Abstract
Purpose
This study aims to estimate the prevalence of insomnia and related risk factors during the Delta wave of the COVID-19 pandemic in the Kingdom of Bahrain.
Methods
An analytical cross-sectional study included 646 individuals from the general population aged 18 years and over, living in the Kingdom of Bahrain during the Delta wave of the pandemic. Data were collected by an anonymous online questionnaire using the snowball-sampling technique between June and August 2021. We used the Insomnia Severity Index (ISI) and the generalized anxiety disorder scale (GAD-7) to measure the level of insomnia and anxiety, respectively.
Results
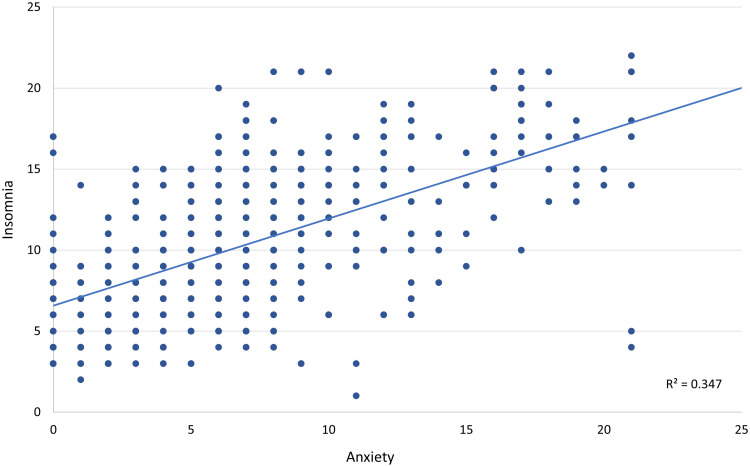
A total of 646 individuals participated in the study. Most of the participants were females (86%). The mean age was 38.7 ± 12.7 years (age range 18–89) and around half of the participants were 35 years or older. Clinical insomnia was reported by 20% [95% CI, 16.9–20.0] of the participants, and 50.1% [95% CI, 46.2–50.1] had subclinical insomnia according to ISI. The proportion of insomnia was significantly higher among females, healthcare workers, participants with lower educational levels, a lower or decreased monthly income during the pandemic, or participants who reported anxiety symptoms (all P < 0.01). Scales of anxiety and insomnia revealed a high correlation (r2 = 0.347, P< 0.01). The logistic regression model confirmed that factors independently associated with insomnia are female gender (OR=1.94, 95% CI, 1.00–3.76, P < 0.050) as well as presence of anxiety (GAD-7 score ≥ 5) [OR=12.98, 95% CI, 5.61–30.00, P < 0.001].
Conclusion
The burden of insomnia was significant among the general population in the Kingdom of Bahrain during the Delta wave of the COVID-19 pandemic despite the low severity of this variant. Mental health programs are a high priority during the pandemic and afterward. Detection of insomnia could be used to treat some mental health problems at an early stage.
Keywords: insomnia prevalence, Insomnia Severity Index, anxiety, risk factors, predictors, Bahrain
Introduction
The entire world is experiencing a challenging situation because of the coronavirus disease (COVID-19) pandemic, emerging from Wuhan, China, in December 2019.1 As COVID-19 has rapidly spread worldwide, it has unexpectedly caused deaths and profoundly affected millions of lives. Social isolation, lockdowns, fear of contamination, and the dramatic changes to everyday life, might affect mental health and cause disruption in regular sleep habits and patterns.2
The Delta variant of COVID-19 was the variant of concern classified by the World Health Organization on May 11, 2021.3 In contrast to the previous variant of COVID-19, the Delta variant has higher transmissibility, shorter incubation period, stronger pathogenicity, and was responsible for more cases and deaths worldwide.4 The widespread of COVID-19 Delta variant infections has resulted in increased fear and panic.5 The fear of the new COVID-19 variant, the unclear effectiveness of the vaccines at that time, the variability of restrictions, and the uncertainty about getting back to normal life routine could trigger acute worry that might contribute to mental health problems including insomnia.6 Several studies demonstrated an increasing impact of the second wave of the pandemic on mental health and sleep.7–9
Sleep is essential for well-being and optimal physical and mental health.10 It plays a critical role in brain function and body physiology, including metabolism, appetite regulation, hormones, immune competence, and the cardiovascular system.11,12 Normal healthy sleep is characterized by adequate duration, good quality, proper timing and regularity, and the absence of sleep disturbances and disorders.12 The problems of sleep that affect the quantity and quality of sleep are collectively referred to as sleep disruptions, which contribute to significant short-term health outcomes such as stress, somatic and psychological problems.10 Sleep disruptions may also predispose to long-term consequences, including cardiovascular diseases, obesity, type 2 diabetes, and death.10
Sleep problems during the COVID-19 pandemic are widely prevalent and were evaluated in several studies worldwide.13 The global pooled prevalence rate of sleep problems during COVID-19 was 35.7%.13 Insomnia prevalence was the highest among patients with COVID-19 (74.8%), followed by healthcare workers (HCWs) (36.0%) and the general population (32.3%).13 A study conducted in China revealed that 13.6% of the participants developed new-onset insomnia and 12.5% had worsened insomnia symptoms.14 While in France the prevalence of clinical insomnia was estimated to be 19.1%, reaching the upper worldwide levels.1 Studies conducted in Australia, Greece, and Italy reported rates of 40.7%, 37.6%, and 18.6%, respectively.1,15,16 In a study conducted in the USA, 56% of the participants reported at least some evidence of current insomnia, with 5.2% scoring as severe insomnia.17 A study conducted to assess sleep quality among the Saudi population during the COVID-19 pandemic reported a prevalence of insomnia and poor sleep quality of 54.4% and 55.5%, respectively.18 Poor sleep quality combined with moderate and severe stress was estimated to be 60% among HCWs in Bahrain during the pandemic.19
