Abstract
Background
With increasing life expectancy in China, the associated burden of low back and neck pain (spinal pain) on the healthcare system increases, posing a substantial public health challenge. This study aimed to investigate trends in spinal pain incidence across China from 1990 to 2019 and to predict incidence trends between 2020 and 2030.
Methods
Data were derived from the Global Burden of Disease Study (GBD) 2019. The annual percentage change (APC) and average annual percentage change (AAPC) between 1990 and 2019 were calculated using Joinpoint regression analysis. The effects of age, period, and cohort on spinal pain were estimated by an age–period–cohort model. An autoregressive integrated moving average (ARIMA) model was used to forecast incidence trends from 2020 to 2030.
Results
From 1990 to 2019, the age-standardized incidence rate (ASIR) of low back pain (LBP) significantly decreased in both male and female subjects, while the ASIR of neck pain (NP) slightly increased regardless of sex. Joinpoint regression analysis showed that the incidence rates of LBP decreased in all age groups, and incidence rates of NP increased after 45 years old among men and women. The age effects showed that the relative risks (RR) of LBP incidence increased with age, and the group aged 40–49 years had the highest RR for NP incidence, regardless of sex. Period effects showed that the risk of NP continuously increased with increasing time periods, but not in LBP. The cohort effect showed a continuously decreasing trend in later birth cohorts. The prediction results of the ARIMA model show that the ASIR of NP in both male and female subjects in China shows an increasing trend in the next 10 years, and the ASIR of LBP increased in male but decreased in female subjects.
Conclusion
Spinal pain has remained a major public health burden over the past 30 years in China and will likely increase further with population aging. Therefore, spinal pain should be a priority for future research on prevention and therapy, and is especially critical as the aging population increases in China.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40122-022-00422-9.
Keywords: Spinal pain, Low back pain, Neck pain, Incidence, Joinpoint regression analysis, Age–period–cohort model
Key Summary Points
| Why carry out this study? |
| LBP and NP cause functional impairment, diminished quality of life, work disability, potential psychological distress, and increased healthcare costs |
| Additionally, there was no comprehensive study to explore the long-term trends of LBP and NP between different age groups and gender, and to analyze these trends from age, period, and cohort dimensions |
| Use of the ARIMA model to predict the incidence of LBP and NP in China is of great significance for further prevention and control |
| What was learned from the study? |
| The ASIR of LBP presented decreasing trends in China from 1990 to 2019, while the NP incidence slightly increased regardless of sex |
| The relative burden caused by LBP and NP is predicted to continue to increase in the next decade, which that indicates the burden remains high |
Introduction
Spinal pain, including low back pain (LBP) and neck pain (NP), is the leading cause of disability and economic and medical burden in high-income countries and is of increasing concern in low-income and middle-income countries [1–3]. As per the Global Burden of Disease Study (GBD) 2019, LBP is the most common musculoskeletal disease, while NP is the second most common musculoskeletal disease [4]. The prevalence and burden of spinal pain are exceptionally high throughout the world and their impact on daily life also increases with age [4]. As the global population ages, disability and costs attributed to spinal pain are projected to increase. More importantly, in addition to pain, physical and functional disability, spinal pain often leads to mental capacity problems and poses major threats to healthy aging [5]. However, unlike fatal diseases, such as cardiovascular diseases and cancers, spinal pain is often viewed as less important because of its non-fatal nature [6, 7].
With increasing life expectancy, China has become the country with the largest elderly population and the fastest aging population in the world. It means that age-related diseases, such as LBP and NP, are placing an increasing burden on the health system. In 1990, LBP and NP were ranked as the 17th and 21st leading cause of disability-adjusted life years (DALYs) in China, respectively; and in 2017, they rose to the 13th and 9th leading cause, respectively [8]. To achieve The Healthy China 2030 blueprint, we need to face the challenges in constructing a healthy China [9]. Thus, it is necessary to investigate the secular trends of the burden of LBP and NP in recent decades to judge the gap between current conditions and the Healthy China 2030 goals. Some previous studies, using data from the GBD 2017, reported DALYs, years lived with disability (YLDs), and years of life lost (YLLs) but no incidence of LBP and NP in China from 1990 to 2017 [10, 11]. A recent study has focused on LBP and NP incidence across time and reported changes in age-specific rates [12]. However, the incidence across time was not reported by gender, as previous studies have shown a difference in the incidence of spinal pain between men and women [2, 12]. Moreover, this approach fails to distinguish cohort from period effects. Distinguishing the relative contributions of period and cohort effects to overall temporal trends helps to determine the success of early policy interventions and identify future goals.
The GBD 2019 provides a standardized approach for estimating the burden of LBP and NP in China [4]. The current study aimed to (1) examine the temporal trends in the incidence of LBP and NP by gender; (2) investigate the independent effects of age, period, and cohort on LBP and NP incidence from 1990 to 2019, and compare these effects by gender; and (3) predict the incidence of LBP and NP by gender from 2020 to 2030 in China.
Methods
Data Source
Incidence data (1990–2019) were obtained from the GBD 2019 study, which was provided by the Institute for Health Metrics and Evaluation. The GBD 2019 study used the up-to-date sources of epidemiological data and improved standardized methods to comprehensively estimate disease burden (e.g., incidence, prevalence, mortality, and DALYs) for 369 diseases and injuries and 87 risk factors in 204 countries and territories [4, 13]. Details of the data, methodology used, and statistical modeling for the GBD 2019 have been reported in previous studies [4, 13]. In our study, we retrieved the incidence of LBP and NP for successive 5-year age groups from 5–9 years to 90–94 years and age-standardized groups in China to conduct the trends analysis. All the data was downloaded from the official website of GBD 2019 (http://ghdx.healthdata.org/gbd-results-tool). The incidence of LBP and NP was estimated using the Bayesian meta-regression model (DisMod-MR 2.1) to ensure consistency among estimates. The original data used to inform the models were mainly sourced from literature published between 1990 and 2019, epidemiological surveys of LBP and NP, and health surveys [1, 3, 4, 13]. In addition, the study did not require ethical approval because it used publicly available data.
Case Definition
The case definition of LBP in the GBD 2019 is as follows: “pain on the posterior aspect of the body ranging from the lower margin of the twelfth ribs to the lower gluteal folds, with or without pain involving one or both lower limbs, and the pain should last for at least one day [4].” The case definition for NP is “neck pain [± pain referred into the upper limb(s)] that lasts for at least one day [4].” International Classification of Diseases, Ninth Revision (ICD-9) and ICD-10 codes are utilized to define LBP (ICD9: 724; ICD10: M54.3, M54.4, M54.5) and NP (ICD9: 723.1; ICD10: M54.2), respectively.
Statistical Analysis
ASIR with 95% uncertainty intervals (UIs) of LBP and NP were reported according to age and gender. All the rates are reported per 100,000 population. All statistical tests were two-sided, and p < 0.05 indicated statistically significant differences.
Joinpoint regression analysis was used to determine temporal trend changes in the disease burden of LBP and NP. Significant changes in the time points were tested by the Monte Carlo permutation method. Average annual percentage change (AAPC) was calculated for the entire period analyzed from 1990 to 2019, and APC was calculated for each segmented by the model. The APC and AAPC were used to characterize the changing trends of ASIR of LBP and NP. Its hypothesis test was whether AAPC/APC was significantly different from zero; APC/AAPC > 0 means an increasing trend, and APC/AAPC < 0 means decreasing trend during the segment. The analysis was performed with Joinpoint Regression Program software (version 4.9.0.1; Statistical Research and Applications Branch, National Cancer Institute).
The age–period–cohort model was used to assess the effects of age, period, and cohort on incidence trends [14, 15]. In this study, age effects mainly reflect the influence of age change on disease incidence. Period effects refer to the effects of changes over time on all age groups, presumably the result of changes in social, cultural, or economic environments. The cohort effects reflect the characteristics of each generation and take into account the risk factors and exposure to environmental factors present early in life that may adversely affect them later in life. The age–period–cohort model requires an equal time interval in age, period, and cohort. Otherwise, overlapping information will occur in adjacent queues. For age–period–cohort analyses, the incidences and population data were arranged into consecutive 5-year periods from 1990 to 2019. The age groups were selected at successive 5-year age intervals from 5–9 years to 90–94 years, resulting in 18 age groups in total. The sample comprised 23 consecutive cohorts, which ranged from those born in 1900 to 1904 (median, 1902) to those born from 2010 to 2014 (median, 2012). The period of 1990 to 1994 and the birth cohort of 1900 to 1904 were defined as the reference groups, respectively. The age–period–cohort model parameters were estimated by using an intrinsic estimator (IE) with a basis Poisson log-linear model because the three parameters have a linear relationship. Additionally, Deviance, Bayesian information criterion (BIC), and Akaike information criterion (AIC) were used to assess the degree of fitting the model. Relative risk (RR) (exp(coef.) = ecoef.) was used to interpret the estimated parameters of the model. Age–period–cohort analysis was conducted using STATA 15.0 software (StataCorp, College Station, TX, USA).
