Abstract
Purpose:
To investigate the time to detect progression in glaucomatous eyes using different optical coherence tomography (OCT) test intervals.
Methods:
Participants with manifest glaucoma from the African Descent and Glaucoma Evaluation Study (ADAGES), a multicenter, prospective, observational cohort study, were included. A total of 2,699 OCT tests from 171 glaucomatous and 149 normal eyes of 182 participants, with at least 5 tests and 2 years of follow-up, were analyzed. Computer simulations (n = 10,000 eyes) were performed to estimate time to detect progression of global circumpapillary retinal nerve fiber layer thickness (cpRNFL) measured with OCT tests. Simulations were based on different testing paradigms (every 4, 6, 12 and 24 months) and different rates of change (µm/year). Time to detect significant progression (P < 0.05) at 80% and 90% power were calculated for each paradigm and rate of cpRNFL change.
Results:
As expected, more frequent testing resulted in shorter time to detect progression. While there was clear disadvantage for testing at intervals of 24 vs 12 months (~22.4% time [25 months] increase in time to progression detection) and when testing 12 vs 6 months (~22.1% time [20 months] increase), the improved time to detect progression was less pronounced when comparing 6 vs 4 months (~11.5% time [10 months] reduction).
Conclusion:
With high specificity and less variability than perimetry, a 6-month testing interval provides a reasonable trade-off for following glaucoma patients using OCT.
Keywords: optical coherence tomography, glaucoma, progression
Synopsis/Precis:
With high specificity and less variability than perimetry, more frequent testing resulted in shorter time to detect progression, though a 6-month testing interval provides a reasonable trade-off for following glaucoma patients using optical coherence tomography.
INTRODUCTION
Glaucoma is an acquired optic neuropathy characterized by the death of retinal ganglion cells (RGC) and their axons and associated anatomical changes to the optic nerve head (ONH) and retinal nerve fiber layer (RNFL),1–3 that results in irreversible vision loss. Once glaucoma is diagnosed, treatment decisions depend upon the rate of progression and aim to halt or slow further irreversible vision loss. Progression monitoring is often based upon clinical findings and ancillary testing, including functional (visual fields, VF) and structural (optical coherence tomography, OCT) tests.
Enabling non-invasive, high-resolution cross-sectional imaging of the retina in vivo, OCT has revolutionized the management and diagnosis of glaucoma, allowing objective evaluation of neural structures affected by the disease.4–6 However, the optimal intervals at which the test should be administered to most effectively detect disease progression remains unknown. There are broad recommendations from the American Academy of Ophthalmology (AAO) and European Glaucoma Society (EGS) on how frequently patients should be followed with clinical and ancillary examination: in general, patients who have shown long-term stability can be followed every 6 to 12 months, depending on disease severity, whereas patients with evidence of progression may require more frequent follow-up.7,8 However, to date there is scant data in the literature to support these positions and no consensus on the recommended frequency of OCT testing. This information is important and timely, especially during the SARS-CoV-2 (COVID-19) era, when the use of automated perimetry can be limited because of the risk of viral exposure.9,10
The purpose of this study is to investigate the statistical power and minimum time to detect statistically significant progression with OCT in eyes with established glaucoma at different levels of disease severity and rates of retinal nerve fiver layer (RNFL) change.
MATERIALS AND METHODS
Participants
The multicenter African Descent and Glaucoma Evaluation Study (ADAGES) collaboration (clinicaltrials.gov Identifier: NCT00221923) includes the Hamilton Glaucoma Center at the Department of Ophthalmology, University of California-San Diego (UCSD) (data coordinating center), Edward S. Harkness Eye Institute at Columbia University Irving Medical Center and the Department of Ophthalmology at University of Alabama-Birmingham (UAB). The institutional review boards at all sites approved the study methodology, which adheres to the tenets of the Declaration of Helsinki and to the Health Insurance Portability and Accountability Act. All participants gave written informed consent. ADAGES enrollment began in January 2003 and ended in July 2006, and follow-up continued into 2017 for this study.
ADAGES is an observational, prospective cohort study that aimed to identify factors accounting for differences in glaucoma onset and rate of progression between individuals of African (AD) and European (ED) descent with or suspected glaucoma. Treatment was applied at each physician’s discretion.
The ocular testing performed in ADAGES has been described elsewhere.11 In brief, participants underwent a comprehensive ophthalmic examination, including annual review of medical history, best-corrected visual acuity, slit-lamp biomicroscopy, intraocular pressure measurement (Goldmann tonometry), dilated funduscopic examination, pachymetry, simultaneous stereoscopic optic disc photography, and semiannual standard automated perimetry (SAP) Humphrey 24–2 field test using the Swedish interactive threshold algorithm (SITA) (Carl Zeiss Meditec, Inc., Dublin, CA, USA). The structure of the optic disc and RNFL was semiannually measured with a variety of OCT scans, including spectral-domain OCT Optic Disc Cube Scans (Cirrus HD-OCT software; Carl Zeiss Meditec, Inc., Dublin, CA, USA).
Inclusion criteria
All participants had open angles, a best-corrected visual acuity ≥ 20/40, and a refractive error < 5.0 diopters sphere and < 3.0 diopters cylinder at study entry. At least one high-quality stereophotograph and one reliable SAP Humphrey 24–2 field test result at baseline were required. Both eyes were included, except in cases where only one eye met the study criteria. All participants were older than 18 years. Diabetic participants without evidence of retinopathy were included.
Exclusion criteria
Participants were excluded if they had a history of intraocular surgery (except for uncomplicated cataract surgery or uncomplicated glaucoma surgery), secondary causes of glaucoma (e.g., iridocyclitis, trauma), other systemic or ocular diseases known to affect the VF (e.g., pituitary lesions, demyelinating diseases, etc.), significant cognitive impairment, history of stroke, Alzheimer disease, or dementia, problems other than glaucoma affecting color vision, an inability to perform VF examinations reliably, or a life-threatening disease that precluded retention in the study.
