Abstract
Background
We aimed to assess differences in health literacy between those who improved CPAP non‐adherent and those who remained non‐adherent.
Methods
We included patients newly diagnosed with sleep apnea syndrome who had started CPAP therapy between February 2019 and October 2020 with ≥6 follow‐up months or who self‐interrupted CPAP therapy <6 months. We recorded the CPAP wearing time after 3 and 6 months. Patients were divided into the CPAP adherent (using CPAP for ≥4 h per night) and non‐adherent (self‐interrupted CPAP therapy/using CPAP for <4 h per night) groups. We compared the European Health Literacy Survey Questionnaire 47 (HLS‐EU‐Q47) score between those who were CPAP non‐adherent after 3 months and become CPAP adherent after 6 months, and those who remained non‐adherent after 6 months.
Results
At 3 months, 34 patients were CPAP non‐adherent. After 6 months, there were 7 and 27 patients in the CPAP adherent and non‐adherent groups, respectively. There was a significant difference in the HLS‐EU‐Q47 score between the patients who became adherent to CPAP and who remained non‐adherent after 6 months.
Conclusion
Previously non‐adherent patients who subsequently became adherent tended to have higher health literacy.
Keywords: adherence, CPAP, health literacy, HLS‐EU‐Q47, SAS
This report is the first time to focus on health literacy and clarify the difference between patient with improve CPAP adherence and those who do not. Previously non‐adherent patients who subsequently became adherent tended to have higher health literacy.
![]()
1. INTRODUCTION
Sleep apnea syndrome is among the sleep‐related respiratory disorders characterized by repeat apnea, hypoxia, and respiratory effort‐related arousal during sleep. 1 The standard therapy for sleep apnea syndrome is continuous positive airway pressure (CPAP) therapy, which has been shown to improve daytime sleepiness, quality of life (QOL), 2 , 3 impaired glucose tolerance, hypertension, and cardiovascular events. 4 , 5 , 6 , 7 However, CPAP adherence can be problematic since some patients self‐interrupt CPAP usage or use it for a shorter‐than‐expected duration. 8 , 9
It has been suggested that only 30% to 80% of patients are CPAP adherent. 10 Factors associated with CPAP non‐adherence include mild severity of sleep apnea syndrome, mild subjective symptoms, depression, claustrophobia, and poor upper airway patency. 11 We do not have much problem for patients with good CPAP adherence, but not with poor CPAP adherence. Some patients with poor adherence to CPAP can improve later, 9 and few studies have examined the differences.
On the other hand, poor medication adherence and poor control of chronic diseases, including diabetes mellitus, are associated with poor health literacy. 12 , 13 , 14 , 15 Health literacy is defined as an individual's capacity to obtain, process, and understand basic health information and services required for appropriate health decisions. 16 There has been increasing attention on health literacy in the field of chronic disease management, with a report indicating that it is an important factor. 17
Health literacy can be categorized into three domains: health care, disease prevention, and health promotion. Some tools have been developed to comprehensively measure these domains of health literacy. 18 This includes the European Health Literacy Survey Questionnaire 47 (HLS‐EU‐Q47), 19 which was used in this study. We hypothesized that CPAP adherence is associated with health literacy and, therefore, aimed to examine the relationship between CPAP adherence and health literacy.
2. METHODS
This observational study was conducted according to the STROBE guidelines.
2.1. Participants
We included patients who visited the sleep apnea specialist outpatient department of X University Hospital between February 2019 and October 2020. Five sleep specialist physicians were in charge of managing the patients. The patients were newly diagnosed with sleep apnea syndrome and had started CPAP therapy, with ≥6 follow‐up months or self‐interruption of CPAP therapy <6 months.
