Abstract
The protective efficacy of several live, recombinant anthrax vaccines given in a single-dose regimen was assessed with Hartley guinea pigs. These live vaccines were created by transforming ΔANR and ΔSterne, two nonencapsulated, nontoxinogenic strains of Bacillus anthracis, with four different recombinant plasmids that express the anthrax protective antigen (PA) protein to various degrees. This enabled us to assess the effect of the chromosomal background of the strain, as well as the amount of PA produced, on protective efficacy. There were no significant strain-related effects on PA production in vitro, plasmid stability in vivo, survival of the immunizing strain in the host, or protective efficacy of the immunizing infection. The protective efficacy of the live, recombinant anthrax vaccine strains correlated with the anti-PA antibody titers they elicited in vivo and the level of PA they produced in vitro.
A major factor in the virulence of Bacillus anthracis is its secretion of two binary toxins, lethal toxin and edema toxin (35, 46). These two toxins possess a common cell receptor-binding (B) component but have distinct biochemically active (A) components. Lethal toxin consists of the cell-binding component, protective antigen (PA) (9), plus an A protein, lethal factor (LF) (28). Likewise, edema toxin is comprised of the same B protein, PA, plus a second A protein, edema factor (EF) (28). All three of these toxin proteins are encoded on a naturally occurring, 184-kb plasmid known as pX01 (28, 34, 35, 46). A third virulence factor is the antiphagocytic poly-d-glutamic acid capsule encoded on a separate 90-kb plasmid known as pX02 (13, 48).
PA binds to a cell surface receptor, where it is proteolytically activated (26, 41), creating a site for LF or EF binding. Once assembled, the toxin complex is internalized by receptor-mediated endocytosis (11, 12). PA serves as a carrier to facilitate entry of LF and EF into the host cell cytoplasm (10, 30, 41). Consistent with the central role of PA in anthrax toxin action, vaccination with PA alone can induce protective immunity to anthrax (23).
The anthrax vaccine currently licensed for human use in the United States is composed of a sterile culture supernatant of an attenuated pXO1+, pXO2− B. anthracis strain containing various amounts of PA, as well as lesser quantities of LF and EF, adsorbed to aluminum hydroxide (14, 34a, 37). The undefined nature of the components and the requirement for six immunizations over 18 months followed by annual boosters (3) suggest the need for an improved, alternative vaccine (44).
In an attempt to create an anthrax vaccine that provides high levels of protective efficacy without such a prolonged vaccination schedule, many efforts have focused on creating live, attenuated anthrax vaccines (1, 19, 22, 29, 36, 47) or on combining purified anthrax PA with various adjuvants (23). A live, attenuated anthrax vaccine similar to the pXO1+, pXO2− Sterne veterinary vaccine is used in humans in the former Soviet Union (39) although reactogenicity may be a problem (42). Other efforts have focused on the creation of live, recombinant anthrax vaccines by using B. subtilis, vaccinia virus, or Salmonella typhimurium as a vector to express the cloned PA gene in the vaccinated host (7, 17, 18, 20, 22, 49). However, no attempts have been made to create a recombinant, live anthrax vaccine by using small, high-copy-number plasmids in B. anthracis to obtain enhanced expression of the PA gene.
We report here the construction of three new gram-negative/ gram-positive shuttle vectors that express the B. anthracis PA gene alone in two nontoxinogenic, nonencapsulated anthrax stains. Our objective was to assess these recombinant strains for the ability to serve as live anthrax vaccines and to test the most promising strains as one-shot vaccines in guinea pigs. A derivative of one of these strains may fulfill our goal of replacing the current human anthrax vaccine with a safe, efficacious, and more easily administered vaccine effective in a single dose.
MATERIALS AND METHODS
Bacterial strains.
