ABSTRACT
BACKGROUND:
Methicillin-resistant Staphylococcus aureus (MRSA) infection is a worldwide concern given its presence even in non-hospitalized healthy individuals, such as university students.
OBJECTIVE:
To identify in the literature the prevalence of colonization by MRSA among healthcare students.
DESIGN AND SETTING:
Integrative review of the literature conducted in Universidade Federal do Piauí.
METHOD:
A search for primary studies was performed in the following databases: Medical Literature Analysis and Retrieval System on-line; Cumulative Index to Nursing and Allied Health Literature; Web of Science; Scopus; and LILACS.
RESULTS:
This review included 27 studies that demonstrated MRSA infection prevalence ranging from 0.0 to 15.3% among students.
CONCLUSION:
The prevalence of colonization of MRSA among healthcare students is high, and the nasal cavity was cited as an important reservoir location for these microorganisms.
KEY WORDS (MeSH terms): Students, health occupations; Methicillin resistance; Methicillin-resistant Staphylococcus aureus; Staphylococcus aureus; Students
AUTHORS’ KEYWORDS: Multiresistance, Healthcare students, Colonization, Microorganisms
INTRODUCTION
Staphylococcus aureus is considered to be a persistent member of the human endogenous microbiota and has historically been associated with important and serious cases of infection. It has the ability to rapidly develop resistance to antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) is considered to be a paradigm for bacterial infections, since it is associated with high rates of morbidity and mortality.1–3
In assisting carriers of bacterial infections or colonized or infected patients, or in handling contaminated objects, healthcare workers’ hands can become contaminated. These workers may subsequently transmit the microorganism to other patients. However, this situation is not exclusive to the hospital environment. Clinically manifested diseases in the community or in professionals and/or patients may lead to situations in which some individuals are asymptomatic carriers, also called colonized individuals or simply carriers, when the disease is present in the host organism without causing apparent manifestations.1,4 In the United States and Taiwan, the prevalence of strains acquired in the community is 52%, thus exceeding the proportion of strains acquired in hospital environments.5 There have also been reports of cases of MRSA acquired in the community.6,7
Healthcare students play an important role in the epidemiology and pathogenesis of Staphylococcus aureus infection and can act as a source of dissemination both in the community and in hospital environments, and for carrying bacteria from one of these environments to another.1
In Brazil, this topic has been little addressed, but it is known that the presence of MRSA among students has been gradually spreading.1 Hence, it has become relevant to summarize the knowledge of MRSA that has resulted from research on this subject.
OBJECTIVE
The objective of this study was to identify in the literature the prevalence of colonization by methicillin-resistant Staphylococcus aureus among healthcare students.
METHODS
Research design
This study was an integrative review of the literature, incorporating a method of searching for secondary data.8 To preserve methodological rigor, the following steps were taken to conduct this review: formulation of the research question; idealization of sampling plan and data collection strategies; extraction of relevant data from studies included in the review; and, finally, analysis and interpretation of the data.8
The research question was elaborated in accordance with the PVO strategy (P – population; V – variable of interest; O – outcome). Thus, in line with the objective of the study, the following structure was used: P - healthcare students; V – methicillin-resistant Staphylococcus; O – prevalence.9 Therefore, the following question was asked: “What evidence is available in the literature regarding the prevalence of methicillin-resistant Staphylococcus aureus colonization among healthcare students?”
Data collection period
Searching for and selection of studies took place between the months of November 2019 and January 2020 and were carried out by two independent reviewers. Any divergences were resolved by a third reviewer.
Selection criteria
After the search stage, original articles were selected, based on reviewing their titles and abstracts, in accordance with the following inclusion criteria: original articles covering the population of undergraduate students in the field of healthcare who experienced clinical activities that brought them into direct contact with patients.
The full text of each article was then read, with a view to choosing studies that answered the research question. Through this process, articles involving high school or technical students, those that did not comply with selection criteria mentioned above, those that did not answer the research question and those that were duplicates were excluded, as also were opinion articles, theoretical reflections, dissertations and book chapters.
Data collection
The following databases were selected: Medical Literature Analysis and Retrieval System online (MEDLINE) via National Library of Medicine National Institutes of Health (PubMed); Cumulative Index to Nursing and Allied Health Literature (CINAHL); Web of Science; Scopus; and Literatura Latino-americana e do Caribe em Ciências da Saúde (LILACS) via Biblioteca Virtual em Saúde (BVS).