The ARIMA (p, d, q) model was applied to forecast the incidence trends of LBP and NP from 2020 to 2030. The letters p, d, and q respectively represent the orders of autoregression, degree of difference, and order of moving average [16]. The ARIMA equation is
where ϕ and θ are the autoregressive and moving average parameters, respectively. Yt represents the differenced time series, and εt is the value of the random shock at time t. α is a constant. The construction of this model requires the following steps. First, the Augmented Dickey–Fuller (ADF) test is used to determine whether the sequence is stationary or not. If the result of the ADF test is significant, the sequence is stable. Second, the parameters of the ARIMA model were roughly determined by the figures of the autocorrelation function (ACF) and the partial autocorrelation function (PACF). The ARIMA function was used to select the optimal model with the lowest value in BIC and highest R2 (the coefficient of determination, a statistic that indicates the goodness of fit of a model). The Ljung–Box Q test, ACF, and PACF of residuals were implemented to judge whether the residuals of the optimal model meet the requirements of white noise sequences. Finally, after the constructed model was tested for white noise and passed, we applied this model to forecast the incidence rate of LBP and NP from 2020 to 2030. Time series analyses were conducted using SPSS (Version 22.0, IBM; New York) and R 3.6.2.
Results
Descriptive Analysis
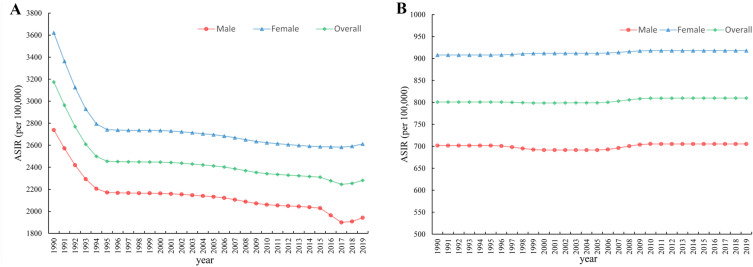
Trends in the sex-specific ASIR for LBP and NP in China from 1990 to 2019 are shown in Fig. 1. Generally, the ASIR of LBP continuously decreases from 1990 to 2019. The ASIR of NP has remained roughly stable over the three decades. The sex-specific incidence rates for LBP and NP stratified by age group in China in 1990 and 2019 are presented in Table 1. In 2019, the ASIR of LBP in China were 1941.68 (95% UI 1711.82–2201.90) and 3174.26 (95% UI 2806.28–3598.26) per 100,000 male and female subjects, respectively. The ASIR were 705.36 (95% UI 556.68–888.37) in male subjects and 917 (95% UI 721.91–1172.30) in female subjects for NP per 100,000 population. The ASIR changed from 3174.26 (95% UI 2806.28–3598.26) to 2280.67 (95% UI 2017.18–2572.62) for LBP and from 800.68 (95% UI 634.43–1016.63) to 809.91 (95% UI 641.89–1028.61) for NP in China from 1990 to 2019, per 100,000 population, respectively. For both sexes, the incidence rates of LBP increased with increasing age. For female subjects, the highest incidence rates of NP were observed in the group aged 45–49 years. The peak incidence of NP in male subjects was concentrated in the group aged 55–74 years.
Fig. 1.
Trends of low back pain (A) and neck pain (B) by sex in China from 1990 to 2019. ASIR, age-standardized incidence rates
Table 1.
Sex- and age-specific rates of low back and neck pain in China in 1990 and 2019 and their average annual percentage changes (AAPC) from 1990 to 2019
| Categories | Male subjects | Female subjects | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Rates in 1990, 95% UI (per 100,000 population) | Rates in 2019, 95% UI (per 100,000 population) | AAPC, 95% CI (%, 1990–2019) | Rates in 1990, 95% UI (per 100,000 population) | Rates in 2019, 95% UI (per 100,000 population) | AAPC, 95% CI (%, 1990–2019) | Rates in 1990, 95% UI (per 100,000 population) | Rates in 2019, 95% UI (per 100,000 population) | AAPC, 95% CI (%, 1990–2019) | |
| LBP | |||||||||
| ASIR | 2738.75 (2410.91, 3105.47) | 1941.68 (1711.82, 2201.90) | − 1.17 (− 1.27, − 1.07)* | 3621.49 (3207.02, 4105.59) | 2611.58 (2314.87, 2947.58) | − 1.12 (− 1.16, − 1.07)* | 3174.26 (2806.28, 3598.26) | 2280.67 (2017.18, 2572.62) | − 1.16 (− 1.23, − 1.08)* |
| 5–9 years | 382.79 (202.63, 621.65) | 377.64 (199.41, 608.82) | − 0.05 (− 0.06, − 0.03)* | 593.49 (340.88, 937.75) | 581.63 (335.17, 914.48) | − 0.08 (− 0.10, − 0.06)* | 483.91 (273.02, 767.13) | 471.35 (265.84, 745.10) | − 0.10 (− 0.11, − 0.08)* |
| 10–14 years | 1129.95 (730.85, 1640.54) | 1172.65 (771.88, 1677.11) | 0.11 (0.10, 0.13)* | 1612.71 (1078.59, 2285.23) | 1605.60 (1085.68, 2273.34) | − 0.03 (− 0.07, 0.02)* | 1363.52 (900.26, 1935.79) | 1370.78 (921.04, 1957.04) | 0.00 (− 0.03, 0.03) |
| 15–19 years | 1514.21 (990.40, 2158.16) | 1559.45 (1042.29, 2188.92) | 0.07 (0.03, 0.12)* | 1938.24 (1293.27, 2740.87) | 1860.98 (1250.16, 2613.83) | − 0.16 (− 0.23, − 0.10)* | 1720.48 (1142.96, 2432.62) | 1700.07 (1142.90, 2381.29) | − 0.06 (− 0.16, 0.03) |
| 20–24 years | 1695.76 (1038.63, 2417.34) | 1514.59 (951.70, 2168.86) | − 0.42 (− 0.61, − 0.23)* | 2037.51 (1241.60, 2934.35) | 1607.27 (992.41, 2325.61) | − 0.82 (− 0.96, − 0.68)* | 1862.79 (1141.42, 2678.33) | 1558.85 (959.69, 2255.30) | − 0.63 (− 0.77, − 0.49)* |
| 25–29 years | 1914.62 (1223.22, 2661.19) | 1333.73 (821.69, 1855.94) | − 1.25 (− 1.43, − 1.06)* | 2379.66 (1545.49, 3302.57) | 1424.75 (875.44, 7987.79) | − 1.77 (− 1.83, − 1.70)* | 2141.0 (1375.03, 2969.93) | 1378.42 (849.67, 1914.87) | − 1.51 (− 1.63, − 1.39)* |
| 30–34 years | 2352.03 (1558.49, 3385.98) | 1454.13 (921.24, 2164.79) | − 1.67 (− 1.79, − 1.54)* | 2962.43 (2001.18, 4268.23) | 1604.22 (1033.68, 2348.52) | − 2.06 (− 2.11, − 2.00)* | 2644.13 (1775.35, 3833.80) | 1528.31 (977.14, 2259.49) | − 1.84 (− 1.90, − 1.77)* |
