Abstract
Brain-derived neurotrophic factor (BDNF), an exercise-induced neurotrophin, is an important factor in memory consolidation and cognitive function. This study evaluates the association between plasma BDNF levels and frailty in community-dwelling older adults. Plasma BDNF levels were analyzed in a total of 302 individuals aged 70–84 years from the Korean Frailty and Aging Cohort Study. There were 30 (9.9%) participants with frailty. They were older and had a higher prevalence of dementia and depression than those without frailty. There were no differences in the proportion of male sex between the frail and non-frail groups. Plasma BDNF levels were significantly lower in participants with frailty than in those without frailty. The presence of frailty was significantly associated with plasma BDNF levels (odds ratio 0.508, 95% confidence interval 0.304–0.849) as well as age, hemoglobin, and the presence of dementia, and depression. After adjustment for confounding factors, the significant association between plasma BDNF and frailty was maintained (0.495, 0.281–0.874). This association remained consistent after exclusion of individuals with dementia, depression, stroke, diabetes, and osteoporosis. Plasma BDNF levels were significantly associated with frailty in community-dwelling older adults. Our study may suggest the possible role of BDNF as a novel biomarker of frailty.
Subject terms: Biomarkers, Endocrinology
Introduction
Brain-derived neurotrophic factor (BDNF) is the most abundant neurotrophin that regulates neuronal survival, differentiation, and synaptic plasticity in the brain1. The amount of plasma BDNF has been considered to partly reflect its secretion in the brain2, although other potential sources contribute to its circulating levels including platelets, vascular endothelial and smooth muscle cells, and activated macrophages and lymphocytes3,4. Growing evidence has suggested that blood BDNF levels could be used as a biomarker for diagnosis, prognosis, and treatment monitoring of Alzheimer’s disease5. Blood BDNF levels are involved in the recurrent and severity of depression6. In addition, it is well established that lower levels of circulating BDNF are related to a high risk of stroke7 and poor recovery after stroke8. Furthermore, low levels of blood BDNF accompany impaired glucose metabolism9 and low bone mineral density10.
Regular exercise is known to reduce the risk of cardiometabolic diseases, dementia, and depression11–13. Recent studies suggested that BDNF may be a key mediator linking vascular and metabolic benefits of exercise with protection from neurodegenerative diseases11. In fact, little has been known about the sources and mechanisms underlying exercise-induced changes in circulation levels of BDNF14. BDNF is identified as a contraction-inducible protein in skeletal muscle because it has been shown to be produced by skeletal muscle during exercise and enhance lipid oxidation in skeletal muscle via activation of AMP-activated protein kinase (AMPK)15. However, the BDNF synthesized by the skeletal muscle during physical exercise acts on the muscle in an autocrine and paracrine manner15. Interestingly, exercise provokes synthesis of fibronectin type III domain-containing protein 5 (FNDC5) and its cleaved, circulating form irisin, which may cross the blood–brain barrier and induces BDNF production16. In obese animals, administration of BDNF mimetic induces mitochondrial biogenesis, promotes lipid oxidation in skeletal muscle, and alleviates metabolic derangement17. Serum BDNF levels are significantly elevated in humans in response to exercise training18. Recent human studies demonstrated the correlation of blood BDNF and skeletal muscle function. Serum BDNF was positively correlated with skeletal muscle strength, but not with muscle mass, in patients with heart failure19. Moreover, decline in BDNF was associated with deterioration in muscle strength and physical performance in Japanese hemodialysis patients20.
Frailty, a clinical syndrome of decline in reserve and resistance to stressors across multiple physiologic systems, is common in elderly individuals21. As such, frailty has been associated with adverse outcomes including prevalent cardiovascular disease (CVD) and mortality22,23. Fried et al.21 defined a clinical phenotype of frailty, in which three or more of the following five criteria are present: unintentional weight loss, self-reported exhaustion, weakness, slowness, and low physical activity. Therefore, loss of muscle mass and function in elderly individuals can contribute to greater vulnerability to frailty. Despite the possible role of blood BDNF in muscle function, the relationship between circulating BDNF and frailty has not yet been fully elucidated. Exploration off frailty biomarkers may support the early identification of elderly individuals with frailty and easier monitoring during intervention24. Therefore, we aimed to investigate whether plasma BDNF levels are correlated with frailty in community-dwelling Korean older adults. We also conducted sensitivity analyses to exclude individuals with BNDF-related comorbidities including dementia, depression, stroke, diabetes, CVD, and osteoporosis.
Results
Study subject characteristics
This study included a total of 302 participants with median age 75 years (IQR 73–79 years). Among them, 30 (9.33%) had physical frailty. Baseline characteristics of the study population were shown in Table 1. Frail group had higher age compared to non-frail group. There were no differences in the proportion of male sex, current smoker, regular drinker, and low income; BMI and blood pressure; TC, FPG, HOMA-IR, hs-CRP, hemoglobin, and creatinine; in the prevalence of diabetes, hypertension, dyslipidemia, and obesity between the frail and non-frail groups. However, participants with frailty had higher proportion of dementia (40% vs. 14%, P < 0.001) and depression (43.3% vs. 13.6%, P < 0.001) compared to those without frailty.