The descriptors and keywords used in the search were applied in accordance with particularities of each database. They were obtained by consulting the Descritores em Ciências da Saúde (DeCS), Medical Subject Headings (MeSH) and titles from CINAHL. During the search, descriptors were cross-referenced with each other using the Boolean operators “or” and “and”. Descriptors were inserted in the English language, since all journals indexed in these databases have descriptors in English in their articles; with the exception of BVS, in which descriptors were inserted in English and Portuguese. To expand the search, there was no limitation on the time of publication or language. Table 1 shows the descriptors used in this study and summarizes how the search was carried out.
Table 1. Descriptors used in the search strategy for primary articles. Teresina (PI), Brazil, 2020.
| Data Source | |
|---|---|
| Descriptors and Keywords | |
| BVS | |
| Estudantes OR Estudantes de Ciências da Saúde OR Estudantes de Enfermagem OR Estudantes de Farmácia OR Estudantes de Medicina OR Aluno OR Alunos OR Estudante OR Enfermeiras Estudantes OR Alunos de Enfermagem OR Estudante de Enfermagem OR Enfermeiros Estudantes | |
| Staphylococcus aureus | |
| Resistência à meticilina | |
| PubMed/ WEB OF SCIENCE/ SCOPUS | |
| “Students” OR “Students, Health Occupations” OR “Students, Nursing” OR “Students, Pharmacy” OR “Students, Medical” OR Students, Dental” OR “Health Occupations Students” OR “Health Occupations Student” OR “Student, Nursing” OR “Nursing Student” OR “Nursing Students” OR “Pharmacy Students” OR “Student, Pharmacy” OR “Pharmacy Student” OR “Medical Students” OR “Student, Medical” OR “Medical Student” OR “Dental Students” OR “Student, Dental” OR “Dental Student” | |
| “Staphylococcus aureus” | |
| “Methicillin Resistance” OR “Resistance, Methicillin” OR “Methicillin-Resistant” OR “Methicillin Resistant” | |
| CINAHL | |
| Students, Health Occupations | |
| Staphylococcus aureus | |
| Methicillin-Resistant Staphylococcus Aureus | |
Data processing and analysis
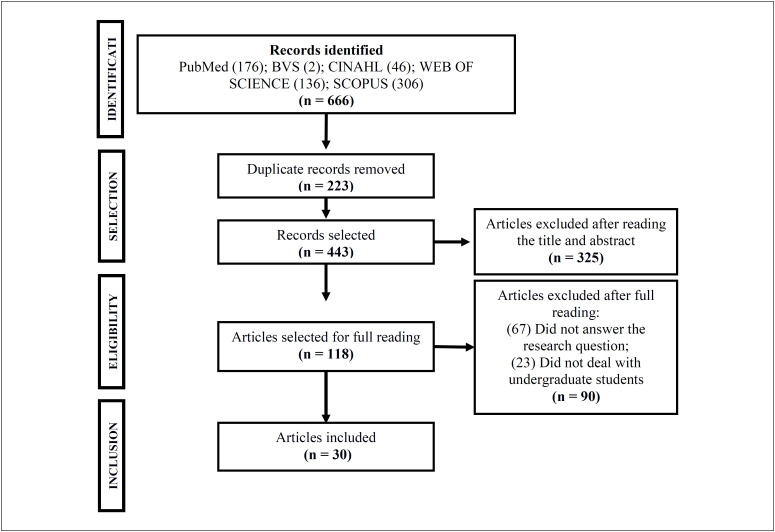
The studies thus found were exported to the Endnote reference manager software, version 20 (Clarivate Analytics, Philadelphia, United States), in order to identify duplicates and gather together all publications. In addition, the reference lists of these articles were consulted in order to find any additional studies. The selection of studies followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)9 (Figure 1).
Figure 1. Study selection flowchart. Teresina (PI), Brazil, 2020.
For data analysis and extraction, a data collection instrument that had been validated by Ursi was chosen for this study and was adapted for use in it.10 Furthermore, the protocol for this review was previously assessed by experts in the method used. After fully evaluating the texts, a descriptive analysis on the results found was carried out, in which a synthesis of all the studies included in the review was presented, along with comparisons between them.
