Abstract
Background
An increasing number of children, adolescents and adults with intellectual disabilities and/or autism are being admitted to general psychiatric wards and cared for by general psychiatrists.
Aims
The aim of this systematic review was to consider the likely effectiveness of in-patient treatment for this population, and compare and contrast differing models of in-patient care.
Method
A systematic search was completed to identify papers where authors had reported data about the effectiveness of in-patient admissions with reference to one of three domains: treatment effect (e.g. length of stay, clinical outcome, readmission), patient safety (e.g. restrictive practices) and patient experience (e.g. patient or family satisfaction). Where possible, outcomes associated with admission were considered further within the context of differing models of in-patient care (e.g. specialist in-patient services versus general mental health in-patient services).
Results
A total of 106 studies were included and there was evidence that improvements in mental health, social functioning, behaviour and forensic risk were associated with in-patient admission. There were two main models of in-patient psychiatric care described within the literature: admission to a specialist intellectual disability or general mental health in-patient service. Patients admitted to specialist intellectual disability in-patient services had greater complexity, but there were additional benefits, including fewer out-of-area discharges and lower seclusion rates.
Conclusions
There was evidence that admission to in-patient services was associated with improvements in mental health for this population. There was some evidence indicating better outcomes for those admitted to specialist services.
Keywords: Intellectual disability, neurodevelopmental disorders, autism spectrum disorders, psychiatric in-patient treatment, mental health, hospital
People with intellectual and other developmental disabilities, such as autism, have an increased prevalence of mental health problems relative to the general population,1,2,3,4,5,6,7,8 and governments of some countries, such as England, have pledged to reduce admissions to in-patient psychiatric settings for this population. The launch of a national service model for people with intellectual disabilities and/or autism in England shifted focus toward increasing community-based provision within a national programme of in-patient bed closure.9,10 However, in England at the end of June 2021, there were 2075 in-patients with intellectual disabilities occupying beds specifically commissioned for this group, and 57% of them had a length of stay of over 2 years; more broadly, in other mental health beds, there were 1040 people with intellectual disabilities admitted during June 2021, and a total of 3600 in-patients with intellectual disabilities were in these types of beds.11 There is a push to ensure that in-patient services implement the most effective treatment service model, bearing in mind that despite the recognised high cost of in-patient admission, there is a lack of substantial evidence about the effectiveness of these services for this group.12,13,14,15
Aims of the review
The aim of this review was to undertake a systematic search of the available literature about in-patient mental healthcare for individuals with intellectual disabilities and/or autism who have additional mental health, behavioural or forensic needs. The specific aims were to (a) consider and describe the different models of service provision, and (b) evaluate the outcomes from admission across the three domains of treatment effectiveness, patient safety and patient experience.
Method
A series of electronic database searches were completed, with the final search being completed on 1 March 2021, using PsycINFO, Medline, PubMed and CINHAL. A grey literature search was also conducted on OpenGrey (http://www.opengrey.eu). The complete search terms are found in Table 1. Backward searching of publications that met our eligibility criteria was used to identify any further eligible papers. EPPI Reviewer software (Version 4 for Windows; EPPI-Centre, UCL Social Science Research Institute, University College London, UK; https://eppi.ioe.ac.uk/cms/)16 was used to collate the results, and once duplicates were removed, the titles and abstracts were screened against the eligibility criteria (Table 1). Papers that described admission to an in-patient psychiatric service via accident and emergency services were included. No date limit was applied to the searches, and studies involving children, adolescents and adults were included. Title and abstract screening, as well as full-text reviews, were completed by two authors. This systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO; identifier CRD42019136568) before the searches and review had been completed.
Table 1.
Search terms and eligibility criteria
Broad search terms
| |
| Example search string (((‘intellect* disab*’ or ‘learn* disab*’ or ‘developmental disab*’ or ‘developmental disorder’ or ‘mental retard*’ or ‘mental handicap*’ or ‘mental impair*’ or ‘mental subnormal*’ or autis* or Asperger* or asd or ASD or pdd or ‘pervasive developmental disorder’ or ‘developmental delay’) AND (‘hospital*’ or ‘unit’ or ‘facilit*’ or ‘service’ or secur*) AND (‘forensic’ or ‘mental illness’ or ‘mental health’)) AND (treat* or interven* or therap* or program* or outcome or effect* or ‘patient admission’ or intake or re-admission or discharg* or pathway) NOT (biomarkers or plasticity or stroke or cerebrovascular or accident or cva or cerebral or vascular or event or cve or ‘transient or ischaemic attack’ or tia or ‘perceived devaluation and discrimination scale’ or ‘copy number variation’))). | |
| Inclusion criteria | Exclusion criteria |
|
|
|
|
|
|
|
|
|
|
Eligible studies were initially classified by methodology to ascertain the size and quality of the evidence base available, to address the aims of the review and explore in-patient treatment. Studies were then categorised according to patient population (adult or child/adolescent) and in-patient service type (general mental health (GMH), specialist intellectual disabilities or forensic/secure service), to allow for consideration and description of current models of in-patient care. Because of the variability across studies and the large amount of extracted data, a data science approach was used to collect/clean, investigate, analyse and visualise the results, using Python Version 3.7 for Windows, distributed as part of Anaconda3 (Austin, TX, USA; https://www.anaconda.com). Twenty-five of the included studies comprised a sample already included in another study; for example, the authors reported a further follow-up study of a previous sample or were a review that included studies identified in our search. To avoid double-counting, data from these papers were not extracted and were only included in the synthesis if they added new information (e.g. an additional outcome measure or reporting on a specific patient group, such as those with intellectual disabilities and personality disorders). Studies excluded and the associated reason is detailed within Supplementary Table 1 available at https://doi.org/10.1192/bjo.2022.571. Quality appraisal methods were considered, but not used. The reasons for this were first that there was marked heterogeneity in research designs across the included studies, and synthesising information using a single or several tools, using different rating scales, would have added additional complexity to an already complex synthesis and make comparisons challenging. Second, considering that most of the included studies used observational designs, drawing on convenience samples, issues associated with bias are generally ostensible. Where sources of bias were apparent, these were identified and included within our synthesis to help facilitate the interpretation of evidence.
Studies were organised by outcome from admission across three domains. These domains were adopted from the UK Department of Health's Transparency in Outcomes Framework.9 We used three of the four domains for assessing quality: measures of effectiveness, patient safety and patient experience of the National Health Service (NHS). The fourth domain, efficiency (concerning value for money), was not included as part of this review as data were not available. This framework was used to organise findings, including any potential difference in outcomes between the models of care, and was developed for public health services. Similar service quality indicators are found internationally.17,18,19,20 According to each of the three domains, specific outcomes were identified within the included studies (e.g. clinical assessment within the effectiveness domain, observation levels within the safety domain and quality of life within the patient experience domain). The specific outcomes selected to evaluate in-patient treatment were informed by existing research,21,22 and developed to be consistent across quality frameworks. This was done to ensure as much of the available literature was captured by the framework, and findings regarding treatment outcomes were recorded and organised using key indicators associated with admission outcomes. Eligible studies were categorised by the broad domain, and then further categorised by specific outcomes investigated.
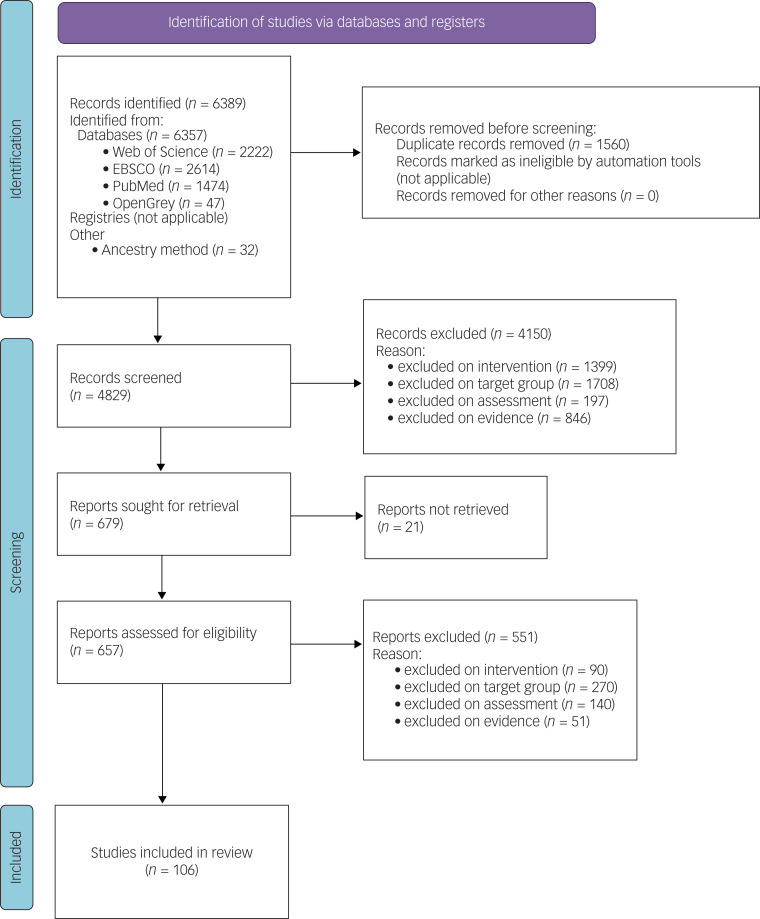
As shown by the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) diagram (Fig. 1), 4829 potential studies remained after the removal of duplicates, with 4150 studies excluded following title and abstract screening. Six-hundred and fifty-seven articles were included in the full-text review and, following further exclusions, 106 studies met the eligibility criteria and were incorporated in the synthesis. All studies included in the review can be found in Supplementary Table 2, along with a summary of their findings.
Fig. 1.
Diagram of systematic search results and screening process.
Results
The majority of eligible studies were published within the past 30 years, with most involving children and young people taking place more recently. Of the studies that focused on adults, there were eight published in the 1990s, 28 published in the 2000s, 40 published in the 2010s and nine published in the 2020s. Of the studies that focused on children, none were published in the 1990s, one was published in the 2000s, 14 were published in the 2010s and six were published in the 2020s. Eighty-five studies included samples of adults, whereas 21 studies included samples of children and adolescents, both with intellectual disabilities and/or autism. Studies ranged in size from small samples of fewer than ten participants with qualitative research methodologies,23 to large-scale studies using population or census records and healthcare databases.24,25 The majority of studies were conducted in the UK, Scandinavia and Canada; however, a smaller number of studies took place in other European countries, Asia and Australia.26,27,28,29,30,31,32,33
Methodologically, most studies lacked appropriate comparison samples or did not collect data prospectively at intervals (data collection periods ranged from 1 month to over 10 years, with a median of 36 months), and instead were cross-sectional and observational, describing a single group of participants (Table 2). For studies that included a comparison group, there was variability in the amount of detail provided, with some specifying sampling strategies or matching criteria34 and others providing little information.35 For retrospective studies, many were case file reviews, but were considered valuable because important clinical information was reported that highlighted the care pathways of patients. There was a single clinical trial.36
Table 2.
The number of eligible studies by type of design, and the data capture intervals used
| Study design methodology | Number of studies (%) |
|---|---|
| Retrospective case note, chart or file review | 50 (47.17) |
| Audit, case register or census data analysis | 19 (17.92) |
| Cross-sectional | 15 (14.15) |
| Mixed methods | 10 (9.43) |
| Literature review | 4 (3.77) |
| Prospective comparative or evaluation study | 3 (2.83) |
| Systematic review | 2 (1.87) |
| Qualitative data collection | 2 (1.87) |
| Controlled trial | 1 (0.94) |
| Data capture time intervals | |
| <1 month | 1 (1.33) |
| 1–6 months | 4 (5.33) |
| 6–12 months | 9 (12.0) |
| 1–3 years | 22 (29.33) |
| 3–5 years | 9 (12.0) |
| 5–10 years | 18 (24.0) |
| ≥10 years | 7 (9.33) |
The studies about in-patient care for adults characterised three different in-patient services or unit types: 22 studies focused on GMH in-patient services, 38 studies focused on specialist in-patient intellectual disability services and 25 studies focused on forensic/secure services (both GMH and specialist intellectual disabilities services). The literature about the in-patient treatment of children and adolescents was sparse, but included 14 studies about GMH and/or specialist intellectual disabilities services, as well as seven studies about admissions via other services (i.e. accident and emergency departments because of crisis associated with mental health or behaviour that challenges, which resulted in admission or transfer to a service for in-patient psychiatric treatment) (Supplementary Table 2).
Participants
Twenty-four papers included duplicate or potentially duplicate participants (such as subsamples of a larger population or a later follow-up study), reducing the total number of papers where data were extracted to 82. Not all of the 82 studies provided data that could be extracted. However, 16 studies included information about GMH in-patient services, 30 studies focused on specialist intellectual disability in-patient services and 17 studies were about forensic or secure in-patient services. Data were extracted from 13 studies about children and young people within either GMH or specialist intellectual disability in-patient services, and data were extracted from six studies about the admission of children or adolescents with intellectual disabilities and/or autism via accident and emergency departments (Supplementary Table 2).
