Abstract
Introduction:
Telemedicine could increase timely access to primary care—a key dimension of care quality.
Methods:
Among patient-scheduled appointments with their own primary care providers using the online portal in a large integrated health care delivery system, we measured the association between visit type (telemedicine or in-person) and appointment timeliness. We calculated the calendar days between the scheduling date and the actual appointment time.
Results:
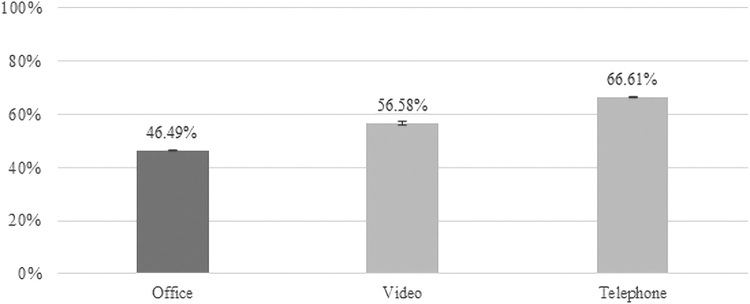
Overall, 2,178,440 primary care visits were scheduled and 14% were done through telemedicine. The mean calendar days between the scheduling and the appointment time were 1.80 for telephone visits, 2.29 for video visits, and 3.52 for in-person visits. After multivariate adjustment, 66.61% (confidence interval [95% CI]: 66.44–66.79) of telephone visits, 56.58% (95% CI: 55.90–57.27) of video visits, and 46.49% (95% CI: 46.42–46.57) of in-person visits were scheduled to occur within 1 day of making the appointment.
Conclusions:
In a setting with comparable in-person and telemedicine scheduling availability, choosing telemedicine was associated with more timely access to primary care.
Keywords: telemedicine, video visits, health care access, primary care
Introduction
Telemedicine (telephone and video visits) can offer direct real-time convenient access to a clinician without needing to arrange for time off from work, transportation or parking logistics, or account for wait times usually required for a traditional office visit.1,2 Patients in the United States spend an average of 2 h for a 20-min in-person office visit, including ∼40 min of travel time.3,4 These barriers have been found to be more common among certain minority groups, resulting in disparities in health care access.4–7 Telemedicine access can help patients overcome many barriers to in-person care.1,2 Overall, telemedicine has the potential to expand access and timeliness of care, reduce disparities, and improve health outcomes.
However, challenges including variations in state laws and reduced reimbursement limited widespread access to telemedicine services. This changed in 2020, as the coronavirus disease 2019 (COVID-19) pandemic propelled shifts in care delivery to support telemedicine and curtail the spread of the virus. In response to the pandemic, new temporary emergency federal policy changes reduced key telemedicine barriers. With the future of telemedicine still unclear, more evidence is needed to guide policy makers on how telemedicine access for routine ambulatory primary care impacts health care access, including timeliness, care quality, and outcomes.
Although the convenience of telemedicine is often noted, to our knowledge, no previous studies have quantitatively examined the degree to which telemedicine access is associated with how quickly patients are able to access care from familiar providers. We conducted an observational cross-sectional study to measure the association between primary care visit type (telemedicine vs. in-person office visits) and timeliness of the appointment. Among patient-scheduled in-person office or telemedicine (video or telephone) appointments with their own primary care providers using the patient portal, we measured the association between type of visit and appointment timeliness (time from scheduling to the actual visit time).
Methods
SETTING AND POPULATION
We examined patient-initiated primary care visits in a large integrated health care delivery system with over four million members, Kaiser Permanente Northern California (KPNC). KPNC offers services in the northern region of California across the continuum of care including outpatient primary and specialty care, inpatient care, pharmacy, laboratory, and imaging services. Beginning in 2016, patients scheduling a primary care appointment through the online patient portal were asked to choose visit type: office, video, or telephone visit.