In this study, patients with less than 5 visits and less than 2 years of follow-up were excluded. Only Cirrus Optic Disc Cube OCT scans with signal strength ≥ 6 and deemed of good quality by the Imaging Data Evaluation and Analysis (IDEA) Reading Center were included in this study.
Glaucoma Definition
Glaucomatous optic neuropathy was defined as excavation, neuroretinal rim thinning or notching, localized or diffuse retinal nerve fiber layer defect, or vertical cup-disc ratio asymmetry > 0.2 between eyes (not explained by differences in disc size) based on masked grading of stereophotographs by two graders using standardized protocols from the IDEA Reading Center. Only photographs of adequate quality were used for evaluation. Disagreements were resolved by consensus or adjudication by a third experienced grader. An abnormal 24–2 VF was defined if the pattern standard deviation was P < 0.05 or the Glaucoma Hemifield Test result was “outside normal limits.” An abnormality had to be confirmed with an additional VF test.11
Simulations and statistical analyses
The methods employed for the simulation and definition of progression have been described elsewhere.12–16 In brief, instead of VF data, rates of OCT progression for each eye were calculated after performing linear regression of global circumpapillary (cp) RNFL thickness (microns) over time (years) using ordinary least squares estimation. The residuals of the regression, defined as the difference between the best fitted value and the observed measurement of the cpRNFL average thickness were obtained for each data point of each eye. The standard deviation (SD) of these residuals were calculated for each 10 µm bin of the best cpRNFL thickness value (< 65 µm, 65 – 75 µm, 75 – 85 µm and > 85 µm). Because a previous study showed that residuals derived from VF testing (and, therefore, test variability) were different between individuals of African (AD) and European (ED) descent,17 we also compared the variability of OCT RNFL thickness measurements between racial groups.
Computer simulations were used to estimate the time to detect progression with OCT with different testing paradigms (every 4, 6, 12 and 24 months). Using different rates of average cpRNFL thickness change, we simulated different slopes for non-progressors (0 µm/year), approximated age-related loss (−0.5 µm/year),15,16 “significant” glaucoma progressors (−1 µm/year)16 and “rapid” glaucoma progressors (greater than the 95th percentile of slopes of glaucomatous eyes, (−2.5 µm/year). This was achieved by generating 10,000 sequences of OCT tests (or 10,000 simulated eyes for each scenario) where the “true” cpRNFL average thickness values were determined in 3 steps. First, the baseline values were stablished for each severity group:18 early (90.5 µm), moderate (79.5 µm) and severe (65.9 µm) glaucoma. Second, the variability values were generated by the normal distribution of the residuals of our sample, divided for every 10 µm bin of best-fitted cpRNFL global thickness values (< 65 µm, 65 – 75 µm, 75 – 85 µm and > 85 µm). Third, different rates of change over time (0, −0.5, −1.0 and −2.5 µm/year) were simulated. The OCT testing paradigms required 2 tests at baseline followed by single tests performed at 4, 6, 12 or 24- month intervals. Progression was defined when a statistically significant (P < 0.05) negative cpRNFL average thickness slope was detected on 2 consecutive visits. The time to detect significant progression at 80% and 90% power was calculated for each baseline severity, rate of change, and testing paradigm. The simulations were done for the sufficient time to get 100% of progression detection. This time varies (from 5 to 20 years) according to cpRNFL average thickness slope, test intervals and glaucoma severity.
All statistical analyses and computer simulations were performed using Stata Version 16 (StataCorp LP, College Station, TX, USA).
RESULTS
A total of 2,699 OCT tests from 171 glaucomatous and 149 normal eyes of 182 participants were included. Mean ± SD age of the participants at baseline was 67.3 ± 10.4 years and the follow-up time was 4.1 ± 1.1 years (range: 2.0 – 7.8 years) over 8.3 ± 3.3 visits (range: 5 – 19 visits). The median and interquartile range (IQR) of average baseline cpRNFL thickness were 76 µm (IQR: 66 to 84.5 µm). The demographic and baseline characteristics are summarized in Table 1.
Table 1.
Patients and eyes characteristics
| African Descent | European Descent | Total | P Value | |
|---|---|---|---|---|
| Patients | 55 (30.2%) | 112 (61.5%) | 182 (100%) | - |
| Age (years) | 63.9 (61.3 to 66.5)* | 69.5 (67.6 to 71.3)* | 67.3 (65.8 to 68.8)* | < 0.01 |
| Gender | 0.87 | |||
| Male | 26 (14.3%) | 51 (28.0%) | 86 (47.2%) | - |
| Female | 29 (15.9%) | 61 (33.5%) | 96 (52.7%) | - |
| Eyes | 99 (30.9%) | 194 (60.6%) | 320 (100%) | - |
| Eyes with Glaucoma | 66 (20.6%) | 87 (27.2%) | 171 (53.4%) | - |
| Eyes without Glaucoma | 33 (10.3%) | 107 (33.4%) | 149 (46.6%) | - |
| Follow-up Time (years) | 4.0 (3.7 to 4.2)* | 4.2 (4.0 to 4.4)* | 4.2 (4.0 to 4.3)* | 0.14 |
| Total Visits | 8.2 (7.5 to 8.8)* | 8.4 (7.9 to 8.8)* | 8.4 (8.1 to 8.8)* | 0.85 |
| Baseline Average cpRNFL (µm) | 73.9 (70.9 to 76.8)* | 77.2 (75.3 to 79.0)* | 75.9 (74.5 to 77.5)* | 0.16 |
| Baseline Visual Field MD (dB) | −6.0 (−7.5 to −4.5)* | −3.2 (−4.0 to −2.4)* | −4.2 (−4.9 to −3.5)* | < 0.01 |
| Eyes by Glaucoma Severity (RNFL thickness) | ||||
| < 65 µm | 28 (8.7%) | 31 (9.7%) | 65 (20.3%) | |
| 65 −75 µm | 30 (9.4%) | 53 (16.6%) | 92 (28.7%) | |
| 75 to 85 µm | 19 (5.9%) | 62 (19.4%) | 85 (26.6%) | |
| > 85 µm | 22 (6.1%) | 48 (15.0%) | 78 (24.4%) |
RNFL = Retinal Nerve Fiber Layer
MD = Mean Deviation
Mean and 95% confidence interval
The SD of cpRNFL thickness residuals for each 10 µm bin of their best fitted value are shown in Figure 1. The variability of cpRNFL thickness measurements were compared between AD and ED and there was no statistically significant difference between residuals in the overall sample (p = 0.067) and in eyes without glaucoma (p = 0.913), but we found significantly larger SD of residuals in AD compared to ED in eyes with glaucoma (p = 0.021). The ED patients had similar variability when comparing eyes with or without glaucoma (p=0.112), while AD patients had higher variability when they had glaucoma (p=0.036). The variability tended to be higher when average cpRNFL thickness was also higher, except in AD eyes with glaucoma in which the variability did not vary with RNFL thickness. There was no difference between signal strength of the OCT tests between AD and ED patients overall (p = 0.116) and when stratified by those with and without glaucoma (p = 0.218)
Figure 1.
