases and resident/fellow involved cases is important. Generally, within an academic medical center, attending surgeons are tasked with the responsibility of balancing education and providing safe care to patients. These conflicts are additionally complicated by external pressures from health care systems, patients, and family members. The length of hospital stay is not only a financial consideration but also a patient safety consideration. Longer hospital stays increase the economic burden of these injuries. Furthermore, elderly patients remaining in the hospital for longer periods of time may be more likely to sustain medical complications including kidney injury, pneumonia, or thromboembolic events. Limiting costs while providing efficient care is increasingly emphasized in all of orthopaedic surgeries as value-based reimbursement models are emerging. These pressures, coupled with patients and family members becoming increasingly more aware of trainee involvement, make training of the next generation of surgeons difficult. 7 The findings in the present study are reassuring that trainee involvement does not appear to be a risk factor for an increased length of hospital stay. When evaluating the entire cohort and stratified by CPT code, the length of stay was not significantly different between trainee-involved cases or attending-only cases. With work hour restrictions and increased diversity of orthopaedic procedures, residency programs must seek optimal procedural exposure for their trainees to prepare them for independent practice. A helpful consideration is the use and emphasis of cadaver laboratories for resident education to practice.
Conclusion
Trainee participation during DRF ORIF is not associated with an increased risk of short-term (30 days) medical or surgical postoperative complications. Length of hospital stay was not impacted by resident/fellow involvement.
Funding Statement
Funding None.
Conflict of Interest None declared.
Ethical Approval
This study was determined to be exempt from the Institutional Review Board of Maimonides Medical Center.
References
- 1.Nasca T J, Philibert I, Brigham T, Flynn T C. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 2.Van Heest A E, Dougherty P J. CORR® curriculum–orthopaedic education: operative assessment and the ACGME milestones: time for change. Clin Orthop Relat Res. 2015;473(03):775–778. doi: 10.1007/s11999-014-4131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stern P J, Albanese S, Bostrom M.Orthopaedic surgery milestones J Grad Med Educ 20135(1, Suppl 1)36–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ames S E, Ponce B A, Marsh J L, Hamstra S J. Orthopaedic surgery residency milestones: initial formulation and future directions. J Am Acad Orthop Surg. 2020;28(01):e1–e8. doi: 10.5435/JAAOS-D-18-00786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Court-Brown C M, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(08):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 6.Court-Brown C M, Clement N D, Duckworth A D, Aitken S, Biant L C, McQueen M M. The spectrum of fractures in the elderly. Bone Joint J. 2014;96-B(03):366–372. doi: 10.1302/0301-620X.96B3.33316. [DOI] [PubMed] [Google Scholar]
- 7.Nahhas C R, Yi P H, Culvern C. Patient attitudes toward resident and fellow participation in orthopedic surgery. J Arthroplasty. 2019;34(09):1884–1.888E8. doi: 10.1016/j.arth.2019.04.035. [DOI] [PubMed] [Google Scholar]
- 8.Basques B A, Saltzman B M, Korber S S. Resident involvement in arthroscopic knee surgery is not associated with increased short-term risk to patients. Orthop J Sports Med. 2020;8(12):2.32596712096746E15. doi: 10.1177/2325967120967460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basques B A, Saltzman B M, Mayer E N. Resident involvement in shoulder arthroscopy is not associated with short-term risk to patients. Orthop J Sports Med. 2018;6(12):2.325967118816293E15. doi: 10.1177/2325967118816293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casp A J, Patterson B M, Yarboro S R, Tennant J N. The effect of time during the academic year or resident training level on complication rates after lower-extremity orthopaedic trauma procedures. J Bone Joint Surg Am. 2018;100(22):1919–1925. doi: 10.2106/JBJS.18.00279. [DOI] [PubMed] [Google Scholar]