All visit types (office, telephone, and video) had comparable scheduling availability, but “routine physicals” were only offered as in-person office visits. Available clinicians included patients' own primary care provider or other primary care providers the patient had seen in a previous in-person visit. Telemedicine visits (video or telephone) were largely exempt from out-of-pocket cost sharing. Although patients could also schedule primary care visits over the phone or in-person, we focused exclusively on primary care visits scheduled using the online portal because patients scheduling these visits were consistently asked to choose between all three visit modalities (office, telephone, and video).
In this observational study, we included all primary care appointments (except routine physicals) scheduled through the patient portal from January 1, 2016, to May 31, 2018. To define a relatively distinct patient-initiated care-seeking episode, rather than follow-up care from a prior episode, we excluded visits that occurred within 7 days of other prior clinical encounters (office, video, phone, emergency department, or hospitalization). For each visit included, we calculated the number of calendar days between the scheduling date and the actual appointment time. For ease of interpretation, we also created a binary measure by categorizing visits as timely if the actual visit took place by the end of the following calendar day after the patient scheduled the appointment.
STATISTICAL ANALYSIS
We defined “timeliness” based on the timing of the visit relative to the time it was scheduled, and not due to any clinical assessment of urgency. We compared the mean number of calendar days between the scheduling date and the actual appointment time by visit modality. We also used multivariate logistic regression to examine the association between visit type (telemedicine telephone or video visits vs. in-person office visits) and our binary measure of visit timeliness.
We adjusted for several important patient characteristics, including patient sociodemographic characteristics (age, gender, neighborhood socioeconomic status, and language preference), in-person visit barriers (cost sharing, travel time from home to nearest clinic, and paid parking structure), technology access (neighborhood-level internet access, visit scheduled by a proxy, patients' mobile portal access, or video visits in the prior year), whether the visit was with the patient's own primary care provider, pre-existing chronic conditions, ICD10 primary diagnosis grouping, and medical center.
Our model used standard errors adjusted for patient clustering. For easier interpretation, we calculated adjusted rates using results from the logistic model as if every visit from the entire cohort was scheduled as an office visit, video visit, or telephone visit. All analyses were conducted using Stata 14.2 (StataCorp, College Station, TX).
The KPNC institutional review board approved and waived consent for this study.
Results
Overall, 2,178,440 eligible primary care visits were scheduled by 1,131,722 patients during the study period; 22.2% were of ages 65+, 45.1% male, 59.8% white; and 15.6% lived in lower socioeconomic status neighborhoods (Table 1). Among all portal-scheduled visits, 14% were chosen to be through telemedicine (telephone and video), and 93.5% of telemedicine visits were telephone visits.
Table 1.
Patient-Scheduled Primary Care Visits: Characteristics by Visit Type
| |
TOTAL |
OFFICE VISIT |
VIDEO VISIT |
TELEPHONE VISIT |
|---|---|---|---|---|
| ALL (N = ) |
2,178,440 |
1,870,552 |
20,115 |
287,773 |
| % | ||||
| Age | ||||
| <18 | 13.5 | 14.2 | 17.9 | 8.5 |
| 18–<45 | 31.4 | 29.9 | 49.7 | 39.8 |
| 45–<65 | 32.9 | 32.7 | 26.7 | 34.6 |
| 65+ | 22.2 | 23.2 | 5.7 | 17.1 |
| Gender | ||||
| Male | 45.1 | 46.1 | 43.2 | 39.1 |
| Race/ethnicity | ||||
| White | 59.8 | 60.0 | 49.3 | 58.6 |
| Black | 5.2 | 4.9 | 6.9 | 6.6 |
| Hispanic | 13.2 | 13.2 | 12.2 | 13.8 |
| Asian | 20.6 | 20.6 | 30.2 | 19.5 |
| Other | 1.3 | 1.3 | 1.5 | 1.4 |
| Neighborhood socioeconomic level | ||||
| Lower | 15.6 | 15.4 | 15.2 | 16.6 |
| Higher | 84.4 | 84.6 | 84.8 | 83.4 |
Note: Study unit shown is patient visit, percentages shown are column percentages. Neighborhood measures based on patient's residential address.