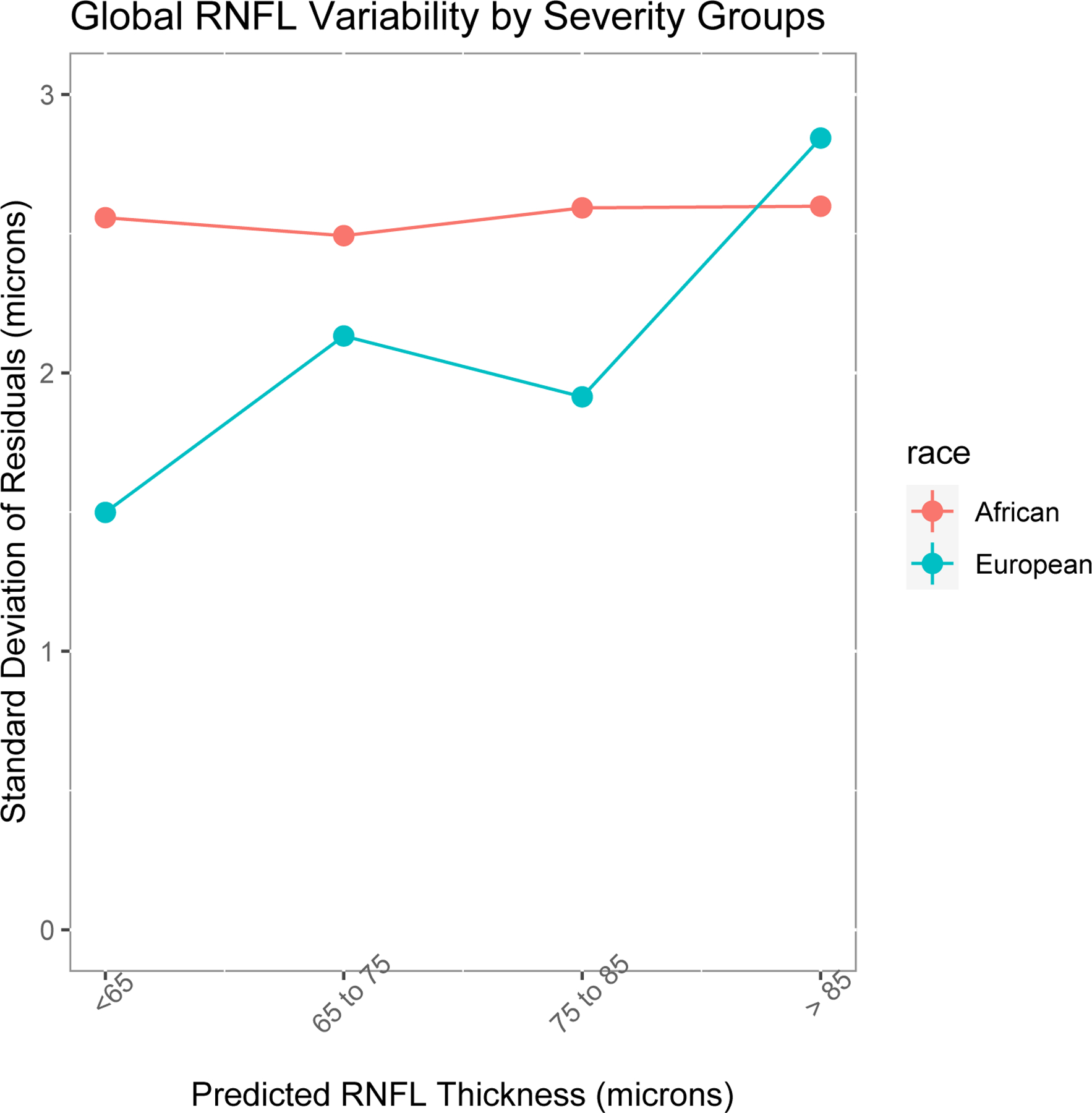
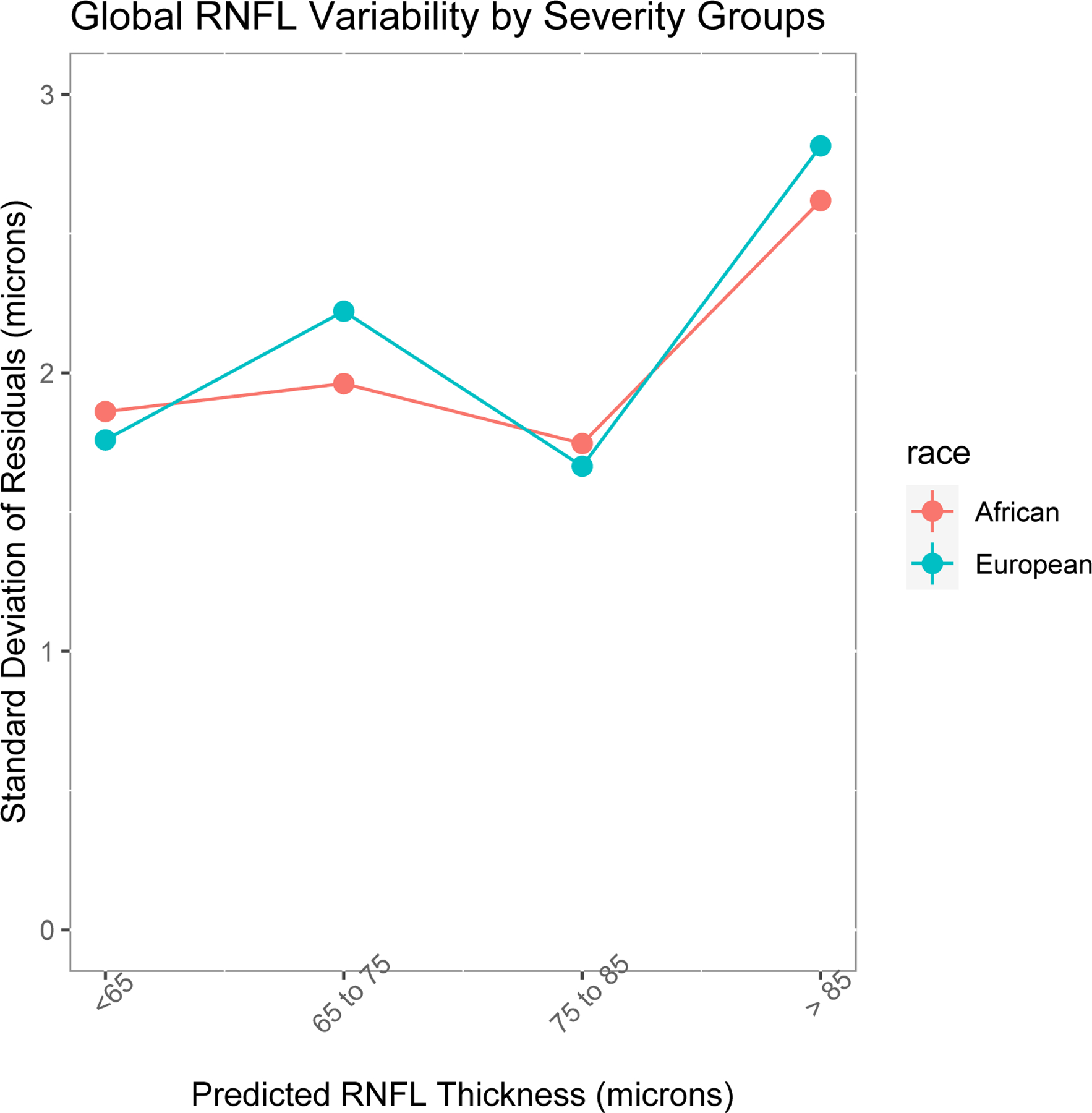
Variability of global circumpapillary retinal nerve fiber layer (cpRNFL) thickness measured with optical coherence tomography (OCT). The variability is described as the standard deviation (µm) of global cpRNFL thickness residuals at 4 levels of RNFL thickness, representing different stages of glaucoma severity. (A) Comparison in eyes with glaucoma by ancestry; (B) comparison in eyes without glaucoma by ancestry.
We analyzed the time and power to detect progression by severity group (early, moderate and severe glaucoma). The time to detect statistically significant progression (negative slope at P < 0.05) at 80% and 90% power for testing paradigms of 4, 6, 12 and 24-month intervals for each group, at different rates of cpRNFL change (−0.5, −1.0 and −2.5 µm/year), are shown in Table 2. Note that eyes with severe and moderate glaucoma (thinner cpRNFL at baseline) had similar time to detect progression across the different rates of change, whereas eyes with early glaucoma (thicker cpRNFL at baseline) required more time to detect progression.
Table 2.
Time (years) to detect progression at different statistical power of global circumpapillary retinal nerve fiber layer thickness with optical coherence tomography using different test paradigms.
|
Time to Detect Progression (years)
at 80% Power |
Time to Detect Progression (years)
at 90% Power |
|||||||
|---|---|---|---|---|---|---|---|---|
| 4-months interval | 6-months interval | 12-months interval | 24-month s interval | 4-months interval | 6-months interval | 12-months interval | 24-months interval | |