The bacterial strains and plasmids used in this study are listed in Table 1.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Relevant characteristic(s) | Source (reference[s]) |
|---|---|---|
| B. anthracis | ||
| ΔANR | Nontoxinogenic (pX01−) nonencapsulated (pX02−) | USAMRIIDa |
| ΔSterne-1 | Nontoxinogenic, nonencapsulated | USAMRIID |
| Ames | PA+ LF+ EF+ (pX01+) Cap+ (pX02+) | USDAb |
| E. coli | ||
| HB101 | F−mcrB mrr hsdS20 recA13 λ− | GIBCO BRLc |
| GM2163 | dam-13::Tn9 dcm-6 hsdR2 mcrA mcrB1 | S. Leppla, NIHd |
| Plasmids | ||
| pC194 | CmrrepH | USAMRIID (14) |
| pUB110 | Kanr PmrrepU | USAMRIID (30, 31) |
| pPA102 | pUB110 with PA gene inserted | USAMRIID (19) |
| pBLKSPPA | pBluescript with PA gene inserted | USAMRIID (28) |
| pJB1 | pBLKSPAA fused with pC194 | This study |
| pJB2 | pBLKSPAA fused with pUB110 | This study |
| pJB3 | pBLKSPAA fused with pUB110 in opposite orientation to pJB2 | This study |
USAMRIID, U.S. Army Medical Research Institute of Infectious Diseases.
USDA, U.S. Department of Agriculture, Ames, Iowa.
Grand Island, N.Y.
NIH, National Institutes of Health.
Enzymes.
Restriction endonuclease BstYI was obtained from New England Biolabs Inc. (Beverly, Mass.). All other nucleases, proteases, phosphatases, and ligases were from GIBCO BRL (Grand Island, N.Y.) and were used as recommended by the suppliers.
Experimental animals.
Female Hartley guinea pigs weighing 400 to 450 g at the start of vaccination were obtained from Charles River Laboratories (Wilmington, Mass.). In conducting the research described in this report, we adhered to the Guide for the Care and Use of Laboratory Animals (6) as promulgated by the Institute of Laboratory Animal Resources, National Research Council. Our facilities are fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
DNA extraction and purification.
Plasmid DNA was extracted from Escherichia coli by the boiling method (31); resuspended in 10 mM Tris–1 mM EDTA (pH 8.0) (all chemicals were purchased from Sigma Chemical Co. [St. Louis, Mo.] unless otherwise noted), mixed with 8 volumes of saturated LiCl, and purified with a CirclePrep kit (Bio 101, Inc., La Jolla, Calif.). B. subtilis plasmid DNA was extracted in identical fashion, except that cells were preincubated for 30 min at 37°C with fivefold more lysozyme. B. anthracis plasmid DNA was prepared as previously described (24), except that E buffer and lysis buffer contained 15% (wt/vol) sucrose, samples were rapidly heated to 60°C in a boiling water bath and lysed for 1 h, and lysis was terminated by adding  volume of 2 M Tris (pH 7) containing 3-mg/ml proteinase K followed by 30 min of incubation at 37°C.
volume of 2 M Tris (pH 7) containing 3-mg/ml proteinase K followed by 30 min of incubation at 37°C.
Construction of shuttle vectors expressing anthrax PA.
Plasmids pBLKSPPA in E. coli and pC194 and pUB110 in B. subtilis were prepared as described above. pC194 was digested with BstYI, and pUB110 and pBLKSPPA were digested with BamHI. Plasmid pBLKSPPA was then treated with phosphatase. pBLKSPPA was mixed with pC194 or pUB110, and the vectors were fused by ligation with T4 DNA ligase before transformation into E. coli HB101.
Transformation and selection of E. coli and B. anthracis.
E. coli HB101 and GM2163 were transformed by a 45-s heat shock in calcium-containing medium as previously described (31). E. coli transformants were initially selected on L agar plates containing 5 μg of chloramphenicol (CM)/ml for pC194-based vectors or 12.5 μg of kanamycin (KAN)/ml for pUB110-based vectors with subsequent selection including 100 μg of ampicillin/ml for shuttle vectors. For successful transformation into B. anthracis, plasmids had to be demethylated by passage through GM2163 (38). B. anthracis strains were grown in BYGT medium (1.9% brain heart infusion extract, 0.5% yeast extract, 0.2% glucose, 0.4% glycerol, 0.1 M Tris [pH 8.0]) (all dehydrated culture media were purchased from Difco Laboratories, Detroit, Mich.) to an optical density at 590 nm of 0.2 to 0.4 absorbance units and transformed by electroporation in 0.4-cm cuvettes at 10 kV/cm as previously described (8) with 0.1 μg of CM/ml added during recovery to induce drug resistance gene expression from pC194-based vectors. Anthrax transformants were selected on L agar plates containing 10 μg of CM/ml for pC194-based vectors or 25 μg of KAN/ml for pUB110-based vectors. After each transformation, vector integrity was verified by analytical restriction digestion with ClaI, HindIII-BglI, or EcoRI.