Continuous positive airway pressure therapy indications were based on the Japanese insurance system; specifically, having symptoms such as daytime drowsiness and morning headache, ≥20 episodes of apnea, hypoxia, and respiratory effort–related arousal during sleep assessed by means of polysomnography (PSG; apnea–hypopnea index [AHI] ≥20) or having 40 episodes of apnea and hypoxia during sleep based on the out‐of‐center sleep test (AHI≥40). We used WatchPAT®; Philips Respironics Inc., PA, USA or SAS‐2100®; Teijin Pharma Ltd., Tokyo, Japan for out‐of‐center sleep test. We also used SLEEPMATE®10, SLEEPMATE®AirMini; Teijin Pharma Ltd., Tokyo, Japan, or DreamStation®; Philips Respironics Inc., PA, USA for CPAP.
We excluded patients who did not consent to study participation, did not answer the minimum number of required items on the HLS‐EU‐Q47, and those with the lowest or highest HLS‐EU‐Q47 score for all items.
Regarding sample size estimation, the Mann–Whitney U test (two‐sided test) was conducted using the HLS‐EU‐Q47 score, a confidence interval of 95%, and detection power of 0.8, with reference to a previous study on CPAP non‐adherent patients 9 , 10 as well as focus group discussions with experts and research teams. The required sample size was estimated as 31 patients.
2.2. CPAP adherence
We defined patients who were using CPAP for ≥4 h per night as CPAP adherent. 5 , 6 , 20 Contrastingly, we defined patients who self‐interrupted CPAP therapy or used CPAP for <4 h per night as CPAP non‐adherent. CPAP adherence was determined at 3 and 6 months after starting CPAP therapy, with the CPAP adherent and non‐adherent groups being defined at each time as the 3M adherent, 3M non‐adherent, 6M adherent, and 6M non‐adherent group. Moreover, the patients who were the 3M non‐adherent and improved to CPAP adherent at 6 months after starting CPAP therapy were defined as the 3M non‐adherent 6M adherent group. Those who were the 3M non‐adherent and still CPAP non‐adherent at 6 months after starting CPAP therapy were defined as the 3M non‐adherent 6M non‐adherent group.
In this study, we did not conduct any educational program for improving health literacy.
2.3. Data collection
The HLS‐EU‐Q47 was developed by the European Health Literacy Survey consortium and is comprised of 47 questions, including 16, 15, and 16 questions about health care literacy (HC‐HL), disease prevention health literacy (DP‐HL) and health promotion health literacy (HP‐HL), respectively. HC‐HL represents the ability to access, understand, evaluate and make informed decisions on medical issues and comply with medical advice. 19 DP‐HL is the ability to access, interpret and evaluate medical information and make informed decisions to protect against health risk factors. 19 HP‐HL represents the ability to regularly update oneself, interpret, evaluate and make informed decisions on health determinants in the social and physical environment and engage in joint action. 19
The Japanese version of the HLS‐EU‐Q47 was developed and validated as an appropriate tool to measure health literacy. All the questions had 5 answer options that were scored as follows: 1 = very easy, 2 = fairly easy, 3 = fairly difficult, 4 = very difficult, 5 = do not know/not applicable, which was considered as a missing value. 21
Based on previous literature, the minimum number of valid responses was 43 among 47 questions. 22 All the patients completed the self‐administered HLS‐EU‐Q47 at the first visit. Similar to the original scale, the scores were standardized on a metric between 0 and 50 based on the following formula 22 :
We compared the HLS‐EU‐Q47 score between the 3M non‐adherent 6M adherent group and the 3M non‐adherent 6M non‐adherent group.
We also compared the components of health literacy, including HC‐HL, DP‐HL, and HP‐HL. Moreover, we investigated factors which can be associated with CPAP adherence, including age; gender; height; weight; body mass index (BMI); smoking history; depressive mood; disinterest; claustrophobia; nose‐related diseases; difficulty falling asleep; sufficient sleeping time; AHI; Epworth Sleepiness Scale (ESS). Sleep latency of ≥30 min was considered long sleep latency, 23 while ≥6 sleeping hours was considered sufficient sleep time. 23
We additionally classified patients according to their HLS‐EU‐Q47 scores; “Excellent” for patients who scored HLS‐EU‐Q47 > 42, and “Inadequate” for patients who scored HLS‐EU‐Q47 < 25. 22 We compared CPAP using times per night for “Excellent” and “Inadequate” groups.
