Abstract
Background
The electronic Personal Health Record (ePHR) is a health information system that registers health data on newly arriving migrants and was implemented in eight European countries (Bulgaria, Croatia, Cyprus, Greece, Italy, Romania, Serbia and Slovenia). This is a cross-sectional study aimed to describe the health problems and health status of all migrants attended at health clinics as part of the health assessment programme established in the reception centres (2016–2019).
Methods
Data were collected on demographics, clinical and laboratory findings and diagnostics performed, including medical records. We classified all diseases using pre-specified algorithms according to information on pre-specified variables from the ePHR questionnaire, ICD-10 codes, positive laboratory findings or review of medical records. Crude proportions were calculated and odds ratios (OR) estimated using logistic regression modelling.
Results
The ePHR dataset contained a total of 19 564 clinical episodes in 14 436 individuals, recorded between January 2016 and October 2019. Most individuals (75%) were refugees or asylum seekers (22%) from 92 different nationalities. There were 2531/19 564 (12.9%) infectious diseases episodes reported during the study period, being 1283/2531 (50.7%) of them pharyngo-tonsillitis, 529 (20.9%) scabies, 158 (6.2%) viral hepatitis and 156(6.1%) lower respiratory infections. There were 2462 (17.1%) individuals with non-communicable diseases reported; including 821 (5.7%) cardiovascular diseases, 1183 (8.2%) neurological condition, 644 (4.5%) Diabetes mellitus and 212 (1.5%) kidney disease cases. Having Diabetes Mellitus (adjusted OR, aOR 3.3, [95% confidence interval, CI 2.7–4.1], P < 0.001), and neurological disorders (aOR 1.8, [95% CI 1.4–2.2], P < 0.001) were associated with cardiovascular disorders in the multivariable logistic regression model.
Mental health problems were reported in 641/14 436 (4.4%) individuals and were associated with increasing age. Furthermore, 610 episodes of acute injuries were reported among 585/14 436 (4.1%) people, 517 (88.4%) of them in men (P < 0.001).
Conclusions
The ePHR is a valuable tool to efficiently collect health-related data to better address migrant health issues. We described a mostly healthy population with many acute infectious disease episodes particularly in children, but also with significant number of chronic conditions and less frequent injuries or mental health problems.
Keywords: Migrant, refugees, health data, electronic patient record, reception centres, health condition, chronic diseases, infectious diseases, mental health
Introduction
Migration is a significant, complex and growing global phenomenon influenced by geographical, socio-economic and political factors.1 Since 2015, European migration policies have been influenced by realities and perception of migration at its southern borders.2 Over 128 000 irregular arrivals of migrants coming mainly from African and Asian countries to Europe via the Mediterranean migration routes were recorded in 2019.3 The Eastern Mediterranean route was the most important among the three Mediterranean migration routes between 2015 and 2020 due to large numbers of refugees from the Syrian civil war who arrived in the EU in 2015.4
The need to address the health of migrant populations was highlighted by the 2016 United Nations Summit for Refugees and Migrants,5 including appropriate health care in arrival, transit and destination countries for humanitarian and public health reasons.6 As reflected in the Global Compact for Safe, Orderly and Regular Migration,7 it is essential to have available, disaggregated and comparable data on migrant health to have a good understanding of health needs of migrants and for public health planning.8 The need for good data relates to two dimensions, both with an urgent need for improvement. The first dimension is the capacity of the health information system (HIS) to capture and share the relevant health care information safely between healthcare facilities or countries, which is challenging since migrants in irregular situations, are often cared for by actors outside the mainstream health system9 and/or often not eligible for routine care.10 The second dimension is related to monitoring and surveillance, particularly important for infectious diseases surveillance including coronavirus disease of 2019 (COVID-19), but also for health service planning. Although there are some initiatives to monitor and surveillance imported disease diseases in migrant and travellers in sentinel clinics,11,12 migrant health data are usually not systematically collected by routine HIS.13
In addition to the inclusion of key variables related to refugees and migrants (e.g. country of birth, length of stay and reason for migration) into existing data collection systems,14 other proactive approaches to data collection for refugees and migrants are urgently needed.13
The electronic Personal Health Record (ePHR) is a HIS for newly arriving migrants, which allows recording of the medical history, diagnoses, signs and symptoms for first and follow-up consultations. It was developed by the International Organization for Migration (IOM).15 The objective of the study was to present the ePHR tool and to describe health problems and health status in the migrant cohort who either were attended for a medical problem or underwent a comprehensive health assessment in the reception/health centres.
Methods
Design
This is a cross-sectional study of all migrants who underwent consultations or health assessments between 2016 and 2019 in all reception centres for migrants, in eight European countries where ePHR was established. All migrants being attended in the centres were considered newly arrived since the arrived usually few months prior, and certainly within the last 5 years.
Study sites and implementation phases
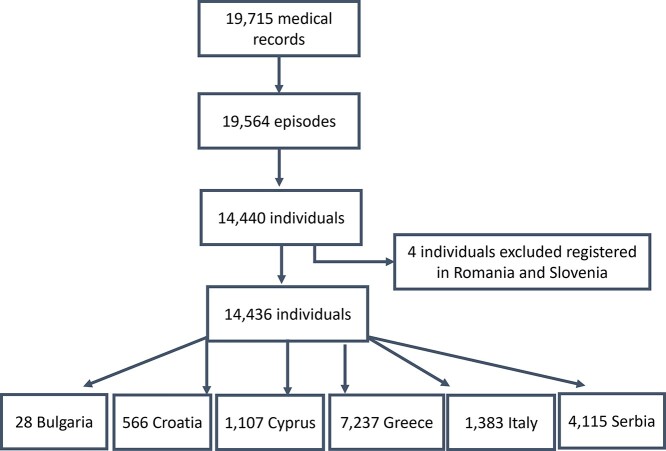
The first phase of the ePHR was implemented in Italy and Croatia, Slovenia and Greece (2016–2017). In the second phase (2017–2019), four new countries (Bulgaria, Cyprus, Romania and Serbia) were included. In the facilities located in Romania and Slovenia, the tool was only implemented as a pilot test, and therefore they were not included in the analysis. Annex 1 (Supplementary data are available at JTM online) show detailed aspects of each centre.