Preparation of B. anthracis culture supernatants.
Five-milliliter aliquots of FA medium (3.3% tryptone, 2% yeast extract [dialyzed overnight against water], 0.2% l-histidine, 0.8% Na2HPO4, 0.4% KH2PO4, 0.74% NaCl) were inoculated with isolated colonies, grown for 16 h at 37°C, and shaken at 120 to 150 rpm in 100-ml bottles. Cultures were chilled on ice and then made up to 0.1 mM phenylmethylsulfonyl fluoride; 1 mM EDTA, and 100 μM o-phenanthroline. The bacteria were sedimented to a pellet for 2 min at 15,000 × g before sterile filtration of the supernatant through 0.2-μm-pore-size cellulose acetate filters (Nalgene, Rochester, N.Y.). Filtrates were then concentrated to 1 ml and washed twice in a Centri-Prep concentrator (Amicon, Beverly, Mass.) with 12 ml of 50 mM HEPES (pH 7.5)–0.1 mM phenylmethylsulfonyl fluoride–5 mM EDTA–100 μM o-phenanthroline before concentration to 0.5 to 0.7 ml. Concentrated samples were rapidly frozen and stored in 50 to 100-μl aliquots at −70°C.
Assay of PA in culture supernatants.
PA was measured in an assay that involved lysis of a macrophage cell line in the presence of 1-μg/ml LF and various amounts of PA, as described previously (40). Culture supernatants were serially diluted, and PA was assayed by comparison with dilutions of highly pure PA protein produced as previously described (28).
Immunoblotting.
Immunoblotting was performed as previously described (43) by using the PhastSystem for electrophoresis and electroblotting (Pharmacia LKB, Piscataway, N.J.), 20 mM Tris–500 mM NaCl (pH 7.5) (TBS)–5% Carnation instant milk as the blocking buffer, and TBS–0.1% Tween 20 (Bio-Rad Laboratories, Richmond, Calif.) as the wash buffer. The primary antibody used was a rabbit polyclonal antiserum against PA, and the secondary antibody was a goat anti-rabbit–horseradish peroxidase conjugate (Bio-Rad Laboratories, Richmond, Calif.). Blots were developed with the ECL system and Hyperfilm (Amersham Inc., Arlington Heights, Ill.).
Assessment of plasmid stability in B. anthracis in vitro.
B. anthracis spores were diluted in ice-cold L broth (1.0% tryptone, 0.5% yeast extract, 1.0% NaCl) and assayed in triplicate on L agar plates containing or lacking 10 μg of CM/ml or 25 μg of KAN/ml. Five-milliliter cultures of a 107-fold dilution of spores were grown overnight at 37°C in L broth lacking antibiotic. The final culture density and plasmid retention were assayed on L agar with and without antibiotics. The percentage of plasmid loss per generation was equal to 100 × {1 −10[log(final % Kanr/initial % Kanr/no. of generations]}.
Preparation and purification of B. anthracis spores.
Single colonies were inoculated into 5 ml of FA medium containing the appropriate antibiotic in a 100-ml bottle and shaken for 5 h at 37°C. One-tenth-milliliter aliquots were spread on L agar plates with antibiotic, and the plates were incubated overnight at 37°C and for 3 days at room temperature. Bacterial lawns were scraped off the plates, washed three times with sterile water, heat shocked for 30 min at 60°C, washed with water, purified on 58% Renografin-76 (Bristol-Myers Squibb, Princeton, N.J.) in water, as previously described (22), and washed once more with water. They were then sedimented to a pellet at 10,000 × g and resuspended finally in 1% phenol in water. Typical yields ranged from 0.5 × 109 to 5.0 × 109 spores per plate, depending on the strain and plasmid.
Persistence of B. anthracis infection and plasmid stability in vivo.