Table 1.
Baseline characteristics of study population according to the presence of frailty.
| Variables | Total | No Frailty | Frailty | P-value |
|---|---|---|---|---|
| N | 302 | 272 | 30 | |
| Age | 75 (73, 79) | 75 (72, 78) | 78.5 (75, 80) | 0.001 |
| Male, n (%) | 148 (49) | 134 (49.3) | 14 (46.7) | 0.787 |
| BMI, kg/m2 | 25.15 ± 3.37 | 25.15 ± 3.3 | 25.13 ± 4.01 | 0.977 |
| SBP, mmHg | 131.76 ± 14.94 | 132.06 ± 14.79 | 128.98 ± 16.24 | 0.284 |
| DBP, mmHg | 77.84 ± 9.07 | 78.05 ± 9.07 | 75.97 ± 8.95 | 0.234 |
| Current smoker, n (%) | 24 (7.9) | 21 (7.7) | 3 (10) | 0.661 |
| Regular drinking, n (%) | 57 (18.9) | 54 (19.9) | 3 (10) | 0.191 |
| Low income, n (%) | 110 (36.4) | 95 (34.9) | 15 (50) | 0.104 |
| Total cholesterol | 171 (147, 194) | 171 (146, 194) | 173.5 (153, 194) | 0.858 |
| FPG, mg/dL | 98 (91, 116) | 98 (90.5, 114) | 103.5 (93, 123) | 0.129 |
| HOMA-IR | 1.54 (1.02, 2.66) | 1.50 (1.00, 2.63) | 1.97 (1.24, 3.07) | 0.140 |
| hs-CRP, mg/dL | 0.72 (0.46, 1.34) | 0.73 (0.47, 1.33) | 0.63 (0.42, 2.19) | 0.974 |
| Hemoglobin, g/dL | 13.63 ± 1.34 | 13.68 ± 1.28 | 13.16 ± 1.76 | 0.124 |
| Creatinine, mg/dL | 0.82 (0.7, 0.96) | 0.82 (0.7, 0.96) | 0.88 (0.72, 1.06) | 0.203 |
| BDNF, ng/mL | 7.41 (5.03, 11.41) | 7.54 (5.19, 11.60) | 4.94 (3.02, 7.91) | 0.008 |
| Diabetes, n (%) | 98 (32.5) | 84 (30.9) | 14 (46.7) | 0.080 |
| Hypertension, n (%) | 199 (65.9) | 176 (64.7) | 23 (76.7) | 0.190 |
| Dyslipidemia, n (%) | 128 (42.4) | 117 (43) | 11 (36.7) | 0.463 |
| Obesity, n (%) | 150 (49.7) | 138 (50.7) | 12 (40) | 0.264 |
| Dementia, n (%) | 50 (16.6) | 38 (14) | 12 (40) | < 0.001 |
| Depression, n (%) | 50 (16.6) | 37 (13.6) | 13 (43.3) | < 0.001 |
Data are expressed as percentage or as mean (IQR) or mean ± SD, unless otherwise noted. Groups were compared using χ2 test for categorical variables and independent two-sample t-test or Mann-Whiney U-test for continuous variables after log-transformation of skewed variables including plasma BDNF. BDNF, brain-derived neurotrophic factor; BMI, body mass index; DBP, diastolic blood pressure; FPG, fasting plasma glucose; HOMA-IR, homeostasis model assessment-insulin resistance; hs-CRP, high-sensitivity C-reactive protein; SBP, systolic blood pressure.
Plasma BDNF levels in participants with and without frailty
Plasma BDNF levels were significantly lower in participants with frailty than in those without frailty (median [IQR]: 4.94 [3.02, 7.91] vs. 7.54 [5.19, 11.60] ng/mL, P = 0.008) (Table 1, Fig. 1). When divided by sex, plasma BDNF levels were lower in frail subjects compared to control subjects, but not in statistically significant in women (Fig. 1).
Figure 1.
Plasma brain-derived neurotrophic factor levels according to the presence of frailty in total participants (A), males (B), and females (C).
Association between plasma BDNF levels and frailty
Next, we performed univariate and multivariate logistic analyses to identify the association between the presence of frailty and plasma BDNF concentration and metabolic parameters (Table 2). In a univariate analysis, an increase in plasma BDNF was associated with a reduced risk of frailty (odds ratio [OR] 0.508, 95% confidence interval [CI] 0.304–0.849, P = 0.01). On the other hand, an increase in age and the presence of dementia or depression were associated with an increased risk of frailty. The association between plasma BDNF and frailty remained in the multivariate analysis after adjustment for confounding factors (OR 0.495, 95% CI 0.281–0.874, P = 0.015).
Table 2.