Numerous intrinsic and extrinsic risk factors (biological, psychological, genetic, and social factors) contribute to sleep deprivation and disruption development11,20 Several studies reported that the general population experienced elevated stress and mental problems during the COVID-19 pandemic.1,21–23 Gender, educational level, risk of acquisition of COVID-19 infection, social or economic impact, isolation status, stress, or medical problems were all risk factors associated with mental health problems including insomnia during the pandemic.18,19,24–26 Females had a significantly increased risk compared to males as reported in several studies.14–18,27 Greater sleep difficulties were found among younger age groups (18–30 years).16,28 Individuals with postgraduate levels reported lower levels of insomnia severity than participants with lower educational levels.1,16 Young adults living with their parents had more severe insomnia, which was explained by some aspects of the home quarantine such as an increase in virtual social life, time with parents at home, and lack of physical social life with peers.28 Healthcare workers facing the COVID-19 pandemic, with several critical patients, deaths, and tremendous workloads, were also at high risk of mental health problems including sleep disturbance and insomnia.19 Studies found that individuals who were infected with COVID-19 appeared to be the most affected group with sleep problems.21 In addition, being pessimistic about the vaccine was a risk factor for insomnia symptoms.22
Alterations in arousal states are associated with multiple neuropsychiatric disorders, including generalized anxiety disorders.29 Previous studies have identified insomnia as a predisposing factor for various mental disorders including anxiety.30–32 Anxiety and insomnia are strongly associated; however, the understanding of their relationships remains limited.30,33 A population based, longitudinal study conducted in UK revealed that insomnia was associated with preexisting anxiety, depression, and pain at baseline, and it is a risk factor for the subsequent onset of anxiety and other problems.32 Similarly, a meta-analysis reported that insomnia increases the risk for psychopathology and predisposes to anxiety.30
Despite the wealth of research related to insomnia that affected the global population during the COVID-19 pandemic, few studies were conducted in the Arab countries during the Delta wave of this crisis to evaluate insomnia in the general population. Evaluating insomnia during the Delta wave is essential since the degree of uncertainty and population vaccinated might vary. To the best of our knowledge, this is the first study to capture the prevalence of insomnia and its related risk factors among the general population of the Kingdom of Bahrain during the Delta wave of the COVID-19 pandemic.
Materials and Methods
Study Design
This analytical cross-sectional study was conducted between June and August 2021.
Target Population and Sample Size
The target population was Bahraini nationals living in the Kingdom of Bahrain during the period February 2020-August 2021. The sample size was calculated based on the prevalence of insomnia among general populations during the COVID-19 pandemic, where Z= 1.96, P= expected prevalence (expressed as a decimal point) = 0.10, E= margin of error = 0.02. The total estimated sample size was 864. Any Bahraini who is 18 years or older, can read and have access to the online survey were eligible to participate. Bahraini participants who were living abroad were excluded from the study.
Study Tool and Sampling Method
An anonymous online questionnaire was distributed using the snowball-sampling technique. The questionnaire was available in Arabic and could be accessed via an online platform (Google forms). Information about the study and eligibility criteria including consent were introduced in the form. All respondents provided informed consent by agreeing to the electronic survey before answering the questionnaire. At the end of the study survey, 646 (74.8% of the calculated sample size) submitted fully completed study questionnaires.
The questionnaire is composed of five sections as independent variables (sociodemographic information, mental and physical health conditions, COVID-19-related stressful life events, COVID-19 vaccine uptake and intent, and Anxiety level using the generalized anxiety disorder scale (GAD-7)). The GAD-7 is composed of seven questions and each question can be answered by one of four responses, which are summed to obtain a total score ranging from 0 to 21. A score of 0–4 indicates minimal anxiety, 5–9 indicates mild anxiety, 10–14 indicates moderate anxiety and 15–21 indicates severe anxiety.34,35 Insomnia, the outcome variable, was measured by the Insomnia Severity Index (ISI). It is a self-reported questionnaire composed of seven questions, (1) “perceived severity of difficulties initiating sleep”, (2) “difficulties staying asleep”, (3) ‘early morning awakenings’, (4) “satisfaction with current sleep pattern”, (5) ‘interference with daily functioning, (6) “noticeability of impairment attributed to the sleep problem” and (7) “degree of distress or concern caused by the sleep problem”. Each question can be answered by one of five responses, which are summed to obtain a total score ranging from 0 to 28. A score of 0–7 indicates no clinically significant insomnia, 8–14 indicates subclinical insomnia, 15–21 indicates clinical insomnia of moderate severity and 22–28 indicates severe clinical insomnia.36 The ISI (including the Arabic version) revealed adequate internal reliability (Cronbach’s alpha scores of >0.7),37,38 even when administered online.39
Statistical Analyses
Categorical variables were presented as frequencies and percentages, and continuous variables were presented as mean and standard deviation. The sample was categorized into 3 groups according to the outcome variable (reported insomnia using ISI): no clinical insomnia, subclinical insomnia, and clinical insomnia. Regression analysis was performed to test the correlation between continuous variables. χ2 test permitted to test the association between independent variables considered as predictors and insomnia as an outcome. A Logistic regression model estimated the adjusted odds ratios and 95% confidence limits considering clinical insomnia as the outcome categorized in two levels (Clinical versus subclinical and normal). Relationship between insomnia and anxiety, considering respective continuous scales, was tested by Pearson correlation coefficient. A p-value of less than 0.05 was considered statistically significant.