| 35–39 years | 3137.79 (2060.57, 4576.74) | 2253.24 (1466.70, 3314.34) | − 1.15 (− 1.23, − 1.06)* | 3816.21 (2471.15, 5641.05) | 2188.36 (1441.13, 3225.42) | − 1.87 (− 1.93, − 1.81)* | 3465.39 (2268.79, 5061.95) | 2221.41 (1466.15, 3263.67) | − 1.48 (− 1.55, − 1.40)* |
| 40–44 years | 3662.33 (2489.55, 5230.11) | 2898.70 (1969.26, 4103.90) | − 0.79 (− 0.83, − 0.75)* | 4585.58 (3101.52, 6566.14) | 2810.12 (1868.14, 4069.78) | − 1.65 (− 1.70, − 1.59)* | 4101.43 (2775.41, 5824.18) | 2855.33 (1923.63, 4094.83) | − 1.20 (− 1.25, − 1.16)* |
| 45–49 years | 3939.91 (2641.28, 5482.68) | 2926.59 (1970.70, 4090.02) | − 1.02 (− 1.06, − 0.97)* | 5562.14 (3798.25, 7835.63) | 3850.47 (2591.74, 5304.56) | − 1.28 (− 1.35, − 1.22)* | 4753.23 (3204.10, 6549.88) | 3379.77 (2286.53, 4633.90) | − 1.15 (− 1.21, − 1.10)* |
| 50–54 years | 4201.28 (2732.93, 5989.75) | 2858.16 (1836.21, 4038.72) | − 1.30 (− 1.35, − 1.24)* | 6760.97 (4500.13, 9418.15) | 4827.75 (3192.72, 6749.43) | − 1.13 (− 1.16, − 1.09)* | 5405.94 (3575.53, 7588.10) | 3838.39 (2502.17, 5384.86) | − 1.14 (− 1.18, − 1.10)* |
| 55–59 years | 4742.28 (3251.53, 6588.97) | 3154.85 (2152.44, 4328.83) | − 1.38 (− 1.47, − 1.30)* | 7569.70 (5332.93, 10,260.47) | 5466.38 (3838.07, 7428.50) | − 1.11 (− 1.15, − 1.06)* | 6087.59 (4232.46, 8317.05) | 4305.17 (3006.00, 5863.10) | − 1.17 (− 1.19, − 1.15)* |
| 60–64 years | 5979.87 (4068.35, 8107.83) | 3517.70 (2390.10, 4757.40) | − 1.79 (− 2.07, − 1.52)* | 8377.27 (5847.32, 11,209.26) | 6222.30 (4309.57, 8341.60) | − 1.00 (− 1.03, − 0.97)* | 7142.27 (4940.25, 9627.37) | 4836.59 (3345.26, 4863.59) | − 1.33 (− 1.40, − 1.25)* |
| 65–69 years | 7347.07 (4960.24, 9966.51) | 3791.30 (2513.88, 5329.35) | − 2.25 (− 2.46, − 2.04)* | 9027.18 (6194.13, 12,115.05) | 6725.33 (4583.22, 9114.37) | − 0.99 (− 1.01, − 0.96)* | 8201.14 (5587.23, 11,131.08) | 5285.19 (3576.85, 7215.29) | − 1.49 (− 1.65, − 1.32)* |
| 70–74 years | 7974.52 (5656.88, 10,927.16) | 4158.84 (2903.48, 5777.82) | − 2.33 (− 2.66, − 2.00)* | 9291.78 (6572.54, 12,676.28) | 6781.88 (4751.90, 9279.78) | − 1.05 (− 1.07, − 1.02)* | 8680.99 (6141.14, 11,857.37) | 5503.25 (7562.44, 3849.33) | − 1.58 (− 1.71, − 1.45)* |
| 75–79 years | 8863.27 (5943.62, 12,078.44) | 5529.27 (3601.47, 7707.21) | − 1.67 (− 1.89, − 1.46)* | 10,228.33 (6914.91, 14,107.07) | 7664.55 (5129.60, 10,482.36) | − 0.97 (− 1.02, − 0.91)* | 9640.88 (6485.92, 13,148.58) | 6653.18 (4447.83, 9146.88) | − 1.27 (− 1.36, − 1.19)* |
| 80–84 years | 9562.76 (6547.33, 13,031.83) | 7047.78 (4726.16, 9689.63) | − 1.08 (− 1.21, − 0.95)* | 11,230.54 (7724.26, 15,213.56) | 8838.08 (5991.07, 12,058.38) | − 0.80 (− 0.84, − 0.76)* | 10,587.09 (7316.73, 14,384.46) | 8051.71 (5433.46, 11,021.77) | − 0.94 (− 0.98, − 0.90)* |
| 85–89 years | 8977.37 (6296.90, 12,016.95) | 7113.19 (4922.34, 9547.94) | − 0.82 (− 0.88, − 0.75)* | 11,117.40 (7932.10, 14,721.79) | 9176.20 (6416.95, 12,188.63) | − 0.64 (− 0.67, − 0.60)* | 10,449.74 (7402.15, 13,874.31) | 8453.92 (5899.94, 11,225.34) | − 0.71 (− 0.74, − 0.69)* |
| 90–94 years | 8605.68 (6283.79, 11,497.13) | 7015.78 (5078.38, 9405.61) | − 0.70 (− 0.73, − 0.66)* | 11,025.56 (8121.61, 14,597.50) | 9600.45 (7114.49, 12,787.95) | − 0.45 (− 0.48, − 0.42)* | 10,559.85 (7765.88, 13,993.46) | 9155.47 (6782.91, 12,186.91) | − 0.48 (− 0.53, − 0.42)* |
| NP | |||||||||
| ASIR | 701.86 (556.48, 888.59) | 705.36 (556.68, 888.37) | 0.02 (0.02, 0.02)* | 907.82 (717.61, 1162.61) | 917 (721.91, 1172.30) | 0.04 (0.04, 0.04)* | 800.68 (634.43, 1016.63) | 809.91 (641.89, 1028.61) | 0.04 (0.04, 0.04)* |
| 5–9 years | 51.63 (17.18, 111.06) | 51.10 (16.73, 108.05) | − 0.04 (− 0.04, − 0.03)* | 49.21 (16.27, 104.82) | 49.48 (15.89, 106.75) | 0.02 (0.02, 0.02)* | 50.47 (17.01, 107.89) | 50.36 (16.50, 106.94) | − 0.01 (− 0.01, − 0.01)* |
| 10–14 years | 172.06 (86.98, 314.31) | 173.53 (86.4, 312.36) | 0.03 (0.03, 0.03)* | 184.51 (88.71, 336.24) | 185.41 (88.76, 349.53) | 0.02 (0.02, 0.02)* | 178.09 (88.56, 324.78) | 178.97 (86.41, 329.84) | 0.02 (0.02, 0.02)* |
| 15–19 years | 279.58 (123.60, 526.69) | 284.51 (129.78, 520.68) | 0.06 (0.06, 0.07)* | 340.05 (152.09, 646.24) | 341.96 (151.79, 649.88) | 0.02 (0.02, 0.02)* | 308.99 (137.96, 579.52) | 311.30 (139.30, 573.60) | 0.03 (0.02, 0.03)* |
| 20–24 years | 440.84 (197.76, 889.84) | 435.29 (186.87, 853.16) | − 0.05 (− 0.05, − 0.04)* | 551.73 (246.44, 1074.63) | 551.48 (243.77, 1093.27) | − 0.00 (− 0.00, − 0.00)* | 495.04 (219.06, 1008.44) | 490.78 (215.85, 951.19) | − 0.03 (− 0.04, − 0.02)* |
| 25–29 years | 752.29 (322.18, 1460.18) | 703.23 (297.32, 1392.28) | − 0.24 (− 0.24, − 0.24)* | 950.65 (397.55, 1846.01) | 875.73 (390.77, 1688.37) | − 0.29 (− 0.31, − 0.26)* | 848.85 (359.81, 1651.78) | 787.93 (345.99, 1531.86) | − 0.26 (− 0.27, − 0.25)* |
| 30–34 years | 1037.70 (567.97, 1748.57) | 946.35 (514.05, 1576.68) | − 0.32 (− 0.32, − 0.32)* | 1323.30 (721.25, 2230.08) | 1184.20 (649.44, 1985.05) | − 0.39 (− 0.39, − 0.38)* | 1174.37 (651.24, 1938.51) | 1063.9 (584.43, 1761.88) | − 0.34 (− 0.35, − 0.34)* |
| 35–39 years | 1141.05 (460.76, 2089.30) | 1052.87 (412.04, 1979.75) | − 0.28 (− 0.30, − 0.26)* | 1480.50 (586.89, 2682.90) | 1389.10 (547.12, 2590.43) | − 0.22 (− 0.24, − 0.21)* | 1304.96 (523.28, 2337.19) | 1217.82 (477.48, 2245.36) | − 0.24 (− 0.26, − 0.23)* |
