Abstract
Spinal metastasis is a common issue causing significant pain and disability in cancer patients. A multidisciplinary approach consisting of chemotherapy, radiotherapy, and surgical treatment is used for treating patients with metastatic spinal tumors. Due to recent advancements in medical and radiation oncology, like tumor genetics and stereotactic radiotherapy, this treatment strategy would change inevitably. Therefore, the decision-making systems developed for assisting physicians and surgeons to choose the most appropriate treatment for each patient with spinal metastasis need to evolve. In this review, the recent developments, validations, and modifications of these systems, as well as suggestions for future systems have been discussed. Recently, separation surgery combined with stereotactic radiotherapy (hybrid therapy) has gained popularity. Additionally, the evidence for hybrid therapy presented in the literature has been reviewed.
Keywords: Spinal metastasis, Separation surgery, Stereotactic radiosurgery, Hybrid therapy, Prognostic model
Introduction
Spinal metastasis is a common problem resulting in adverse effects on the clinical course of patients with spinal metastasis [1]. The incidence of spinal metastasis has been increasing due to the growing number of cancer patients and an increase in their survival rates [2]. Spinal metastasis affects up to 70% of cancer patients, whereas 10%–20% of cases are symptomatic, causing pain, neurological deficits, and quality-of-life deterioration [3].
Spinal metastasis surgery is predominantly palliative and aims at preserving or improving the quality of life by achieving pain controlling and preserving ambulatory function [4]. A multidisciplinary approach consisting of chemotherapy, radiotherapy, and surgical treatment is used for treating metastatic spinal cancers because of variable treatment responses among cancer patients [5]. As a result, several authors established multiple decisionmaking systems for treating metastatic spinal tumors. This could assist physicians and surgeons in determining the most appropriate treatment option for each patient [6]. However, recent advancements in oncology and methodology have demanded a further evolution of these decision-making systems. In the current review, the developments, validations, and modifications in these systems presented in recent studies have been discussed [7].
Growing evidence is available for separation surgery combined with stereotactic radiosurgery (SRS) for treating spinal metastasis. In this study, several techniques and evidence for the efficacy of hybrid therapy for metastatic spinal tumors have been reviewed.
Present and Future of Decision-Making Systems
1. Classification-based prognostic models
Many authors have devised several “classification-based” prognostic models, like the Tomita, Tokuhashi, Bauer, and Katagiri scoring systems, to estimate the survival of patients with metastatic spinal tumors [8-13]. In these scoring systems, a patient’s life expectancy is predicted by the total prognostic score calculated by adding the scores assigned to each prognostic factor. Each decision-making or scoring system has different prognostic factors. However, the factors commonly included in most systems are the histological subtype of primary cancer and the presence of visceral metastasis (Table 1). Spine surgeons and oncologists can use these scoring systems to select patients with a sufficient life expectancy and decide if surgical treatment is needed.
Table 1.
Prognostic factors in decision-making systems
| Study | Primary tumor | Performance status | No. of vertebral metastases | Bone metastasis | Visceral metastasis | Previous systemic treatment | Other factors |
|---|---|---|---|---|---|---|---|
| Modified Bauer [9] (1995) | O | O | O | ||||
| Tomita [10] (2001) | O | O | O | ||||
| Revised Tokuhashi [11] (2005) | O | O | O | O | O | ||
| Revised Katagiri [14] (2014) | O | O | O | O | O | Brain metastasis, WBC, Hb, platelet, albumin, bilirubin, CRP, LDH | |
| NESMS [21] (2015) | O | O | O | O | O | Serum albumin | |
| SORG [20] (2016) | O | O | O | O | O | Age, WBC, Hb, brain metastasis |
WBC, white blood cell; Hb, hemoglobin; CRP, C-reactive protein; LDH, lactate dehydrogenase; NESMS, New England Spinal Metastasis Score; SORG, Spine Oncology Research Group.
However, in recent studies, these survival prediction systems have shown poor accuracy [14-17]. In a nationwide study done in France, the survival prediction accuracy was 42.8% and 25.6% for the Tokuhashi and Tomita scoring systems, respectively [18]. The inability to reflect prolonged survival due to novel developments in cancer treatments, like molecular targeted therapies, immunotherapy, and hormonal therapies, leads to the occurrence of inaccuracies in these systems.
More recently, the New England Spinal Metastasis Score (NESMS), consisting of a modified Bauer score, serum albumin level, and ambulatory status, was introduced in 2015 [19] (Table 2). The authors developed the scoring system using multi-institutional data and validated the system retrospectively [20,21] and prospectively [22,23] as an accurate and reliable prediction tool for spinal metastasis. In a recently published prospective study, the authors reported that the NESMS differentiated patient survival notably better than the traditional scoring systems (Tokuhashi, Tomita, and Spinal Instability Neoplastic Score [SINS]) [24].
Table 2.
The New England Spinal Metastasis Score
| Components | Modified Bauer points | NESMS points |
|---|---|---|
| Modified Bauer score components | ||
| Primary tumor is not lung | 1 | |
| Primary tumor is breast or kidney | 1 | |
| Solitary skeletal metastasis | 1 | |
| No visceral metastasis | 1 | |
| Modified Bauer score | ||
| ≤2 | 0 | |
| ≥3 | 2 | |
| Serum albumin (g/dL) | ||
| <3.5 | 0 | |
| ≥3.5 | 1 | |
| Ambulatory status | ||
| Non-ambulatory | 0 | |
| Intact or impaired | 1 |
NESMS, New England Spinal Metastasis Score.
Many authors have also utilized novel methodologies, including machine-learning algorithms, to develop decision-making systems. The Skeletal Oncology Research Group (SORG) conducted a study comparing the estimated survival of 649 patients predicted by classic, nomogram, and boosting algorithms [25]. In their study, the authors suggested that the nomogram was intuitive and accurate. More recently, the SORG created a novel prognostic prediction model for spinal metastasis using a machine-learning algorithm [26], which is referred to as one of the “second-generation models” [27]. Subsequent studies have externally validated these models [28-30].
2. Principle-based systems
Principle-based decision-making systems could provide more specific treatment suggestions for each patient with spinal metastasis based on their oncologic, systemic, and functional status in contrast to prognostic models, which only predict patients’ life expectancy. Additionally, these systems could reflect advancements in systemic, radiation, and surgical treatments, like molecular target therapy, SRS, and separation surgery, better than classificationbased prognostic models (Table 3).
Table 3.
The NOMS decision framework
| Neurologic (N) | Oncologic (O) | Mechanical (M) | Systemic (S) | Decision |
|---|---|---|---|---|
| Low-grade ESCC+no myelopathy | Radiosensitive | Stable | cEBRT | |
| Radiosensitive | Unstable | Stabilization followed by cEBRT | ||
| Radioresistant | Stable | SRS | ||
| Radioresistant | Unstable | Stabilization followed by SRS | ||
| High-grade ESCC±myelopathy | Radiosensitive | Stable | cEBRT | |
| Radiosensitive | Unstable | Stabilization followed by cEBRT | ||
| Radioresistant | Stable | Able to tolerate surgery | Decompression/stabilization followed by SRS | |
| Radioresistant | Stable | Unable to tolerate surgery | cEBRT | |
| Radioresistant | Unstable | Able to tolerate surgery | Decompression/stabilization followed by SRS | |
| Radioresistant | Unstable | Unable to tolerate surgery | Stabilization followed by cEBRT |
Adapted from Chang SY, et al. Orthop Surg 2019;11:552-9 [35].
