Summary
Objectives
During the worldwide COVID-19 pandemic, elective cardiac surgery was suspended to provide ICU beds for COVID-19 patients and those requiring urgent cardiac surgery. The aim of this study is to assess the effect of the pandemic on outcomes of patients awaiting elective cardiac surgery.
Design
A multi-centre prospective cohort study.
Setting
The elective adult cardiac surgery waiting list as of 1 March 2020 across seven UK cardiac surgical centres.
Participants
Patients on the elective adult cardiac surgery waiting list as of 1 March 2020 across seven UK cardiac surgical centres.
Main outcome measures
Primary outcome was surgery, percutaneous therapy or death at one year
Methods
Data were collected prospectively on patients on the elective adult cardiac surgery waiting list as of 1 March 2020 across seven UK cardiac surgical centres. Primary outcome was surgery, percutaneous therapy or death at one year. Demographic data and outcomes were obtained from local electronic records, anonymised and submitted securely to the lead centre for analysis.
Results
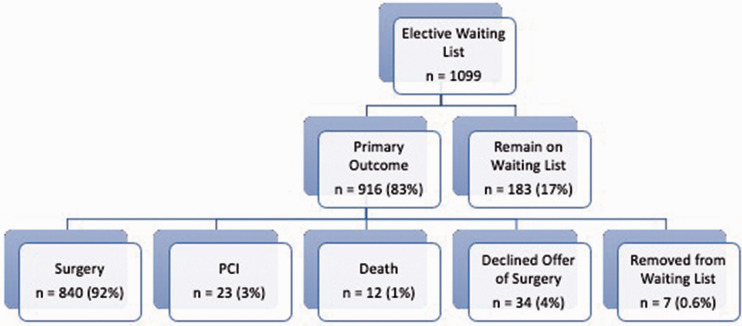
On 1 March 2020, there were 1099 patients on the elective waiting list for cardiac surgery. On 1 March 2021, 83% (n = 916) had met a primary outcome. Of these, 840 (92%) had surgery after a median of 195 (118–262) days on waiting list, 34 (3%) declined an offer of surgery, 23 (3%) had percutaneous intervention, 12 (1%) died, 7 (0.6%) were removed from the waiting list. The remainder of patients, 183 (17%) remained on the elective waiting list.
Conclusions
This study has shown, for the first time, significant delays to treatment of patients awaiting elective cardiac surgery. Although there was a low risk of mortality or urgent intervention, important unmeasured adverse outcomes such as quality of life or increased perioperative risk may be associated with prolonged waiting times.
Keywords: Cardiology and cardiovascular medicine, effectiveness of care, evidence based practice, ischaemic heart disease, valvar diseases
Objective
The National Health Service (NHS) is the publicly funded healthcare system in the United Kingdom (UK), providing both elective and emergency care to the population. Elective cardiac surgery is provided at specialist centres across the country, with a government-mandated target of all patients receiving surgery within 18 weeks of referral. 1 Patients are prioritised based on urgency. However, there are regional variations in time to operation.
Adverse events can occur while patients await cardiac surgery, with long waiting times, previously the norm in many countries. 2 Patients requiring coronary artery bypass graft surgery (CABG), the most common procedure performed, have a death rate of 1.1 per 1000 patient weeks. 3
During the worldwide coronavirus (COVID-19) pandemic, elective cardiac surgery in the UK was suspended to provide intensive care unit (ICU) beds for COVID-19 patients and those requiring urgent cardiac surgery. The outcomes of cardiac surgery in patients who develop COVID-19 infection in the perioperative period are poor and, therefore, given the low risk of elective surgery, strict screening protocols and COVID-19 protective measures were required before resumption of elective operating. 4,5 This led to significant delays in treatment; however, the extent and effect of this on morbidity and mortality are unknown.
The aim of this study was to assess the effect of the pandemic on outcomes of patients awaiting elective cardiac surgery.
Methods
Patient population
All cardiac surgery centres in the UK were invited to collaborate. The patient cohort for this study was all adult patients on the elective waiting list for cardiac surgery as a snapshot on 1 March 2020. Exclusions were age <18 years, those added after 1 March 2020, those awaiting transplantation and mechanical device therapy. Demographic data were collected from locally maintained electronic patient data records.