| 40–44 years | 1240 (593.09, 2114.82) | 1226.39 (577.20, 2101.92) | − 0.04 (− 0.04, − 0.03)* | 1744.92 (837.90, 2994.77) | 1763.48 (830.87, 3055.37) | 0.04 (0.04, 0.04)* | 1480.40 (709.53, 2533.17) | 1489.35 (705.46, 2573.01) | 0.02 (0.01, 0.03)* |
| 45–49 years | 1154.63 (448.01, 2015.12) | 1228.41 (466.07, 2160.09) | 0.22 (0.20, 0.23)* | 1785.47 (695.35, 3052.58) | 1861.65 (766.18, 3158.64) | 0.15 (0.15, 0.15)* | 1452.55 (561.18, 2498.02) | 1539.02 (617.58, 2661.68) | 0.20 (0.19, 0.21)* |
| 50–54 years | 1116.08 (488.97, 2095.47) | 1241.94 (554.61, 2361.22) | 0.38 (0.38, 0.38)* | 1675.03 (783.79, 3194.28) | 1792.73 (815.22, 3336.99) | 0.24 (0.22, 0.27)* | 1379.14 (626.71, 2612.60) | 1516.06 (671.64, 2862.27) | 0.33 (0.29, 0.37)* |
| 55–59 years | 1297.53 (591.72, 2184.36) | 1413.31 (658.83, 2443.46) | 0.30 (0.30, 0.30)* | 1650.63 (730.53, 2871.83) | 1823.84 (812.20, 3163.84) | 0.35 (0.30, 0.41)* | 1465.54 (650.68, 2530.36) | 1617.61 (731.77, 2811.90) | 0.34 (0.33, 0.36)* |
| 60–64 years | 1354.09 (676.84, 2271.87) | 1429.25 (706.81, 2484.44) | 0.19 (0.18, 0.20)* | 1577.96 (761.52, 2766.41) | 1765.35 (838.19, 3107.18) | 0.39 (0.39, 0.39)* | 1462.64 (710.21, 2529.20) | 1596.51 (767.56, 2779.33) | 0.31 (0.29, 0.32)* |
| 65–69 years | 1348.84 (591.96, 2247.31) | 1410.42 (622.43, 2386.53) | 0.16 (0.15, 0.18)* | 1625.03 (696.73, 2714.50) | 1748.80 (743.38, 2868.89) | 0.26 (0.26, 0.26)* | 1489.24 (628.45, 2456.43) | 1582.71 (672.44, 2574.67) | 0.21 (0.21, 0.22)* |
| 70–74 years | 1340.98 (476.74, 2797.31) | 1676.76 (599.28, 3303.18) | 0.12 (0.11, 0.13)* | 1621.23 (584.09, 3324.51) | 1676.76 (599.28, 3303.18) | 0.12 (0.12, 0.12)* | 1491.29 (534.59, 3152.53) | 1535.54 (554.26, 3111.77) | 0.10 (0.09, 0.11)* |
| 75–79 years | 1202.31 (449.24, 2372.55) | 1202.58 (460.49, 2310.65) | 0.00 (− 0.01, 0.00) | 1339.05 (505.22, 2663.36) | 1393.50 (535.72, 2670.96) | 0.14 (0.13, 0.15)* | 1280.21 (490.94, 2568.26) | 1303.07 (505.64, 2508.97) | 0.06 (0.05, 0.07)* |
| 80–84 years | 1102.22 (491.31, 1963.38) | 1085.00 (436.45, 1951.75) | − 0.05 (− 0.06, − 0.05)* | 1096.41 (449.76, 1986.78) | 1136.51 (481.11, 1999.88) | 0.13 (0.12, 0.14)* | 1098.65 (466.97, 1946.64) | 1113.86 (465.59, 1946.21) | 0.05 (0.05, 0.06)* |
| 85–89 years | 986.08 (430.11, 1708.69) | 988.46 (435.08, 1691.66) | 0.01 (0.01, 0.01)* | 878.59 (367.83, 1547.10) | 891.73 (368.62, 1532.73) | 0.06 (0.04, 0.08)* | 912.12 (387.76, 1578.23) | 925.60 (392.58, 1601.01) | 0.06 (0.04, 0.07)* |
| 90–94 years | 873.71 (436.59, 1467.43) | 874.41 (448.18, 1486.98) | 0.00 (− 0.00, 0.01) | 675.81 (335.53, 1160.28) | 678.47 (321.00, 1141.20) | 0.02 (0.01, 0.03)* | 713.90 (356.50, 1206.12) | 712.20 (344.79, 1207.54) | − 0.03 (− 0.09, 0.03) |
UI uncertainty interval, CI confidence interval, ASIR age-standardized incidence rates, AAPC average annual percentage change
*Indicated the AAPC was significantly different from zero at the α = 0.05 level
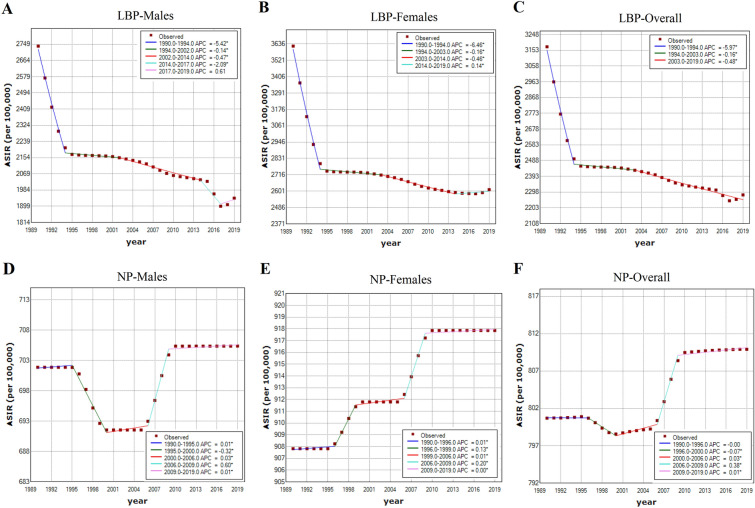
Joinpoint Regression Analysis
The AAPC of age-sex-specific rates of LBP and NP from 1990 to 2019 are presented in Table 1. From 1990 to 2019, the ASIR of LBP in China decreased by 1.17% (95% CI 1.07–1.27%) (Fig. 2A) in male subjects and 1.12% (95% CI 1.07–1.16%) (Fig. 2B) in female subjects. The ASIR of NP increased by 0.02% (95% CI 0.02–0.02%) (Fig. 2D) in male subjects and 0.04% (0.04–0.04%) (Fig. 2E) in female subjects. Except for the age groups 10–14 and 15–19 years in male subjects, a significant decrease in sex-specific incidence rates was observed in LBP in other age groups. Moreover, the incidence of AAPC for NP increased significantly after the group aged 45–49 years in men and the group aged 40–44 years in women, respectively.
Fig. 2.
Joinpoint regression analysis in sex-specific age-standardized incidence rates of low back and neck pain in China from 1990 to 2019. A low back pain in male subjects; B low back pain in female subjects; C low back pain in both sexes; D neck pain in male subjects; E neck pain in female subjects; F neck pain in both sexes. An asterisk indicates that the annual percentage change is statistically significantly different from zero at the α = 0.05 level
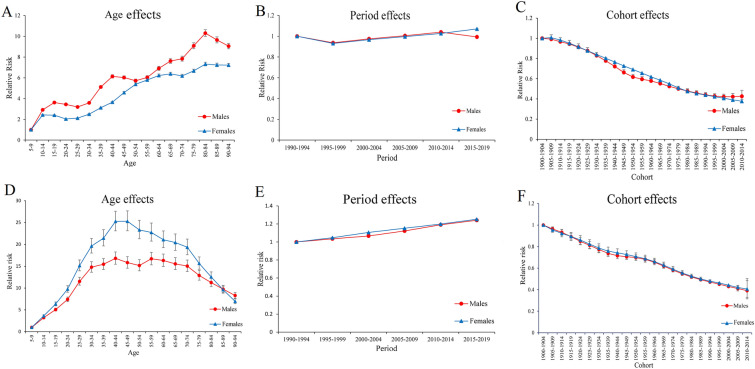
Age–Period–Cohort Analysis with the Intrinsic Estimator Method
The estimated RR of LBP incidence due to effects of age, period, and cohort are presented in Table 2. When the period and cohort effects were controlled, we found that the age effects were significantly related to the incidence of LBP among both male and female subjects (Fig. 3A). The age RR on LBP incidence showed an overall increasing trend among both male and female subjects, except for the subpeak for the group aged 40–44 years and group aged 80–84 years for male subjects. The highest RR of age effect were 10.31(95% CI 9.99–10.63) and 7.33 (95% CI 7.15–7.51) belonging to the group aged 80–84 years, for male and female subjects, respectively. Slight increments in RR due to period effects were observed in NP (Fig. 3B). For the period effect, the period RR in male subjects first decreased from 1990–1994 to 1995–1999, then slightly increased to 2010–2014 and finally decreased again. The period RR in female subjects first decreased from 1990–1994 to 1995–1999, then slightly increased to 2015–2019. From the cohort effects, the RR of LBP incidence continuously decreased in later birth cohorts in both men and women (Fig. 3C).
Table 2.
