Abstract
There is presently a rural hospital shortage in the United States with 180 closures since 2005 and hundreds of additional institutions at risk. Although the hospital closure phenomenon is well-established, less is known about the spillover impact on the operations and financial wellbeing of surrounding healthcare institutions. This preliminary study quantified how discrete rural hospital closures impact institutions in their regional proximity, finding a significant increase in inpatient admissions and emergency department visits for these “bystander hospitals.”
Introduction
For decades, rural US communities lacking healthcare infrastructure have relied on critical access hospitals, defined as short-term, general acute non-federally funded hospitals, and federally funded, Rural-Urban Commuting Area (RUCA) type-4 or higher facilities. Such organizations are normally under 100 beds and serve as points of emergency care or limited inpatient clinical interventions—effectively security nets on the frontline of rural healthcare. Hospital closures over the past two decades have begun dismantling this protection. Since 2005, there have been 180 rural hospital closures, with nearly 700 more in precarious financial condition, and 200 on the verge of collapse(1–3).
Multiple factors have likely converged to precipitate this trend over the last several decades, ranging from state-level decisions to decline Medicaid expansion, lower health technology implementation, to the growing influence of private equity firms in the healthcare market, and rising regional health system competition. In fact, one-third of rural closures are attributable to states declining Medicaid expansion, resulting in less reimbursement and lower operating margins and opportunities for growth and service maintenance4,5. Unfortunately, these hospitals often lack critical access hospital designation, which provides protections that allow operation within a safer margin, leaving larger hospitals to contend with shrinking profit margins at a greater expense to solvency. Similarly, states declining Medicaid expansion have experienced the worst hospital profitability and an increased number of closures in the past decade,6 leaving vulnerable rural hospitals with limited ability to bill for complex, underinsured patient populations. Moreover, rural communities have limited healthcare infrastructure, often lacking opportunities to leverage other services to balance healthcare gaps. These regions are also disproportionately affected by population stagnation and slow economic/job growth7, reducing market incentives to serve smaller patient populations.
Although the phenomenon of rural hospital closures is well-established, less is known about the spillover impact of this trend on surrounding healthcare institutions (i.e., “bystander hospitals”). This study sought to quantify how discrete rural hospital closures impact regional environments, specifically visits and admissions at rural bystander hospitals. We hypothesized that, given the increased number of closures and relative scarcity of bystander hospitals in regions where closures occur, there would be significant impact to existing institutions through increased hospital admissions and emergency department visits. We also hypothesized that each hospital type (nonprofit, for-profit, government) would respond differently to these increased volumes.
Study Data and Methods
Using a repository of rural hospital closures created by the University of North Carolina Cecil G. Sheps Center for Health Services Research, we identified US hospital closures over the past 15 years. Criteria for inclusion were hospitals that had been fully closed between 2005–2016 and with >25-bed capacity2. We then designated surrounding hospitals within a 30-mile radius of each closed hospital as “bystander hospitals,” and identified CMS billing identification numbers. This number was chosen because the average distance for residents of rural communities to travel to a hospital is 17 miles3. We assumed that, in the event of a local closure, it would nearly double that standard time, and therefore used an even calculation of 30 miles. Using the American Hospital Association Annual Survey, we examined each institution’s admissions and emergency department visits within the study timeframe. The AHA survey is a national survey performed with over 5,000 hospitals that includes information on inpatient volumes, emergency admissions, cost for leases, and equipment usage per unit.
We examined average rate-of-change for inpatient admissions and emergency department visits in surrounding hospitals both two years before and after relevant hospital closures. These results were normalized to temporal change after their collection. A two-tailed t-test was performed to establish if there was significant difference in admissions and emergency department visits two years preceding and following the closure, and this was confirmed by one-way ANOVA tests. Both calculations were adjusted for outliers within the hospital dataset and within the ambulance response range of the hospital closure in question via the interquartile range (IQR) method by multiplying the IQR by 1.5 to create a range outside the Q1 and Q38.
In order to show the big-picture impact of bystander hospitals taking on spillover patients, overall cost increase was evaluated by documenting hospital inpatient volumes (this was an estimate as data was not available). Inpatient volume was determined from the American Hospital Association (AHA) survey. Cost per patient was estimated by multiplying inpatient general medicine average length-of-stay from the American Hospital Directory by the inpatient hospital cost of care per inpatient day based on hospital type (private, public, government) in each state (Kaiser Family Foundation). These designations were used to evaluate whether there were differences in how each hospital type would handle increase in volumes in rural areas, as each institution has differences in its operational ethos. Data from two years prior to hospital closure established a baseline of performance and the two years after the hospitals’ closure was used to show the change. Other variables included were the Case Mix Index and total profit margins from the American Hospital Directory’s database. Case Mix Index was used both as a method to indicate severity of patient population and as an indirect variable to assess reimbursement.9 The American Hospital Directory is a for-profit service that catalogs information from 7,000 hospitals across the US using CMS information and third-party surveys to obtain statistics on hospital functionality.