| Slope −0.5 µm/year | ||||||||
| Early Glaucoma | 9.4 | 10.5 | 12.6 | 15.1 | 10.5 | 11.8 | 13.9 | 16.7 |
| Moderate Glaucoma | 7.4 | 8.5 | 10.5 | 13.0 | 8.3 | 9.5 | 11.9 | 14.7 |
| Severe Glaucoma | 7.7 | 8.7 | 10.7 | 13.1 | 8.5 | 9.6 | 11.8 | 14.5 |
| Slope −1 µm/year | ||||||||
| Early Glaucoma | 5.7 | 6.3 | 7.5 | 9.0 | 6.4 | 7.0 | 8.4 | 10.1 |
| Moderate Glaucoma | 4.6 | 5.3 | 6.5 | 7.9 | 5.2 | 6.0 | 7.3 | 9.0 |
| Severe Glaucoma | 4.7 | 5.3 | 6.5 | 8.0 | 5.2 | 5.9 | 7.2 | 9.0 |
| Slope −2.5 µm/year | ||||||||
| Early Glaucoma | 2.8 | 3.1 | 3.8 | 4.8 | 3.1 | 3.5 | 4.3 | 5.6 |
| Moderate Glaucoma | 2.5 | 2.9 | 3.6 | 4.4 | 2.9 | 3.3 | 4.1 | 5.1 |
| Severe Glaucoma | 2.5 | 2.7 | 3.4 | 4.3 | 2.8 | 3.1 | 3.8 | 5.1 |
As expected, more frequent testing resulted in shorter time to detect progression. Nonetheless, while there was clear disadvantage for testing every 24 vs 12 months (~22.4% time [25 months] increase) and when testing 12 vs 6 months (~22.1% time [20 months] increase), the improved time to detect progression was less pronounced when comparing 6 vs 4 months (~11.5% time [10 months] reduction). The power to detect progression was comparatively higher in ED patients in moderate and severe glaucoma than early glaucoma, while AD patients did not demonstrate differences in the power to detect progression across the severity stages. Considering −6.0 µm as an estimate of clinically relevant global cpRNFL thinning,19–21 testing at 6 or 4 month intervals appeared similarly effective in detecting early OCT changes in terms of statistical power of detection for different glaucoma severity stages.