NOMS, neurologic, oncologic, mechanical, and systemic; ESCC, epidural spinal cord compression; cEBRT, conventional external beam radiation; SRS, stereotactic radiosurgery.
The NOMS framework was first introduced in 2006 as a principle-based decision-making system [31]. In this framework, the neurologic (N) component was assessed using the Bilsky grade [32]. The oncologic (O) component is determined based on the expected response to available treatments, primarily radiotherapy, whereas the mechanical (M) component is determined by assessing the spinal column stability using the SINS. This could guide surgeons in deciding whether to perform surgical stabilization regardless of other components [33]. Finally, the systemic (S) component determines whether the patient can tolerate the suggested treatment. The most appropriate treatment for each spinal metastasis patient is suggested based on these four components, including novel treatment modalities, like SRS and separation surgery [31].
Paton et al. [34] introduced the “LMNOP” system as a modification of the NOMS framework. Two additional components were added: the number and location of metastatic spinal lesions (L) and the response to previous treatment (P). The response to previous systemic therapy or radiotherapy was considered to be an important factor in selecting an appropriate treatment option for each patient. For example, a newly diagnosed cancer patient with symptomatic spinal metastasis (synchronous metastasis), having several residual cancer treatment options, is expected to have longer survival compared to those with spinal metastasis diagnosed during the course of cancer treatment (metachronous metastasis) [35].
3. Current trends and future directions
The prognostic models or decision-making systems for metastatic spinal tumors need to evolve due to recent advancements in cancer genetics and the introduction of novel treatment techniques. The suggestions for future spinal metastasis decision-making systems based on the trends evident in the recent literature are as follows: (1) development and validation using a multi-institutional or multinational database; (2) consideration of tumor genetics; (3) utilization of novel methodologies, like artificial intelligence; and (4) integration of prognostic models and principle-based decision-making systems.
The sample size is crucial for the performance of predictive algorithms and decision-making systems. Studies with a large sample size from a multi-institutional or multinational cohort should be conducted for developing an accurate and reliable prognostic model. Therefore, recently introduced predictive algorithms have been developed and validated using multi-institutional databases [19,25,36]. Additionally, a large database from multicenter and multinational tumor registries should be a prerequisite in developing future prognostic models for spinal metastasis.
The evolution of biological treatments, like targeted molecular therapy and immunotherapy, has brought a paradigm shift in cancer treatment. Determining the genetic subtypes of primary malignancy provides a guide for these biological treatments. Hence, its importance has been increasing [37]. Examples of target mutations include epidermal growth factor receptor (EGFR) in nonsmall cell lung cancer, v-raf murine sarcoma viral oncogene homolog B1 in melanoma, and hormonal receptors in breast and prostate cancers. Recently, Kim et al. [38] discovered that the addition of EGFR mutation positivity to the NESMS system improves its discrimination ability. Their results emphasize the importance of genetic profiles while establishing treatment strategies for spinal metastasis.
Novel computational methodologies are being utilized for developing prognostic models for metastatic spinal tumors. Traditionally, scoring systems have been created based on regression analysis (logistic or proportional hazard). However, the SORG used multiple machinelearning algorithms, like gradient boosting, decision trees, random forests, and neural networks, for developing their prognostic models [25,39]. More recently, Karhade et al. [36] developed and introduced predictive algorithms for 6-week mortality in patients with spinal metastasis using five different machine-learning algorithms. These algorithms could assist surgeons in identifying patients for whom surgery could do more harm than good [36]. These evolving computational methodologies would be extensively utilized in predicting the prognosis of spinal metastatic tumors.
Finally, classification- and principle-based systems should be integrated into future decision-making systems. Classification-based systems or prognostic models, estimate the patient’s remaining survival, whereas principlebased systems estimate the most appropriate treatment option based on these survival estimations. Generally, two separate systems are used by oncologists and spine surgeons while choosing an appropriate decision-making process for patients with spinal metastasis. Therefore, novel decision-making systems should combine these two systems and estimate the remaining survival and the most appropriate management option, simultaneously.
Radiotherapy for Spinal Metastasis
1. Stereotactic radiosurgery bringing a paradigm shift
Stereotactic radiotherapy is effective in local tumor control with relatively low complication rates in patients with spinal metastasis [7]. In the treatment of spinal metastasis, SRS has become a game-changer because of recent technical improvements, like radiation delivery systems (imageguided, intensity-modulated) and software [40]. Previous studies have revealed that SRS locally controls spinal metastatic tumors for an extended period, which is not influenced by the tumor histology or radiosensitivity of primary cancer [41]. The effectiveness of SRS, independent of tumor histology, has expanded the role of radiotherapy in managing patients with spinal metastases.
The clinical practice of surgeons treating patients with spinal metastases has been reshaped by SRS by reducing the invasiveness of surgical treatment. For example, in single metastatic lesions not accompanied by spinal cord compression, SRS could be applied as a definitive treatment [42]. Curative surgical procedures with high complication rates, like total en-bloc spondylectomy (TES), have been replaced by SRS, which demonstrated a local control rate of 84%–88% in single metastatic lesions [43,44]. In patients with high-grade metastatic epidural spinal cord compression (MESCC), the effectiveness of adjuvant SRS reduces the need for aggressive debulking surgery and makes separation surgery, in which tumor resection is limited to decompressing the spinal cord.
2. Vertebral compression fracture following stereotactic radiosurgery
An increased risk of vertebral compression fractures (VCF) after radiotherapy is a pitfall of SRS. VCF is reported after SRS in up to 36% of patients, compared to 5% after conventional radiotherapy [45]. VCF is dosedependent and occurs more frequently when over 20 Gy per fraction of radiation dose is given to patients having risk factors [46]. The risk factors for VCF after SRS are as follows: (1) older age, (2) lytic lesions, and (3) spinal malalignment. In patients with these risk factors, a radiation dose of less than 16–18 Gy per fraction is recommended [47]. Additionally, preventive stabilization surgery could be considered before performing SRS. SINS could be applied to assess the mechanical instability of the metastatic lesion and predict further vertebral collapse after SRS. This could assist in deciding whether to perform surgical stabilization before SRS or not [33,48].
3. The interval between surgery and radiotherapy
In the literature, controversy exists on the adequate timing of adjuvant radiotherapy following surgical treatment. This could be associated with wound complications. Based on recent systemic reviews and expert opinions, it is recommended to keep an interval of 2 weeks (minimum of 7 days) between surgery and radiotherapy [49,50]. A few authors believe that SRS could shorten the interval compared to conventional radiotherapy. In a previous study, Versteeg et al. [51] reported that no increase in wound complications was seen at 90 days after surgery, despite administering SRS within 24 hours of surgery. The findings of previous studies suggest that SRS was associated with fewer wound complications than conventional radiotherapy when administered at a similar time interval between surgeries [52-54]. However, due to the lack of highlevel evidence, the extent to which the interval between surgery and adjuvant SRS could be reduced remains debatable. It should also be noted that minimally invasive surgical techniques, discussed later in this review, could reduce the interval between surgery and radiotherapy.