Guinea pigs were inoculated intramuscularly (i.m.) in the upper hind leg with spores as described below. They were killed 1, 3, or 7 days later, and the entire inoculated muscle was removed. Muscles were minced with scissors in ice-cold, sterile phosphate-buffered saline (PBS) with 0.1% gelatin and dispersed with a motorized Teflon tissue grinder in a final volume of 40 to 50 ml. Homogenates were plated immediately on L agar containing or lacking antibiotic to determine plasmid retention in vivo. The values presented represent the mean CFU from three animals at each time point for each recombinant strain.
Vaccination and challenge of guinea pigs.
Hartley guinea pigs in groups of 17 to 20 each received one 0.5-ml dose i.m. of a live vaccine strain containing 109 spores in PBS with 0.1% gelatin or one 0.5-ml dose of PBS-gelatin alone as a control. Six weeks after vaccination, guinea pigs were challenged i.m. in the thigh with 200,000 spores of the virulent B. anthracis Ames strain (100 spores = 1 50% lethal dose [LD50]) which had been prepared and stored as previously described (22). Deaths of animals were recorded for 3 weeks after challenge.
Serological studies.
Two days before challenge, guinea pigs were bled by cardiac puncture. Sera were assayed for antibody to PA by enzyme-linked immunosorbent assay as described previously (18, 29, 49).
Statistical analysis.
Product limit survival estimates involving time to death after challenge were used to compare live vaccines to a PBS control and to each other. The product limit survival estimates were calculated by using the Lifetest procedure of the SAS statistical software package (SAS Institute Inc., Cary, N.C.). The association between protective efficacy and anti-PA antibody response was also determined by the Lifetest procedure.
RESULTS AND DISCUSSION
Construction and stability of shuttle vectors containing the PA of B. anthracis.
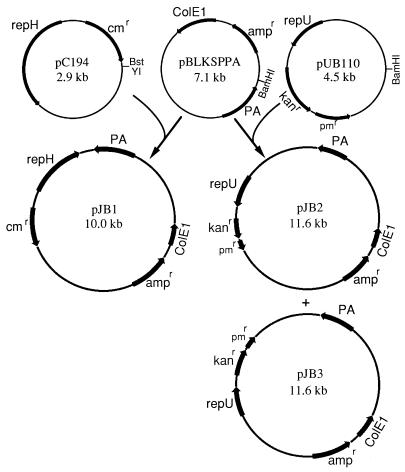
Three new gram-negative/gram-positive shuttle vectors containing the anthrax protective antigen gene were constructed in E. coli and transformed into the ΔANR and ΔSterne stains of B. anthracis (Table 1), both of which lacked pX01 and pX02, as described in Materials and Methods and Fig. 1. In addition to their ability to replicate in E. coli and Bacillus species, all three of these vectors contained six unique cloning sites in the multiple cloning site derived from pBluescript.
FIG. 1.
Construction of shuttle vectors for expression of PA in B. anthracis. Plasmid pBLKSPPA is a pBluescript vector which contains the anthrax PA gene and its endogenous promoter inserted into a multiple cloning site on a ClaI-BamHI fragment. This vector was digested with BamHI, treated with phosphatase, and ligated to gram-positive vectors pUB110 and pC194, which had been digested with BamHI and BstYI, respectively, to create PA-producing shuttle vectors pJB1, pJB2, and pJB3.
Although the replication of these shuttle vectors in B. anthracis was under the control of pC194 or pUB110, both of which were originally isolated from Staphylococcus aureus (15, 32, 33), none of the vectors showed any sign of deletion or rearrangement in B. anthracis (data not presented). Some of the vectors were also well maintained in the absence of antibiotic selection pressure in vitro (Table 2), a feature which is essential to their use in a live vaccine since they must be maintained in the host, where no selection pressure is present.
TABLE 2.
Plasmid stability in the absence of antibiotic selection in vitro
| Strain (plasmid) | % Kanr or Cmr
|
No. of generations | % Plasmid loss/ generation | |
|---|---|---|---|---|
| Initial | Final | |||
| ΔANR(pPA102) | 95.2 ± 1.1a | 113 ± 9.7 | 17.3 ± 0.1 | NLOb |
| ΔSterne(pPA102) | 104.3 ± 4.7 | 92.4 ± 5.2 | 17.8 ± 0.5 | 0.8 ± 0.2 |
| ΔANR(pJB1) | 80.6 ± 4.7 | 50.7 ± 15.6 | 17.3 ± 0.6 | 3.2 ± 1.4 |
| ΔSterne(pJB2) | 91.1 ± 4.3 | 1.7 ± 0.4 | 19.7 ± 0.4 | 18.6 ± 1.1 |
| ΔANR(pJB3) | 96.4 ± 7.8 | 0.7 ± 0.4 | 18.2 ± 0.5 | 25.0 ± 2.5 |
| ΔSterne(pJB3) | 91.9 ± 4.2 | 77.7 ± 8.0 | 18.3 ± 0.3 | 1.2 ± 0.8 |
Results all represent the mean ± the standard error of the mean of three determinations.