Adults with intellectual disabilities and/or autism
The characteristics of adult participants were explored across the different in-patient service types. The participant data available within studies were variable, and reporting of age, ethnicity, gender, level of intellectual disability, Full-Scale IQ and detention status was inconsistent; most studies did not adequately describe their samples (Supplementary Table 2). For example, although 16 studies were about adults with intellectual disabilities and/or autism within GMH in-patient services, data about degree of intellectual disability was only reported in three studies. Adults with intellectual disabilities within GMH in-patient services tended to have mild-to-borderline intellectual disabilities and were a similar age as those without intellectual disabilities who used the same service. However, there was evidence that adults with severe-to-profound intellectual disabilities were admitted to GMH in-patient services, but were more frequently admitted to specialist in-patient intellectual disability services (Supplementary Table 2, and Table 3).5,6,52
More males than females with intellectual disabilities and/or autism were admitted to in-patient services, and this was most notable for patients with autism, children and adolescents, and those admitted to forensic services (Table 3). A greater percentage of adults from Black and minority ethnic backgrounds with intellectual disabilities and/or autism were found among those admitted to GMH in-patient services, whereas a greater percentage of White adults with intellectual disabilities and/or autism were admitted to specialist intellectual disability in-patient services or forensic in-patient services. It was noted that for all services, adults from Black and ethnic minority backgrounds appeared to be overrepresented.
Table 3.
Participant characteristics as reported in studies where data were available
| Mean age in years (s.d.) [minimum, maximum] <number of studies reporting data> | Mean full-scale IQ (s.d.) [minimum, maximum] <number of studies reporting data> | % Severity of intellectual disabilities <number of studies reporting data> | % Male <number of studies reporting data> | % Ethnicity <number of studies reporting data> | |
|---|---|---|---|---|---|
| General mental health in-patient services | |||||
| Adults with intellectual disabilities and/or autism | 39.90 (12.52) [15.00–70.00] <2> |
Not reported | Mild: 70.62 <3> Moderate: 46.00 <3> Severe/profound: 11.10 <3> Borderline/none: 52.75 <2> |
70.86 <6> | White: 39.75 <2> BAME: 57.20 <1> |
| Adults without intellectual disabilities and/or autism | 39.16 (13.13) [not reported] <4> |
Not reported | Not applicable | 48.83 <4> | White: 49.55 <2> BAME: 65.00 <1> Other/unknown: 3.2 <1> |
| Specialist intellectual disability in-patient services | |||||
| Adults with intellectual disabilities and/or autism | 34.43 (9.01) [14.00–68.00] <19> |
64.00 (8.96) [46.00–84.00] <1> |
Mild: 68.69 <16> Moderate: 17.24 <12> Severe/profound: 20.67 <11> Borderline/none: 5.86 <4> Unspecified: 24.80 <2> |
72.98 <25> | White: 73.01 <7> BAME: 25.63 <5> Other/unknown: 7.03 <3> |
| Forensic/secure in-patient services | |||||
| Adults with intellectual disabilities and/or autism | 33.75 (11.52) [15.00–56.00] <11> |
62.25 (11.40) [44.00–84.00] <4> |
Mild: 54.03 <3> Moderate: 14.00 <4> Severe/profound: 0 <1> Borderline/none: 32.54 <2> Unspecified: 3.22 <2> |
76.54 <14> | White: 79.98 <3> BAME: 17.04 <3> Other/unknown: 2.90 <1> |
| Adults without intellectual disabilities and/or autism | 32.35 (11.52) [18.00–64.00] <3> |
Not reported | Not applicable | 82.83 <4> | Not reported |
| Children and young people in-patient services | |||||
| Children and young people with intellectual disabilities and/or autism | 12.64 (3.09) [1.00–21.00] <8> |
Not reported | Mild: 18.38 <1> Moderate: 21.45 <1> Severe/profound: 26.00 <1> Borderline/none: 9.20 <2> Unspecified: 9.20 <1> |
73.15 <9> | White: 70.60 <2> BAME: 40.00 <1> Other/unknown: 9.40 <2> |
| Children and young people without intellectual disabilities and/or autism | 14.40 (2.51) [1.00–21.00] <1> |
Not reported | Not applicable | 57.99 <1> | White: 39.00 <1> BAME: 58.00 <1> Other/unknown: 3.0 <1> |
| In-patients with autism | |||||
| Adults with autism | 32.27 (10.86) [17.00–52.00] <6> |
59.00 (not reported) [not reported] <1> |
Not reported | 95.93 <6> | Not reported |
| Children with autism | 12.25 (3.2) [1.00–18.00] <2> |
Not reported | 27.5% reported as having intellectual disabilities with level not specified | 95.01 <5> | White: 70.60 <2> BAME: 40.00 <1> Other/unknown: 9.40 <2> |
BAME, Black and minority ethnic.
Children and adolescents with intellectual disabilities and/or autism
Nineteen papers were identified that focused on children and adolescents with intellectual disabilities and/or autism, with the oldest included paper published in 2006. Children and adolescents with intellectual disabilities and/or autism tended to be younger than comparison samples without developmental disabilities (Table 3). However, these data were extracted from relatively few papers because, as with the adult literature, authors did not robustly describe their included participants.
Autism
Twenty-one papers focused specifically on in-patients with autism. Of these, seven reported data about participants with autism within a larger sample that included participants with intellectual disabilities,53 and data for these participants were extracted where possible, or were contained within previous literature reviews.54
Ten of the included studies involved adults with autism, with a single paper exploring this group within GMH in-patient services.55 Three studies investigated autism within specialist intellectual disability in-patient services35,56,57 and six were about adults with autism within forensic in-patient services, including one forensic service for patients with intellectual disabilities.53,54,58–60,83
Eleven of the included papers involved children and adolescents with autism. Six of these papers were about children and adolescents with autism, including those with intellectual disabilities, who were admitted via accident and emergency departments within general hospitals because of mental health crises and/or behaviour that challenges.25,61–65 A single follow-up paper66 reported on the same set of participants with autism within an earlier study,67 and to avoid double-counting, the data were not extracted and included Table 3.
Models of service provision
GMH and specialist intellectual disability in-patient service models of care for adults
The studies identified referred to two broad approaches to in-patient mental health for adults with intellectual disabilities and/or and autism: (a) admission to in-patient general psychiatric or mental health services (with other patients who do not have intellectual disabilities and/or autism)68 or (b) admission to in-patient specialist services designed for those with intellectual disabilities and/or autism.3
For adults with intellectual disabilities and/or autism in GMH in-patient services, it was noted that admission could be to GMH beds26,69 or ‘specialist intellectual disability beds’ located within an otherwise GMH service.2,5,8 Specialist beds within GMH services were typically described as a separate ward or unit,5 with a few authors reporting that staff within these services had specialist knowledge of intellectual disabilities or treatment and therapeutic programmes adapted for this group.8,70 Specialist intellectual disability services or units tended to be smaller, with reports of 6- or 14-bed units,1,7 compared with GMH services.71 It was noted that ‘specialist’ in this context was not clearly defined, but included reference to the training of staff and the adaptation of interventions to meet the needs of in-patients.
Both the GMH and specialist intellectual disability in-patient service models for adults were characterised by 24-h care and a ‘locked’ environment, although some patients were described as having free ‘access’ to the community, depending on the nature of their admission or detention status.5,72 Patients had access to psychiatry and nursing care, and frequently, a multidisciplinary team including nursing, psychologists and allied health professions, such as speech and language therapy and occupational therapy.73
Therapeutic and treatment services offered in GMH and specialist in-patient intellectual disability services included group and individual psychotherapy, medication, and behavioural and educational programmes. Further details regarding treatment components specifically for patients with intellectual disabilities were sparse, but were described more so within papers about specialist in-patient intellectual disability services rather than GMH in-patient services, and included staffing levels,74 staff training programmes or requirements,1,14 ratio of different types of nurses (those with training in intellectual disabilities versus mental health),1,3,73 patient/staff ratios4 and use/availability of ‘adapted’ treatment or therapeutic programmes.14 Those that did report such information were frequently pilot studies or retrospective case reviews of new service models; for example, enhanced out-patient services compared with in-patient treatment,75 or studies on early or new specialist intellectual disability in-patient services.2,5
Within studies, GMH and specialist intellectual disability in-patient services were described using different language, such as acute assessment and treatment,76 or services for ‘longer-stay’ patients.77 Some authors described the purpose for admission and the expected duration of stay, such as admission for assessment and treatment,78 or emergency care/admission with short stays.26
Details of ‘aftercare’ following discharge, including collaborative working with community services, were absent from much of adult literature. The impact of an enhanced community assessment and treatment team on in-patient admissions was evaluated within one study,75 although such an approach to evaluation appears to be the exception. Other groups of authors reported a poor availability of community placements that resulted in ‘bed-blocking’ and delayed discharges,73,79 and a single study referred to ‘telepsychiatric’ support for patients ‘discharged’ (resided in family home but still a ‘patient’) during the COVID-19 pandemic.33
No autism-specific service treatment models or service/unit types for adults were identified in the review.
Secure forensic service models of care for adults
Twenty-five papers illustrated that forensic services in the UK followed the same two broad treatment models – GMH (where services also treated those without intellectual disabilities and/or autism)27,54,58 and specialist in-patient services for those with intellectual disabilities87 – and covered levels 1 and 4 of the Royal College of Psychiatrists’22 tiered model of forensic provision for intellectual disabilities: low-, medium- and high-secure services, and ‘locked rehabilitation’ units. Studies from The Netherlands reported a similar tiered structure of forensic services,60,82,85 whereas within Canada, the use of forensic beds within a GMH model was described rather than the use of specialist in-patient provision.27,84 Six studies explored those detained within GMH forensic services, three of which focused on the admission of patients with autism to low-, medium- and high-secure units.37,58,60,82,84,85
As might be expected, GMH and specialist intellectual disability forensic services had an increased focus on security and increased restrictions on community access, but were otherwise comparable to other in-patient units in terms of the availability of care and treatment delivered by psychiatry, nursing and psychology.88,89 Fewer papers provided information such as staff/patient ratios or specialist training in intellectual disabilities or forensic mental health compared with studies about GMH or specialist intellectual disability in-patient services, although some offence-specific treatments were described.88
Service models of in-patient treatment for children and adolescents
In-patient service models for the treatment of children and adolescents with intellectual disabilities and/or autism were comparable to adult services, with admissions to two broad types of services: GMH28,33 or specialist intellectual disability services.90,91
Both GMH and specialist intellectual disability services for children and adolescents with intellectual disabilities and/or autism were described as ‘locked’, and 24-h care was provided by nurses, psychologists, psychiatrists and allied health professionals.28,92,93 Studies that included child and adolescent participants provided more information about staffing, service structure and approach than found within the adult literature, allowing for differentiation between GMH and specialist intellectual disabilities and/or autism in-patient services.94 For example, Smith and Berney93 described the differences between patient need within two ‘open’ wards with different levels of dependence based on severity of intellectual disabilities, and one low-secure ward within their specialist intellectual disabilities service; they described how these wards used focused behavioural and activities-based programmes more so than GMH units. Others focused on describing staff training programmes, and the care pathway for children and adolescents with autism.66,67,95
In-patient service models for children and young people, both GMH and specialist, attempted to integrate collaboration with community teams or ‘outreach programmes’ as part of treatment (more so than that seen in the adult literature). In-patient and community services were part of the same ‘team’ or ‘hub’, to directly reduce/avoid in-patient admission or readmission.66,92
Several papers were identified that explored the admission of children and adolescents with intellectual disabilities and/or autism to accident and emergency departments.30,62 Although not considered a model of in-patient psychiatric treatment, the authors of these papers reported that children and adolescents with intellectual disabilities and/or autism were more likely to visit or be admitted to a general hospital because of mental ill health compared with those without disabilities, often leading to further admission to in-patient psychiatric services.25,30,64 These findings highlight how accident and emergency is utilised by families and carers of children and adolescents with intellectual disabilities and/or autism, which is likely, at least in part, a result of the poor provision of community-based services for this group.
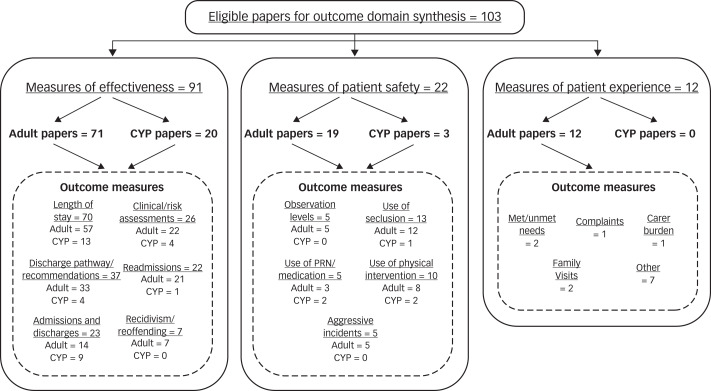
Outcomes associated with in-patient admission
Two narrative reviews15,96 and one systematic review54 were excluded to avoid double-counting. A total of 103 papers reported at least one outcome within one of the three outcome domains investigated: measures of effectiveness, measures of patient safety and measures of patient experience. A variety of outcome measures were used within each domain, and although reporting was variable, most outcome measures were classified as falling within the effectiveness domain (reported in 90 papers), with patient experience being the rarest outcome domain reported. The categorisation of papers according to outcome domain is found within Figure 2. Twenty-two studies (22%) reported outcomes that were categorised as falling within more than one domain. Across all studies, regardless of the type of service model, there was a focus on reporting data about length of stay and discharge pathway. Authors describing specialist in-patient services tended to report clinical and risk outcomes, whereas authors who focused on GMH in-patient services tended to report admission and discharge rates. Authors of studies about in-patient forensic services focused on measures of patient safety, behaviour that challenges and offending behaviour, including crime. It was notable that none of the included studies about GMH in-patient services reported information about the use of physical interventions, including seclusion. It was notable that there were relatively fewer studies that considered outcomes for children and adolescents with intellectual disabilities and/or autism following admission to in-patient settings.