2.4. Statistical analysis
All statistical analyses were performed using SPSS Statistics for Windows 26.0 (IBM Corp., NY, USA). Statistical significance was set at p < 0.05. The Mann–Whitney U test (two‐sided test) was used for between‐group comparisons of the HLS‐EU‐Q47, HC‐HL, DP‐HL, and HP‐HL scores and between‐group comparisons of “Excellent” and “Inadequate.”
Moreover, Pearson's chi‐square test (two‐sided test) and the Mann–Whitney U test (two‐sided test) were used for between‐group comparisons of age; gender; height; weight; BMI; smoking history; depressive mood; disinterest; claustrophobia; nose‐related diseases; difficulty falling asleep; sufficient sleeping time; AHI; ESS. We used AHI regarding the severity of sleep apnea syndrome.
2.5. Ethical approvals
This study was approved by the ethics committee of X University Graduate School of Medicine. Before providing informed consent, the patients received an explanation of the research. This study was registered at UMIN Clinical Trials Registry (UMIN‐CRT) (UMIN000037793).
3. RESULTS
During the study period, 91 patients started CPAP therapy for the first time. We excluded nine patients who did not consent to study participation. Of the remaining 82 patients, we excluded 31 patients, of which 17 patients were transferred to other hospitals within 6 months, 11 patients did not answer the minimum number of the HLS‐EU‐Q47 items, and 3 patients received the lowest or highest score for all the HLS‐EU‐Q47 items (Figure 1). As a result of the remaining 51 patients, 17 patients were 3M adherent, and 34 patients were 3M non‐adherent. Among the 34 patients, 7 (20.6%) patients were changed to CPAP adherent after 6 months (the 3M non‐adherent 6M adherent group) and 27 (79.4%) patients were still CPAP non adherent after 6 months (the 3M non‐adherent 6M non‐adherent group), respectively.
FIGURE 1.
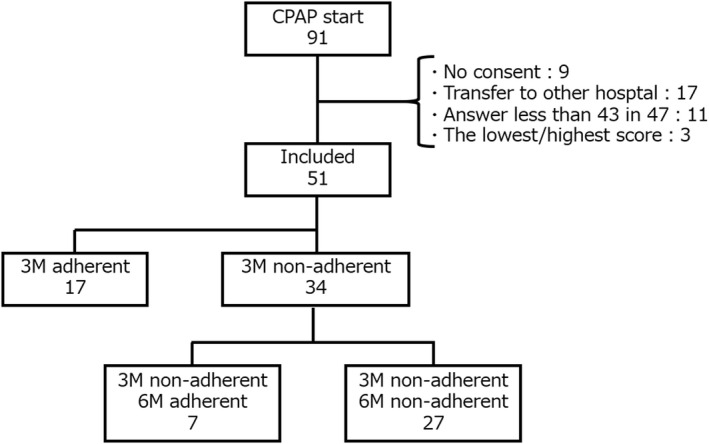
Study flowchart. Following the adherence of patients who started CPAP after 3 and 6 months. No consent: The patients who did not consent to study participation. Answer less than 43 in 47: The patients who did not answer the minimum number of items on the HLS‐EU‐Q47. The lowest/highest score: The patients who received the lowest or highest score for all the HLS‐EU‐Q47 items. CPAP: Continuous positive airway pressure, HLS‐EU‐Q47: European Health Literacy Survey Questionnaire 47, 3M adherent/3M non‐adherent: CPAP adherent/non‐adherent after 3 months, 3M non‐adherent 6M adherent/non‐adherent: CPAP non‐adherent after 3 months and CPAP adherent/non‐adherent after 6 months
There was significant difference in the HLS‐EU‐Q47 score between the 3M non‐adherent 6M adherent group and the 3M non‐adherent 6M non‐adherent group (45.4 vs. 33.6, respectively; p = 0.015). Moreover, there were significant between‐group differences in the score for HC‐HL (44.4 vs. 30.2; p = 0.002) and DP‐HL (48.9 vs. 36.7; p = 0.031), but there was no significant difference between the two groups in the score for HP‐HL (42.7 vs. 33.3; p = 0.054) (Table 1).
