Abstract
Background
The relationship between triglyceride-glucose (TyG) index, an emerging marker of insulin resistance, and the risk of incident heart failure (HF) was unclear. This study thus aimed to investigate this relationship.
Methods
Subjects without prevalent cardiovascular diseases from the prospective Kailuan cohort (recruited during 2006–2007) and a retrospective cohort of family medicine patients from Hong Kong (recruited during 2000–2003) were followed up until December 31st, 2019 for the outcome of incident HF. Separate adjusted hazard ratios (aHRs) summarizing the relationship between TyG index and HF risk in the two cohorts were combined using a random-effect meta-analysis. Additionally, a two-sample Mendelian randomization (MR) of published genome-wide association study data was performed to assess the causality of observed associations.
Results
In total, 95,996 and 19,345 subjects from the Kailuan and Hong Kong cohorts were analyzed, respectively, with 2,726 cases of incident HF in the former and 1,709 in the latter. Subjects in the highest quartile of TyG index had the highest risk of incident HF in both cohorts (Kailuan: aHR 1.23 (95% confidence interval: 1.09–1.39), PTrend <0.001; Hong Kong: aHR 1.21 (1.04–1.40), PTrend =0.007; both compared with the lowest quartile). Meta-analysis showed similar results (highest versus lowest quartile: HR 1.22 (1.11–1.34), P < 0.001). Findings from MR analysis, which included 47,309 cases and 930,014 controls, supported a causal relationship between higher TyG index and increased risk of HF (odds ratio 1.27 (1.15–1.40), P < 0.001).
Conclusion
A higher TyG index is an independent and causal risk factor for incident HF in the general population.
Clinical Trial Registration
URL: https://www.chictr.org.cn; Unique identifier: ChiCTR-TNRC-11,001,489.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-022-01658-7.
Keywords: Heart failure, Triglyceride-glucose index, Risk stratification, Mendelian randomization, Insulin resistance
Introduction
Heart failure (HF) is associated with significant morbidity and mortality, with contemporary five-year survival rates of less than 50% [1]. The prevalence of HF has been estimated to be 1–2% in developed countries and is projected to double by 2060 [2, 3]. Given the enormous public health and socioeconomic burden caused by HF, it is critically important to identify individuals at high risk of HF and to implement preventive interventions as early as possible [4].
Recently, the role of metabolic disorders in the development of HF has been increasingly investigated [5]. Insulin resistance, a hallmark of type II diabetes mellitus and metabolic syndrome, has been associated with adverse cardiac remodeling and dysfunction [6]. Molecular studies have provided ample evidence for the etiological role of insulin resistance in the development of HF [7, 8]. However, the gold standard method for measuring insulin sensitivity, the hyperinsulinaemic-euglycaemic clamp test, is time-consuming and invasive [9], which has impeded its widespread use in clinical practice.
The triglyceride-glucose (TyG) index, a simple, dimensionless marker derived from fasting blood triglyceride and glucose levels as measured in routine biochemical tests, has been proposed and validated as a surrogate marker of insulin resistance [10]. Previous studies have found a positive association between TyG index and the risk of various metabolic and atherosclerotic cardiovascular diseases [11, 12]. However, few studies have been conducted to investigate the association between TyG index and the risk of incident HF, and whether the association is causal remains undetermined.
Mendelian randomization (MR) makes use of genetic variants as instrumental variables (IVs) to generate causal estimates of the long-term effects of risk factors on outcomes [13]. MR analysis can overcome the limitations of residual confounding and reverse causation in conventional observational studies [13, 14]. With the development of genome-wide association studies (GWAS), MR is highly suited to investigate the causal association between TyG index and HF [15, 16].
As such, the present study aimed to assess the association between the TyG index and the risk of incident HF, as well as using a two-sample MR study to determine whether such associations were causal in nature.
Methods
Study design and population
Study subjects were identified from two Chinese studies, the Kailuan cohort in northern China and a territory-wide cohort in Hong Kong. The protocol for this study was in accordance with the guidelines of the Helsinki Declaration and this study was approved by the Ethics Committee at the Kailuan General Hospital and the Institutional Review Board of the University of Hong Kong / Hospital Authority Hong Kong West Cluster.
The Kailuan Study is a prospective cohort that based on a community in the Tangshan City. Details of the study has been published elsewhere [17]. In brief, a total of 101,510 subjects (aged 18–98 years; 81,110 males) were enrolled in the Kailuan Study at baseline (2006–2007), and received an interview of standardized questionnaires and clinical examinations at 11 hospitals responsible for health care of the community. The subjects were then followed up with repeated questionnaires, clinical and laboratory examinations every two years. All subjects gave informed consent to their enrolment in this study. Subjects with prevalent cancer and cardiovascular diseases, including HF, atrial fibrillation (AF), myocardial infarction, and ischemic stroke were excluded, as well as those with missing baseline levels of triglyceride (TG) or fasting blood glucose (FBG).
Data for the Hong Kong cohort were extracted retrospectively from the Clinical Data Analysis and Reporting System (CDARS), an administrative electronic medical records database that records the basic demographics, diagnoses, selected procedures, medication prescriptions, and selected laboratory measurements of all patients that attended public healthcare institutions in Hong Kong which serve an estimated 90% of the population [18]. Diagnoses in CDARS were recorded using International Classification of Diseases, Ninth revision (ICD-9) codes regardless of the time of data entry, as ICD-10 has not been implemented in CDARS to date. The ICD-9 codes used for identifying comorbid conditions and the outcome (HF) were summarized in Table S1. CDARS has been extensively used in prior studies and has been shown to have good diagnostic coding accuracy [19–22]. As only retrospective, deidentified data were used, the requirement for individual patient consent has been waived. For this study, adult patients (18 years old or above) attending a family medicine clinic in Hong Kong during the years 2000–2003 with at least one set of paired FBG and fasting TG levels at baseline were included. Patients with a history of ischemic heart disease, stroke, HF, AF, or cancer were excluded, as well as those who were pregnant at the time of inclusion, and those with missing baseline low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and total cholesterol levels.
Data collection and definitions
The data collected and definitions used in this study are detailed in Supplementary Methods [17, 23, 24]. The TyG index was calculated using the following formula, ln [fasting TG (mg/dl)×FBG (mg/dl) / 2] [25].
Outcomes and follow-up
In the Kailuan cohort, all subjects were followed from the baseline examination until the date of onset of HF, date of death, or end of follow-up (December 31st, 2019), whichever came first. HF was primarily diagnosed by experienced cardiologists in accordance with the guidelines of the European Society of Cardiology [26]. Cases of incident HF were supplemented by information from the Municipal Social Insurance Institutions, hospital discharge register, and death certificates.
In the Hong Kong cohort, all patients were followed up from inclusion until the first recorded diagnosis of HF, death, or the end of follow-up (December 31st, 2019), whichever came first. HF events of both hospitalized and outpatient episodes were identified using ICD-9 codes as summarized in Table S1.
Two-sample MR analysis
Mendelian randomization is built upon three main assumptions [27]. First, single-nucleotide polymorphisms (SNPs) selected as instrumental variables should be robustly associated with the exposure, here as TyG index. Second, the genetic instruments should not be related to factors that confound the exposure-outcome association. Third, genetic variants should affect outcome (HF) only through the exposure (TyG index).