Fig. 2.
A frequency count of the number of studies categorised according to one of three outcome domains: measures of effectiveness, measures of patient safety or measures of patient experience. The outcomes associated with in-patient admission reported within each study were also categorised. Length of stay was the most frequently reported outcome measure for children, adolescents and adults with intellectual disabilities and/or autism, followed by discharge and clinical or risk assessments for adult patients. CYP, children and young people.
GMH and specialist intellectual disability in-patient services for adults
Measures of effectiveness
There were 70 studies categorised as investigating measures of effectiveness within GMH and specialist intellectual disability in-patient services.
Length of stay
Thirty-nine studies reported information about length of stay within GMH and/or specialist intellectual disability in-patient services. Thirteen of these studies reported length-of-stay data for adults with intellectual disabilities and/or autism within GMH units only, with no comparison with data from specialist intellectual disability services.2,14,26,29,34,52,68,76,98–102 Eight of the 13 studies compared length-of-stay data for adults with and without intellectual disabilities and/or autism in GMH services,26,29,34,52,68,98,100,102 and five reported length-of-stay data for patients with intellectual disabilities and/or autism only.2,14,76,99,101 Three of the 13 studies reported medians,52,98,100 with nine reporting the mean. A single study reported a range for length-of-stay data and the mean or median could not be extracted102 The authors of all but two studies52,102 reported that adults with intellectual disabilities and/or autism had a longer length of stay compared with in-patients without intellectual disabilities and/or autism. The average in-patient stay within GMH in-patient services for those with intellectual disabilities and/or autism ranged from 29.40 days to substantially longer admissions of over 5 years.2,34 When length of stay was averaged across studies, the mean length of stay for those with intellectual disabilities and/or autism was substantially shorter within GMH in-patient services than the length of stay for those without intellectual disabilities and/or autism (Table 4). However, when in-patients without intellectual disabilities and/or autism who were classed as ‘long stay’ were excluded, the difference in length of stay between those with and without intellectual disabilities and/or autism within GMH in-patient services disappeared (Table 3). Examining the median length of stay as reported within studies52,98,100 also indicated that those with intellectual disabilities and/or autism had a shorter length of stay compared with patients without intellectual disabilities and/or autism within GMH in-patient services (Table 4).52,79
Table 4.
Mean and median length of stay for in-patients within general mental health and specialist intellectual disability in-patient services
| Mean length of stay in days (s.d.) [minimum, maximum] <number of studies reporting data> | Median length of stay in days (s.d.) [minimum, maximum] <number of studies reporting data> | |
|---|---|---|
| General mental health in-patient services | ||
| Adults with and without intellectual disabilities and/or autism | 679.05 (719.93) [8.60–1328.60] <4> n = 2646 | – |
| Adults with intellectual disabilities and/or autism | 552.71 (933.87) [29.40–2402.40] <6> n = 885 | 22.92 (11.66) [8.00–38.50] <6> n = 1163 |
| Adults without intellectual disabilities and/or autism | 3683.73 (5442.02) [22.00–9937.20] <3> n = 1892 | 45.75 (69.59) [8.00–150.00] <4> n = 519 |
| Excluding identified ‘long-stay’ patients | 557.72 (756.60) [22.00–1092.00] <2> n = 1866 | |
| Specialist intellectual disability in-patient services | 1240.39 (4114.28) [17.90–15 530.75] <14> n = 842 | 567.62 (723.95) [119.00–1820.00] <5> n = 508 |
| Adults with intellectual disabilities and/or autism | ||
| Excluding identified ‘long-stay’ patients | 141.13 (105.01) [17.90–385.20] <13> n = 779 | |
A further 26 studies reported length-of-stay data for adults with intellectual disabilities and/or autism in specialist in-patient intellectual disability services. Eleven studies explored length of stay within specialist intellectual disabilities services and/or GMH services, and comparisons were made between the two5,7,24,105–107 or between those with and without intellectual disabilities.55,77,79,102,108 The remaining 15 papers reported data about in-patients with intellectual disability and/or autism in specialist intellectual disability services only (Table 3).1,3,4,6,8,14,35,73–75,78,104,109–111 The mean and the average median length of stay within specialist in-patient intellectual disability services was longer compared with GMH in-patient services, but was shorter when those identified as long stay were removed (Table 4).
There was a single study about the admission of adults with intellectual disabilities and a history of forensic mental health problems to GMH in-patient services,97 and length of stay was shorter for this group than for adults with intellectual disabilities who did not have forensic mental health problems. It is likely that this was because many were transferred to specialist forensic services following their admission, as there is evidence that forensic mental health needs are associated with discharge to non-community settings.7
A diagnosis of autism was associated with a longer length of stay within both GMH and specialist intellectual disability in-patient services.35,55 The authors of one study reported that those with intellectual disabilities and autism had a longer length of stay than those with intellectual disabilities without co-occurring autism.55
Discharge pathway
Across 24 studies, the percentage of in-patients with intellectual disabilities and/or autism who were discharged to their residence before admission ranged from 40 to 83%,2–4,6,57,101 whereas 27.5–45% were discharged to a different residence/new placement.2–4,6 The authors of a single study reported that discharge to a new location was associated with a longer in-patient admission and difficulties with internalising or externalising behaviours, whereas discharge to the same residence as before admission was associated with living in a socially deprived area.101 Those discharged from specialist intellectual disability in-patient services were reported as less likely to be from ‘out of area’,7 and more likely to go back to the family home, than those discharged from GMH in-patient services.26
Three studies reported ‘delayed discharge’ rates ranging from 10 to 63% for in-patients with intellectual disabilities.73,79,111 However, the authors of a single study reported that in-patients with intellectual disabilities were no more difficult to discharge or more likely to stay beyond their discharge date than in-patients without intellectual disabilities, but were more likely to be discharged to their prior accommodation compared with in-patients without intellectual disabilities within GMH in-patient services.68 Discharges from both GMH and specialist intellectual disability in-patient services to the community tended to be high.1,2,104 For example, Xenitidis et al104 reported that 84% of all admissions from community settings and 81% of all admissions from non-community settings were discharged to the community. Within the same study, a history of fire setting was noted to be associated with discharge to non-community settings. Within more recent studies, discharges to group homes and shared residential settings rather than to family homes appeared to be more frequent, suggesting changes in the model of community care for this group over time.75,105,111
In two studies from Canada, higher levels of recommended care were seen as being needed for adults with intellectual disabilities and/or autism compared with those without disabilities, which included considering whether someone could manage in the community themselves, required residential support or continued to require in-patient care.55,70 Consideration for increasing outreach programmes and more intensive discharge planning for adults with intellectual disabilities were reported as needed.55
Clinical outcomes
Seventeen papers reported outcomes from assessments of mental health, psychiatric symptoms or risk and challenging behaviour.1,4,6–8,14,26,35,36,38,73,75,77,78,103,106,110 A range of clinical assessments were used to measure mental health symptoms and index outcome from treatment during an in-patient stay. Examples of these included the Clinical Global Impression Scale;26,40 assessments of behaviour and functioning, such as the Global Assessment of Functioning Scales,7,44,106 Aberrant Behaviour Checklist14,39 and Reiss Screen for Maladaptive Behaviour;35,36,140 and measures of overall health outcomes such as the Health of the Nation Outcome Scales (HoNOS), including the version for people with intellectual disabilities.8,37
Admission to in-patient services, either GMH or specialist intellectual disability in-patient services, was associated with improvements in symptoms during the stay,7,26,106 with some demonstrating continued improvements at follow-up.4,14 The authors of a single study reported that admission to a GMH in-patient service was associated with increased clinical symptoms at both admission and discharge, compared with admission to specialist intellectual disability in-patient services.106 The author of another paper reported that adults with autism tended to have increased difficulties with adaptive behaviour and functioning when admitted to psychiatric services, compared with those with intellectual disabilities without comorbid autism.35 van Minnen et al36 completed a clinical trial where adults with intellectual disabilities were randomised to either in-patient admission or enhanced community-based treatment. Their findings indicated that psychiatric symptoms at the end of the trial did not differ between the two groups, and they argued that enhanced treatment in the community may be appropriate for some people with intellectual disabilities who are experiencing mental health crisis.
A single paper made comparisons between elderly longer-stay patients with and without intellectual disabilities.77 They reported that elderly in-patients without intellectual disabilities within GMH in-patient services had more problems with relationships, occupation, activities and depressed mood, compared with elderly patients with intellectual disabilities within a specialist intellectual disability in-patient service. The authors suggested that the differences between the groups supported the use of specialist in-patient services for those with intellectual disabilities.
Readmissions
Readmission was considered within 16 papers.1,3–7,14,52,72,73,101,102,107,111,115,116 Rates for adults with intellectual disabilities across the included studies ranged from 8 to 53%. Four studies reported rates of multiple readmission (an individual discharged and readmitted more than once during the study period) of between 6 and 38% for specialist intellectual disability in-patient services.1,3,5,115 The readmission rates to GMH in-patient services for adults with intellectual disabilities ranged from 9 to 36.3%,5,7,52 with no significant difference in readmission rates between GMH and specialist intellectual disability in-patient services.5,7 A single study reported significantly higher rates of readmission for those with ‘developmental disabilities’ compared with those without.102 Those with borderline-to-moderate intellectual disabilities were noted to have higher readmission rates compared with those with a greater severity of intellectual disabilities in two studies.14,72 It was noted that generally there has been a significant reduction in readmission rates for individuals with intellectual disabilities over time.107,111 In one study, admission to accident and emergency departments was more likely following discharge from a psychiatric hospital for adults with intellectual disabilities, over a period of up to 26 months.116
Measures of patient safety
Nine papers focused on measures of patient safety with adults with intellectual disabilities and/or autism.52,56,71,73,74,78,104,112,117
Observation levels
Only two papers included information about observations levels for adults with intellectual disabilities within either GMH or specialist intellectual disability in-patient services.68,73 Within GMH in-patient services, adults with intellectual disabilities required significantly higher staffing levels than those without intellectual disabilities,68 and within specialist intellectual disability units, just under a third required specialist observation levels over a 15-month period.73 Lohrer et al68 reported ‘enhanced observations’ were used with 12.5% of adults without intellectual disabilities compared with 43.5% of adults with intellectual disabilities within GMH in-patient services. The use of enhanced observations with adults without intellectual disabilities is at a rate similar to that reported by others.118,119
Seclusion, physical interventions and pro re nata medication
The authors of six papers reported data about the use of seclusion and broader physical interventions within specialist intellectual disability in-patient services.52,56,71,74,112,117 A single study reported data about the use of pro re nata medication,52 and two studies compared seclusion rates for in-patients with and without intellectual disabilities. Turner and Mooney117 reported that adults with intellectual disabilities experienced seclusion at almost twice the rate of those without intellectual disabilities in a GMH in-patient service (6.4 v. 3.5%), but those admitted to specialist in-patient services spent significantly less time in seclusion than those with intellectual disabilities admitted to GMH services. In contrast, a recent study by Van Melle et al71 reported that neither a diagnosis of intellectual disability or autism was associated with increased seclusion use in GMH services.
No further comparisons were made with in-patients without intellectual disabilities and/or autism, but some reductions in the use of physical interventions and pro re nata medication were associated with new programmes or changes in practice.15,52
Within a survey of hospitals in a single study, higher use of seclusion and physical intervention were seen within the independent sector compared with the NHS in the UK, although the rates of patient injuries were the same.112 Comparing the data reported about the use of restrictive interventions with adults with intellectual disabilities with other studies indicated that they were used more frequently used.121 Bakken and Hoidal74 reported that 51% of in-patients with intellectual disabilities experienced seclusion, which was higher than that reported by other authors within low- and medium-secure forensic services.122
Measures of patient experience
There were only eight papers that reported outcomes associated with the patient experience for adults with intellectual disabilities.8,36,38,112,123–126 All studies made use of measures of patient experience within specialist intellectual disability in-patient services, but made no comparisons with patients without intellectual disabilities. A single literature review included patient experiences of those with intellectual disabilities and/or autism within GMH services.124
Met and unmet need
Two studies measured met and unmet needs as reported by family, staff and patients, with admission being associated with increased met needs and decreased unmet needs.8,123 Hall et al8 explored staff, patient and parent/carer views of in-patient needs compared with those receiving treatment in the community. Patients reported satisfaction with their met needs following community treatment; however, staff reports were not consistent, with staff identifying more unmet needs compared with those who had received in-patient care.8 Hellerud and Bakken123 reported that admission to in-patient services was associated with an increase in met needs, but families expressed concern about the risk of abuse, lack of specialist knowledge and challenges with understanding the detention process, as well as cultural and language differences in how mental health is understood. Two further studies explored patient views and experiences during admission within in-patient specialist intellectual disability services, and topics such as discomforting environments, staff support and relationships, being far from home and family, and limited opportunities to participate in decision-making were noted.125,126
Carer burden
Carer burden was examined within the only clinical trial included within this systematic review, and was noted to be high on initial baseline assessment.36 Carer burden did not increase for those who were allocated to outreach community-based treatment, and decreased slightly over time, but not significantly. Comparisons with those allocated to in-patient admission could not be made because of missing data.
