Abstract
Introduction
A recent phase 3, randomized, placebo- and tramadol-controlled trial (56-week treatment/24-week safety follow-up) demonstrated efficacy of tanezumab 10 mg in patients with chronic low back pain (CLBP) and a history of inadequate response to standard-of-care analgesics. Here, we report on the clinical meaningfulness of treatment response in this study, focused on secondary measures of pain, interference with daily functions, overall disease status, and satisfaction with treatment.
Methods
Patients received placebo (up to week 16; n = 406), subcutaneously administered (SC) tanezumab 5 mg (every 8 weeks; n = 407), SC tanezumab 10 mg (every 8 weeks; n = 407), or orally administered tramadol prolonged-release (100–300 mg/day; n = 605) for 56 weeks. Patient’s global assessment of low back pain (PGA-LBP), Brief Pain Inventory-short form (BPI-sf), Treatment Satisfaction Questionnaire for Medication (TSQM), and modified Patient-Reported Treatment Impact (mPRTI) were assessed at weeks 16 and 56.
Results
At week 16, significant (p < 0.05) improvements over placebo were evident with tanezumab for the PGA-LBP (10 mg) and most BPI-sf (both doses), TSQM (both doses), and mPRTI (both doses) items assessed. Improvements over baseline persisted for the PGA-LBP and BPI-sf at week 56. However, the magnitude of improvements was modestly lower at week 56 relative to week 16. Tramadol did not improve PGA-LBP or BPI-sf scores versus placebo at week 16. Most differences between tanezumab and tramadol at week 56 did not reach the level of statistical significance for all endpoints.
Conclusions
The totality of the evidence as captured by measures of pain, interference with daily function, patient overall assessment of disease status, and satisfaction with treatment demonstrates the clinically meaningful benefit of tanezumab for some patients with CLBP compared with placebo.
ClinicalTrials.gov: NCT02528253.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40122-022-00424-7.
Keywords: Chronic low back pain, Nerve growth factor, Function, Pain, Tanezumab, Tramadol
Key Summary Points
| Why carry out this study? |
| Chronic low back pain is one of the most common causes of long-term disability and there is a need for novel agents that provide meaningful symptomatic improvement. |
| We report on the clinical meaningfulness of treatment response (based on secondary measures of pain, interference with daily functions, overall disease status, and satisfaction with treatment) in a recently completed, long-term, phase 3, randomized, and tramadol-controlled trial of subcutaneously administered tanezumab (5 mg and 10 mg) in patients with chronic low back pain and a history of inadequate response to standard-of-care analgesics. |
| What was learned from the study? |
| Tanezumab provided significant improvement in overall disease status, pain and interference with daily function, treatment satisfaction, and treatment preference compared to placebo at week 16. Tramadol did not improve disease status, pain, or daily function scores versus placebo at week 16. |
| Improvements (over baseline) in disease status, pain, and daily function persisted at week 56 but the magnitude of improvement was modestly lower than at week 16 and, across all endpoints, most differences between tanezumab and tramadol did not reach the level of statistical significance at week 56. |
| Measures of pain, interference with daily function, overall assessment of disease status, and satisfaction with treatment demonstrate that tanezumab is capable of providing clinically meaningful benefit to some patients with chronic low back pain. |
Introduction
Globally, chronic low back pain (CLBP) is one of the five most common causes of long-term disability [1–4]. A multidisciplinary approach (including core muscle exercises, physiotherapy, cognitive behavioral therapy, and pharmacologic analgesics) is recommended to improve both pain and function in patients with CLBP [5]. Among pharmacologic therapies, non-steroidal anti-inflammatory drugs (NSAIDs) are recommended as first-line treatment, with tramadol or duloxetine as second-line treatments [6].
While these drugs provide varying levels of pain relief in patients with CLBP, long-term efficacy data is sparse and their use in this population is limited by minimal (NSAIDs and duloxetine) or questionable (opioids) benefits on function [6–9]. An emphasis on pain reduction as the primary measure of treatment success, rather than a diverse group of assessments that capture the global effects of chronic pain on the lives of patients, may have contributed to broad overreliance on the use of opioids for CLBP [7]. Clinical assessments narrowly based on pain intensity fail to account for the deterioration in physical function, loss of mobility, inability to perform everyday activities, loss of independence, limitations on social interaction, increased absenteeism, and loss of productivity associated with CLBP [10–12]. Thus, there is a need for novel agents that provide meaningful improvements in symptoms beyond pain intensity, such as interference with daily function.
Nerve growth factor (NGF) plays an important role in the modulation and sensitization of nociceptors and a growing body of evidence demonstrates that NGF-mediated sensitization (peripheral and central) contributes to the hyperalgesia that is characteristic of many chronic pain states including CLBP [13–15]. Thus, NGF has become an attractive therapeutic target in the context of CLBP and anti-NGF medicines are currently in clinical development. One such medicine is tanezumab, a humanized IgG type 2 monoclonal antibody that sequesters NGF and disrupts NGF-mediated signaling pathways [15].
An 80-week (56-week treatment/24-week safety follow-up), randomized, double-blind, placebo- and tramadol-controlled phase 3 study of subcutaneously administered (SC) tanezumab (5 mg and 10 mg) in patients with CLBP, which is among the longest and largest randomized controlled trials of an analgesic for CLBP conducted to date, was recently completed and primary findings have been published [16]. Tanezumab 10 mg met the primary pain endpoint (based on low back pain intensity [LBPI] score) and all key secondary pain and physical function (based on Roland Morris Disability Questionnaire [(RMDQ] score) endpoints [16]. Tanezumab 5 mg did not meet the primary pain endpoint, which prevented formal analysis of the key secondary endpoints for this dose per the predefined testing strategy [16].
Here, we focus on the clinical meaningfulness of response to tanezumab and to tramadol in this recently completed trial through assessment of secondary measures of pain, interference with daily functions, global disease status, and treatment satisfaction.
Methods
Data were derived from a phase 3, randomized, double-blind, placebo- and tramadol-controlled trial investigating the efficacy and safety of SC tanezumab (ClinicalTrials.gov, NCT02528253) [16]. The study protocol was approved by an institutional review board or independent ethics committee for each participating investigational center and all patients provided written informed consent. This study was conducted in compliance with ethical principles of the Declaration of Helsinki and Good Clinical Practice Guidelines.
Patients
Patients aged 18 years or more with axial predominant CLBP (primary location between the 12th thoracic vertebra and lower gluteal folds, with or without radiation into the posterior thigh) of at least 3 months’ duration were eligible. Key inclusion criteria included a low back pain intensity (LBPI) score of at least 5 (on an 11-point numeric rating scale), a patient’s global assessment of low back pain (PGA-LBP) score of “fair,” “poor,” or “very poor” (on a 5-point scale from “very good” to “very poor”), and a history of inadequate response (insufficient pain relief at maximum tolerated dose or intolerance/contraindication) to at least three different categories of standard-of-care analgesics (predominantly acetaminophen, NSAIDs, and opioids). Full details of inclusion and exclusion criteria have been published previously [16].