RESULTS
The final sample for this review comprised 30 primary articles, which were characterized taking into account the authors, year of publication, country, objective and main results (Table 2). These studies were published in the years 2010, 2012, 2013, 2014, 2015, 2016, 2017, 2018 and 2019.3,5,7,11–37
Table 2. Characterization of studies included in this review (n = 30). Teresina (PI), Brazil, 2020.
| Article | Authors/Year | Location | Objective | Site |
|---|---|---|---|---|
| A1 | Prates et al.11 2010 | Brazil | To determine the prevalence of nasal transportation of S. aureus in university students. | Nostrils |
| A2 | Syafinaz et al.12 2012 | Malaysia | To determine the prevalence of S. aureus nasal carriers among medical students. | Nostrils |
| A3 | Bettin et al.13 2012 | Colombia | To investigate the nasal transportation of Panton-Valentin leukocidin-positive S. aureus strains, categories of transportation and risk factors associated with colonization, in medical students. | Nostrils |
| A4 | Chen et al.14 2012 | China | To investigate whether clinical exposure in the hospital affects MRSA nasal transportation among medical students. | Nostrils |
| A5 | Sabri et al.16 2013 | Palestine | To investigate the prevalence of nasal transportation of S. aureus and MRSA. | Nostrils |
| A6 | López-Aguilera et al.15 2013 | Spain | To determine the prevalence of nasal carriers of sensitive and methicillin-resistant S. aureus and evaluate knowledge of and adherence to hand hygiene among students. | Nostrils |
| A7 | Mat Azis et al.17 2014 | Malaysia | To evaluate the transportation of S. aureus and its persistence in students of health sciences. | Nostrils |
| A8 | Malik et al.18 2014 | Brunei | To determine the prevalence of the status of nasal carrier of S. aureus and MRSA among healthy young people. | Nostrils |
| A9 | Krishnamurthy et al.19 2014 | India | To examine the influence of exposure to the hospital environment on MRSA transportation, MRSA antimicrobial resistance patterns and presence of genes that encode five determinants of extracellular pathogenicity. | Nostrils, throat and hand palms |
| A10 | Demirel et al.20 2014 | Turkey | To investigate the prevalence of methicillin-sensitive (CA-MSSA) and resistant (CA-MRSA) S. aureus, including inducible sleepers (ID-MRSA), in S. aureus and MRSA strain genotypes from nasal cultures. | Nostrils |
| A11 | Renushri et al.21 2014 | India | To assess the influence of exposure to the hospital environment on MRSA transportation. | Nostrils and throat |
| A12 | Ribeiro et al.22 2014 | Brazil | To identify S. aureus and MRSA in university students. | Nostrils and palm hands |
| A13 | Holý et al.24 2015 | Czech Republic | To investigate the prevalence of nasal transportation of S. aureus and MRSA in healthy people aged 18–26 years. To find out whether the prevalence of nasal transportation strains of S. aureus and MRSA varies over the years of studies. To compare general medical students from year 1 and year 5 for nasal transportation of S. aureus and MRSA strains. | Nostrils |
| A14 | Zakai et al.23 2015 | Saudi Arabia | To identify MRSA nasal carrier status among medical students during their clinical rotations. | Nostrils |
| A15 | Collazos Marín et al.25 2015 | Colombia | To establish the genetic diversity of S. aureus isolates and detect the presence of mecA gene in isolated strains in asymptomatic medical students who were in their clinical rotation phase in a hospital. | Nostrils |
| A16 | Petti et al.26 2015 | Italy | To evaluate the MRSA carrier rate in a sample of dental students. | Nostrils, throat and palm hands |
| A17 | Hogan et al.3 2016 | Madagascar | To examine the prevalence and clonal epidemiology of nasal S. aureus and MRSA among healthcare professionals and non-medical university students. | Nostrils |
| A18 | Javaeed et al.27 2016 | Pakistan | To assess the prevalence of MRSA transportation in healthy medical students. | Nostrils |
| A19 | Subri et al.28 2016 | Malaysia | To determine the prevalence of nasal colonization of S. aureus and its susceptibility to antibiotics among pre-clinical and clinical physicians and nursing students. | Nostrils |