Complaints and visits
It was noted in one study that fewer complaints and a higher number of visitors were reported for adults with intellectual disabilities within NHS specialist intellectual disability in-patient services in the UK, compared with the private/independent sector.112
Assessments of quality of life
Two studies made references to assessments of quality of life: one following admission to a specialist intellectual disability assessment and treatment unit,38 and the other following discharge from GMH and/or specialist intellectual disability services.124 Davies et al38 reported significant increases in quality of life at discharge (compared with at admission), indicating improvements in quality of life during admission. A literature review by Chowdhury and Benson124 reported improvements in quality of life after discharge from in-patient services to homes in the community, with improvements being most prominent within the first 6 months to 1 year, after which improvements plateaued or declined.
Secure forensic services for adults
The authors of 24 studies considered one of the outcome domains following admission to forensic or secure in-patient services for adults with intellectual disabilities and/or autism.21,23,27,50,53,58–60,80–88,122,127,130–132
The majority of studies took place within the UK, with the exception of two studies describing adults with and without intellectual disabilities with forensic needs detained within GMH, specialist intellectual disability and forensic in-patient services in Canada;27,84 and two studies (using the same sample) that included forensic patients in UK and The Netherlands.82,85 Within the UK, in-patient forensic services are traditionally categorised into locked rehabilitation, low-, medium- and high-secure services. These units tend to be characterised by high staff/patient ratios, with increasing assessment of risk resulting in increased restrictions (i.e. more locked areas), higher numbers of restricted items and increased safety in physical structure (e.g. removal of ligature points).133 The number of included papers across the four levels of security were as follows: two for locked rehabilitation, five for low secure, ten for medium secure and seven for high secure. The majority focused on describing the care pathway and outcomes.
Measures of effectiveness
Effectiveness, mostly length of stay, was considered within 19 studies.21,27,50,53,58,80,81,83,85–89,122,127,130–132
Length of stay
Forensic in-patients in the UK tended to have a shorter length of stay than those in similar services within The Netherlands.60 Within the UK, adults with intellectual disabilities were reported to have a longer length of stay than patients without intellectual disabilities within medium- and high-secure in-patient units,27,80,131 but this difference was only found to be significant in one paper.131 A single study explored length of stay within low-secure units, but made no comparisons with those without intellectual disabilities.89 Previous studies reported data to suggest that people with intellectual disabilities who have forensic needs tend to have a lengthy hospital stay, which can exceed 10 years.21,81 However, within one study, when length of stay was calculated using all admissions to secure/forensic in-patient services, adults with intellectual disabilities had a shorter length of stay than those without intellectual disabilities.81 Stays within in-patient forensic services tended to be longer than those within GMH and specialist intellectual disability in-patient services,52,100 and increased risk associated with criminal offending behaviours is likely to account for the longer length of stay within forensic hospitals.134
Length of stay for individuals with intellectual disabilities were comparable across low- and medium-secure in-patient services within another study,127 whereas a longer stay was noted for patients with intellectual disabilities and a co-occurring personality disorder.131,132 Whether detention in hospital was ordered by a court did not appear to lead to a longer length of stay.89
For those with both autism and intellectual disabilities, one study reported no significant differences in length of stay compared with those with intellectual disabilities,53 whereas in two further studies, adults with autism were reported to have a shorter length of stay.28,83 However, there are studies indicating that adults with autism have longer stays within in-patient forensic services.135,136 Senn et al60 reported that in-patients with autism were less prevalent within forensic services in the UK compared with The Netherlands.
Discharge pathway
Nine studies reported information relating to discharge outcomes for forensic services.50,53,81,87,89,122,127,130,132
Discharges from secure/forensic in-patient services were frequently characterised by involvement with another service or care provider, rather than absolute discharge to the community. As perhaps would be expected, there was evidence that low-secure services discharged more frequently to the community, with earlier studies showing more discharges to a home or the family home and later studies more likely to describe discharge to ‘group’ homes or residential care.127,130 Within several papers, it was reported that between 20 and 91% of those discharged within the UK remained subject to the Mental Health Act (1983).50,122,127,130
Individuals within medium- and high-secure care tended to stay within secure in-patient services, and discharges tended to be associated with transfer to another secure in-patient setting.50,89 This was not only illustrated by discharge data, but also by the source of the admission as described by Chester et al,81 who reported that 51.5% of patients with intellectual disabilities were admitted from medium-secure, 10.6% from low-secure and 13.6% from high-secure settings. A similar pattern was found for patients without intellectual disabilities, although this group were significantly more likely to be admitted from a high-secure service and significantly less likely to be admitted to high- or medium-secure services direct from the community. They also noted that patients with intellectual disabilities were less likely to be admitted to hospital via a court-ordered admission, and more likely to experience transfer to services of the same or increasing security than patients without intellectual disabilities.81 For those with intellectual disabilities and a diagnosis of personality disorder, there were no differences in discharge outcomes within a forensic in-patient service compared with those with intellectual disabilities without a diagnosis of personality disorder.132
Clinical outcomes
Numerous clinical or risk assessments and outcome measures were discussed within five papers about admission to forensic in-patient services.58,81,88,89,131 These included the HoNOS scores for people with intellectual disabilities;37 the Historical, Clinical and Risk Management – 20 (HCR-20);49 the Psychopathy Checklist Screening Version;51 and mental health and behaviour measures, such as the Emotional Problems Scale – Behaviour Rating Scale and Self-Report Inventory.137 Most comparisons were made between groups of adults with intellectual disabilities, where authors demonstrated that risk and symptoms were improved at discharge compared with admission, lower for those who had been discharged compared with current in-patients, and higher for those who were subject to more restrictive practices.21,58,83 These findings suggest that admission is associated within clinical improvements over time.
There was some evidence that adults with intellectual disabilities who have associated forensic needs tend to score higher on the HCR-20 compared with those without intellectual disabilities.81 In a different study, this was also the case for adults with intellectual disabilities who had a personality disorder, who scored higher on the HCR-20 than those with intellectual disabilities without a diagnosis of personality disorder and those with personality disorder without intellectual disabilities.131 In a further study, HoNOS scores for adults with Asperger syndrome significantly decreased from admission to discharge, and higher scores on this measure were not associated with increased use of seclusion for this patient group.58
Criminal offending or ‘offending-like’ behaviours
Further offending behaviours or reconvictions (including aggression and violence) were examined in eight papers exploring forensic in-patient services for individuals with intellectual disabilities.50,81,85,88,89,128,130,131 Reconviction rates were lower than displays of ‘offending-like behaviours’, with the former ranging from 3 to 11% for those discharged, and the latter ranging from 30 to 58% over follow-up periods of 5–12 years.51,130 A diagnosis of personality disorder was associated with a higher post-discharge conviction rate in adults without intellectual disabilities, while individuals with intellectual disabilities and a co-occurring personality had a higher post-discharge conviction rate than individuals with intellectual disabilities without personality disorder.131 In a single study within the UK, there was evidence that more frequent aggression was observed by those with intellectual disabilities detained under Part II compared with Part III of the Mental Health Act, 1983.89 Challenging behaviour and violent incidents were noted to reduce over longer admissions,88 and further instances of offending-like behaviours were associated with readmission and transfers to higher-security services.130 Those with intellectual disabilities and/or autism were not more likely to display physical violence compared with those with intellectual disabilities and/or autism.85
Readmission
Readmission rates for adults with intellectual disabilities within in-patient forensic services were reported to vary from 20 to 44% across low-, medium- and high-secure services across five papers.27,50,88,127,130
Readmission to medium- and low-secure units was associated with discharge to the community, along with multiple changes to residence, rather than discharge or transfer to another in-patient service; this is unsurprising, considering that this group remained within in-patient services.50,130 Readmission appeared to be because of criminal offending or behaviour that challenges, rather than mental ill health.130 However, in a single study comparing adults with and without intellectual disabilities who have forensic histories, there was no difference in readmission rates over a 10-year period.27
Measures of patient safety
Aspects of patient safety were examined within ten studies.53,58,82–85,88,89,122,132
Use of observation levels, seclusion rates and physical intervention
A small number of papers explored observation levels, seclusion rates and physical interventions within in-patient forensic services.53,58,83,89,122,132 Studies predominantly reported data about rates of seclusion, physical intervention and/or rapid tranquilisation or enhanced observations. No significant differences were noted in use of seclusion or physical restraint for those with and without intellectual disabilities within high-security hospitals.84 Several papers53,122,132 explored patient safety outcomes in a medium-secure service across a 6-year period, and reported no significant differences in use of seclusion, physical intervention or observation levels between adults with intellectual disabilities with and without comorbid personality disorder.88
However, the authors of one paper reported significantly higher levels of enhanced observations and use of physical interventions for in-patients with autism compared with in-patients without autism.53 Further papers reported that the use of seclusion with adults with autism in medium- and low-secure services was higher than those with a diagnosis of paranoid schizophrenia, but lower than those with a diagnosis of emotionally unstable personality disorder or antisocial personality disorder.132 There was some evidence to indicate that in-patients with autism within high-secure hospitals are secluded more frequently and for longer, compared with in-patients without autism.83
Reed et al89 compared those detained under Part III and Part II of the Mental Health Act, 1983, within the UK in a low-secure unit. They noted the higher use of physical restraint, intervention and seclusion, and more instances of aggression, among those detained under Part II compared with Part III (which are those who were admitted to hospital as a result of criminal proceedings). Those detained under Part II were more likely to have a diagnosis of pervasive developmental disorder, which included autism, whereas those detained under Part III were more likely to have a diagnosis of personality disorder and present with self-harm.89
Measures of patient experience
Four studies investigated aspects of the patient experience within forensic in-patient services.21,23,59,129 A systematic review and Delphi study21 identified patient and carer experience as an important indicator of service quality within in-patient forensic services for people with intellectual disabilities and/or autism. Three studies, excluding the systematic review by Morrissey et al,21 investigated patient experience within in-patient forensic services,23,59,129 with one focusing specifically on family and home visits.129 Two papers made use of semi-structured interviews and identified hospital admission as ‘helpful’, although the environment was characterised as ‘noisy’ and ‘stressful’, with both studies recognising loss of freedoms and restrictions of personal items as challenging for patients.23,59 Restriction of items associated with circumscribed interests was noted to be difficult for adults with autism. Despite these restrictions, satisfaction with quality of life were comparable or higher for adults with autism within high-security settings compared with other detained forensic patient groups.59 Williams et al23 interviewed a small sample of seven women with intellectual disabilities detained in hospital. They reported that these women found hospital admission helpful, including the treatment offered, but at the same time, they found their setting undesirable, experienced some interpersonal conflict with other in-patients and wanted to live in the community.
Family contact and home visits were shown to be high in a retrospective case file review of in-patients within a medium-secure, low-secure and ‘locked rehab’ forensic service, with 81% maintaining some degree of contact with their relatives. This included 44% receiving a family visitor and 54% undertaking a home visit during a 12-month period.129
In-patient treatment for children and adolescents
Measures of effectiveness
There were 20 different studies that investigated aspects of effectiveness associated with admission to a psychiatric in-patient service for children and adolescents.25,28,30,31,33,61–67,90–95,138,139
Length of stay
Mean length of stay was available from 13 papers for children and adolescents (minimum 13.4 days, maximum 263 days).28,33,61–63,66,67,90–95 Length-of-stay data indicated that a shorter length of stay was associated with admission to specialist higher-dependency intellectual disability in-patient services compared with secure open in-patient services93 and GMH in-patient services.90 Further still, one group of authors reported that there were no differences in length of stay for children and adolescents with or without autism who also had intellectual disabilities.91 However, a database review of public health services in Canada noted longer psychiatric hospital stays for adolescents and young adults with autism compared with those in infancy and childhood.61 The findings from three further studies indicated that the implementation of an autism-specific care pathway shortened length of stay for children with autism, but not significantly.66,67,95
Two papers focused specifically on adolescent GMH in-patient services during the COVID-19 pandemic,33,62 noting a shorter in-patient length of stay after the COVID-19 outbreak, and although based on small numbers, a shorter length of stay was noted for adolescents with autism compared with those with both autism and intellectual disabilities.33
Discharge pathway
Only one paper explored the discharge pathway from specialist intellectual disability in-patient services,93 and another explored discharge pathways from forensic medium-secure units.139 Smith and Berney93 examined discharges of children and adolescents with moderate intellectual disabilities from one open unit, and those with mild intellectual disabilities from a different open or low-secure unit. Both Smith and Berney93 and Livanou et al139 reported that discharges from secure units were most often to another specialist and highly staffed unit, including forensic in-patient or secure services, sometimes for adults. Discharge from the open units was more likely to be back to the family home.93 It was noted that males with neurodevelopmental disabilities, including those with intellectual disabilities and autism, were more likely to be transferred to an adult secure psychiatric service (low, medium or high), but the authors did not report whether these services were specialist.139
Clinical outcomes
Four studies measured symptoms over time following in-patient admission for children and adolescents with intellectual disabilities and/or autism.28,33,90,94 The authors of two studies reported improved symptoms following admission to a GMH in-patient service for children with intellectual disabilities and/or autism.22,33 There was also evidence to indicate improvements in symptoms following admission to a specialist intellectual disability in-patient service that included children with autism.94 The authors of the final study to examine clinical outcomes reported that children with intellectual disabilities and/or autism admitted to specialist intellectual disability in-patient services had fewer symptoms and problems at discharge (compared with admission), than children admitted to GMH in-patient services.90 However, overall, the degree of symptoms and problems was higher for children and adolescents with intellectual disabilities and/or autism compared with those without intellectual disabilities and/or autism, at both admission and discharge.