TyG index-associated variants were retrieved from a previous GWAS based on the UK Biobank cohort [16]. In brief, the identified GWAS included 273,368 subjects with genetic data who were aged 40–69 and free from diabetes mellitus and lipid metabolism disorders. The effects of the instrumental SNPs on TyG index, as a continuous variable, were acquired at the genome-wide level of significance (P < 5 × 10− 8) by using linear regression adjusted for age, sex, and the top 5 genetic principal components to control population stratification. These SNPs were further pruned by linkage disequilibrium with R2 < 0.01 and those that were significantly associated with TG or glucose were also excluded. In total, 192 IVs were selected for TyG index initially. Summary statistics data for the associations of TyG index-associated SNPs with HF were extracted from the published GWAS performed by the Heart Failure Molecular Epidemiology for Therapeutic Targets (HERMES) Consortium on 47,309 cases and 930,014 controls of European ancestry [28]. HF cases from 26 cohorts of the HERMES Consortium were identified based on the clinical diagnosis of HF of any etiology with no specific criteria for left ventricular ejection fraction. Details of subject selection were published elsewhere [28].
Statistical analysis
Continuous variables were presented as mean ± standard deviation (SD) or median with interquartile range (IQR) depending on their distribution. Categorical variables were presented as frequencies and percentages.
Kaplan-Meier curves were used to visualize the cumulative incidence of HF across quartiles of the TyG index. The association between baseline TyG index and the risk of incident HF was analyzed using the Cox proportional hazards model, with hazard ratios (HR) with 95% confidence intervals (CI) as the summary statistics. The Cox regression was performed with a staged approach, as detailed in Supplementary Methods. The association between the risks of HF and the observed spectrum of TyG index was also modelled and visualized using fractional polynomial curves with full multivariable adjustments. Furthermore, competing risk regression using the Fine and Gray sub-distribution model was performed to address the potentially confounding issue of competing risk, with death from any cause as the competing event. Sub-hazard ratios (SHR) with 95% CI were used as the summary statistics. Sensitivity analyses were conducted by excluding subjects with less than two-year follow-up time, and, separately, those with medications at baseline.
A priori subgroup analyses were performed for age (< 65 vs. ≥ 65), gender (male vs. female), diabetes (yes vs. no), hypertension (yes vs. no), dyslipidemia (yes vs. no) for both cohorts, and, for the Kailuan cohort, for obesity (yes vs. no), and hs-CRP level (< 1 mg/dl vs. ≥ 1 mg/dl).
To combine the results from the two cohorts, we extracted hazard ratios from the fully adjusted model and performed a meta-analysis using the inverse variance method with random effects to estimate the association between TyG index, both as categorical and continuous variables, and the risk of incident HF.
In the MR analysis, the summary exposure and outcome data were first harmonized, and SNPs significantly associated with incident HF were excluded (P < 5 × 10− 8). Causal effects of TyG index on HF were estimated by the inverse-variance weighted (IVW) method. Weighted median, MR-Egger, and pleiotropy residual sum and outlier (MR-PRESSO) methods were used for supplementary analyses. Directional pleiotropy was assessed by MR-Egger intercepts and heterogeneity among genetic variants was evaluated by Cochran’s Q test.
To test the validity of causal effects estimates, several sensitivity analyses were conducted. First, MR analysis were conducted in SNPs pruned by linkage disequilibrium with R2 < 0.001. Second, multivariable MR (MVMR) using the IVW method was conducted to further investigate the direct causal effect of TyG index on HF after adjusting for confounders including body mass index (BMI) [29], systolic blood pressure (SBP) [30], diastolic blood pressure (DBP) [30], LDL-c [31], HDL-c [31], and DM [32]. An additional sensitivity analysis was performed by excluding any SNP significantly associated with these confounders (P < 5 × 10− 8).
All statistical analyses for the Kailuan and Hong Kong cohorts were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC), Stata 16.1 software (StataCorp, College Station, TX), and/or RevMan (Version 5.1; Cochrane Collaboration, Oxford, UK). The MR analyses were performed by the TwoSampleMR, MR-PRESSO and MVMR packages with R version 4.0.2. All p values were two-sided, with p < 0.05 considered statistically significant.
Results
Of the 101,510 subjects who took part in the Kailuan study, 95,996 subjects were analyzed after applying the exclusion criteria (Figure S1). For the Hong Kong cohort, 24,338 patients were identified for inclusion, and 19,345 patients were analyzed after applying the exclusion criteria (Figure S2). Tables 1 and 2 show the baseline characteristics of subjects according to the baseline TyG index quartiles of two cohorts.
Table 1.
The baseline characteristics of subjects in the Kailuan Cohort
