Abstract
PURPOSEWe aimed to determine the safety and feasibility of transradial access (TRA) in bronchial artery and non-bronchial systemic artery (NBSA) embolization in patients with non-massive hemoptysis.
METHODS This retrospective study was approved by the Institutional Review Board. Among the 300 patients treated for hemoptysis with bronchial artery and NBSA embolization between April 2018 and July 2019, 19 procedures in 19 patients were conducted by TRA and were retrospectively analyzed. TRA was considered when the bronchial artery or NBSA originated from the arch vessel or its tributaries. The exclusion criteria of TRA included Barbeau C or D waveform and a radial artery diameter of less than 1.8 mm on ultrasound. TRA was also avoided in cases of the high-origin bronchial artery (i.e., T4 or higher level of the aorta). The hemoptysis-free time was estimated using the Kaplan–Meier method.
RESULTS The technical success (i.e., embolization of all target artery with TRA) rate was 94.7% (18 out of 19 patients). In terms of the target arteries, embolization with TRA was technically successful in treating 47 out of 48 arteries (97.9%). The 1-month and 6-month hemoptysis-free rates were 89.5% (17/19) and 73.7% (14/19), respectively. The only adverse event was iatrogenic dissection of the bronchial artery with little clinical significance in 1 patient. No access site complications were identified on post-procedure day 1 ultrasonography.
CONCLUSION With proper patient selection, TRA offers a safe and effective approach to embolize the bronchial arteries and NBSAs in patients with hemoptysis.
Main points
Transradial embolization of the bronchial and non-bronchial systemic artery yielded a sufficiently high effectiveness and safety profile.
Transradial embolization for hemoptysis can provide an easier selection of the culprit arteries from the subclavian artery or its tributaries.
The number of arch vessels that should be crossed can be reduced by the proper use of transradial access in treating patients with hemoptysis.
With a careful patient selection, transradial access offers a safe and effective approach to embolize the bronchial and non-bronchial systemic arteries. Thus, it needs to be considered as a supplement or substitute of transfemoral access.
In arterial interventional procedures, transradial access (TRA) provides benefits including better patient comfort, fewer access site complications, earlier ambulation, and decreased hospital costs.1,2 Therefore, the TRA has been increasingly used for procedures such as chemoembolization, radioembolization, renal artery interventions, uterine artery embolization, and prostate artery embolization procedures.3-6 Despite this trend, few reports have explored the application of TRA for embolization in patients with hemoptysis.7
Bronchial artery embolization is a safe, effective, and minimally invasive treatment option for hemoptysis.8-11 Conventionally, it is indicated as a treatment for massive hemoptysis, which is defined as 300-600 mL of bleeding within 24 h.12-14 Recently, however, this procedure has been widely performed to treat mild-to-moderate hemoptysis as well,12-14 as the safety profile in recent practice has been satisfactory, probably because of the use of small-bore microcatheters and super-selective technique.15,16 Although the hypertrophic bronchial artery is usually the cause of bleeding in many cases, non-bronchial systemic arteries (NBSA) and ectopic bronchial arteries sometimes serve as culprit arteries. Because these vessels frequently originate from the arch vessels,17,18 using transfemoral access (TFA), catheterization of the culprit arteries can be difficult, especially in patients with tortuous arch vessel anatomy. By contrast, TRA from the ipsilateral radial artery can be more technically advantageous by providing a short and straight course to the target vessels.
Given the known benefits of TRA in noncoronary interventions and the additional advantage in embolotherapy for hemoptysis, the efficacy of TRA in this procedure needs to be scrutinized. Therefore, this retrospective study was conducted to determine the safety and efficacy of TRA in bronchial artery and NBSA embolization for non-massive hemoptysis.