Study Results
Fifty-three hospital closures and 93 bystander hospitals met criteria (18 for-profit, 37 nonprofit and 29 government institutions) during the study period. Geographically, 66% of closures were in the South (Florida, Virginia, North Carolina, South Carolina, Georgia, Alabama, Texas, Louisiana, Tennessee, Oklahoma, Arkansas, Kentucky) and 21% in Appalachia (Pennsylvania, West Virginia, Virginia, Kentucky, Tennessee, Alabama, Georgia, North Carolina). Average emergency department visits increased by 3.59% two years prior to a hospital’s closure; however, at two years post-closure the average rate of increase rose to 10.22% (F(4,47)=2.77, p=0.0375) (Fig 1). Average bystander hospital admissions fell by 5.73% in the two years preceding the hospital closure but increased 1.17% in the two years after (F(4,46)=3.05, p=0.0259) (Fig 2).
Figure 1. Average Percent Change of ED in Bystander Hospitals two years before and after closure.
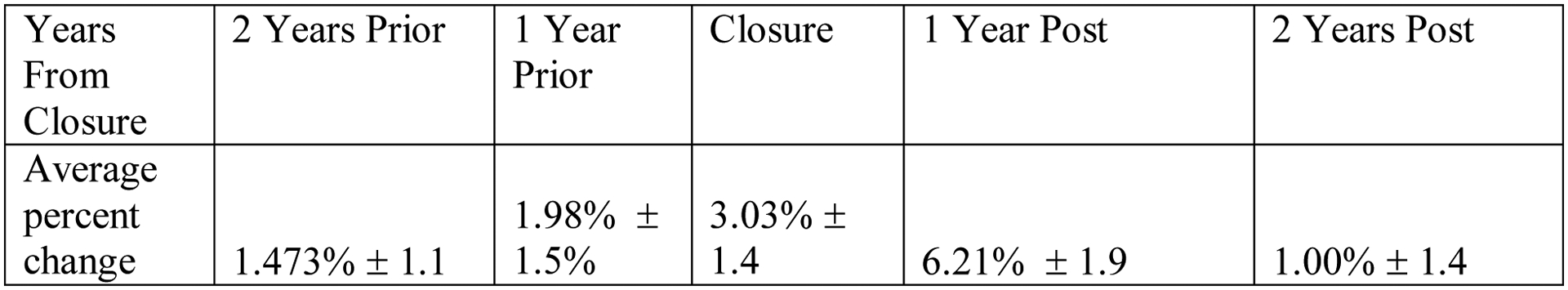
Figure 1 shows a five-year span with the two years preceding the hospital closure and two years afterwards along with the year of closure. Percentages shown represent the average percent-change in volume of emergency department visits for all of the bystander hospitals compared to the previous year.
Figure 2. Average Percent Change of Admission in Bystander Hospitals two years before and after closure.
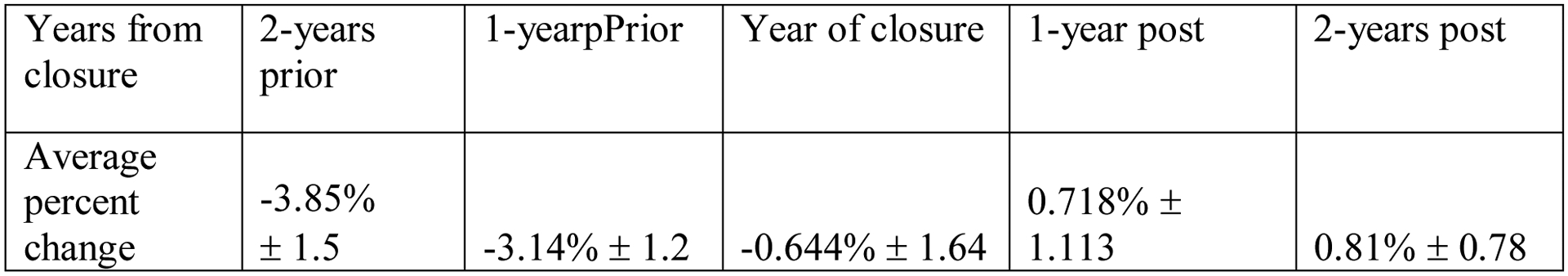
Figure 2 shows a five-year span with the two years preceding the hospital closure and two years afterwards along with the year of closure. Percentages represent the average percent change in volume of in-patient admissions for all of the bystander hospitals compared to the previous year.