| TyG index | |||||
|---|---|---|---|---|---|
| Characteristics | Total | Q1 | Q2 | Q3 | Q4 |
| 3.60–8.18 | 8.19–8.57 | 8.58–9.05 | 9.06–12.51 | ||
| Subjects (n) | 95,996 | 23,997 | 24,000 | 24,001 | 23,998 |
| TyG index | 8.65 ± 0.69 | 7.85 ± 0.27 | 8.38 ± 0.11 | 8.79 ± 0.14 | 9.58 ± 0.46 |
| Age, years | 51.4 ± 12.5 | 50.2 ± 13.7 | 51.4 ± 12.7 | 52.1 ± 12.2 | 52.0 ± 11.4 |
| Male, n (%) | 76,364(79.6) | 17,655(73.6) | 18,994(79.1) | 19,501(81.3) | 20,214(84.2) |
| Height (cm) | 167.4 ± 7.0 | 166.7 ± 7.0 | 167.5 ± 7.0 | 167.6 ± 7.0 | 167.9 ± 6.9 |
| BMI (kg/m2) | 25.0 ± 3.5 | 23.4 ± 3.2 | 24.6 ± 3.3 | 25.6 ± 3.3 | 26.4 ± 3.4 |
| Completed high school, n (%) | 18,746(19.5) | 5673(23.6) | 4483(18.7) | 4448(18.5) | 4142(17.3) |
| Income ≥ 800¥, n (%) | 13,133(13.7) | 3563(14.9) | 3093(12.9) | 3234(13.5) | 3243(13.5) |
| Daily Smoker, n (%) | 28,675(29.9) | 6902(28.8) | 6741(28.1) | 7173(29.9) | 7859(32.8) |
| Daily alcohol user, n (%) | 16,725(17.4) | 3891(16.2) | 3834(16.0) | 4125(17.2) | 4875(20.3) |
| Activity physical activity, n (%) | 13,935(14.5) | 3654(15.2) | 3356(14.0) | 3535(14.7) | 3390(14.1) |
| Systolic BP, mmHg | 131 ± 21 | 124 ± 20 | 129 ± 20 | 132 ± 21 | 136 ± 21 |
| Diastolic BP, mmHg | 83 ± 12 | 80 ± 11 | 83 ± 11 | 85 ± 1 | 87 ± 12 |
| FBG, mmol/L | 5.47 ± 1.67 | 4.80 ± 0.68 | 5.09 ± 0.76 | 5.44 ± 1.11 | 6.54 ± 2.66 |
| TC, mg/dL | 190.9 ± 44.1 | 179.3 ± 35.6 | 190.2 ± 37.3 | 197.9 ± 39.0 | 196.4 ± 58.1 |
| LDL-c, mg/dL | 90.6 ± 35.2 | 84.3 ± 35.8 | 92.2 ± 33.3 | 94.7 ± 33.99 | 91.2 ± 36.7 |
| HDL-c, mg/dL | 59.8 ± 15.5 | 60.5 ± 15.7 | 60.3 ± 14.8 | 59.3 ± 15.1 | 59.0 ± 16.3 |
| TG, mg/dL |
112.4 (78.8-170.8) |
62.0 (51.3–72.6) |
97.4 (86.7–108.0) |
137.2 (120.4-158.4) |
245.1 (192.9–346.0) |
| hs-CRP, mg/dl |
0.80 (0.30–2.16) |
0.60 (0.21–1.84) |
0.72 (0.29–1.99) |
0.88 (0.33–2.16) |
1.02 (0.40–2.61) |
| eGFR, mL/min/1.73m2 | 82.3 ± 25.7 | 85.8 ± 26.8 | 81.8 ± 25.4 | 81.4 ± 22.8 | 80.5 ± 27.2 |
| Diabetes Mellitus, n (%) | 8408(8.8) | 223(0.9) | 542(2.3) | 1699(7.1) | 5944(24.8) |
| Hypertension, n (%) | 4,1072(42.8) | 6847(28.5) | 9651(40.2) | 11,316(47.2) | 13,258(55.3) |
|
Anti-hypertensive drugs, n (%) |
9453(9.9) | 1440(6.0) | 1915(8.0) | 2714(11.3) | 3384(14.1) |
| Lipid-lowering drugs, n (%) | 709(0.7) | 81(0.3) | 130(0.5) | 168(0.7) | 330(1.4) |
| Diabetes drugs, n (%) | 2048(2.1) | 121(0.5) | 209(0.9) | 442(1.8) | 1273(5.3) |
Abbreviations: BMI: body mass index; BP: blood pressure; FBG: fasting blood glucose; TC: total cholesterol; LDL-c: low density lipoprotein cholesterol; HDL-c: low density lipoprotein cholesterol; TG: triglyceride; eGFR: estimated glomerular filtration rate; hs-CRP: high sensitivity C-reactive protein
Table 2.
The baseline characteristics of subjects in the cohort from Hong Kong
| TyG index | |||||
|---|---|---|---|---|---|
| Characteristics | Total | Q1 | Q2 | Q3 | Q4 |
| 4.78–6.89 | 6.90–7.31 | 7.32–7.80 | 7.81–11.38 | ||
| Subjects (n) | 19,345 | 4,861 | 4,859 | 4,812 | 4,813 |
| TyG index | 7.36 ± 0.68 | 6.54 ± 0.27 | 7.10 ± 0.12 | 7.54 ± 0.14 | 8.26 ± 0.42 |
| Age, years | 60.1 ± 12.9 | 58.1 ± 13.9 | 60.6 ± 12.9 | 60.6 ± 12.3 | 61.3 ± 12.2 |
| Male, n (%) | 7738 (40.0) | 1780 (36.6) | 1971 (40.6) | 1935 (40.2) | 2052 (42.6) |
| Systolic BP, mmHg | 139 ± 21 | 136 ± 21 | 139 ± 20 | 140 ± 20 | 142 ± 20 |
| Diastolic BP, mmHg | 76 ± 11 | 75 ± 12 | 76 ± 11 | 77 ± 11 | 77 ± 11 |
| FBG, mmol/L | 6.79 ± 3.18 | 5.35 ± 0.97 | 5.96 ± 1.41 | 6.72 ± 2.19 | 9.16 ± 4.94 |
| TC, mg/dL | 208.4 ± 42.0 | 197.0 ± 39.8 | 207.4 ± 40.9 | 212.4 ± 41.1 | 217.2 ± 43.5 |
| LDL-c, mg/dL | 124.7 ± 37.4 | 119.6 ± 35.5 | 128.3 ± 37.2 | 128.5 ± 37.3 | 122.4 ± 38.9 |
| HDL-c, mg/dL | 52.6 ± 14.6 | 61.0 ± 15.7 | 53.9 ± 14.0 | 49.5 ± 12.1 | 46.0 ± 11.7 |
| TG, mg/dL |
124.0 (88.6-179.8) |
743.5 (60.2–88.6) |
115.1 (98.3–132.0) |
160.3 (127.5-189.5) |
221.4 (159.4-292.3) |
| Dyslipidemia, n (%) | 9099 (47.0) | 1930 (39.7) | 2273 (46.8) | 2446 (50.8) | 2450 (50.9) |
| Diabetes Mellitus, n (%) | 6524(33.7) | 559 (11.5) | 1138 (23.4) | 1816 (37.7) | 3011 (62.6) |
| Hypertension, n (%) | 11,809 (61.0) | 2591 (53.3) | 2974 (61.2) | 3037 (63.1) | 3207 (66.6) |
| Chronic kidney disease, n (%) | 2930 (15.2) | 543 (11.2) | 730 (15.0) | 744 (15.5) | 913 (19.0) |
| Anti-hypertensive drugs, n (%) | 3834 (19.8) | 755 (15.5) | 990 (20.4) | 1011 (21.0) | 1078 (22.4) |
| Lipid-lowering drugs, n (%) | 1586 (8.2) | 303 (6.2) | 373 (7.7) | 419 (8.7) | 491 (10.2) |
| Diabetes drugs, n (%) | 995 (5.1) | 110 (2.3) | 194 (4.0) | 246 (5.1) | 445 (9.3) |
| Antiplatelets, n (%) | 814 (4.2) | 159 (3.3) | 191 (3.9) | 216 (4.5) | 248 (5.2) |
In the Kailuan cohort, there were 2,726 cases (2.8%) of incident HF over a mean follow-up of 12.3 ± 2.2 years, with an overall incidence rate of 2.3 (95% CI 2.2–2.4) cases per 1000 person years. In the Hong Kong cohort, there were 1,709 cases (7.0%) of incident HF over a mean follow-up of 16.2 ± 4.3 years, with an overall incidence rate of 5.5 (95% CI 5.3–5.8) cases per 1000 person years. Over the study duration, 10,825 subjects (11.3%) in the Kailuan cohort died (9,985 (10.1%) without developing HF), while 6,372 patients (32.9%) in the Hong Kong cohort died (4,996 (25.8%) without developing HF).