Methods
Patients
This retrospective study was approved by our institutional review board (approval number: 2019-3977) and the requirement for informed consent from patients was waived. An electronic medical record search engine was used to retrieve 300 embolization procedures for hemoptysis at a tertiary hospital from April 2018 to July 2019. Among these, 20 procedures in 20 patients were initially planned to be conducted using TRA, and 18 cases were actually performed using TRA. The remaining 2 patients were treated with transfemoral embolization because of small sizes of the radial artery (≤1.8 mm) on ultrasonography (US). In 1 patient, the embolization procedure commenced with a TFA; however, additional TRA was required to catheterize the NBSA from the subclavian artery. Overall, 19 hemoptysis patients treated by transradial embolization were included in this study. Descriptive statistics of demographic data are presented in Table 1.
Table 1.
Demographic data of the 19 patients in this study
| Variable | Descriptive statistics |
|---|---|
|
Sex
a
Male Female |
13 (68.42) 6 (31.58) |
| Age (years) b | 66 (59-75) |
| Etiology a | |
| Tuberculosis | 9 (47.37) |
| Bronchiectasis | 4 (21.05) |
| NTM infection | 3 (15.79) |
| Pneumonia | 1 (5.26) |
| Actinomycosis | 1 (5.26) |
| Castleman’s disease | 1 (5.26) |
| Smoking history a | |
| Never-smoker | 11 (57.89) |
| Ex-smoker | 8 (42.11) |
| Current smoker | 0 (0) |
| Hemoglobin (g/dL) b | 12.6 (10.8-13.6) |
| Platelet (/uL) c | 226,789 ± 55,778 |
| INR b | 1.02 (0.99-1.07) |
| SpO 2 (%) b | 98 (96-100) |
NTM, non-tuberculous mycobacteria; INR, international normalized ratio.
aThe numbers in parentheses are percentages; b data are the median (interquartile range); cdata are the mean ± standard deviation.
Pre-procedural evaluation
Patients presenting with hemoptysis were initially evaluated by pulmonologists or emergency physicians. The patients were routinely scanned by a multidetector computed tomography (CT) scanner (Aquilion ONE; Canon Medical Systems, IQon-Spectral CT; Philips Healthcare, or iCT 256; Philips Healthcare) for contrast-enhanced thoracic CT angiography with a 1 mm slice thickness. Arterial phase images with multiplanar reconstruction (axial and coronal) were obtained for the evaluation of hypertrophied culprit vessels. Subsequently, interventional radiologists were consulted for evaluation of the feasibility and potential benefits of embolotherapy.
Interventional radiologists reviewed the CT images to identify the presence of hypertrophied bronchial arteries and NBSA. Tubular enhancing structures in the mediastinum or around the central airways connected to aorta or its major branches were regarded as bronchial arteries.17,18 A bronchial artery with a diameter of greater than 2 mm was defined as a hypertrophied bronchial artery and was considered a source of hemoptysis.17 With regard to the origin, bronchial arteries originating outside of the T5-T6 level of the aorta were considered to be ectopic bronchial arteries.19 NBSA was defined as a systemic artery (e.g., intercostal arteries, inferior phrenic arteries, or branches from the subclavian arteries) that courses to the lung parenchyma, usually through the inferior pulmonary ligament or through the adherent pleura.20 When enlarged NBSA were associated with pleural thickening (≥3 mm), it was regarded as the NBSA responsible for hemoptysis.20 Interventional radiologists performed the embolization procedure if there was evidence of hypertrophied bronchial arteries or NBSA.
Decision of vascular access
Decisions regarding vascular access for each patient were based on the operator’s discretion. In general, TRA was considered when there was the ectopic bronchial artery or NBSA originated from the subclavian artery or its branches. However, if the ectopic bronchial artery arose from the aortic arch or a high level of descending thoracic aorta (i.e., T4 vertebral body or higher level), TFA was preferred. When the orthotopic bronchial arteries were the only culprit vessels, TFA was considered first. Once the TRA was considered, US evaluation of the radial artery and Barbeau test21 (i.e., a modified Allen test with the use of pulse oximetry) were performed. The test was conducted with a pulse oximeter on the patients’ index finger, and pulse waveform changes depending on manual compression of the radial and ulnar artery were analyzed by the operator. Patients with Barbeau type C or D or a radial artery diameters of less than 1.8 mm underwent the procedure with TFA.22 The laterality of punctured radial artery was determined by the location of target vessels. The left radial artery was usually punctured in cases of embolizing the orthotopic bronchial arteries and branches from the left subclavian artery because this pathway crosses only the left vertebral artery among the 4 major arteries toward the brain. However, if there were culprit vessels originating from the right subclavian artery, the right radial artery was selected as the access site.