NLO, no loss observed in three independent cultures.
Also shown in Table 2 is the stability of plasmid pPA102, pUB110 derivative that contains the PA gene but can only replicate in gram-positive species (Table 1). This vector was also well maintained in the absence of antibiotic selection pressure.
Characterization of PA production by the recombinant anthrax strains.
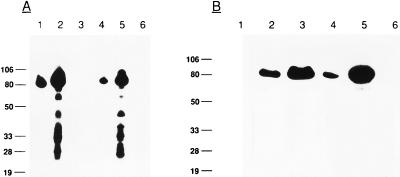
All of the recombinant anthrax strains produced and secreted mature PA of approximately 83 kDa, as determined by reactivity with anti-PA antibodies and comigration with purified PA (Fig. 2B, lane 5). In all strains, at least 80% of the PA was present as the intact 83-kDa species. The additional bands in some samples (Fig. 2A, lanes 2 and 5) were degradation products of PA as determined by reactogenicity with anti-PA antibodies.
FIG. 2.
Immunoblot demonstrating production of PA by recombinant anthrax strains. Sterilely filtered, concentrated culture supernatants were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 10 to 15% gradient gels, electroblotted to nitrocellulose, and probed with anti-PA antibodies. Panel A lanes: 1, ΔANR(pJB1); 2, ΔANR(pPA102); 3, ΔANR control with no plasmid; 4, ΔSterne(pJB1); 5, ΔSterne(pPA102); 6, ΔSterne control with no plasmid. Panel B lanes: 1, ΔANR control with no plasmid; 2, ΔANR(pJB3); 3, ΔSterne(pJB2); 4, ΔSterne(pJB3); 5, purified PA from the Sterne strain; 6, ΔSterne control with no plasmid. The positions of molecular mass standards (sizes are in kilodaltons) are indicated on the left. Approximately equal volumes were applied to all of the lanes.
The amounts of PA produced by the various strains were determined by a macrophage lysis assay, which measures biologically active PA by comparison with known amounts of purified PA (Table 3). Levels of PA production were significantly greater from the pUB110-based plasmids than from the pC194-based plasmids (Table 3). The differences in PA production did not appear to be due to altered growth characteristics of the strains because all strains grew to approximately the same final optical density at 590 nm (data not presented). In some cases, variations in the amount of PA produced may have been due to transcriptional interference. For instance, the adjacent repH and PA genes on pJB1 were transcribed in opposite directions, and pJB2 and pJB3 were identical, except for the orientation of the pUB110 insert (Fig. 1). Transcriptional interference may also explain the reduced stability of pJB2 relative to pJB3 in ΔSterne (Table 2).
TABLE 3.
Levels of PA expression from recombinant anthrax strains
| Strain (plasmid) | Parenta | Amt (μg/ml)b |
|---|---|---|
| ΔANR(pPA102) | pUB110 | 49.2 ± 21.7 |
| ΔSterne(pPA102) | pUB110 | 54.9 ± 16.7 |
| ΔANR(pJB1) | pC194 | 2.74 ± 0.52 |
| ΔSterne(pJB1) | pC194 | 2.34 ± 0.65 |
| ΔSterne(pJB2) | pUB110 | 21.4 ± 3.1 |
| ΔANR(pJB3) | pUB110 | 6.35 ± 0.82 |
| ΔSterne(pJB3) | pUB110 | 7.06 ± 1.17 |
Parent plasmid of the shuttle vector that directs plasmid replication and drug resistance in the B. anthracis host.
Results are the mean ± the standard error of the mean of three or four experiments measuring PA release into the culture supernatant during a 16-h incubation.