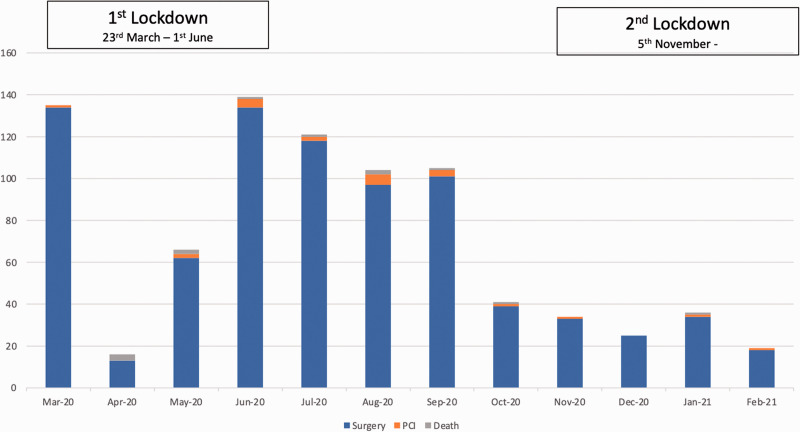
A global health emergency was declared by the World Health Organization on 31 January 2020. On 23 March 2020, the UK government announced a national lockdown. This was eased from 1 June 2020 with local lockdowns introduced by city. A second national lockdown came into force on 5 November with limited easing through December 2020 prior to a further lockdown on 6 January 2021.
Patient and public involvement
Approval was obtained from the clinical effectiveness unit at the lead trust (Barts Health NHS Trust; clinical effectiveness unit ID 11120). All patients in this study had their cases reviewed and were contacted by the clinical teams during the COVID-19 pandemic. Patient and public involvement was not carried out in the design of this study which was expedited to capture the cohort at the peak of the COVID-19 pandemic. Results will be discussed with patients.
Data transfer and storage
The anonymised dataset from each centre was transferred via an Amazon Web Service portal to the lead centre for analysis. Submission is secure, using HTTPS/SSL protocols. Each centre was allocated a user login, restricted only to the uploading of data files to the bucket. Access to download and archive of the submitted files into a designated archive sub-folder was restricted to the St Bartholomew’s research team only.
Outcomes and analysis
Primary outcome was cardiac surgery, percutaneous intervention or death as determined by local electronic patient records. Outcomes were determined on 1 March 2021. Results are presented as mean (± standard deviation) for normally distributed variables and median (1st–3rd quartile) for non-parametric data. The study was approved by local clinical effectiveness units.
Results
On 1 March 2020, there were 1099 patients on the elective waiting list for cardiac surgery at seven cardiac surgery centres in the UK. This represents a quarter of cardiac surgery centres in the country. Median age was 65 years (56–75 years) and 772 (70%) were male. The median time from being added to the waiting list until inclusion in the study on 1 March 2020 was 47 days (18–93 days). The operations awaited were CABG (n = 415), valve (n = 254), CABG + valve (n = 164), aortovascular (n = 117), congenital (n = 59) and other (n = 90).
One-year outcomes
One-year outcomes are shown in Figure 1. Overall, 916 (83%) patients met a primary outcome. In total, 840 (92% of those meeting an outcome) underwent surgery, 34 (3% of outcomes) declined an offer of surgery, 23 (2%) had percutaneous intervention, 12 (1%) died and 7 (0.6%) were removed from the waiting list. A total of 183 (17% of the total study population) remained on the elective waiting list.
Figure 1.
Outcomes of patients on elective waiting list on 1 March 2021.
Time to operation in the 840 patients who received surgery was 195 days (118–262 days), as shown in Table 1. They had been on the list for 45 days (18–90 days) prior to 1 March 2020. Median age was 66 years (56–74 years) and 592 (70%) were male. Procedures were CABG (n = 361), valve (n = 211), CABG + valve (n = 127), aortovascular (n = 101), congenital (n = 10) and other (n = 30).