Surgery for Spinal Metastasis
1. Surgical indications
The purpose of surgical treatment for patients with metastatic spinal tumors is pain relief and improving neurological deficits through nerve decompression and stabilization. Surgical indications for spinal metastasis generally include uncontrolled pain and neurological deficits, like motor weakness in the extremities [55]. As suggested by the decision-making systems, radioresistant tumors with high-grade epidural spinal cord compression are a typical indication for surgical treatment [31,34].
Mechanical instability is considered an independent indication for stabilization, as suggested in the NOMS and LMNOP systems [31,34]. SINS is an independent tool developed to guide surgeons in determining the need for surgical stabilization in each patient based on clinical and radiological findings [56] (Table 4). A score of ≥13 is evidence of spinal instability warranting surgical stabilization. For patients with impending instability (intermediate SINS score of 7–12), the decision of performing surgical stabilization is often difficult. Lenschow et al. [57] reviewed 331 spinal metastasis patients with intermediate SINS and found no significant differences in neurological outcomes between instrumented and noninstrumented patients. However, an increase in surgical complications was noted in the instrumented group [57]. Kim et al. [58] suggested that surgical stabilization should be performed in patients having >50% vertebral body collapse with intermediate SINS.
Table 4.
Spinal Instability Neoplastic Score system
| SINS component | Score |
|---|---|
| Location | |
| Junctional (occiput–C2, C7–T2, T11–L1, L5–S1) | 3 |
| Mobile spine (C3–C6, L2–L4) | 2 |
| Semi rigid (T3–T10) | 1 |
| Rigid (S2–S5) | 0 |
| Paina) | |
| Yes | 3 |
| Occasional pain but not mechanical | 1 |
| Pain-free lesion | 0 |
| Bone lesion | |
| Lytic | 2 |
| Mixed (lytic/blastic) | 1 |
| Blastic | 0 |
| Radiographic spinal alignment | |
| Subluxation/translation present | 4 |
| De novo deformity (kyphosis/scoliosis) | 2 |
| Normal alignment | 0 |
| Vertebral body collapse | |
| >50% collapse | 3 |
| <50% collapse | 2 |
| No collapse with >50% body involved | 1 |
| None of the above | 0 |
| Posterolateral involvement of spinal elementsb) | |
| Bilateral | 3 |
| Unilateral | 1 |
| None of the above | 0 |
SINS, Spinal Instability Neoplastic Score.
Pain improvement with recumbency and/or pain with movement/loading of spine.
Facet, pedicle, or costovertebral joint fracture or replacement with tumor.
Estimated life expectancy is considered the most important deciding factor in performing surgery for metastatic spinal tumors. Based on the findings of previous studies, more than 3 months of estimated survival is a prerequisite for proceeding with surgical treatment [59,60]. Several prognostic models have been utilized for predicting the survival period of patients with spinal metastases. Additionally, the performance status of the patient should be good enough to have sufficient tolerance for the surgical treatment. Surgical treatment for spinal metastasis can be performed on patients with any previously mentioned surgical indications (e.g., mechanical instability or MESCC) on meeting these conditions.
2. Separation surgery and stereotactic radiosurgery (hybrid therapy)
As mentioned previously, the improved local control ability of SRS, regardless of tumor histology, further reduces the need for invasive surgical procedures in patients with spinal metastases [61] (Fig. 1). The role of decompressive surgery in MESCC can be refined to secure the spinal cord in the era of SRS [62]. “Separation surgery” is defined as a surgical procedure in which the tumor resection is limited to decompressing the spinal cord and creating a gap between the spinal cord and the tumor to provide a safe target for SRS [63]. Circumferential decompression (360°) was performed to ensure a complete re-expansion of the dural sac with at least a 2–3 mm gap between the tumor and spinal cord. Among several surgical approaches, the posterolateral transpedicular approach described by Bilsky et al. [64] is a safe, effective, and versatile method for circumferential spinal cord decompression.
Fig. 1.
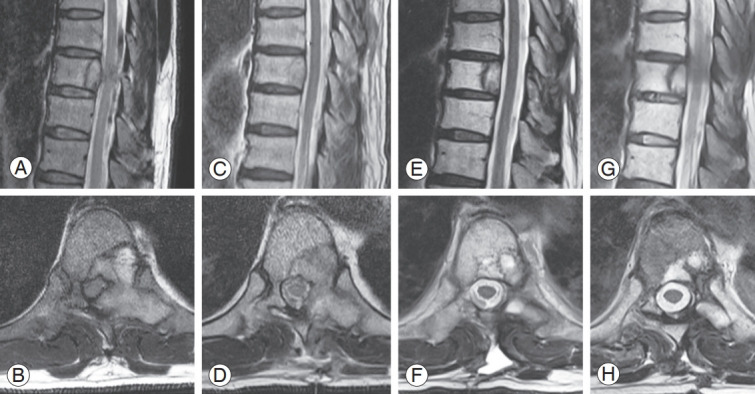
A case of metastatic epidural spinal cord compression treated by hybrid therapy (separation surgery and stereotactic radiosurgery [SRS]). (A, B) Preoperative magnetic resonance imaging (MRI) shows severe spinal cord compression at T9. (C, D) MRI at postoperative 2 weeks after separation surgery shows a gap created between the spinal cord and residual tumor. (E, F) Following a single-fraction SRS, which was performed 3 weeks after the separation surgery, the residual tumor was completely ablated. (G, H) At postoperative 2 years, there is no evidence of tumor in the follow-up MRI.
In separation surgery, ventral decompression is the most challenging and crucial surgical step along with intraoperative confirmation of sufficient decompression. In previous studies, sufficient ventral decompression has been associated with improved long-term local control [65]. For adequate ventral decompression, the removal of 20% of the posterior vertebral body after posterior longitudinal ligament resection is generally required [63]. Intraoperative confirmation of ventral decompression can be performed with a stereotactic navigation system or ultrasonography [66] (Fig. 2).
Fig. 2.