The mean calendar days between the scheduling date and the actual appointment time were 1.8 days for telephone visits, 2.3 days for video visits, and 3.5 days for in-person visits. After multivariate adjustment, 66.6% (confidence interval [95% CI]: 66.4–66.8) of telephone visits, 56.6% (95% CI: 55.9–57.3) of video visits, and 46.5% (95% CI: 46.4–46.6) of in-person visits were scheduled to occur within 1 day of making the appointment (Fig. 1).
Fig. 1.
Adjusted percentage of primary care visits scheduled within 1 day by visit type: office visit, video telemedicine, telephone telemedicine. Note: Adjusted rates are calculated using results from logistic regression adjusted for patient sociodemographic characteristics (age, gender, neighborhood socioeconomic status, and language preference), in-person visit barriers (cost sharing, travel time from home to nearest clinic, and paid parking structure), technology access (neighborhood internet access level, mobile portal access in the prior year, portal proxy access, and video visits in the prior year), whether the visit was with the patient's own primary care provider, pre-existing chronic conditions, ICD10 primary diagnosis grouping, and medical center, with standard errors adjusted for clustering by patient.
Discussion
In a setting with comparable in-person and telemedicine scheduling availability, patients choosing telemedicine for primary care appointment were able to complete their visits more quickly than those choosing in-person office visits. Over two-thirds of telephone visits and over half of video visits were scheduled to occur within 1 day of making the appointment, compared with fewer than half of in-person visits. On average, telephone visits were scheduled ∼50% sooner than office visits.
Timely access to health care depends on multilevel factors. It is a key dimension of care quality and is associated with improved health outcomes.4,8 Because our study focused on patients in a single health care system with comparable access to telemedicine and office visits, differences in timeliness were likely driven by patient and visit level factors such as medical need, preferences, and logistical considerations. Our prior analyses showed that choosing telemedicine was associated with sociodemographic characteristics (e.g., older patients were more likely to choose in-person visits), technology access, and in-person visit barriers (e.g., paid parking structures).2
Our new results suggest that the convenience of telemedicine, which allows patients to access health care without having to arrange transportation or account for wait times, made it possible for them to see trusted health care providers more quickly. It is possible that patients with more urgent concerns chose to schedule a telemedicine visit because they would be able to complete it more quickly. Thus, these findings could have important implications for health outcomes.
Given the ongoing COVID-19 pandemic, internal and family medicine leaders have propelled temporary changes in reimbursement and cost-sharing policies to encourage practices across the country to offer their patients telemedicine visits with their existing providers.9,10 Beyond limiting potential exposure to infectious diseases, telemedicine can help patients to overcome key barriers to seeking in-person care, including transportation, job flexibility, and time.11–13 Previous research found that racial/ethnic minorities face greater barriers for accessing in-person care.4
Accordingly, our previous study found that certain patient groups, including those living in poorer neighborhoods or facing more barriers to in-person care, such as higher cost sharing and living further away, were more likely to choose telemedicine visits.2 Thus, expanding access to telemedicine may reduce disparities in health care access and improve the timeliness of care. For patients facing barriers to in-person care, without access to telemedicine they may not be able to seek timely medical attention, which could have detrimental effects on their health. Although the convenience of telemedicine is widely recognized and cited, our results are the first to quantitatively demonstrate the degree to which comparable telemedicine access provides patients a timelier way to seek care from familiar providers.
LIMITATIONS
We did not examine the appropriateness of using telemedicine or the health impacts of telemedicine-associated timeliness. This study was not designed to identify which clinical conditions or specific concerns may benefit most from timely visits. In addition, the study was conducted at a single large integrated delivery system and limited to patient-initiated appointments scheduled online. Thus, results may not be generalizable to other less-integrated telemedicine delivery settings or different patient-initiated appointment-scheduling workflows.