Associations between the TyG index and the risk of incident HF
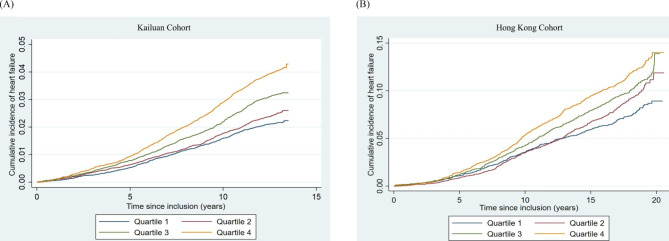
Tables 3 and 4 show the associations between the TyG index, assessed both as a categorial and continuous variable, with the respective risks of incident HF in the Kailuan and Hong Kong cohorts. The cumulative incidence of incident HF for the Kailuan and the Hong Kong cohort is shown in Fig. 1A and 1B, respectively. After fully adjusting for potential confounders, patients in the highest quartile of the TyG index had significantly higher risks of incident HF than those in the lowest quartile in both the Kailuan (HR 1.23 (95% CI 1.09–1.39), P < 0.001) and Hong Kong (HR 1.21 (95% CI 1.04–1.40), P = 0.007) cohorts. Similarly, every unit increment in the TyG index was associated with a 17% and a 13% increase in the risk of HF in the Kailuan (HR 1.17 (95% CI 1.10–1.24), P < 0.001) and Hong Kong (HR 1.13 (95% CI 1.05–1.22), P < 0.001) cohorts, respectively. Fractional polynomial curves with full multivariable adjustment (Figure S3) showed a possible threshold effect in the prognostic value of the TyG index, with a lower TyG index showing no significant association with the risk of incident HF, and a higher TyG index showing a grossly linear relationship with the said risk. This was consistent with the multivariable Cox regression analysis as shown in Tables 3 and 4 with TyG index analyzed as quartiles. Competing risk regression using the Fine and Gray sub-distribution model with death from any cause as the competing event also showed positive associations between a higher TyG index and a high risk of incident HF (Tables 3 and 4). Sensitivity analyses produced consistent and similar results (Tables 3 and 4).
Table 3.
Association between baseline TyG and incident heart failure in the Kailuan cohort
| Q1 | Q2 | Q3 | Q4 | P for trend | Per 1-unit increment | P value | |
|---|---|---|---|---|---|---|---|
| Number of patients | 23,997 | 24,000 | 24,001 | 23,998 | |||
| HF cases | 497 | 576 | 729 | 924 | |||
| Persons | 23,997 | 24,000 | 24,001 | 23,998 | |||
| Person-years | 297,098 | 295,908 | 294,857 | 292,552 | |||
| HF incidence 1 | 1.67(1.53–1.83) | 1.95(1.79–2.11) | 2.47(2.30–2.66) | 3.16(2.96–3.37) | |||
| Model 1 2 | 1 | 1.16(1.03–1.31) | 1.48(1.32–1.66) | 1.90(1.70–2.11) | < 0.001 | 1.44(1.37–1.51) | < 0.001 |
| Model 2 3 | 1 | 1.12(1.00-1.27) | 1.41(1.26–1.58) | 1.90(1.70–2.12) | < 0.001 | 1.47(1.40–1.55) | < 0.001 |
| Model 3 4 | 1 | 1.00(0.88–1.12) | 1.12(1.00-1.26) | 1.23(1.09–1.39) | < 0.001 | 1.17(1.10–1.24) | < 0.001 |
| Sensitivity analysis | |||||||
| Sensitivity analysis 1 5 | 1 | 1.00(0.88–1.13) | 1.14(1.01–1.28) | 1.23(1.10–1.41) | < 0.001 | 1.18(1.10–1.25) | < 0.001 |
| Sensitivity analysis 2 6 | 1 | 0.97(0.84–1.11) | 1.11(0.98–1.27) | 1.17(1.02–1.34) | 0.006 | 1.13(1.06–1.22) | < 0.001 |
| Competing risk regression 7 | 1 | 1.01(0.90–1.14) | 1.14(1.02–1.29) | 1.25(1.10–1.41) | < 0.001 | 1.18(1.10–1.25) | < 0.001 |
1 HF incidence; The incidence rates per 1000 person years with the corresponding 95% confidence intervals are shown
2 Model 1: Unadjusted. The hazard ratios with the corresponding 95% confidence intervals are shown
3 Model 2: Age-sex adjusted. The hazard ratios with the corresponding 95% confidence intervals are shown
4 Model 3: Adjusted for age, gender, education, income, physical activity, smoking status, alcohol intake, diabetes, LDL-c, HDL-c, SBP, DBP, BMI, eGFR, hs-CRP, anti-hypertensive drugs, anti-diabetes drugs, and lipid-lowering drugs. The hazard ratios with the corresponding 95% confidence intervals are shown
5 Sensitivity analysis 1: exclude follow-up time less than 2 years, remained 95,275 subjects with 2,497 HF cases. The hazard ratios with the corresponding 95% confidence intervals are shown
6 Sensitivity analysis 2: exclude subjects with medication at baseline (anti-hypertension drugs, lipid lower drugs, anti-diabetes drugs), remained 85,118 subjects with 2,118 HF cases. The hazard ratios with the corresponding 95% confidence intervals are shown
7 Competing risk regression: sub-hazard ratios with the corresponding 95% confidence intervals are shown
Table 4.
Association between baseline TyG index and incident heart failure in the cohort from Hong Kong
| Q1 | Q2 | Q3 | Q4 | P for trend | Per 1-unit increment | P value | |
|---|---|---|---|---|---|---|---|
| Number of patients | 4,861 | 4,859 | 4,812 | 4,813 | |||
| HF cases | 342 | 404 | 454 | 509 | |||
| Persons | 4861 | 4859 | 4812 | 4813 | |||
| Person-years | 79,353 | 77,644 | 77,335 | 75,360 | |||
| HF incidence 1 | 4.31(3.88–4.79) | 5.20(4.72–5.74) | 5.87(5.34–6.42) | 6.75(6.19–7.37) | |||
| Model 1 2 | 1 | 1.21(1.05–1.40) | 1.36(1.19–1.57) | 1.58(1.38–1.82) | < 0.001 | 1.30(1.22–1.39) | < 0.001 |
| Model 2 3 | 1 | 1.09(0.94–1.26) | 1.23(1.07–1.42) | 1.39(1.21–1.59) | < 0.001 | 1.23(1.14–1.31) | < 0.001 |
| Model 3 4 | 1 | 1.07(0.92–1.23) | 1.17(1.01–1.35) | 1.21(1.04–1.40) | 0.007 | 1.13(1.05–1.22) | 0.001 |
| Sensitivity analysis | |||||||
| Sensitivity analysis 1 5 | 1 | 1.07(0.92–1.23) | 1.17(1.01–1.35) | 1.22(1.05–1.41) | 0.005 | 1.14(1.05–1.23) | 0.001 |
| Sensitivity analysis 2 6 | 1 | 1.16(0.98–1.37) | 1.22(1.03–1.45) | 1.29(1.08–1.53) | 0.005 | 1.16(1.06–1.27) | 0.001 |
| Competing risk regression 7 | 1 | 1.06(0.91–1.22) | 1.21(1.04–1.40) | 1.24(1.07–1.44) | 0.001 | 1.15(1.06–1.24) | < 0.001 |
1 HF incidence; The incidence rates per 1000 person years with the corresponding 95% confidence intervals are shown
2 Model 1: Unadjusted. The hazard ratios with the corresponding 95% confidence intervals are shown
3 Model 2: Age-sex adjusted. The hazard ratios with the corresponding 95% confidence intervals are shown
4 Model 3: Adjusted for age, sex, hypertension, diabetes mellitus, chronic kidney disease, dyslipidemia, antihypertensives, anti-diabetic drugs, antiplatelets, lipid-lowering drugs. The hazard ratios with the corresponding 95% confidence intervals are shown
5 Sensitivity 1: exclude follow-up time less than 2 years, remained 19,227 subjects with 1,709 HF cases. The hazard ratios with the corresponding 95% confidence intervals are shown
6 Sensitivity 2: exclude those with medications at baseline, remained 14,842 subjects with 1,223 HF cases. The hazard ratios with the corresponding 95% confidence intervals are shown
7 Competing risk regression: sub-hazard ratios with the corresponding 95% confidence intervals are shown
Fig. 1.