Sex-specific relative risks of low back pain in China due to effects of age, period, and cohort
| Factor | Incidence in male subjects | Incidence in female subjects | ||
|---|---|---|---|---|
| RR (95% CI) | P value | RR (95% CI) | P value | |
| Age | ||||
| 5–9 | 1 | 1 | ||
| 10–14 | 2.92 (2.87–2.97) | < 0.001 | 2.42 (2.39–2.45) | < 0.001 |
| 15–19 | 3.63 (3.55–3.70) | < 0.001 | 2.41 (2.38–2.44) | < 0.001 |
| 20–24 | 3.44 (3.37–3.51) | < 0.001 | 2.04 (2.01–2.06) | < 0.001 |
| 25–29 | 3.20 (3.14–3.26) | < 0.001 | 2.12 (2.09–2.14) | < 0.001 |
| 30–34 | 3.59 (3.52–3.67) | < 0.001 | 2.50 (2.47–2.54) | < 0.001 |
| 35–39 | 5.11 (5.00–5.24) | 0.005 | 3.12 (3.07–3.18) | < 0.001 |
| 40–44 | 6.13 (5.99–6.29) | < 0.001 | 3.66 (3.59–3.72) | < 0.001 |
| 45–49 | 6.03 (5.88–6.19) | < 0.001 | 4.58 (4.50–4.67) | < 0.001 |
| 50–54 | 5.72 (5.58–5.87) | < 0.001 | 5.38 (5.27–5.49) | < 0.001 |
| 55–59 | 6.04 (5.88–6.20) | < 0.001 | 5.80 (5.67–5.92) | < 0.001 |
| 60–64 | 6.91 (6.72–7.11) | < 0.001 | 6.23 (6.09–6.37) | < 0.001 |
| 65–69 | 7.62 (7.40–7.85) | < 0.001 | 6.38 (6.23–6.53) | < 0.001 |
| 70–74 | 7.84 (7.61–8.08) | < 0.001 | 6.19 (6.04–6.34) | < 0.001 |
| 75–79 | 9.08 (8.81–9.37) | < 0.001 | 6.67 (6.51–6.83) | < 0.001 |
| 80–84 | 10.31 (9.99–10.63) | < 0.001 | 7.33 (7.15–7.51) | < 0.001 |
| 85–89 | 9.65 (9.36–9.95) | < 0.001 | 7.24 (7.07–7.41) | < 0.001 |
| 90–94 | 9.05 (8.80–9.32) | < 0.001 | 7.23 (7.07–7.39) | < 0.001 |
| Period | ||||
| 1990–1994 | 1 | 1 | ||
| 1995–1999 | 0.94 (0.94–0.94) | < 0.001 | 0.93 (0.93–0.93) | < 0.001 |
| 2000–2004 | 0.97 (0.97–0.97) | < 0.001 | 0.97 (0.97–0.97) | < 0.001 |
| 2005–2009 | 1.00 (1.00–1.01) | < 0.001 | 1.00 (1.00–1.00) | 0.692 |
| 2010–2014 | 1.04 (1.04–1.04) | < 0.001 | 1.03 (1.03–1.03) | < 0.001 |
| 2015–2019 | 0.99 (0.99–0.99) | 0.555 | 1.07 (1.07–1.07) | < 0.001 |
| Cohort | ||||
| 1900–1904 | 1 | 1 | ||
| 1905–1909 | 0.99 (1.00–1.03) | < 0.001 | 1.01 (1.00–1.01) | < 0.001 |
| 1910–1914 | 0.97 (0.98–1.01) | < 0.001 | 0.98 (0.97–0.99) | < 0.001 |
| 1915–1919 | 0.94 (0.95–0.98) | < 0.001 | 0.95 (0.94–0.96) | < 0.001 |
| 1920–1924 | 0.91 (0.92–0.95) | < 0.001 | 0.92 (0.91–0.93) | < 0.001 |
| 1925–1929 | 0.88 (0.89–0.91) | < 0.001 | 0.88 (0.87–0.89) | < 0.001 |
| 1930–1934 | 0.83 (0.84–0.86) | < 0.001 | 0.84 (0.83–0.85) | < 0.001 |
| 1935–1939 | 0.78 (0.79–0.81) | < 0.001 | 0.80 (0.79–0.81) | < 0.001 |
| 1940–1944 | 0.72 (0.73–0.75) | < 0.001 | 0.76 (0.76–0.77) | < 0.001 |
| 1945–1949 | 0.66 (0.67–0.69) | < 0.001 | 0.73 (0.72–0.73) | < 0.001 |
| 1950–1954 | 0.62 (0.62–0.64) | 0.069 | 0.69 (0.69–0.70) | < 0.001 |
| 1955–1959 | 0.59 (0.60–0.62) | < 0.001 | 0.65 (0.65–0.66) | < 0.001 |
| 1960–1964 | 0.58 (0.58–0.60) | < 0.001 | 0.62 (0.62–0.62) | 0.001 |
| 1965–1969 | 0.55 (0.55–0.58) | < 0.001 | 0.58 (0.58–0.59) | < 0.001 |
| 1970–1974 | 0.52 (0.53–0.55) | < 0.001 | 0.55 (0.55–0.55) | < 0.001 |
| 1975–1979 | 0.50 (0.50–0.52) | < 0.001 | 0.51 (0.51–0.51) | < 0.001 |
| 1980–1984 | 0.48 (0.48–0.50) | < 0.001 | 0.47 (0.47–0.48) | < 0.001 |
| 1985–1989 | 0.46 (0.46–0.48) | < 0.001 | 0.45 (0.45–0.45) | < 0.001 |
| 1990–1994 | 0.44 (0.44–0.46) | < 0.001 | 0.44 (0.44–0.44) | < 0.001 |
| 1995–1999 | 0.43 (0.42–0.45) | < 0.001 | 0.42 (0.42–0.42) | < 0.001 |
| 2000–2004 | 0.42 (0.42–0.45) | < 0.001 | 0.41 (0.40–0.41) | < 0.001 |
| 2005–2009 | 0.42 (0.41–0.45) | < 0.001 | 0.39 (0.38–0.40) | < 0.001 |
| 2010–2014 | 0.43 (0.39–0.48) | < 0.001 | 0.38 (0.35–0.40) | < 0.001 |
| Deviance | 244.27 | 80.29 | ||
| AIC | 12.88 | 11.60 | ||
| BIC | − 55.39 | − 219.37 | ||
RR denotes the relative risk of low back pain incidence in particular age, period, or birth cohort relative to the average level of all ages, periods, or birth cohorts combined
RR relative risk, CI confidence interval, AIC Akaike information criterion, BIC Bayesian information criterion
Fig. 3.
Relative risks of the incidence of low back pain and neck pain in China from 1990 to 2019 due to effects of age, period, and cohort. A Age effects on low back pain; B period effects on low back pain; C cohort effects on low back pain; D age effects on neck pain; E period effects on neck pain; F cohort effects on neck pain
The estimated RR of NP incidence due to effects of age, period, and cohort are presented in Table 3. With regard to NP, the age RR revealed an inverted U-shaped pattern among both male and female subjects, with the highest risk of the age group 40–44 years and 45–49 years, for male and female subjects, respectively (Fig. 3D). The estimated period effect showed progressively increasing trends in male and female subjects during the entire period, indicating that the period effect significantly contributed to the increasing incidence of NP (Fig. 3E). Regarding the cohort effects, we also observed the RR of NP incidence continuously decreased in later birth cohorts, regardless of sex, which was similar to LBP (Fig. 3F).
Table 3.
Sex-specific relative risks of neck pain in China due to effects of age, period, and cohort
| Factor | Incidence in male subjects | Incidence in female subjects | ||
|---|---|---|---|---|
| RR (95% CI) | P value | RR (95% CI) | P value | |
| Age | ||||
| 5–9 | 1.00 | 1.00 | ||
| 10–14 | 3.22 (3.06–3.40) | < 0.001 | 3.62 (3.42–3.83) | < 0.001 |
| 15–19 | 5.06 (4.75–5.39) | < 0.001 | 6.36 (5.93–6.81) | < 0.001 |
| 20–24 | 7.40 (6.89–7.94) | < 0.001 | 9.75 (9.04–10.53) | < 0.001 |
| 25–29 | 11.52 (10.67–12.45) | < 0.001 | 15.14 (13.95–16.43) | < 0.001 |
| 30–34 | 14.78 (13.64–16.01) | < 0.001 | 19.62 (18.02–21.36) | < 0.001 |
| 35–39 | 15.44 (14.23–16.76) | < 0.001 | 21.43 (19.65–23.37) | < 0.001 |
| 40–44 | 16.80 (15.46–18.26) | < 0.001 | 25.27 (23.12–27.61) | < 0.001 |
| 45–49 | 15.83 (14.55–17.21) | < 0.001 | 25.30 (23.13–27.68) | < 0.001 |
| 50–54 | 15.17 (13.94–16.51) | < 0.001 | 23.31 (21.30–25.52) | < 0.001 |
| 55–59 | 16.70 (15.31–18.20) | < 0.001 | 22.73 (20.75–24.90) | < 0.001 |
| 60–64 | 16.31 (14.95–17.80) | < 0.001 | 21.07 (19.23–23.09) | < 0.001 |
| 65–69 | 15.53 (14.23–16.96) | < 0.001 | 20.43 (18.63–22.39) | < 0.001 |
| 70–74 | 15.03 (13.76–16.41) | < 0.001 | 19.35 (17.65–21.22) | < 0.001 |
| 75–79 | 12.89 (11.82–14.06) | < 0.001 | 15.64 (14.29–17.12) | < 0.001 |
| 80–84 | 11.26 (10.34–12.27) | < 0.001 | 12.54 (11.48–13.70) | 0.652 |
| 85–89 | 9.75 (8.97–10.60) | 0.125 | 9.60 (8.82–10.45) | < 0.001 |
| 90–94 | 8.29 (7.66–8.97) | < 0.001 | 6.95 (6.42–7.52) | < 0.001 |
| Period | ||||
| 1990–1994 | 1.00 | 1.00 | ||
| 1995–1999 | 1.03 (1.03–1.04) | < 0.001 | 1.05 (1.05–1.05) | < 0.001 |
| 2000–2004 | 1.07 (1.07–1.07) | < 0.001 | 1.11 (1.10–1.11) | 0.015 |
| 2005–2009 | 1.12 (1.12–1.12) | 0.039 | 1.15 (1.15–1.15) | < 0.001 |
| 2010–2014 | 1.19 (1.19–1.19) | < 0.001 | 1.20 (1.20–1.20) | < 0.001 |