Association of brain-derived neurotrophic factor or metabolic parameters with the presence of frailty.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age | 1.187 (1.067, 1.321) | 0.002 | 1.135 (1.007, 1.278) | 0.038 |
| Sex | 0.901 (0.423, 1.918) | 0.787 | ||
| BMI | 0.998 (0.893, 1.117) | 0.977 | ||
| SBP | 0.986 (0.961, 1.012) | 0.283 | ||
| Current smoking | 1.328 (0.372, 4.745) | 0.662 | ||
| Regular drinking | 0.449 (0.131, 1.534) | 0.201 | ||
| Low income | 1.863 (0.873, 3.975) | 0.108 | ||
| TC | 1.001 (0.99, 1.012) | 0.864 | ||
| FPG | 1.009 (0.999, 1.02) | 0.091 | ||
| HOMA-IR | 1.015 (0.908, 1.135) | 0.789 | ||
| hs-CRP | 1.066 (0.939, 1.21) | 0.322 | ||
| Hemoglobin | 0.742 (0.556, 0.991) | 0.044 | 0.868 (0.637, 1.182) | 0.368 |
| Creatinine | 4.45 (0.864, 22.917) | 0.074 | ||
| BDNF | 0.508 (0.304, 0.849) | 0.010 | 0.495 (0.281, 0.874) | 0.015 |
| Dementia | 4.105 (1.832, 9.199) | 0.001 | 2.253 (0.868, 5.847) | 0.095 |
| Depression | 4.857 (2.18, 10.82) | < 0.001 | 3.411 (1.405, 8.281) | 0.007 |
Univariate and multivariate logistic regression analyses for the presence of physical frailty as the dependent variable and plasma BNDF value and metabolic parameters as the independent variables. In a multivariate logistic regression model, all factors that were found to be significant in univariate analyses were used. BDNF, brain-derived neurotrophic factor; BMI, body mass index; CI, confidence interval; FPG, fasting plasma glucose; HOMA-IR, homeostasis model assessment-insulin resistance; hs-CRP, high-sensitivity C-reactive protein; OR, odds ratio; SBP, systolic blood pressure; TC, total cholesterol.
Altered circulating BDNF levels are known to be related to metabolic and neuropsychiatric disorders including dementia, depression, stroke, diabetes, CVD, and osteoporosis6–8,10,25. Therefore, sensitivity analyses were performed by excluding participants with these comorbidities (Supplementary Table 1), and consistent results were obtained.ROC analysis was used to assess the sensitivity and specificity of BDNF in predicting frailty (Fig. 2). The optimal cutoff value of BDNF that predicted frailty was ≤ 4.79 ng/ml, with a sensitivity of 50% and a specificity of 80.5% (the area under the curve 0.647, 95% CI 0.590 to 0.701, P = 0.011).
Figure 2.
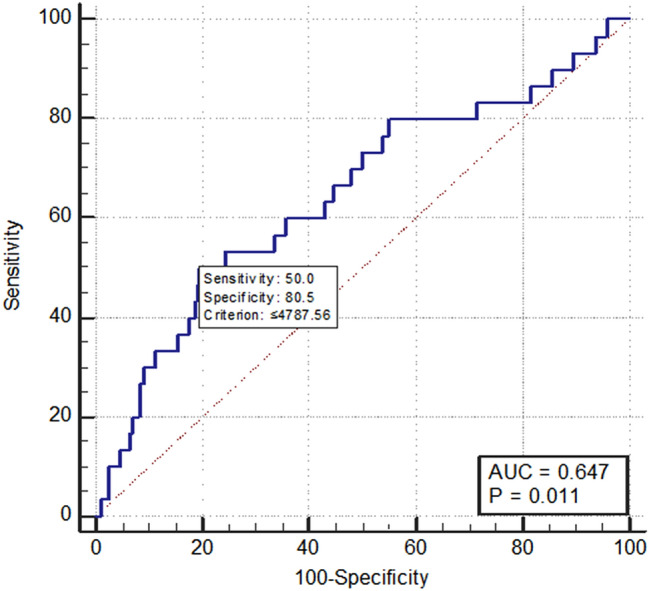
Receiver operating characteristic curves of plasma brain-derived neurotrophic factor levels for estimating frailty.
Discussion
In the present study, plasma BDNF levels were significantly lower in individuals with frailty than in those without among community-dwelling older adults. We also found that plasma BNDF was significantly associated with frailty, regardless of the presence of dementia or depression. Interestingly, the association between plasma BDNF and frailty remained even after exclusion of the effects of dementia, depression, and metabolic disorders, including stroke, diabetes, CVD, and osteoporosis.