The data was entered into Excel and then exported to Statistical Package for the Social Sciences (SPSS) software version 28 for analysis.
Ethical Considerations
The study was conducted following the Declaration of Helsinki, and the protocol was approved by the Research and Ethics Committee of the College of Medicine and Medical Sciences at Arabian Gulf University (approval number: E019-PI-6/21). Participants were provided information about the study and informed that participation is voluntary and refusal to participate would not affect them in any way. All respondents provided informed consent in the electronic survey prior started answering the questions. Furthermore, all data collected were kept under confidentiality and anonymity and not used for other purposes.
Results
Sample Characteristics
A total of 646 individuals participated in the study. The majority of the participants were females (86%). The mean age was 38.70 ± 12.658 years (age range 18–89) and around half of the participants were 35 years or older. Around three-quarters of the participants were married (76%), and 65% reported having a diploma or bachelor’s degree as an educational level. More than half of the participants (57.7%) reported living in private houses and the majority (97.1%) reported living during the COVID-19 pandemic with their families. Regarding employment status, 46.0% of participants were employed, 4.6% self-employed, 11.6% were students, 6.8% unemployed, 11.0% homemakers, and 20.0% retired. Among those who were employed, 42.4% were HCWs and 71.7% had combined, morning and evening shifts. More than half of the participants (59.9%) reported a monthly income of ≥ 800 Bahraini Dinars (≥ 2122 USD) and 37.5% reported that their income decreased during the COVID-19 pandemic. The sociodemographic characteristics of the study participants are presented in Table 1.
Table 1.
The Sociodemographic of the Study Participants (N=646)
| Characteristica | n (%) |
|---|---|
| Gender | |
| Male | 90 (13.9) |
| Female | 556 (86.1) |
| Age group | |
| <30 Year | 193 (29.9) |
| 30 - < 35 Year | 75 (11.6) |
| ≥ 35 Year | 377 (58.4) |
| Marital status | |
| Single | 129 (20.0) |
| Married | 491 (76.0) |
| Divorced or widowed | 26 (4.0) |
| Educational | |
| Secondary and below | 104 (16.1) |
| Diploma or bachelor’s | 420 (65.0) |
| Postgraduate | 122 (18.9) |
| Employment status | |
| Employed | 327 (50.6) |
| Unemployed | 44 (6.8) |
| Retired | 129 (20.0) |
| Housewife | 71 (11.0) |
| Student | 75 (11.6) |
| Occupation field | |
| Healthcare | 274 (42.4) |
| Education | 106 (16.4) |
| Others | 266 (41.2) |
| Working time | |
| Morning | 183 (28.3) |
| Morning and evening | 463 (71.7) |
| Incomeb | |
| < 800 BHD | 259 (40.1) |
| ≥ 800 BHD | 387 (59.9) |
| Type of residence | |
| Flat/apartment | 148 (22.9) |
| Private house | 373 (57.7) |
| Shared house | 125 (19.3) |
| Household Status | |
| Live alone | 12 (1.8) |
| Live with family | 627 (97.1) |
| Live with relatives/friends | 7 (1.1) |
Note: aFrequency count and (%).
Abbreviation: bBHD, Bahraini Dinar.
COVID-19 and Health-Related Factors of the Participants
Details about COVID-19 and the health-related factors of the participants are presented in Table 2. More than a third of the participants (38.9%) reported having medical problems and 35.6% were under medications. A proportion of 6.2% reported suffering from mental health problems and 2.9% required medications for these problems. Some participants relied on medications to help them sleep (6.5%).
Table 2.
COVID-19 and Health Profiles of the Study Participants (N=646)
| Variablea | n (%) |
|---|---|
| Chronic medical problems | |
| Yes | 251 (38.9) |
| No | 395 (61.1) |
| On medication for chronic medical problem | |
| Yes | 230 (35.6) |
| No | 416 (64.4) |
| Use medication to help sleep | |
| Yes | 42 (6.5) |
| No | 604 (93.5) |
| Diagnosed with mental health problem (pre-COVID-19 pandemic) | |
| Yes | 40 (6.2) |
| No | 627 (93.8) |
| On medication(s) for mental health problem | |
| Yes | 19 (2.9) |
| No | 627 (97.1) |
| Anxiety | |
| No symptoms or minimal (GAD-7 score less than 5)b | 206 (31.9) |
| Anxiety symptoms (GAD-7 score ≥ 5) | 440 (68.1) |
| Workplace exposure to COVID-19 | |
| Yes | 164 (25.4) |
| No | 482 (74.6) |
| Diagnosed with COVID-19 infection | |
| Yes | 162 (25.1) |
| No | 484 (74.9) |
| Self-isolation/quarantine | |
| Yes | 381 (59.0) |
| No | 265 (41.0) |
| COVID-19 related death experience among relatives and friends | |
| Yes | 372 (57.6) |
| No | 274 (42.4) |
| Vaccinated against COVID-19 | |
| Yes | 559 (86.5) |
| No, but planning to be vaccinated | 48 (7.5) |
| No, not planning to be vaccinated | 39 (6.0) |
Note: aFrequency count and (%).