TABLE 1.
Comparison of the HLS‐EU‐Q47 score between the 3M non‐adherent 6M adherent group and the 3M non‐adherent 6M non‐adherent group
| 3M non‐adherent 6M adherent (n = 7) | 3M non‐adherent 6M non‐adherent (n = 27) | p‐value | |
|---|---|---|---|
| HLS‐EU‐Q47 a | 45.4 (39.2–48.2) | 33.6 (32.9–35.8) | 0.015* |
| HC‐HL a | 44.4 (41.7–45.2) | 30.2 (29.1–32.6) | 0.002* |
| DP‐HL a | 48.9 (42.2–50.0) | 36.7 (35.8–42.9) | 0.031* |
| HP‐HL a | 42.7 (33.9–49.5) | 33.3 (30.9–38.3) | 0.054 |
Note: 3M non‐adherent 6M adherent/non‐adherent: CPAP non‐adherent after 3 months and CPAP adherent/non‐adherent after 6 months.
Abbreviations: CPAP, continuous positive airway pressure; DP‐HL, disease prevention health literacy; HC‐HL, health care health literacy; HLS‐EU‐Q47, European Health Literacy Survey Questionnaire 47; HP‐HL, health promotion health literacy.
Median (1st and 3rd quartiles).
p < 0.05.
Among the factors associated with CPAP adherence, there was no significant difference between the two groups in age; gender; height; weight; BMI; smoking history; depressive mood; disinterest; claustrophobia; nose‐related diseases; difficulty falling asleep; sufficient sleeping time; ESS, excepting AHI (Table 2).
TABLE 2.
Comparison of clinical characteristics between patients in the 3M non‐adherent 6M adherent group and the 3M non‐adherent 6M non‐adherent group
| 3M non‐adherent 6M adherent (n = 7) | 3M non‐adherent 6M non‐adherent (n = 27) | p‐value | |
|---|---|---|---|
| Age, years a | 58.0 (53.0–67.0) | 57.0 (51.0–64.5) | 0.68 |
| Gender, M (%)/F (%) | 5 (71.4)/2 (28.6) | 21 (77.8)/6 (22.2) | 0.40 |
| Height, cm a | 172.0 (168.0–176.0) | 167.0 (164.0–172.5) | 0.34 |
| Weight, kg a | 88.0 (66.5–94.5) | 79.0 (69.9–88.0) | 0.68 |
| BMI, kg/m2 a | 29.5 (24.8–29.9) | 28.0 (25.7–31.8) | 0.90 |
| Smoking history, no (%) | 5 (71.4) | 13 (48.1) | 0.27 |
| Depressive mood, no (%) | 2 (28.6) | 8 (29.6) | 0.96 |
| Disinterest, no (%) | 1 (14.3) | 6 (22.2) | 0.52 |
| Claustrophobia, no (%) | 0 (0.0) | 2 (7.4) | 0.46 |
| Nose related disease, no (%) | 4 (57.1) | 8 (29.6) | 0.18 |
| Difficulty falling asleep, no (%) | 1 (14.3) | 9 (36.0) b | 0.27 |
| Sufficient sleep time, no (%) | 3 (42.9) | 18 (72.0) b | 0.15 |
| AHI a | 59.0 (48.1–62.4) | 42.0 (32.6–50.3) | 0.039* |
| ESS a | 7.0 (6.0–12.5) | 6.0 (5.0–9.0) b | 0.40 |
Note: 3M non‐adherent 6M adherent/non‐adherent: CPAP non‐adherent after 3 months and CPAP adherent/non‐adherent after 6 months.