Embolization procedure
All transradial procedures were performed by one operator (J.W.C., 3 years of experience as an attending in interventional radiology) in the single-plane angiography suite (Allura Xper FD20; Philips Healthcare, Axiom Artis; Siemens, or Azurion; Philips Healthcare). The radial artery was punctured under direct US visualization using a 21-gauge echogenic-tip needle. After needle puncture, a 5 F hydrophilic vascular sheath (Prelude; Merit Medical) was introduced over the 0.018-inch guidewire. A solution of 2 mg of verapamil, 200 µg of nitroglycerin, and 1000 IU of heparin was injected slowly through the access sheath. Culprit arteries originating from the ipsilateral subclavian artery were catheterized using a 90 cm Davis catheter (Cook Medical) and a 110 cm microcatheter (Progreat lambda), and orthotopic bronchial arteries and intercostal arteries were selected using a 100 cm Cobra1 (Cook Medical) or a 110 cm Ultimate1 (Merit Medical) and 130 cm long microcatheter (Progreat lambda). In terms of embolic materials, polyvinyl alcohol (PVA) particles (Contour; Boston Scientific) which ranges 250-355 µm were primarily utilized, and larger PVA (500-710 µm) or gelatin sponge particles (1400-2000 µm) were added in patients with extensive systemic-to-pulmonary artery shunts. A wrist hemostasis band (PreludeSYNC, Merit Medical) was used to compress the puncture site for 60 min.
Post-procedural management
The puncture sites were sonographically evaluated the day after the procedure. Bronchoscopy was only conducted for a select group of patients with a high risk of lung cancer as post-infectious (e.g., tuberculosis, non-tuberculous mycobacteria infection) chronic inflammation is the main cause of hemoptysis in South Korea.23 In general, patients were discharged within 48 h of the procedure and oral tranexamic acid (for 7 days) was prescribed. The patients were advised to visit a pulmonologist 1 month after the procedure, and follow-up was continued every 3 months. In cases of recurrent hemoptysis or active lung disease such as tuberculosis or non-tuberculous mycobacteria infection, patients were treated according to the pulmonologists’ discretion.
Outcome
Technical success was defined as successful radial artery access and completion of the intended procedure (i.e., embolization of all target arteries) without conversion to TFA. Hemoptysis-free time was defined as the time from the date of embolization to the first recurrence date of hemoptysis. The occurrence of adverse events was investigated from the day of the procedure to discharge based on the medical records and post-procedural US findings and was graded according to the Society of Interventional Radiology Adverse Event Severity Scale.24
Statistical analysis
The hemoptysis-free time was calculated using the Kaplan–Meier method. Statistical analyses were performed using commercial statistics software (SPSS, version 25.0; SPSS, Inc.). Descriptive statistics of the data were presented with n (%). The D'Agostino-Pearson test was performed for numerical variables, and normalized and non-normalized variables were presented as mean ± standard deviation and median (interquartile range), respectively.
Results
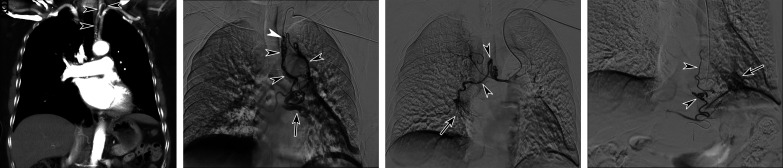
The embolization procedure using TRA was technically successful in 18 out of 19 patients (technical success rate, 94.7%). Transradial embolization was incomplete in 1 patient who had 2 orthotopic bronchial arteries and 1 NBSA (right fourth intercostal artery). One of the bronchial arteries had a very tortuous course from the aorta, and iatrogenic dissection occurred while a microcatheter entered the distal part of the artery. For the patient with incomplete embolization, crossover to TFA was not considered because the bronchial arterial flow was almost blocked due to iatrogenic dissection and the remaining target arteries were successfully embolized with TRA. In terms of the target arteries, 29 bronchial arteries (22 orthotopic and 7 ectopic bronchial arteries) and 19 NBSAs were planned to be treated, and embolization was successfully performed in all targets except the above-mentioned artery with iatrogenic dissection (Table 2). Seven ectopic bronchial arteries and 9 NBSAs originated from the subclavian artery or its branches and were successfully catheterized via the ipsilateral TRA (Figure 1). Next-day US examination of the punctured radial artery revealed a patent lumen and normal arterial waveform in all 19 patients. No access site complications including puncture site hematoma were observed. The patients were discharged within 10 days from the procedure (mean: 2.6 days).