Abbreviation: bGAD-7, general anxiety disorder scale.
Around a quarter of the participants (25.4%) worked since February 2020, at the start of COVID-19 precautionary measures for the pandemic, in places at high risk of being in contact with COVID-19 cases. Around a quarter (25.1%) were diagnosed with COVID-19 and 59% have been in self-isolation/quarantine during the COVID-19 pandemic. More than half (57.6%) of the participants had family members or close friends or colleagues who died from COVID-19 complications. The majority of the responders were vaccinated against COVID-19 (86.5%).
Prevalence of Insomnia
According to the Insomnia Severity Index (ISI), 20% of participants reported clinical insomnia (19.8% symptoms of moderate insomnia, and 0.2% symptoms of severe insomnia), 50.1% reported subclinical insomnia and 29.9% of the participants had an absence of insomnia. The mean Insomnia score for the study participants was 10.33 (SD± 4.42).
Factors Associated with Insomnia
Clinical insomnia prevalence was significantly higher among female participants compared to males (21.1% Vs 12.2%, p=0.050). This prevalence was also significantly higher among participants with a secondary educational level or below, working in healthcare and with a monthly income of < 800 BHD (< 2122 USD) compared to their counterparts (all p-values < 0.01). There were significant differences in insomnia prevalence concerning to changes in monthly income during the COVID-19 pandemic (p < 0.01). The rate of clinical insomnia was significantly higher among participants who reported anxiety symptoms (GAD-7 score ≥ 5) compared to participants who reported absence or only minimal anxiety symptoms (GAD-7 score less than 5) (28.0% compared to 2.9%, p < 0.001). This finding is confirmed using regression analysis which revealed a significant correlation between insomnia and anxiety (R = 0.59, R2 = 0.347, p = 0.01) (Figure 1). Participants using medications to help them sleep reported more clinical insomnia compared to their counterparts (40.5% vs 18.6%, p < 0.001). Table 3 shows the associations between sociodemographic factors and the severity of insomnia. Levels of insomnia were also significantly associated with workplace exposure to COVID-19 (p< 0.05).
Figure 1.
Correlation between anxiety and insomnia scores considering the continuous scales (ISI and GAD-7) for both measurements. The X axis represents the GAD-7 scale values and the Y axis is ISI values. R2 is the correlation coefficient.
Table 3.
The Association Between Levels of Insomnia and Sociodemographic Variables
| Variablesa | Levels of Insomnia | P. Valueb | ||
|---|---|---|---|---|
| Normal n (%) | Subclinical n (%) | Clinical n (%) | ||
| Gender | ||||
| Male | 35 (38.9) | 44 (48.9) | 11 (12.2) | 0.050 |
| Female | 158 (28.5) | 279 (50.3) | 118 (21.2) | |
| Age group | ||||
| 30 Year | 52 (26.9) | 100(51.8) | 41 (21.3) | 0.218 |
| 30 - < 35 Year | 16 (21.3) | 40 (53.3) | 19 (25.4) | |
| ≥ 35 Year | 124 (32.9) | 183(48.7) | 69 (18.4) | |
| Marital status | ||||
| Single | 26 (20.2) | 75 (58.1) | 28 (21.7) | 0.097 |
| Married | 158 (32.2) | 237 (48.4) | 95 (19.4) | |
| Divorced and widowed | 9 (34.6) | 11 (42.3) | 6 (23.1) | |
| Educational | ||||
| Secondary and below | 27 (26.2) | 49 (47.6) | 27 (26.2) | < 0.01 |
| Diploma or bachelor’s | 113 (26.9) | 224 (53.3) | 83 (19.8) | |
| Postgraduate | 53 (43.4) | 50 (41.0) | 19 (15.6) | |
| Employment status | ||||
| Employed | 95 (31.9) | 135 (45.5) | 67 (22.6) | 0.306 |
| Self-Employed | 7 (23.3) | 16 (53.3) | 7 (23.4) | |
| Unemployed | 12 (27.3) | 27 (61.4) | 5 (11.3) | |
| Others | 79 (28.9) | 145 (52.9) | 50 (18.2) | |
| Occupation field | ||||
| Healthcare | 93 (33.9) | 117 (42.7) | 64 (23.4) | < 0.01 |
| Education | 37 (34.9) | 53 (50.0) | 16 (15.1) | |
| Others | 63 (23.8) | 153 (57.7) | 49 (18.5) | |
| Incomec | ||||
| < 800 BHD | 58 (22.5) | 143 (55.4) | 57 (22.1) | < 0.01 |
| ≥ 800 BHD | 135 (34.9) | 180 (46.5) | 72 (18.6) | |
| Income affected during COVID-19 | ||||
| Decreased | 52 (21.6) | 141 (58.5) | 48 (19.9) | < 0.01 |
| No change | 122 (34.8) | 155 (44.1) | 74 (21.1) | |
| Increased | 19 (35.8) | 27 (51.0) | 7 (13.2) | |
| Type of residence | ||||
| Flat/apartment | 38 (25.7) | 76 (51.4) | 34 (22.9) | 0.057 |
| Private house | 122 (32.8) | 189 (50.8) | 61 (16.4) | |
| Shared house | 33 (26.4) | 58 (46.4) | 34 (27.2) | |
Notes: aFrequency count and (%). bPearsons Chi square test, significant at p<0.05.
