Abstract
In Japan, comprehensive genomic profiling (CGP) tests for refractory cancer patients have been approved since June 2019, under the requirement that all cases undergoing CGP tests are annotated by the molecular tumor board (MTB) at each government‐designated hospital. To investigate improvement in precision oncology, we evaluated and compared the proportion of cases receiving matched treatments according to CGP results and those recommended to receive genetic counseling at all core hospitals between the first period (11 hospitals, June 2019 to January 2020) and second period (12 hospitals, February 2020 to January 2021). A total of 754 and 2294 cases underwent CGP tests at core hospitals in the first and second periods, respectively; 28 (3.7%) and 176 (7.7%) patients received matched treatments (p < 0.001). Additionally, 25 (3.3%) and 237 (10.3%) cases were recommended to receive genetic counseling in the first and second periods, respectively (p < 0.001). The proportion was associated with the type of CGP test: tumor‐only (N = 2391) vs. tumor‐normal paired (N = 657) analysis (10.0% vs. 3.5%). These results suggest that recommendations regarding available clinical trials in networked MTBs might contribute to increasing the numbers of matched treatments, and that tumor‐normal paired rather than tumor‐only tests can increase the efficiency of patient referrals for genetic counseling.
Keywords: comprehension genomic profiling test, genetic counseling, genomically matched therapy, molecular tumor board, precision oncology
We investigated the improvement in precision oncology by evaluating and comparing the proportion of patients receiving genomically‐matched therapies and referred to genetic counseling among all designated core hospitals between two study periods (First period: 11 hospitals, June 2019 to January 2020; Second period: 12 hospitals, February 2020 to January 2021). Our results revealed that both the proportion of matched therapies and referrals to genetic counseling improved chronologically, from 3.7% to 7.7% (p 0.001) and 3.3% to 10.3% (p 0.001), respectively.
Abbreviations
- CGP
comprehensive genomic profiling
- IND
investigational new drug
- MHLW
Ministry of Health, Labour and Welfare
- MTB
molecular tumor board
- NCCH
National Cancer Center Hospital
- PGV
pathogenic germline variants
1. INTRODUCTION
Comprehensive genomic profiling (CGP) tests have been covered by the Japanese Public Health Insurance System since June 2019 (https://www.mhlw.go.jp/content/12400000/000514782.pdf). To assure the quality of precision oncology based on the result of CGP tests, the Ministry of Health, Labour and Welfare (MHLW) restricted reimbursement for CGP tests to those performed at designated hospitals (https://www.mhlw.go.jp/content/12400000/000514782.pdf), 1 which numbered 226 as of September 2019 (Core: 12, Hub: 33, Cooperative: 181; https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/gan/gan_byoin.html).
The current challenge in precision oncology is the accessibility to genomically matched therapies. We previously reported that 3.7% of tested cases received genomically matched treatment in the first 8 months after reimbursement for CGP tests at 11 Cores. 2 To provide patients with opportunities to receive genomically matched therapies, the National Cancer Center Hospital (NCCH) launched a prospective, patient‐proposed platform trial of targeted agents (NCCH1901; jRCTs031190104) in October 2019. As of June 2021, 15 molecular‐targeted agents, including two immune checkpoint inhibitors, were available in this trial (https://jrct.niph.go.jp/latest‐detail/jRCTs031190104). In addition, since June 2019, the molecular tumor boards (MTBs) across all Cores and Hubs have been systematically networked to enhance sharing of information of available clinical trials for investigational new drugs (INDs) and to increase the proportion of patients who receive genomically matched treatments.
Genetic counseling plays an important role in dealing with germline findings detected by the CGP tests. In our previous report, 3.3% of tested cases were referred for genetic counseling among the 11 Cores. 2
Here, we investigated the proportion of patients receiving genomically matched therapies and referral for genetic counseling. Moreover, we explored factors affecting the accessibility of genomically matched drugs by focusing on the drug therapy type, such as INDs, NCCH1901, off‐label use, and approved drugs, and the factors associated with differences in the proportion of patients referred for genetic counseling.