Health assessment protocol
A free and voluntary health assessment was offered to all individuals at implementation sites, following a standardized protocol13 (Annex 2, Supplementary data are available at JTM online) and conducted by qualified, culturally competent health professionals (doctors or nurses). All patients underwent a routine physical and mental health examination, including assessment of pulse rate, blood pressure and temperature. Routine screening for infections or other diseases was not systematically performed. In this regard, specific investigations, such as electrocardiography, chest radiography or specific blood tests, were performed for patients, where history or examination prompted the need for such. Vaccination status was also checked (but these data were not available as part of this study), and additional complementary tests are ordered when requested.
The questionnaire used in the health assessment15 includes information on patient, past medical history, immunization records, exam and laboratory findings, diagnostics, summary findings, treatment and post-arrival recommendation. Personnel received in-person or online training on the ePHR system. There was also a handbook for health professionals available in nine European languages with a framework on the health assessment to refugees and migrants.16 The ePHR contains securely held individual’s data, accessible to authorised users across sites and countries and is fully compliant with the EU General Dara Protection Regulation and the IOM data protection policy.17
Data sources and management
Data were collected from all reception centres in six of the eight countries that implemented the ePHR as part of the project Re-Health. For this study, data were extracted on demographics (sex, age, country of birth and country of examination), past medical history, exam and laboratory findings, diagnostics performed and summary findings, which included the diagnosis identified through the International Classification of Diseases-10th Revision (ICD-10, version 2016–1). Vaccination data and information on drugs registered were not available and therefore not included for the purpose of this study.
Diseases were grouped into the following categories: cardio-vascular diseases, neurological disorders, diabetes, respiratory diseases, urogenital problems, mental illness, haematological disorders, gastro-intestinal diseases, ocular and ear problems, neoplasia, injuries, congenital abnormalities and infectious diseases.
Data were recorded as binary(yes/no), using ICD-10 and free text information, sometimes overlappingly. There was a significant proportion of missing data, particularly for the binary variables providing information on the presence or not of the following conditions: cardiovascular diseases, neurological disorders, mental illness, gastro-intestinal diseases, hepatic, renal, urogenital, haematological diseases, diabetes, osteo-articular, eyes and ear disorders, cancer, lung diseases, tattoos or piercings, alcohol consumption and skin problems. We therefore classified all diseases using pre-specified imputation algorithms (Annex 3, Supplementary data are available at JTM online). In brief, for each health condition, we included:
Information about binary variables pre-specified in the questionnaire related to such conditions;
ICD-10 codes;
Positive laboratory findings (e.g. HIV serological test);
Information on medical records.
In all medical records and for each group of diseases or health conditions, key words were identified using simple natural language processing algorithms. Those records that identified such key words were manually reviewed to confirm the health condition. Although the ePHR system was available in several European languages, almost all patient records were in English, with few in local languages. Therefore, key words were also identified in these languages.
Cardio-vascular disorders included all diseases registered in ICD-10 Chapter IX: hypertension, arrhythmias, ischemic cardiopathy, any type of cardiopathy and vascular diseases, except cerebrovascular diseases (stroke), which was included among neurological disorders.
Neurological disorders included stroke and all diseases in ICD-10 Chapter VI: central nervous system diseases and peripheric neurological disorders.
Mental illness was considered when either a mental condition or an alteration of the mental state was present in the record, and all diseases present in the ICD-10 Chapter XIX: anxiety and stress, panic attack or depression.
Further details are provided in Annex 3 (Supplementary data are available at JTM online).
The health examination programme did not include formal screening. All tuberculosis, HIV and viral hepatitis cases reported were based on the review of medical records and ICD-10 codes registered by health professionals. This was based on the evidence provided by the patient, and some of them based on laboratory data.
Health episodes were classified into acute and chronic events, with the former considered if lasting < 4 weeks. The following conditions were classified as acute events: pediculosis, scabies, other skin infections, pharyngo-tonsillitis, sinusitis, upper respiratory infections, lower respiratory infections, gastro-intestinal infections and injuries.
Statistical analysis
Data were presented as proportions, means or medians, using chi-squared, Fisher-Exact tests, t-test or Wilcoxon–Mann–Whitney–U. For cardiovascular diseases and mental health, a multivariable logistic regression was used to identify patient characteristics associated with such health conditions.
A number of variables related to medical past history, exam and laboratory finding had a high proportion of missing values. Missing data were examined for randomness and if this applied, a full case analysis performed. For some variables, where this was appropriate and after careful descriptive analysis and stakeholder discussions and if this was justifiable within the logic of the HIS, we reclassified missing data to a negative value. Detailed information for the re-classification of each missing value is provided in Annex 4 (Supplementary data are available at JTM online). We also performed a sensitivity analysis comparing the imputation of missing data with missing data being excluded from the analysis.
All data analyses were performed using Stata-16 (Stata-Corp-LP, USA).
Ethics
The application and analysis of ePHR was done in full compliance with IOM/UN data protection principles15 including patient confidentiality, consent, compliant data sharing and anonymization for analysis purposes. Internal IOM approval was granted, no external approval was needed, as this study is a service evaluation of routine systems and care. The reporting of this study conforms to the STROBE statement (Annex 4, Supplementary data are available at JTM online).
Results
The data set contained 19 564 clinical episodes for 14 440 individuals from 12 451 families in total and 14 436 individuals included in the analysis during the study period (Figure 1). All episodes were recorded between January 2016 and October 2019.
Figure 1.
Flow diagram of the medical records registered at the ePHR centres.