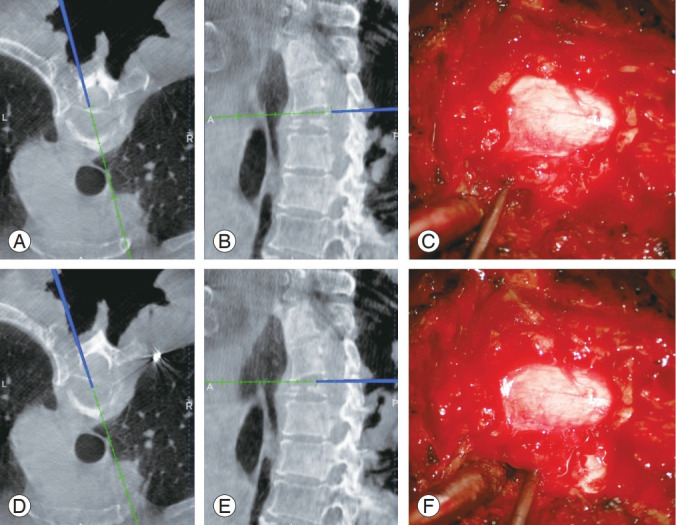
Adequate ventral decompression confirmed by the stereotactic spinal navigation system during a separation surgery using a transpedicular approach. (A–C) Before ventral decompression, the navigation probe is located on the posterior surface of the vertebral body. (D–F) After ventral decompression is achieved by removing the posterior vertebral body, the navigation probe is located within the vertebral body.
Interdisciplinary decision-making systems, like the NOMS framework, include separation surgery as the treatment of choice for patients with high-grade spinal cord compression of radioresistant tumors when combined with SRS [31]. Additionally, several previous studies have reported favorable outcomes of separation surgery followed by SRS (hybrid therapy) [67-69]. A recent metaanalysis by Kang et al. [70] reported that the pooled local progression rate at 1 year following hybrid therapy was 10.2%. Additionally, their study revealed that factors like low doses per fraction, previous radiotherapy, and colorectal cancer were significantly associated with local tumor progression [70]. Favorable results of hybrid therapy limit spine surgeons from performing en-bloc resections in patients with spinal metastasis carrying significant surgical morbidity.
3. Minimally invasive or minimal-access surgery
Minimally invasive surgery (MIS) or minimal-access surgery for spinal metastasis could reduce surgical morbidities and facilitate quick recovery after surgery. This would allow cancer patients to restart their oncological treatment promptly. Previous studies have introduced tubular retractor systems and thoracoscopic assistance for anterior surgeries [71,72], minimally invasive approaches for decompression, and corpectomy for posterior surgeries [73,74]. Other MIS techniques, like percutaneous pedicle screw fixations and image-guided stereotactic navigation systems, are also effective treatment modalities in spinal metastasis surgery [68,75].
In previous studies, it was revealed that compared to open surgery, MIS displays equivalent surgical outcomes and has fewer complications at the surgical site [76-80]. Additionally, a recent systematic review comprising of 26 studies summarized that MIS could potentially reduce surgical site infections (SSIs), hospital stay, and blood loss in patients with spinal metastasis without decreasing instrument accuracy and overall patient outcomes [81].
4. Role of curative surgery (en-bloc resection)
Surgical treatment for spinal metastasis is performed for palliative purposes and the role of curative tumor resection, including TES, is limited. En-bloc resection of the metastatic spinal tumor should only be considered in isolated metastatic lesions of slow-growing malignancy, with an expected survival of more than 2 years and an acceptable performance status because of the high surgical morbidity [82]. En-bloc resection for spinal metastasis could also be considered in conditions where SRS is not available [83].
Previous studies have reported improved survival and function following spinal metastasectomy [84-86]. Recently, Kato et al. [87] reported medium-to-long-term clinical outcomes of spinal metastasis, in which the 3-year and 5-year survival rates for 124 patients were 70% and 60%, respectively. Contrastingly, some authors recently reported that spinal metastasectomy, including TES, for spinal metastasis did not affect oncological outcomes [88]. These conflicting results and recent reports of improved efficacy of novel radiotherapies suggest that a more careful patient selection through a multidisciplinary team approach is required for determining whether curative surgery should be performed for spinal metastasis.
5. Prevention of perioperative complications
The reported overall complication rate ranges from 10% to 66.7% after surgical treatment for metastatic spinal tumors [89]. Minimizing all possible perioperative complications is crucial in patients with spinal metastasis because it has been reported that 30-day postoperative complications are associated with worse patient survival [90]. In this review, the following common perioperative complications occurring after surgery in metastatic spinal tumors have been discussed: (1) SSI, (2) failure of instrumentation, and (3) intraoperative bleeding.
SSI is experienced by up to 30% of patients treated surgically for spinal metastasis patients. SSI is more prevalent than in patients undergoing other spinal surgeries [89]. Moreover, SSI is the most common reason for reoperation after surgical treatment of metastatic spinal tumors [91,92]. Following spinal metastasis surgery, the proposed risk factors for SSI are poor nutrition, diabetes mellitus, smoking, obesity, and adjuvant therapies, like radiotherapy and systemic treatment [93-95]. Therefore, to minimize the incidence of SSI, all possible preventive measures (e.g., nutritional therapy and an adequate interval between surgery and radiotherapy) should be administered promptly by a multidisciplinary team. Recently, a web-based calculator that can predict the occurrence of SSI and the associated risk of reoperation has been developed to help minimize SSI [96].
Instrumentation failure is the second reason for reoperation after surgery for metastatic spinal tumors [91]. The risk factors suggested for instrumentation failure are longlevel surgery, combined chest wall resection, and higher preoperative SINS [97-99]. However, it is controversial if adjuvant radiotherapy should be considered to be a risk factor for instrumentation failure [100]. Prolonged survival of patients with spinal metastasis is also associated with increased instrumentation failures [101]. Currently, limited evidence is available on the role of additional fusion procedures during surgical stabilization in reducing instrumentation failure [93,102,103]. This study suggests that the two types of instrumentation failure, early and late, should be distinguished in future studies because the mechanisms of these two failures are different [104]. Early failure occurs due to insufficient fixation strength or stability of the construct, whereas late failure occurs due to deformity progression due to tumor progression or lack of fusion.
Intraoperative bleeding can often be extensive in spinal metastasis surgery, leading to serious cardiovascular or cerebral complications [105]. Therefore, before surgery for a metastatic spinal tumor, preoperative embolization has been recommended for hypervascular tumors, like kidney and thyroid cancers. A recent meta-analysis reported significantly less intraoperative blood loss, fewer blood transfusions, and shorter surgical duration in the embolization group for hypervascular tumors [106]. However, in this analysis, scanty evidence was available to support the routine administration of preoperative embolization for nonhypervascular spinal metastases [106]. Nevertheless, when aggressive debulking surgery, like piecemeal corpectomy, is planned, preoperative embolization can help in reducing intraoperative bleeding [107]. To maintain the effect of preoperative embolization and avoid increased bleeding due to reperfusion, the delay between embolization and surgery should be minimized and not exceed 24 hours [108].
Conclusions
The decision-making process for patients with metastatic spinal tumors is challenging and requires a multidisciplinary approach. Recent advancements in radiotherapy and surgical techniques have markedly improved clinical outcomes in patients with spinal metastases. Therefore, the ongoing evolution of decision-making systems should also play a crucial role in state-of-art care for metastatic spinal tumors.
Footnotes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: SHH, SYC; data curation: SHH, DHK, SYC; formal analysis: HK, DHK; methodology: BSC, SYC; project administration: BSC, HK; visualization: SHH, DHK; writing–original draft: SHH, BSC, HK, SYC; writing–review & editing: SHH, BSC,HK, DHK, SYC.