2. METHODS
2.1. Data collection
We collected data on cases that underwent CGP tests at all Cores between June 2019 and January 2020 (first period) and between February 2020 and January 2021 (second period). As one hospital was newly designated as Core in April 2020, the data were collected from 11 Cores in the first period and 12 Cores in the second period. We evaluated the number of cases that received genomically matched treatments and the number of patients who were recommended to be referred for genetic counseling in both periods. To investigate the factors affecting drug accessibility and frequency of genetic counseling references, information on the types of CGP tests (i.e., tumor‐only test or tumor‐normal paired test) and drug types in matched therapies were also collected. The NCC Institutional Review Board (IRB) officially confirmed that the present study did not require IRB approval or patient consent.
2.2. Evaluation of improvement
To assess improvements in drug accessibility and frequency of genetic counseling references, the proportions of patients receiving matched treatments and referrals to genetic counseling between the first and second periods were compared using Fisher's exact test. The degree of association between the proportion of patients receiving matched therapies and the number enrolled in clinical trials was assessed using Spearman's rank correlation.
All statistical analyses were performed with R version 3.5.1 (R Foundation for Statistical Computing).
3. RESULTS
3.1. Increase in patients receiving genomically matched therapies
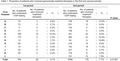
A total of 754 (range; 5‐172) and 2294 (range; 83‐450) cases underwent CGP tests at Cores in the first and second periods, respectively. The proportion of patients receiving genomically matched therapies increased at 10 hospitals (except hospital E). Among all Cores, a total of 28 and 176 cases received matched treatments in the first and second periods, respectively (p < 0.001, 3.7% vs. 7.7%) (Table 1 ).
TABLE 1.
Proportion of patients who received genomically matched therapies in the first and second periods
| Core hospital | 1st period | 2nd period | P value | ||
|---|---|---|---|---|---|
| No. of patients who underwent CGP testing | No. of patients who received “matched” therapies (%) | No. of patients who underwent CGP testing (%) | No. of patients who received “matched” therapies | ||
| A | 75 | 3 (4.0%) | 138 | 18 (13.0%) | |
| B | 73 | 2 (2.7%) | 201 | 12 (6.0%) | |
| C | 5 | 0 (0.0%) | 102 | 3 (2.9%) | |
| D | 41 | 0 (0.0%) | 158 | 6 (3.8%) | |
| E | 160 | 16 (10.0%) | 251 | 23 (9.2%) | |
| F | 172 | 4 (2.3%) | 450 | 47 (10.4%) | |
| G | 13 | 1 (7.7%) | 83 | 9 (10.8%) | |
| H | 85 | 0 (0.0%) | 218 | 15 (6.9%) | |
| I | 13 | 0 (0.0%) | 142 | 16 (11.3%) | |
| J | 24 | 0 (0.0%) | 221 | 6 (2.7%) | |
| K | 93 | 2 (2.2%) | 179 | 9 (5.0%) | |
| L | ‐ | ‐ | 151 | 12 (7.9%) | |
| Total | 754 | 28 (3.7%) | 2294 | 176 (7.7%) | <0.001 |
Abbreviation: CGP, comprehensive genomic profiling.
In the second period, 107 of the 176 cases who received matched treatments (4.7% of the 2295 cases) participated in clinical trials including INDs (n = 60) and NCCH1901 (n = 47), and 17 cases (0.7% of the 2295 cases) received genomically matched drugs as off‐label use. The remaining 52 cases (2.3% of the 2295 cases) received approved drugs (Table 2 ). In terms of INDs, the most common treatments were FGFR inhibitors for FGFR/FGF alterations (n = 13), followed by PARP inhibitors for BRCA1/2 alterations (n = 7) and immune checkpoint inhibitors for high tumor mutation burden (TMB‐high) (n = 7). Regarding approved drugs, pembrolizumab for microsatellite instability‐high (MSI‐high) tumors was the most common (n = 12) (Table S1 ). Compared with the first period, cases enrolled in clinical trials (2.1% vs. 4.7%, p = 0.002) and receiving approved drugs (1.1% vs. 2.3%, p = 0.048) were significantly higher in the second period (Table 2 ).