Moreover, the study cohort may not fully represent patients in the wider population or KPNC members who scheduled visits without using the portal. We used observational data in a setting where patients self-selected the visit type when scheduling the visit. Thus, visit types were not equally distributed and results should not be interpreted as causal. Lastly, we used data collected before the ongoing COVID-19 pandemic that has caused substantial shifts in health care delivery. Future studies should examine the impact of the increase in telemedicine during the pandemic on health care access, quality, and outcomes.
Conclusions
Our study found that before the COVID-19 pandemic, choosing telemedicine was associated with more timely access to primary care, which may have implications for health outcomes. Widespread access to routine telemedicine for primary care has historically been constrained by variations in state and federal laws and limited reimbursement. It is unclear whether the temporary increase in telemedicine access will persist once the threat of the COVID-19 pandemic subsides. Although telemedicine has been used and studied among rural regions and specialty consultation, evidence remains particularly limited on use of telemedicine in routine ambulatory primary care with familiar providers.10,14–17
KPNC is unique in having offered its members access to routine telemedicine visits with their familiar primary care providers in a setting that integrates care across the continuum before the pandemic. This is distinct from direct-to-consumer telehealth-only care that is not integrated with ongoing in-person health care services. More evidence is needed on the value, benefits, and limitations of telemedicine for integrated routine ambulatory primary care outside of pandemic conditions to inform long-term policy decisions and care delivery practices.
Authors' Contributions
All authors contributed equally.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was funded by a grant from the Agency for Healthcare Research and Quality (R011HS25189).
REFERENCES
- 1. Reed ME, Huang J, Parikh R, et al. Patient-provider video telemedicine integrated with clinical care: Patient experiences. Ann Intern Med 2019;171:222–224. [DOI] [PubMed] [Google Scholar]
- 2. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open 2020;3:e205873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Daschle T, Dorsey ER. The return of the house call. Ann Intern Med 2015;162:587–588. [DOI] [PubMed] [Google Scholar]
- 4. Ray KN, Chari AV, Engberg J, Bertolet M, Mehrotra A. Disparities in time spent seeking medical care in the United States. JAMA Intern Med 2015;175:1983–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shi L, Chen C-C, Nie X, Zhu J, Hu R. Racial and socioeconomic disparities in access to primary care among people with chronic conditions. J Am Board Fam Med 2014;27:189–198. [DOI] [PubMed] [Google Scholar]
- 6. Brown EJ, Polsky D, Barbu CM, Seymour JW, Grande D. Racial disparities in geographic access to primary care in Philadelphia. Health Aff 2016;35:1374–1381. [DOI] [PubMed] [Google Scholar]
- 7. Newacheck PW, Hughes DC, Stoddard JJ. Children's access to primary care: Differences by race, income, and insurance status. Pediatrics 1996;97:26–32. [PubMed] [Google Scholar]
- 8. Carroll JG. Crossing the quality chasm: A new health system for the 21st century. Qual Manag Healthc 2002;10:60–61. [Google Scholar]
- 9. Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: An American College of Physicians position paper. Ann Intern Med 2015;163:787–789. [DOI] [PubMed] [Google Scholar]
- 10. Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient perceptions of telehealth primary care video visits. Ann Fam Med 2017;15:225–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for U.S. adults. Health Serv Res 2012;47(1 Pt 2):462–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Levesque JF, Harris MF, Russell G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int J Equity Health 2013;12:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Reed ME, Parikh R, Huang J, Ballard DW, Barr I, Wargon C. Real-time patient-provider video telemedicine integrated with clinical care. N Engl J Med 2018;379:1478–1479. [DOI] [PubMed] [Google Scholar]
- 14. Burke BL Jr., Hall RW. Telemedicine: Pediatric applications. Pediatrics 2015;136:e293–e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kahn JM. Virtual visits—Confronting the challenges of telemedicine. N Engl J Med 2015;372:1684–1685. [DOI] [PubMed] [Google Scholar]
- 16. Mehrotra A, Jena AB, Busch AB, Souza J, Uscher-Pines L, Landon BE. Utilization of telemedicine among rural medicare beneficiaries. JAMA 2016;315:2015–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA 2013;310:2395–2396. [DOI] [PubMed] [Google Scholar]