Abbreviation: cBHD, Bahraini Dinar.
Surprisingly, clinical insomnia was not significantly associated with COVID-19 history of infection, isolation, having a related death among relatives, or the vaccination status and acceptance (Table 4).
Table 4.
The Association Between Levels of Insomnia with COVID-19 and Health-Related Factors
| Variablesa | Levels of Insomnia | P. Valueb | ||
|---|---|---|---|---|
| Normal n (%) | Subclinical n (%) | Clinical n (%) | ||
| Medical health problems | ||||
| Yes | 71 (28.4) | 128 (51.2) | 51 (20.4) | 0.798 |
| No | 122 (30.9) | 195 (49.4) | 78 (19.7) | |
| On medication(s) for medical health problem(s) | ||||
| Yes | 62 (27.1) | 125 (54.6) | 42 (18.3) | 0.235 |
| No | 131 (31.5) | 198 (47.6) | 87 (20.9) | |
| Diagnosed with mental health problem (pre-COVID-19 pandemic) | ||||
| Yes | 11 (27.5) | 18 (45.0) | 11 (27.5) | 0.472 |
| No | 182 (30.1) | 305 (50.4) | 118 (19.5) | |
| On medication for mental health problem | ||||
| Yes | 6 (31.6) | 9 (47.4) | 4 (21.1) | 0.972 |
| No | 182 (30.1) | 305 (50.4) | 118 (19.5) | |
| Anxiety | ||||
| No symptoms or minimal (GAD-7 score less than 5)c | 116 (56.3) | 84 (40.8) | 6 (2.9) | < 0.001 |
| Anxiety symptoms (GAD-7 score ≥ 5) | 77 (17.5) | 239 (54.5) | 123 (28.0) | |
| Workplace exposure to COVID-19 | ||||
| Yes | 62 (37.8) | 67 (40.9) | 35 (21.3) | 0.014 |
| No | 131 (27.2) | 256 (53.3) | 94 (19.5) | |
| Diagnosed with COVID-19 infection | ||||
| Yes | 48 (29.6) | 78 (48.1) | 36 (22.2) | 0.704 |
| No | 145 (30.0) | 245 (50.7) | 93 (19.3) | |
| Self-isolation/quarantine | ||||
| Yes | 110 (28.9) | 190 (49.8) | 81 (21.3) | 0.580 |
| No | 83 (31.4) | 133 (50.4) | 48 (18.2) | |
| COVID-19 related death experience among relatives and friends | ||||
| Yes | 99 (26.6) | 198 (53.2) | 75 (20.2) | 0.083 |
| No | 94 (34.4) | 125 (45.8) | 54 (19.8) | |
| Vaccinated against COVID-19 | ||||
| Yes | 172 (30.8) | 276 (49.5) | 110 (19.7) | 0.338 |
| No, but planning to be vaccinated | 8 (16.7) | 28 (58.3) | 12 (25.0) | |
| No, not planning to be vaccinated | 13 (33.3) | 19 (48.7) | 7 (17.9) | |
Notes: aFrequency count and (%). bPearson Chi square test, significant at p<0.05.
Abbreviation: cGAD-7, general anxiety disorder scale.
The results of multivariate analysis using binary logistic regression identified the independent factors that predicted insomnia status (categorized in two levels: clinical versus sub-clinical and normal). It showed that females are at higher risk for clinical insomnia compared to males (OR= 1.939, 95CI% = 1.00–3.762, p < 0.05). According to the level of anxiety, the results showed that the participants who have anxiety symptoms (GAD-7 score ≤5) are more likely to have clinical insomnia compared to the participants who have no or only minimal anxiety (GAD-7 score <5) [OR= 12.975, 95CI% = 5.611–30.005, p < 0.001]. The other socio-economic, co-morbidities, and COVID-19-related experiences were not significantly associated with this outcome.