The data revealed that the host background had no demonstrable effect on the level of PA production by these plasmids. Plasmids pPA102, pJB1, and pJB3 produced equivalent levels of PA, whether in ΔANR or in ΔSterne (Table 3).
The B. anthracis strains containing pPA102 produced 49 to 55 μg of PA/ml in vitro (Table 3). This was more than the 15 to 20 μg of PA/ml produced with added bicarbonate by the Sterne strain containing native plasmid pX01 (20, 28) but was equivalent to the reported 42 μg/ml produced by B. subtilis containing pPA102 (20). With the native plasmid, toxin production is regulated by a trans activator encoded on the pX01 toxin plasmid and is increased in the presence of bicarbonate (2, 27, 47). However, pX01 was not present in the recombinant anthrax strains (Table 1), and the high levels of PA production reported in Table 3 were measured in the absence of bicarbonate.
These high PA production level may have been due to a copy number effect. While plasmid copy number was not measured, pUB110 is known to be a multicopy plasmid in B. subtilis (5), whereas pX01 is present in only one or two copies per cell of B. anthracis (25). In addition, pPA102 has undergone a spontaneous deletion which may have removed a negative regulatory region upstream of the PA gene (20). Alternatively, the deletion may have allowed readthrough from the adjacent phleomycin resistance (pmr) gene, derived from pUB110, into the PA gene to increase PA transcription (Fig. 1) (20). Further studies are needed to address these possibilities. This deletion has not occurred in pJB2 or pJB3, and the pmr gene is far removed from the PA gene (Fig. 1).
Persistence of the recombinant B. anthracis strains and plasmid stability in vivo.
The recombinant PA-producing strains are highly attenuated. They lack the antiphagocytic poly-d-glutamic acid capsule, the ability to produce functional toxins, and other possible virulence factors encoded on pX01 and pX02 (Table 1). Neither death nor obvious illness occurred when animals received a dose of 109 ΔANR or ΔSterne spores containing the recombinant plasmids (data not presented).
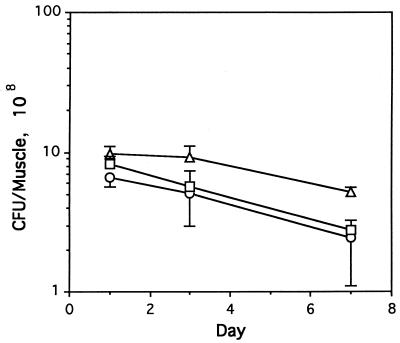
To ascertain if these strains were still capable of prolonged survival in the host, doses of 109 spores of three of the strains were injected i.m. into guinea pigs. The isolated, inoculated muscles were homogenized and cultured 1, 3 and 7 days later. Bacteria from the animals were also tested for retention of antibiotic resistance to determine if the stresses of the host environment induced rapid loss of recombinant plasmids.
As seen in Fig. 3, the vaccinating infection was quite persistent, with 2 × 108 to 5 × 108 bacteria, representing 20 to 50% of the initial inoculum, present in the guinea pig muscle after 7 days. Plasmid retention was also excellent, with no significant loss observed after 1 week in vivo (Table 4). Considering the relatively high instability of pJB2 in vitro (Table 2), the high rate of plasmid retention in vivo suggests that this strain did not proliferate to a great extent in the muscle.
FIG. 3.
Recovery of B. anthracis from guinea pig muscle after inoculation with 109 spores of three recombinant anthrax strains. Bacteria were assayed by dilution and plating 1, 3, and 7 days after inoculation of 109 spores of strains ΔANR(pPA102) (○), ΔSterne(pPA102) (▵), ΔSterne(pJB2) (□). The values shown are mean CFU per milliliter ± the standard deviation of three animals killed at each time point.
TABLE 4.
Plasmid stability in vivoa
| Strain (plasmid) | % Kanr
|
||
|---|---|---|---|
| Day 1 | Day 3 | Day 7 | |
| ΔANR(pPA102) | 108 ± 8b | 113 ± 38 | 70 ± 30 |
| ΔSterne(pPA102) | 96 ± 8 | 98 ± 4 | 107 ± 9 |
| ΔSterne(pJB2) | 98 ± 14 | 95 ± 21 | 127 ± 12 |
B. anthracis strains were inoculated on day 0 and isolated from the leg muscles of three guinea pigs at each time point for each strain and plated in the presence and absence of KAN to determine plasmid retention.