Table 1.
Outcomes of those waiting elective surgery on 1 March 2020.
| No. of patients | Median (Q1–Q3) age (years) | Male | Median (Q1–Q3) time on waiting list at 1 March 2020 (days) | Median (Q1–Q3) time to outcome (days) | |
|---|---|---|---|---|---|
| Surgery | 840 | 66 (56–74) | 592 | 45 (18–90) | 195 (118–262) |
| Declined surgery | 34 | 61 (54–69) | 24 | 105 (68–133) | n/a |
| Percutaneous intervention | 23 | 75 (71–76) | 14 | 46 (27–65) | 230 (149–264) |
| Died | 12 | 76 (74–80) | 10 | 93 (135) | 458 (392–527) |
| Remained on waiting list | 183 | 65 (53–73) | 129 | 54 (20–118) | 419 (385–483) |
| Removed from waiting list | 7 | 73 (66–77) | 3 | 72 (19–117) | n/a |
In the 23 patients (3%) who underwent percutaneous intervention, the median age was 75 years (71–76 years) and 14 (61%) were male. Time to intervention was 230 days (149–264 days). Interventions were percutaneous coronary intervention (PCI) (n = 8), transcatheter aortic valve intervention (TAVI) (n = 11), balloon aortic valvuloplasty (BAV) (n = 2), Mitraclip (n = 1) and thoracic endovascular aortic repair (TEVAR) (n = 1). Of these, 17 were elective, 4 were urgent (PCI [n = 2], TAVI [n = 1] and BAV [n = 1]). Two were emergency (PCI [n = 1] and balloon aortic valvuloplasty [n = 1]). Timings of the elective cases were March/April/May (n = 2), June/July/August (n = 8), September/October/November (n = 4) and December/January/February (n = 2).
Twelve patients (1%) died without intervention at a median 458 days (392–527 days) since being added to the waiting list. Median age was 76 years (74–80 years) and 10 (83%) were male. The cause of death in these patients is unknown.
Seven patients were removed from the waiting list. Median age was 73 years (66–77 years) and 3 (43%) were male. They had been on the waiting list for median 72 days (19–117 days) at the start of this study. Five were awaiting valve surgery, one CABG and one major aortic. The reason for their removal is unknown.
As of 1 March 2021, 183 (17%) patients who were already on the waiting list a year earlier on 1 March 2020, remained on the elective waiting list for cardiac surgical intervention. Median age was 65 years (53–73 years) and 129 (70%) were male. Their median wait at this time was 419 days (385–483 days). They had already been on the list for a median of 54 days (20–118 days) prior to 1 March 2020. Planned procedures were CABG (n = 35), valve (n = 66), CABG + valve (n = 17), aortovascular (n = 17), congenital (n = 31) and other (n = 17).
Urgency of intervention
There were 38 patients who underwent non-elective interventions. Of these, 35 (92%) were urgent and 3 (8%) were emergency. Of the urgent interventions, 31 underwent surgery and four had percutaneous intervention at a median wait of 149 days (112–201 days). Surgical procedures were CABG (n = 8), valve (n = 13), aortovascular (n = 4), CABG +valve (n = 4) and other (n = 2), while percutaneous were BAV (n = 1), TAVI (n = 1) and PCI (n = 2). Median age was 58 years (46–73 years) and 21 were male. Emergency interventions were aortovascular surgery in one patient after 109 days wait, BAV 191 days and percutaneous coronary intervention 133 days.
Time to surgery
In those patients undergoing surgery, mean time to intervention was 195 days (118–262 days). Figure 2 shows the number of surgical procedures performed per month over the year. As can be seen, there is an initial significant drop in April due to the national lockdown, which then gradually returns to higher levels over two months.
Figure 2.
Outcomes by month, showing surgery, percutaneous intervention or death for patients on the elective waiting list on 1 March 2021.