| 2015–2019 | 1.24 (1.24–1.24) | < 0.001 | 1.25 (1.25–1.25) | < 0.001 |
| Cohort | ||||
| 1900–1904 | 1.00 | 1.00 | ||
| 1905–1909 | 0.96 (0.94–0.98) | < 0.001 | 0.95 (0.93–0.98) | < 0.001 |
| 1910–1914 | 0.93 (0.91–0.96) | < 0.001 | 0.92 (0.89–0.96) | < 0.001 |
| 1915–1919 | 0.89 (0.86–0.92) | < 0.001 | 0.89 (0.86–0.93) | < 0.001 |
| 1920–1924 | 0.85 (0.82–0.88) | < 0.001 | 0.86 (0.82–0.90) | < 0.001 |
| 1925–1929 | 0.81 (0.78–0.85) | < 0.001 | 0.82 (0.78–0.86) | < 0.001 |
| 1930–1934 | 0.77 (0.74–0.81) | < 0.001 | 0.79 (0.75–0.83) | < 0.001 |
| 1935–1939 | 0.74 (0.71–0.77) | < 0.001 | 0.76 (0.72–0.80) | < 0.001 |
| 1940–1944 | 0.72 (0.69–0.74) | < 0.001 | 0.74 (0.71–0.78) | < 0.001 |
| 1945–1949 | 0.71 (0.68–0.73) | < 0.001 | 0.73 (0.69–0.76) | < 0.001 |
| 1950–1954 | 0.70 (0.67–0.72) | < 0.001 | 0.71 (0.67–0.74) | < 0.001 |
| 1955–1959 | 0.68 (0.66–0.71) | < 0.001 | 0.69 (0.66–0.72) | < 0.001 |
| 1960–1964 | 0.65 (0.63–0.68) | 0.232 | 0.66 (0.63–0.69) | 0.338 |
| 1965–1969 | 0.62 (0.60–0.64) | 0.045 | 0.63 (0.60–0.66) | 0.024 |
| 1970–1974 | 0.58 (0.56–0.60) | < 0.001 | 0.59 (0.57–0.62) | < 0.001 |
| 1975–1979 | 0.55 (0.53–0.56) | < 0.001 | 0.55 (0.53–0.58) | < 0.001 |
| 1980–1984 | 0.52 (0.50–0.53) | < 0.001 | 0.52 (0.51–0.54) | < 0.001 |
| 1985–1989 | 0.49 (0.48–0.50) | < 0.001 | 0.50 (0.48–0.52) | < 0.001 |
| 1990–1994 | 0.47 (0.46–0.48) | < 0.001 | 0.48 (0.47–0.49) | < 0.001 |
| 1995–1999 | 0.45 (0.45–0.45) | < 0.001 | 0.46 (0.45–0.47) | < 0.001 |
| 2000–2004 | 0.43 (0.42–0.44) | < 0.001 | 0.44 (0.44–0.44) | < 0.001 |
| 2005–2009 | 0.41 (0.39–0.43) | < 0.001 | 0.42 (0.40–0.44) | < 0.001 |
| 2010–2014 | 0.39 (0.32–0.48) | 0.001 | 0.41 (0.33–0.50) | 0.001 |
| Deviance | 16.60 | 38.30 | ||
| AIC | 9.43 | 9.80 | ||
| BIC | − 283.05 | − 261.35 | ||
RR denotes the relative risk of neck pain incidence in particular age, period, or birth cohort relative to the average level of all ages, periods, or birth cohorts combined
RR relative risk, CI confidence interval, AIC Akaike information criterion, BIC Bayesian information criterion
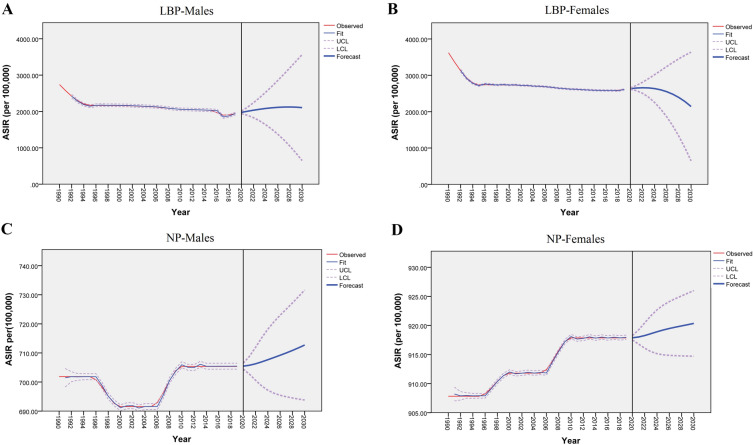
Result and Test of the Forecasting Model
The results of the ADF test of time series data for LBP in male and female subjects indicated that they were all non-stationary time series. Therefore, the time series of LBP needs to be differentiated to make them steady-state sequences. According to the results of the ADF test (by Unitroot-Ttest function), the incidences of LBP by taking second-order difference are stable sequences among both male and female subjects (male subjects, P < 0. 001; female subjects, P = 0.004). It revealed that d = 2 among both sexes. ACF and PACF were also used to estimate other parameters (Supplementary Figs. S1–S4). ARIMA (0, 2, 1) and ARIMA (1, 2, 1) are considered the optimal model for forecasting the trend of LBP incidence in male and female subjects, respectively. Model parameters are shown in Supplementary Tables S1–S2. The p values associated with the parameters are less than 0.05. The ACF and PACF plots of model residuals for male and female subjects (Supplementary Figs. S5–S6), combined with the Ljung–Box Q test (male subjects: χ2 = 1.62, df = 17, p = 1.00; female subjects: χ2 = 3.89, df = 16, p = 1.00), indicate that the residual sequences contain white noise. According to the ARIMA (0, 2, 1) and ARIMA (1, 2, 1) models, the fitted and predicted values are presented in Fig. 4. Moreover, the forecast results from 2020 to 2030 are shown in Table 4. From 2020 to 2030, the LBP incidence rates showed downward trends in female subjects. On the contrary, slight increments in male subjects are observed. According to the predicted results, the LBP incidence rates for male subjects would increase to 2106.15/per 100,000 in 2030. Meanwhile, the incidence for female subjects would decrease to 2141.86/per 100,000 in 2030.
Fig. 4.
Forecast of low back and neck pain incidence rates (per 100,000) from 2020–2030 through ARIMA. A Low back pain in male subjects; B low back pain in female subjects; C neck pain in male subjects; D neck pain in female subjects
Table 4.
Prediction of LBP incidence in China for the next 10 years according to ARIMA models with 95% confidence interval (per 100,000 population)
| Year | Male subjects | Female subjects | ||||
|---|---|---|---|---|---|---|
| ARIMA (0,2,1) | ARIMA (1,2,1) | |||||
| Forecast | Lower limit | Upper limit | Forecast | Lower limit | Upper limit | |
| 2020 | 1974.89 | 1938.05 | 2011.73 | 2633.36 | 2613.33 | 2653.39 |
| 2021 | 2006.18 | 1894.14 | 2118.22 | 2650.00 | 2578.17 | 2721.84 |
| 2022 | 2034.98 | 1827.37 | 2242.59 | 2657.55 | 2505.73 | 2809.37 |
| 2023 | 2060.70 | 1740.51 | 2380.89 | 2653.23 | 2396.41 | 2910.04 |
| 2024 | 2082.77 | 1635.19 | 2530.35 | 2634.91 | 2251.09 | 3018.72 |
| 2025 | 2100.61 | 1512.36 | 2688.85 | 2600.82 | 2070.53 | 3131.12 |
| 2026 | 2113.64 | 1372.59 | 2854.69 | 2549.41 | 1855.21 | 3243.61 |
| 2027 | 2121.29 | 1216.19 | 3026.39 | 2479.20 | 1605.29 | 3353.11 |
| 2028 | 2122.97 | 1043.30 | 3202.65 | 2388.79 | 1320.67 | 3456.90 |
| 2029 | 2118.12 | 853.94 | 3382.31 | 2276.79 | 1001.04 | 3552.54 |
| 2030 | 2106.15 | 648.04 | 3564.27 | 2141.86 | 645.90 | 3637.82 |
With regard to NP, the time series also need to be differentiated to make the data stable. According to the results of the ADF test (by Unitroot-Ttest function), the incidences of NP by taking second-order difference are stable sequences among both male and female subjects (male, P = 0. 001; female P = 0.001). It revealed that d = 1 among both sexes. The figures of ACF and PACF for NP in male and female subjects are shown in Supplementary Figs. S7–S10. ARIMA (3, 1, 0) and ARIMA (2, 1, 1) are considered the optimal models for forecasting the trend of NP incidence in male and female subjects, respectively. Model parameters are shown in Supplementary Tables S3–S4. Similarly, the p values associated with the parameters are less than 0.05. The ACF and PACF of residuals (Supplementary Figs. S11–S12), as well as the results of test of white noise, indicate that the residual sequences contain white noise among both sex (male: χ2 = 23.12, df = 15, p = 0.08; female: χ2 = 13.58, df = 15, p = 0.56). As shown in Fig. 4 and Table 5, the ARIMA (3,1,0) and the ARIMA (2,1,1) models are used to forecast the trend of NP incidence of male and female subjects from 2020 to 2030, respectively. From 2020 to 2030, the NP incidence rates show slight increments among both male and female subjects. The incidence for male subject is forecast to grow to 712.72/per 100,000 in 2030. Meanwhile, the incidence for female subjects is forecast to increase to 920.35/per 100,000 in 2030.
Table 5.