When stable eyes were simulated (slope of average RNFL thickness = 0 µm/year), which estimates the false-positive rates for each group, the power to detect progression did not change among early, moderate and severe glaucoma. This false positive rate ranged between 1.01 and 2.04%, depending on testing intervals (Figure 2).
Figure 2.
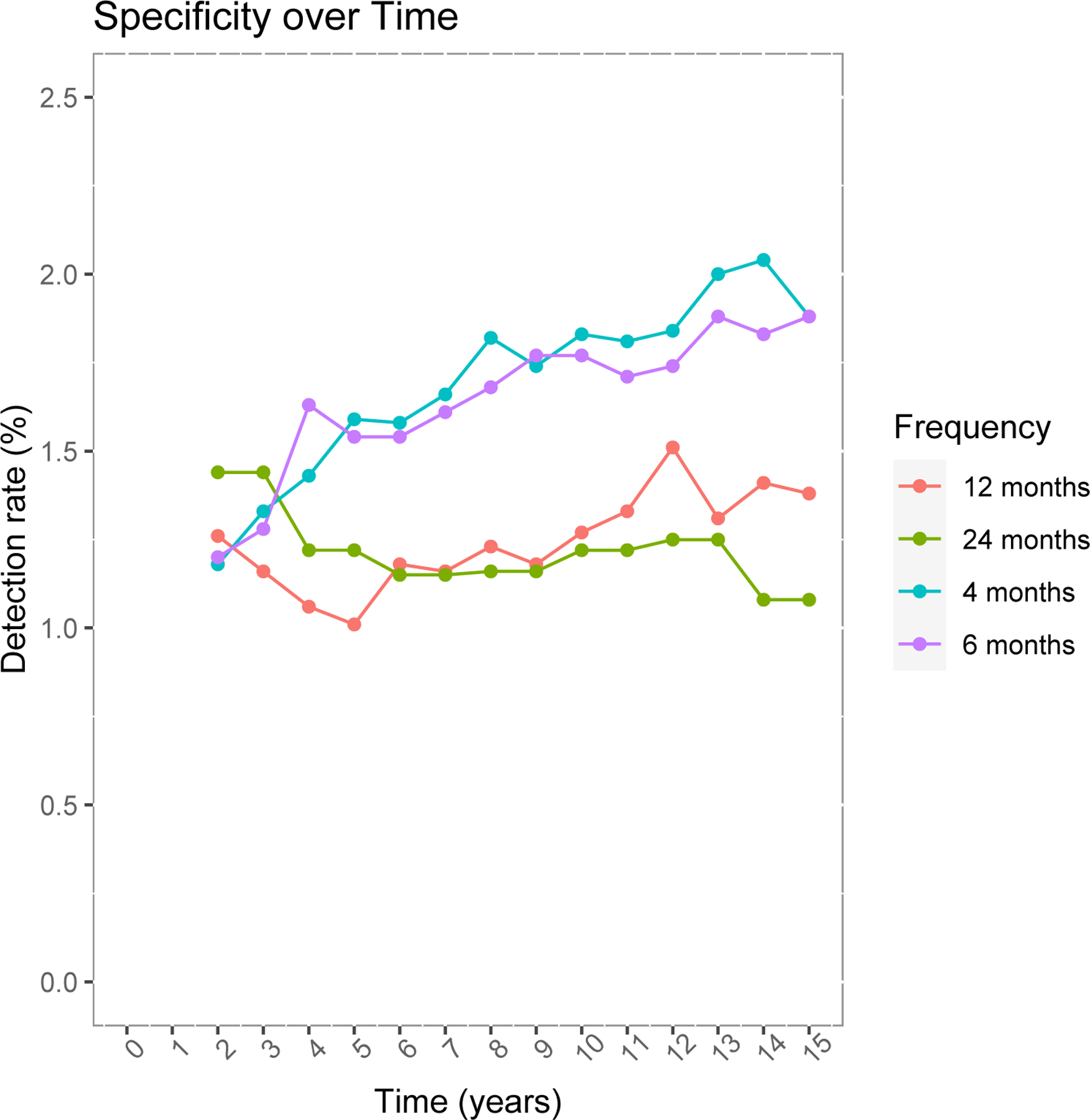
Power to detect progression (%) of retinal nerve fiber layer (RNFL) in stable eyes (slope of average RNFL thickness = 0 µm/year) with optical coherence tomography in different test intervals (4, 6, 12 and 24 months).