BDNF plays a crucial role in the development and functioning of the central nervous system. It is well established that dysfunction of BDNF has been involved in the progression of multiple neurological diseases and psychiatric disorders such as Alzheimer’s disease, stroke, and depression5–8. BDNF interacts with receptor tyrosine kinase TrkB and activates downstream intracellular signaling pathways: mainly the phosphatidylinositol 3-kinase (PI3K)/Akt and the mitogen-activated protein kinase/extracellular-signal-regulated kinase (MAPK/ERK) pathways26, Furthermore, BDNF is an important modulator of inflammation and has an antioxidant effect with enhancing sestrin2 expression through NF-κB-dependent pathway in rat cortical neurons27. Accumulating evidence also suggests that oxidative stress contributes to the dysfunction of BDNF in the pathophysiology of neurodegenerative disorders and psychiatric disorders28. Through the regulation of the activity of certain transcription factors, BNDF promotes neuronal differentiation, survival, and regeneration. Thus, potential therapeutic benefits of BDNF has been studied widely in Alzheimer's disease, stroke, and depression29. Down-regulation of BDNF results in neuronal susceptibility to oxidative stress and dysfunction induced by neurotoxic amyloid-β in Alzheimer’s disease11. Circulating BDNF derives from both central and peripheral sources3,4, because BDNF can cross the blood brain barrier in both directions30. Many investigations have been conducted on the value of blood BDNF as a biomarker of dementia, depression, and stroke5–8. Consistent with previous studies, we confirmed that plasma BDNF was associated with the presence of dementia and depression in this nationwide multicenter study.
BDNF and TrkB signaling in hypothalamus has a role for feeding behavior and energy homeostasis31,32. BDNF heterozygous mice exhibited abnormalities in eating behavior or locomotor activity and developed hyperplasia and obesity in early adulthood33. Additionally, BDNF administration had beneficial effects on glucose metabolism and insulin sensitivity in db/db mice and obese diabetic mice, but these effects of BDNF were not solely dependent on food intake34,35. In humans, individuals with type 2 diabetes showed low circulating levels of BDNF, and low plasma BDNF was associated with the severity of insulin resistance9. In their study, cerebral output of BDNF was abrogated during hyperglycemic clamp conditions, leading to decreased plasma BDNF levels. Another cohort study also showed that low levels of BDNF is an independent risk factor for diabetes and obesity25,36. On the other hand, diabetic patients older than 65 years were more likely to have higher prevalence of frailty than nondiabetic individuals37,38. In the present study, the association between BDNF and frailty persisted even after excluding individuals with diabetes.
Furthermore, BDNF may be a key mediator linking vascular and metabolic benefits of exercise with protection from neurodegenerative diseases11. The sources and mechanisms underlying exercise-induced increases in circulation levels of BDNF has not known well14. BDNF is a contraction-induced muscle cell-derived protein that can increase lipid oxidation in skeletal muscle though AMPK activation15. However, muscle-derived BDNF during physical exercise acts on the muscle in an autocrine and paracrine manner and does not release into circulation15. Platelets are known to take up BDNF from other sources via blood circulation, store it, and release it in response to stimuli such as traumatic muscle injury4. In addition, exercise is capable of increasing BDNF in various brain regions as well as circulating BDNF levels18, partly by induction of FNDC5 and its cleaved and secreted form irisin16. Therefore, it has been proposed that circulating BDNF levels reflect BDNF secreted by the brain in response to exercise39. Recently, it has been reported that lower blood BDNF levels are associated with skeletal muscle strength and physical performance, but not with muscle mass, in patients with heart failure19 and patients with hemodialysis20. Although loss of muscle mass and function in elderly can precede frailty, few studies were conducted on the association between plasma BDNF concentrations and frailty. Plasma BDNF concentrations were lower with frailty determined by Fried Frailty Phenotype and that plasma BNDF levels were normalized by exercise in Brazilian elderly women18. In addition, plasma BDNF levels were associated with frailty defined according to a Japanese version of CHS criteria in Japanese hemodialysis patients20. However, these studies were based on a small number of subjects and specific groups and did not evaluate the influence of cardiometabolic variables as well as the impact of associated chronic disorders, such as dementia, depression, stroke, diabetes, CVD, and osteoporosis. In the present study, we observed that plasm BDNF levels were significantly lower in participants with frailty. Furthermore, the presence of frailty was significantly associated with plasma BDNF levels even after extensive adjustment for confounding factors, including age and neurodegenerative diseases. Since the sensitivity of plasma BDNF in predicting frailty was low in the ROC analysis, it is necessary to use BDNF together with several other risk factors of frailty to increase sensitivity and specificity to increase the usefulness of BDNF as a screening test for frailty. Circulating levels of BDNF has been shown to decline with increasing age24. In sensitivity analyses after excluding dementia, depression, and insulin resistance-related metabolic diseases, which is closely related to BDNF, the association was maintained.