Admission and readmission
Ten studies reported admission and readmission rates.25,30,31,61,62,64,65,92,138,139 Evidence suggested that children and adolescents with mild intellectual disabilities were more likely to be admitted to GMH in-patient services, and those with more severe intellectual disabilities were more likely to be admitted to specialist intellectual disability in-patient services.90,93 Males were more likely to be admitted to forensic in-patients services.139 There was also evidence from a single study that readmission rates to specialist intellectual disability in-patient services were lower than that seen following discharge from GMH in-patient services for children and adolescents with intellectual disabilities and/or autism.92
For in-patients with autism, admissions were noted by some groups as disproportionately higher than for those without autism, and increased over time.25,31,41,63,93 This included increased admissions of children with autism with and without intellectual disabilities to non-psychiatric settings for mental ill health.61,62,65 Although Kalb et al25 noted an increased admission rate for those with autism compared with those without autism, they reported that there had been no change in the number of children and adolescents with autism presenting to accident and emergency departments because of mental ill health or behaviour that challenges, in the USA between the years 2010 and 2013. However, in another study64 from the USA with just over 2 million participants, a significant increase in hospital admission during the years 1999–2009 was associated with a diagnosis of autism, excluding intellectual disabilities, and the most cited reason for admission was psychiatric disorder; teenagers with autism were more likely to be admitted, a finding echoed by data from Canada.61 Within these two studies, psychiatric care was the most expensive medical cost incurred for children and young people with autism. A substantial increase was noted in the number of discharges of children and adolescents with autism within another study,64 but there was no associated increase in rates of admission for children and adolescents who had both autism and intellectual disabilities.64 A single study noted a decrease in child and adolescent admissions to both the emergency room and psychiatric in-patient units for those diagnosed with autism during the first month of the COVID-19 outbreak.62
Measures of patient safety
The literature about patient safety within child and adolescent in-patient services for those with intellectual disabilities and/or autism was scant. There were only three published papers within this domain, and they were about the same clinical service, using the same data;66,67,95 both physical interventions and intramuscular injection as pro re nata medication were examined when used with children and adolescents with autism. The authors reported that following the implementation of a new, autism-specific in-patient care pathway, the use of physical interventions and intramuscular injection decreased when compared with the previous care pathway.66,67
Discussion
The aim of this systematic review was twofold: to describe the different models of psychiatric in-patient service provision for children, adolescents and adults with intellectual disabilities and/or autism; and to evaluate outcomes from admission with reference to treatment effectiveness, patient safety and patient experience, as found within the literature.
Generally, there were two main models of in-patient psychiatric care described, but there was complexity and there are differences between countries. These were admission to a specialist intellectual disability or a GMH in-patient service, whether for children, adolescents or adults with intellectual disabilities and/or autism, with or without forensic needs. It was noted that specialist intellectual disability in-patient services appeared more common in the UK. Within GMH in-patient services, admissions were to beds within the same unit as patients without intellectual disabilities and/or autism, or to beds that were said to be specifically for people with intellectual disabilities and/or autism, sometimes located elsewhere, and where staff may have specialist knowledge, but were characterised as part of a GMH in-patient service.8,70 It was the case that although these services were within or described as GMH services, they did provide some specialist assessment and treatment specific to those with intellectual disabilities and/or autism, indicating a need for specialist staff and services when working with this patient population within GMH services. All services provided 24-h care, some were locked, and in-patients had access to a multidisciplinary team and a range of bio-psychosocial interventions, whereas specialist services tended to have staff with specialist training and experience in working with people with intellectual disabilities and/or autism, and ‘adapted’ clinical interventions and care pathways.1,3–5,8,14,36,50 This was not always the case within GMH in-patient services.
It was noted that adults with borderline-to-mild intellectual disabilities appeared more likely to be admitted to GMH in-patient services compared with those with more severe disabilities, who were more likely to be admitted to specialist in-patient service.5,6,52 More males with intellectual disabilities and/or autism tended to be admitted, and this was most marked for people with autism and those admitted to forensic in-patient services. There was evidence that although those from Black and minority ethnic communities were overrepresented, they were more likely to be admitted to GMH in-patient services, whereas those who were White tended to be admitted to specialist services.
Effectiveness
GMH and specialist intellectual disability in-patient services for adults
Considering treatment effectiveness, data about length of stay indicated that adults with intellectual disabilities and/or autism had a similar mean length of stay within GMH in-patient services than those without intellectual disabilities and/or autism, when long-stay patients were excluded. The mean length of stay within specialist intellectual disability in-patient services was substantially shorter compared with mean length of stay for adults with intellectual disabilities and/or autism admitted to GMH in-patient services, again, when long-stay patients were excluded. However, when the median length of stay was examined, differences were observed. The average median length of stay revealed that adults with intellectual disabilities had the shortest length of stay within GMH in-patient services, staying for a shorter period than those without intellectual disabilities, whereas those admitted to special intellectual disability in-patient services had the longest length of stay (Table 4). However, there are limitations associated with these data. First, they are based on relatively few observations. Second, not all authors reported both the mean and median length of stay. Third, studies took place at different times and within different countries, where services may be organised differently. These findings are likely a result of too few observations within and across studies, and a much larger study would be needed to provide a robust estimate. Finally, a shorter length of stay may not be associated with greater effectiveness, and indeed, the opposite may be true. It may be more appropriate to examine readmission within a short period of time (e.g. 30 days), which appears to be more likely for people with intellectual disabilities,42 or the frequency of delayed discharge.43
Considering discharge, a substantial proportion of in-patients returned to their prior residence when discharged compared with those who moved to live at a new location,2–4,6,14,57,75 which appeared to be associated with a longer length of stay.101 Those discharged from specialist in-patient services were less likely to be from out of area and more likely to return to live at home.7,26 There was some evidence that this group required higher levels of care on discharge from hospital.55 There was evidence to suggest that readmission rates to GMH or specialist in-patient intellectual disability services did not differ,5,7 but they may be more likely to attend the accident and emergency department for a period of time following discharge.116 However, there was evidence that those with borderline-to-moderate intellectual disabilities had higher readmission rates compared with those with more severe intellectual disabilities.14,72
Admission to a psychiatric hospital was associated with a reduction in clinical symptoms,7,26,106 however, there was some evidence that admission to a GMH in-patient service was associated with an increase in clinical symptoms for some patients with intellectual disabilities and/or autism,106 with further evidence that in-patients with autism experience an increase in symptoms on admission compared with those with intellectual disabilities without autism.35 The only clinical trial to have been completed in this area evidenced that both in-patient admission and enhanced care in the community led to improvements in psychiatric symptoms, and there was no difference between the two care models36
Secure forensic services
Data about length of stay for adults with intellectual disabilities and/or autism admitted to forensic services suggested that this group may stay for longer27,80,131,135,136 or shorter periods58,81,83 than in-patients without intellectual disabilities and/or autism, indicating inconsistency within the literature. There was some evidence that a diagnosis of personality disorder may be associated with a longer length of stay within forensic services.131,132 There was also evidence that in-patients with autism have a longer length of stay.135,136
Discharge into community settings were more frequent from low-secure services, whereas moving to another forensic in-patient service was more common within medium- and high-secure hospitals.50,89 It was noted that over time, discharge to residential care settings as opposed to the family home had become more common.127,130 There was evidence that admission to secure forensic services was associated with improvements in clinical symptoms and a reduction in criminogenic risk,21,58,83 including challenging behaviour and aggression.130 There was also evidence that readmission rates for those with intellectual disabilities and/or autism were not elevated following discharge, compared with those without intellectual disabilities and/or autism.27
In-patient services for children and adolescents
For children and adolescents, there was evidence that admission to specialist higher-dependency services was associated with a shorter length of stay compared with open secure in-patient services93 and GMH in-patient services.90 For children and adolescents with autism, there was evidence that this group had a longer length of stay compared with other groups.61 There was also some evidence that admission rates were shortened during the COVID-19 pandemic.33,62 There were relatively fewer papers that focused specifically on discharge pathways for children and adolescents; however, there was tentative evidence to indicate that when admitted to secure services, they were more likely to transfer to another specialist unit, including secure in-patient services, whereas those within non-secure units tended to return home.93,139
There was evidence that admission to in-patient services was associated with a reduction in clinical symptoms among children and adolescents with intellectual disabilities and/or autism,28,33,90,94 bearing in mind that this conclusion is based on fewer papers than similar conclusions in the literature for adults included within this systematic view. There was also evidence that admission to a specialist in-patient service was associated with greater improvements and few readmissions, compared with admission to GMH in-patient services.90,93 However, admission rates over time for children and adolescents with autism were noted to be increasing,31,63,93 including admissions to non-psychiatric settings despite being admitted for problematic mental health.25,64
As with the adult literature, children and adolescents with mild intellectual disabilities appeared more likely to be admitted to GMH in-patient services, whereas those with more severe intellectual disabilities were more likely to be admitted to specialist in-patient services.90,93
Patient safety
GMH and specialist intellectual disability in-patient services for adults
Patient observation levels were noted to be higher for in-patients with intellectual disabilities compared with those without intellectual disabilities,68 with higher observations rates needed within GMH in-patient services. In-patients with intellectual disabilities were secluded more frequently than those without intellectual disabilities, but the rate was lower within specialist services.117 However, there was evidence from a single study that seclusion rates were not elevated for in-patients with intellectual disabilities and/or autism within GMH in-patient settings,71 and further evidence suggested that seclusion and physical interventions were higher for in-patients with intellectual disabilities and/or autism within independent sector hospitals compared with the NHS in the UK.112
Secure forensic services
There was evidence that there were no differences in the use of seclusion, physical interventions and observation levels for those with and without intellectual disabilities and/or autism within secure forensic services.84,88,122,132 This was not the case for in-patients with autism, where increased observation levels and physical interventions, including seclusion, were reported.53,58
In-patient services for children and adolescents
Relatively few papers had been published that focused on patient safety during admission for children and adolescents with intellectual disabilities and/or autism, which is surprising, considering the inherent vulnerability of this population. There was some evidence that the implementation of an autism-focused care pathway led to reduction in the use of physical interventions, including pro re nata medication.66,67
It is important to note that Morrissey et al21 defined patient safety within forensic services for people with intellectual disabilities as being defined by premature death and suicide, physical health problems, excessive use of medication, restrictive practices (restraint, seclusion, aggression), and victimisation and safeguarding concerns. Within the included studies, there was little focus on these domains other than restrictive practices, and this should be addressed in future studies. There is literature focused on understanding the experience of being restrained for people with intellectual disabilities that indicates that it is a negative experience, leading to increased distress in some cases, with some having experienced abuse;45,46,47 there is also some evidence that increased observation levels may improve engagement and relationships48, and little focus upon children and adolescents.
Patient experience
GMH and specialist intellectual disability in-patient services for adults
None of the included studies focused on the experiences of in-patients with intellectual disabilities within GMH in-patient services. Findings from the included papers about admission to specialist in-patient services indicated an increased rate of met need associated with admission.8,123 There was evidence to indicate that family members have difficulties with understanding aspects of an in-patient admission, and expressed concern about the risk of abuse and lack of specialist knowledge,123 but also expressing relief that their loved one is receiving care.123 In-patients reported concerns about staying within challenging environments, issues with staff support and relationships, being away home and family, and concerns about being able to take part in decision-making.125,126 There was evidence that admission was associated with improvements in quality of life.38,124
Secure forensic services
Patients were seen to characterise their admission as helpful, but found the environment challenging, particularly with the restrictions that are common within secure forensic services.23,59 There was some evidence that adults with autism reported satisfaction with their quality of life within high-secure hospitals, compared with other in-patients.59 There was also evidence that family contact and home visits were frequent within low-secure, medium-secure and ‘locked rehab’ forensic services.129
In-patient services for children and adolescents
None of the eligible studies focused on the patient experience associated with admission to a psychiatric hospital for children and adolescents with intellectual disabilities and/or autism, or their families.