Kaplan-Meier curve of the cumulative incidence of incident heart failure stratifying by quartiles of the triglyceride-glucose index. (A) Kailuan cohort and (B) Hong Kong cohort
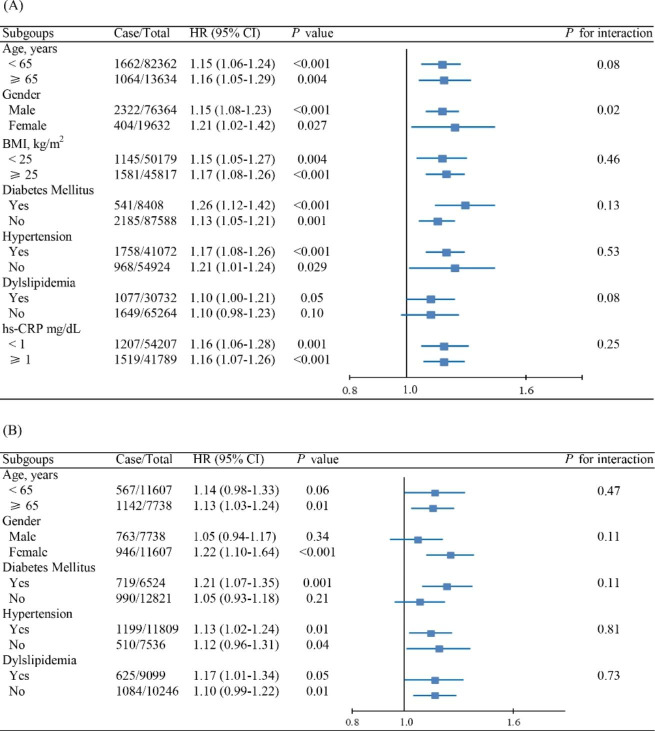
Results of subgroup analyses are shown in Fig. 2A and Fig. 2B for the Kailuan and Hong Kong cohorts, respectively. Generally, the TyG index, analyzed as a continuous variable, was positively associated with the risk of HF across various subgroups. There was significant interaction between gender and the TyG index in the Kailuan cohort (P for interaction = 0.02), but not in the Hong Kong cohort (P for interaction = 0.11). The association between TyG index and the risk of incident HF was more prominent in female subjects than in male subjects in both cohorts [HR 1.21 (95% CI 1.02–1.47) for female vs. 1.15 (95% CI 1.08–1.23) for male in the Kailuan cohort, and 1.22 (95% CI 1.10–1.64) vs. 1.05 (95% CI 0.94–1.17) in the Hong Kong cohort].
Fig. 2.
Subgroup analysis of the association between TyG index and incident HF for the (A) Kailuan cohort and (B) Hong Kong cohort
Abbreviations: TyG: triglyceride-glucose; HR: hazard ratio; CI: confidence interval
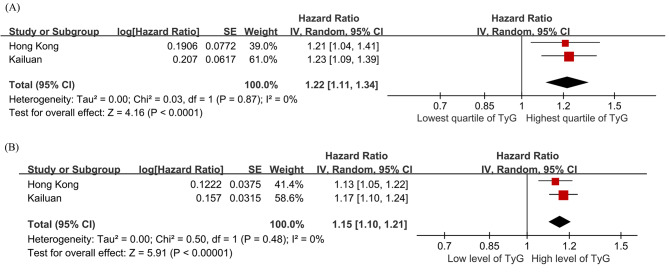
A random-effect meta-analysis combining the results from the two cohorts showed that the risk of incident HF of subjects in the highest quartile of the TyG index was 22% higher (95% CI 11% − 34%, P < 0.0001; Fig. 3A) than those in the lowest quartile, with every unit increment of the TyG index being associated with a 15% increase in the risk of incident HF (95% CI 10% − 21%, P < 0.00001; Fig. 3B). Similarly, subjects in the highest quartile of the TyG index had a 25% (95% CI 13% − 37%) increase in the sub-hazard of incident HF.
Fig. 3.
Forest plots for the meta-analysis of the association between TyG index with HF risk. (A) TyG index analyzed as a categorical variable. (B) TyG index analyzed as a continuous variable
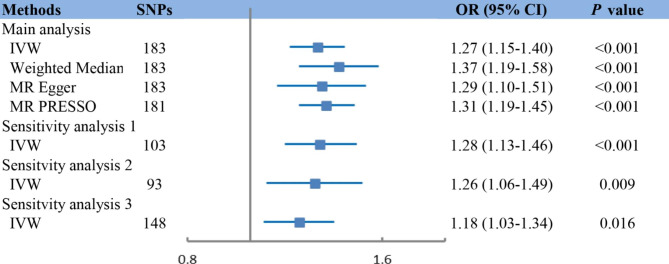
Two-sample MR analysis
The associations between genetically determined TyG index and the risk of incident HF as estimated by two-sample MR are presented in Fig. 4. Analysis using the IVW method demonstrated that genetic predisposition to increased TyG index was significantly associated with an increased risk of incident HF (OR 1.27, 95% CI 1.15–1.40, P < 0.001). The Cochran’s Q statistic indicated significant heterogeneity across SNPs, while no indication of directional pleiotropy was found by MR-Egger intercept (Table S2). The association remained consistent when using complementary methods for analysis, including weighted median, MR-Egger and MRPRESSO (Fig. 4).
Fig. 4.
Mendelian randomization (MR) association between genetically determined TyG index and HF. Sensitivity analysis 1: MR analysis through IVW method in SNPs pruned by linkage disequilibrium with R2 < 0.001 Sensitivity analysis 2: Multivariable MR through IVW method after adjusting for cofounders including BMI, SBP, DBP, LDL-c, HDL-c, and DM. Sensitivity analysis 3: MR analysis through IVW method after excluding any SNPs significantly associated with those confounders, including BMI, SBP, DBP, LDL-c, HDL-c, and DM.
Abbreviations: SNPs: single-nucleotide polymorphisms; OR: odds ratio; IVW: inverse-variance weighted
To verify the causal effect of TyG index on HF, we performed multivariable MR analysis by adjusting for HF risk factors, including BMI, blood pressure, and lipids. The association remained stable after adjusting for single risk factors (Table S3) and in a fully adjusted model (OR 1.20, 95% CI 1.02–1.41, P = 0.03; Fig. 4). Furthermore, results of the sensitivity analysis, in which 32 SNPs with potential pleiotropy were excluded, confirmed the positive association between genetically determined TyG index and HF risk (OR 1.19, 95% CI 1.05–1.35, P = 0.01).
Discussion
Utilizing observational data from two large Chinese cohorts and a two-sample MR analysis based on public GWAS datasets, this study demonstrated that a high TyG index was an independent and causal risk factor for incident HF in the general population.