Values represent the mean ± the standard deviation from three animals.
Although the sample size was small, there were no obvious differences in survival of the strains in vivo, suggesting that neither host background nor level of PA production affected persistence (Fig. 3). These results are consistent with observations of Pezard et al., who showed that persistence of Sterne strain-derived mutants in the mouse footpad is unrelated to the production of PA (35).
Protective efficacy of the live, recombinant anthrax vaccines.
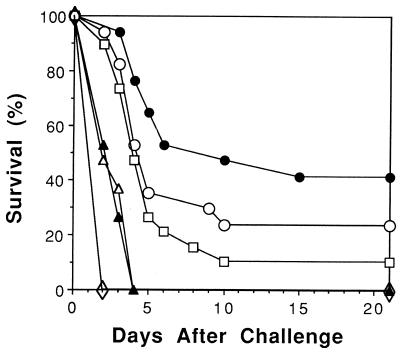
With plasmid stability (Table 2) and PA production (Table 3) as criteria, the five most promising recombinant anthrax strains were selected for use in a live-vaccine trial with the guinea pig, the animal model most frequently used in recent studies to evaluate anthrax vaccines (21). Each guinea pig was vaccinated once with 109 spores of a selected strain and challenged i.m. 6 weeks later with 2,000 LD50 of Ames, a fully virulent anthrax strain.
While only three of the live vaccines partially protected animals from death after this rigorous challenge (Table 5), detailed analysis of survival estimates based on time to death after challenge (Fig. 4) demonstrated that all of the live vaccines provided statistically significant protection relative to the PBS control (Table 5). This analysis also revealed that the best protection was induced by ΔSterne(pPA102) and ΔANR(pPA102) and that there was no statistically significant difference between these two strains. A live anthrax vaccine containing a modified pX01 plasmid that produces only the PA component of anthrax toxin provides mice with similar levels of protection against the attenuated Sterne strain (36). However, fully virulent strains were not tested in the latter study. In two additional experiments, ΔSterne(pPA102) gave 64% (7 survivors; 11 challenged) and 50% (6 survivors; 12 challenged) survival against a challenge dose of 100 LD50 (data not shown).
TABLE 5.
Protective efficacy of a single dose of recombinant B. anthracis against anthrax infection in guinea pigs
| Vaccinationa | No. survived/no. challenged (%)b | Time to death (days)c |
P value vs:
|
Serological responsef | |
|---|---|---|---|---|---|
| PBSd | Next entrye | ||||
| ΔSterne(pPA102) | 7/17 (41) | 9.8 ± 1.3 | 0.0001 | 0.1534 | 2,111 |
| ΔANR(pPA102) | 4/17 (24) | 6.0 ± 0.7 | 0.0001 | 0.3145 | 926 |
| ΔSterne(pJB2) | 2/19 (11) | 5.1 ± 0.6 | 0.0001 | 0.0004 | 192 |
| ΔSterne(pJB3) | 0/19 (0) | 2.8 ± 0.2 | 0.0002 | 0.6673 | 33 |
| ΔANR(pJB3) | 0/19 (0) | 2.8 ± 0.2 | 0.0005 | 0.0005 | 132 |
| PBS | 0/20 (0) | 2.0 ± 0.0 | <10 | ||
Guinea pigs were vaccinated i.m. with a single dose of 109 spores or PBS.
Animals were challenged with 2,000 LD50 of Ames spores i.m. 6 weeks after vaccination.
Harmonic mean time to death ± the standard error of the mean.
P value versus the PBS control of the survival estimate calculated by using the Log Rank test from the Lifetest procedure of the SAS Statistical Software package.
P value versus the subsequent entry in this table [i.e., entry 2, ΔANR(pPA102), versus entry 3, ΔSterne(pJB2)] of the survival estimate calculated by using the Log Rank test from the Lifetest procedure of the SAS Statistical Software package.
Reciprocal geometric mean anti-PA titer of prechallenge sera (determined by enzyme-linked immunosorbent assay).
FIG. 4.