| A20 | Ansari et al.29 2016 | Nepal | To evaluate the rate of nasal colonization of S. aureus, its methicillin-resistant strains and risk factors in medical students before clinical exposure. | Nostrils |
| A21 | Okamo et al.30 2016 | Tanzania | To determine the prevalence of S. aureus and MRSA nasal transportation among medical students, and the antimicrobial susceptibility of isolated profiles of S. aureus, and to verify the association of S. aureus nasal transportation with demographic and clinical characteristics. | Nostrils |
| A22 | Baek et al.31 2016 | South Korea | To determine the prevalence rate of nasal colonization by MRSA among dental students and identify the characteristics of the strains isolated. | Nostrils |
| A23 | Radhakrishna et al.32 2016 | India | To establish the prevalence and pattern of S. aureus antibiograms, with special emphasis on MRSA among students of the second year. | Nostrils |
| A24 | Abroo et al.7 2017 | Iran | To investigate the prevalence, antimicrobial susceptibility and molecular factors characteristic of CA (community acquired) MRSA among two groups of college students (medical and non-medical). | Nostrils |
| A25 | Budri et al.33 2018 | Ireland | To investigate co-located nasal Staphylococcus aureus and coagulase-negative staphylococci (CoNS), recovered from healthy medical students in a preclinical year and the transportation of genes and common elements to both species that may contribute to the evolution of S. aureus and MRSA. | Nostrils |
| A26 | Al-Tamimi et al.34 2018 | Jordan | To investigate the prevalence, standard antimicrobial susceptibility, antibiotic resistance genes and risk factors of medical students with MRSA. | Nostrils |
| A27 | Suhaili et al.35 2018 | Malaysia | To evaluate the antimicrobial susceptibility profile of S. aureus strains isolated from university students and to determine the prevalence of resistance to constitutive and inducible clindamycin, in which the latter would be capable of causing therapeutic failure due to false in vitro susceptibility to clindamycin. | Nostrils |
| A28 | Onanuga et al.36 2019 | Nigeria | To determine the antibiogram and the virulent characteristics of nasal S. aureus, accessing its profile of resistance to antibiotics and potential pathogens in healthy students at the University of the Niger Delta, Bayelsa State, Nigeria. | Nostrils |
| A29 | Szymanek-Majchrzak et al.37 2019 | Poland | To evaluate and compare the level of colonization of S. aureus (MRSA or MSSA) among medical students and evaluate the sensitivity of the strains. | Nostrils |
| A30 | Efa et al.5 2019 | Ethiopia | To determine the nasal transportation of MRSA and its antimicrobial susceptibility patterns among medical students at the Jimma University Medical Center (JUMC), southwestern Ethiopia. | Nostrils |
Regarding the locations of the studies, they were carried out in Brazil, Malaysia, Colombia, China, Palestine, Spain, Brunei, India, Turkey, Czech Republic, Saudi Arabia, Madagascar, Pakistan, Nepal, Tanzania, South Korea, Iran, Ireland, Jordan, Italy, Nigeria, Poland and Ethiopia.3,5,7,11,12,14–22,24–37
The populations addressed by the researchers of these 30 studies were nursing students, medical students, health science students and dental students.3,5,7,12–18,20,21,23–25,27,29–30,33–37 Two studies involved students from more than one undergraduate course.11,22,28
To detect colonizing microorganisms, samples were collected using the technique of swab smears from nasal specimens, in all of these studies except for four studies, in which specimens were collected from more than one anatomical site.3,5,7,15–17,18–27–30,33–37
Regarding the prevalence of MRSA, the student population in some studies was divided into groups before exposure to healthcare and after such exposure.14,19,21,23,26 The percentages found are shown in Table 3.
Table 3. Prevalence of methicillin-resistant Staphylococcus aureus, according to the studies included in this review.