Table 2.
Origins of the 48 target arteries
| Variable | Descriptive statistics |
|---|---|
| Orthotopic bronchial artery T5 level T6 level |
22 4 (18.18) 18 (81.82) |
| Ectopic bronchial artery Right thyrocervical trunk Left thyrocervical trunk Right internal thoracic artery Left internal thoracic artery Right subclavian artery |
7 2 (28.57) 1 (14.29) 1 (14.29) 1 (14.29) 2 (28.57) |
| Non-bronchial systemic artery Intercostal artery Right internal thoracic artery Left internal thoracic artery Left subclavian artery branch Right inferior phrenic artery Left inferior phrenic artery Right thyrocervical trunk Right lateral thoracic artery Right thoracodorsal artery |
19 7 (36.84) 2 (10.53) 1 (5.26) 1 (5.26) 2 (10.53) 1 (5.26) 3 (15.79) 1 (5.26) 1 (5.26) |
Data are presented as n (%).
Figure 1. a-d.
Computed tomography (CT) image and angiographies of a 69-year-old woman who complained of hemoptysis. A coronal-reformatted image of CT angiography (a) demonstrating the ectopic left bronchial artery (arrowheads) originated from the thyrocervical trunk. Selective angiography of the ectopic left bronchial artery (b) showed hypertrophied vessels (black arrowheads) and shunt to the pulmonary vein (arrow). Note that the microcatheter (white arrowhead) in the culprit artery had advanced deep enough to perform safe embolization. After catheterization of the orthotopic right bronchial artery, selective angiography (c) presented the bronchial artery hypertrophy (arrowheads) and abnormal lung staining (arrow). Celiac angiography (d) demonstrated the hypertrophied esophageal branch (arrowheads) of left gastric artery associated with abnormal lung staining (arrow). The patient was successfully treated using transradial embolotherapy.
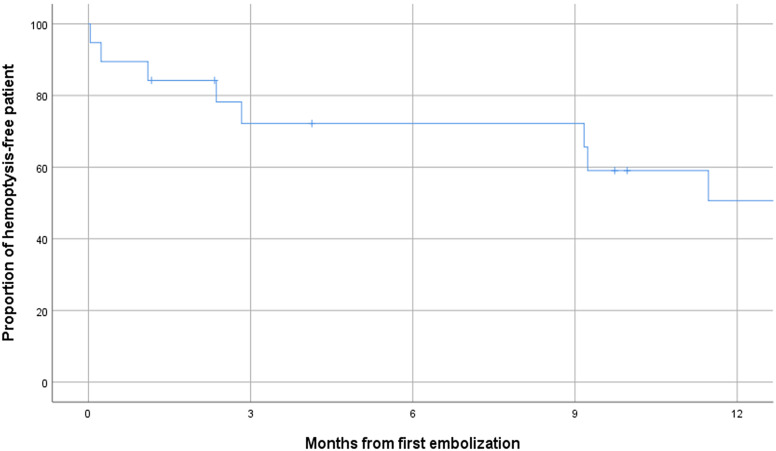
The 1-month and 6-month hemoptysis-free rates were 89.5% (17/19, 95% CI = 69.31-100.00%) and 73.7% (14/19, 95% CI = 54.05-96.39%), respectively (Figure 2). All patients were alive until the end of the 6-month follow-up. Two patients experienced early hemoptysis recurrence within 1 month after embolization. One patient complained of blood-tinged sputum the next day of the procedure, and bronchoscopy revealed an aspirated pill in the posterobasal segment of left lower lobar bronchus with mucosal inflammation. The other patient who had taken dual antiplatelet agents due to previous coronary artery intervention and cerebral infarction suffered from recurrent hemoptysis 1 week after the embolization. Next-day bronchoscopy was performed in 4 patients (21.2%, 4/19). With the exception of the patient with the aspirated pill, 1 patient presented with mild bleeding in the segmental bronchus and the remaining 2 patients had no abnormal findings on bronchoscopy. Early recurrence of hemoptysis related to the aspirated pill was the only adverse event in this study (severity: moderate adverse event).