Our study has some limitations. Due to the intrinsic limitations of the cross-sectional study design, we could not determine the existence of a causal relationship between plasma BDNF and frailty. Decline in BDNF levels is accompanied by loss of muscle strength and physical performance caused by a decrease in physical activity and ageing, and as a result, it is thought to contribute to the development of frailty. Given the association between oxidative stress and frailty and the importance of oxidative stress in BDNF dysfunction28,40, interplay between BDNF and oxidative stress may contribute to the pathogenesis of frailty. Further studies are needed on the underlying mechanisms by which BDNF and TkrB signaling play a role in the development of frailty. Another limitation of the present study is that our study was limited to Korean men and women. Thus, it is difficult to apply our study results to different ethnic groups. Nevertheless, this study benefitted from using a nationally representative multicenter sample of community-dwelling elderly Korean adults from KFACS cohort database. Furthermore, multivariate analyses after adjusting for various confounding factors and extensive sensitivity analyses demonstrated consistent results, which may support the robustness of the present findings.
Conclusions
We observed an association between plasma BDNF levels and frailty among community-dwelling older adults in Korea. Plasma BDNF levels were significantly lower in participants with frailty than in those without frailty. We also found a significant association between plasma BNDF levels and frailty, even after excluding participants with BDNF-related metabolic and neuropsychiatric disorders, such as dementia, depression, diabetes, CVD, stroke, and osteoporosis. Therefore, the results of our study may suggest the possible role of BDNF as a novel biomarker of frailty.
Methods
Data source and study population
This study was conducted using data from the Korean Frailty and Aging Cohort Study (KFACS), in which community-dwelling adults aged 70–84 years were recruited from 10 different medical centers nationwide using quota sampling methods stratified by age and sex41. Among 1,455 participants recruited to the KFACS in 2017, a total 717 individuals were included according to the following exclusion criteria: alcohol consumption > 14 drinks per week for men and > 7 drinks per week for women (n = 463), chronic liver diseases, including viral hepatitis and aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels greater than two-fold the upper limit of the normal levels (n = 21), blood creatinine level > 1.5 mg/dL (n = 25), any inflammatory disease with white blood cell count > 10,000/μL (n = 16), any kind of cancer (n = 19), and body composition data using bioelectrical impedance analysis (BIA) instead of dual-energy x-ray absorptiometry (DXA) measurements (n = 194). Of the remaining 717 participants, 317 individuals were randomly selected for the analysis of the plasma BDNF level. The final analysis included 302 participants, after 15 participants with missing data from an on-site interview about medical history and lifestyle factors and laboratory measurement.
Assessment of frailty
Frailty was defined using the Fried Frailty Phenotype, also called Cardiovascular Health Study (CHS) Frailty Phenotype21 with modified cut-offs41, consisting of five components of frailty: unintentional weight loss (4.5 kg in past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity. Detailed information on above five components was described previously41. Grip strength was measured two times for each hand using a digital hand grip dynameter (Takei TKK 5401; Takei Scientific Instruments Co., Tokyo, Japan), and the highest value was used for the analysis. Gait speed was walking speed over 4 m using an automatic timer (Gaitspeedometer; Dynamicphysiology, Daejeon, Korea), with acceleration and deceleration phases of 1.5 m. The level of physical activity (kcal/week) was determined using the International Physical Activity Questionnaire (IPAQ) and metabolic equivalent scores were derived from vigorous, moderate, and mild activities in the questionnaire. Total CHS frailty scores were calculated by assigning a value of 1 to positive responses on each of the above five components (range: 0–5). Participants were considered as frail if the total score was 3–5 and non-frail if the total score was 0–2.
Laboratory measurements
Blood samples were obtained at approximately 8 am after an 8-h fast in each center and transported to the core laboratory (Seegene Inc., Seoul, Korea). After centrifugation, the plasma samples were stored in a deep freezer until analysis. Blood chemistry tests including fasting plasma glucose (FPG), total cholesterol (TC), creatinine, hemoglobin, and high-sensitivity C-reactive protein (hs-CRP) were conducted using a Cobas 8000 C702 analyzer (Roche Diagnostics, Mannheim, Germany) except for plasma insulin. Plasma insulin was analyzed using a Cobas 8000 e602 analyzer (Roche Diagnostics) and HbA1c levels were measured using a Tosoh HLC-723 G8 analyzer (Tosoh Corporation, Tokyo, Japan). Homeostasis model assessment-insulin resistance (HOMA-IR) was calculated using the following formula: fasting plasma glucose (mmol/L) times fasting serum insulin (mU/L) divided by 40542. Plasma BDNF levels were measured using a quantitative sandwich enzyme-linked immunosorbent assay kit (catalog no. BEK-2211; Biosensis, Thebarton, Australia).