The average profit total margin of bystander hospitals was 0.75% with a median profit margin of 2.15%. In for-profit institutions, average profit margin was −0.64%, with a Medicare mix index of 1.217, average cost-to-charge ratio of 1:4.62, and an average patient-per-day cost of $2090.00 (Table 1). For nonprofit institutions, average profit margin was 1.56% with a Medicare Mix Case Index of 1.26, average cost to charge ratio of 3.00, and average cost of $2,475.00. For government hospitals, average profit margin was 0.59%, Medicare case mix index was 1.168, cost to charge ratio was 2.79, and average patient cost was $2,224.00 per patient. The average change in cost for nonprofit hospitals was $7,275,860 as opposed to for-profit institutions that experienced a mean change of $1,354,805. Additionally, nearly all bystander institutions were larger than the closed hospital bed number.
Table 1.
A breakdown of the profit margin, case mix, inpatient charge, length-of-stay, expense per day, cost of inpatient stay, and cost of admission increase across for-profit, governmental, and non-profit hospitals. Also reported is the increase charge of admission with these institutions. This demonstrates the differences between the hospital types that are receiving overflow and provides a sense of what their disease populations contrasted with their inpatient stay and associated costs and charges.
| Type of Hospital | Profit Margin | Medicare Case Mix Index | Inpatient Charge | LOS of Inpatient Med | Expense Per day (based on state and Hospital type) | Cost of Inpt stay | Cost of Admission Increase |
|---|---|---|---|---|---|---|---|
| For Profit | −0.64% | 1.22 | $41,428.89 | 4.81 | $2,090.28 | $ 9,652.13 | $1354,805.62 |
| Government | 0.59% | 1.17 | $ 23,538.72 | 3.94 | $ 2,224.66 | $ 8,812.47 | $2,073,923.12 |
| NonProfit | 1.49% | 1.26 | $29,601.67 | 3.98 | $ 2,436.17 | $ 9,752.85 | $3,516,759.51 |
Discussion
We observed a significant increase in inpatient admissions and emergency department visits in “bystander” healthcare institutions two years following rural hospital closures. To our knowledge, this is the first attempt to quantify the downstream impact of admissions and emergency department visits with respect to proximate hospitals in rural regions.
This finding, combined with the low (~1–1.2) CMS Mix Case Index, suggests that reimbursements could be relatively low for both types of visits, showing a possible stagnation or loss in revenue that is not paired with other more highly reimbursed service lines (e.g., Orthopedics, Neurosurgery, Cardiology) (see Table 1). Such a trend could be explained by lower billing amounts due to lack of specialty care since most patients are being seen for less severe issues. Although at first glance, an increase of patients would seem positive for a hospital, the type of patient is important as well as the required staffing required for patient support10. For-profit and nonprofit entities operating in the contemporary healthcare landscape require case-mix diversification through high cashflow specialties with profit-neutral specialties to maintain positive total profit margins.11 Greater numbers of inpatient general medicine patients increase costs through facilities and staffing, creating challenges for hospital growth and viability.12
Given these populations have large Medicare and Medicaid utilization, current federal policies that reduce reimbursements can lead to even steeper losses. Critical access hospitals have had an easier time avoiding these problems given the 2006 CMS requirement that these hospitals adhere to the distance guidelines (i.e., over 30-miles to the nearest hospital).
The increasing costs of inpatient services are also significant. The nonprofit sector was hardest hit with a $7,275,866 increase in per year hospital costs. For-profit institutions only experienced a $1,354,805 cost increase; however, these hospitals have had a −0.64% profit margin on average, demonstrating financial loss. While this could be attributed to various reasons beyond the scope of our study, one major cause could be the tax-exempt status of nonprofits as well as the taxpayer funding of government sites8. Both advantages allow an offset of costs in the form of cash infusions from taxpayers or the lack of taxes taking a portion of profits that could pay for extra costs. Government establishments are at a middle point with a 0.59% profit margin and a little over $2 million increase in cost, but due to their ability to subsidize, this would not inherently result in closure.