DISCUSSION
Based upon actual measurements of OCT variability from a large prospective cohort, we simulated different progression rates of OCT global cpRNFL thinning for different baseline levels of severity and various testing frequency paradigms. Our findings demonstrate, as expected, that more frequent testing increases the statistical power to detect progression of global cpRNFL thickness in patients with manifest glaucoma. Simulations also showed that more frequent testing (at intervals of 4 and 6 months) resulted in earlier detection of OCT changes among progressing eyes, particularly in those with less rapid slopes, with acceptable specificity (i.e., low false positive rates at slopes = 0 µm/year). Although Yu et al.22 evaluated test frequency in their test-retest variability models, we investigated time to detection OCT changes considering both different test intervals and stages of glaucoma severity, which are advantageous in routine settings.
Different rates of glaucoma progression are often observed in clinical practice among patients treated for long periods of follow-up, which can complicate early detection across the disease spectrum.14,23,24 Because VF measures are subjective and have inherent short- and long-term variability at both central and peripheral regions,14,24,25 OCT serve as a more objective biomarker for the follow-up of glaucomatous patients, as it correlates significantly with VF decay.26,27
The optimal frequency of VF testing was previously studied using computer simulations aiming to identify test intervals with greater power to detect statistically significant glaucoma progression.14 Various models have been proposed to define clinically acceptable frequencies of testing, considering both time and power, based on global VF metrics (mean deviation, MD) trend slopes. Studies have found that 80% of fast progressors (eyes with MD slope of −2.0 dB/year) will be detected after 2–3 years, if tested at 6 month intervals.14 Using comparable paradigms, we observed that 80% of eyes categorized as “rapid” progressors (cpRNFL thickness slopes of −2.5 µm/year) will be detected at 2.8, 2.5, and 2.5 years if tested at 4 month intervals, and at 3.1, 2.9, and 2.7 years if tested at 6 month intervals, for the early, moderate and severe OCT damage groups, respectively. Although the specificity to detect progressive changes differed little among the different testing frequencies (Figure 2), how “similar” two or more specificities seem is largely dependent upon their effect on sensitivity. Therefore, the results regarding the power and time to detect progression (Table 2) should be interpreted in light of these differences.
An “optimal” interval of testing should take into account the cost and benefits of prevention of visual impairment, quality of life, and life expectancy. Such parameters were not included in our analysis and warrant further evaluation. Nevertheless, assuming the time to detect more than - 3dB loss in the VF MD as an estimate of significant vision impairment,25,28 the approximate corresponding global cpRNFL thinning based upon reported structure-function graphs using Spectral Domain-OCT (SD-OCT),19–21 is −6 to −8 µm in early of disease stages. Then, considering −6 µm as a significant threshold of global structural loss, both the 6 and 4 months-intervals testing showed a reasonable trade-off for detecting early OCT changes. Given the modest difference in effect when the 6- and 4-months are compared, we believe that the 6-month paradigm with SD-OCT provides a reasonable balance between statistical power, burden to patients and the needs of healthcare systems. Notwithstanding the above, specific groups of high-risk patients may benefit from shorter intervals of SD-OCT examination, such as 4 months, particularly those with early glaucoma. Interestingly, these conclusions are consistent with the frequencies observed for the VF testing.14 The ease, speed, and reproducibility and patient preference of OCT strongly favor the use of OCT to detect rapid progression in clinical practice as compared to perimetry, which has a longer testing duration, is less reproducible, and is more burdensome to patients and technical staff.
Of note, we found greater variability among AD vs ED in glaucoma subjects, which is consistent with what has been reported with perimetry.29 The clinical implication, similar to was reported with perimetry, is that progression detection may be delayed among AD patients. For that reason, clinicians may consider more frequent OCT testing among patients of AD. In addition, we found little effect of RNFL variability on severity in AD subjects, suggesting its greater robustness across disease severity stages compared to perimetry. Our findings are based upon the assumption of a normal distribution of residuals at the different severity bins, as previously done in studies using similar methodology. Future work on the effect of resampling residuals from non-normal distributions on the power and time to detect progression are warranted. Nonetheless, one should be reminded that OCT summary statistics (e.g., global cpRNFL) appears less useful in later stages of the disease due to a floor effect.30–33
Our work has some limitations. The relatively small sample sizes limits the characterization of the differences between AD and ED. The lack of a gold-standard for glaucoma progression also affects the estimate of specificity. As reported in studies looking at VF progression, simulations of stable eyes over time have been used to estimate specificity. Moreover, test variability may be higher for the long- compared to short-term periods,29 which can potentially impact the estimates of specificity in our study. Lastly, our results apply only to global cpRNFL measurements, and might be improved by an SD-OCT parameter that reflects the often localized nature of glaucoma progression.
In summary, these results provide guidance in optimizing the frequency of OCT testing to improve the power to detect statistically significant progression in glaucomatous eyes with different OCT severity levels and rates of change. These results can be used to develop validated guidelines for testing in clinical settings.
Funding/Support:
National Eye Institute Grants U10EY14267, EY08208, EY11008, EY019869, EY13959, 1EY027510, EY029058, EY025253 (CGDM) – Bethesda, MD; Eyesight Foundation of Alabama – Birmingham, AL; Alcon Laboratories Inc. – Fort Worth, TX; Allergan Inc. – Dublin, Ireland; Pfizer Inc. – New York, NY; Merck Inc. – Rahway, NJ; Santen Inc. – Osaka, Japan; unrestricted departmental grant from Research to Prevent Blindness, New York, NY (Department of Ophthalmology, Columbia University Medical Center and Department of Ophthalmology, University of California San Diego), Edith C. Blum Foundation, New York, NY, Bernard Schwartz Travel Grant from the American Glaucoma Society, San Francisco, CA.
Footnotes
Trial Registration: clinicaltrials.gov Identifier: NCT00221923
Conflict of Interest Statement: No conflicting relationship exists for any author.