References
- 1.White AP, Kwon BK, Lindskog DM, Friedlaender GE, Grauer JN. Metastatic disease of the spine. J Am Acad Orthop Surg. 2006;14:587–98. doi: 10.5435/00124635-200610000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Laufer I, Sciubba DM, Madera M, et al. Surgical management of metastatic spinal tumors. Cancer Control. 2012;19:122–8. doi: 10.1177/107327481201900206. [DOI] [PubMed] [Google Scholar]
- 3.Perrin RG, Laxton AW. Metastatic spine disease: epidemiology, pathophysiology, and evaluation of patients. Neurosurg Clin N Am. 2004;15:365–73. doi: 10.1016/j.nec.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Nathan SS, Healey JH, Mellano D, et al. Survival in patients operated on for pathologic fracture: implications for end-of-life orthopedic care. J Clin Oncol. 2005;23:6072–82. doi: 10.1200/JCO.2005.08.104. [DOI] [PubMed] [Google Scholar]
- 5.Curtin M, Piggott RP, Murphy EP, et al. Spinal metastatic disease: a review of the role of the multidisciplinary team. Orthop Surg. 2017;9:145–51. doi: 10.1111/os.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed AK, Goodwin CR, Heravi A, et al. Predicting survival for metastatic spine disease: a comparison of nine scoring systems. Spine J. 2018;18:1804–14. doi: 10.1016/j.spinee.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Barzilai O, Fisher CG, Bilsky MH. State of the art treatment of spinal metastatic disease. Neurosurgery. 2018;82:757–69. doi: 10.1093/neuros/nyx567. [DOI] [PubMed] [Google Scholar]
- 8.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2001;26:298–306. doi: 10.1097/00007632-200102010-00016. [DOI] [PubMed] [Google Scholar]
- 9.Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005;30:2186–91. doi: 10.1097/01.brs.0000180401.06919.a5. [DOI] [PubMed] [Google Scholar]
- 10.Bauer HC, Wedin R. Survival after surgery for spinal and extremity metastases: prognostication in 241 patients. Acta Orthop Scand. 1995;66:143–6. doi: 10.3109/17453679508995508. [DOI] [PubMed] [Google Scholar]
- 11.van der Linden YM, Dijkstra SP, Vonk EJ, Marijnen CA, Leer JW, Dutch Bone Metastasis Study Group Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer. 2005;103:320–8. doi: 10.1002/cncr.20756. [DOI] [PubMed] [Google Scholar]
- 12.Bartels RH, Feuth T, van der Maazen R, et al. Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer. 2007;110:2042–9. doi: 10.1002/cncr.23002. [DOI] [PubMed] [Google Scholar]
- 13.Katagiri H, Okada R, Takagi T, et al. New prognostic factors and scoring system for patients with skeletal metastasis. Cancer Med. 2014;3:1359–67. doi: 10.1002/cam4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hessler C, Vettorazzi E, Madert J, Bokemeyer C, Panse J. Actual and predicted survival time of patients with spinal metastases of lung cancer: evaluation of the robustness of the Tokuhashi score. Spine (Phila Pa 1976) 2011;36:983–9. doi: 10.1097/BRS.0b013e3181e8f7f8. [DOI] [PubMed] [Google Scholar]
- 15.Zoccali C, Skoch J, Walter CM, Torabi M, Borgstrom M, Baaj AA. The Tokuhashi score: effectiveness and pitfalls. Eur Spine J. 2016;25:673–8. doi: 10.1007/s00586-015-4339-6. [DOI] [PubMed] [Google Scholar]
- 16.Nater A, Tetreault LA, Kopjar B, et al. Predictive factors of survival in a surgical series of metastatic epidural spinal cord compression and complete external validation of 8 multivariate models of survival in a prospective North American multicenter study. Cancer. 2018;124:3536–50. doi: 10.1002/cncr.31585. [DOI] [PubMed] [Google Scholar]
- 17.Nakajima H, Watanabe S, Honjoh K, et al. Prognosis after palliative surgery for patients with spinal metastasis: comparison of predicted and actual survival. Cancers (Basel) 2022;14:3868. doi: 10.3390/cancers14163868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tabourel G, Terrier LM, Dubory A, et al. Are spine metastasis survival scoring systems outdated and do they underestimate life expectancy?: caution in surgical recommendation guidance. J Neurosurg Spine. 2021;35:527–34. doi: 10.3171/2020.12.SPINE201741. [DOI] [PubMed] [Google Scholar]
- 19.Ghori AK, Leonard DA, Schoenfeld AJ, et al. Modeling 1-year survival after surgery on the metastatic spine. Spine J. 2015;15:2345–50. doi: 10.1016/j.spinee.2015.06.061. [DOI] [PubMed] [Google Scholar]
- 20.Schoenfeld AJ, Le HV, Marjoua Y, et al. Assessing the utility of a clinical prediction score regarding 30-day morbidity and mortality following metastatic spinal surgery: the New England Spinal Metastasis Score (NESMS) Spine J. 2016;16:482–90. doi: 10.1016/j.spinee.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 21.Shi DD, Chen YH, Lam TC, et al. Assessing the utility of a prognostication model to predict 1-year mortality in patients undergoing radiation therapy for spinal metastases. Spine J. 2018;18:935–40. doi: 10.1016/j.spinee.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Schoenfeld AJ, Blucher JA, Barton LB, et al. Design of the prospective observational study of spinal metastasis treatment (POST) Spine J. 2020;20:572–9. doi: 10.1016/j.spinee.2019.10.021. [DOI] [PubMed] [Google Scholar]
- 23.Schoenfeld AJ, Ferrone ML, Schwab JH, et al. Prospective validation of a clinical prediction score for survival in patients with spinal metastases: the New England Spinal Metastasis Score. Spine J. 2021;21:28–36. doi: 10.1016/j.spinee.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Schoenfeld AJ, Ferrone ML, Blucher JA, et al. Prospective comparison of the accuracy of the New England Spinal Metastasis Score (NESMS) to legacy scoring systems in prognosticating outcomes following treatment of spinal metastases. Spine J. 2022;22:39–48. doi: 10.1016/j.spinee.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paulino Pereira NR, Janssen SJ, van Dijk E, et al. Development of a prognostic survival algorithm for patients with metastatic spine disease. J Bone Joint Surg Am. 2016;98:1767–76. doi: 10.2106/JBJS.15.00975. [DOI] [PubMed] [Google Scholar]
- 26.Karhade AV, Thio QC, Ogink PT, et al. Predicting 90-day and 1-year mortality in spinal metastatic disease: development and internal validation. Neurosurgery. 2019;85:E671–81. doi: 10.1093/neuros/nyz070. [DOI] [PubMed] [Google Scholar]
- 27.Pennington Z, Ehresman J, Cottrill E, et al. To operate, or not to operate?: narrative review of the role of survival predictors in patient selection for operative management of patients with metastatic spine disease. J Neurosurg Spine. 2020;34:135–49. doi: 10.3171/2020.6.SPINE20707. [DOI] [PubMed] [Google Scholar]