Discussion
This study aimed at evaluating insomnia prevalence and its association with potential risk factors among the general population of the Kingdom of Bahrain during the Omicron variant wave of the COVID-19 pandemic. The majority of participants in this study were female, and this is consistent with other studies using online questionnaires.21,25,28 Clinical Insomnia prevalence was 20.0%, which is in the range reported in previous studies conducted during the COVID-19 pandemic.13,21 For example, an international, multi-center study that included 22,330 adults (18 years or older) from the general population in 13 countries and four continents in which sleep problems were evaluated by Insomnia Severity Index (ISI), 17.4% (ISI ≥15) of respondents were identified with probable insomnia disorder while 36.7% of respondents (ISI ≥10) had insomnia symptoms.21 Similarly, the insomnia proportion was 19.1% and 18.6% during the COVID-19 pandemic among the French and Italian adult general population, respectively.1,28
In contrast, some countries had a higher proportion of sleep problems compared to our study. A meta-analysis and systemic review that was conducted to assess sleep problems during the COVID-19 pandemic and included 44 studies from 13 countries revealed sleep problems prevalence rate of 35.7% across studies conducted in the general population, although no standard criteria were used across studies to define sleep problems.13 In addition, sleep problems were identified in 37.6% of the Greek population during the COVID-19 pandemic using Athens Insomnia Scale.16 While in the Gulf Cooperation Countries region, the proportion of insomnia was 54.4% using the Pittsburgh Sleep quality index.18 The discrepancy with our results is most likely explained by the use of different tools to measure insomnia.
Studies have reported a persistent impact of the pandemic on mental health and sleep across the different waves of the pandemic.8,9,22 In alignment with this study’s findings, a study conducted in Georgia revealed that the prevalence of insomnia disorder among the general population during the second wave of the pandemic was 24.2%.8 While a study conducted in Italy revealed that sleep quality returned to the baseline level after the first lockdown and then worsened again during the second lockdown period.9 Other studies found a persistent similar impact on mental health during the first and second waves of the pandemic.22,40 Many factors were proposed to contribute to the variation of mental health outcomes across the different waves of the pandemic which include the degree of restriction measures and lockdown, social isolation, availability of the vaccine, and degree of uncertainty.7–9,22,40 Our data supported by the findings of the literature indicate the persistent negative impact of the pandemic on sleep and mental well-being over time.
Although comparisons of insomnia proportions in various studies conducted in different countries are challenging given the obvious differences in method, diagnostic/screening scales used, cut-off points to define insomnia and sleep problems, the timing of the study (conducted in different phases of the pandemic) and sample representativeness, findings in this study indicate the importance of clinical insomnia during the period of COVID-19 pandemic in the Kingdom of Bahrain, even during the least severe variant wave.
To the best of our knowledge, no studies were conducted before or during the pandemic in the Kingdom of Bahrain, as an Arab country, to evaluate sleep problems in general and insomnia in particular among the general population. However, the proportions reported in a multicenter international study revealed that rates of insomnia symptoms and disorder were about twice as high during the first wave of the pandemic as prevalence rates typically reported in non-pandemic times.41,42
Consistent with the literature, the insomnia proportion found in this study was higher among females18,43,44 and among lower educational levels individuals.1,44 Financial security appears to be associated with insomnia during the COVID-19 pandemic in this study. The proportion of insomnia was higher among participants who had low monthly incomes and those who reported that their monthly income decreased during the period of the pandemic. Studies showed that the economic impact caused by the COVID-19 pandemic was a major factor causing psychological morbidities including insomnia in individuals who are directly or indirectly affected by the situation.45,46
The proportion of insomnia in the current study was significantly higher among participants who work in the healthcare field compared to workers in other fields. The proportion of insomnia among health care workers who participated in this s Healthcare workers have been facing the COVID-19 pandemic, with several critical patients, deaths, and tremendous workloads.47 Working in places that require providing services to suspected or confirmed cases of COVID-19 could act as a triggering factor or initiator of a hyperarousal state, which could lead to a higher incidence of insomnia and other sleep problems, compared with the general population.48 In addition, shift work was associated with a greater risk of sleep problems.27,48 A study conducted to assess sleep disorders among a sample of predominantly US frontline HCWs during the COVID-19 pandemic revealed that 95.5% of participants reported poor sleep and 30% reported moderate or severe insomnia.49 Poor sleep quality combined with moderate-to-severe stress were reported among 60% of both front-line HCWs and non-frontline HCWs in a study conducted in the first wave of the pandemic in the Kingdom of Bahrain.19 Front-line HCWs who dealt with suspected or confirmed cases of COVID-19 had poor sleep quality compared to those who did not deal with patients directly or do not work on the front line.19,50 Mental health problems experienced by HCWs decrease productivity and affect the quality of care provided.51,52
In contrast to other studies’ findings,1,16,21 clinical insomnia in this study was not significantly associated with COVID-19 history of infection, isolation, having a related death among relatives, or the vaccination status and acceptance. This could be due to the adaptation of people after 15 months of experience with the pandemic and alleviation of the precautionary measures as well as less severe outcomes of the Omicron variant.
This study revealed an association between insomnia and anxiety. Insomnia is a frequent symptom of several mental disorders.31,33,53 Anxiety and insomnia are closely linked, yet the understanding of their prospective relationships remains limited.30,33 A meta-analysis revealed that insomnia at baseline increased the odds of anxiety at follow-up.30 Studies proposed that specific interactions of genetic and environmental risk factors might contribute to a brain arousal profile, which is associated with an increased risk for mental disorders.29,54 This could hypothesize that early detection and intervention against insomnia may reduce the risk of developing other mental disorders. It might also demonstrate the importance of screening psychiatric disorders, including depression and anxiety, using insomnia as an early warning clinical indicator.30
Anxiety and, to a lesser extent, the female gender appear to be the predictors of insomnia in our context. Evaluating sleep problems in the Kingdom of Bahrain in different stages of the pandemic and post-pandemic is essential for proper follow-up and interventions.