Abbreviations: AHI, apnea–hypopnea index; BMI, body mass index; CPAP, continuous positive airway pressure; ESS, Epworth Sleepiness Scale.
Median (1st and 3rd quartiles).
2 missing values.
p < 0.05.
Among the 51 patients, 10 were “Excellent” and 6 were “Inadequate.” There was no significant difference in CPAP using the time between “Excellent” and “Inadequate” after 3 months (222.5 vs. 141.0 min, respectively; p = 0.093) and after 6 months (265.0 vs. 164.5 min, respectively; p = 0.378).
4. DISCUSSION
Among 3M non‐adherent patients, we observed a significant difference in health literacy and AHI between the patients who became adherent to CPAP and who remained non‐adherent after 6 months.
According to the past literature about making a questionnaire to predict CPAP adherence, three questions about health literacy were asked: “How often do you have someone help you read hospital materials?”, “How confident are you filling out medical forms by yourself?”, and “How often do you have problems learning about your medical condition because of difficulty understanding written information.” 24 , 25 Question 1 met the significance level and was included in the questionnaire. 24 The items related to reading comprehension of medical information were also included in HLS‐EU‐Q47, mainly in HC‐HL. 22 However, questions 2 and 3 are also related to reading comprehension, which suggests the difficulty of assessing health literacy with fewer questions. The HLS‐EU‐Q47 provides a comprehensive assessment of health literacy using 47 questions. No study has examined overall health literacy and CPAP adherence, which is considered a novelty of this study.
In the analysis of the HLS‐EU‐Q47 items, there were significant differences in the HC‐HL and DP‐HL score between the 3M non‐adherent 6M adherent group and the 3M non‐adherent 6M non‐adherent group. HC‐HL evaluates the acquisition, understanding, evaluation, and utilization of information in healthcare, which includes the ability to understand and follow the doctor's instructions. 22 Therefore, patients with a high HC‐HL score show improved CPAP adherence. DP‐HL evaluates the acquisition, understanding, evaluation, and utilization of information in disease prevention. 22 Treating sleep apnea syndrome with CPAP is known to decrease blood pressure and total cholesterol. 26 Therefore, patients with a high DP‐HL score show improved CPAP adherence. HP‐HL evaluates the acquisition, understanding, evaluation, and utilization of information in health promotion, which includes the ability to understand and utilize information that facilitates health promotion, including exercise and nutrition. 22 In this study, there was no significant difference in the HP‐HL. But the difference is expected to become significant as the number of cases increases, since treating sleep apnea syndrome can lead to better health.
It may appear that the percentage of CPAP adherent is low, but this is because patients who could not be followed up for 6 months, for reasons such as being transferred to another hospital, were not included. Most of these patients were stable; therefore, they were requested to be transferred to a neighboring hospital. These patients, who were likely to be in the CPAP adherent group if they continued to be followed up, were not included in the study. To support this theory, the majority of the excluded 31 patients used CPAP more than 4 h per night.
In this study, there was a significant difference between the two groups in AHI as well as health literacy. Since there is a literature suggesting an association between high AHI and CPAP adherence, 11 this is not a surprising result. There was no literature suggesting an association between high AHI and good health literacy; rather, poor health literacy has been suggested to increase the likelihood of sleep apnea syndrome. 27 Therefore, AHI is not a confounding factor of CPAP adherence and good health literacy.