| General students | Students before clinical exposure | Students after clinical exposure | |
|---|---|---|---|
| A1 | 2.4% | – | – |
| A2 | 0.0% | – | – |
| A3 | 1.61% | – | – |
| A4 | 2.2% | 1.9% | 2.4% |
| A5 | 9.0% | – | – |
| A6 | 2.1% | – | – |
| A7 | 3.3% | – | – |
| A8 | – | 0.0% | – |
| A9 | 6.8 % | 4.0% | 9.0% |
| A10 | 3.0% | – | – |
| A11 | 8.2% | 4.0% | 11.8% |
| A12 | 1.9% | – | – |
| A13 | 0.0% | – | – |
| A14 | 15.3% | 0.0% | 6.7% |
| A15 | 14.3% | – | – |
| A16 | 3.2% | 3.1% | 0.0% |
| A17 | 1.3% | – | – |
| A18 | 5.5% | – | – |
| A19 | 0.0% | – | – |
| A20 | – | 4.0% | – |
| A21 | 0.3% | 0.0% | 0.3% |
| A22 | 3.1% | – | 3.1% |
| A23 | 6.1% | – | – |
| A24 | 13.1% | – | – |
| A25 | 2.1% | 2.1% | – |
| A26 | 4.1% | – | – |
| A27 | 8% | – | – |
| A28 | 7.1% | – | – |
| A29 | 0.1% | – | – |
| A30 | 8.4% | – | – |
DISCUSSION
Worldwide, occurrence of healthcare-associated infections (HAI) is one of the main public health problems, with severe human and economic repercussions. According to the Centers for Disease Control and Prevention (CDC), MRSA infections have outperformed HIV as the leading cause of morbidity and mortality in the United States.38
Studies have revealed high prevalence of MRSA in patients and healthcare professionals with exposure to the healthcare system.23,38,39 However, the results systematized in the present study revealed that presence of MRSA has also been reported among non-hospitalized healthy individuals, such as undergraduate students, ranging from 0.0% to 15.3%.14,25,26
Data in the literature have highlighted occurrences of MRSA infection in healthy populations that live in agglomerations or experience such conditions but which have little or no contact with healthcare services, as is the case of undergraduate students within the field of healthcare.1,40 This was observed in the present study, thus indicating that MRSA infection was present in students who were not exposed to hospital environments. This may indicate the presence of community-acquired MRSA strains.1 It needs to be borne in mind that in the studies discussed here, students who had been hospitalized within the last few months had been excluded, considering that hospitalization could be a confounding factor for occurrences of MRSA.
Identification of high frequencies of MRSA in students before they were exposed to experiences of clinical care is a matter for concern. It indicates that there is a need for effective infection prevention and control policies, in relation to hygiene and surveillance.5
Clinical practice among students in the field of healthcare is part of the teaching-learning process. In relation to this process, there is exposure to occupational risks, especially through recognition of the variability of care provided to patients.1,5 In this regard, studies that have addressed the prevalence of MRSA among students after exposure to hospital environments can provide evidence that exposure to MRSA in hospitals can play a critical role in achieving nasal colonization by MRSA.
According to the literature, the nostrils are the main colonization site for Staphylococcus aureus, whose prevalence reaches, on average, 40% in the adult population.1,5–6 Possibly for this reason, the nasal cavity was the site most chosen by researchers for sample collection in their studies, thus showing the importance of the upper airways in transmission and acquisition of pathogenic microorganisms. The throat and palms are also important reservoirs for MRSA.19,21,22,26
It is known that students in the field of healthcare, as they progress through the curriculum with increasing complexity of care practices, whether in hospitals or other healthcare delivery environments, become carriers of microbes. In this, acquisition of Staphylococcus aureus is considered to be a major concern, especially with regard to MRSA.1
Thus, MRSA rates in students may increase according to their clinical exposure, as well as from isolated occurrences. In another study, there was greater potential for virulence in samples from groups working in clinics.5 This aspect of infection could not be analyzed in the present study, since the studies included in this review were cross-sectional, which did not allow the study sample to be monitored.
The prevalences found need to be analyzed with caution, considering that occurrences of infections caused by MRSA may differ according to the scenarios within which they occur. This may be due to measures that are taken to control infection and may be dependent on effective implementation.5 Likewise, the MRSA rate also varies in different locations.27,41
This study presented some limitations due to the choice of databases and keywords. Use of the CINAHL database may have restricted the search, as it is a specific database for the field of nursing. In addition, the choice of databases and keywords may have camouflaged studies on the same topic that were not indexed in the same database. Hence, it can be suggested that similar investigations should be conducted, with cross-referencing of other databases, in order to investigate Brazilian scientific production on colonization by Staphylococcus aureus among healthcare students.
CONCLUSION
The prevalence of colonization by methicillin-resistant Staphylococcus aureus among healthcare students is high, and the nasal cavity was cited in this study as an important reservoir for these microorganisms.
Efforts need to be made to implement standards and routines that are designed to limit the spread of MRSA strains among students, given that once MRSA has become established within a community, its eradication and control is difficult. Furthermore, in view of the high morbidity and mortality and exponential growth of series of microbial resistance, implementation of control strategies is prudent.
Therefore, education on infection control measures in undergraduate healthcare courses is of great importance, as also is implementation of adequate and effective infection control programs to reduce the prevalence of MRSA.