Despite the importance of the findings and the originality of this study, it suffers from several limitations. The most obvious is the lack of representativeness of males, a bias frequently encountered in online surveys where male proportions are around 20–30% in most studies.1,16,21,25,28 A higher proportion of HCWs in our sample, could lead to an overestimation of the estimated insomnia proportion as this group is at higher risk. In addition, some important mental and medical conditions that could be linked directly to insomnia such as depression, obstructive sleep apnea, and restless leg syndrome were not investigated in this study. The main reason was the concern of a classification bias of these problems due to the self-reported online survey. We highly recommend evaluating insomnia considering these variables in future studies using the best study methodology that will enable collecting such information. To a lesser extent, a selection bias due to limited access to internet tools and skills might have occurred in this study. A recall bias regarding exposure factors might cause a classification bias that could impact the value of estimated risk factors even though some factors are significant and difficult to ignore in this context such as COVID-19 health-related events. All these limitations justify a future study using, a representative sample, and a face-to-face data collection approach. Further studies in the primary care setting might be indicated to evaluate the impact of early detection of insomnia on psychological health and well-being.
Conclusion
Despite the absence of baseline information, the present study suggested a significant burden of insomnia among the general population in the Kingdom of Bahrain during the Omicron wave of the COVID-19 pandemic. Female gender and anxiety appear to be predictors of this condition in our context. Insomnia could be a good indicator of the early detection of mental health problems, particularly in primary healthcare setting.
Acknowledgments
We would like to thank the study participants for their valuable contributions to this study.
Abbreviations
ISI, Insomnia Severity Index; GAD, General Anxiety Disorders; HCWs, healthcare workers.
Disclosure
The authors report no conflicts of interest in this study.
References
- 1.Kokou-Kpolou CK, Megalakaki O, Laimou D, Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thakur V, Bhola S, Thakur P, et al. Waves and variants of SARS-COV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection. 2021;50(2):309–325. doi: 10.1007/s15010-021-01734-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu J, Liu Y, Xia H, et al. BNT162B2-elicited neutralization of B.1.617 and other SARS-COV-2 variants. Nature. 2021;596(7871):273–275. doi: 10.1038/s41586-021-03693-y [DOI] [PubMed] [Google Scholar]
- 5.Bal A, Destras G, Gaymard A, et al. Two-step strategy for the identification of SARS-COV-2 variant of concern 202012/01 and other variants with Spike deletion H69–V70, France, August to December 2020. Eurosurveillance. 2021;26(3). doi: 10.2807/1560-7917.es.2021.26.3.2100008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feder KA, Pearlowitz M, Goode A, et al. Linked clusters of SARS-COV-2 variant B.1.351 — maryland, January–February 2021. MMWRss. 2021;70(17):627–631. doi: 10.15585/mmwr.mm7017a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Quervain D, Aerni A, Amini E, et al. The Swiss Corona Stress Study: November 2021. OSF Preprints; 2021. [Google Scholar]
- 8.Basishvili T, Oniani N, Sakhelashvili I, et al. Insomnia, pre-sleep arousal, psychosocial factors and changes in sleep pattern during the second wave lockdown of the COVID-19 pandemic in Georgia. Brain Sci. 2021;12(1):17. doi: 10.3390/brainsci12010017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conte F, Cellini N, De Rosa O, et al. Dissociated profiles of sleep timing and sleep quality changes across the first and second wave of the COVID-19 pandemic. J Psychiatr Res. 2021;143:222–229. doi: 10.1016/j.jpsychires.2021.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medic G, Wille M, Hemels ME. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151. doi: 10.2147/nss.s134864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colten HR, Altevogt BM. Institute of medicine committee on sleep medicine and research. Sleep Disord Sleep Dep. 2006;47–54. doi: 10.17226/11617 [DOI] [Google Scholar]
- 12.Watson NF, Badr MS, Belenky G, et al.; Consensus Conference Panel. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. J Clinl Sleep Med. 2015;11(6):591–592. doi: 10.5664/jcsm.4950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clinl Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Y, Qin Q, Sun Q, Sanford LD, Vgontzas AN, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clinl Sleep Med. 2020;16(8):1417–1418. doi: 10.5664/jcsm.8524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Killgore WD, Cloonan SA, Taylor EC, Fernandez F, Grandner MA, Dailey NS. Suicidal ideation during the COVID-19 pandemic: the role of insomnia. Psychiatry Res. 2020;290:113134. doi: 10.1016/j.psychres.2020.113134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alharbi AS, Alshahrani SM, Alsaadi MM, Al-Jahdali HH, Wali SO, BaHammam AS. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: a cross-sectional study. Saudi Med J. 2021;42(4):384. doi: 10.15537/smj.2021.42.4.20200735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jahrami H, BaHammam AS, AlGahtani H, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25(1):503–511. doi: 10.1007/s11325-020-02135-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark I, Landolt HP. Coffee, caffeine, and sleep: a systematic review of epidemiological studies and randomized controlled trials. Sleep Med Rev. 2017;31:70–78. doi: 10.1016/j.smrv.