In emergency departments, the increase in visits suggests that patients have indeed been coming from closed institutions to bystander institutions, even in rural settings. It is also suggestive that the rise in inpatient admissions are a byproduct. This is thus suggestive of an increase in inpatient admission volumes, as the more ED visits occur, the more inpatient admissions follow (Fig 2).14
These findings may portend a daunting future for healthcare in the rural US. While previous literature has described the acute effects hospital closures have on communities, this study suggests a significant spillover effect on hospitals within the geographic region15. This establishes cyclical processes at play in the rural healthcare sector whereby nonprofit health companies lose money on rural hospitals not built as high-profit institutions. The accountability these hospitals have to their communities is more intimate, as they serve as regional lifelines and their closure directly impacts the population’s health. This is especially true at present, as rural America is experiencing a disproportionate rise in deaths of despair (i.e., rising excess mortality and morbidities from suicide, alcoholism, and drug poisonings that is contributing to declining life expectancy in the US), and loss of infrastructure and job security that further decrease the quality of public health efforts in their current manifestation16,17,18,19.
In addition, this pattern of closures has occurred during an era of heavy consolidation in medicine whereby health systems are buying small hospitals to expand care networks. At present, 72% of hospitals are affiliated with a health network with wide reach and ample catch basins of patients20. These healthcare networks provide a care network for smaller hospitals which often are incentivized to become acquired by these networks. If not, they risk being put out-of-business through competition via health systems or bought out via private equity groups21. A hospital’s solvency is based on the amount of reimbursements Medicare gives for cash positive service lines.22 If a hospital cannot meet these requirements, they can be at a higher risk of bankruptcy.
Limitations
This study has several limitations. First, the cost figures utilized are largely estimated based on exact number of admissions multiplied by state averages based on hospital type. This was chosen as the metric because hospital financial data is not public information and hospitals share information through the AHA. Secondly, our dataset of hospitals was extracted from UNC’s Sheps Center supplemented with information from the AHD and AHA, which might omit other rural definitions for hospitals or might not mention other hospitals entirely. Thirdly, the data used for hospital admissions is assumed to be general medicine as it is assumed that for small hospital most people would be admitted to hospitalist service with consulting services providing specialty care. However, this may not hold true in all institutions as some may have admitting services. Moreover, there is no way to control for external community factors in each of these regions that could have had their own independent effect to closure. Local economies, population loss, and catastrophic events can lead to an inhospitable environment for a healthcare facility as well. Lastly, the sample size was significantly reduced with the parameters of the study. This was due to the strict criteria applied to the hospital analyzed, as the institutions were required to be completely closed with >25 beds to indicate there would be a sizable spillover effect for the surrounding healthcare infrastructure.
Conclusion
The significant spillover reflected in rising emergency department visits and inpatient admissions rates for bystander hospitals in regional proximity to closed hospitals demonstrates the burden on such closures for regional healthcare systems. Regional scarcity caused by hospital closures increases patient load for other institutions, and this cycle tends to perpetuate itself until there is either a regional monopoly or no infrastructure exists. Such closures also exert detrimental effects on the fiscal health of regions, as the folding of healthcare systems causes infrastructure and business that surround them to suffer. In the absence of regulatory oversight or public health programs in regions affected by closures, poor health outcomes, including “diseases of despair,” are likely to continue proliferating, disproportionately affecting the most vulnerable. In the COVID-19 era, it will be especially necessary to focus on hospital closures given increased risk of maintaining solvency due to delayed and deferred care atop already tight margins. Future analysis of this data and other research prospects in this field should examine the reasons why fluctuations are linked to closures and how types of hospitals are affected.
Supplementary Material
Acknowledgments:
We appreciate the support of the Penn State Clinical and Translational Science Institute.
This project was supported in part by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR002014. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH
Footnotes
Competing interests statement:
The authors have no competing interests to disclose.