Socio-demographic characteristics are summarised in Table 1. The median age of the recorded population was 25 (IQR 18–34) years and 77.7% (11 221) were male. In addition, 10 874 (75.3%) individuals were refugees and 3171 (22.0%) were asylum seekers; individuals were of 92 different nationalities with 8207 of them from Southern Asia (57.0%), 3389 (23.5%) from Western Asia and 1521 (10.6%) from Western Africa. The most frequent nationalities were Afghan (3662, 25.4%), Pakistani (2584, 17.9%) and Syrian (2319, 16.1%).
Table 1.
General characteristics of the population attended in adults and children
| Bulgaria (%) n = 28 | Croatia N = 566 |
Cyprus (%) n = 1107 | Greece n = 7237 |
Italy n = 1383 |
Serbia n = 4115 |
Total 14 436 |
|
|---|---|---|---|---|---|---|---|
| Sex (male) | 9 (32.1) | 384 (67.8) | 730 (65.9) | 5188 (71.7) | 1189 (86) | 3721 (90.4) | 11 221 (77.7) |
| Age group 0–17 18–39 >439 |
2 (7.1) 18 (64.3) 8 (28.6) |
163 (28.8) 334 (59.0) 69 (12.2) |
385 (34.8) 645 (58.3) 77 (7.0) |
838 (11.6) 4449 (61.5) 1950 (26.9) |
573 (41.4.4) 786 (56.8) 24 (1.7) |
1601 (38.9) 2311 (56.2) 203 (4.9) |
3562 (24.7) 8543 (59.2) 2331 (16.1) |
| Region of origina Africa America Asia Europe Oceania |
0 0 28 (100) 0 0 |
18 (3.2) 3 (0.5) 536 (94.7) 8 (1.4) 1 (0.2) |
154 (13.9) 0 950 (85.8) 2 (0.2) 1 (0.1) |
1047 (14.5) 4 (0.1) 6134 (85.2) 18 (0.3) 0 |
1285 (92.9) 1 (0.1) 96 (6.9) 1 (0.1) 0 |
134 (3.3) 3 (0.1) 3950 (96.0) 22 (0.5) 6 (0.2) |
2638 (18.3) 11 (0.1) 11 694 (81.2) 51 (0.4) 8 (0.1) |
| Living with no family | 28 (100) | 346 (61.1) | 555 (50.1) | 5836 (80.6) | 1366 (98.8) | 3466 (84.2) | 11 597 (80.3) |
| Number (proportion) of patients with more than one visit | 0 (0) | 26 (4.6) | 7 (0.6) | 1152 (15.9) | 30 (2.2) | 1333 (32.4) | 2548 (17.7) |
| Follow-up (days)b Median (IQR) in those with more than one visit |
1 (1–1) | 334 (268–455) | 1 (1–1) | 41 (15–110) | 68 (30–116) | 37 (13–105) | 40 (14–109) |
| Number of visits Median (range) | 1 (1–1) | 1 (1–3) | 1 (1–4) | 1 (1–7) | 1 (1–3) | 1 (1–42) | 1 (1–42) |
| Smoking | 2 (7.1) | 162 (28.6) | 14 (1.3) | 459 (6.3) | 172 (12.4) | 47 (1.1) | 856 (5.9) |
| Alcohol consumption | 0 (0) | 30 (5.4) | 6 (7.4) | 81 (5.4) | 30 (2.5) | 10 (1.1) | 157 (3.7) |
aThere are 34 observations registered in Greece with an unknown nationality.
bMedian of follow-up days in patients with more than one visit.
Identification of medical conditions
During the study period, 5699 (39.5%) of patients, who attended, did not report any health condition at the health assessment, and 1742 (12.1%) reported an acute condition that only needed one visit including skin disorders, acute infectious diseases or injuries. A chronic condition, which included all conditions with a clinical history of >4 weeks and was reported in 6995 (48.4%) individuals. This included cardiovascular, neurological, musculoskeletal, onco-haematological, gastrointestinal, urogenital, kidney or liver diseases, congenital abnormalities, disabilities (See Annex 5, Supplementary data are available at JTM online) and also chronic infections such viral hepatitis, HIV or tuberculosis.
Infectious diseases
There were 2531/19 564 (12.9%) episodes of infectious diseases during the study period including 1283 (50.7%) pharyngo-tonsillitis, 529 (20.9%) scabies, and 158 (6.2%) viral hepatitis (being 110 hepatitis C infections) and 156 (6.1%) lower respiratory infections. Also, 1409 (55.7%) infectious disease episodes were reported among children, in particular pharyngo-tonsillitis (731, 57%) scabies (329, 62%) and pediculosis (108, 93%; Annex 6, Supplementary data are available at JTM online).
Other infections including HIV and viral hepatitis were more commonly reported in older age groups (89.5 and 90% in adults, respectively).
There were not outbreaks reported during the study period.
Non communicable diseases
The crude proportion for all conditions with 95% confidence interval (CI) is presented in Table 2. In total, 821 (5.7%) individuals were reported with a cardiovascular disease. Most of the cardiovascular disorders were hypertension (324 cases, 2.2%), ischemic heart disease (97, 0.7%), other cardiac problems (85, 0.7%), vascular diseases (29, 0.2%) and arrhythmias (25, 0.2%).
Table 2.