Discussion
The COVID-19 pandemic has had a dramatic and significant impact on healthcare systems across the world. 6 The pandemic has caused significant morbidity and mortality to the general population while placing a massive strain on healthcare resources. The GlobalSurg collaborative showed that, in multiple surgical specialties, the outcomes of those undergoing surgery with COVID-19 infection were significantly poorer than those without. 7 In the UK, this was also shown in patients undergoing cardiac surgery. 8
This is the first study to assess the effect of the COVID-19 pandemic on patients on the waiting list for elective cardiac surgery. Many cardiac ICUs were requisitioned and their staff redeployed for the care of COVID-19 patients. Elective surgical operations were consequently postponed. In addition, there were concerns regarding outcomes in those with COVID-19 infection undergoing surgery, and surgeons were reticent to proceed with operations for non-life threatening cardiac conditions where the risks of COVID infection were peaking in the community. The impact of this on patients awaiting surgery is unknown as one indirect, adverse consequence of the pandemic could include patients having poorer than expected outcomes, despite not contracting the virus. With multiple waves of the pandemic expected to interrupt healthcare, a measure of such adverse events is vital in planning for responses to future surges.
Multiple solutions to maintain urgent cardiac surgery during the pandemic have been suggested. In the UK, several regional systems have been employed such as the Pan London Emergency Cardiac Surgery service. 5 Simultaneously a review of the records of all patients on the waiting list was performed, based on the Royal College of Surgeon classification. This takes into account symptomatic and prognostic benefit providing a standardised national prioritisation. On this basis, urgent outpatient operations were gradually reintroduced throughout the country as resources became available. Proposed strategies to maintain elective cardiac surgery include dedicated standalone centres providing regional elective cardiac surgery or ring-fenced beds within each individual unit. This was reliant on there being sufficient capacity in terms of beds and staff to maintain any service at all.
This study has shown that at five months into the pandemic, around half of patients were still waiting for surgery and 13% of this cohort of patients remained on the waiting list at one-year follow-up. The number of patients in this study being operated on recovered rapidly after the initial lockdown in April 2020 and then gradually fell after six months. During this time, surgical capacity was near normal; therefore, these results suggest that some other factor may be influencing the delay in surgery.
There were 16 patients from the original cohort who underwent elective percutaneous intervention over the study duration. The timing of this was spread throughout the follow-up and not particularly during the initial peak of COVID-19. Therefore, although it is possible that patients were diverted to reduce the surgical waiting list, it seems more likely that these patients were identified during review of the waiting list that percutaneous therapy might be more appropriate or that their clinical condition may have changed on review prior to surgery. This cohort represented the existing patients on the waiting list at the beginning of the pandemic and as additional patients were accumulating over the study period, these too will need to have been prioritised. Patient aversion to attending hospital as a result of the pandemic meant that the incidence of delayed presentations and higher risk patients was increased, and these may have affected timing and nature of treatment for the stable patients on the elective waiting list, particularly those who were already deemed to have been stable to wait.
Although not in our original protocol, we have identified a small but significant cohort of patients who had been offered, but declined, surgery. The cause for this is unclear but likely to include concerns about breaking isolation and the risk of contracting COVID-19 during their hospital stay.
We have shown a 1% mortality for patients waiting for elective cardiac surgery during the pandemic. There are no contemporary studies to allow comparison and there also are very few historic studies. Waiting lists are generally maintained at a local hospital level and not shared widely, making such publications rare. Furthermore, the granularity of data limits the information that can be gleaned from such studies. A 2019 study from a public health hospital in Brazil of 274 patients awaiting CABG showed a mean wait of 143 days with a mortality of 11.3% at a mean of 338 days (17–995 days) wait. 9 Both mortality and time-to-surgery were much higher than would be expected or accepted in a UK setting, particularly outside of a pandemic. National policy indicates that from the point of referral, patients should wait no longer than 18 weeks (i.e. 126 days) for non-urgent hospital treatments. A systematic review on mortality awaiting elective cardiac surgery that included 22 studies and 66,410 patients estimated 1.1 deaths per 1000 patients wait weeks. 3 Our study compares favourably with this. These studies show a similar trend to ours in that patients who died on the waiting list had generally been waiting longer. This may reflect the natural history of severe cardiovascular disease but may also be a surrogate for disease complexity. We should, however, not be reassured by these results, as there are likely to be significant unmeasured adverse outcomes associated with prolonged waits for surgery. These include increased anxiety, reduced quality of life, loss of earning or increase perioperative risk. Further waves of the pandemic could significantly increase wait times which may manifest in greater mortality.