Figure 2.
The Kaplan–Meier curve of the hemoptysis-free rate after transradial embolization.
Discussion
The present study showed that TRA enabled successful embolization for 47 out of 48 culprit arteries (97.9%) in 19 patients when it was applied to a selected patient group with favorable anatomy. The 1-month and 6-month hemoptysis-free rates were 89.5% (17/19) and 73.7% (14/19), respectively, which is comparable with the previous literature of bronchial artery embolization (BAE) with TFA.25 While major complication rates of bronchial artery embolization (BAE) have been variously reported from 0% to 6.6%,25 there was no severe adverse event in the present study. In aggregate, transradial embolization of the bronchial artery and NBSA yielded sufficiently high effectiveness and safety profile comparable to the transfemoral procedure.
In addition to the known benefits of TRA in arterial intervention (e.g., early ambulation, low risk of bleeding at the puncture site), TRA in the management of hemoptysis has specific advantages relevant to the procedure. During embolotherapy with TFA, catheterization of culprit arteries from the arch vessel or its tributaries is occasionally precluded by the tortuous aortic arch or arch vessel. As the stable positioning of a microcatheter in culprit arteries is vital to perform this procedure, the anatomical hurdles should be overcome to manage hemoptysis. In these cases, TRA ipsilateral to the target artery provides a short and straight course, which allows strong back support and easy control of the coaxial system and ultimately facilitates catheterization of the target arteries. Furthermore, TRA may reduce the risk of serious adverse events during the procedure. Patients with upper lobe lesions frequently have multiple culprit arteries from the subclavian artery and its tributaries. Embolization of the arteries with TFA requires prolonged catheterization across at least 1 major artery to the brain. When a patient has a tortuous aortic arch, in particular, embolization of the subclavian artery branches with TFA occasionally prolongs the procedure time owing to the difficulty of catheter manipulation. A long and tortuous course of the coaxial system may also prevent a microcatheter from being advanced deep into the culprit artery, which enhances the risk of non-target embolization. By using TRA properly, however, both the number of arch vessels that should be crossed and the procedure time can be reduced. If a patient has the bronchial artery in or just distal to the aortic arch (i.e., areas difficult to access by TRA) as well as NBSA from the subclavian artery, the combination of TRA and TFA can be considered, given a minimal increase of puncture site complication risks by adding TRA. Therefore, TRA needs to be considered, as a supplement or substitute of TFA, when patients have culprit arteries from the subclavian artery or its tributaries.
Transradial embolization of the bronchial artery and NBSA also has some disadvantages compared with the transfemoral procedure. When the orthotopic or ectopic bronchial artery originates from the aortic arch or upper level of the descending thoracic aorta, in TRA, it may be more difficult to manipulate the catheters and to select the intended vessels than in TFA. In left TRA, a catheter has to be bent toward the descending thoracic aorta after passing through the subclavian artery, hence the catheter tip naturally toward the lateral side of the aorta. Selection of the bronchial artery, typically arising from the anteromedial aspect of the aorta, immediately after this angulation can be extremely difficult. In right TRA, a catheter primarily entering in the ascending part of the aorta has to cross over to the descending thoracic aorta; hence the catheter is naturally S-shaped. The S-shape angle can become pronounced as the aortic arch becomes tortuous. Fine manipulation of a catheter while overcoming this course may also be difficult. In addition, patients with bilateral lung disease can have culprit arteries from both subclavian arteries. TRA appears to be inappropriate for these patients in a single session. For these reasons, TRA should be used in patients with hemoptysis after careful consideration of the individual anatomy using pre-procedural CT angiography.