TABLE 2.
Proportion of patients who received genomically matched therapies by drug and therapy type
| Core hospital | 1st Period | 2nd Period | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | Clinical trials | Off‐label use | Approved drugs | All | Clinical trials | Off‐label use | Approved drugs | |||
| Investigational drugs | NCCH1901 | Investigational drugs | NCCH1901 | |||||||
| A | 75 | 3 (4.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 138 | 1 (0.7%) | 7 (5.1%) | 2 (1.4%) | 8 (5.8%) |
| B | 73 | 2 (2.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 201 | 1 (0.5%) | 3 (1.5%) | 0 (0.0%) | 8 (4.0%) |
| C | 5 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 102 | 1 (1.0%) | 1 (1.0%) | 1 (1.0%) | 0 (0.0%) |
| D | 41 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 158 | 1 (0.6%) | 0 (0.0%) | 0 (0.0%) | 5 (3.2%) |
| E | 160 | 7 (4.4%) | 0 (0.0%) | 2 (1.3%) | 7 (4.4%) | 251 | 9 (3.6%) | 9 (3.6%) | 1 (0.4%) | 4 (1.6%) |
| F | 172 | 2 (1.2%) | 0 (0.0%) | 1 (0.6%) | 1 (0.6%) | 450 | 28 (6.2%) | 4 (0.9%) | 7 (1.6%) | 8 (1.8%) |
| G | 13 | 1 (7.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 83 | 0 (0.0%) | 7 (8.4%) | 0 (0.0%) | 2 (2.4%) |
| H | 85 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 218 | 2 (0.9%) | 7 (3.2%) | 1 (0.5%) | 5 (2.3%) |
| I | 13 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 142 | 6 (4.2%) | 4 (2.8%) | 4 (2.8%) | 2 (1.4%) |
| J | 24 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 221 | 1 (0.5%) | 1 (0.5%) | 1 (0.5%) | 3 (1.4%) |
| K | 93 | 1 (1.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 179 | 0 (0.0%) | 4 (2.2%) | 0 (0.0%) | 5 (2.8%) |
| L | ‐ | ‐ (‐) | ‐ (0.0%) | ‐ (‐) | ‐ (‐) | 151 | 10 (6.6%) | 0 (0.0%) | 0 (0.0%) | 2 (1.3%) |
| Total | 754 | 16 (2.1%) | 0 (0.0%) | 3 (0.4%) | 8 (1.1%) | 2294 | 60 (2.6%) | 47 (2.0%) | 17 (0.7%) | 52 (2.3%) |
For the entire period, the proportion of patients receiving matched therapies was 6.7%, and there was variability in the proportion of therapy types among the 12 Cores (range; 2.4‐10.4%) (Figure S1 ). The proportion of patients receiving matched therapies at each hospital correlated positively with the number of cases enrolled in clinical trials (Spearman's rank correlation coefficient, R = 0.73) (Figure S2).
3.2. Increase in referrals for genetic counseling
While 25 cases (3.3%, range 0%‐15.4%) were referred for genetic counseling in the first period, 237 cases (10.3%, range 2.9%‐20.3%) were recommended to receive genetic counseling in the second period, indicating a significantly higher proportion in the second study period (p < 0.001) (Table 3).
TABLE 3.