Previous studies have found independent associations between TyG index and risks of atherosclerotic cardiovascular diseases, including myocardial infarction and ischemic stroke [25, 33]. In a recent analysis of data from the Atherosclerosis Risk in Communities (ARIC) study, Huang et al. also reported an association between higher TyG index and higher risk of incident HF in an American population, with every standard deviation’s increase in TyG index (corresponding to a TyG index of 0.6) associated with a 15% increase in risk [34]. Our study confirmed these findings in two larger cohorts from distinct geographical regions in China. Unlike the ARIC study which was restricted to subjects between the ages of 45–64 years old, our study included adult patients across the full age range. As such, our study more closely reflects real-life practice, and our findings are thus more directly generalizable.
Importantly, utilizing MR of GWAS data, we demonstrated that the association between TyG and HF was causal by nature. The magnitude of increase in risk per unit increment of TyG index were 15% (95% CI: 10-21%) in real-world cohorts and 27% (95% CI: 15-40%) in MR analysis. Although the exact underlying mechanism for the association between TyG index and HF remains to be confirmed by further molecular studies, the well-established relationship between TyG index and insulin resistance suggests that insulin resistance may at least be an important driver of such association [10]. This was further reinforced by the results from the Kailuan cohort showing that the association between TyG index and HF was independent of chronic inflammation, as well as previous studies observing associations between insulin resistance and higher risks of incident HF independent of myocardial ischaemia [35–37]. Insulin resistance may lead to excessive circulating free fatty acids and triglycerides, which induces cardiac lipotoxicity by generating toxic lipid intermediates, and decreases cardiac efficiency by increasing fatty acid oxidation [38, 39]. Insulin resistance is also associated with disturbances of the systemic metabolic and inflammatory milieu, including increased concentrations of proinflammatory cytokines, adipokines, and catecholamines, which may trigger low-grade inflammation and chronic hypercatecholaminemia that result in detrimental effects on cardiac function [40]. Furthermore, insulin resistance is involved in the maladaptive activation of the renin-angiotensin-aldosterone system, with chronic hyperinsulinaemia inducing increased release of angiotensinogen from adipose tissue and upregulation of angiotensin II receptor expression, eventually resulting in adverse cardiac remodeling and dysfunction [41]. Nonetheless, the mechanisms between insulin resistance and HF are incompletely understood to date, and remain an important area of further research.
Another major finding of the present study is that the association between TyG index and the risk of HF was stronger in females than in males. Between-gender differences are common in cardiovascular medicine. Previous studies have shown that women with disorders of glucose metabolism have a greater risk of coronary heart disease than men [33, 42]. HF caused by obesity, diabetes, or metabolic syndrome was also found to be more common in women [43]. These observations may be mediated by between-gender differences in molecular mechanisms, particularly those in hormonal axes, which not only influence glucose and lipid metabolism, but also cardiac function. Females are known to be less likely than males to develop insulin resistance [44] but are at higher risk of diabetic cardiomyopathy [45], implying that females may be more susceptible to cardiac damage induced by insulin resistance. Gender differences in nitric oxide synthase (NOS) activity and signaling, which are critical in metabolic regulation and in modulating responses to insulin resistance, are thought to be central to these observations [46]. The higher baseline levels of NOS in females predisposes to higher levels of uncoupled NOS on exposure to oxidative stress, which exacerbates the effects of insulin resistance, such as myocardial fibrosis and hypertrophy [46]. Additionally, considering that the mean age of subjects in this study implied that the female subjects were mostly postmenopausal, the postmenopausal decline in the protective effects of estrogen may contribute to gender differences in the susceptibility to insulin resistance-induced cardiac damage [43]. Notwithstanding the existing evidence as discussed above, further studies exploring the gender differences in susceptibility to insulin resistance-induced cardiac damage should provide important insights and better understanding of diabetic cardiomyopathy.
Having derived consistent findings from two geographically distinct regions in China, our results suggest that the TyG index, as a surrogate marker of insulin resistance, may be widely applicable and prognostically useful regardless of geographical region. As subjects with prevalent major cardiovascular diseases were excluded from the present study, the analyzed cohorts had relatively low cardiovascular risks. Our results supported the TyG index as a potentially viable and effective tool for cardiovascular risk stratification in the general population. Of note, insulin resistance in many previous studies was measured by the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) which requires measurements of fasting insulin and glucose [35, 36]. However, measuring insulin levels is expensive, and the HOMA-IR has been mostly confined to research uses with low clinical utilization. In contrast, the TyG index is simple to measure, has been validated against the euglycemic-hyperinsulinemic clamp test which is considered the gold standard for measuring insulin resistance [10], and may outperform the HOMA-IR in identifying insulin resistance [47]. It has also been shown to be excellent at detecting insulin resistance in non-diabetic patients [48], which is important as insulin resistance and its associated cardiovascular damage precedes overt type II diabetes mellitus [49]. The TyG index may therefore facilitate recognition of patients at elevated risk of incident HF, for which efficacious measures for primary prevention exist [4].
Strengths and limitations
The strengths of our study included the large sample size, long follow-up time, and having demonstrated reproducible results across two independent observational cohorts and MR analysis. Our findings were further strengthened by multiple subgroup and sensitivity analyses yielding largely consistent results. To the best of the authors’ knowledge, this was one of the first studies demonstrating causality between higher TyG index and higher risk of incident HF. Nonetheless, some limitations must be noted. First, we were unable to compare the predictive power of different methods for assessing insulin resistance in our observational study, since fasting insulin levels were unavailable for most subjects. Second, inherent to all observational studies, there may be residual or unmeasured confounders that we were not able to address. Nonetheless, we have included multiple important risk factors for incident HF in the multivariable regression models, and the numerous sensitivity analyses yielded consistent results which reinforced the validity of our findings. Third, the MR analysis was restricted to patients of European descent to reduce bias from population stratification, which may limit extrapolation of our MR results to other populations. Nevertheless, given that associations between TyG index and the risk of incident HF observed in a recent report in an American cohort (the ARIC study) were comparable to our findings as observed in Chinese cohorts, the causality established by our MR analysis is likely true in Chinese population as well. Fourth, no information was available about the subtype of incident HF. Given the different metabolic mechanisms contributing to the pathogenesis of different types of HF [50], further research in this regard is warranted. Fifth, diagnoses of the Hong Kong cohort were identified using ICD-9 codes and could not be individually adjudicated due to the retrospective, deidentified nature of the database, as well as the large sample size. Regardless, all diagnostic codes were entered by treating clinicians, who were completely independent of the authors. CDARS has also been shown to have good coding accuracy, specifically for cardiovascular outcomes [51].
Conclusion
As observed from two large, geographically distinct Chinese cohorts, a higher TyG index was independently associated with higher risk of incident HF. MR analysis demonstrated that the association was likely causal in nature. Further studies are warranted to confirm our findings and fully elucidate the underlying biological mechanisms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors appreciate all the subjects involved in this study, their families, and the members of the survey team from the Kailuan community.
The authors are grateful to Mr.Shucheng Si of Cheeloo College of Medicine in Shandong University for the instructions on Mendelian randomization analysis.
Abbreviations
- HF
heart failure.
- AF
atrial fibrillation.
- HR
hazard ratios.
- CI
confidence intervals.
- MR
mendelian randomization.
- GWAS
genome-wide association studies.
- LDL-C
low-density lipoprotein cholesterol.
- HDL-C
high-density lipoprotein cholesterol.
- TG
triglyceride.
- FBG
fasting blood glucose.