Treatment
A full description of the trial design has been published previously [16]. Briefly, the study included a 56-week double-blind treatment period and a 24-week safety follow-up period. Patients were randomized in a 1:1:2:2:3 ratio to receive placebo/SC tanezumab 5 mg (switch from placebo to tanezumab at week 16), placebo/SC tanezumab 10 mg (switch from placebo to tanezumab at week 16), SC tanezumab 5 mg, SC tanezumab 10 mg, or orally administered tramadol prolonged-release (once daily with titration [up or down depending on pain relief and tolerability] from 100 to 300 mg/day over the first 4 weeks of treatment). SC tanezumab was administered every 8 weeks.
To limit exposure in patients who did not respond adequately to treatment, patients were discontinued from the study at week 16 (prior to the third SC dose) if they did not have at least a 30% reduction from baseline in average LBPI at week 16 and at least a 15% reduction from baseline in average LBPI at any week from weeks 1 to 15. Patients were also discontinued at week 32 (prior to the fifth SC dose) if they did not have at least a 30% reduction from baseline in average LBPI.
During the 56-week treatment period, rescue medication in the form of acetaminophen/paracetamol (maximum dose of 3000 mg/day) was allowed up to 3 days per week through week 16 and then daily after week 16. Likewise, adjunctive analgesics such as pregabalin, gabapentin, skeletal muscle relaxants, benzodiazepines, sedative/hypnotics, anxiolytics, antidepressants (except monoamine oxidase inhibitors), and topical analgesics were allowed after week 16. NSAIDs and opioids were prohibited throughout the full treatment period. Pre-existing, stable, non-pharmacologic treatment regimens were allowed for the first 16 weeks of study treatment, and new regimens could be initiated after week 16.
Assessments
Patient’s overall assessment of disease status was assessed using the self-administered patient global assessment of low back pain questionnaire, with scores ranging from 1 (“very good”) to 5 (“very poor”). The PGA-LBP was administered at baseline and at weeks 2, 4, 8, 16, 24, 32, 40, 48, 56, and 64. This manuscript reports mean change in PGA-LBP from baseline at week 16 (end of placebo-controlled treatment) and week 56 (end of overall treatment).
Pain severity and impact on daily functions over the past 24 h were assessed using the self-administered Brief Pain Inventory-short form (BPI-sf) questionnaire. Data on worst pain, average pain, and pain interference were assessed in this study. Scores for individual questions ranged from 0 to 10, with higher scores indicating greater pain severity or pain interference. An overall pain interference index (range, 0–10) is based on seven pain interference questions relating to physical and social functioning. The BPI-sf was administered at baseline and at weeks 2, 4, 8, 16, 24, 32, 40, 48, 56, and 64. This manuscript reports mean change in BPI-sf scores (worst pain, average pain, and the overall interference index) from baseline at week 16 (end of placebo-controlled treatment) and week 56 (end of overall treatment).
Patient satisfaction with study medication was assessed at weeks 16 and 56 using the self-administered 11-item Treatment Satisfaction Questionnaire for Medication (TSQM). Most TSQM items are scored on a 7-point Likert scale, with higher scores indicating greater satisfaction. The 11 individual items are used to calculate four endpoints of “effectiveness,” “side effects,” “convenience,” and “global satisfaction,” which are scored from 0 to 100 with a higher score indicating greater satisfaction.
Treatment preference and willingness to use study treatment were assessed at weeks 16 and 56 using the self-administered 4-item modified Patient Reported Treatment Impact (mPRTI) questionnaire. Data on three of the four items were collected in this study including types of treatments used prior to study enrollment, patient preference of study treatment relative to previous treatments, and patient willingness to use study treatment in the future. Preference and willingness questions were scored using a 5-point Likert scale, with lower scores indicating greater preference or willingness for study medication.
Rescue medication use was recorded, using an electronic diary, daily up to week 16 and then weekly from weeks 16 to 80. The incidence and number of days of rescue use were assessed at weeks 2, 4, 8, 12, 16, 24, 32, 40, 48, 56, and 64, while the amount of rescue medication taken was assessed at weeks 2, 4, 8, 12, and 16. This manuscript reports incidence, number of days, and amount of rescue medication data at week 16 (end of placebo-controlled treatment) and incidence and number of days of rescue medication data at week 56 (end of overall treatment).
Statistical Analysis
Changes from baseline in PGA-LBP and BPI-sf score were compared between treatment groups using an analysis of covariance model with baseline score and baseline average LBPI score as covariates, treatment as a fixed effect, study site as a random variable, and a multiple imputation approach to missing data.
TSQM and mPRTI responses were compared between treatment groups via analysis of covariance and a Cochran–Mantel–Haenszel test using observed data (i.e., no imputation for missing data), respectively. Incidence of rescue medication use was compared between treatment groups using a logistic regression analysis. Mean number of days of rescue medication use and amount of rescue medication used were compared between groups using a negative binomial model with terms for baseline average LBPI score and treatment group. Missing data were imputed using a last-observation-carried-forward approach.
For all comparisons, significance was declared if the 2-tailed test for the difference between treatment groups was significant at the 0.05 level. All comparisons were unadjusted for multiplicity. Patient disposition values and all efficacy analyses were based on the efficacy population, which included all patients who received at least one dose of study treatment grouped according to assigned treatment (i.e., the intent-to-treat population). See primary publication for more detail [16].
Results
Patients
Overall, 1825 patients received at least one dose of study treatment (placebo, 406; tanezumab 5 mg, 407; tanezumab 10 mg, 407; tramadol, 605). Of these patients, 77.8% completed treatment up to week 16 (placebo, 78.6%; tanezumab 5 mg, 77.6%; tanezumab 10 mg, 83.0%; tramadol, 73.9%). Across all groups, 53.6% of treated patients met efficacy criteria to remain in the study (see “Methods” for details) and received study treatment at week 16 (placebo/tanezumab 5 mg, 49.0%; placebo/tanezumab 10 mg, 46.6%; tanezumab 5 mg, 58.0%; tanezumab 10 mg, 59.5%; tramadol, 50.7%). Overall, 34.6% of treated patients completed the 56-week treatment phase (placebo/tanezumab 5 mg, 30.7%; placebo/tanezumab 10 mg, 31.4%; tanezumab 5 mg, 34.4%; tanezumab 10 mg, 39.1%; tramadol, 34.0%). “Patient meets protocol-specified pain criteria for discontinuation” and “insufficient clinical response” were among the most common reasons for discontinuation during the 56-week treatment phase (both reasons combined: placebo/tanezumab 5 mg, 32.2%; placebo/tanezumab 10 mg, 39.7%; tanezumab 5 mg, 27.5%; tanezumab 10 mg, 27.3%; tramadol, 26.8%). Please see the primary publication for a more detailed overview of patient disposition during the trial and reasons for treatment discontinuation. The mean dose of tramadol in the tramadol treatment arm was 203 mg at week 16 and 209 mg at week 56.
Baseline demographics and baseline characteristics were similar across groups. The overall population was largely female (57.0%), white (72.4%), had an approximate mean age of 49 years, and had mean baseline LBPI and RMDQ scores of approximately 7.2 and 15.0, respectively. A majority of patients had a painDETECT score of 12 or lower at baseline, indicating that a neuropathic component to their CLBP was unlikely (Fig. 1). The proportion of patients with a score of 19 or higher (indicating a neuropathic component was likely) was low; placebo, 15.5%; tanezumab 5 mg, 13.0%; tanezumab 10 mg, 8.6%; and tramadol, 13.1%. Prior CLBP treatments were similar across all treatment groups, with ranges of 90.5–92.9% for acetaminophen or low-dose NSAIDs, 81.9–87.6% for prescription NSAIDs, and 67.9–73.5% for opioids.