- 28.Karhade AV, Ahmed AK, Pennington Z, et al. External validation of the SORG 90-day and 1-year machine learning algorithms for survival in spinal metastatic disease. Spine J. 2020;20:14–21. doi: 10.1016/j.spinee.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Bongers ME, Karhade AV, Villavieja J, et al. Does the SORG algorithm generalize to a contemporary cohort of patients with spinal metastases on external validation? Spine J. 2020;20:1646–52. doi: 10.1016/j.spinee.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Shah AA, Karhade AV, Park HY, et al. Updated external validation of the SORG machine learning algorithms for prediction of ninety-day and one-year mortality after surgery for spinal metastasis. Spine J. 2021;21:1679–86. doi: 10.1016/j.spinee.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 31.Laufer I, Rubin DG, Lis E, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013;18:744–51. doi: 10.1634/theoncologist.2012-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bilsky M, Smith M. Surgical approach to epidural spinal cord compression. Hematol Oncol Clin North Am. 2006;20:1307–17. doi: 10.1016/j.hoc.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976) 2010;35:E1221–9. doi: 10.1097/BRS.0b013e3181e16ae2. [DOI] [PubMed] [Google Scholar]
- 34.Paton GR, Frangou E, Fourney DR. Contemporary treatment strategy for spinal metastasis: the “LMNOP” system. Can J Neurol Sci. 2011;38:396–403. doi: 10.1017/s031716710001177x. [DOI] [PubMed] [Google Scholar]
- 35.Chang SY, Chang BS, Lee CK, Kim H. Remaining systemic treatment options: a valuable predictor of survival and functional outcomes after surgical treatment for spinal metastasis. Orthop Surg. 2019;11:552–9. doi: 10.1111/os.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karhade AV, Fenn B, Groot OQ, et al. Development and external validation of predictive algorithms for 6-week mortality in spinal metastasis using 4,304 patients from 5 institutions. Spine J. 2022 Jul 14; doi: 10.1016/j.spinee.2022.07.089. [Epub]. [DOI] [PubMed] [Google Scholar]
- 37.Choi D, Bilsky M, Fehlings M, Fisher C, Gokaslan Z. Spine oncology: metastatic spine tumors. Neurosurgery. 2017;80(3S):S131–7. doi: 10.1093/neuros/nyw084. [DOI] [PubMed] [Google Scholar]
- 38.Kim H, Chang SY, Son J, Mok S, Park SC, Chang BS. The effect of adding biological factors to the decisionmaking process for spinal metastasis of non-small cell lung cancer. J Clin Med. 2021;10:1119. doi: 10.3390/jcm10051119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karhade AV, Shin JH, Schwab JH. Prognostic models for spinal metastatic disease: evolution of methodologies, limitations, and future opportunities. Ann Transl Med. 2019;7:219. doi: 10.21037/atm.2019.04.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alongi F, Arcangeli S, Filippi AR, Ricardi U, Scorsetti M. Review and uses of stereotactic body radiation therapy for oligometastases. Oncologist. 2012;17:1100–7. doi: 10.1634/theoncologist.2012-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamada Y, Katsoulakis E, Laufer I, et al. The impact of histology and delivered dose on local control of spinal metastases treated with stereotactic radiosurgery. Neurosurg Focus. 2017;42:E6. doi: 10.3171/2016.9.FOCUS16369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bilsky MH, Laufer I, Burch S. Shifting paradigms in the treatment of metastatic spine disease. Spine (Phila Pa 1976) 2009;34(22 Suppl):S101–7. doi: 10.1097/BRS.0b013e3181bac4b2. [DOI] [PubMed] [Google Scholar]
- 43.Garg AK, Shiu AS, Yang J, et al. Phase 1/2 trial of single-session stereotactic body radiotherapy for previously unirradiated spinal metastases. Cancer. 2012;118:5069–77. doi: 10.1002/cncr.27530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ho JC, Tang C, Deegan BJ, et al. The use of spine stereotactic radiosurgery for oligometastatic disease. J Neurosurg Spine. 2016;25:239–47. doi: 10.3171/2016.1.SPINE151166. [DOI] [PubMed] [Google Scholar]
- 45.Sahgal A, Whyne CM, Ma L, Larson DA, Fehlings MG. Vertebral compression fracture after stereotactic body radiotherapy for spinal metastases. Lancet Oncol. 2013;14:e310–20. doi: 10.1016/S1470-2045(13)70101-3. [DOI] [PubMed] [Google Scholar]
- 46.Sahgal A, Atenafu EG, Chao S, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol. 2013;31:3426–31. doi: 10.1200/JCO.2013.50.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boyce-Fappiano D, Elibe E, Schultz L, et al. Analysis of the factors contributing to vertebral compression fractures after spine stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2017;97:236–45. doi: 10.1016/j.ijrobp.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 48.Chang SY, Ha JH, Seo SG, Chang BS, Lee CK, Kim H. Prognosis of single spinal metastatic tumors: predictive value of the spinal instability neoplastic score system for spinal adverse events. Asian Spine J. 2018;12:919–26. doi: 10.31616/asj.2018.12.5.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar N, Madhu S, Bohra H, et al. Is there an optimal timing between radiotherapy and surgery to reduce wound complications in metastatic spine disease?: a systematic review. Eur Spine J. 2020;29:3080–115. doi: 10.1007/s00586-020-06478-5. [DOI] [PubMed] [Google Scholar]
- 50.Lee RS, Batke J, Weir L, Dea N, Fisher CG. Timing of surgery and radiotherapy in the management of metastatic spine disease: expert opinion. J Spine Surg. 2018;4:368–73. doi: 10.21037/jss.2018.05.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Versteeg AL, van der Velden JM, Hes J, et al. Stereotactic radiotherapy followed by surgical stabilization within 24 h for unstable spinal metastases; a stage I/IIa study according to the IDEAL framework. Front Oncol. 2018;8:626. doi: 10.3389/fonc.2018.00626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keam J, Bilsky MH, Laufer I, et al. No association between excessive wound complications and preoperative high-dose, hypofractionated, image-guided radiation therapy for spine metastasis. J Neurosurg Spine. 2014;20:411–20. doi: 10.3171/2013.12.SPINE12811. [DOI] [PubMed] [Google Scholar]
- 53.Moulding HD, Elder JB, Lis E, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine. 2010;13:87–93. doi: 10.3171/2010.3.SPINE09639. [DOI] [PubMed] [Google Scholar]