Strengths and limitations
Within this systematic review, we have synthesised data and findings across a large number of papers with differing methodologies, which was challenging because of the breadth of the findings and associated heterogeneity. Although challenging, our focus on admissions for children, adolescents and adults with intellectual disabilities and/or autism across GMH, specialist intellectual disability and forensic in-patient services is a strength. Our search strategy and inclusive approach allowed for a thorough synthesis of findings across a range of studies. A further strength is the method we used to integrate and synthesise our findings according to whether they were relevant to key aspects care (treatment effectiveness, patient safety or patient experience), an approach taken by others who have completed related work.21 However, the included literature is problematic because of a preponderance of observational designs where researchers have collected data retrospectively or prospectively, describing and contrasting different groups. Although highly informative and valuable, these designs do not allow for clear conclusions about causality. Further, in-patient psychiatric care has changed over time. The majority of studies involving adults took place from 2000 to 2019, with only eight studies having taken place before 1999. Regarding studies involving children, which were sparse compared with the adult literature, only one study took place before 2009, with all other studies being conducted after this period. The design of in-patient psychiatric care changes with time, as units and services are redesigned or new services, interventions and policies are developed and implemented. These changes may have had an impact on some of our outcomes (e.g. length of stay, seclusion rates, physical interventions and prescribing). For example, there was evidence that length of stay was shortened following the implementation of an autism-specific care pathway.66,67,95 Although in-patient psychiatric care has changed over time, it is also the case that definitions of both autism and intellectual disabilities have changed, which may have led to heterogeneity between studies and affected the conclusions drawn. The majority of the included papers took place after the year 2000, and diagnostic conceptualisation of both intellectual disabilities and autism were relatively clear. Nevertheless, wider societal and professional understanding of both intellectual disabilities and autism has improved throughout this period, which would mean that specialised knowledge about developmental disabilities within GMH in-patient services has also improved.
However, the evidence as it stands indicates that admission to a psychiatric hospital is associated with improvements in clinical symptoms for children, adolescents and adults with intellectual disabilities, whether they are admitted to GMH, specialist intellectual disability or forensic in-patient services. There is a lack of sufficient evidence to drawn firm conclusions about whether GMH in-patient services with specialist expertise are helpful for some patients, when compared with specialist intellectual disability in-patient services characterised as not being part of GMH services. It was notable that there was a single clinical trial comparing enhanced community treatment with in-patient treatment, demonstrating that both forms of treatment are associated with improvements in clinical symptoms, but there were issues with missing data.36 However, undertaking research into complex mental healthcare systems, operating within both in-patient and community settings, is challenging, as interventions are multi-professional and multifaceted, with a focus on the biological, psychological and social. It was noted that there was no description of psychiatric liaison. Richer and more thorough descriptions of the interventions that are offered to patients with intellectual disabilities and/or autism who have mental health disorders remains needed, along with greater focus on studies that describe lived experience. Comparing and contrasting different models of care proved challenging, as much of this information may be found within documents that are not readily available within the peer-reviewed literature (e.g., service specifications for in-patient services, including details about staffing levels and eligibility criteria for admission; or data about observation levels, length of stay, seclusion rates or use of pro re nata medication, which may be seen as sensitive and are not consistently placed within the public domain). Nevertheless, there was some evidence that admission to specialist services is associated with better outcomes for patients with intellectual disabilities and/or autism, recognising that services should work effectively to avoid unnecessary admission where possible, in accordance with national policies within some countries.9,10
Future directions
There was evidence that admission to specialist intellectual disability in-patient services is associated with better outcomes across several domains for patients with intellectual disabilities and/or autism, recognising that admission to these services was more likely for those with more severe intellectual disabilities. This in somewhat unsurprising considering that these services have expertise in working with this population, compared with GMH in-patient services. However, we were not able to conclude with certainty that these improvements are caused by an in-patient admission, because of the preponderance of observational designs within the included literature and the challenges of conducting clinical trials within this area. There were few studies that focused on describing patient safety and experience, including restrictive practices, within GMH in-patients services, which should be addressed in future studies, noting evidence that those with mild disabilities may be more likely to be admitted to these services. Further, there was a relative paucity of studies about the lived experiences of children and adolescents with intellectual disabilities and/or autism and their family following admission to an in-patient service, which should also be addressed in future studies. Finally, although conducting clinical trials to examine outcomes from an in-patient admission for this population presents design challenges, large observational studies over time and the inclusion of common outcome measures would allow researchers to model causality and make comparisons between different service types, and would be remarkably valuable.
Supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1192/bjo.2022.571.
click here to view supplementary material
Data availability
The data that support the findings of this study are available from the corresponding author, P.E.L., on reasonable request.
Author contributions
All authors made substantial contributions to the conception, design and interpretation of data; revising the work for important intellectual content; approved the final version to be published and agreed to be accountable for all aspects of the work in ensuring accuracy and integrity. C.L.M. and P.E.L. were responsible for the initial acquisition of data and analysis, along with the drafting of the initial version of the manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
R.A. is a member of the BJPsych Editorial Board. All other authors have no known conflicts of interest to declare.
References
- 1.Hurst J, Nadarajah J, Cumella S. In-patient care for people with a learning disability and a mental illness. Psychiatrist 1994; 18(1): 29–31. [Google Scholar]
- 2.Singh I, Khalid M, Dickinson M. Psychiatric admission services for people with learning disability. Psychiatrist 1994; 18(3): 151–2. [Google Scholar]
- 3.Trower T, Treadwell L, Bhaumik S. Acute in-patient treatment for adults with learning disabilities and mental health problems in a specialised admission unit. Br J Dev Disabil 1998; 44(86): 20–9. [Google Scholar]
- 4.Raitasuo S, Taiminen T, Salokangas R. Inpatient care and its outcome in a specialist psychiatric unit for people with intellectual disability: a prospective study. J Intellect Disabil Res 1999; 43(2): 119–27. [DOI] [PubMed] [Google Scholar]
- 5.Alexander R, Piachaud J, Singh I. Two districts, two models: in-patient care in the psychiatry of learning disability. Br J Dev Disabil 2001; 47(93): 105–10. [Google Scholar]
- 6.Tajuddin M, Nadkarni S, Biswas A, Watson MJ, Bhaumik S. A study of the use of an acute inpatient unit for adults with learning disability and mental health problems in Leicestershire, UK. Br J Dev Disabil 2004; 50(98): 59–68. [Google Scholar]
- 7.Xenitidis K, Gratsa A, Bouras N, Hammond R, Ditchfield H, Holt G, et al. Psychiatric inpatient care for adults with intellectual disabilities: generic or specialist units? J Intellect Disabil Res 2004; 48: 11–8. [DOI] [PubMed] [Google Scholar]
- 8.Hall I, Parkes C, Samuels S, Hassiotis A. Working across boundaries: clinical outcomes for an integrated mental health service for people with intellectual disabilities. J Intellect Disabil Res 2006; 50(8): 598–607. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health. Transparency in Outcomes: A Framework for the NHS. A Consultation on Proposals. Department of Health, 2010. (https://webarchive.nationalarchives.gov.uk/ukgwa/20130104234835/http://www.dh.gov.uk/en/Consultations/Closedconsultations/DH_117583). [Google Scholar]
- 10.NHS England. Supporting People with a Learning Disability and/or Autism who Display Behaviour that Challenges, including those with a Mental Health Condition. Service Model for Commissioners of Health and Social Care Services. NHS England, 2015. (https://www.england.nhs.uk/wp-content/uploads/2015/10/service-model-291015.pdf). [Google Scholar]
- 11.NHS Digital. Learning Disability Services Monthly Statistics (AT: June 2021, MHSDS: April 2021). NHS Digital, 2021. (https://digital.nhs.uk/data-and-information/publications/statistical/learning-disability-services-statistics/at-june-2021-mhsds-april-2021-final).
- 12.Moss S, Emerson E, Bouras N, Holland A. Mental disorders and problematic behaviours in people with intellectual disability: future directions for research. J Intellect Disabil Res 1997; 41: 440–7. [DOI] [PubMed] [Google Scholar]
- 13.Adams D, Hastings RP, Alston-Knox C, Cianfaglione R, Eden K, Felce D, et al. Using Bayesian methodology to explore the profile of mental health and well-being in 646 mothers of children with 13 rare genetic syndromes in relation to mothers of children with autism. Orphanet J Rare Dis 2018; 13: 185–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lunsky Y, White SF, Palucka AM, Weiss J, Bockus S, Gofine T. Clinical outcomes of a specialised inpatient unit for adults with mild to severe intellectual disability and mental illness. J Intellect Disabil Res 2010; 54(1): 60–9. [DOI] [PubMed] [Google Scholar]
- 15.Chaplin R. General psychiatric services for adults with intellectual disability and mental illness. J Intellect Disabil Res 2004; 48: 1–10. [DOI] [PubMed] [Google Scholar]
- 16.Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4: Software for Research Synthesis. Social Science Research Unit, UCL Institute of Education, 2010. (https://eppi.ioe.ac.uk/cms/er4/Features/tabid/3396/Default.aspx).
- 17.Hermann RC, Leff HS, Palmer RH, Yang D, Teller T, Provost S, et al. Quality measures for mental health care: results from a national inventory. Med Care Res Rev 2000; 57(Suppl 2): 136–54. [DOI] [PubMed] [Google Scholar]
- 18.Hermann RC, Mattke S, Somekh D, Silverhielm H, Goldner E, Glover G, et al. Quality indicators for international benchmarking of mental health care. Int J Qual Health Care 2006; 18(Suppl 1): 31–8. [DOI] [PubMed] [Google Scholar]
- 19.Meehan TJ, Stedman TJ, Neuendorf KE, Francisco ID, Neilson MG. Benchmarking Australia's mental health services: is it possible and useful? Aust Health Rev 2007; 31(4): 623–7. [DOI] [PubMed] [Google Scholar]
- 20.McEwan KL, Goldner EM. Keeping mental health reform on course: selecting indicators of mental health system performance. Can J Commun Ment Health 2009; 21(1): 5–16. [DOI] [PubMed] [Google Scholar]
- 21.Morrissey C, Langdon PE, Geach N, Chester V, Ferriter M, Lindsay WR, et al. A systematic review and synthesis of outcome domains for use within forensic services for people with intellectual disabilities. Br J Psychiatry Open 2017; 3(1): 41–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Royal College of Psychiatrists. People with Learning Disability and Mental Health, Behavioural or Forensic Problems: The Role of In-Patient Services. Royal College of Psychiatrists, Faculty of Psychiatry of Intellectual Disability, 2013. (https://www.rcpsych.ac.uk/docs/default-source/members/faculties/intellectual-disability/id-fr-id-03.pdf?sfvrsn=cbbf8b72_2). [Google Scholar]
- 23.Williams EM, Thrift S, Rose J. The subjective experiences of women with intellectual disabilities and offending behaviour: exploring their experiences of ‘home’. Int J Dev Disabil 2018; 64(3): 132–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glover G, Brown I, Hatton C. How psychiatric in-patient care for people with learning disabilities is transforming after Winterbourne View. Tizard Learn Disabil Rev 2014; 19(3): 146–9. [Google Scholar]
- 25.Kalb LG, Stuart EA, Vasa RA. Characteristics of psychiatric emergency department use among privately insured adolescents with autism spectrum disorder. Autism 2019; 23(3): 566–73. [DOI] [PubMed] [Google Scholar]