Footnotes
Nursing Postgraduate Program, Universidade Federal do Piauí (UFPI), Teresina (PI), Brazil; Nursing Postgraduate Program, Universidade Federal de Mato Grosso do Sul, Três Lagoas (MG), Brazil; and Department of Dentistry, Centro Universitário Santo Agostinho, Teresina (PI), Brazil
Sources of funding: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), grant number 88882.446296/2019-01
REFERENCES
- 1.Carvalho MS, Andrade DF, Sousa ÁF, et al. Nasal colonization with Staphylococcus aureus in nursing students: ground for monitoring. Rev Bras Enferm. 2016;69(6):1046–1051. doi: 10.1590/0034-7167-2016-0210. [DOI] [PubMed] [Google Scholar]
- 2.Abulkasim GS, Shukla HK, Masih H. Antimicrobial resistance of staphylococcus aureus among healthy and adult students. Int J Pharm Sci Res. 2017;8(12):5247–5251. Available from: https://ijpsr.com/bft-article/antimicrobial-resistance-of-staphylococcus-aureus-among-healthy-and-adult-students/?view=fulltext. [Google Scholar]
- 3.Hogan B, Rakotozandrindrainy R, Al-Emran H, et al. Prevalence of nasal colonisation by methicillin-sensitive and methicillin-resistant Staphylococcus aureus among healthcare workers and students in Madagascar. BMC Infect Dis. 2016;16(1):420–420. doi: 10.1186/s12879-016-1733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almeida GCM, Lima NG, Santos MM, Melo MCN, Lima KC. Colonização nasal por Staphylococcus sp. em pacientes internados. Acta Paul Enferm. 2014;27(3):273–279. doi: 10.1590/1982-0194201400046. [DOI] [Google Scholar]
- 5.Efa F, Alemu Y, Beyene G, Gudina EK, Kebede W. Methicillin-resistant Staphylococcus aureus carriage among medical students of Jimma University, Southwest Ethiopia. Heliyon. 2019;5(1):e01191. doi: 10.1016/j.heliyon.2019.e01191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moremi N, Claus H, Vogel U, Mshana SE. The role of patients and healthcare workers Staphylococcus aureus nasal colonization in occurrence of surgical site infection among patients admitted in two centers in Tanzania. Antimicrob Resist Infect Control. 2019;8:102–102. doi: 10.1186/s13756-019-0554-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abroo S, Hosseini Jazani N, Sharifi Y. Methicillin-resistant Staphylococcus aureus nasal carriage between healthy students of medical and nonmedical universities. Am J Infect Control. 2017;45(7):709–712. doi: 10.1016/j.ajic.2017.02.034. [DOI] [PubMed] [Google Scholar]
- 8.Galvão CM, Mendes KDS, Silveira RCCP. Revisão integrativa: método de revisão para sintetizar as evidências disponíveis na literatura. In: Brevidelli MM, Sertório SCM, editors. Trabalho de conclusão de curso: guia prático para docentes e alunos da área da saúde. São Paulo: Iátria; 2010. pp. 105–126. [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ursi ES, Gavão CM. Prevenção de lesões de pele no perioperatório: revisão integrativa da literatura [Perioperative prevention of skin injury: an integrative literature review] Rev Lat Am Enfermagem. 2006;14(1):124–131. doi: 10.1590/s0104-11692006000100017. [DOI] [PubMed] [Google Scholar]
- 11.Prates KA, Torres AM, Garcia LB, et al. Nasal carriage of methicillin-resistant Staphylococcus aureus in university students. Braz J Infect Dis. 2010;14(3):316–318. [PubMed] [Google Scholar]
- 12.Syafinaz AM, Nur Ain NZ, Nadzirahi SN, et al. Staphylococcus aureus Nasal Carriers Among Medical Students in A Medical School. Med J Malaysia. 2012;67(6):636–638. [PubMed] [Google Scholar]
- 13.Bettin A, Causil C, Reyes N. Molecular identification and antimicrobial susceptibility of Staphylococcus aureus nasal isolates from medical students in Cartagena, Colombia. Braz J Infect Dis. 2012;16(4):329–334. doi: 10.1016/j.bjid.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Chen CS, Chen CY, Huang YC. Nasal carriage rate and molecular epidemiology of methicillin-resistant Staphylococcus aureus among medical students at a Taiwanese university. Int J Infect Dis. 2012;16(11):e799–e803. doi: 10.1016/j.ijid.