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 21.Morin CM, Bjorvatn B, Chung F, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. doi: 10.1016/j.sleep.2021.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salfi F, D’Atri A, Tempesta D, Ferrara M. Sleeping under the waves: a longitudinal study across the contagion peaks of the COVID‐19 pandemic in Italy. J Sleep Res. 2021;30(5). doi: 10.1111/jsr.13313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meaklim H, Junge MF, Varma P, Finck WA, Jackson ML. Pre-existing and post-pandemic insomnia symptoms are associated with high levels of stress, anxiety, and depression globally during the COVID-19 pandemic. J Clinl Sleep Med. 2021;17(10):2085–2097. doi: 10.5664/jcsm.9354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang C, Song W, Hu X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatry. 2021;21(1). doi: 10.1186/s12888-021-03108-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krishnan V, Gupta R, Grover S, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62(4):370. doi: 10.4103/psychiatry.indianjpsychiatry_523_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bacaro V, Chiabudini M, Buonanno C, et al. Insomnia in the Italian population during COVID-19 outbreak: a snapshot on one major risk factor for depression and anxiety. Front Psychiatry. 2020;11. doi: 10.3389/fpsyt.2020.579107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Lecea L, Carter ME, Adamantidis A. Shining light on wakefulness and arousal. Biol Psychiatry. 2012;71(12):1046–1052. doi: 10.1016/j.biopsych.2012.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. doi: 10.1016/j.smrv.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 31.Chen P-J, Huang -CL-C, Weng S-F, et al. Relapse insomnia increases greater risk of anxiety and depression: evidence from a population-based 4-year cohort study. Sleep Med. 2017;38:122–129. doi: 10.1016/j.sleep.2017.07.016 [DOI] [PubMed] [Google Scholar]
- 32.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30(3):274–280. doi: 10.1093/sleep/30.3.274 [DOI] [PubMed] [Google Scholar]
- 33.Pigeon WR, Bishop TM, Krueger KM. Insomnia as a precipitating factor in new onset mental illness: a systematic review of recent findings. Curr Psychiatry Rep. 2017;19(8):1–11. doi: 10.1007/s11920-017-0802-x [DOI] [PubMed] [Google Scholar]
- 34.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 35.Swinson RP. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evid Based Med. 2006;11(6):184. doi: 10.1136/ebm.11.6.184 [DOI] [PubMed] [Google Scholar]
- 36.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suleiman KH, Yates BC. Translating the insomnia severity index into Arabic. J Nurs Scholarsh. 2011;43(1):49–53. doi: 10.1111/j.1547-5069.2010.01374.x [DOI] [PubMed] [Google Scholar]
- 38.Morin CM. Insomnia: Psychological Assessment and Management. Guilford press; 1993. [Google Scholar]
- 39.Thorndike FP, Ritterband LM, Saylor DK, Magee JC, Gonder-Frederick LA, Morin CM. Validation of the insomnia severity index as a web-based measure. Behav Sleep Med. 2011;9(4):216–223. doi: 10.1080/15402002.2011.606766 [DOI] [PubMed] [Google Scholar]
- 40.Pieh C, Budimir S, Humer E, Probst T. Comparing mental health during the COVID-19 lockdown and 6 months after the lockdown in Austria: a longitudinal study. Front Psychiatry. 2021;12. doi: 10.3389/fpsyt.2021.625973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morin CM, LeBlanc M, Bélanger L, Ivers H, Mérette C, Savard J. Prevalence of insomnia and its treatment in Canada. Can J Psychiatry. 2011;56(9):540–548. doi: 10.1177/070674371105600905 [DOI] [PubMed] [Google Scholar]
- 42.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 43.Cellini N, Conte F, De Rosa O, et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. doi: 10.1016/j.sleep.2020.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salfi F, Lauriola M, Amicucci G, et al. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol Stress. 2020;13:100259. doi: 10.1016/j.ynstr.2020.100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li X, Lu P, Hu L, Huang T, Lu L. Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int J Environ Res Public Health. 2020;17(15):5627. doi: 10.3390/ijerph17155627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252–264. doi: 10.1016/j.neubiorev.2021.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.San Martin AH, Serrano JP, Cambriles TD, et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020;75:388–394. doi: 10.1016/j.sleep.2020.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stewart NH, Koza A, Dhaon S, Shoushtari C, Martinez M, Arora VM. Sleep disturbances in frontline health care workers during the COVID-19 pandemic: social media survey study. J Med Internet Res. 2021;23(5):e27331. doi: 10.2196/27331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abdulah DM, Musa DH. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med. 2020;2:100017. doi: 10.1016/j.sleepx.2020.100017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555–567. doi: 10.7326/m19-1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim M, Kim T, Lee D, et al. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Ann Occup Environ Med. 2018;30(1):1–8. doi: 10.1186/s40557-018-0244-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baglioni C, Nanovska S, Regen W, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142(9):969. doi: 10.1037/bul0000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gatt JM, Nemeroff CB, Schofield PR, et al. Early life stress combined with serotonin 3A receptor and brain-derived neurotrophic factor valine 66 to methionine genotypes impacts emotional brain and arousal correlates of risk for depression. Biol Psychiatry. 2010;68(9):818–824. doi: 10.1016/j.biopsych.2010.06.025 [DOI] [PubMed] [Google Scholar]