Fig. 1.
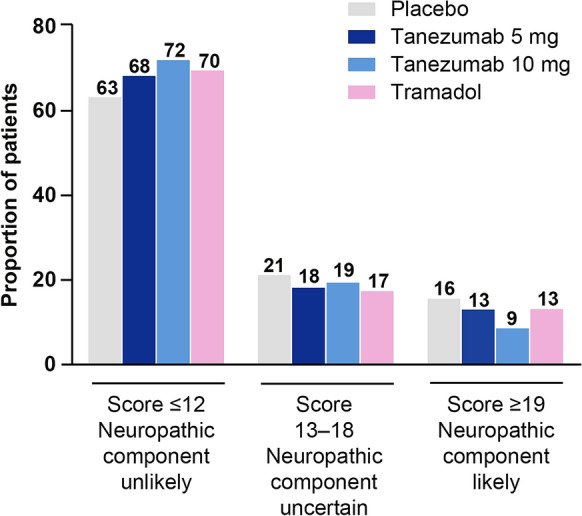
Baseline painDETECT categories. PainDETECT is a 9-item questionnaire used to identify neuropathic pain components in patients with chronic pain [35]. Total scores range from − 1 to 38. A score of 12 or lower indicates that pain is unlikely to have a neuropathic component, while a score of 19 or higher suggests that pain is likely to have a neuropathic component
Efficacy at Week 16
PGA-LBP
Compared with placebo, changes in PGA-LBP score at week 16 were significantly greater in the tanezumab 10 mg group but not in the tanezumab 5 mg or tramadol groups; LS mean difference from placebo was − 0.12 for tanezumab 5 mg, − 0.16 for tanezumab 10 mg, and 0.01 for tramadol (Table 1). Both tanezumab groups, however, exhibited significant improvements over tramadol; LS mean difference from tramadol was − 0.13 for tanezumab 5 mg and − 0.17 for tanezumab 10 mg.
Table 1.
Change from baseline in PGA-LBP scores at week 16 and week 56
| Placebo (N = 406) | Tanezumab 5 mg (N = 407) | Tanezumab 10 mg (N = 407) | Tramadol (N = 605) | |
|---|---|---|---|---|
| Week 16 PGA-LBP | ||||
| Mean (SD) score at baselinea | 3.48 (0.62) | 3.47 (0.61) | 3.53 (0.63) | 3.50 (0.63) |
| LS mean (SE) change from baseline | − 0.86 (0.05) | − 0.98 (0.05) | − 1.02 (0.05) | − 0.85 (0.04) |
| LS mean (SE) difference vs placebo | – | − 0.12 (0.07) | − 0.16 (0.07) | 0.01 (0.06) |
| p value vs placebo | – | 0.0717 | 0.0207 | 0.8399 |
| LS mean (SE) difference vs tramadol | – | − 0.13 (0.06) | − 0.17 (0.06) | – |
| p value vs tramadol | – | 0.0299 | 0.0060 | – |
| Week 56 PGA-LBP | ||||
| LS mean (SE) change from baseline | – | − 0.76 (0.06) | − 0.74 (0.07) | − 0.66 (0.06) |
| LS mean (SE) difference vs tramadol | – | − 0.10 (0.08) | − 0.07 (0.08) | – |
| p value vs tramadol | – | 0.2346 | 0.3634 | – |
PGA-LBP scores range from 1 to 5; negative values represent an improvement in pain, disability, and disease status, respectively
LS least-squares, PGA-LBP patient global assessment of low back pain, SD standard deviation, SE standard error
aBaseline n is 406, 405, 407, and 605 for placebo, tanezumab 5 mg, tanezumab 10 mg, and tramadol, respectively
BPI-sf
Improvements in BPI-sf “worst pain” score at week 16 were significantly greater in both tanezumab groups, but not the tramadol group, compared with the placebo group; LS mean difference versus placebo was − 0.52 for tanezumab 5 mg, − 0.54 for tanezumab 10 mg, and − 0.24 for tramadol (Table 2). Similar results were observed for “average pain”; LS mean difference versus placebo was − 0.37 for tanezumab 5 mg, − 0.46 for tanezumab 10 mg, and − 0.17 for tramadol. No significant differences were observed between the tanezumab and tramadol groups for “worst pain” or “average pain.” Improvements in the BPI-sf pain interference index were significantly greater in both tanezumab groups, but not the tramadol group, compared to the placebo group; LS mean difference versus placebo was − 0.41 for tanezumab 5 mg, − 0.58 for tanezumab 10 mg, and − 0.15 for tramadol. LS mean differences versus tramadol were significantly greater for tanezumab 10 mg (− 0.43) but not for tanezumab 5 mg (− 0.26).
Table 2.
Change from baseline in Brief Pain Inventory-short form (BPI-sf) scores at week 16 and week 56
| Placebo (N = 406) | Tanezumab 5 mg (N = 407) | Tanezumab 10 mg (N = 407) | Tramadol (N = 605) | |
|---|---|---|---|---|
| Week 16 worst pain | ||||
| Mean (SD) score at baselinea | 7.92 (1.14) | 7.95 (1.11) | 7.92 (1.19) | 7.92 (1.18) |
| LS mean (SE) change | − 2.67 (0.15) | − 3.18 (0.14) | − 3.21 (0.14) | − 2.90 (0.12) |
| LS mean (SE) difference vs placebo | – | − 0.52 (0.19) | − 0.54 (0.19) | − 0.24 (0.17) |
| p value vs placebo | – | 0.0058 | 0.0038 | 0.1707 |
| LS mean (SE) difference vs tramadol | – | − 0.28 (0.17) | − 0.31 (0.17) | – |
| p value vs tramadol | – | 0.1083 | 0.0734 | – |
| Week 16 average pain | ||||
| Mean (SD) score at baselinea | 6.95 (1.17) | 7.00 (1.18) | 6.88 (1.21) | 6.97 (1.21) |
| LS mean (SE) change | − 2.47 (0.14) | − 2.84 (0.14) | − 2.93 (0.14) | − 2.64 (0.12) |
| LS mean (SE) difference vs placebo | – | − 0.37 (0.18) | − 0.46 (0.18) | − 0.17 (0.16) |
| p value vs placebo | – | 0.0365 | 0.0092 | 0.2923 |
| LS mean (SE) difference vs tramadol | – | − 0.20 (0.16) | − 0.29 (0.16) | – |
| p value vs tramadol | – | 0.2231 | 0.0724 | – |
| Week 16 Pain Interference Indexb | ||||
| Mean (SD) score at baselinea | 6.03 (1.89) | 6.28 (1.81) | 6.16 (1.93) | 6.21 (1.88) |
| LS mean (SE) change | − 2.65 (0.14) | − 3.06 (0.14) | − 3.23 (0.14) | − 2.80 (0.12) |
| LS mean (SE) difference vs placebo | – | − 0.41 (0.18) | − 0.58 (0.18) | − 0.15 (0.17) |
| p value vs placebo | – | 0.0270 | 0.0019 | 0.3906 |
| LS mean (SE) difference vs tramadol | – | − 0.26 (0.17) | − 0.43 (0.17) | – |
| p value vs tramadol | – | 0.1209 | 0.0107 | – |
| Week 56 worst pain | ||||
| LS mean (SE) change | – | − 2.66 (0.19) | − 2.74 (0.18) | − 2.45 (0.15) |
| LS mean (SE) difference vs tramadol | – | − 0.21 (0.22) | − 0.29 (0.22) | – |
| p value vs tramadol | – | 0.3438 | 0.1876 | – |
| Week 56 average pain | ||||
| LS mean (SE) change | – | − 2.32 (0.17) | − 2.51 (0.17) | − 2.29 (0.14) |
| LS mean (SE) difference vs tramadol | – | − 0.03 (0.20) | − 0.22 (0.20) | – |
| p value vs tramadol | – | 0.8752 | 0.2663 | – |
| Week 56 overall pain interference indexb | ||||