Diseases most frequently reported in the population attended
| Age frequency of cases (%) | Sex frequency of cases (%) | ||||||
|---|---|---|---|---|---|---|---|
| 0–17 (n = 3567) | 18–39 (n = 8539) | >39 (n = 2330) | P-value | Male (n = 11 221) | Female (n = 3215) | P-value | |
| Cardio-vascular (n = 821; 71 missing) |
38 (1.0) | 263 (3.1) | 520 (22.4) | P < 0.001 | 546 (4.9) | 273 (8.6) | <0.001 |
| DM (n = 644) | 11 (0.3) | 185 (2.2) | 448 (19.3) | <0.001 | 450 (4.0) | 194 (6.0) | <0.001 |
| Neurological disorders* (n = 1183, 76 missing) |
208 (5.9) | 704 (8.3) | 271 (11.7) | <0.001 | 909 (8.2) | 274 (8.6) | 0.456 |
| Mental Health (n = 641, 10 missing) | 44 (1.2) | 422 (5.0) | 175 (7.5) | <0.001 | 440 (3.9) | 227 (7.1) | <0.001 |
| Urogenital diseases (n = 667) | 98 (2.8) | 414 (4.9) | 155 (6.7) | <0.001 | 486 (4.3) | 237 (7.4) | <0.001 |
| Haematological disorders (n = 511) | 42 (1.2) | 364 (4.3) | 105 (4.5) | <0.001 | 385 (3.4) | 126 (3.9) | 0.187 |
| Nephropathies (n = 212) | 21 (0.6) | 132 (1.6) | 59 (2.5) | <0.001 | 168 (1.5) | 44 (1.4) | 0.593 |
| Hepatopathies (n = 399) | 8 (0.2) | 312 (3.7) | 79 (3.4) | <0.001 | 374 (3.3) | 25 (0.8) | <0.001 |
| Cancer (n = 64, 10 missing) | 5 (0.1) | 34 (0.4) | 25 (1.1) | <0.001 | 31 (0.3) | 33 (1.0) | <0.001 |
| Musculoskeletal conditions (n = 1888) | 143 (4.0) | 1238 (14.5) | 507 (21.8) | <0.001 | 1488 (13.3) | 400 (12.4) | 0.225 |
| Ear and eye disorders (n = 867, 10missing) | 182 (5.1) | 447 (5.2) | 238 (10.2) | <0.001 | 625 (5.6) | 242 (7.5) | <0.001 |
| Respiratory conditions (including ID) (n = 1626) | 632 (17.9) | 747 (8.8) | 247 (10.8) | <0.001 | 1293 (11.7) | 333 (10.5) | 0.057 |
| Gastro-intestinal diseases (n = 1560) | 282 (7.9) | 975 (11.4) | 303 (13.0) | <0.001 | 1183 (10.5) | 377 (11.7) | 0.057 |
| Skin disorders (n = 1567) | 587 (16.5) | 874 (10.2) | 106 (4.6) | <0.001 | 1332 (11.9) | 235 (7.3) | <0.001 |
| Congenital abnormalities and perinatal disorders (n = 9) |
9 (0.3) | 0 (0) | 0 (0) | <0.001 | 7 (0.6) | 2 (0.06) | 0.997 |
| Infectious diseases** (n = 2531) | 1409/6590 (21.4) | 944/9573 (9.9) | 178/3401 (5.2) | <0.001 | 2199/14919 (14.7) | 404/4645 (8.7) | <0.001 |
| Injuries** (n = 610) | 228/6590 (3.5) | 317/9573 (3.3) | 65/3401 (1.9) | <0.001 | 532/14919 (3.6) | 58/4645 (1.2) | <0.001 |
* . It includes headache.
* * Estimates based on 19 564 episodes.
Cardiovascular diseases were higher in the >39 years old group (520, 22.4%) compared with young adults (18–39 years, 263, 3.1%) and with children (38, 1.0%, P < 0.001) and also in the female population (273, 8.6% vs 546, 4.9% in males, respectively, P < 0.001). Hypertension was also more common in women (119, 3.7% vs 205, 1.8%, P < 0.001; Table 3).
Table 3.
Factors associated with Cardio-vascular diseases
| n = (%) | P-value | OR (CI95%) | aOR | |
|---|---|---|---|---|
| Age group < 18 18–39 >39 |
38 (1.1) 263 (3.1) 520 (22.4) |
<0.001 | — 2.96 (2.10–4.16) 26.76 (19.16–37.38) |
— 2.69 (1.90–3.80) 18.53 (13.16–26.09) |
| Sex (female) | 273 (8.6) | <0.001 | 1.83 (1.57–2.12) | 1.48 (1.25–1.75) |
| Continent Asia America Africa Europe Oceania |
638 (5.5) 4 (7.8) 171 (6.5) 0 (0) 0 (0) |
<0.001 | — 1.47 (0.53–4.08) 1.20 (1.01–1.43)—— |
— 0.74 (0.24–2.33) 1.53 (1.26–1.86)—— |
| Smoking | 48 (5.7) | 0.985 | 1.00 (0.74–1.35) | 1.06 (0.76–1.46) |
| Diabetes | 200 (31.3) | <0.001 | 9.64 (8.01–11.60) | 3.31 (2.68–4.09) |
| Neurological disorders | 131 (11.2) | <0.001 | 2.29 (1.88–2.79) | 1.78 (1.41–2.24) |
| Mental health problems | 91 (14.4) | <0.001 | 3.00 (2.38–3.80) | 1.82 (1.38–2.41) |
| Cancer | 12 (18.8) | <0.001 | 3.85 (2.05–7.24) | 1.62 (0.78–3.34) |
Notes: Unadjusted and adjusted logistic regression calculating odds ratio (OR), adjusted odds ratio (aOR) and 95% CI of factors associated with cardio-vascular diseases. Adjusted for age-group, sex, continent of origin of the migrant, smoking, diabetes mellitus, having neurological disorders, having mental health problems and cancer.
Also, 1183 individuals (8.2%) had a neurological condition recorded, many of them headache or migraine (332, 28.1%), followed by epilepsy (89, 7.5%), stroke (16, 1.4%, being 77.8% of them past episodes) and peripheral neuropathy (9, 0.8%), including neuralgia, atypical facial pain and mononeuropathies of upper limb.