- 54.Redmond KJ, Sciubba D, Khan M, et al. A phase 2 study of post-operative stereotactic body radiation therapy (SBRT) for solid tumor spine metastases. Int J Radiat Oncol Biol Phys. 2020;106:261–8. doi: 10.1016/j.ijrobp.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 55.Laufer I, Zuckerman SL, Bird JE, et al. Predicting neurologic recovery after surgery in patients with deficits secondary to MESCC: systematic review. Spine (Phila Pa 1976) 2016;41(Suppl 20):S224–30. doi: 10.1097/BRS.0000000000001827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee CH, Hong JT, Lee SH, et al. Is the spinal instability neoplastic score accurate and reliable in predicting vertebral compression fractures for spinal metastasis?: a systematic review and qualitative analysis. J Korean Neurosurg Soc. 2021;64:4–12. doi: 10.3340/jkns.2020.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lenschow M, Lenz M, von Spreckelsen N, et al. Impact of spinal instrumentation on neurological outcome in patients with intermediate Spinal Instability Neoplastic Score (SINS) Cancers (Basel) 2022;14:2193. doi: 10.3390/cancers14092193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim YH, Kim J, Chang SY, Kim H, Chang BS. Treatment strategy for impending instability in spinal metastases. Clin Orthop Surg. 2020;12:337–42. doi: 10.4055/cios20014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.White BD, Stirling AJ, Paterson E, Asquith-Coe K, Melder A, Guideline Development Group Diagnosis and management of patients at risk of or with metastatic spinal cord compression: summary of NICE guidance. BMJ. 2008;337:a2538. doi: 10.1136/bmj.a2538. [DOI] [PubMed] [Google Scholar]
- 60.Choi D, Crockard A, Bunger C, et al. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 2010;19:215–22. doi: 10.1007/s00586-009-1252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Conti A, Acker G, Kluge A, et al. Decision making in patients with metastatic spine. the role of minimally invasive treatment modalities. Front Oncol. 2019;9:915. doi: 10.3389/fonc.2019.00915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Orenday-Barraza JM, Cavagnaro MJ, Avila MJ, et al. 10-Year trends in the surgical management of patients with spinal metastases: a scoping review. World Neurosurg. 2022;157:170–86. doi: 10.1016/j.wneu.2021.10.086. [DOI] [PubMed] [Google Scholar]
- 63.Di Perna G, Cofano F, Mantovani C, et al. Separation surgery for metastatic epidural spinal cord compression: a qualitative review. J Bone Oncol. 2020;25:100320. doi: 10.1016/j.jbo.2020.100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bilsky MH, Boland P, Lis E, Raizer JJ, Healey JH. Single-stage posterolateral transpedicle approach for spondylectomy, epidural decompression, and circumferential fusion of spinal metastases. Spine (Phila Pa 1976) 2000;25:2240–50. doi: 10.1097/00007632-200009010-00016. [DOI] [PubMed] [Google Scholar]
- 65.Pennington Z, Pairojboriboon S, Chen X, et al. Utility of expanded anterior column resection versus decompression-alone for local control in the management of carcinomatous vertebral column metastases undergoing adjuvant stereotactic radiotherapy. Spine J. 2022;22:835–46. doi: 10.1016/j.spinee.2021.10.016. [DOI] [PubMed] [Google Scholar]
- 66.Kelly PD, Zuckerman SL, Yamada Y, et al. Image guidance in spine tumor surgery. Neurosurg Rev. 2020;43:1007–17. doi: 10.1007/s10143-019-01123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hu JX, Gong YN, Jiang XD, et al. Local tumor control for metastatic epidural spinal cord compression following separation surgery with adjuvant CyberKnife stereotactic radiotherapy or image-guided intensity-modulated radiotherapy. World Neurosurg. 2020;141:e76–85. doi: 10.1016/j.wneu.2020.04.183. [DOI] [PubMed] [Google Scholar]
- 68.Nasser R, Nakhla J, Echt M, et al. Minimally invasive separation surgery with intraoperative stereotactic guidance: a feasibility study. World Neurosurg. 2018;109:68–76. doi: 10.1016/j.wneu.2017.09.067. [DOI] [PubMed] [Google Scholar]
- 69.Laufer I, Iorgulescu JB, Chapman T, et al. Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. J Neurosurg Spine. 2013;18:207–14. doi: 10.3171/2012.11.SPINE12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kang DH, Chang BS, Kim H, Hong SH, Chang SY. Separation surgery followed by stereotactic ablative radiotherapy for metastatic epidural spinal cord compression: a systematic review and meta-analysis for local progression rate. J Bone Oncol. 2022;36:100450. doi: 10.1016/j.jbo.2022.100450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Huang TJ, Hsu RW, Li YY, Cheng CC. Minimal access spinal surgery (MASS) in treating thoracic spine metastasis. Spine (Phila Pa 1976) 2006;31:1860–3. doi: 10.1097/01.brs.0000225995.56028.46. [DOI] [PubMed] [Google Scholar]
- 72.Kan P, Schmidt MH. Minimally invasive thoracoscopic approach for anterior decompression and stabilization of metastatic spine disease. Neurosurg Focus. 2008;25:E8. doi: 10.3171/FOC/2008/25/8/E8. [DOI] [PubMed] [Google Scholar]
- 73.Saigal R, Wadhwa R, Mummaneni PV, Chou D. Minimally invasive extracavitary transpedicular corpectomy for the management of spinal tumors. Neurosurg Clin N Am. 2014;25:305–15. doi: 10.1016/j.nec.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 74.Donnelly DJ, Abd-El-Barr MM, Lu Y. Minimally invasive muscle sparing posterior-only approach for lumbar circumferential decompression and stabilization to treat spine metastasis: technical report. World Neurosurg. 2015;84:1484–90. doi: 10.1016/j.wneu.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 75.Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 2013;108:499–503. doi: 10.1002/jso.23418. [DOI] [PubMed] [Google Scholar]
- 76.Lu VM, Alvi MA, Goyal A, Kerezoudis P, Bydon M. The potential of minimally invasive surgery to treat metastatic spinal disease versus open surgery: a systematic review and meta-analysis. World Neurosurg. 2018;112:e859–68. doi: 10.1016/j.wneu.2018.01.176. [DOI] [PubMed] [Google Scholar]
- 77.Yang Z, Yang Y, Zhang Y, et al. Minimal access versus open spinal surgery in treating painful spine metastasis: a systematic review. World J Surg Oncol. 2015;13:68. doi: 10.1186/s12957-015-0468-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Spiessberger A, Arvind V, Gruter B, Cho SK. Thoracolumbar corpectomy/spondylectomy for spinal metastasis: a pooled analysis comparing the outcome of seven different surgical approaches. Eur Spine J. 2020;29:248–56. doi: 10.1007/s00586-019-06179-8. [DOI] [PubMed] [Google Scholar]
- 79.Cui Y, Shi X, Mi C, Wang B, Pan Y, Lin Y. Comparison of minimally invasive tubular surgery with conventional surgery in the treatment of thoracolumbar metastasis. Cancer Manag Res. 2021;13:8399–409. doi: 10.2147/CMAR.S332985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hinojosa-Gonzalez DE, Roblesgil-Medrano A, Villarreal-Espinosa JB, et al. Minimally invasive versus open surgery for spinal metastasis: a systematic review and meta-analysis. Asian Spine J. 2022;16:583–97. doi: 10.31616/asj.2020.0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Flynn SC, Eli IM, Ghogawala Z, Yew AY. Minimally invasive surgery for spinal metastasis: a review. World Neurosurg. 2022;159:e32–9. doi: 10.1016/j.wneu.2021.11.097. [DOI] [PubMed] [Google Scholar]