| LS mean (SE) change | – | − 2.32 (0.17) | − 2.44 (0.17) | − 2.21 (0.15) |
| LS mean (SE) difference vs tramadol | – | − 0.11 (0.20) | − 0.23 (0.20) | – |
| p value vs tramadol | – | 0.5818 | 0.2562 | – |
Scores for all items range from 0 to 10; negative values indicate improvement in pain or pain interference
LS least-squares, SD standard deviation, SE standard error
aBaseline n is 406, 405, 407, and 605 for placebo, tanezumab 5 mg, tanezumab 10 mg, and tramadol, respectively
bSeven individual items relating to physical and social functioning contribute to calculation of the overall pain interference index
TSQM
Both tanezumab groups demonstrated improvement over placebo for most TSQM endpoints at week 16 (Table 3). LS mean “effectiveness” scores were significantly better in the tanezumab 5 mg (63.69), tanezumab 10 mg (62.87), and tramadol (61.39) groups compared with the placebo (56.67) group; no significant difference was observed between the tanezumab and tramadol groups. LS mean “side effect” scores were also significantly better in both tanezumab groups (5 mg, 79.26; 10 mg, 79.51) compared with the placebo (66.95) and tramadol (70.83) groups. LS mean “convenience” scores were significantly better in the tanezumab 10 mg (76.37) group, but not the tanezumab 5 mg (75.68) and tramadol (74.63) groups, compared with the placebo (73.11) group; no significant difference was observed between the tanezumab and tramadol groups. Finally, LS mean “global satisfaction” scores were significantly better in both tanezumab groups (5 mg, 70.32; 10 mg, 68.64), but not the tramadol (67.12) group, compared with the placebo (64.90) group; no significant difference was observed between the tanezumab and tramadol groups.
Table 3.
Treatment Satisfaction Questionnaire for Medication (TSQM) scores at week 16 and week 56
| Placebo (N = 406) | Tanezumab 5 mg (N = 407) | Tanezumab 10 mg (N = 407) | Tramadol (N = 605) | |
|---|---|---|---|---|
| Week 16 effectiveness domain | ||||
| LS mean (SE) score | 56.67 (1.50) | 63.69 (1.48) | 62.87 (1.48) | 61.39 (1.30) |
| LS mean (SE) difference vs placebo | – | 7.02 (2.01) | 6.21 (2.01) | 4.72 (1.89) |
| p value vs placebo | – | 0.0005 | 0.0021 | 0.0125 |
| LS mean (SE) difference vs tramadol | – | 2.31 (1.87) | 1.49 (1.86) | – |
| p value vs tramadol | – | 0.2176 | 0.4235 | – |
| Week 16 side effects domain | ||||
| LS mean (SE) score | 66.95 (3.76) | 79.26 (3.31) | 79.51 (3.31) | 70.83 (2.15) |
| LS mean (SE) difference vs placebo | – | 12.30 (4.96) | 12.55 (4.96) | 3.88 (4.29) |
| p value vs placebo | – | 0.0143 | 0.0124 | 0.3675 |
| LS mean (SE) difference vs tramadol | – | 8.42 (3.89) | 8.67 (3.90) | – |
| p value vs tramadol | – | 0.0319 | 0.0276 | – |
| Week 16 convenience domain | ||||
| LS mean (SE) score | 73.11 (1.16) | 75.68 (1.16) | 76.37 (1.15) | 74.63 (1.04) |
| LS mean (SE) difference vs placebo | – | 2.57 (1.38) | 3.26 (1.38) | 1.52 (1.30) |
| p value vs placebo | – | 0.0627 | 0.0187 | 0.2419 |
| LS mean (SE) difference vs tramadol | – | 1.05 (1.28) | 1.74 (1.27) | – |
| p value vs tramadol | – | 0.4124 | 0.1730 | – |
| Week 16 global satisfaction domain | ||||
| LS mean (SE) score | 64.90 (1.41) | 70.32 (1.39) | 68.64 (1.38) | 67.12 (1.22) |
| LS mean (SE) difference vs placebo | – | 5.42 (1.86) | 3.74 (1.86) | 2.22 (1.75) |
| p value vs placebo | – | 0.0037 | 0.0449 | 0.2038 |
| LS mean (SE) difference vs tramadol | – | 3.20 (1.73) | 1.52 (1.72) | – |
| p value vs tramadol | – | 0.0644 | 0.3775 | – |
| Week 56 effectiveness domain | ||||
| LS mean (SE) score | – | 72.66 (2.12) | 72.51 (2.01) | 71.21 (1.79) |
| LS mean (SE) difference vs tramadol | – | 1.45 (2.62) | 1.30 (2.53) | – |
| p value vs tramadol | – | 0.5806 | 0.6084 | – |
| Week 56 side effects domain | ||||
| LS mean (SE) score | – | 78.92 (6.32) | 89.37 (4.76) | 76.20 (3.09) |
| LS mean (SE) difference vs tramadol | – | 2.71 (6.95) | 13.17 (5.60) | – |
| p value vs tramadol | – | 0.6991 | 0.0265 | – |
| Week 56 convenience domain | ||||
| LS mean (SE) score | – | 78.72 (1.69) | 80.52 (1.60) | 78.42 (1.45) |
| LS mean (SE) difference vs tramadol | – | 0.30 (1.99) | 2.10 (1.92) | – |
| p value vs tramadol | – | 0.8795 | 0.2758 | – |
| Week 56 global satisfaction domain | ||||
| LS mean (SE) score | – | 78.11 (1.83) | 78.49 (1.73) | 74.57 (1.55) |
| LS mean (SE) difference vs tramadol | – | 3.54 (2.27) | 3.93 (2.19) | – |
| p value vs tramadol | – | 0.1197 | 0.0743 | – |
Week 16 numbers for placebo/tanezumab 5 mg/tanezumab 10 mg/tramadol were 329/338/343/456 for the effectiveness, convenience, and global satisfaction domains and 39/49/49/120 for the side effect domain. Week 56 numbers for tanezumab 5 mg/tanezumab 10 mg/tramadol were 141/159/206 for the effectiveness, convenience, and global satisfaction domains and 9/17/41 for the side effect domain
Each domain score ranges from 0 to 100, with higher scores indicating greater satisfaction
LS least-squares, SE standard error
mPRTI
All active treatments demonstrated significantly better mPRTI scores at week 16 compared with placebo in response to the questions “Overall, do you prefer the drug that you received in this study to previous treatment?” and “Are you willing to use the same drug that you have received in this study for your low back pain?”; no significant difference was observed between the tanezumab and tramadol groups for either question (Table 4).