Other variables and definitions
During their visit, the participants’ body weight, height, and systolic and diastolic blood pressure (SBP and DBP, respectively) were measured. Body mass index (BMI) was calculated as body weight (kg) divided by height squared in meters (m2). Information on age, sex, smoking status, alcohol consumption, physical activity, income, and medical history (including previous diagnosis of diabetes, hypertension, dyslipidemia, stroke, angina, myocardial infarction and osteoporosis) of the participants was assessed by on-site interviews. Regular drinking was defined as alcohol intake ≥ 2 times/week. Income levels were dichotomized at the lower 20% level. Obesity was defined as BMI ≥ 25 kg/m2. Chronic kidney disease was defined as an estimated glomerular filtration rate < 60 mL/min/1.73 m2 calculated by the Chronic Kidney Disease Epidemiology Collaboration Eq. 43. Diabetes was defined as FPG ≥ 126 mg/dL, HbA1c ≥ 6.5%, or previous diagnosis of diabetes. CVD was defined as a previous diagnosis of both angina and myocardial infarction. Cognitive function was evaluated using the Mini-Mental State Examination (MMSE), and dementia was defined as a MMSE score < 2444. Depression was determined using the Korean version of the Short Form Geriatric Depression Scale with a score of ≥ 645.
Statistical analysis
Data are presented as the means ± standard deviations or median (interquartile range) for continuous variables, and as counts and percentages (%) for categorical variables. Comparisons of baseline characteristics between participants with and without physical frailty were performed using independent two-sample t-test or Mann-Whiney U-test for continuous variables and the χ2 test for categorical variables. Because of the highly skewed distribution in levels of plasma BDNF, the natural log transformation of the data was used for statistical analysis. Univariate and multivariate logistic regression analyses for the presence of physical frailty as the dependent variable and plasma BNDF value, age, sex, BMI, SBP, current smoking, regular drinking, low income, and laboratory data including TC, FPG, HOMA-IR, hs-CRP, hemoglobin, creatinine, and dementia and depression as the independent variables. In a multivariate logistic regression model, all factors that were found to be significant in univariate analyses were used. We also conducted sensitivity analyses to exclude the effects of BDNF-related comorbidities such as dementia, depression, stroke, diabetes, CVD, and osteoporosis. Receiver operating characteristic (ROC) analysis was used to verify the predictive validity of plasma BDNF for estimating frailty. A P–value < 0.05 was considered statistically significant throughout the analysis. All statistical analyses were conducted by an experienced professional statistician using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics
The study was performed according to the 1964 Declaration of Helsinki. The study protocol for the KFACS was approved by the institutional review board of the Korea University Guro Hospital (Approval no. 2020GR0139). Written informed consents were obtained from all participants.
Supplementary Information
Acknowledgements
We are grateful to the study participants and the staff of the Korean Frailty and Aging Cohort Study for their cooperation in this study.
Abbreviations
- BMI
Body mass index
- BDNF
Brain-derived neurotrophic factor
- CHS
Cardiovascular Health Study
- CI
Confidence interval [CI]
- CVD
Cardiovascular disease
- HOMA-IR
Homeostasis model assessment-insulin resistance
- hs-CRP
High-sensitivity C-reactive protein
- KFACS
Korean Frailty and Aging Cohort Study
- OR
Odds ratio
Author contributions
E.R., M.K., C.W.W., and K.M.C. conceived and designed the study. E.R., E.S., M.J.P., M.K., C.W.W., and K.M.C. contributed to the data acquisition. E.R., S.Y.H., and K.M.C. contributed to the statistical analyses. E.R., H.J.Y., S.H.B., C.W.W. and K.M.C. contributed to the data interpretation. E.R., C.W.W., and K.M.C. wrote the manuscript. All authors have approved the submitted manuscript.
Funding
This research was supported by a grant from the Korea Health Technology R & D Project through the Korean Health Industry Development Institute (KHIDI), which is funded by the Ministry of Health &; Welfare, Republic of Korea (Grant number: HI15C3153), and the Research Program funded by the National Institute of Health, Korea Disease Control and Prevention Agency (2021-ER0605-00). This work was also supported by Korea University Guro Hospital (Korea Research-Driven Hospital) and grant funded by Korea University Medicine (K2210431) and a grant from the National Research Foundation of Korea (NRF) funded by the Ministry of Education of Korea (Grant number: 2020R1I1A1A01070499). The funders had no role in the study's design, collection, analysis, or interpretation of the data or the preparation, review, or approval of the manuscript.
Data availability
The data used to support the findings of this study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Chang Won Won and Kyung Mook Choi.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-19706-3.