The limitations of this study include its retrospective and non-comparative nature. Because the patients were selected for TRA in a non-randomized manner, the clinical outcomes such as the hemoptysis-free and adverse event rates were subject to potential selection bias. In addition, a single-center experience by a single operator may hamper the generalizability of the study results. A small sample size may limit the identification of uncommon adverse events related to TRA.
In conclusion, with careful patient selection, TRA offers a safe and effective approach to embolize the bronchial arteries and NBSAs for patients with hemoptysis.
Funding Statement
This research was funded by the National Research Foundation of Korea (Grant No. NRF-2018R1D1A1A02086183).
Footnotes
Conflict of interest disclosure The authors declared no conflicts of interest.
References
- 1. Liu LB, Cedillo MA, Bishay V.et al. Patient experience and preference in transradial versus transfemoral access during transarterial Radioembolization: a randomized single-center trial. J Vasc Interv Radiol. 2019;30(3):414 420. 10.1016/j.jvir.2018.10.005) [DOI] [PubMed] [Google Scholar]
- 2. Wu T, Sun R, Huang Y.et al. Transradial arterial chemoembolization reduces complications and costs in patients with hepatocellular carcinoma. Indian J Cancer. 2015;52(suppl 2):e107 e111. 10.4103/0019-509X.172505) [DOI] [PubMed] [Google Scholar]
- 3. Posham R, Biederman DM, Patel RS.et al. Transradial approach for noncoronary interventions: a single-center review of safety and feasibility in the first 1,500 cases. J Vasc Interv Radiol. 2016;27(2):159 166. 10.1016/j.jvir.2015.10.026) [DOI] [PubMed] [Google Scholar]
- 4. Bhatia S, Harward SH, Sinha VK, Narayanan G. Prostate artery Embolization via Transradial or Transulnar versus transfemoral arterial access: technical results. J Vasc Interv Radiol. 2017;28(6):898 905. 10.1016/j.jvir.2017.02.029) [DOI] [PubMed] [Google Scholar]
- 5. Resnick NJ, Kim E, Patel RS, Lookstein RA, Nowakowski FS, Fischman AM. Uterine artery embolization using a transradial approach: initial experience and technique. J Vasc Interv Radiol. 2014;25(3):443 447. 10.1016/j.jvir.2013.11.010) [DOI] [PubMed] [Google Scholar]
- 6. Bishay VL, Biederman DM, Ward TJ.et al. Transradial approach for hepatic Radioembolization: initial results and technique. AJR Am J Roentgenol. 2016;207(5):1112 1121. 10.2214/AJR.15.15615) [DOI] [PubMed] [Google Scholar]
- 7. Fujii H, Fujita A, Nakamura H, Sasaki T, Sugimoto H. Endovascular embolization of an aberrant bronchial artery originating from the internal mammary artery in a patient with hemoptysis. Case Rep Radiol. 2016;2016:2707195. 10.1155/2016/2707195) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sopko DR, Smith TP. Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2011;28(1):48 62. 10.1055/s-0031-1273940) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chun JY, Belli AM. Immediate and long-term outcomes of bronchial and non-bronchial systemic artery embolisation for the management of haemoptysis. Eur Radiol. 2010;20(3):558 565. 10.1007/s00330-009-1591-3) [DOI] [PubMed] [Google Scholar]
- 10. Ittrich H, Klose H, Adam G. Radiologic management of haemoptysis: diagnostic and interventional bronchial arterial embolisation. RoFo. 2015;187(4):248 259. 10.1055/s-0034-1385457) [DOI] [PubMed] [Google Scholar]