Table 4.
Modified Patient Reported Treatment Impact (mPRTI) scores at week 16 and week 56
| Placebo (N = 406) | Tanezumab 5 mg (N = 407) | Tanezumab 10 mg (N = 407) | Tramadol (N = 605) | ||
|---|---|---|---|---|---|
| Week 16 | |||||
| Current or most recent treatment you were receiving for low back pain before enrolling? | Injectable prescription medicines | 20 (6.2%) | 21 (6.3%) | 22 (6.5%) | 39 (8.7%) |
| Prescription medicines taken by mouth | 213 (66.1%) | 211 (63.4%) | 229 (67.4%) | 287 (63.8%) | |
| Surgery | 2 (< 1.0%) | 2 (< 1.0%) | 1 (< 1.0%) | 1 (< 1.0%) | |
| Prescription medicines and surgery | 7 (2.2%) | 9 (2.7%) | 10 (2.9%) | 14 (3.1%) | |
| No treatment | 80 (24.8%) | 90 (27.0%) | 78 (22.9%) | 109 (24.2%) | |
| Overall, do you prefer the drug that you received in this study to previous treatment? | Yes, I definitely prefer the drug that I am receiving now | 150 (46.6%) | 172 (51.7%) | 191 (56.2%) | 232 (51.6%) |
| I have a slight preference for the drug that I am receiving now | 57 (17.7%) | 62 (18.6%) | 50 (14.7%) | 89 (19.8%) | |
| I have no preference either way | 62 (19.3%) | 66 (19.8%) | 55 (16.2%) | 82 (18.2%) | |
| I have a slight preference for my previous treatment | 24 (7.5%) | 14 (4.2%) | 23 (6.8%) | 17 (3.8%) | |
| No, I definitely prefer my previous treatment | 29 (9.0%) | 19 (5.7%) | 21 (6.2%) | 30 (6.7%) | |
| p value vs placebo | – | 0.0333 | 0.0244 | 0.0265 | |
| p value vs tramadol | – | 0.9512 | 0.8052 | – | |
| Willing to use the same drug that you have received in this study for your low back pain? | Yes, I would definitely want to use the same drug again | 167 (51.9%) | 191 (57.4%) | 210 (61.8%) | 251 (55.8%) |
| I might want to use the same drug again | 61 (18.9%) | 80 (24.0%) | 58 (17.1%) | 98 (21.8%) | |
| I am not sure | 51 (15.8%) | 36 (10.8%) | 38 (11.2%) | 64 (14.2%) | |
| I might not want to use the same drug again | 11 (3.4%) | 10 (3.0%) | 13 (3.8%) | 13 (2.9%) | |
| No, I definitely would not want to use the same drug again | 32 (9.9%) | 16 (4.8%) | 21 (6.2%) | 24 (5.3%) | |
| p value vs placebo | – | 0.0045 | 0.0099 | 0.0206 | |
| p value vs tramadol | – | 0.4266 | 0.5733 | – | |
| Week 56 | |||||
| Current or most recent treatment you were receiving for low back pain before enrolling? | Injectable prescription medicines | – | 6 (4.3%) | 13 (8.2%) | 9 (4.4%) |
| Prescription medicines taken by mouth | – | 91 (64.5%) | 102 (64.2%) | 147 (71.4%) | |
| Surgery | – | 2 (1.4%) | 0 | 3 (1.5%) | |
| Prescription medicines and surgery | – | 7 (5.0%) | 4 (2.5%) | 3 (1.5%) | |
| No treatment | – | 35 (24.8%) | 40 (25.2%) | 44 (21.4%) | |
| Overall, do you prefer the drug that you received in this study to previous treatment? | Yes, I definitely prefer the drug that I am receiving now | – | 90 (63.8%) | 104 (65.4%) | 129 (62.6%) |
| I have a slight preference for the drug that I am receiving now | – | 30 (21.3%) | 36 (22.6%) | 42 (20.4%) | |
| I have no preference either way | – | 15 (10.6%) | 12 (7.5%) | 22 (10.7%) | |
| I have a slight preference for my previous treatment | – | 2 (1.4%) | 4 (2.5%) | 7 (3.4%) | |
| No, I definitely prefer my previous treatment | – | 4 (2.8%) | 3 (1.9%) | 6 (2.9%) | |
| p value vs tramadol | – | 0.6107 | 0.2846 | – | |
| Willing to use the same drug that you have received in this study for your low back pain? | Yes, I would definitely want to use the same drug again | – | 99 (70.2%) | 114 (71.7%) | 133 (64.6%) |
| I might want to use the same drug again | – | 23 (16.3%) | 31 (19.5%) | 41 (19.9%) | |
| I am not sure | – | 15 (10.6%) | 10 (6.3%) | 26 (12.6%) | |
| I might not want to use the same drug again | – | 0 | 2 (1.3%) | 4 (1.9%) | |
| No, I definitely would not want to use the same drug again | – | 4 (2.8%) | 2 (1.3%) | 2 (< 1.0%) | |
| p value vs tramadol | – | 0.5358 | 0.1082 | – | |
Week 16 n was 322, 333, 340, and 450 for placebo, tanezumab 5 mg, tanezumab 10 mg, and tramadol, respectively
Week 56 n week 56 was 141, 159, and 206 for tanezumab 5 mg, tanezumab 10 mg, and tramadol, respectively
Rescue Medication (Acetaminophen/Paracetamol) Usage
Approximately one-third of all patients (30.7–33.6% across all groups) used rescue medication at week 16, and the LS mean number of days that rescue medication was used was low (1.0–1.2 days/week). The LS mean amount of rescue medication (acetaminophen/paracetamol) used was 1297–1538 mg per week. No significant differences in these parameters were observed across treatment groups.
Efficacy at Week 56
PGA-LBP
Sustained improvements (relative to baseline) in PGA-LBP score were observed in all active treatment groups at week 56, though improvements appeared modestly smaller in magnitude relative to week 16 and no significant differences were observed between the tanezumab and tramadol groups; LS mean difference from tramadol was − 0.10 for tanezumab 5 mg and − 0.07 for tanezumab 10 mg (Table 1).
BPI-sf
Sustained improvements (relative to baseline) in BPI-sf “worst pain,” “average pain,” and the overall pain interference index were observed in all active treatment groups at week 56, though improvements appeared modestly smaller in magnitude relative to week 16 and no significant differences were observed between the tanezumab and tramadol groups (Table 2).
TSQM
Generally, TSQM scores for “effectiveness,” “side effects,” “convenience,” and “global satisfaction” were slightly higher in all active treatment groups relative to week 16. No significant differences were observed for the tanezumab groups compared with tramadol, except the tanezumab 10 mg group for “side effects” (Table 3).
mPRTI
A majority of patients (more than 60%) in all active treatment groups indicated that they “definitely” preferred the study medication at week 56 in response to the question “Overall, do you prefer the drug that you received in this study to previous treatment?” (Table 4). Likewise, more than 60% in all active groups indicated that they would “definitely” want to use the study medication again in response to the question “Are you willing to use the same drug that you have received in this study for your low back pain?” No significant differences were observed between the tanezumab and tramadol groups regarding responses to these questions.