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 15.López-Aguilera S, Goñi-Yeste M del M, Barrado L, et al. Colonización nasal por Staphylococcus aureus en estudiantes de medicina: importancia en la transmisión hospitalaria [Staphylococcus aureus nasal colonization in medical students: importance in nosocomial transmission] Enferm Infecc Microbiol Clin. 2013;31(8):500–505. doi: 10.1016/j.eimc.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Sabri I, Adwan K, Essawi TA, Farraj MA. Molecular characterization of methicillin-resistant Staphylococcus aureus isolates in three different Arab world countries. Eur J Microbiol Immunol (Bp) 2013;3(3):183–187. doi: 10.1556/EuJMI.3.2013.3.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mat Azis N, Hamid AAB, Pung HP, et al. Staphylococcus aureus infection risk in a population of health sciences students at a public university. Iranian J Publ Health. 2014;43(Suppl 12):112–116. Available from: https://ijph.tums.ac.ir/index.php/ijph/article/view/4887. [Google Scholar]
- 18.Malik NFA, Muharram SH, Abiola O. Staphylococcus aureus nasal carriage in young healthy adults in Brunei Darussalam. Brunei Int Med J. 2014;10(2):78–84. [Google Scholar]
- 19.Krishnamurthy V, Saha A, Renushri BV, Nagaraj ER. Methicillin Resistant Staphylococcus aureus Carriage, Antibiotic Resistance and Molecular Pathogenicity among Healthy Individuals Exposed and Not Exposed to Hospital Environment. J Clin Diagn Res. 2014;8(7):DC04–DC08. doi: 10.7860/JCDR/2014/8409.4638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demirel G, Findik D, Dagi HT, Arslan U. Community-acquired methicillin-resistant Staphylococcus aureus and genotypes among university students in Turkey. Southeast Asian J Trop Med Public Health. 2014;45(6):1401–1409. [PubMed] [Google Scholar]
- 21.Renushri BV, Saha A, Nagaraj ER, et al. Screening for methicillin-resistant Staphylococcus aureus carriers among individuals exposed and not exposed to the hospital environment and their antimicrobial sensitivity pattern. Annals of Tropical Medicine and Public Health. 2014;7(1):19–24. Available from: https://cyberleninka.org/article/n/503731. [Google Scholar]
- 22.Ribeiro IF, Silva SFR, Silva SL, et al. Identificação de Staphylococcus aureus e Staphylococcus aureus resistente à meticilina em estudantes universitários. Rev Ciênc Farm Básica Apl. 2014;35(2):299–302. Available from: https://rcfba.fcfar.unesp.br/index.php/ojs/article/view/145/143. [Google Scholar]
- 23.Zakai SA. Prevalence of methicillin-resistant Staphylococcus aureus nasal colonization among medical students in Jeddah, Saudi Arabia. Saudi Med J. 2015;36(7):807–812. doi: 10.15537/smj.2015.7.11609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holý O, Vlčková J, Matoušková I, Kolář M. Prevalence výskytu nosního nosičství kmenů Staphylococcus aureus a meticilin rezistentních kmenů S. aureus (MRSA) u studentů všeobecného lékařství LF UP v Olomouci [The prevalence of nasal carriage of Staphylococcus aureus and methicillin-resistant S. aureus (MRSA) among general medicine students of the Palacky University Olomouc] Epidemiol Mikrobiol Imunol. 2015;64(2):98–101. [PubMed] [Google Scholar]
- 25.Collazos Marín LF, Estupiñan Arciniegas G, Chavez Vivas M. Characterization of Staphylococcus aureus Isolates That Colonize Medical Students in a Hospital of the City of Cali, Colombia. Int J Microbiol. 2015;2015:358489–358489. doi: 10.1155/2015/358489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petti S, Kakisina N, Volgenant CM, et al. Low methicillin-resistant Staphylococcus aureus carriage rate among Italian dental students. Am J Infect Control. 2015;43(12):e89–e91. doi: 10.1016/j.ajic.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Javaeed A, Khan S, Haqsubhani RU, Ghauri SK, Jahan S. Methicillin Resistant Staphylococcus Aureus Prevalence of Nasal Carriage among Healthy MBBS Students of Continental Medical College, Lahore. P J M H S. 2016;10(3):1057–1059. Available from: https://pjmhsonline.com/2016/july_sep/pdf/1057.pdf. [Google Scholar]
- 28.Subri NIBM, Hlaing SS, Myint T, et al. Nasal Carriage of Staphylococcus aureus and Its Antibiotic Susceptibility Pattern among Medical and Nursing Students. Asian J Pharm. 2016;10(4):736–740. doi: 10.22377/ajp.v10i04.917. [DOI] [Google Scholar]