Proportion of patients referred for genetic counseling in the first and second periods
| Core hospital | 1st period | 2nd period | P value | ||
|---|---|---|---|---|---|
| No. of patients who underwent CGP testing | No. of patients referred for genetic counseling (%) | No. of patients who underwent CGP testing | No. of patients referred for genetic counseling (%) | ||
| A | 75 | 3 (4.0%) | 138 | 28 (20.3%) | |
| B | 73 | 0 (0.0%) | 201 | 21 (10.4%) | |
| C | 5 | 0 (0.0%) | 102 | 3 (2.9%) | |
| D | 41 | 1 (2.4%) | 158 | 15 (9.5%) | |
| E | 160 | 5 (3.1%) | 251 | 22 (8.8%) | |
| F | 172 | 2 (1.2%) | 450 | 25 (5.6%) | |
| G | 13 | 2 (15.4%) | 83 | 7 (8.4%) | |
| H | 85 | 0 (0.0%) | 218 | 37 (17.0%) | |
| I | 13 | 0 (0.0%) | 142 | 25 (17.6%) | |
| J | 24 | 2 (8.3%) | 221 | 18 (8.1%) | |
| K | 93 | 10 (10.8%) | 179 | 13 (7.3%) | |
| L | ‐ | ‐ | 151 | 23 (15.2%) | |
| Total | 754 | 25 (3.3%) | 2294 | 237 (10.3%) | <0.001 |
Abbreviation: CGP, comprehensive genomic profiling.
For the entire period, 2391 cases and 657 cases were assessed by tumor‐only analysis and tumor‐normal paired analysis, respectively. While the proportion of cases recommended to receive genetic counseling was higher among those who underwent tumor‐only analysis versus tumor‐normal paired analysis (10.0 vs. 3.5%), the actual consultation rate for recommended cases was higher in cases of paired analysis (82.6 vs. 51.5%) (Table 4). Among cases recommended for genetic counseling by tumor‐only analysis, 25.5% of cases received genetic tests to confirm pathogenic germline variants (PGVs), and 14.6% of cases had PGVs. On the other hand, no additional genetic tests were performed in any except two of the patients who underwent tumor‐normal paired analysis.
TABLE 4.
Proportion of patients referred for genetic counseling by test type
| No. of patients who underwent CGP test | No. of patients recommended for genetic counseling | No. of patients who received genetic counseling | ||||
|---|---|---|---|---|---|---|
| T‐only analysis | T/N paired analysis | T‐only analysis (%) | T/N paired analysis (%) | T‐only analysis (%) | T/N paired analysis (%) | |
| A | 195 | 18 | 28 (14.4%) | 3 (16.7%) | 13 (46.4%) | 3 (100%) |
| B | 264 | 10 | 21 (8.0%) | 0 (0.0%) | 21 (100%) | 0 (‐) |
| C | 59 | 48 | 1 (1.7%) | 2 (4.2%) | 1 (100%) | 1 (50.0%) |
| D | 141 | 58 | 13 (9.2%) | 3 (5.2%) | 13 (100%) | 3 (100%) |
| E | 383 | 28 | 27 (7.0%) | 0 (0.0%) | 14 (51.9%) | 0 (‐) |
| F | 255 | 367 | 17 (6.7%) | 10 (2.7%) | 5 (29.4%) | 7 (70.0%) |
| G | 48 | 48 | 6 (12.5%) | 3 (6.3%) | 6 (100%) | 3 (100%) |
| H | 293 | 10 | 37 (12.6%) | 0 (0.0%) | 9 (24.3%) | 0 (‐) |
| I | 138 | 17 | 25 (18.1%) | 0 (0.0%) | 7 (28.0%) | 0 (‐) |
| J | 226 | 19 | 20 (8.8%) | 0 (0.0%) | 10 (50.0%) | 0 (‐) |
| K | 246 | 26 | 21 (8.5%) | 2 (7.7%) | 12 (57.1%) | 2 (100%) |
| L | 143 | 8 | 23 (16.1%) | 0 (0.0%) | 12 (52.2%) | 0 (‐) |
| Total | 2391 | 657 | 239 (10.0%) | 23 (3.5%) | 123 (51.5%) | 19 (82.6%) |
Note: T‐only analysis: only tumor samples evaluated; T/N paired analysis: paired tumor/normal samples evaluated.
Abbreviation: CGP, comprehensive genomic profiling.