Rescue Medication (Acetaminophen/Paracetamol) Usage
Approximately one-third of all patients (34.9–35.6% across all active groups) used rescue medication at week 56, and the LS mean number of days that rescue medication was used was low (1.2–1.4 days/week); no significant differences in these parameters were observed between the tanezumab and tramadol groups. The LS mean amount of rescue medication used at week 56 is not provided since it was not assessed after week 16.
Discussion
This study demonstrates that tanezumab 10 mg provides significantly greater improvement in measures of pain and pain interference with daily functions than placebo in patients with moderate-to-severe CLBP and a history of inadequate response to other analgesics after 16 weeks of treatment. Moreover, tanezumab 10 mg is associated with greater improvement in global assessment of disease status and better treatment satisfaction scores than placebo at week 16. Improvements in interference with daily functions observed with tanezumab 10 mg, relative to placebo and to tramadol, are of particular importance in the CLBP population since reduction in pain intensity alone is an imperfect measure of therapeutic success [17].
The first 16 weeks of the treatment period allow for robust assessment of response to tanezumab and tramadol since, during this time, a placebo treatment arm was utilized, use of rescue medication was limited to 3 days per week, adjunctive analgesics were prohibited, and new non-pharmacologic treatment regimens could not be initiated. At week 16 tanezumab 10 mg significantly improved BPI-sf worst pain, BPI-sf average pain, the BPI-sf pain interference index, global assessment of disease status, satisfaction with medication effectiveness, satisfaction with medication side effects, global satisfaction with medication, preference for study medication over prior treatment, and willingness to use study medication in the future scores compared with placebo. The totality of this evidence (based on measures of pain, interference with daily functions, global disease status, and treatment satisfaction) support the conclusion that tanezumab 10 mg provided clinically meaningful benefit to some patients in the study. These findings support the previously published primary efficacy findings of this study in which tanezumab 10 mg was shown to improve mean LBPI (Supplementary Table 1), the proportion of patients experiencing at least 30% and at least 50% improvement in LBPI (Supplementary Fig. 1A), mean RMDQ score (Supplementary Table 1), and the proportion of patients experiencing at least 30% and at least 50% improvement in RMDQ (Supplementary Fig. 1B) compared to placebo at week 16 [16]. It should be noted that, although the 5 mg dose of tanezumab did not meet the primary LBPI endpoint at week 16 [16], it demonstrated improvements over placebo on most secondary efficacy endpoints at week 16.
Findings with tanezumab contrast with those of tramadol, which did not significantly improve any measures of pain, interference with daily functions, or global assessment of disease status compared with placebo at week 16. Improvements in pain, interference with daily functions, and global assessment of disease status favored tanezumab over tramadol at week in 16 all cases, often reaching the level of statistical significance. This may be due, in part, to the dose of tramadol utilized. The mean/median dose of tramadol at week 16 was 203/200 mg and titration to higher doses (up to 300 mg/day was allowed) was likely limited by tolerability, since opioid-related adverse events were common in the tramadol group [16]. The trial also enriched for patients with inadequate response to analgesics (opioids were among the most common) and, as a result, may have inadvertently enriched for patients who were inadequate responders to tramadol since the mechanism of action of tramadol overlaps with that of traditional opioids. However, the lack of meaningful effect on pain and daily functions (in particular) with tramadol (compared to placebo) observed in this study is consistent with previous short-term studies of tramadol and other opioids for CLBP [6, 7, 9, 18]. Movement-evoked pain has a substantial impact on physical function and there is evidence from the perioperative literature that the analgesic benefit of this drug class may be reduced for these episodic symptoms that interfere with everyday activity in patients with CLBP [18, 19]. Sensitization (peripheral and central) is a key mechanism underlying persistent movement-evoked pain [20], and anti-NGF therapies have demonstrated efficacy against movement-induced pain in animal models [21, 22]. Taken together, these lines of clinical and preclinical evidence might suggest a role for NGF-mediated nociceptive sensitization and hyperalgesia in the context of movement (i.e., mechanical)-induced pain and may explain why tanezumab, but not tramadol, improved functional outcomes in this study of CLBP. Notably, improvements in physical function have also been observed in patients with osteoarthritis treated with tanezumab or other anti-NGF therapies [15, 23–25].
Numerical improvements (over baseline) in pain, interference with daily functions, and global assessment of disease status were maintained in the tanezumab groups at week 56, though magnitude of improvement was modestly lower relative to week 16 and most treatment effects were not significantly greater than tramadol (mean/median dose was 209/200 mg at week 56). The treatment period from week 16 to 56, however, was primarily designed to assess safety, and several factors limit the ability to make conclusions on long-term efficacy and comparisons between groups. The lack of difference between the tanezumab and tramadol groups at week 56 was likely due, in part, to discontinuation of patients; approximately 65% of patients across all groups discontinued treatment, predominately for efficacy-related reasons including proactive discontinuation of non-responders at weeks 16 and 32. The result of these discontinuations is that the study becomes enriched for responders at later time points and later time points have a high degree of imputation due to missing data. Increased use of rescue medication was also allowed after week 16. While the incidence and number of days of rescue medication use was similar across groups at week 56, the amount of rescue medication used was not assessed and could have masked the effects of study medication. The use of adjunct analgesics (excluding NSAIDs) also increased after week 16, though overall use during the treatment period was similar across groups (11–14% through week 64).
This study (including the secondary measures reported here and the primary measures reported previously [16]) employed a variety of patient-reported assessments of pain intensity, function, global disease status, treatment satisfaction, and treatment preference. The totality of evidence from these measures demonstrates that tanezumab 10 mg provides clinically meaningful benefit to some patients with CLBP. Clinically meaningful relates to effects that are perceived by the patient as beneficial, as opposed to statistically significant which simply means effects were different from placebo. Reduction in pain is a key goal for patients with CLBP. Thus, we used the LBPI (which rates pain severity on a scale from 0 to 10) to assess improvement in pain intensity. To characterize meaningful effects, we examined the proportion of patients achieving 30% and 50% improvement in LBPI, thresholds that are considered moderate and substantial, respectively, improvements in pain for patients with chronic pain conditions. Since improvement in function is also key goal for patients with CLBP, we also utilized the RMDQ. The RMDQ is a validated back pain-specific outcome measure that is more sensitive to change than other functional measures in patients with axial-predominant CLBP [26]. The mean change in RMDQ from baseline achieved among tanezumab-treated patients at week 16 exceeded the minimal clinically important difference for this measure [26]. In addition to change in mean score, we utilized 30% and 50% improvement thresholds (as we did for LBPI) to assess meaningful response with the RMDQ. The BPI-sf is widely used to assess pain and is validated for use across several indications, including low back pain [27, 28]. A key benefit of the BPI-sf is that it assesses both pain intensity (worst and average pain) and the impact of pain on a variety of daily activities. The importance of tools, such as the PGA-LBP, that provide a patient’s perspective on their overall disease status is increasingly being recognized in chronic pain conditions [29]. The PGA-LBP asks a simple question: “Considering all the ways your low back pain affects you, how are you doing today?” and answers are rated on a 5-point Likert scale form 1 = very good to 5 = very poor. A benefit of the PGA-LBP is that it is not focused solely on pain or function, but rather addresses all aspects of CLBP (anxiety, depression, socialization, etc.). Studies have demonstrated associations between patient satisfaction with treatment and clinical outcomes [30–32], which warranted utilization of the TSQM (a generic measure of treatment satisfaction applicable to any indication or treatment) and the mPRTI to assess preference of study medication relative to medications the patient has used in the past.