- CRP
c-reactive protein.
- BMI
body mass index.
- SBP
systolic blood pressure.
- DBP
diastolic blood pressure.
- DM
diabetes.
- TyG
Triglyceride-glucose.
- CDARS
Clinical Data Analysis and Reporting System.
- ICD
International Classification of Diseases.
- SNP
single-nucleotide polymorphism.
- HERMES
Heart Failure Molecular Epidemiology for Therapeutic Targets.
- SD
standard deviation.
- IQR
interquartile range.
- IVW
inverse-variance weighted.
- PRESSO
pleiotropy residual sum and outlier.
- ARIC
Atherosclerosis Risk in Communities.
- NOS
nitric oxide synthase.
- HOMA-IR
Homeostatic Model Assessment for Insulin Resistance.
Author contributions
X.L. and J.C. designed this study, conducted the main analysis, drafted the manuscript and served as the equally contributing first authors of the manuscript. B.G., S.P., X.W., and X.L. contributed to acquisition of data, analysis and interpretation of data. Z.J., J.H., Y.L., D.S., S.T., and S.W. contributed to the revision of the draft of the manuscript. S.C., G.T., and S.L. contributed to study concept and design, study supervision or coordination, revision of the drafting of the manuscript and served as the corresponding authors of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81970273), the Clinical Research Plan of Shenkang Hospital Development Center of Shanghai (No. SHDC2020CR4009, SHDC2020CR6012), the Shanghai Pujiang Program (21PJD057), and the Clinical Research Plan of Shanghai Municipal Health Commission (No. 202040461).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was performed according to the guidelines of the Helsinki Declaration and was approved by the Ethics Committee of Kailuan General Hospital (approval number: 2006-05) and the Institutional Review Board of the University of Hong Kong / Hospital Authority Hong Kong West Cluster (reference number: UW 20–250).
All the genetic data used in this study were derived from GWAS for which ethical approval and patient consent were previously obtained.
Consent for publication
Not applicable.
Competing interests
These authors declare that they have no conflicts of interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xintao Li and Jeffrey Shi Kai Chan have contributed equally to this work and share first authorship.
Contributor Information
Songwen Chen, Email: chensongwen@hotmail.com.
Gary Tse, Email: garytse86@gmail.com.
Shaowen Liu, Email: shaowen.liu@hotmail.com.
References
- 1.Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat reviews Cardiol. 2016;13(6):368–78. doi: 10.1038/nrcardio.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 3.de Boer RA, Nayor M, deFilippi CR, Enserro D, Bhambhani V, Kizer JR, Blaha MJ, Brouwers FP, Cushman M, Lima JAC, et al. Association of Cardiovascular Biomarkers With Incident Heart Failure With Preserved and Reduced Ejection Fraction. JAMA Cardiol. 2018;3(3):215–24. doi: 10.1001/jamacardio.2017.4987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greene SJ, Butler J. Primary Prevention of Heart Failure in Patients With Type 2 Diabetes Mellitus. Circulation. 2019;139(2):152–4. doi: 10.1161/CIRCULATIONAHA.118.037599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho KL, Karwi QG, Connolly D, Pherwani S, Ketema EB, Ussher JR, Lopaschuk GD. Metabolic, structural and biochemical changes in diabetes and the development of heart failure. Diabetologia. 2022;65(3):411–23. doi: 10.1007/s00125-021-05637-7. [DOI] [PubMed] [Google Scholar]
- 6.Kishi S, Gidding SS, Reis JP, Colangelo LA, Venkatesh BA, Armstrong AC, Isogawa A, Lewis CE, Wu C, Jacobs DR, Jr. et al: Association of insulin resistance and glycemic metabolic abnormalities with LV structure and function in middle age: The CARDIA study. JACC Cardiovasc Imaging 2017, 10(2):105–114. [DOI] [PubMed]
- 7.Riehle C, Abel ED. Insulin Signaling and Heart Failure. Circ Res. 2016;118(7):1151–69. doi: 10.1161/CIRCRESAHA.116.306206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Velez M, Kohli S, Sabbah HN. Animal models of insulin resistance and heart failure. Heart Fail Rev. 2014;19(1):1–13. doi: 10.1007/s10741-013-9387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antuna-Puente B, Disse E, Rabasa-Lhoret R, Laville M, Capeau J, Bastard JP: How can we measure insulin sensitivity/ resistance? Diabetes Metab 2011, 37(3):179–188. [DOI] [PubMed]
- 10.Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, Jacques-Camarena O, Rodríguez-Morán M. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51. doi: 10.1210/jc.2010-0288. [DOI] [PubMed] [Google Scholar]
- 11.Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76. doi: 10.1186/s12933-021-01268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zou S, Yang C, Shen R, Wei X, Gong J, Pan Y, Lv Y, Xu Y. Association Between the Triglyceride-Glucose Index and the Incidence of Diabetes in People With Different Phenotypes of Obesity: A Retrospective Study. Front Endocrinol (Lausanne) 2021;12:784616. doi: 10.3389/fendo.2021.784616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith GD, Ebrahim S. ’Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32(1):1–22. doi: 10.1093/ije/dyg070. [DOI] [PubMed] [Google Scholar]
- 14.Larsson SC, Burgess S, Michaëlsson K. Association of Genetic Variants Related to Serum Calcium Levels With Coronary Artery Disease and Myocardial Infarction. JAMA. 2017;318(4):371–80. doi: 10.1001/jama.2017.8981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Peng S, Guan B, Chen S, Zhou G, Wei Y, Gong C, Xu J, Lu X, Zhang X, et al. Genetically Determined Inflammatory Biomarkers and the Risk of Heart Failure: A Mendelian Randomization Study. Front Cardiovasc Med. 2021;8:734400. doi: 10.3389/fcvm.2021.734400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Si S, Li J, Li Y, Li W, Chen X, Yuan T, Liu C, Li H, Hou L, Wang B, et al. Causal Effect of the Triglyceride-Glucose Index and the Joint Exposure of Higher Glucose and Triglyceride With Extensive Cardio-Cerebrovascular Metabolic Outcomes in the UK Biobank: A Mendelian Randomization Study. Front Cardiovasc Med. 2020;7:583473. doi: 10.3389/fcvm.2020.583473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu S, Huang Z, Yang X, Zhou Y, Wang A, Chen L, Zhao H, Ruan C, Wu Y, Xin A, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–93. doi: 10.1161/CIRCOUTCOMES.111.963694. [DOI] [PubMed] [Google Scholar]
- 18.Kong X, Yang Y, Gao J, Guan J, Liu Y, Wang R, Xing B, Li Y, Ma W. Overview of the health care system in Hong Kong and its referential significance to mainland China. J Chin Med Assoc. 2015;78(10):569–73. doi: 10.1016/j.jcma.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Chan JSK, Satti DI, Lee YHA, Hui JMH, Lee TTL, Chou OHI, Wai AKC, Ciobanu A, Liu Y, Liu T, et al: High visit-to-visit cholesterol variability predicts heart failure and adverse cardiovascular events: a population-based cohort study. Eur J Prev Cardiol 2022. [DOI] [PubMed]