In total, 644 (4.5%) cases of Diabetes mellitus were reported. Diabetes was more frequently reported among older age-groups (448, 19.3% in > 40 years old, 185, 2.2% in 18–39-year-old group and 11, 0.3% in 0–17 year-old group; P < 0.001). Diabetes cases were more common among individuals from Asia (548, 4.7%) or Africa (82, 3.1%), although the differences were not significant after adjusting by age and sex. Only, eight cases of DM Type I were reported (1.2%), the remainder was Type II (320, 49.7%) or unknown (316, 49.1%). DM was associated with cardiovascular diseases (OR 9.6 [95% CI 8.0–11.6]; P < 0.001), and with female sex (OR 1.5 [95% CI 1.3–1.8]; P < 0.001).
Having Diabetes mellitus (aOR 3.3, [95% CI 2.7–4.1], P < 0.001), and neurological disorders (aOR 1.7, [95% CI 1.4–2.2], P < 0.001), being > 40 years old (aOR18.5, [95% CI 13.2–26.1]; P < 0.001) and being female (aOR 1.5, [95%CI 1.3–1.8]; P < 0.001) was associated with cardiovascular disorders in the multivariable logistic regression model (Table 3).
In total 212 (1.5%) cases of kidney disease were reported including chronic renal failure, nephrolithiasis, bladder disorders or haematuria. In addition, 399 (2.8%) cases of chronic liver diseases were reported, which was more frequent among >40 years (79/2330, 3.4%) and 19–39 years (312/8539, 3.7%, P < 0.001) and more frequent in males (374, 3.2% vs 1%, P < 0.001).
Mental health problems
In total, 641(4.4%) people had a mental health condition, being more frequent depressive episodes (152, 1.1%) followed by anxiety (150, 1%), post-traumatic stress disorders (PTSD) (102, 0.7%). They were more often reported from locations in Greece (481/7228, 6.7%), Bulgaria (2/28, 7.1%) and Croatia (37/566, 6.5%; P < 0.001).
Mental health problems were higher in the older group (175, 7.5%, P < 0.001, [adjusted OR 6.70, CI95% 4.13–10.89]) and female (211, 6.6% vs 430, 3.8%, P < 0.001; [aOR 1.56, 95%CI 1.16–2.12]).
They were more frequent in individuals from Africa (149, 5.7%) compared with Asia (484, 4.1%, P < 0.001; [OR 1.39, 95CI% 1.15–1.67]) although in the multivariable analysis, after adjusting for being exposed to torture or violence, the association was the opposite (Table 4). Having injuries, drug addictions and been exposed to previous torture or violence were also associated with having mental health problems. In those reporting torture or violence, mental health problems were associated with the region of origin, higher in migrants from Asia (52/320, 16.3%) compared Africa (69/824 8.4%; P < 0.001), whereas in the group not reporting violence or torture there were no differences in mental health problems by region of origin (P = 0.29).
Table 4.
Factors and conditions associated with Mental Health problems
| n (%) | P-value | OR | aOR | |
|---|---|---|---|---|
| Age-group < 18 18–39 >39 |
44 (1.2) 422 (5.0) 175 (7.5) |
<0.001 | — 4.17 (3.05–5.70) 6.51 (4.65–9.09) |
3.79 (2.51–5.71) 6.70 (4.13–10.89) |
| Sex (female) | 211 (6.6) | <0.001 | 1.76 (1.49–2.09) | 1.56 (1.16–2.12) |
| Migrant type Asylum seeker Refugees Other migrant groups |
116 (3.7) 37 (9.5) 488 (4.5) |
<0.001 | — 1.24 (1.01–1.52) 2.75 (1.87–4.05) |
— 1.40 (1.04–1.90) 3.27 (2.05–5.21) |
| Continent Asia America Africa Europe Oceania |
484 (4.1) 4 (7.8) 149 (5.7) 1 (9.1) 0 (0) |
0.008 | — 1.97 (0.71–5.49) 1.39 (1.15–1.67) 2.31 (0.30–18.12) — |
— 0.39 (0.48–3.22) 0.48 (0.34–0.67) 3.29(0.38–28.76) 1 (empty) |
| Having suffered torture or violence | 123 (10.7) | <0.001 | 2.96 (2.40–3.63) | 2.55 (1.82–3.55) |
| Injuries | 43 (7.4) | <0.001 | 1.76 (1.27–2.42) | 1.56 (0.93–2.63) |
| Drug addiction | 7 (53.9) | <0.001 | 25.36 (8.50–75.67) | 12.50(3.88–40.35) |
| Alcohol abuse | 32 (20.4) | <0.001 | 4.67 (3.09–7.04) | 3.58 (2.89–5.62) |
Notes: Unadjusted and adjusted logistic regression calculating odds ratio (OR), adjusted odds ratio (aOR) and 95% CI of factors associated with mental health problems. Adjusted for age-group, sex, continent of origin of the migrant, type of migrants, having suffered torture or violence, injuries, drug addiction and alcohol abuse.
Injuries
In total, 610 episodes of acute injuries were reported among 585 people, 88.4% (517) of them in men (P < 0.001), 382 (62.6%) in adults and 228 (37.4%) in children (P < 0.001; Table 2). There were 387 episodes (63.4%) of superficial injuries (wounds), 141 (23.1%) blunt traumas (including contusion or fractures), 45 bites, 15 assault and 14 burns. Most episodes were reported among individuals from Southern-Asia (70.7%) and Western-Asia (12.3%) and the majority were reported from Serbian health centres (306, 50.2%). Wounds were more frequently reported in men (P < 0.001). No episodes of injuries were reported in individuals with disabilities.
Disabilities
Disabilities were identified among 45 (0.31%) individuals with similar proportions in adults and children (P = 0.92). The most frequent ones were sequels of trauma, related to war, including blindness or visual defects, deafness or hypoacusis, hemiplegia, female genital mutilation, congenital abnormalities and mental disabilities.
Discussion
We provide a snapshot of health and disease among a vulnerable migrant population, which arrived in Southern Europe between 2016 and 2019 reported through the ePHR. The picture, which emerges shows a young, mostly healthy population with many acute infectious disease episodes particularly in children, but also with a by no means insignificant number of chronic conditions, providing important lessons for healthcare and public health.