- 11. Tom LM, Palevsky HI, Holsclaw DS.et al. Recurrent bleeding, survival, and longitudinal pulmonary function following Bronchial artery Embolization for Hemoptysis in a U.S. adult population. J Vasc Interv Radiol. 2015;26(12):1806-13.e1. 10.1016/j.jvir.2015.08.019) [DOI] [PubMed] [Google Scholar]
- 12. Lee MK, Kim SH, Yong SJ.et al. Moderate hemoptysis: recurrent hemoptysis and mortality according to bronchial artery embolization. Clin Respir J. 2015;9(1):53 64. 10.1111/crj.12104) [DOI] [PubMed] [Google Scholar]
- 13. Woo S, Yoon CJ, Chung JW.et al. Bronchial artery embolization to control hemoptysis: comparison of N-butyl-2-cyanoacrylate and polyvinyl alcohol particles. Radiology. 2013;269(2):594 602. 10.1148/radiol.13130046) [DOI] [PubMed] [Google Scholar]
- 14. Bhalla A, Kandasamy D, Veedu P, Mohan A, Gamanagatti S. A retrospective analysis of 334 cases of hemoptysis treated by bronchial artery embolization. Oman Med J. 2015;30(2):119 128. 10.5001/omj.2015.26) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tanaka N, Yamakado K, Murashima S.et al. Superselective bronchial artery embolization for hemoptysis with a coaxial microcatheter system. J Vasc Interv Radiol. 1997;8(1 Pt 1):65 70. 10.1016/s1051-0443(97)70517-7) [DOI] [PubMed] [Google Scholar]
- 16. Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010;33(2):240 250. 10.1007/s00270-009-9788-z) [DOI] [PubMed] [Google Scholar]
- 17. Gagnon S, Quigley N, Dutau H, Delage A, Fortin M. Approach to hemoptysis in the modern era. Can Respir J. 2017;2017:1565030. 10.1155/2017/1565030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ketai LH, Mohammed TL, Kirsch J.et al. ACR appropriateness criteria(R) hemoptysis. J Thorac Imaging. 2014;29(3):W19 W22. 10.1097/RTI.0000000000000084) [DOI] [PubMed] [Google Scholar]
- 19. Yener Ö, Türkvatan A, Yüce G, Yener AÜ. The normal anatomy and variations of the bronchial arteries: evaluation with multidetector computed tomography. Can Assoc Radiol J. 2015;66(1):44 52. 10.1016/j.carj.2014.07.001) [DOI] [PubMed] [Google Scholar]
- 20. Chung MJ, Lee JH, Lee KS, Yoon YC, Kwon OJ, Kim TS. Bronchial and nonbronchial systemic arteries in patients with hemoptysis: depiction on MDCT angiography. AJR Am J Roentgenol. 2006;186(3):649 655. 10.2214/AJR.04.1961) [DOI] [PubMed] [Google Scholar]
- 21. Barbeau GR, Arsenault F, Dugas L, Simard S, Larivière MM. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen’s test in 1010 patients. Am Heart J. 2004;147(3):489 493. 10.1016/j.ahj.2003.10.038) [DOI] [PubMed] [Google Scholar]
- 22. Fischman AM, Swinburne NC, Patel RS. A technical guide describing the use of transradial access technique for endovascular interventions. Tech Vasc Interv Radiol. 2015;18(2):58 65. 10.1053/j.tvir.2015.04.002) [DOI] [PubMed] [Google Scholar]
- 23. Lee JH, Kwon SY, Yoon HI.et al. Haemoptysis due to chronic tuberculosis vs. bronchiectasis: comparison of long-term outcome of arterial embolisation. Int J Tuberc Lung Dis. 2007;11(7):781 787. [PubMed] [Google Scholar]
- 24. Tam AL, Findeiss L, Dake MD.et al. Standards 2.0: methodology update. J Vasc Interv Radiol. 2018;29(10):1347 1349. 10.1016/j.jvir.2018.05.018) [DOI] [PubMed] [Google Scholar]
- 25. Panda A, Bhalla AS, Goyal A. Bronchial artery embolization in hemoptysis: a systematic review. Diagn Interv Radiol. 2017;23(4):307 317. 10.5152/dir.2017.16454) [DOI] [PMC free article] [PubMed] [Google Scholar]