- 20.Tsoi MF, Chung MH, Cheung BMY, Lau CS, Cheung TT. Epidemiology of gout in Hong Kong: a population-based study from 2006 to 2016. Arthritis Res Ther. 2020;22(1):204. doi: 10.1186/s13075-020-02299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou J, Liu X, Chou OH, Li L, Lee S, Wong WT, Zhang Q, Chang C, Liu T, Tse G, et al: Lower risk of gout in sodium glucose cotransporter 2 (SGLT2) inhibitors versus dipeptidyl peptidase-4 (DPP4) inhibitors in type-2 diabetes. Rheumatology (Oxford) 2022. [DOI] [PubMed]
- 22.Chan JSK, Lakhani I, Lee TTL, Chou OHI, Lee YHA, Cheung YM, Yeung HW, Tang P, Ng K, Dee EC, et al: Cardiovascular outcomes and hospitalizations in Asian patients receiving immune checkpoint inhibitors: a population-based study. Curr Probl Cardiol 2022:101380. [DOI] [PubMed]
- 23.Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, Kurella Tamura M, Feldman HI. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713–35. doi: 10.1053/j.ajkd.2014.01.416. [DOI] [PubMed] [Google Scholar]
- 24.Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, Crews DC, Doria A, Estrella MM, Froissart M, et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N Engl J Med. 2021;385(19):1737–49. doi: 10.1056/NEJMoa2102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang A, Wang G, Liu Q, Zuo Y, Chen S, Tao B, Tian X, Wang P, Meng X, Wu S, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46. doi: 10.1186/s12933-021-01238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich A, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26(11):1115–40. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 27.Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30(7):543–52. doi: 10.1007/s10654-015-0011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G, Hedman ÅK, Wilk JB, Morley MP, Chaffin MD, et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11(1):163. doi: 10.1038/s41467-019-13690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, Powell C, Vedantam S, Buchkovich ML, Yang J, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, Ntritsos G, Dimou N, Cabrera CP, Karaman I, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50(10):1412–25. doi: 10.1038/s41588-018-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Willer CJ, Schmidt EM, Sengupta S, Peloso GM, Gustafsson S, Kanoni S, Ganna A, Chen J, Buchkovich ML, Mora S, et al. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45(11):1274–83. doi: 10.1038/ng.2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahajan A, Go MJ, Zhang W, Below JE, Gaulton KJ, Ferreira T, Horikoshi M, Johnson AD, Ng MC, Prokopenko I, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46(3):234–44. doi: 10.1038/ng.2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, Wang A. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20(1):19. doi: 10.1186/s12933-020-01210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang R, Lin Y, Ye X, Zhong X, Xie P, Li M, Zhuang X, Liao X. Triglyceride-glucose index in the development of heart failure and left ventricular dysfunction: analysis of the ARIC study. Eur J Prev Cardiol 2022. [DOI] [PubMed]
- 35.Banerjee D, Biggs ML, Mercer L, Mukamal K, Kaplan R, Barzilay J, Kuller L, Kizer JR, Djousse L, Tracy R, et al. Insulin resistance and risk of incident heart failure: Cardiovascular Health Study. Circ Heart Fail. 2013;6(3):364–70. doi: 10.1161/CIRCHEARTFAILURE.112.000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vardeny O, Gupta DK, Claggett B, Burke S, Shah A, Loehr L, Rasmussen-Torvik L, Selvin E, Chang PP, Aguilar D, et al. Insulin resistance and incident heart failure the ARIC study (Atherosclerosis Risk in Communities) JACC Heart Fail. 2013;1(6):531–6. doi: 10.1016/j.jchf.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wamil M, Coleman RL, Adler AI, McMurray JJV, Holman RR. Increased Risk of Incident Heart Failure and Death Is Associated With Insulin Resistance in People With Newly Diagnosed Type 2 Diabetes: UKPDS 89. Diabetes Care. 2021;44(8):1877–84. doi: 10.2337/dc21-0429. [DOI] [PubMed] [Google Scholar]
- 38.Kolwicz SC, Jr, Purohit S, Tian R. Cardiac metabolism and its interactions with contraction, growth, and survival of cardiomyocytes. Circ Res. 2013;113(5):603–16. doi: 10.1161/CIRCRESAHA.113.302095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yazıcı D, Sezer H. Insulin Resistance, Obesity and Lipotoxicity. Adv Exp Med Biol. 2017;960:277–304. doi: 10.1007/978-3-319-48382-5_12. [DOI] [PubMed] [Google Scholar]
- 40.Nishida K, Otsu K. Inflammation and metabolic cardiomyopathy. Cardiovasc Res. 2017;113(4):389–98. doi: 10.1093/cvr/cvx012. [DOI] [PubMed] [Google Scholar]
- 41.Samuelsson AM, Bollano E, Mobini R, Larsson BM, Omerovic E, Fu M, Waagstein F, Holmäng A. Hyperinsulinemia: effect on cardiac mass/function, angiotensin II receptor expression, and insulin signaling pathways. Am J Physiol Heart Circ Physiol. 2006;291(2):H787–96. doi: 10.1152/ajpheart.00974.2005. [DOI] [PubMed] [Google Scholar]
- 42.Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57(8):1542–51. doi: 10.1007/s00125-014-3260-6. [DOI] [PubMed] [Google Scholar]
- 43.Gerdts E, Regitz-Zagrosek V. Sex differences in cardiometabolic disorders. Nat Med. 2019;25(11):1657–66. doi: 10.1038/s41591-019-0643-8. [DOI] [PubMed] [Google Scholar]
- 44.Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal JF, Montagner A, Gourdy P. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63(3):453–61. doi: 10.1007/s00125-019-05040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Toedebusch R, Belenchia A, Pulakat L. Diabetic Cardiomyopathy: Impact of Biological Sex on Disease Development and Molecular Signatures. Front Physiol. 2018;9:453. doi: 10.3389/fphys.2018.00453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murphy E, Amanakis G, Fillmore N, Parks RJ, Sun J. Sex Differences in Metabolic Cardiomyopathy. Cardiovasc Res. 2017;113(4):370–7. doi: 10.1093/cvr/cvx008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vasques AC, Novaes FS, de Oliveira Mda S, Souza JR, Yamanaka A, Pareja JC, Tambascia MA, Saad MJ, Geloneze B. TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pract. 2011;93(3):e98–100. doi: 10.1016/j.diabres.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 48.Toro-Huamanchumo CJ, Urrunaga-Pastor D, Guarnizo-Poma M, Lazaro-Alcantara H, Paico-Palacios S, Pantoja-Torres B, Ranilla-Seguin VDC, Benites-Zapata VA. Triglycerides and glucose index as an insulin resistance marker in a sample of healthy adults. Diabetes Metab Syndr. 2019;13(1):272–7. doi: 10.1016/j.dsx.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 49.Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122. doi: 10.1186/s12933-018-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lakhani I, Leung KSK, Tse G, Lee APW. Novel Mechanisms in Heart Failure With Preserved, Midrange, and Reduced Ejection Fraction. Front Physiol. 2019;10:874. doi: 10.3389/fphys.2019.00874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong AY, Root A, Douglas IJ, Chui CS, Chan EW, Ghebremichael-Weldeselassie Y, Siu CW, Smeeth L, Wong IC. Cardiovascular outcomes associated with use of clarithromycin: population based study. BMJ. 2016;352:h6926. doi: 10.1136/bmj.h6926. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.