- 26.Gowda GS, Gopika G, Kumar CN, Manjunatha N, Yadav R, Srinivas D, et al. Clinical outcome and rehabilitation of homeless mentally ill patients admitted in mental health institute of South India: “know the unknown” project. Asian J Psychiatr 2017; 30: 49–53. [DOI] [PubMed] [Google Scholar]
- 27.Lin E, Barbaree H, Selick A, Ham E, Wilton AS, Lunsky Y. Intellectual and developmental disabilities and Ontario's forensic inpatient system: a population-based cohort study. Psychol Crime Law 2017; 23(9): 914–26. [Google Scholar]
- 28.Imran N, Bodla ZH, Asif A, Shoukat R, Azeem MW. Pakistan's first child & adolescent psychiatry inpatient unit: characteristics of admitted patients and response to treatment over a 7-year period. Pak J Med Sci 2021; 37(2): 305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Lorenzo R, Olmi T, Riolo G, Galeazzi GM, Ferri P. Factors associated with long-stays in an Italian psychiatric intensive treatment facility: 1-year retrospective observational analysis. Psychiatr Q 2019; 90(1): 185–96. [DOI] [PubMed] [Google Scholar]
- 30.Theodoratos O, McPherson L, Franklin C, Tonge B, Einfeld S, Lennox N, et al. Psychopathology of adolescents with an intellectual disability who present to general hospital services. Australas Psychiatry 2017; 25(5): 481–5. [DOI] [PubMed] [Google Scholar]
- 31.Medel-Herrero A, Gomez-Beneyto M. The impact of the 2008 economic crisis on the increasing number of young psychiatric inpatients. Rev Psiquiatr Salud Ment (Engl Ed) 2019; 12(1): 28–36. [DOI] [PubMed] [Google Scholar]
- 32.Gomez-Ramiro M, Fico G, Anmella G, Vazquez M, Sague-Viavella M, Hidalgo-Mazzei D, et al. Changing trends in psychiatric emergency service admissions during the COVID-19 outbreak: report from a worldwide epicentre. J Affect Disord 2021; 282: 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ozbaran NB, Kose S, Barankoglu I, Dogan N, Bildik T. A new challenge for child psychiatrists: inpatient care management during coronavirus pandemic. Asian J Psychiatr 2020; 54: 102303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lunsky Y, Bradley E, Durbin J, Koegl C, Canrinus M, Goering P. The clinical profile and service needs of hospitalized adults with mental retardation and a psychiatric diagnosis. Psychiatr Serv 2006; 57(1): 77–83. [DOI] [PubMed] [Google Scholar]
- 35.Kokoski C, Lunsky Y. Brief report: exploring treatment outcomes of individuals with autism spectrum disorder in a specialized dual diagnosis inpatient program. J Dev Disabil 2009; 15: 110–3. [Google Scholar]
- 36.van Minnen A, Hoogduin C, Broekman T. Hospital vs. outreach treatment of patients with mental retardation and psychiatric disorders: a controlled study. Acta Psychiatr Scand 1997; 95(6): 515–22. [DOI] [PubMed] [Google Scholar]
- 37.Roy A, Matthews H, Clifford P, Fowler V, Martin DM. Health of the Nation Outcome Scales for people with learning disabilities (HoNOS–LD). Br J Psychiatry 2002; 180(1): 61–6. [DOI] [PubMed] [Google Scholar]
- 38.Davies B, Josham S, Francis N. An evaluation of outcomes for service users with an intellectual disability admitted to an assessment and treatment unit. J Intellect Disabil 2021; 25(4): 441–8. [DOI] [PubMed] [Google Scholar]
- 39.Aman MG, Singh NN, Stewart AW, Field CJ. The Aberrant Behavior Checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic 1985; 89(5): 485–91. [PubMed] [Google Scholar]
- 40.Guy W. Clinical Global Impressions (CGI) Scale. Handbook of Psychiatric Measures. American Psychiatric Association, 2000. [Google Scholar]
- 41.Kalb LG, Stuart EA, Freedman B, Zablotsky B, Vasa R. Psychiatric-related emergency department visits among children with an autism spectrum disorder. Pediatr Emerg Care 2012; 28(12): 1269–76. [DOI] [PubMed] [Google Scholar]
- 42.Balogh R, Lin E, Dobranowski K, Selick A, Wilton AS, Lunsky Y. All-cause, 30-day readmissions among persons with intellectual and developmental disabilities and mental illness. Psychiatr Serv 2018; 69(3): 353–57. [DOI] [PubMed] [Google Scholar]
- 43.Lin E, Balogh R, Chung H, Dobranowski K, Durbin A, Volpe T, et al. Looking across health and healthcare outcomes for people with intellectual and developmental disabilities and psychiatric disorders: population-based longitudinal study. Br J Psychiatry 2021; 218(1): 51–7. [DOI] [PubMed] [Google Scholar]
- 44.Hall RC. Global Assessment of Functioning: a modified scale. Psychosomatics 1995; 36(3): 267–75. [DOI] [PubMed] [Google Scholar]
- 45.Jones P, Stenfert Kroese B. Service users’ views of physical restraint procedures in secure settings for people with learning disabilities. Br J Learn Disabil 2007; 35(1): 50–4. [Google Scholar]
- 46.Fish R, Hatton C. Gendered experiences of physical restraint on locked wards for women. Disabil Soc 2017; 32(6): 790–809. [Google Scholar]
- 47.Fish R, Culshaw E. The last resort? Staff and client perspectives on physical intervention. J Intellect Disabil 2005; 9(2): 93–107. [DOI] [PubMed] [Google Scholar]
- 48.Fish R. Women's experiences of special observations on locked wards. Disabil Soc 2022; 37(3): 528–33. [Google Scholar]
- 49.Webster C, Douglas K, Eaves D, Hart S. HCR-20. Assessing Risk for Violence. Version 2. Mental Health. Law, and Policy Institute, Simon Fraser University, 1997. [Google Scholar]
- 50.Halstead S, Cahill A, Fernando L, Isweran M. Discharges from a learning-disability medium secure unit: what happens to them? Br J Forensic Pract 2001; 3: 11–21. [Google Scholar]
- 51.Hart SD, Cox DN, Hare RD. Hare Psychopathy Checklist: Screening Version (PCL: SV). Multi-Heath Systems, 1995. [Google Scholar]
- 52.Burge P, Ouellette-Kuntz H, Saeed H, McCreary B, Paquette D, Sim F. Acute psychiatric inpatient care for people with a dual diagnosis: patient profiles and lengths of stay. Can J Psychiatry 2002; 47(3): 243–9. [DOI] [PubMed] [Google Scholar]
- 53.Esan F, Chester V, Gunaratna IJ, Hoare S, Alexander RT. The clinical, forensic and treatment outcome factors of patients with autism spectrum disorder treated in a forensic intellectual disability service. J Appl Res Intellect Disabil 2015; 28(3): 193–200. [DOI] [PubMed] [Google Scholar]
- 54.Allely CS. A systematic PRISMA review of individuals with autism spectrum disorder in secure psychiatric care: prevalence, treatment, risk assessment and other clinical considerations. J Crim Psychol 2018; 8(1): 58–79. [Google Scholar]
- 55.Lunsky Y, Gracey C, Bradley E. Adults with autism spectrum disorders using psychiatric hospitals in Ontario: clinical profile and service needs. Res Autism Spectr Disord 2009; 3(4): 1006–13. [Google Scholar]
- 56.Larue C, Goulet MH, Prevost MJ, Dumais A, Bellavance J. Identification and analysis of factors contributing to the reduction in seclusion and restraint for a population with intellectual disability. J Appl Res Intellect Disabil 2018; 31(2): e212–22. [DOI] [PubMed] [Google Scholar]
- 57.Prichard AE, Palucka AM, Reid M, Yunsky Y. Review of admissions of individuals with autism spectrum disorders to a specialized dual diagnosis program. J Dev Disabil 2007; 16(1): 76–84. [Google Scholar]
- 58.Griffiths C, Roychowdhury A, Girardi A. Seclusion: the association with diagnosis, gender, length of stay and HoNOS-secure in low and medium secure inpatient mental health service. J Forens Psychiatry Psychol 2018; 29(4): 656–73. [Google Scholar]
- 59.Murphy D, Mullens H. Examining the experiences and quality of life of patients with an autism spectrum disorder detained in high secure psychiatric care. Adv Autism 2017; 3(1): 3–14. [Google Scholar]
- 60.Senn D, Bulten E, Tomlin J, Vollm B. A comparison of English and Dutch long-stay patients in forensic psychiatric care. Front Psychiatry 2020; 11: 574247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Croteau C, Mottron L, Dorais M, Tarride JE. Use, costs, and predictors of psychiatric healthcare services following an autism spectrum diagnosis: population-based cohort study. Autism 2019; 23(8): 2020–30. [DOI] [PubMed] [Google Scholar]
- 62.Diaz de Neira MD, Blasco-Fontecilla H, Garcia Murillo L, Perez-Balaguer A, Mallol L, Forti A, et al. Demand analysis of a psychiatric emergency room and an adolescent acute inpatient unit in the context of the COVID-19 pandemic in Madrid, Spain. Front Psychiatry 2021; 11: 557508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lokhandwala T, Khanna R, West-Strum D. Hospitalization burden among individuals with autism. J Autism Dev Disord 2012; 42(1): 95–104. [DOI] [PubMed] [Google Scholar]
- 64.Nayfack A, Huffman L., Feldman H, Chan J, Saynina O, Wise P. Hospitalizations of children with autism increased from 1999 to 2009. J Autism Dev Disord 2014; 44(5): 1087–94. [DOI] [PubMed] [Google Scholar]
- 65.Robinson LA, Menezes M, Mullin B, Cook BL. A comparison of health care expenditures for Medicaid-insured children with autism spectrum disorder and asthma in an expanding accountable care organization. J Autism Dev Disord 2020; 50(3): 1031–44. [DOI] [PubMed] [Google Scholar]
- 66.Cervantes P, Kuriakose S, Donnelly L, Filton B, Marr M, Okparaeke E, et al. Sustainability of a care pathway for children and adolescents with autism spectrum disorder on an inpatient psychiatric service. J Autism Dev Disord 2019; 49(8): 3173–80. [DOI] [PubMed] [Google Scholar]
- 67.Kuriakose S, Filton B, Marr M, Okparaeke E, Cervantes P, Siegel M, et al. Does an autism spectrum disorder care pathway improve care for children and adolescents with ASD in inpatient psychiatric units? J Autism Dev Disord 2018; 48(12): 4082–9. [DOI] [PubMed] [Google Scholar]
- 68.Lohrer SP, Greene E, Browning CJ, Lesser MS. Dual diagnosis: examination of service use and length of stay during psychiatric hospitalization. J Dev Phys Disabil 2002; 14(2): 143–58. [Google Scholar]
- 69.Schmitz-Buhl M, Gairing SK, Rietz C, Haussermann P, Zielasek J, Gouzoulis-Mayfrank E. A retrospective analysis of determinants of involuntary psychiatric in-patient treatment. BMC Psychiatry 2019; 19(1): 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lunsky Y, Bradley E, Durbin J, Koegl C. A comparison of patients with intellectual disability receiving specialised and general services in Ontario's psychiatric hospitals. J Intellect Disabil Res 2008; 52(11): 1003–12. [DOI] [PubMed] [Google Scholar]
- 71.Van Melle AL, Noorthoorn EO, Widdershoven GAM, Mulder CL, Voskes Y. Does high and intensive care reduce coercion? Association of HIC model fidelity to seclusion use in the Netherlands. BMC Psychiatry 2020; 20(1): 469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Seager M, Bell G, O'Brien G. Readmissions to learning disability hospitals a study of failed discharge due to physical health problems, relapsing mental illness and severe behavioural problems. J Intellect Disabil 2000; 4(4): 321–31. [Google Scholar]
- 73.Slevin E, McConkey R, Truesdale-Kennedy M, Taggart L. People with learning disabilities admitted to an assessment and treatment unit: impact on challenging behaviours and mental health problems. J Psychiatr Ment Health Nurs 2008; 15(7): 537–46. [DOI] [PubMed] [Google Scholar]
- 74.Bakken TL, Hoidat SH. Specialized psychiatric services: patient characteristics, referral practice and length of stay in a representative clinical sample 2010–2016. Int J Dev Disabil 2019; 65(4): 277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Richings C, Cook R, Roy A. Service evaluation of an integrated assessment and treatment service for people with intellectual disability with behavioural and mental health problems. J Intellect Disabil 2011; 15(1): 7–19. [DOI] [PubMed] [Google Scholar]
- 76.Mackenzie-Davies N, Mansell J. Assessment and treatment units for people with intellectual disabilities and challenging behaviour in England: an exploratory survey. J Intellect Disabil Res 2007; 51(10): 802–11. [DOI] [PubMed] [Google Scholar]
- 77.Ashaye O, Mathew G, Dhadphale M. A comparison of older longstay psychiatric and learning disability inpatients using the health of the nation outcome scales. Int J Geriatr Psychiatry 1997; 12(5): 548–52. [DOI] [PubMed] [Google Scholar]
- 78.Sandhu D, Tomlins R. Clinical needs and outcomes of adults with intellectual disabilities accessing an inpatient assessment and treatment service and the implication for development of community services. J Intellect Disabil 2017; 21(1): 5–19. [DOI] [PubMed] [Google Scholar]
- 79.Perera C, Simpson N, Douds F, Campbell M. A survey of learning disability inpatient services in Scotland in 2007. J Intellect Disabil 2009; 13(2): 161–71. [DOI] [PubMed] [Google Scholar]
- 80.Butwell M, Jamieson E, Leese M, Taylor P. Trends in special (high-security) hospitals 2: residency and discharge episodes, 1986–1995. Br J Psychiatry 2000; 176: 260–5. [DOI] [PubMed] [Google Scholar]
- 81.Chester V, Vollm B, Tromans S, Kapugama C, Alexander RT. Long-stay patients with and without intellectual disability in forensic psychiatric settings: comparison of characteristics and needs. BJPsych Open 2018; 4(4): 226–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huitema A, Verstegen N, de Vogel V. A study into the severity of forensic and civil inpatient aggression. J Interpers Violence 2021; 36(11-12): NP6661–79. [DOI] [PubMed] [Google Scholar]
- 83.Murphy D, Bush E-L, Puzzo I. Incompatibilities and seclusion of patients with an autism spectrum disorder detained in high-secure psychiatric care. J Intellect Disabil Offend Behav 2017; 8(4): 188–200. [Google Scholar]