- 11.Cvetanovich G L, Schairer W W, Haughom B D, Nicholson G P, Romeo A A. Does resident involvement have an impact on postoperative complications after total shoulder arthroplasty? An analysis of 1382 cases. J Shoulder Elbow Surg. 2015;24(10):1567–1573. doi: 10.1016/j.jse.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 12.Edelstein A I, Lovecchio F C, Saha S, Hsu W K, Kim J Y. Impact of resident involvement on orthopaedic surgery outcomes: an analysis of 30,628 patients from the American College of Surgeons National Surgical Quality Improvement Program Database. J Bone Joint Surg Am. 2014;96(15):e131. doi: 10.2106/JBJS.M.00660. [DOI] [PubMed] [Google Scholar]
- 13.Giordano L, Oliviero A, Peretti G M, Maffulli N. The presence of residents during orthopedic operation exerts no negative influence on outcome. Br Med Bull. 2019;130(01):65–80. doi: 10.1093/bmb/ldz009. [DOI] [PubMed] [Google Scholar]
- 14.Gross C E, Chang D, Adams S B, Parekh S G, Bohnen J D. Surgical resident involvement in foot and ankle surgery. Foot Ankle Surg. 2017;23(04):261–267. doi: 10.1016/j.fas.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Haughom B D, Schairer W W, Hellman M D, Yi P H, Levine B R. Resident involvement does not influence complication after total hip arthroplasty: an analysis of 13,109 cases. J Arthroplasty. 2014;29(10):1919–1924. doi: 10.1016/j.arth.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Haughom B D, Schairer W W, Hellman M D, Yi P H, Levine B R.Does resident involvement impact post-operative complications following primary total knee arthroplasty? An analysis of 24,529 cases J Arthroplasty 201429071468–147200., e1462 [DOI] [PubMed] [Google Scholar]
- 17.Kagan R, Hart C, Hiratzka S L, Mirarchi A J, Mirza A J, Friess D M. Does resident participation in the surgical fixation of hip fractures increase operative time or affect outcomes? J Surg Educ. 2021;78(04):1269–1274. doi: 10.1016/j.jsurg.2020.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Khazi Z M, Gulbrandsen T R, Shamrock A G. Resident involvement is not associated with increased risk of postoperative complications after arthroscopic knee surgery: a propensity-matched study. Arthroscopy. 2020;36(10):2689–2695. doi: 10.1016/j.arthro.2020.04.040. [DOI] [PubMed] [Google Scholar]
- 19.Kim R B, Garcia R M, Smith Z A, Dahdaleh N S. Impact of resident participation on outcomes after single-level anterior cervical diskectomy and fusion: an analysis of 3265 patients from the American College of Surgeons National Surgical Quality Improvement Program Database. Spine. 2016;41(05):E289–E296. doi: 10.1097/BRS.0000000000001230. [DOI] [PubMed] [Google Scholar]
- 20.Kothari P, Lee N J, Lakomkin N. Impact of resident involvement on morbidity in adult patients undergoing fusion for spinal deformity. Spine. 2016;41(16):1296–1302. doi: 10.1097/BRS.0000000000001522. [DOI] [PubMed] [Google Scholar]
- 21.Lee N J, Kothari P, Kim C. The impact of resident involvement in elective posterior cervical fusion. Spine. 2018;43(05):316–323. doi: 10.1097/BRS.0000000000001477. [DOI] [PubMed] [Google Scholar]
- 22.Louie P K, Schairer W W, Haughom B D, Bell J A, Campbell K J, Levine B R. Involvement of residents does not increase postoperative complications after open reduction internal fixation of ankle fractures: an analysis of 3251 cases. J Foot Ankle Surg. 2017;56(03):492–496. doi: 10.1053/j.jfas.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 23.Neuwirth A L, Stitzlein R N, Neuwirth M G, Kelz R K, Mehta S. Resident participation in fixation of intertrochanteric hip fractures: analysis of the NSQIP Database. J Bone Joint Surg Am. 2018;100(02):155–164. doi: 10.2106/JBJS.16.01611. [DOI] [PubMed] [Google Scholar]