References
- 1.Huang EJ, Reichardt LF. Neurotrophins: Roles in neuronal development and function. Annu. Rev. Neurosci. 2001;24:677–736. doi: 10.1146/annurev.neuro.24.1.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lommatzsch M, et al. The impact of age, weight and gender on BDNF levels in human platelets and plasma. Neurobiol. Aging. 2005;26:115–123. doi: 10.1016/j.neurobiolaging.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Nakahashi T, et al. Vascular endothelial cells synthesize and secrete brain-derived neurotrophic factor. FEBS Lett. 2000;470:113–117. doi: 10.1016/s0014-5793(00)01302-8. [DOI] [PubMed] [Google Scholar]
- 4.Fujimura H, et al. Brain-derived neurotrophic factor is stored in human platelets and released by agonist stimulation. Thromb. Haemost. 2002;87:728–734. [PubMed] [Google Scholar]
- 5.Song JH, Yu JT, Tan L. Brain-derived neurotrophic factor in alzheimer's disease: Risk, mechanisms, and therapy. Mol. Neurobiol. 2015;52:1477–1493. doi: 10.1007/s12035-014-8958-4. [DOI] [PubMed] [Google Scholar]
- 6.Dell'Osso L, et al. Associations between brain-derived neurotrophic factor plasma levels and severity of the illness, recurrence and symptoms in depressed patients. Neuropsychobiology. 2010;62:207–212. doi: 10.1159/000319946. [DOI] [PubMed] [Google Scholar]
- 7.Pikula A, et al. Serum brain-derived neurotrophic factor and vascular endothelial growth factor levels are associated with risk of stroke and vascular brain injury: Framingham Study. Stroke. 2013;44:2768–2775. doi: 10.1161/STROKEAHA.113.001447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stanne TM, et al. Low circulating acute brain-derived neurotrophic factor levels are associated with poor long-term functional outcome after ischemic stroke. Stroke. 2016;47:1943–1945. doi: 10.1161/STROKEAHA.115.012383. [DOI] [PubMed] [Google Scholar]
- 9.Krabbe KS, et al. Brain-derived neurotrophic factor (BDNF) and type 2 diabetes. Diabetologia. 2007;50:431–438. doi: 10.1007/s00125-006-0537-4. [DOI] [PubMed] [Google Scholar]
- 10.Nose S, et al. Serum brain-derived neurotrophic factor levels mirror bone mineral density in amenorrheic and eumenorrheic athletes. Int. J. Sports Med. 2019;40:276–282. doi: 10.1055/a-0835-6119. [DOI] [PubMed] [Google Scholar]
- 11.Wang R, Holsinger RMD. Exercise-induced brain-derived neurotrophic factor expression: Therapeutic implications for Alzheimer's dementia. Ageing Res. Rev. 2018;48:109–121. doi: 10.1016/j.arr.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Demurtas J, et al. Physical activity and exercise in mild cognitive impairment and dementia: An umbrella review of intervention and observational studies. J. Am. Med. Dir. Assoc. 2020;21:1415–1422.e1416. doi: 10.1016/j.jamda.2020.08.031. [DOI] [PubMed] [Google Scholar]
- 13.Jung I, et al. Changes in patterns of physical activity and risk of heart failure in newly diagnosed diabetes mellitus patients. Diabetes Metab. J. 2022;46:327–336. doi: 10.4093/dmj.2021.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh JJ, Tschakovsky ME. Exercise and circulating BDNF: Mechanisms of release and implications for the design of exercise interventions. Appl. Physiol. Nutr. Metab. 2018;43:1095–1104. doi: 10.1139/apnm-2018-0192. [DOI] [PubMed] [Google Scholar]
- 15.Matthews VB, et al. Brain-derived neurotrophic factor is produced by skeletal muscle cells in response to contraction and enhances fat oxidation via activation of AMP-activated protein kinase. Diabetologia. 2009;52:1409–1418. doi: 10.1007/s00125-009-1364-1. [DOI] [PubMed] [Google Scholar]
- 16.Wrann CD, et al. Exercise induces hippocampal BDNF through a PGC-1alpha/FNDC5 pathway. Cell Metab. 2013;18:649–659. doi: 10.1016/j.cmet.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wood J, et al. BDNF mimetic alleviates body weight gain in obese mice by enhancing mitochondrial biogenesis in skeletal muscle. Metabolism. 2018;87:113–122. doi: 10.1016/j.metabol.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Coelho FM, et al. Physical therapy intervention (PTI) increases plasma brain-derived neurotrophic factor (BDNF) levels in non-frail and pre-frail elderly women. Arch. Gerontol. Geriatr. 2012;54:415–420. doi: 10.1016/j.archger.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Nakano I, et al. Serum brain-derived neurotrophic factor levels are associated with skeletal muscle function but not with muscle mass in patients with heart failure. Int. Heart J. 2020;61:96–102. doi: 10.1536/ihj.19-400. [DOI] [PubMed] [Google Scholar]
- 20.Miyazaki S, Iino N, Koda R, Narita I, Kaneko Y. Brain-derived neurotrophic factor is associated with sarcopenia and frailty in Japanese hemodialysis patients. Geriatr. Gerontol. Int. 2021;21:27–33. doi: 10.1111/ggi.14089. [DOI] [PubMed] [Google Scholar]