- 82.Kato S, Demura S, Shinmura K, et al. Surgical metastasectomy in the spine: a review article. Oncologist. 2021;26:e1833–43. doi: 10.1002/onco.13840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barzilai O, Boriani S, Fisher CG, et al. Essential concepts for the management of metastatic spine disease: what the surgeon should know and practice. Global Spine J. 2019;9(1 Suppl):98S–107S. doi: 10.1177/2192568219830323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kato S, Demura S, Shinmura K, et al. Clinical outcomes and survivals after total en bloc spondylectomy for metastatic leiomyosarcoma in the spine. Eur Spine J. 2020;29:3237–44. doi: 10.1007/s00586-020-06461-0. [DOI] [PubMed] [Google Scholar]
- 85.Yonezawa N, Murakami H, Demura S, et al. Perioperative complications and prognosis of curative surgical resection for spinal metastases in elderly patients. World Neurosurg. 2020;137:e144–51. doi: 10.1016/j.wneu.2020.01.093. [DOI] [PubMed] [Google Scholar]
- 86.Higuchi T, Yamamoto N, Hayashi K, et al. Long-term patient survival after the surgical treatment of bone and soft-tissue metastases from renal cell carcinoma. Bone Joint J. 2018;100-B:1241–8. doi: 10.1302/0301-620X.100B9.BJJ-2017-1163.R3. [DOI] [PubMed] [Google Scholar]
- 87.Kato S, Demura S, Murakami H, et al. Medium to long-term clinical outcomes of spinal metastasectomy. Cancers (Basel) 2022;14:2852. doi: 10.3390/cancers14122852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ohashi M, Hirano T, Watanabe K, et al. En Bloc Spondylectomy for spinal metastases: detailed oncological outcomes at a minimum of 2 years after surgery. Asian Spine J. 2019;13:296–304. doi: 10.31616/asj.2018.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Igoumenou VG, Mavrogenis AF, Angelini A, et al. Complications of spine surgery for metastasis. Eur J Orthop Surg Traumatol. 2020;30:37–56. doi: 10.1007/s00590-019-02541-0. [DOI] [PubMed] [Google Scholar]
- 90.Paulino Pereira NR, Ogink PT, Groot OQ, et al. Complications and reoperations after surgery for 647 patients with spine metastatic disease. Spine J. 2019;19:144–56. doi: 10.1016/j.spinee.2018.05.037. [DOI] [PubMed] [Google Scholar]
- 91.Quraishi NA, Rajabian A, Spencer A, et al. Reoperation rates in the surgical treatment of spinal metastases. Spine J. 2015;15(3 Suppl):S37–43. doi: 10.1016/j.spinee.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 92.Tarawneh AM, Pasku D, Quraishi NA. Surgical complications and re-operation rates in spinal metastases surgery: a systematic review. Eur Spine J. 2021;30:2791–9. doi: 10.1007/s00586-020-06647-6. [DOI] [PubMed] [Google Scholar]
- 93.Galgano M, Fridley J, Oyelese A, et al. Surgical management of spinal metastases. Expert Rev Anticancer Ther. 2018;18:463–72. doi: 10.1080/14737140.2018.1453359. [DOI] [PubMed] [Google Scholar]
- 94.Isogai N, Yagi M, Nishimura S, et al. Risk predictors of perioperative complications for the palliative surgical treatment of spinal metastasis. J Orthop Sci. 2021;26:1107–12. doi: 10.1016/j.jos.2020.09.005. [DOI] [PubMed] [Google Scholar]
- 95.Sebaaly A, Shedid D, Boubez G, et al. Surgical site infection in spinal metastasis: incidence and risk factors. Spine J. 2018;18:1382–7. doi: 10.1016/j.spinee.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 96.Hersh AM, Feghali J, Hung B, et al. A web-based calculator for predicting the occurrence of wound complications, wound infection, and unplanned reoperation for wound complications in patients undergoing surgery for spinal metastases. World Neurosurg. 2021;155:e218–28. doi: 10.1016/j.wneu.2021.08.041. [DOI] [PubMed] [Google Scholar]
- 97.Park SJ, Lee CS, Chang BS, et al. Rod fracture and related factors after total en bloc spondylectomy. Spine J. 2019;19:1613–9. doi: 10.1016/j.spinee.2019.04.018. [DOI] [PubMed] [Google Scholar]
- 98.Amankulor NM, Xu R, Iorgulescu JB, et al. The incidence and patterns of hardware failure after separation surgery in patients with spinal metastatic tumors. Spine J. 2014;14:1850–9. doi: 10.1016/j.spinee.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 99.Kumar N, Patel R, Tan JH, et al. Symptomatic construct failure after metastatic spine tumor surgery. Asian Spine J. 2021;15:481–90. doi: 10.31616/asj.2020.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wong YC, Chau WW, Kwok KO, Law SW. Incidence and risk factors for implant failure in spinal metastasis surgery. Asian Spine J. 2020;14:878–85. doi: 10.31616/asj.2020.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zaborovskii N, Schlauch A, Ptashnikov D, et al. Hardware failure in spinal tumor surgery: a hallmark of longer survival? Neurospine. 2022;19:84–95. doi: 10.14245/ns.2143180.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Suvithayasiri S, Santipas B, Wilartratsami S, Ruangchainikom M, Luksanapruksa P. Non-fusion palliative spine surgery without reconstruction is safe and effective in spinal metastasis patients: retrospective study. Sci Rep. 2021;11:17486. doi: 10.1038/s41598-021-97056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yee TJ, Saadeh YS, Strong MJ, et al. Survival, fusion, and hardware failure after surgery for spinal metastatic disease. J Neurosurg Spine. 2021;34:665–72. doi: 10.3171/2020.8.SPINE201166. [DOI] [PubMed] [Google Scholar]
- 104.Kumar N, Patel R, Tan BW, et al. Asymptomatic construct failure after metastatic spine tumor surgery: a new entity or a continuum with symptomatic failure? Asian Spine J. 2021;15:636–49. doi: 10.31616/asj.2020.0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Swann MC, Hoes KS, Aoun SG, McDonagh DL. Postoperative complications of spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30:103–20. doi: 10.1016/j.bpa.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 106.Gao ZY, Zhang T, Zhang H, Pang CG, Xia Q. Effectiveness of preoperative embolization in patients with spinal metastases: a systematic review and meta-analysis. World Neurosurg. 2021;152:e745–57. doi: 10.1016/j.wneu.2021.06.062. [DOI] [PubMed] [Google Scholar]
- 107.Yoo SL, Kim YH, Park HY, et al. Clinical significance of preoperative embolization for non-hypervascular metastatic spine tumors. J Korean Neurosurg Soc. 2019;62:106–13. doi: 10.3340/jkns.2018.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hong CG, Cho JH, Suh DC, Hwang CJ, Lee DH, Lee CS. Preoperative embolization in patients with metastatic spinal cord compression: mandatory or optional? World J Surg Oncol. 2017;15:45. doi: 10.1186/s12957-017-1118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