4. DISCUSSION
Our results indicate a chronological improvement in the proportion of matched treatments and genetic counseling for cancers over the study period. A total of 754 and 2294 cases underwent CGP testing at core hospitals in the first and second periods, respectively, of whom 28 (3.7%) and 176 (7.7%) received matched treatments (p < 0.001). The proportion of patients referred for genetic counseling also increased from 3.3% to 10.3% (p < 0.001) during this period.
Evaluation of the improvement of drug accessibility by treatment type showed that cases enrolled in clinical trials (2.1% vs. 4.7%, p = 0.002) and those who received approved drugs (1.1% vs. 2.3%, p = 0.048) increased significantly over time. Moreover, we showed a positive correlation between the number of cases enrolled in clinical trials and the proportion receiving matched treatments at each hospital (R = 0.73). These results suggest that improvement of enrollment in clinical trials might contribute to an increase in the number of matched treatments.
In the framework of Japanese precision oncology, CGP test results of each patient are required to be discussed in an MTB. 1 As the MTB makes recommendations for genomically matched treatments, including new investigational drugs, sharing the information of available clinical trials across all MTBs is important to improve accessibility to matched drugs.
The MTB also evaluates whether referral for genetic counseling is warranted based on the CGP test result. While tumor‐only analyses only identify presumed germline pathogenic variants, tumor‐normal paired analysis can confirm PGVs. Therefore, paired analysis can lead to more efficient referral of patients for genetic counseling in the MTB as compared with tumor‐only analysis.
In conclusion, we achieved chronological improvement in the proportion of matched therapies and referrals for genetic counseling. For further improvement of precision oncology in Japan, it might be necessary to establish a systematically networked framework to share the latest information on clinical trials across all MTBs.
FUNDING INFORMATION
This work was supported by a Health Labour Sciences Special Research Grant (19EA1007) from the MHLW, Japan.
DISCLOSURE
Kuniko Sunami received research funds from Sysmex. Yoichi Naito received lecture fees from Chugai, Pfizer, Eli Lilly, and Novartis, and research funds from Daiichi‐Sankyo, Taiho, Pfizer, and Boehringer Ingelheim. Daisuke Ennishi received lecture fees from Kyowa Kirin and Eisai, and research funds from Chugai and Nihon Shinyaku. Hidenori Kage received research funds from Konica Minolta. Masashi Kanai receives annual profit from Therabiopharma Inc. and received manuscript fees from Chugai. Hirotsugu Kenmotsu received research funds from AstraZeneca, Novartis, Loxo Oncology, Daiichi‐Sankyo, and Chugai. Takafumi Koyama received research lecture fees from Sysmex and research funds from PACT Pharma. Takayuki Yoshino received lecture fees from Taiho, Chugai, Eli Lilly, Takeda, Merck Biopharma, Bayer Yakuhin, and Ono, and research funds from MSD, Ono, Sanofi, Daiichi‐Sankyo, Parexel International, Amgen, Taiho, and Sumitomo Dainippon Pharma. None of the other authors have any conflicts of interest. Katsuya Tsuchihara is the associate editor of the journal.
Supporting information
Table S1
Figure S1
Figure S2
ACKNOWLEDGMENTS
The authors thank all MTB members at the 12 Cores, and Hideki Ueno and Yuichiro Ohe for supporting this study. This study was supported by grants from the MHLW Japan.
Sunami K, Naito Y, Komine K, et al. Chronological improvement in precision oncology implementation in Japan. Cancer Sci. 2022;113:3995‐4000. doi: 10.1111/cas.15517
Kuniko Sunami and Yoichi Naito contributed equally to this work.
REFERENCES
- 1. Ebi H, Bando H. Precision oncology and the universal health coverage system in Japan. JCO Precis Oncol. 2019;3:PO.19.00291. doi: 10.1200/po.19.00291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sunami K, Naito Y, Aimono E, et al. The initial assessment of expert panel performance in core hospitals for cancer genomic medicine in Japan. Int J Clin Oncol. 2021;26(3):443‐449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Figure S1
Figure S2