Prediction of NP incidence in China for the next 10 years according to ARIMA models with 95% confidence interval (per 100,000 population)
| Year | Male subjects | Female subjects | ||||
|---|---|---|---|---|---|---|
| ARIMA (3,1,0) | ARIMA (2,1,1) | |||||
| Forecast | Lower limit | Upper limit | Forecast | Lower limit | Upper limit | |
| 2020 | 705.46 | 704.43 | 706.49 | 917.88 | 917.49 | 918.26 |
| 2021 | 705.76 | 702.70 | 708.82 | 918.01 | 916.80 | 919.22 |
| 2022 | 706.27 | 700.60 | 711.94 | 918.26 | 916.08 | 920.45 |
| 2023 | 706.93 | 698.66 | 715.20 | 918.58 | 915.51 | 921.66 |
| 2024 | 707.67 | 697.17 | 718.16 | 918.91 | 915.14 | 922.68 |
| 2025 | 708.43 | 696.14 | 720.71 | 919.21 | 914.95 | 923.48 |
| 2026 | 709.20 | 695.45 | 722.95 | 919.48 | 914.85 | 924.10 |
| 2027 | 710.00 | 694.93 | 725.06 | 919.71 | 914.80 | 924.61 |
| 2028 | 710.84 | 694.51 | 727.18 | 919.92 | 914.77 | 925.07 |
| 2029 | 711.75 | 694.13 | 729.38 | 920.13 | 914.73 | 925.53 |
| 2030 | 712.72 | 693.81 | 731.63 | 920.35 | 914.70 | 926.00 |
Discussion
To our best knowledge, this is the first study to explore the long-term trends of spinal pain incidence in China from 1990 to 2019 using the age–period–cohort framework based on data from the GBD 2019 study. From 1990 to 2019, the ASIR of LBP decreased by an annual average of 1.16%, while the incidence of NP has slightly increased by 0.04%. In addition, a significant AAPC increase in the incidence rate for NP was observed in the group aged 45–85 years among both male and female subjects. Figure 1A shows that the point incidence of LBP sharply decreased from 1990 to 1995. However, since 1995, the decreasing rate of LBP incidence began to slow. There are some possible reasons for the phenomenon. First, in the past, the degree of automation and mechanization of industrial and agricultural production in China was relatively low, and it was mainly carried out by manual labor and manual operation, especially in the vast rural areas, where the intensity of manual labor was relatively high, resulting in a large number of patients with LBP caused by manual labor. With the reform and opening up policy in China, mechanization and automation have increased significantly, the Chinese population had increased income and paid more attention to health at that time, and many people prefer some light labor occupations. This may account for the rapid decline in the incidence of low back pain in China from 1990 to 1995. Second, with the development and transformation of China’s economy, the increasing proportion of the working-age population who spend most of their time in front of a computer and always sustained postures is contributing to the increased incidence of LBP and leading to a slower decrease in LBP incidence since 1995, although developments in athletics facilities contribute to LBP prevention. Therefore, there is a need to continue to increase investment in the prevention and treatment of LBP and NP. There are several possible reasons for the increased incidence of NP in China. First, risk factors for NP include obesity, sleep problems, lifestyle, psychosocial stress, work in awkward/sustained postures, and poor general health [17–19]; these risk factors are common in China currently and may account for the increased incidence rate in NP [8]. Second, Wu et al. found that economically developed provinces had higher NP prevalence in 2017 in China [10]. Thus, the increasing proportion of the working-age population who spend most of their time in office environments is also contributing to the increased incidence of NP [20]. Finally, along with the rise in electronic product use, potential risks for NP have also been reported, which may contribute to the increase in incidence [21].
The present study shows that the incidence of spinal pain in 2019 generally increased with age for both sexes. Although age- and sex-based patterns typically increased with age in the incidence of LBP and NP, they peaked in different age groups. As expected, the ASIR of LBP and NP in female subjects was higher than those in male subjects. Meanwhile, in all age groups, the incidence of NP and LBP was higher in female than in male subjects. This was consistent with previous studies [1, 2, 22, 23]. The exact cause of this phenomenon remains poorly understood. Several explanations may account for this sex disparity. First, biological factors of menstrual cycle fluctuations and hormonal factors may play an important role in the etiology and pathophysiology of various musculoskeletal degenerative diseases [24, 25]. Second, psychological factors of the higher sensitivity to pain among women and perceived greater willingness to report the painful symptoms may partly explain it [26]. These findings have important policy implications because women in China have a considerably longer life expectancy than men (male vs female, 74.5 years vs 79.9 years). Considering these factors, it is necessary to allocate more health resources to high-risk groups and develop realistic programs to reduce the burden of spinal pain.
Age is among the most important demographic factors for spinal pain. Age–period–cohort effect analysis showed a continuously increasing age effect for LBP incidence rates with increasing age among male and female subjects. There are several factors that may contribute to the age effect on LBP incidence. Intervertebral disc degeneration is one of the important risk factors for LBP, and its degeneration degree increases with age, which may directly explain the age pattern in a certain extent [27]. On the other hand, aging is associated with pain, and clustering of musculoskeletal pain with other pain conditions is also common, which may restrict physical activity, and further accelerate the deterioration of the musculoskeletal system [28]. This vicious cycle may explain the age pattern in an indirect way. The highest RR of NP due to age effects occurrence was observed in the group aged 40–49 years in female subjects, while in male subjects, it was observed in the group aged 40–44 years and 55–59 years. It indicates these populations are vulnerable groups for NP in China. This has direct implications for clinical practice and policy, as preventive and educational approaches targeting these specific groups should be encouraged.
The period effects for LBP incidence remained stable among both male and female subjects across 30 years, with little evidence of favorable period effects. Developments in athletics facilities coverage, increased awareness of health, and improved public health initiatives in LBP prevention are likely to have contributed to improvement over time. However, these gains may be largely offset by the current increasing economical and sociological pressure upon the people of China [22]. The period effects on NP incidence rates showed progressively increasing trends during the entire period, which suggests that the period effect is a vital factor for the increasing trends of disease burden of NP. This may be due to the faster pace of life as a result of economic development, societal modernization, and the Westernization of its lifestyle. Lifestyle factors have changed substantially in China, including lack of physical activity, greater work pressure, and daily use of the computer for extended periods. These changes may contribute to the occurrence of NP in a direct and indirect way. Recent studies have reported that psychosocial, anxiety, and depression are strongly correlated with the onset of NP [17, 29].
The cohort effects on the incidence rates of NP and LBP showed monotonously decreasing trends in 1900–1904 to 2010–2014 birth cohorts in both male and female subjects, which indicated that the population born in early birth cohorts had a higher risk relative to those born in later birth cohorts. The downward trends of cohort effects may be caused by economic development, environmental and education improvements. The poor environment, low socioeconomic level, and early childhood malnutrition may have profound adverse effects on health status, which will lead to a higher risk in adulthood. Low income is a risk factor for spinal pain and is associated with a poorer prognosis [30]. Barriers to accessing healthcare and diagnosis in lower-income countries may underestimate the incidence in these countries [31]. With the development of the socioeconomic and healthcare systems, later generations living in a better childhood environment have had better nutrition and awareness of physical activity and healthy dietary patterns, which will have played an important role in the lower risk of spinal pain.
The ARIMA model predicts that the incidence of LBP for female subjects in China will show a downward trend in the next 10 years. However, the incidence of LBP in male subjects shows an increasing trend based on predictive value estimates. This upward trend was also observed in the incidence of NP, regardless of sex. This study is the first to implement the ARIMA model to predict the incidence of spinal pain in China, so the results cannot be compared with previous studies. However, the actual incidence curve is thus far consistent with the predicted curve, and all the values were within the 95% confidence interval of the predicate value. Therefore, we can conclude that the selected models have an ideal fitting effect and can be used to predict the incidence of spinal pain in China in the next 10 years. The prediction results of the incidence trend suggest that the risk of spinal pain may be increasing. Although there is clear evidence that spinal pain is a long-term problem characterized by recurrent episodes, minimal attention has been paid to investigating effective strategies to prevent spinal pain [32–34]. Most studies have investigated interventions for spinal pain treatment, and few have examined prevention strategies for spinal pain [35, 36]. Recently, a high-quality systematic review with meta-analysis demonstrated that exercise alone and exercise in combination with education are effective in reducing the risk of low back pain episodes (35% and 45% risk reduction, respectively, at 1 year) [35]. It was reported in another review that exercise programs also seemed likely to prevent episodes of neck pain [37]. Overall, a greater understanding of effective strategies to prevent spinal pain is an important research priority.
The study has strengths. To our knowledge, this is the first study to investigate time trends in spinal pain incidence by gender in China. Second, the GBD 2019 uses uniform and standard methods in data analysis techniques to make these estimates comparable across time. Third, not only alteration during the entire period (assessed by AAPC) but also each segmental period (assessed by APC) was determined using the Joinpoint regression model. Furthermore, age–period–cohort analysis was performed to determine the contribution of spinal pain incidence related to particular periods, rather than the risk carried by a birth cohort. Lastly, use of the ARIMA model to predict the incidence of spinal pain in China is of great significance for further prevention and control.