There are two main limitations to the study. First, our data represent only a proportion of centres across the country and there may be variation in data and outcomes across centres. Reporting bias for centres with the most encouraging return to normal service may have skewed the data. It is possible that some centres were affected disproportionately by disruption to service, increasing or decreasing the waiting times. Furthermore, there is no uniform practice for how each centre prioritised patients and a lack of clarity on decision making for individual cases. This may have influenced timing of operation or decision to delay surgery or move to percutaneous therapy.
Conclusion
This study has shown, for the first time, significant delays to treatment of patients awaiting elective cardiac surgery. Although there was a low risk of mortality or urgent intervention, at one year, important unmeasured adverse outcomes such as quality of life or increased perioperative risk may be associated with prolonged waiting times.
Acknowledgements
The authors thank Giovanni Mariscalco, University Hospital Leicester, Anne Gregg, Frances Bleeks, Paul Gibson and Tina Glennon Royal Victoria Hospital Belfast, Alex Cale Hull and East Yorkshire NHS Trust, Tracey Smailes, James Cook University Hospital, Middlesbrough, Catherine Von Oppell and Mabel Phillips, University Hospital of Wales, Cardiff for data collection and supervision at individual sites.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethics approval
Approval was obtained from the Clinical Effectiveness Unit at the lead trust (Barts Health NHS Trust; Clinical effectiveness unit ID 11120).
Guarantor
MTY.
Contributorship
Martin T Yates – concept, design, data collection, analysis, writing, review of manuscript, responsible for overall content; Damian Balmforth – concept, design, data collection, review of manuscript; Bilal H Kirmani – data collection, review of manuscript; Metesh Acharya – data collection, review of manuscript; Reuben Jeganathan – data collection, review of manuscript; Dumbor Ngaage – data collection, review of manuscript; Mayzar Kanani – data collection, review of manuscript; Indu Deglurkar – data collection, review of manuscript; Ana Lopez-Marco – concept, design, review of manuscript; Julie Sanders – concept, design, review of manuscript; Aung Ye Oo – concept, design, review of manuscript, responsible for overall content.
Provenance
Not commissioned; peer-reviewed by Jullien Gaer and Julie Morris.
ORCID iD
Martin T Yates https://orcid.org/0000-0003-2313-2244
References
- 1.Lewis R, Appleby J. Can the English NHS meet the 18-week waiting list target? J R Soc Med 2006; 99: 10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plomp J, Redekop WK, Dekker FW, et al. On the waiting list for cardiac surgery in The Netherlands in 1994 and 1995: multicenter study. Heart 1999; 81: 593–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Head SJ, da Costa BR, Beumer B, et al. Adverse events while awaiting myocardial revascularization: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2017; 52: 206–217. [DOI] [PubMed] [Google Scholar]
- 4.Yates MT, Balmforth D, Lopez-Marco A, Uppal R, Oo A. Outcomes of patients diagnosed with COVID-19 in the early postoperative period following cardiac surgery. Interactive J Caridothoracic Surg 2020; 31: 483–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain A, Balmforth D, Yates MT, et al. The Pan London Emergency Cardiac Surgery service: coordinating a response to the COVID-19 pandemic. J Card Surg 2020; 35: 1563–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonalumi G, di Mauro M, Garatti A, et al. The COVID-19 outbreak and its impact on hospitals in Italy: the model of cardiac surgery. Eur J Cardiothorac Surg 2020; 57: 1025–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-COV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanders J, Akowuah E, Cooper J, et al. Cardiac surgery outcomes during the COVID-19 pandemic: a retrospective review of the early experience in nine UK centres. J Cardiothoracic Surg 2021; 16: 43–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.da Fonseca VBP, De Lorenzo A, Tura BR, Pittella FJM, da Rocha ASC. Mortality and morbidity of patients on the waiting list for coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg 2018; 26: 34–40. [DOI] [PubMed] [Google Scholar]