Financial disclosures:
B.M.S.: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brasília, DF, Brazil
C.G.D.M.: Consultant: Belite – San Diego, CA; Reichert – Buffalo, NY; Novartis – East Hanover, NJ; Galimedix Therapeutics Inc. – Kensington, MD; Carl Zeiss Meditec Inc. – Dublin, CA; Perfuse Therapeutics – San Francisco, CA; Recipient: Heidelberg Engineering GmbH – Heidelberg, Germany; Topcon Medical Systems – Oakland, NJ.
J.S.P.: Consultant: Allergan, Inc. – Dublin, Ireland.
G.A.C.: No financial disclosures.
C.A.G.: Financial support: Research to Prevent Blindness, New York, NY; Heidelberg Engineering GmbH – Heidelberg, Germany; National Eye Institute – Bethesda, MD; Eyesight Foundation of Alabama – Birmingham, AL.
M.A.F.: National Eye Institute – Bethesda, MD; EyeSight Foundation of Alabama, AL; Research to Prevent Blindness – New York NY; Heidelberg Engineering GmbH – Heidelberg, Germany.
R.N.W.: Consultant: Aerie Pharmaceuticals – Pittsburgh, PA; Allergan Inc – Dublin, Ireland; Bausch Healthcare, Inc. – Bridgewater, NJ; Equinox – Newport Beach, CA; Eyenovia – New York NY; Financial support: Heidelberg Engineering GmbH – Heidelberg, Germany; Carl Zeiss Meditec Inc. – Dublin, CA; Centervue – Fremont, CA; Konan Medical – Irvine, CA; Optovue Inc. – Fremont, CA; Bausch Healthcare, Inc. – Bridgewater, NJ.: Topcon Medical Systems – Oakland, NJ Patent: Toromedes, Inc. – La Jolla, CA; Carl Zeiss Meditec Inc. – Dublin, CA.
L.M.Z.: Financial support: − Carl Zeiss Meditec Inc. – Dublin, CA; Heidelberg Engineering GmbH – Heidelberg, Germany; Optovue Inc. – Fremont, CA; Topcon Medical Systems – Oakland, NJ; National Eye Institute – Bethesda, MD; Heidelberg Engineering GmbH – Heidelberg, Germany. Patent: Carl Zeiss Meditec Inc. – Dublin, CA.
J.M.L.: Consultant: Aerie Pharmaceuticals, Inc. – Pittsburgh, PA; Eyenovia – New York NY; Heidelberg Engineering, GmBH – Heidelberg, Germany; NY;– Laval, Canada; Novartis – East Hanover, NJ; Galimedix Therapeutics Inc. – Kensington, MD; Bausch Healthcare, Inc. – Bridgewater, NJ; Allergan, Inc. – Dublin, Ireland. Financial Support: Heidelberg Engineering, GmBH – Heidelberg, Germany; National Eye Institute – Bethesda, MD; Research to Prevent Blindness, New York, NY;
REFERENCES
- 1.Garcia-Valenzuela E, Shareef S, Walsh J, Sharma SC. Programmed cell death of retinal ganglion cells during experimental glaucoma. Experimental Eye Research 1995;61(1):33–44. doi: 10.1016/S0014-4835(95)80056-5 [DOI] [PubMed] [Google Scholar]
- 2.Sommer A, Miller NR, Pollack I, Maumenee AE, George T. The Nerve Fiber Layer in the Diagnosis of Glaucoma. Archives of Ophthalmology 1977;95(12):2149–2156. doi: 10.1001/archopht.1977.04450120055003 [DOI] [PubMed] [Google Scholar]
- 3.Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: A review. JAMA - Journal of the American Medical Association 2014;311(18):1901–1911. doi: 10.1001/jama.2014.3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong ZM, Wollstein G, Schuman JS. Clinical utility of optical coherence tomography in glaucoma. Investigative Ophthalmology and Visual Science 2016;57(9Special Issue):OCT556–OCT567. doi: 10.1167/iovs.16-19933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wollstein G, Schuman JS, Price LL, et al. Optical coherence tomography longitudinal evaluation of retinal nerve fiber layer thickness in glaucoma. Archives of Ophthalmology 2005;123(4):464–470. doi: 10.1001/archopht.123.4.464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medeiros FA, Zangwill LM, Bowd C, Vessani RM, Susanna R, Weinreb RN. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. American Journal of Ophthalmology 2005;139(1):44–55. doi: 10.1016/j.ajo.2004.08.069 [DOI] [PubMed] [Google Scholar]
- 7.Prum BE, Rosenberg LF, Gedde SJ, et al. Primary Open-Angle Glaucoma - Preferred Practice Pattern. Ophthalmology 2016;123(1):P41–P111. doi: 10.1016/j.ophtha.2015.10.053 [DOI] [PubMed] [Google Scholar]
- 8.European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 3: Treatment principles and options Supported by the EGS Foundation. British Journal of Ophthalmology 2017;101(6):130–191. doi: 10.1136/bjophthalmol-2016-EGSguideline.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liebmann JM. Ophthalmology and Glaucoma Practice in the COVID-19 Era. Journal of Glaucoma Published online 2020. doi: 10.1097/ijg.0000000000001519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shabto J, de Moraes CG, Cioffi GA, Liebmann JM. Review of Hygiene and Disinfection Recommendations for Outpatient Glaucoma Care: A COVID Era Update. Journal of Glaucoma 2020;29:409–416. doi: 10.1097/IJG.0000000000001540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sample PA, Girkin CA, Zangwill LM, et al. The African descent and glaucoma evaluation study (ADAGES): Design and baseline data. Archives of Ophthalmology 2009;127(9):1136–1145. doi: 10.1001/archophthalmol.2009.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crabb DP, Garway-Heath DF. Intervals between visual field tests when monitoring the glaucomatous patient: wait-and-see approach. Invest Ophthalmol Vis Sci 2012;53(6):2770–2776. doi: 10.1167/iovs.12-9476 [DOI] [PubMed] [Google Scholar]