- 29.Ansari S, Gautam R, Shrestha S, et al. Risk factors assessment for nasal colonization of Staphylococcus aureus and its methicillin resistant strains among pre-clinical medical students of Nepal. BMC Res Notes. 2016;9:214–214. doi: 10.1186/s13104-016-2021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Okamo B, Moremi N, Seni J, et al. Prevalence and antimicrobial susceptibility profiles of Staphylococcus aureus nasal carriage among pre-clinical and clinical medical students in a Tanzanian University. BMC Res Notes. 2016;9:47–47. doi: 10.1186/s13104-016-1858-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baek YS, Baek SH, Yoo YJ. Higher nasal carriage rate of methicillin-resistant Staphylococcus aureus among dental students who have clinical experience. J Am Dent Assoc. 2016 May;147(5):348–353. doi: 10.1016/j.adaj.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Radhakrishna M, Taneja A, Rao P. Nasal carriage of Staphylococcus aureus with special emphasis on methicillin-resistant Staphylococcus aureus among students of a south Indian medical college - prevalence and antibiogram pattern. Asian J Pharm Clin Res. 2016;9(8):129–132. doi: 10.22159/ajpcr.2016.v9s2.13274. [DOI] [Google Scholar]
- 33.Budri PE, Shore AC, Coleman DC, et al. Observational cross-sectional study of nasal staphylococcal species of medical students of diverse geographical origin, prior to healthcare exposure: prevalence of SCCmec, fusC, fusB and the arginine catabolite mobile element (ACME) in the absence of selective antibiotic pressure. BMJ Open. 2018 Apr 20;8(4) doi: 10.1136/bmjopen-2017-020391. e020391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Tamimi M, Himsawi N, Abu-Raideh J, Jazar DA, Al-jawaldeh H, Mahmoud SAH. Nasal colonization by methicillin-sensitive and methicillin-resistant Staphylococcus aureus among medical students. J Infect Dev Ctries. 2018;12(5):326–335. doi: 10.3855/jidc.9908. [DOI] [PubMed] [Google Scholar]
- 35.Suhaili Z, Rafee P’, Mat Azis N, et al. Characterization of resistance to selected antibiotics and Panton-Valentine leukocidin-positive Staphylococcus aureus in a healthy student population at a Malaysian University. Germs. 2018;8(1):21–30. doi: 10.18683/germs.2018.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Onanuga A, Eboh DD, Okou GT. Antibiogram and Virulence Characteristics of Multi-drug Resistant Staphylococcus aureus from Nasal Cavity of Healthy Students of Niger Delta University, Amassoma, Bayelsa State, Nigeria. Journal of Clinical and Diagnostic Research. 2019;13(7):24–29. doi: 10.7860/JCDR/2019/41396.13031. [DOI] [Google Scholar]
- 37.Szymanek-Majchrzak K, Kosiński J, Żak K, et al. Prevalence of methicillin resistant and mupirocin-resistant Staphylococcus aureus strains among medical students of Medical University in Warsaw. Przegl Epidemiol. 2019;73(1):39–48. doi: 10.32394/pe.73.05. [DOI] [PubMed] [Google Scholar]
- 38.Centers for disease control and prevention (CDC) Healthcare-associated infections. Current HAI Progress Report. 2019 National and State Healthcare-Associated Infections Progress Report. Available from: http://www.cdc.gov/hai/progress-report/index.html. [Google Scholar]
- 39.Rohde RE, Rowder C, Patterson T, et al. Methicillin resistant Staphylococcus aureus (MRSA): an interim report of carriage and conversion rates in nursing students. Clin Lab Sci. 2012;25(2):94–101. doi: 10.29074/ascls.25.2.94. [DOI] [PubMed] [Google Scholar]
- 40.Evangelista SS, Oliveira AC. Staphylococcus aureus meticilino resistente adquirido na comunidade: um problema mundial. Rev Bras Enferm. 2015;68(1):136–141. doi: 10.1590/0034-7167.2015680119p. [DOI] [PubMed] [Google Scholar]
- 41.Conceição T, de Lencastre H, Aires-de-Sousa M. Carriage of Staphylococcus aureus among Portuguese nursing students: A longitudinal cohort study over four years of education. PLoS One. 2017;12(11) doi: 10.1371/journal.pone.0188855. e0188855. [DOI] [PMC free article] [PubMed] [Google Scholar]