- 21.Fried LP, et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001;56:M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 22.Cawthon PM, et al. Frailty in older men: Prevalence, progression, and relationship with mortality. J. Am. Geriatr. Soc. 2007;55:1216–1223. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- 23.Afilalo J, et al. Frailty assessment in the cardiovascular care of older adults. J. Am. Coll. Cardiol. 2014;63:747–762. doi: 10.1016/j.jacc.2013.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kane AE, Sinclair DA. Frailty biomarkers in humans and rodents: Current approaches and future advances. Mech. Ageing Dev. 2019;180:117–128. doi: 10.1016/j.mad.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li B, Lang N, Cheng ZF. Serum levels of brain-derived neurotrophic factor are associated with diabetes risk, complications, and obesity: A cohort study from Chinese patients with type 2 diabetes. Mol. Neurobiol. 2016;53:5492–5499. doi: 10.1007/s12035-015-9461-2. [DOI] [PubMed] [Google Scholar]
- 26.Zhao H, et al. Molecular mechanisms of brain-derived neurotrophic factor in neuro-protection: Recent developments. Brain Res. 2017;1665:1–21. doi: 10.1016/j.brainres.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 27.Wu CL, Chen SD, Yin JH, Hwang CS, Yang DI. Nuclear factor-kappaB-dependent Sestrin2 induction mediates the antioxidant effects of BDNF against mitochondrial inhibition in rat cortical neurons. Mol. Neurobiol. 2016;53:4126–4142. doi: 10.1007/s12035-015-9357-1. [DOI] [PubMed] [Google Scholar]
- 28.Zhang XY, et al. The interplay between BDNF and oxidative stress in chronic schizophrenia. Psychoneuroendocrinology. 2015;51:201–208. doi: 10.1016/j.psyneuen.2014.09.029. [DOI] [PubMed] [Google Scholar]
- 29.Nagahara AH, Tuszynski MH. Potential therapeutic uses of BDNF in neurological and psychiatric disorders. Nat. Rev. Drug Discov. 2011;10:209–219. doi: 10.1038/nrd3366. [DOI] [PubMed] [Google Scholar]
- 30.Pan W, Banks WA, Fasold MB, Bluth J, Kastin AJ. Transport of brain-derived neurotrophic factor across the blood-brain barrier. Neuropharmacology. 1998;37:1553–1561. doi: 10.1016/s0028-3908(98)00141-5. [DOI] [PubMed] [Google Scholar]
- 31.Rios M. BDNF and the central control of feeding: Accidental bystander or essential player? Trends Neurosci. 2013;36:83–90. doi: 10.1016/j.tins.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu JH, Kim MS. Molecular mechanisms of appetite regulation. Diabetes Metab. J. 2012;36:391–398. doi: 10.4093/dmj.2012.36.6.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kernie SG, Liebl DJ, Parada LF. BDNF regulates eating behavior and locomotor activity in mice. EMBO J. 2000;19:1290–1300. doi: 10.1093/emboj/19.6.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tonra JR, et al. Brain-derived neurotrophic factor improves blood glucose control and alleviates fasting hyperglycemia in C57BLKS-Lepr(db)/lepr(db) mice. Diabetes. 1999;48:588–594. doi: 10.2337/diabetes.48.3.588. [DOI] [PubMed] [Google Scholar]
- 35.Nakagawa T, et al. Brain-derived neurotrophic factor regulates glucose metabolism by modulating energy balance in diabetic mice. Diabetes. 2000;49:436–444. doi: 10.2337/diabetes.49.3.436. [DOI] [PubMed] [Google Scholar]
- 36.El-Gharbawy AH, et al. Serum brain-derived neurotrophic factor concentrations in lean and overweight children and adolescents. J. Clin. Endocrinol. Metab. 2006;91:3548–3552. doi: 10.1210/jc.2006-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoon JW, et al. Hyperglycemia is associated with impaired muscle quality in older men with diabetes: The Korean longitudinal study on health and aging. Diabetes Metab. J. 2016;40:140–146. doi: 10.4093/dmj.2016.40.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peng P, et al. Association between HOMA-IR and frailty among U.S. middle-aged and elderly population. Sci. Rep. 2019;9:4238. doi: 10.1038/s41598-019-40902-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rasmussen P, et al. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp. Physiol. 2009;94:1062–1069. doi: 10.1113/expphysiol.2009.048512. [DOI] [PubMed] [Google Scholar]
- 40.Inglés M, et al. Oxidative stress is related to frailty, not to age or sex, in a geriatric population: Lipid and protein oxidation as biomarkers of frailty. J. Am. Geriatr. Soc. 2014;62:1324–1328. doi: 10.1111/jgs.12876. [DOI] [PubMed] [Google Scholar]
- 41.Won CW, et al. Korean Frailty and Aging Cohort Study (KFACS): Cohort profile. BMJ Open. 2020;10:e035573. doi: 10.1136/bmjopen-2019-035573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews DR, et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 43.Drawz P, Rahman M. Chronic kidney disease. Annals Intern. Med. 2015;162:1–16. doi: 10.7326/AITC201506020. [DOI] [PubMed] [Google Scholar]
- 44.O'Donnell M, et al. Cognitive impairment and risk of cardiovascular events and mortality. Eur. Heart J. 2012;33:1777–1786. doi: 10.1093/eurheartj/ehs053. [DOI] [PubMed] [Google Scholar]
- 45.Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J. Psychosom. Res. 2004;57:297–305. doi: 10.1016/j.jpsychores.2004.01.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author on reasonable request.