This study has several limitations. First, we showed previously non‐adherent patients who subsequently became adherent tended to have higher health literacy in this study, but not the other way around. This means we did not show the patients with good health literacy are more likely to have improved adherence. Although the analysis comparing CPAP using the time between those with “Sufficient” and “Inadequate” health literacy showed no significant difference, those with “Sufficient” health literacy tended to use CPAP for a longer time. It might be a significant difference if the sample size were increased. Additionally, health literacy can be improved by education, 28 which may facilitate the ideal use of CPAP. Future research examining whether efforts to improve health literacy improve CPAP adherence is required. Second, this was a single‐center study in a university hospital; therefore, this study may not be representative of all patients with sleep apnea syndrome. A previous study reported that the average HLS‐EU‐Q47 score in Japan was 25.3, 21 which is lower than the HLS‐EU‐Q47 score in this study. Although few studies in Japan have investigated differences in CPAP adherence and health literacy between visiting hospitals, patients who visit university hospitals may have higher health literacy than those in other hospitals, assuming that one can willingly visit any hospital in Japan. Third, in this study, mask selection and pressure settings for CPAP therapy were at the discretion of each doctor. It was unrealistic to control this given the involvement of the patients' preference. Fourth, not all the patients in this study underwent PSG. Given the Japanese medical insurance system and prevalence of COVID‐19, CPAP may be introduced without PSG when the out‐of‐center sleep test meets the CPAP introduction criteria. Therefore, in this study, for patients who did not undergo PSG, the results of the out‐of‐center sleep test were used as the AHI. Fifth, the frequency of patient visits was not investigated. This may have been a bias because more frequent visits may have provided more opportunities for educational interventions for non‐adherence. Sixth, regarding the interpretation of the CPAP adherence in the present study, the burden of medical expenses for each patient was not considered. This aspect might have influenced the results, but in Japan, the burden of these medical expenses for each patient is generally $40‐50/month (patients, 30%, medical insurance support, 70%), and therefore it is unlikely that cost was a major factor in the CPAP adherence.
5. CONCLUSION
Among CPAP non‐adherent patients after 3 months, we observed a significant difference in health literacy between the patients who became adherent to CPAP and who remained non‐adherent after 6 months. Previously non‐adherent patients who subsequently became adherent tended to have higher health literacy.
CONFLICT OF INTEREST
There are no conflicts of interest to declare for either the lead author or co‐authors.
ACKNOWLEDGMENTS
None.
Li Y, Shikino K, Terada J, Katsumata Y, Kinouchi T, Koshikawa K, The relationship between CPAP and health literacy: A prospective observational study. J Gen Fam Med. 2022;23:370–375. 10.1002/jgf2.568
REFERENCES
- 1. American Academy of Sleep Medicine . International classification of sleep disorders—third edition (ICSD‐3). 3rd ed. Westchester, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2. Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta‐analysis. Arch Intern Med. 2003;163(5):565–71. [DOI] [PubMed] [Google Scholar]
- 3. McDaid C, Durée KH, Griffin SC, Weatherly HLA, Stradling JR, Davies RJO, et al. A systematic review of continuous positive airway pressure for obstructive sleep apnoea‐hypopnoea syndrome. Sleep Med Rev. 2009;13(6):427–36. [DOI] [PubMed] [Google Scholar]
- 4. Martínez‐Cerón E, Barquiel B, Bezos AM, Casitas R, Galera R, García‐Benito C, et al. Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes. A randomized clinical trial. Am J Respir Crit Care Med. 2016;194(4):476–85. [DOI] [PubMed] [Google Scholar]
- 5. Barbé F, Durán‐Cantolla J, Sánchez‐de‐la‐Torre M, Martínez‐Alonso M, Carmona C, Barceló A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161–8. [DOI] [PubMed] [Google Scholar]