Despite the beneficial effects observed here, it should be noted that there is a risk of joint-safety events (predominantly rapidly progressive osteoarthritis) associated with tanezumab and other anti-NGF antibodies [18]. These events have been observed in studies of CLBP and occur in a dose-dependent fashion [16]. In this study, adjudicated joint safety events occurred in 19 patients (placebo, 0; tanezumab 5 mg, 5; tanezumab 10 mg, 13; and tramadol, 1).
Limitations
As described earlier in the discussion, our analyses are limited by certain factors. Findings with tramadol may be limited by the relatively low dose of tramadol utilized in the study and the enrichment of subjects who were inadequate responders to opioids (which have mechanism of action similar to tramadol). In addition, efficacy findings beyond week 16 are limited by elements of study design. First, a substantial proportion of patients were discontinued at later time points. This was primarily due to the discontinuation of non-responders (to avoid unnecessary exposure of patients who were not experiencing an analgesic benefit) at week 16. In addition, increased use of rescue analgesia and the initiation of adjunctive analgesia was allowed after week 16, making direct comparisons between tanezumab and tramadol more difficult. Finally, there was no placebo-comparator group after week 16.
On October 26, 2021, Pfizer Inc. and Eli Lilly and Company announced discontinuation of the tanezumab global clinical development program as a result of the outcomes of regulatory reviews of tanezumab for the treatment of osteoarthritis pain by the US Food and Drug Administration and European Medicines Agency [33, 34].
Conclusion
Overall, tanezumab demonstrated significant improvements over placebo for most measures of pain, interference with daily functions, and treatment satisfaction after 16 weeks of treatment, while changes in pain and interference with daily functions with tramadol were not significantly different from placebo. The effects of tanezumab may be sustained up to 56 weeks, though conclusions on long-term efficacy should be interpreted with caution as a result of elements of study design. These data highlight the potential ability of tanezumab to provide clinically meaningful benefit in some patients with moderate-to-severe CLBP who have had inadequate response to other standard analgesics.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank all participants of the study along with site investigators and staff.
Funding
The study was sponsored by Pfizer and Eli Lilly and Company. Pfizer and Eli Lilly and Company funded the journal’s rapid service fee associated with submission of the manuscript. Pfizer, in collaboration with Eli Lilly and Company, is the manufacturer of tanezumab, which is being investigated for the treatment of chronic pain. Pfizer Inc and Eli Lilly and Company contributed to the study design; Pfizer contributed to the management and collection of data. In their role as authors, employees of Pfizer and Eli Lilly were involved in the interpretation of data, preparation, review, and approval of the manuscript and the decision to submit for publication, along with their co-authors. The study sponsors approved the manuscript from an intellectual property perspective but had no right to veto the publication.
Editorial Assistance
Medical writing support was provided by Matt Soulsby, PhD, of Engage Scientific and was funded by Pfizer and Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
John D. Markman, Thomas J. Schnitzer, Serge Perrot, Said R. Beydoun, Seiji Ohtori and Lars Viktrup were involved in interpretation of data, drafting the article or revising it critically for important intellectual content, and approving the final version to be published. Ruoyong Yang, Christine Bramson, Christine R. West, and Kenneth M. Verburg were involved in study conception and design, acquisition of data, analysis of data, interpretation of data, drafting the article or revising it critically for important intellectual content, and approving the final version to be published.
Disclosures
John D. Markman has received grants or contracts from Grunenthal; has served as a consultant (advisory board) to Pfizer, Eli Lilly and Company, Flexion Therapeutics, Quark Pharmaceuticals, Quartet Medicine, Collegium, Biogen, Novartis, Aptinyx, Nektar, Greenwich Bioscience, Grünenthal, Depomed, Teva Pharmaceutical, KemPharm, Chromocell, Convergence Pharmaceuticals, Inspirion, Sanofi, Daiichi Sankyo, SK Lifescience, and Trevena; has received support to attend meetings from Pfizer and Eli Lilly and Company; has served on a data safety monitoring board for Novartis, Regenacy, Tonix, and Allergan; and has served in a leadership or fiduciary role for the American Pain Society. Thomas J. Schnitzer reports clinical research study support from Pfizer, Eli Lilly and Company, Regeneron, Galapagos, Taiwan Liposome Corporation, Anika Therapeutics, KolonTissureGenex, Novartis, and Techfields; has served as a consultant to Pfizer, Eli Lilly and Company, Glaxo-Smith Kline, AstraZeneca, Noven, Galapagos, Merck, Vertex, Acadia, Grunenthal, Paradigm, Cullgen, Collegium; and has served on a data safety monitoring board for AstraZeneca, Calibr, and TissueTech. Serge Perrot has served as a consultant to Pfizer Inc, Grünenthal, Eli Lilly and Company, Sanofi, and UPSA; and has served as a speaker for Pfizer, Grunenthal, Eli Lilly and Company, UPSA, Sanofi, and Merck. Said R. Beydoun has served as a consultant for CSL, Grifols, Takeda, Mitsubishi Tanabe, Akcea, Alnylam, and Janssen; has served as a speaker for CSL, Grifols, Takeda, Alnylam, and Akcea; and has received research grants (via institution) from Argenx, Alexion, UCB, Ra pharma, Catalyst, and AB Sciences. Seiji Ohtori has no disclosures to report. Lars Viktrup is an employee of, and owns stock in, Eli Lilly and Company. Ruoyong Yang, Candace Bramson, and Christine R. West are employees of, and own stock/options in, Pfizer Inc. Kenneth M. Verburg (no current affiliation) was an employee of Pfizer Inc at the time the study was completed and owns stocks/options.
Compliance with Ethics Guidelines
The study protocol was approved by an institutional review board or independent ethics committee for each participating investigational center (Supplementary Table 2) and all patients provided written informed consent. This study was conducted in compliance with ethical principles of the Declaration of Helsinki and Good Clinical Practice Guidelines.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Contributor Information
John D. Markman, Email: John_Markman@URMC.Rochester.edu
Thomas J. Schnitzer, Email: tjs@northwestern.edu
Serge Perrot, Email: serge.perrot@aphp.fr.
Said R. Beydoun, Email: sbeydoun@usc.edu
Seiji Ohtori, Email: sohtori@faculty.chiba-u.jp.
Lars Viktrup, Email: viktrup_lars@lilly.com.
Ruoyong Yang, Email: Ruoyong.Yang@pfizer.com.
Candace Bramson, Email: Candace.Bramson@pfizer.com.
Christine R. West, Email: Christine.West@pfizer.com
Kenneth M. Verburg, Email: Kenneth.M.Verburg@gmail.com
References
- 1.Institutes for Health Metrics and Evaluation. Global burden of disease (GBD) compare 2017. https://vizhub.healthdata.org/gbd-compare/. Accessed Nov 20, 2019.