In particular, adult women were found to present more cardio-vascular diseases compared with adult men with the same results observed in the complete-case sensitivity analysis. Although this finding is contrary to the established literature, other studies have also reported that migrant women had more risk factors for cardiovascular diseases compared with men.18 This may be an artefact of the migrant population and it could be partially explained by a different health seeking behaviour of migrant women compared with men, being proportionally more women attending the health assessments in the facilities compared with men.
We also found a high proportion of Diabetes Mellitus cases, particularly among underweight or normal weight individuals. This has also been reported in migrant populations from sub-Saharan African countries what could be explained by a metabolically unhealthy normal weight.19 Other studies have also reported higher cardiovascular risk in sub-Saharan African migrants in Europe compared with non-migrants living in both rural and urban areas in SSA20 as we also found it.
In keeping with other studies with similar populations we found a high proportion of infectious diseases and muscular-skeletal disorders.21 Common skin and respiratory infections were more prevalent in children whereas chronic infections such as HIV and TB were more frequent among older age-groups. TB, HIV or infectious hepatitis frequencies might be explained by prevalence rates in countries of origin and adverse circumstances during the migration route and/or in the camps. The high proportion of viral hepatitis reported, particularly hepatitis C, which were mostly reported in individuals from Asia, is noteworthy and should prompt further HCV prevalence studies in Asian migrants, for which there are some studies but focused on Indian, Pakistani or Bangladeshi communities22 but not from other Asian communities (i.e. Middle East region). In addition, many recorded hepatitis infections were reported to health professionals by the patients and had no laboratory confirmation in the system. Although it is possible that this proportion is overestimated, this fact certainly reflects the lack of laboratory capacity accessible to health staff from the reception centres.
Injuries were less frequently reported (4%), which is similar compared with other studies in refugees.23 However, there is literature evidence of injuries associated with the precarious condition of temporary installations,23,24 showing that ~11% of patients examined had suffered from injuries.24 This may be setting specific as supported by our study. Optimising such environments is an important need for the camp/reception centre populations, but also for the receiving country populations,25 as demonstrated in the current COVID pandemic.26
We found a relatively low rate of reported mental health conditions (<5%), and this is lower compared with other publications from similar settings,27–29 particularly in children where there have been reports of increased mental health problems compared with children from non-migrant parents.30 The most common mental health problems reported were depression and anxiety and were more frequently in individuals from African countries, particularly from Algeria and Democratic Republic of Congo. This is well aligned with other studies that reported the African origin as a risk factor for having a mental health associated problem.31,32 However, the majority of PTSD cases were reported in-persons from Asian countries, particularly from Afghanistan, Iran, Iraq and Syria. PTSD is more frequently found in refugees populations, particularly in those with war-related traumatic events, which are the most common trauma experiences among Syrian refugees.33 However, mental health was not assessed using specific questionnaires by qualified personnel, and not routinely assessed using specific intervention guides.34
The ePHR provide a unique opportunity to compile data from highly variable and poorly equipped migrant reception settings, and show its utility for securely recording and transferring medical information between clinicians even across countries, a distinct feature compared with other, similar systems.35 The information stored is in principle available at any time in any place for accredited health professionals, being a feasible solution to address health of migrants and refugees who move to other cities, or countries, what will improve certainly health care provided to users. Initial challenges of the ePHR that included the diversity of health systems’ quality and safety and data protection policies, have significantly progressed, particularly the interoperability of databases in cross-border settings.36 These data could be used to inform policy makers about which are chronic diseases more frequently reported in the populations over time. Our analysis benefits from specific features inbuilt into the ePHR, such as fixed categorical fields and the use of ICD-10 classification coding.
The study has also several limitations. First, the retrospective design may lead to inaccuracy or insufficient information on some variables. A number of variables had considerable amounts of missing data, likely to represent recording issues, and unlikely to be missing at random. We mitigated this limitation by developing a robust and replicable algorithm for imputation, which involved scrutinizing and cross-referencing each variable to complete data fields (not missing at random) based on information in other parts of the record. This included the review of free text of the medical records through specific key words using simple techniques of natural language processing methods, and we thereafter manually reviewed records identified by the key words to confirm the health condition and to avoid misclassification. Also, despite we searched key words in other local languages, we may have missed some key words that were expressing a health condition and that are not commonly used. We also did a sensitivity analysis that explored and confirmed that a complete case approach did not change our findings (difference across sex and age group strata), although certainly overestimated the proportion of cases reported for the majority of chronic diseases. Despite imputation, missing data may also due to under registry of health conditions, and they may have contributed to our unexpected low-reported findings in mental health. The use of this imputation method to facilitate data management should be further evaluated and validated as a proper method to manage missing data and if it could be used- to inform public health strategies.
Second, within the ePHR, laboratory tests have only been recorded in ~3% of the patients. It is therefore also possible that laboratory based diagnoses have been under-reported, including relevant and common conditions in migrant children such as anaemia or vitamin D deficiency or confirmation of viral hepatitis.27 We could not estimate the prevalence of health conditions, particularly for infectious disease since a systematic screening was not implemented. However, we can describe the pattern of chronic diseases, demonstrating a non-negligible proportion of these conditions.
Third, our study population comes mainly from sub-Saharan African and Asian countries. Our population cohort representativeness depends on settings, time and facility set up, and cannot be automatically extrapolated for all migrants on the Southern European border.
Finally, the information on reason for travelling was not recorded; however, the reasons for travel are usually complex and mixed, with common vulnerabilities if following specified routes and travelling irregularly.37 This distinguishes asylum seekers and refugees in our cohort, as the latter have acquired a status, which often allows them more regular means of travel.