- 13.Wu Z, Medeiros FA. Impact of Different Visual Field Testing Paradigms on Sample Size Requirements for Glaucoma Clinical Trials. Scientific Reports 2018;8(1):1–8. doi: 10.1038/s41598-018-23220-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Z, Saunders LJ, Daga FB, Diniz-Filho A, Medeiros FA. Frequency of Testing to Detect Visual Field Progression Derived Using a Longitudinal Cohort of Glaucoma Patients. Ophthalmology 2017;124(6):786–792. doi: 10.1016/j.ophtha.2017.01.027 [DOI] [PubMed] [Google Scholar]
- 15.Leung CKS, Yu M, Weinreb RN, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: A prospective analysis of age-related loss. Ophthalmology 2012;119(4):731–737. doi: 10.1016/j.ophtha.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 16.Wu Z, Saunders LJ, Zangwill LM, Daga FB, Crowston JG, Medeiros FA. Impact of Normal Aging and Progression Definitions on the Specificity of Detecting Retinal Nerve Fiber Layer Thinning. American Journal of Ophthalmology 2017;181:106–113. doi: 10.1016/j.ajo.2017.06.017 [DOI] [PubMed] [Google Scholar]
- 17.Gracitelli CPB, Zangwill LM, Diniz-Filho A, et al. Detection of glaucoma progression in individuals of African descent compared with those of European descent. JAMA Ophthalmology 2018;136(4):329–335. doi: 10.1001/jamaophthalmol.2017.6836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elbendary AM, Mohamed Helal R. Discriminating ability of spectral domain optical coherence tomography in different stages of glaucoma. Saudi Journal of Ophthalmology 2013;27(1):19–24. doi: 10.1016/j.sjopt.2012.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Budenz DL, Fredette MJ, Feuer WJ, Anderson DR. Reproducibility of Peripapillary Retinal Nerve Fiber Thickness Measurements with Stratus OCT in Glaucomatous Eyes. Ophthalmology 2008;115(4). doi: 10.1016/j.ophtha.2007.05.035 [DOI] [PubMed] [Google Scholar]
- 20.Leung CK shun, Cheung CY lui, Weinreb RN, et al. Retinal Nerve Fiber Layer Imaging with Spectral-Domain Optical Coherence Tomography. A Variability and Diagnostic Performance Study. Ophthalmology 2009;116(7):1257–1263.e2. doi: 10.1016/j.ophtha.2009.04.013 [DOI] [PubMed] [Google Scholar]
- 21.Mwanza JC, Oakley JD, Budenz DL, Anderson DR. Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology 2011;118(2):241–248.e1. doi: 10.1016/j.ophtha.2010.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu M, Weinreb RN, Yiu C, et al. Computer Simulation of Progressive Retinal Nerve Fiber Layer Loss in Glaucoma: Performance of Event and Trend Analyses. Investigative Ophthalmology & Visual Science 2011;52(13):9674–9683. doi: 10.1167/iovs.11-8052 [DOI] [PubMed] [Google Scholar]
- 23.de Moraes CG, Liebmann JM, Levin LA. Detection and measurement of clinically meaningful visual field progression in clinical trials for glaucoma. Progress in Retinal and Eye Research 2017;56:107–147. doi: 10.1016/j.preteyeres.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Moraes CG, Paula JS, Blumberg DM, et al. Detection of Progression With 10–2 Standard Automated Perimetry: Development and Validation of an Event-Based Algorithm. American Journal of Ophthalmology 2020;216:37–43. doi: 10.1016/j.ajo.2020.03.046 [DOI] [PubMed] [Google Scholar]
- 25.de Moraes CG, Liebmann JM, Levin LA. Detection and measurement of clinically meaningful visual field progression in clinical trials for glaucoma. Progress in Retinal and Eye Research 2017;56:107–147. doi: 10.1016/j.preteyeres.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Medeiros FA, Zangwill LM, Bowd C, Mansouri K, Weinreb RN. The structure and function relationship in glaucoma: Implications for detection of progression and measurement of rates of change. Investigative Ophthalmology and Visual Science 2012;53(11):6939–6946. doi: 10.1167/iovs.12-10345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Medeiros F, Lisboa R, Weinreb RN, Girkin CA, Liebmann JM, Zangwill LM. A Combined Index of Structure and Function for Staging Glaucomatous Damage. Archives of Ophthalmology 2012;130(9):1107–1116. doi: 10.1001/archophthalmol.2012.827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of Visual Field Loss and Health-related Quality of Life. American Journal of Ophthalmology 2007;143(6):1013–1023. doi: 10.1016/j.ajo.2007.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Urata CN, Mariottoni EB, Jammal AA, et al. Comparison of Short- And Long-Term Variability in Standard Perimetry and Spectral Domain Optical Coherence Tomography in Glaucoma. American Journal of Ophthalmology 2020;210:19–25. doi: 10.1016/j.ajo.2019.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Progress in Retinal and Eye Research 2007;26(6):688–710. doi: 10.1016/j.preteyeres.2007.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hood DC, Anderson SC, Wall M, Kardon RH. Structure versus Function in Glaucoma: An Application of a Linear Model. Investigative Ophthalmology & Visual Science 2007;48(8):3662–3668. doi: 10.1167/iovs.06-1401 [DOI] [PubMed] [Google Scholar]
- 32.Mwanza JC, Budenz DL, Warren JL, et al. Retinal nerve fibre layer thickness floor and corresponding functional loss in glaucoma. British Journal of Ophthalmology 2015;99(6):732 LP–737. doi: 10.1136/bjophthalmol-2014-305745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mwanza JC, Kim HY, Budenz DL, et al. Residual and Dynamic Range of Retinal Nerve Fiber Layer Thickness in Glaucoma: Comparison of Three OCT Platforms. Investigative Ophthalmology & Visual Science 2015;56(11):6344–6351. doi: 10.1167/iovs.15-17248 [DOI] [PMC free article] [PubMed] [Google Scholar]