- 84.Ray I, Simpson AIF, Jones RM, Shatokhina K, Thakur A, Mulsant BH. Clinical, demographic, and criminal behavior characteristics of patients with intellectual disabilities in a Canadian forensic program. Front Psychiatry 2019; 10: 760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Verstegen N, de Vogel V, Huitema A, Didden R, Nijman H. Physical violence during mandatory psychiatric treatment: prevalence and patient characteristics. Crim Justice Behav 2020; 47(7): 771–89. [Google Scholar]
- 86.Vollm BA, Edworthy R, Huband N, Talbot E, Majid S, Holley J, et al. Characteristics and pathways of long-stay patients in high and medium secure settings in England; a secondary publication from a large mixed-methods study. Front Psychiatry 2018; 9: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Devapriam J, Fosker H, Chester V, Gangadharan S, Hiremath A, Alexander RT. Characteristics and outcomes of patients with intellectual disability admitted to a specialist inpatient rehabilitation service. J Intellect Disabil 2020; 24(1): 21–34. [DOI] [PubMed] [Google Scholar]
- 88.Morrissey C, Hobson B, Faulkner E, James T. Outcomes from the national high secure learning disability service: findings and challenges. Adv Ment Health Intellect Disabil 2015; 9: 116–23. [Google Scholar]
- 89.Reed S, Russell A, Xenitidis K, Murphy D. People with learning disabilities in a low secure in-patient unit: comparison of offenders and non-offenders. Br J Psychiatry 2004; 185: 499–504. [DOI] [PubMed] [Google Scholar]
- 90.Chaplin R, Roach S, Johnson H, Thompson P. Inpatient children and adolescent mental health services (CAMHS): outcomes of young people with and without intellectual disability. J Intellect Disabil Res 2015; 59(11): 995–8. [DOI] [PubMed] [Google Scholar]
- 91.Siegel M, Milligan B, Chemelski B, Payne D, Ellsworth B, Harmon J, et al. Specialized inpatient psychiatry for serious behavioral disturbance in autism and intellectual disability. J Autism Dev Disord 2014; 44(12): 3026–32. [DOI] [PubMed] [Google Scholar]
- 92.Gabriels RL, Agnew JA, Beresford C, Morrow MA, Mesibov G, Wamboldt M. Improving psychiatric hospital care for pediatric patients with autism spectrum disorders and intellectual disabilities. Autism Res Treat 2012; 2012: 685053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Smith P, Berney TP. Psychiatric inpatient units for children and adolescents with intellectual disability. J Intellect Disabil Res 2006; 50: 608–14. [DOI] [PubMed] [Google Scholar]
- 94.Siegel M, Doyle K, Chemelski B, Payne D, Ellsworth B, Harmon J, et al. Specialized inpatient psychiatry units for children with autism and developmental disorders: a United States survey. J Autism Dev Disord 2012; 42(9): 1863–9. [DOI] [PubMed] [Google Scholar]
- 95.Donnelly LJ, Cervantes PE, Okparaeke E, Stein CR, Filton B, Kuriakose S, et al. Staff perceptions and implementation fidelity of an autism spectrum disorder care pathway on a child/adolescent general psychiatric inpatient service. J Autism Dev Disord 2021; 51(1): 158–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chaplin R. Annotation: new research into general psychiatric services for adults with intellectual disability and mental illness. J Intellect Disabil Res 2009; 53(3): 189–99. [DOI] [PubMed] [Google Scholar]
- 97.Lunsky Y, Gracey C, Koegl C, Bradley E, Durbin J, Raina P. The clinical profile and service needs of psychiatric inpatients with intellectual disabilities and forensic involvement. Psychol Crime Law 2011; 17(1): 9–23. [Google Scholar]
- 98.Saeed H, Ouellette-Kuntz H, Stuart H, Burge P. Length of stay for psychiatric inpatient services: a comparison of admissions of people with and without developmental disabilities. J Behav Health Serv Res 2003; 30(4): 406–17. [DOI] [PubMed] [Google Scholar]
- 99.Gustafsson C. The prevalence of people with intellectual disability admitted to general hospital psychiatric units: level of handicap, psychiatric diagnoses and care utilization. J Intellect Disabil Res 1997; 41(6): 519–26. [DOI] [PubMed] [Google Scholar]
- 100.Axmon A, Bjorne P, Nylander L, Ahlstrom G. Psychiatric care utilization among older people with intellectual disability in comparison with the general population: a register study. BMC Psychiatry 2016; 16: 389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sheehan R, Mutch J, Marston L, Osborn D, Hassiotis A. Risk factors for in-patient admission among adults with intellectual disability and autism: investigation of electronic clinical records. BJPsych Open 2020; 7(1): e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lunsky Y, Balogh R. Dual diagnosis: a national study of psychiatric hospitalization patterns of people with developmental disability. Can J Psychiatry 2010; 55(11): 721–8. [DOI] [PubMed] [Google Scholar]
- 103.Gustafsson C, Sonnander K. Occurrence of mental health problems in Swedish samples of adults with intellectual disabilities. Soc Psychiatry Psychiatr Epidemiol 2004; 39(6): 448–56. [DOI] [PubMed] [Google Scholar]
- 104.Xenitidis KI, Henry J, Russell AJ, Ward A, Murphy DGM. An inpatient treatment model for adults with mild intellectual disability and challenging behaviour. J Intellect Disabil Res 1999; 43: 128–34. [DOI] [PubMed] [Google Scholar]
- 105.Hemmings CP, O'Hara J, McCarthy J, Holt G, Eoster F, Costello H, et al. Comparison of adults with intellectual disabilities and mental health problems admitted to specialist and generic inpatient units. Br J Learn Disabil 2009; 37(2): 123–8. [Google Scholar]
- 106.White SE, Lunsky Y, Grieve C. Profiles of patients with intellectual disability and mental illness in specialized and generic units in an Ontario psychiatric hospital. J Ment Health Res Intellect Disabil 2010; 3(3): 117–31. [Google Scholar]
- 107.Ganguly S, Gore S, Marston G, Roy A. Trends in admissions to an intellectual disability hospital. Psychiatr Bull 2009; 33(10): 371–4. [Google Scholar]
- 108.O'Brien WH, Beasley JB. Changing environments of inpatient psychiatric care for individuals with intellectual disabilities. Ment Health Aspects Dev Disabil 2007; 10(3): 99–106. [Google Scholar]
- 109.Palucka AM, Raina P, Liu S, Lunksy Y. The clinical profiles of forensic inpatients with intellectual disabilities in a specialized unit. J Learn Disabil Offend Behav 2012; 3(4): 219–27. [Google Scholar]
- 110.Iversen TE, Horndalsveen K, Matre E, Henriksen TF, Fusche S, Kildahl AN, et al. Inpatient treatment of borderline personality disorder in adults with intellectual disability: reflections on practice. Adv Ment Health Intellect Disabil 2019; 13(2): 67–75. [Google Scholar]
- 111.Oxley C, Sathanandan S, Gazizova D, Fitzgerald B, Puri BK. A comparative review of admissions to an intellectual disability inpatient service over a 10-year period. Br J Med Pract 2013; 6(2): a611. [Google Scholar]
- 112.Mansell J, Ritchie F, Dyer R. Health service inpatient units for people with intellectual disabilities and challenging behaviour or mental health problems. J Appl Res Intellect Disabil 2010; 23(6): 552–9. [Google Scholar]
- 113.Prichard EA, Palucka A, Reid M, Lunsky Y. Review of admissions of individuals with autism spectrum disorders to a specialized dual diagnosis program. J Dev Disabil 2010; 16(1): 76–84. [Google Scholar]
- 114.Wing J, Beevor A, Curtis R, Park S, Hadden J, Burns A. Health of the Nation Outcome Scales (HoNOS). Br J Psychiatry 1998; 172(1): 11–8. [DOI] [PubMed] [Google Scholar]
- 115.Lyall R, Kelly M. Specialist psychiatric beds for people with learning disability. Psychiatrist 2007; 31(8): 297–300. [Google Scholar]
- 116.Li X, Srasuebkul P, Reppermund S, Trollor J. Emergency department presentation and readmission after index psychiatric admission: a data linkage study. BMJ Open 2018; 8: e018613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Turner KV, Mooney P. A comparison of seclusion rates between intellectual disability and non-intellectual disability services: the effect of gender and diagnosis. J Forensic Psychiatry Psychol 2015; 27(2): 265–80. [Google Scholar]
- 118.Neilson T, Peet M, Poole J, Ledsham R. Does the nursing care plan help in the management of psychiatric risk? J Adv Nurs 1996; 24(6): 1201–6. [DOI] [PubMed] [Google Scholar]
- 119.Bowers L, Park A. Special observation in the care of psychiatric inpatients: a literature review. Issues Ment Health Nurs 2001; 22(8): 769–86. [DOI] [PubMed] [Google Scholar]
- 120.Bakken TL, Helverschou SB, Eilertsen DE, Heggelund T, Myrbakk E, Martinsen H. Psychiatric disorders in adolescents and adults with autism and intellectual disability: a representative study in one county in Norway. Res Dev Disabil 2019; 31: 1669–77. [DOI] [PubMed] [Google Scholar]
- 121.Steinert T, Lepping P, Bernhardsgrutter R, Conca A, Hatling T, Janssen W, et al. Incidence of seclusion and restraint in psychiatric hospitals: a literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol 2010; 45(9): 889–97. [DOI] [PubMed] [Google Scholar]
- 122.Alexander R, Hiremath A, Chester V, Green F, Gunaratna I, Hoare S. Evaluation of treatment outcomes from a medium secure unit for people with intellectual disability. Adv Ment Health Intellect Disabil 2011; 5(1): 22–32. [Google Scholar]
- 123.Hellerud JMA, Bakken TL. Family and caregivers’ experience of mental illness in migrants with intellectual disability - reflections on practice. Adv Ment Health Intellect Disabil 2019; 13(2): 76–88. [Google Scholar]
- 124.Chowdhury M, Benson BA. Deinstitutionalization and quality of life of individuals with intellectual disability: a review of the international literature. J Policy Pract Intellect Disabil 2011; 8(4): 256–65. [Google Scholar]
- 125.Chinn D, Hall I, Ali A, Hassell H, Patkas I. Psychiatric in-patients away from home: accounts by people with intellectual disabilities in specialist hospitals outside their home localities. J Appl Res Intellect Disabil 2011; 24(1): 50–60. [Google Scholar]
- 126.Beckman E, Nelson E, Labode M. Voices from the newspaper club: patient life at a state psychiatric hospital (1988–1992). J Med Humanit 2022; 43(1): 179–95. [DOI] [PubMed] [Google Scholar]
- 127.Wooster L, McCarthy J, Chaplin E. Outcomes of an inner city forensic intellectual disability service. J Intellect Disabil Offend Behav 2018; 9(1): 1–8. [Google Scholar]
- 128.Williams EM, Rose J. Nonpharmacological treatment for individuals with intellectual disability and “personality disorder”. J Appl Res Intellect Disabil 2020; 33(4): 767–78. [DOI] [PubMed] [Google Scholar]
- 129.Cheshire L, McCarthy J, Devapriam J, Chester V, Graham A, Grace J, et al. Home visits: a reflection on family contact in a specialist forensic intellectual disability service. Adv Ment Health Intellect Disabil 2015; 9(4): 186–95. [Google Scholar]
- 130.Alexander RT, Crouch K, Halstead S, Piachaud J. Long-term outcome from a medium secure service for people with intellectual disability. J Intellect Disabil Res 2006; 50: 305–15. [DOI] [PubMed] [Google Scholar]
- 131.Alexander RT, Chester V, Gray NS, Snowden RJ. Patients with personality disorders and intellectual disability - closer to personality disorders or intellectual disability? A three-way comparison. J Forensic Psychiatry Psychol 2012; 23(4): 435–51. [Google Scholar]
- 132.Alexander RT, Green FN, O'Mahony B, Gunaratna I, Gangadharan SK, Hoare S. Personality disorders in offenders with intellectual disability: a comparison of clinical, forensic and outcome variables and implications for service provision. J Intellect Disabil Res 2010; 54: 650–8. [DOI] [PubMed] [Google Scholar]
- 133.Crichton JH. Defining high, medium, and low security in forensic mental healthcare: the development of the matrix of security in Scotland. J Forens Psychiatry Psychol 2009; 20(3): 333–53. [Google Scholar]
- 134.Bonta J, Andrews DA. The Psychology of Criminal Conduct. Routledge, 2016. [Google Scholar]
- 135.Murphy D. Understanding offenders with autism-spectrum disorders: what can forensic services do? Adv Psychiatr Treat 2010; 16(1): 44–6. [Google Scholar]
- 136.Hare D, Gould J, Mills R, Wing L. A Preliminary Study of Individuals with Autistic Spectrum Disorders in Three Special Hospitals in England. National Autistic Society, 1999. (https://www.researchgate.net/profile/Dougal-Hare/publication/335149129_A_preliminary_study_of_individuals_with_autistic_spectrum_disorders_in_three_special_hospitals_in_England/links/5d52f4c5458515304072d2c0/A-preliminary-study-of-individuals-with-autistic-spectrum-disorders-in-three-special-hospitals-in-England.pdf). [Google Scholar]
- 137.Prout HT, Strohmer DC. EPS: Emotional Problems Scales Professional Manual for Behavior Rating Scales and the Self-Report Inventory. Psychological Assessment Resources, 1991. [Google Scholar]
- 138.Kerkela M, Gyllenberg D, Gissler M, Sillanmaki L, Keski-Santti M, Hinkka-Salomaki S, et al. Cumulative incidences of hospital-treated psychiatric disorders are increasing in five Finnish birth cohorts. Acta Psychiatr Scand 2021; 143(2): 119–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Livanou M, Singh SP, Liapi F, Furtado V. Mapping transitional care pathways among young people discharged from adolescent forensic medium secure units in England. Med Sci Law 2020; 60(1): 45–53. [DOI] [PubMed] [Google Scholar]
- 140.Reiss S. The Reiss Screen for Maladaptive Behavior Test Manual. IDS, 1988. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://doi.org/10.1192/bjo.2022.571.
click here to view supplementary material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, P.E.L., on reasonable request.