Future studies should elucidate the feasibility and sustainability of ePHR system and to compare it with other software recently developed aimed to improve the data collection of the HISs such as the iHRIS38 (Health Workforce Information Systems Software) or the DHIS2 software.39 The use of EHRs across countries in mobile populations may avoid duplicate tests, and over-vaccination of populations since records will be efficiently tracked across the migration journey, preventing that important diseases or drug allergies are missed and improving patient care. This will benefit migrants and refugees but also will protect the public health of host countries.40
Conclusions
Our analysis highlights that ePHR is a valuable tool to efficiently collect health-related data to better address migrant health issues. We described a mostly healthy population with many acute infectious disease episodes particularly in children, but also with significant number of chronic conditions and less frequent injuries or mental health problem. By using PHR we were able to identify and describe the main disease burden in migrants arriving in Europe, thus providing guidance for resource allocation, and establishing appropriate health care services.
Supplementary Material
Acknowledgements
The authors would like to thank the donor that made the implementation of the project possible: DG SANTE, Chafea, in particular Isabel De la Mata, Cinthia Menel-Lemos (DG SANTE) and Paola d’Acapito (Chafea). In addition, we would like to thank to all partners, consultants and stakeholders engaged in the project implementation for their time and participation in the significant and substantial work, a small grasp of it provided in this re-port. We thank the representatives of Ministries of Health, Interior and Local Health Authorities, first reception and other migrant centres, representatives from international organizations, civil society organizations, academia, trainers, health organizations and health professionals, law enforcement officials and other first line responders who participated and contributed to the activities carried out within the project. Finally, we would like to convey thanks to colleagues in IOM EU/EEA country offices of Bulgaria, Croatia (Denis Novosel, Ivan Pitesa), Cyprus (Natasa Xenophontos), Greece (Irini Gerogli, Gianluca Rocco), Serbia (Ranko Petrovic, Berberovic Tamara) and Slovenia (Iva Perhavec), at the IOM Regional Office in Brussels and to Migration Health Division colleagues at IOM HQ and IOM Manila for their valuable contribution to the project. A special thanks to the project team who contributed to the successful project implementation: Roumyana Petrova-Benedict, Isabelle Beauclercq, Jordi Noguera and Federica Viello.
Contributor Information
Dominik Zenner, Global Public Health Unit, Wolfson Institute of Population Health, 58 Turner St, London E1 2AB, UK.
Ana Requena Méndez, Department of Medicine-Solna, Karolinska Institutet, 171 65 Solna, Sweden; Department of Infectious Diseases, Karolinska University Hospital, 171 76, Stockholm, Sweden; Barcelona Institute for Global Health (ISGlobal Campus Clinic), Barcelona 08036, Spain.
Steffen Schillinger, Migration Health Division, International Organization for Migration, 1226. Manila, Philippines.
Elena Val, Migrant Health Division, International Organization for Migration, Regional Office for the EU/EAA and NATO B-1000 Brussels, Belgium.
Kolitha Wickramage, Migration Health Division, International Organization for Migration, 1226. Manila, Philippines.
Authors’ contributions
ARM and DZ did the study design, literature search, coordinated the data analysis and drafted the manuscript; SS developed the data extraction and reviewed the manuscript; EV coordinated the implementation of the ePHR in the field, supported the data analysis and reviewed the manuscript; KW contributed to the study design, data analysis, data interpretation and drafting the manuscript. All authors contributed to the review, editing, final drafting and commenting on the manuscript.
Conflicts of interest
All authors declare no competing interest.
The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the manuscript.
Funding
This work has been supported by a grant from the European Commission (no. 20175101).
Ana Requena-Mendez is funded by Strategic Research Program in Epidemiology at Karolinska Institutet.
References
- 1. Beauchemin C. Family Migration from Sub-Saharan Africa to Europe, Organisation for Economic Co-operation and Development (OECD). Paris, France 2013.
- 2. Study-group-on-the-reception-system . Report on the Reception of Migrants and Refugees in Italy. Ministero dell'Interno, Rome (Italy) http://www.libertaciviliimmigrazione.dlci.interno.gov.it/sites/default/files/allegati/rapporto_accoglienza_eng_isbn_appendice_rev3b.pdf (2015).
- 3. International Organization for Migration . Migration. Flow Monitoring. (15 March 2022, date laset accessed) https://migration.iom.int/europe?type=arrivals (2018).
- 4. Council of the European Union . Eastern Mediterranean Route. 2020. (15 December 2021, date last accessed) https://www.consilium.europa.eu/en/policies/eu-migration-policy/eastern-mediterranean-route/.
- 5. United Nations . General Assembly High-Level Meeting to Address Large Movements of Refugees and Migrants. 2016. (15 December 2021, date last accessed) https://www.un.org/en/development/desa/population/migration/events/ga/2016/addressrefugeesmigrantssummit.html.
- 6. Abubakar I, Aldridge RW, Devakumar D et al. The UCL-Lancet Commission on migration and health: the health of a world on the move. Lancet 2018; 392:2606–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. United Nations . Global Compact for Safe, Orderly and Regular Migration. In: Resolution Adopted by the General Assembly on 19 December 2018. (A/76/642), (15 December 2021, date last accessed).
- 8. International Organization for Migration (IOM) 2015 World Migration Report . Migrants and Cities: New Partnerships to Manage Mobility, International Organization for Migration. 17 Route des Morillons 1211 Geneva 19 Switzerland 2015.