References
- 1.Malone TL, Planey AM, Bozovich LB, Thompson KW, Holmes GM. The economic effects of rural hospital closures. Health Serv Res. 2022;57(3):614–623. doi: 10.1111/1475-6773.13965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.University of North Carolina. Rural Hospital Closures, Cecil G Sheps Center for Health Services Research, 17 May 2021, www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/. [Google Scholar]
- 3.Parker Kim. Horowitz Juliana. Brown Anna. Fry Richard. Cohn D’Vera. Igielnik Ruth. What Unites and Divides Urban, Suburban and Rural Communities. Pew Research Center. 22 May. 2018. https://www.pewresearch.org/social-trends/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/ [Google Scholar]
- 4.Topchik Michael. IVantage Index, 2017, The Chartis Group, www.ivantageindex.com/2017-rural-relevance-study/. [Google Scholar]
- 5.Dranove D, Gartwaite C, Ody Ch. The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal. Issue Brief (Commonw Fund). 2017;12:1–9. [PubMed] [Google Scholar]
- 6.Braga Michael, et al. “Leaving Billions of Dollars on the Table.” USA Today Network News, 28 July 2019, stories.usatodaynetwork.com/ruralhospitals/financialtroubles/. [Google Scholar]
- 7.Lindrooth RC, Perraillon MC, Hardy RY, Tung GJ. Understanding The Relationship Between Medicaid Expansions And Hospital Closures. Health Aff (Millwood). 2018;37(1):111–120. doi: 10.1377/hlthaff.2017.0976 [DOI] [PubMed] [Google Scholar]
- 8.Parker Kim. Horowitz Juliana. Brown Anna. Fry Richard. Cohn D’Vera. Igielnik Ruth. What Unites and Divides Urban, Suburban and Rural Communities. Pew Research Center. 22 May. 2018. https://www.pewresearch.org/social-trends/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/ [Google Scholar]
- 9.Beyer H (1981), Tukey John W.: Exploratory Data Analysis. Addison-Wesley Publishing Company Reading, Mass. — Menlo Park, Cal., London, Amsterdam, Don Mills, Ontario, Sydney: 1977, XVI, 688 S.. Biom. J, 23: 413–414. 10.1002/bimj.4710230408 [DOI] [Google Scholar]
- 10.Bai G, Anderson GF. A More Detailed Understanding Of Factors Associated With Hospital Profitability. Health Aff (Millwood). 2016;35(5):889–897. doi: 10.1377/hlthaff.2015.1193 [DOI] [PubMed] [Google Scholar]
- 11.Wishner Jane, et al. “A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies - Issue Brief.” Kaiser Family Foundation, 19 Apr. 2018, https://www.kff.org/report-section/a-look-at-rural-hospital-closures-and-implications-for-access-to-care-three-case-studies-issue-brief/. [Google Scholar]
- 12.Rosko MD, & Mutter RL (2008). Stochastic frontier analysis of hospital inefficiency: a review of empirical issues and an assessment of robustness. Medical care research and review : MCRR, 65(2), 131–166. 10.1177/1077558707307580 [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum S, Kindig DA, Bao J, Byrnes MK, O’Laughlin C. The Value Of The Nonprofit Hospital Tax Exemption Was $24.6 Billion In 2011. Health Aff (Millwood). 2015. Jul;34(7):1225–33. doi: 10.1377/hlthaff.2014.1424. Epub 2015 Jun 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsia RY, Shen YC. Emergency Department Closures And Openings: Spillover Effects On Patient Outcomes In Bystander Hospitals. Health Aff (Millwood). 2019. Sep;38(9):1496–1504. doi: 10.1377/hlthaff.2019.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holmes George M et al. “The effect of rural hospital closures on community economic health.” Health services research vol. 41,2 (2006): 467–85. doi: 10.1111/j.1475-6773.2005.00497.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skinner HG, Blanchard J, Elixhauser A. Trends in Emergency Department Visits, 2006–2011: Statistical Brief #179. 2014 Sep. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. Feb-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK254201/ [Google Scholar]
- 17.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brignone E, George DR, Sinoway L, et al. Trends in the diagnosis of diseases of despair in the United States, 2009–2018: a retrospective cohort study. BMJ Open. 2020;10(10):e037679. Published 2020 Nov 9. doi: 10.1136/bmjopen-2020-037679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George DR, Snyder B, Van Scoy LJ….Kraschnewski J. (2021). Perceptions on Diseases of Despair by Members of Rural and Urban High-Prevalence Communities: A Qualitative Study. JAMA Network Open. 4(7):e2118134. doi: 10.1001/jamanetworkopen.2021.18134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Probst J, Eberth JM, Crouch E. Structural Urbanism Contributes To Poorer Health Outcomes For Rural America. Health Aff (Millwood). 2019;38(12):1976–1984. doi: 10.1377/hlthaff.2019.00914 [DOI] [PubMed] [Google Scholar]
- 21.“Fast Facts on U.S. Hospitals, 2021: AHA.” American Hospital Association, Health Forum, 2021, www.aha.org/statistics/fast-facts-us-hospitals. [Google Scholar]
- 22.Bruch J, Zeltzer D, Song Z. Characteristics of Private Equity-Owned Hospitals in 2018. Ann Intern Med. 2021;174(2):277–279. doi: 10.7326/M20-1361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turner J, Broom K, Elliott M, Lee JF. A Decomposition of Hospital Profitability: An Application of DuPont Analysis to the US Market. Health Serv Res Manag Epidemiol. 2015;2:2333392815590397. Published 2015 Jul 22. doi: 10.1177/2333392815590397 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