Our study has some limitations. First, data sources in the present study were obtained from GBD 2019; the values were mainly derived from modeled data through the processes in DisMod-MR 2.1, rather than directly measured, resulting in an inevitable bias as described previously [4, 13]. However, many adjusted methods were used to reduce bias in GBD 2019, and the reliability of this source has been confirmed by previous literature and the IHME annual report. Second, the age–period–cohort analysis in this study was based on the estimated cross-sectional data of GBD from 1990 to 2019, which was not a cohort study. Moreover, the interpretation of results focuses on the population level rather than the individual level, which may result in ecological fallacies. Thus, large cohort studies are needed to determine the relative risks of specific locations and specific times. Third, based on GBD 2019, it is insufficient for spinal pain to focus only on LBP and NP. To properly address spinal pain, all spinal areas should be considered, including the upper back. Despite these limitations, this study is nevertheless the first one to comprehensively assess the incidence and trends of spinal pain in China. The results can serve as a baseline for relevant policies and follow-up studies.
Conclusions
Overall, the ASIR of LBP presented decreasing trends in China from 1990 to 2019, while the NP incidence slightly increased regardless of sex. The results of predicting that the relative burden caused by spinal pain will continue to increase in the next decade, which indicates the burden remains high. In addition, age effects showed substantially upward trends in LBP, and it peaked in the group aged 40–50 years in NP. Period effects showed that the risk of NP continuously increased with increasing time periods, but not in LBP. Therefore, spinal pain should be a priority for future research on prevention and therapy, especially critical as the aging population increases in China.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the GBD Collaborators who shared these publicly available data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Funding for the Rapid Service Fee was provided by the Department of Orthopedics, Guigang People’s Hospital.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors' Contributions
ZhaoLin Xie, LiZhang Chen, and JieHua Wei contributed to the conception and study design. JieHua Wei, LiZhang, Shengbin Huang, Ying Li, Jingmao Zheng, Zhilin Cheng contributed to acquisition of data, analysis and interpretation of data. JieHua Wei drafted the manuscript. ZhaoLin Xie, LiZhang, and JieHua Wei revised the article critically for important intellectual content and interpreted the results. All authors read and approved the final manuscript.
Disclosures
ZhaoLin Xie, LiZhang Chen, JieHua Wei, Shengbin Huang, Ying Li, Jingmao Zheng, and Zhilin Cheng have nothing to disclose.
Compliance with Ethics Guidelines
The review and approval were not required for this research by an institutional review board or ethics committee because this study used a public database with epidemiological data and the article was not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available in the GBD Data Tool repository (http://ghdx.healthdata.org/gbd-results-tool).
References
- 1.Chen S, Chen M, Wu X, et al. Global, regional and national burden of low back pain 1990–2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthopaed Transl. 2022;32:49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin Z, Wang D, Zhang H, et al. Incidence trend of five common musculoskeletal disorders from 1990 to 2017 at the global, regional and national level: results from the global burden of disease study 2017. Ann Rheum Dis. 2020;79(8):1014–22. [DOI] [PubMed] [Google Scholar]
- 3.Safiri S, Kolahi A, Hoy D, et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. 2020;368: m791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. [DOI] [PMC free article] [PubMed]
- 5.Briggs A, Cross M, Hoy D, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization world report on ageing and health. Gerontologist. 2016:56:S243–255. [DOI] [PubMed]
- 6.Hartvigsen J, Hancock M, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67. [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet. 2018;391(10137):2384–8. [DOI] [PubMed] [Google Scholar]
- 8.Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan X, Liu X, Shao H. Healthy China 2030: a vision for health care. Value Health Reg Issues. 2017;12:112–4. [DOI] [PubMed] [Google Scholar]
- 10.Wu A, Dong W, Zeng X, et al. Neck pain is the leading cause of disability burden in China: findings from the Global Burden of Disease Study 2017. Ann Transl Med. 2021;9(9):777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu A, Dong W, Liu S, et al. The prevalence and years lived with disability caused by low back pain in China, 1990 to 2016: findings from the global burden of disease study 2016. Pain. 2019;160(1):237–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu D, Wong P, Guo C, Tam L, Gu J. Pattern and trend of five major musculoskeletal disorders in China from 1990 to 2017: findings from the Global Burden of Disease Study 2017. BMC Med. 2021;19(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osmond C. Using age, period and cohort models to estimate future mortality rates. Int J Epidemiol. 1985;14(1):124–9. [DOI] [PubMed] [Google Scholar]
- 15.Clayton D, Schifflers E. Models for temporal variation in cancer rates. I: age-period and age-cohort models. Stat Med. 1987;6(4):449–67. [DOI] [PubMed] [Google Scholar]
- 16.Box GEP, Jenkins MG, Reinsel GC, Ljung GM. Time series analysis: forecasting and control. 5th edn. Hoboken: Wiley; 2015.
- 17.Kim R, Wiest C, Clark K, Cook C, Horn M. Identifying risk factors for first-episode neck pain: a systematic review. Musculoskelet Sci Pract. 2018;33:77–83. [DOI] [PubMed] [Google Scholar]
- 18.Kääriä S, Laaksonen M, Rahkonen O, Lahelma E, Leino-Arjas P. Risk factors of chronic neck pain: a prospective study among middle-aged employees. Eur J Pain. 2012;16(6):911–20. [DOI] [PubMed] [Google Scholar]
- 19.Ben Ayed H, Yaich S, Trigui M, et al. Prevalence, risk factors and outcomes of neck, shoulders and low-back pain in secondary-school children. J Res Health Sci. 2019;19(1): e00440. [PMC free article] [PubMed] [Google Scholar]
- 20.Ye S, Jing Q, Wei C, Lu J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: a cross-sectional study. BMJ Open. 2017;7(4): e014914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Puntumetakul R, Chatprem T, Saiklang P, Phadungkit S, Kamruecha W, Sae-Jung S. Prevalence and associated factors of clinical myelopathy signs in smartphone-using university students with neck pain. Int J Environ Res Public Health. 2022;19(8):4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang L, Ye H, Li Z, et al. Epidemiological trends of low back pain at the global, regional, and national levels. Eur Spine J. 2022;31(4):953–62. [DOI] [PubMed] [Google Scholar]
- 23.Clark P, Denova-Gutiérrez E, Razo C, Rios-Blancas M, Lozano R. The burden of musculoskeletal disorders in Mexico at national and state level, 1990–2016: estimates from the global burden of disease study 2016. Osteoporos Int. 2018;29(12):2745–60. [DOI] [PubMed] [Google Scholar]
- 24.Alpízar-Rodríguez D, Pluchino N, Canny G, Gabay C, Finckh A. The role of female hormonal factors in the development of rheumatoid arthritis. Rheumatology (Oxford). 2017;56(8):1254–63. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y. Menopause as a potential cause for higher prevalence of low back pain in women than in age-matched men. J Orthopaed Transl. 2017;8:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rollman G, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain. 2001;17(1):20–4. [DOI] [PubMed] [Google Scholar]
- 27.Lyu F, Cheung K, Zheng Z, Wang H, Sakai D, Leung V. IVD progenitor cells: a new horizon for understanding disc homeostasis and repair. Nat Rev Rheumatol. 2019;15(2):102–12. [DOI] [PubMed] [Google Scholar]
- 28.Blyth F, Noguchi N. Chronic musculoskeletal pain and its impact on older people. Best Pract Res Clin Rheumatol. 2017;31(2):160–8. [DOI] [PubMed] [Google Scholar]
- 29.Kazeminasab S, Nejadghaderi S, Amiri P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Genebra C, Maciel NM, Bento TPF, Simeão S, Vitta A. Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther. 2017;21(4):274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. 2007;23(12):2820–34. [DOI] [PubMed] [Google Scholar]
- 32.Da Silva T, Mills K, Brown BT, et al. Recurrence of low back pain is common: a prospective inception cohort study. J Physiother. 2019;65(3):159–65. [DOI] [PubMed] [Google Scholar]
- 33.Ailliet L, Rubinstein SM, Hoekstra T, van Tulder MW, de Vet HCW. Long-term trajectories of patients with neck pain and low back pain presenting to chiropractic care: a latent class growth analysis. Eur J Pain. 2018;22(1):103–13. [DOI] [PubMed] [Google Scholar]
- 34.Kongsted A, Kent P, Hestbaek L, Vach W. Patients with low back pain had distinct clinical course patterns that were typically neither complete recovery nor constant pain. A latent class analysis of longitudinal data. Spine J. 2015;15(5):885–94. [DOI] [PubMed] [Google Scholar]
- 35.Steffens D, Maher CG, Pereira LS, et al. Prevention of low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(2):199–208. [DOI] [PubMed] [Google Scholar]
- 36.De Campos TF, Elkins MR. Prevention of spinal pain. J Physiother. 2021;67(3):158–9. [DOI] [PubMed] [Google Scholar]
- 37.de Campos TF, Maher CG, Steffens D, Fuller JT, Hancock MJ. Exercise programs may be effective in preventing a new episode of neck pain: a systematic review and meta-analysis. J Physiother. 2018;64(3):159–65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available in the GBD Data Tool repository (http://ghdx.healthdata.org/gbd-results-tool).