- 24.Phan K, Phan P, Stratton A, Kingwell S, Hoda M, Wai E. Impact of resident involvement on cervical and lumbar spine surgery outcomes. Spine J. 2019;19(12):1905–1910. doi: 10.1016/j.spinee.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi J T, Garcia R M, Cloney M B, Dahdaleh N S. Impact of resident participation on outcomes following lumbar fusion: an analysis of 5655 patients from the ACS-NSQIP database. J Clin Neurosci. 2018;56:131–136. doi: 10.1016/j.jocn.2018.06.030. [DOI] [PubMed] [Google Scholar]
- 26.Zuckerman S L, Lim J, Lakomkin N. Effect of resident and fellow involvement in adult spinal deformity surgery. World Neurosurg. 2019;122:e759–e764. doi: 10.1016/j.wneu.2018.10.135. [DOI] [PubMed] [Google Scholar]
- 27.Mitchell P M, Gavrilova S A, Dodd A C, Attum B, Obremskey W T, Sethi M K. The impact of resident involvement on outcomes in orthopedic trauma: an analysis of 20,090 cases. J Clin Orthop Trauma. 2016;7(04):229–233. doi: 10.1016/j.jcot.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu W Y, Beletsky A, Kordahi A.The cost to attending surgeons of resident involvement in academic hand surgery Ann Plast Surg 201982(5S, Suppl 4):S285–S288. [DOI] [PubMed] [Google Scholar]
- 29.Edgington J P, Petravick M E, Idowu O A, Lee M J, Shi L L. Preferably not my surgery: a survey of patient and family member comfort with concurrent and overlapping surgeries. J Bone Joint Surg Am. 2017;99(22):1883–1887. doi: 10.2106/JBJS.17.00414. [DOI] [PubMed] [Google Scholar]
- 30.Pereira D, Lee D H. CORR synthesis: what is the current understanding of overlapping surgery in orthopaedics, particularly as it relates to patient outcomes and perceptions? Clin Orthop Relat Res. 2021;479(06):1208–1216. doi: 10.1097/CORR.0000000000001584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reilly B M. Don't learn on me—are teaching hospitals patient-centered? N Engl J Med. 2014;371(04):293–295. doi: 10.1056/NEJMp1405709. [DOI] [PubMed] [Google Scholar]
- 32.Lipira A B, Sood R F, Tatman P D, Davis J I, Morrison S D, Ko J H.Complications within 30 days of hand surgery: an analysis of 10,646 patients J Hand Surg Am 201540091852–59000., e1853 [DOI] [PubMed] [Google Scholar]
- 33.Galivanche A R, FitzPatrick S, Dussik C. A matched comparison of postoperative complications between smokers and nonsmokers following open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2021;46(01):1–90000. doi: 10.1016/j.jhsa.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 34.Goodloe J B, Traven S A, Herzog L N, Richardson C M, Daley D N, Slone H S. Elevated BMI is associated with intra-articular comminution, prolonged operative time, and postoperative complications in distal radius fractures. Injury. 2020;51(11):2612–2616. doi: 10.1016/j.injury.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 35.Jiang J J, Phillips C S, Levitz S P, Benson L S. Risk factors for complications following open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2014;39(12):2365–2372. doi: 10.1016/j.jhsa.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 36.Skochdopole A, Tarabishy S, Hermiz S, Mailey B, Herrera F A. Open reduction internal fixation of distal radius fractures: retrospective cohort analysis of the geriatric population using the NSQIP database. Hand. 2020:1.558944720915716E15. doi: 10.1177/1558944720915716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson J M, Holzgrefe R E, Staley C A, Schenker M L, Meals C. The effect of malnutrition on postoperative complications following surgery for distal radius fractures. J Hand Surg Am. 2019;44(09):742–750. doi: 10.1016/j.jhsa.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 38.Wilson J M, Holzgrefe R E, Staley C A, Schenker M L, Meals C G. Use of a 5-Item modified frailty index for risk stratification in patients undergoing surgical management of distal radius fractures. J Hand Surg Am. 2018;43(08):701–709. doi: 10.1016/j.jhsa.2018.05.029. [DOI] [PubMed] [Google Scholar]