- 9. Seidler Y, Novak-Zezula S, Trummer U. ‘Falling off the radar’ of public health: the case of uninsured Chinese patients in Vienna, Austria. Health Policy (New York) 2019; 123:840–4. [DOI] [PubMed] [Google Scholar]
- 10. Lebano A, Hamed S, Bradby H et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health 2020; 20:1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pérez-Molina JA, López-Polín A, Treviño B et al. 6-year review of +Redivi: a prospective registry of imported infectious diseases in Spain. J Travel Med 2017; 24:1–7. 10.1093/jtm/tax035. [DOI] [PubMed] [Google Scholar]
- 12. McCarthy AE, Weld LH, Barnett ED et al. Spectrum of illness in international migrants seen at GeoSentinel clinics in 1997-2009, part 2: migrants resettled internationally and evaluated for specific health concerns. Clin Infect Dis 2013; 56:925–33. [DOI] [PubMed] [Google Scholar]
- 13. Bozorgmehr K, Biddle L, Rohleder S et al. Health evidence network: synthesis report. In: What is the Evidence on Availability and integration of refugee and migrant health data in health information systems in the WHO European Region? WHO Regional Office for Europe, UN City, Marmorvej 51 DK-2100 Copenhagen Φ, Denmark 2019. [PubMed] [Google Scholar]
- 14. World Health Organization . Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region. 2016. (15 December 2021, date last accessed). https://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/publications/2016/strategy-and-action-plan-for-refugee-and-migrant-health-in-the-who-european-region.
- 15. International Organization for Migration . Re-Health: ePHR. 2018. (25 January 2022, date last accessed). https://re-health.eea.iom.int/e-phr.
- 16. International Organization for Migration . Handbook for Health Professionals. Health Assessment of Refugees and Migrants in the EU/EEA 2015. 10.2875/4503212015. [DOI] [Google Scholar]
- 17. International Organization for Migration . IOM Data Protection Policy. International Organization for Migration. Geneva, Switzerland. https://publications.iom.int/system/files/pdf/iomdataprotection_web.pdf (2010).
- 18. Commodore-Mensah Y, Agyemang C, Aboagye JA et al. Obesity and cardiovascular disease risk among Africans residing in Europe and Africa: the RODAM study. Obes Res Clin Pract 2020; 14:151–7. [DOI] [PubMed] [Google Scholar]
- 19. Chilunga F, Henneman P, Ac Meek K et al. Prevalence and determinants of type 2 diabetes among lean African migrants and non-migrants: the RODAM study. J Glob Health 2019; 9:020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boateng D, Agyemang C, Beune R et al. Migration and cardiovascular disease risk among Ghanaian populations in Europe: the RODAM study (research on obesity and diabetes among African migrants). Circ Cardiovasc Qual Outcomes 2017; 10:e004013. [DOI] [PubMed] [Google Scholar]
- 21. Hermans M, Kooistra J, Cannegieter S et al. Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos, Greece. Eur J Epidemiol 2017; 32:851–4. [DOI] [PubMed] [Google Scholar]
- 22. Mann AG, Trotter CL, Balogun MA, Ramsay ME. Hepatitis C in ethnic minority populations in England. J Viral Hepat 2008; 15:421–6. [DOI] [PubMed] [Google Scholar]
- 23. Atiyeh B, Gunn SA. Refugee camps, fire disasters and burn injuries. Ann Burns Fire Disasters 2017; 30:214–7. [PMC free article] [PubMed] [Google Scholar]
- 24. van Berlaer G, Bohle Carbonell F, Manantsoa S et al. A refugee camp in the Centre of Europe: clinical characteristics of asylum seekers arriving in Brussels. BMJ Open 2016; 6:e013963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blitz BK, D’Angelo A, Kofman E, Montagna N. Health challenges in refugee reception: dateline Europe 2016. Int J Environ Res Public Health 2017; 14:1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Greenaway C, Hargreaves S, Barkati S et al. COVID-19: exposing and addressing health disparities among ethnic minorities and migrants. J Travel Med 2020; 27:taaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baauw A, Kist-van Holthe J, Slattery B et al. Health needs of refugee children identified on arrival in reception countries: a systematic review and meta-analysis. BMJ Paediatr Open 2019; 3:e000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Poole DN, Hedt-Gauthier B, Liao S et al. Major depressive disorder prevalence and risk factors among Syrian asylum seekers in Greece. BMC Public Health 2018; 18:908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet 2005; 365:1309–14. [DOI] [PubMed] [Google Scholar]
- 30. Fellmeth G, Rose-Clarke K, Zhao C et al. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet 2018; 392:2567–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Scherer N, Hameed S, Acarturk C et al. Prevalence of common mental disorders among Syrian refugee children and adolescents in Sultanbeyli district, Istanbul: results of a population-based survey. Epidemiol Psychiatr Sci 2020; 29:e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ventriglio A, Bellomo A, Petito A et al. Factors associated to the onset of mental illness among hospitalized migrants to Italy: a chart review. J Immigr Minor Health 2021; 23:425–33. [DOI] [PubMed] [Google Scholar]
- 33. Zbidat A, Georgiadou E, Borho A et al. The perceptions of trauma, complaints, somatization, and coping strategies among Syrian refugees in Germany—a qualitative study of an at-risk population. Int J Environ Res Public Health 2020; 17:693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. World Health Organization . mhGAP Training Manuals for the mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings, version 2.0. (15 January 2022, date last accessed). https://apps.who.int/iris/handle/10665 (2017).
- 35. Chiesa V, Chiarenza A, Mosca D, Rechel B. Health records for migrants and refugees: a systematic review. Health Policy 2019; 123:888–900. [DOI] [PubMed] [Google Scholar]
- 36. Footman K, Knai C, Baeten R, et al. Cross-border health care in Europe. Policy Summary vol. 14. WHO, Copenhagen. (15 January 2022, date last accessed) https://www.euro.who.int/__data/assets/pdf_file/0009/263538/Cross-border-health-care-in-Europe-Eng.pdf. [Google Scholar]
- 37. International Organization for Migration. World Migration Report 2020. Chapter 7 – Migration and Health: Current Issues, Governance and Knowledge Gaps. (15 January 2022, date last accessed). https://publications.iom.int/books/world-migration-report-2020-chapter-7.
- 38. iHRIS Software – Track, Manage, and Plan Your Health Workforce. (15 January 2022, date last accessed). https://www.ihris.org/.
- 39. DHIS2 Overview | DHIS2. (15 January 2022, date last accessed). https://dhis2.org/overview/.
- 40. Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med 2017; 24:1–8. 10.1093/jtm/tax016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.