- 6. Martínez‐García MA, Capote F, Campos‐Rodríguez F, Lloberes P, Díaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407–15. [DOI] [PubMed] [Google Scholar]
- 7. Barbé F, Durán‐Cantolla J, Capote F, de la Peña M, Chiner E, Masa JF, et al. Long‐term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;181(7):718–26. [DOI] [PubMed] [Google Scholar]
- 8. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnea: implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- 9. Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Somiah M, Taxin Z, Keating J, Mooney AM, Norman RG, Rapoport DM, et al. Sleep quality, short‐term and long‐term CPAP adherence. J Clin Sleep Med. 2012;8(5):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee YM, Yu HY, You MA, Son YJ. Impact of health literacy on medication adherence in older people with chronic disease. Collegian. 2017;24:11–8. [DOI] [PubMed] [Google Scholar]
- 13. Esen I, Demirci H, Güçlü M, Aktürk Esen S, Ersin ŞE. The relationship between health literacy, diabetic control, and disease‐specific complications in patients with type 1 diabetes mellitus. South Clin Istanb Eurasia. 2018;29(3):151–6. [Google Scholar]
- 14. Fernandez‐Silva MJ, Alonso‐Gonzalez A, Gonzalez‐Perez E, Gestal‐Otero JJ, Diaz GGJ. Health literacy in patients with type 2 diabetes: a cross‐sectional study using the HLS‐EU‐Q47 questionnaire. Sem Ther. 2019;45(1):30–6. [DOI] [PubMed] [Google Scholar]
- 15. Saeed H, Saleem Z, Naeem R, Shahzadi I, Islam M. Impact of health literacy on diabetes outcomes: a cross‐sectional study from Lahore. Pakistan Public Health. 2018;156:8–14. [DOI] [PubMed] [Google Scholar]
- 16. Nielsen‐Bohlman L, Panzer AM, Kindig DA. Health literacy: a prescription to end confusion. Washington (DC): National Academies Press(US); 2004. [PubMed] [Google Scholar]
- 17. Heinrich C. Health literacy: the sixth vital sign. J Am Acad Nurse Pract. 2012;24(4):218–23. [DOI] [PubMed] [Google Scholar]
- 18. Altin SV, Finke I, Kautz‐Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health. 2014;14:1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sørensen K, Van den Broucke S, Pelikan JM, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS‐EU‐Q). BMC Public Health. 2013;13(13):948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weaver TE, Maislin G, Dinges DF, Bloxham T, George CFP, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nakayama K, Aka W, Togari T, Ishikawa H, Yonekura Y, Sekido A, et al. Comprehensive health literacy in Japan is lower than in Europe: a validated Japanese‐language assessment of health literacy. BMC Public Health. 2015;23(15):505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. HLS‐EU Consortium . Comparative report on health literacy in eight EU member states. The European health literacy survey HLS‐EU (second revised and extended version). July 2014.
- 23. Billings ME, Rosen CL, Wang R, Auckley D, Benca R, Foldvary‐Schaefer N, et al. Is the relationship between race and continuous positive airway pressure adherence mediated by sleep duration? Sleep. 2013;36:221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sawyer AM, King TS, Hanlon A, Richards KC, Sweer L, Rizzo A, et al. Risk assessment for CPAP nonadherence in adults with newly‐diagnosed obstructive sleep apnea: preliminary testing of the index for nonadherence to PAP(I‐NAP). Sleep Breath. 2014;18(4):875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chew LD, Bradley KA, Boyko E. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94. [PubMed] [Google Scholar]
- 26. Sharma SK, Agrawal S, Damodaran D, Sreenivas V, Kadhiravan T, Lakshmy R, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med. 2011;365(24):2277–86. [DOI] [PubMed] [Google Scholar]
- 27. Li JJ, Appleton SL, Wittert GA, Vakulin A, McEvoy RD, Antic NA, et al. The relationship between functional health literacy and obstructive sleep apnea and its related risk factors and comorbidities in a population chohort of men. Sleep. 2014;37(3):571–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promot Int. 2018;33(5):901–11. [DOI] [PubMed] [Google Scholar]