- 2.Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 3.The US Burden of Disease Collaborators The State of US Health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–606. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markman JD, Czerniecka-Foxx K, Khalsa PS, et al. AAPT diagnostic criteria for chronic low back pain. J Pain. 2020;21(11–12):1138–1148. doi: 10.1016/j.jpain.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 5.Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 6.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350:g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou R, Deyo R, Friedly J, et al. Systemic pharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166(7):480–492. doi: 10.7326/M16-2458. [DOI] [PubMed] [Google Scholar]
- 9.Chaparro LE, Furlan AD, Deshpande A, Mailis-Gagnon A, Atlas S, Turk DC. Opioids compared with placebo or other treatments for chronic low back pain: an update of the Cochrane Review. Spine (Phila Pa 1976) 2014;39(7):556–563. doi: 10.1097/BRS.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 10.Bailly F, Foltz V, Rozenberg S, Fautrel B, Gossec L. The impact of chronic low back pain is partly related to loss of social role: a qualitative study. Joint Bone Spine. 2015;82(6):437–441. doi: 10.1016/j.jbspin.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 11.Grabovac I, Dorner TE. Association between low back pain and various everyday performances. Wien Klin Wochenschr. 2019;131(21):541–549. doi: 10.1007/s00508-019-01542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tagliaferri SD, Miller CT, Owen PJ, et al. Domains of chronic low back pain and assessing treatment effectiveness: a clinical perspective. Pain Pract. 2020;20(2):211–225. doi: 10.1111/papr.12846. [DOI] [PubMed] [Google Scholar]
- 13.Barker PA, Mantyh P, Arendt-Nielsen L, Viktrup L, Tive L. Nerve growth factor signaling and its contribution to pain. J Pain Res. 2020;13:1223–1241. doi: 10.2147/JPR.S247472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mantyh PW, Koltzenburg M, Mendell LM, Tive L, Shelton DL. Antagonism of nerve growth factor-TrkA signaling and the relief of pain. Anesthesiology. 2011;115(1):189–204. doi: 10.1097/ALN.0b013e31821b1ac5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmelz M, Mantyh P, Malfait AM, et al. Nerve growth factor antibody for the treatment of osteoarthritis pain and chronic low-back pain: mechanism of action in the context of efficacy and safety. Pain. 2019;160(10):2210–2220. doi: 10.1097/j.pain.0000000000001625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Markman JD, Bolash RB, McAlindon TE, et al. Tanezumab for chronic low back pain: a randomized, double-blind, placebo- and active-controlled, phase 3 study of efficacy and safety. Pain. 2020;161(9):2068–2078. doi: 10.1097/j.pain.0000000000001928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ballantyne JC, Sullivan MD. Intensity of chronic pain—the wrong metric? N Engl J Med. 2015;373(22):2098–2099. doi: 10.1056/NEJMp1507136. [DOI] [PubMed] [Google Scholar]
- 18.Butera KA, Fox EJ, George SZ. Toward a transformed understanding: from pain and movement to pain with movement. Phys Ther. 2016;96(10):1503–1507. doi: 10.2522/ptj.20160211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilron I, Tod D, Goldstein DH, Parlow JL, Orr E. The relationship between movement-evoked versus spontaneous pain and peak expiratory flow after abdominal hysterectomy. Anesth Analg. 2002;95(6):1702–1707. doi: 10.1097/00000539-200212000-00043. [DOI] [PubMed] [Google Scholar]
- 20.Corbett DB, Simon CB, Manini TM, George SZ, Riley JL, 3rd, Fillingim RB. Movement-evoked pain: transforming the way we understand and measure pain. Pain. 2019;160(4):757–761. doi: 10.1097/j.pain.0000000000001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shelton DL, Zeller J, Ho WH, Pons J, Rosenthal A. Nerve growth factor mediates hyperalgesia and cachexia in auto-immune arthritis. Pain. 2005;116(1–2):8–16. doi: 10.1016/j.pain.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 22.Ishikawa G, Koya Y, Tanaka H, Nagakura Y. Long-term analgesic effect of a single dose of anti-NGF antibody on pain during motion without notable suppression of joint edema and lesion in a rat model of osteoarthritis. Osteoarthr Cartil. 2015;23(6):925–932. doi: 10.1016/j.joca.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Berenbaum F, Blanco FJ, Guermazi A, et al. Subcutaneous tanezumab for osteoarthritis of the hip or knee: efficacy and safety results from a 24-week randomised phase III study with a 24-week follow-up period. Ann Rheum Dis. 2020;79(6):800–810. doi: 10.1136/annrheumdis-2019-216296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schnitzer TJ, Easton R, Pang S, et al. Effect of tanezumab on joint pain, physical function, and patient global assessment of osteoarthritis among patients with osteoarthritis of the hip or knee: a randomized clinical trial. JAMA. 2019;322(1):37–48. doi: 10.1001/jama.2019.8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schnitzer TJ, Marks JA. A systematic review of the efficacy and general safety of antibodies to NGF in the treatment of OA of the hip or knee. Osteoarthr Cartil. 2015;23(Suppl 1):S8–17. doi: 10.1016/j.joca.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord. 2006;7(1):82. doi: 10.1186/1471-2474-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramasamy A, Martin ML, Blum SI, et al. Assessment of patient-reported outcome instruments to assess chronic low back pain. Pain Med. 2017;18(6):1098–1110. doi: 10.1093/pm/pnw357. [DOI] [PubMed] [Google Scholar]
- 28.Brief Pain Inventory User Guide. https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf. Accessed 28 Nov 2019.
- 29.Nikiphorou E, Radner H, Chatzidionysiou K, et al. Patient global assessment in measuring disease activity in rheumatoid arthritis: a review of the literature. Arthritis Res Ther. 2016;18(1):251. doi: 10.1186/s13075-016-1151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCracken LM, Evon D, Karapas ET. Satisfaction with treatment for chronic pain in a specialty service: preliminary prospective results. Eur J Pain. 2002;6(5):387–393. doi: 10.1016/S1090-3801(02)00042-3. [DOI] [PubMed] [Google Scholar]
- 31.Rofail D, Myers L. Treatment satisfaction and dissatisfaction in chronic low back pain: a systematic review. J Psychol Psychother. 2016;6:2161-0487. doi: 10.4172/2161-0487.1000260. [DOI] [Google Scholar]
- 32.Treatment Satisfaction Questionnaire for Medication Fact Sheet. https://www.iqvia.com/-/media/iqvia/pdfs/library/fact-sheets/iqvia-tsqm-treatment-satisfaction-questionnaire--for-medication.pdf. Accessed 28 Nov 2019.
- 33.Pfizer Inc Press Release 2021. https://investors.pfizer.com/investor-news/press-release-details/2021/PFIZER-REPORTS-THIRD-QUARTER-2021-RESULTS/default.aspx. Accessed 1 Feb 2022.
- 34.Eli Lilly and Company Press Release 2021. https://investor.lilly.com/static-files/a0b77c52-a997-41c1-9534-5f465903a0b4. Accessed 1 Feb 2022.
- 35.Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006;22(10):1911–1920. doi: 10.1185/030079906X132488. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.