Survival of guinea pigs vaccinated with recombinant, live anthrax vaccines after challenge with 2,000 LD50 of fully virulent B. anthracis. The challenge dose was administered i.m. on day 0. ○, ΔANR(pPA102); •, ΔSterne(pPA102); ▵, ΔANR(pJB3); ▴, ΔSterne(pJB3); □, ΔSterne(pJB2); ◊, saline control. The total numbers of animals challenged were 20 for the saline control, 17 for ΔANR(pPA102) and ΔSterne(pPA102), and 19 for all other groups.
The protection induced by ΔSterne(pPA102) was superior to that induced by ΔSterne(pJB2) (P = 0.0114). ΔSterne(pJB2) provided significantly better protection than ΔSterne(pJB3) (P = 0.0004) (Table 5, P value versus next entry). Likewise, ΔANR(pPA102) protected significantly better than ΔANR(pJB3) (P < 0.0001). Statistical analysis of all of the groups revealed a strong correlation between the anti-PA response induced by the strain (Table 5) and protection measured by either survival (P = 0.0001) or time to death (P = 0.0001). These differences in protective efficacy (Table 5) also correlated strongly with PA production in vitro (Table 3). Thus, the pPA102 strains that produced 49 to 55 μg of PA/ml gave the best protection, the pJB2 strain producing 21 μg of PA/ml gave moderate protection, and the pJB3 strains producing 6 to 7 μg of PA/ml gave minimal protection. Statistical analysis supported the correlation between PA production (Table 3) and both survival (P = 0.0056) and time to death (P = 0.0285). The strains with the higher PA production in vitro (Table 3) also generated the higher anti-PA titers (Table 5) (P = 0.0146). This suggests that PA production in vitro is proportional to production in vivo.
The importance of in vivo production of PA was further supported by an experiment comparing the efficacy of live versus irradiated nonviable spores. In this experiment, all guinea pigs given 109 ΔSterne(pPA102) spores produced an anti-PA antibody response. Six of 12 animals challenged with 100 LD50 of a virulent strain survived. In contrast, none of 12 animals inoculated with irradiated spores survived the lethal challenge and none developed an immune response to PA (data not presented).
The correlation of survival with the anti-PA antibody response, as well as with the production of PA, is most clearly seen when comparing the ΔSterne strains containing the three different plasmids. Thus, survival with ΔSterne(pPA102) was significantly greater than that with ΔSterne(pJB2), which was significantly greater than that with ΔSterne(pJB3) (Table 5). PA production in vitro was 55, 21, and 7 μg/ml, respectively, for the three strains (Table 3), while the reciprocal geometric mean anti-PA antibody titers were 2,111, 192, and 33, respectively (Table 5).
In the course of this study, there were no statistically significant differences between the ΔANR and ΔSterne strains with regard to plasmid stability in vivo (Table 4), PA production (Table 3), persistence in the host at the site of inoculation (Fig. 3), and protective efficacy (Fig. 4 and Table 5).
A single dose of either the ΔANR(pPA102) or the ΔSterne(pPA102) live vaccine was about as effective (Table 5) in the guinea pig model as a single dose of the currently licensed nonliving human anthrax vaccine (23). As the primary factors that correlated with live-vaccine protective efficacy were the immune response to PA and PA production, future efforts to enhance the level of PA production may generate a live vaccine which is superior to current vaccines, even when administered at doses lower than those used here.
ACKNOWLEDGMENTS
We gratefully acknowledge the excellent technical assistance of Steve Tobery and Karen Bostian. We also thank Susan Welkos for provision of strain ΔSterne(pPA102), Gene Nelson and Paul Gibbs for statistical analysis, and John Lowe, Tim Hoover, and Robert Marrero for their helpful advice. In addition, we thank Katheryn Kenyon for critical review of the manuscript.
REFERENCES
- 1.Abalakin V A, Buravtseva N P, Cherkasskii B L. The effect of the protective antigen of Bacillus anthracis on the formation of immunity under the action of live anthrax vaccines. Zh Mikrobiol Epidemiol Immunobiol. 1990;5:72–75. [PubMed] [Google Scholar]
- 2.Bartkus J M, Leppla S H. Transcriptional regulation of the protective antigen gene of Bacillus anthracis. Infect Immun. 1989;57:2295–2300. doi: 10.1128/iai.57.8.2295-2300.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brachman P S, Gold H, Plotkin S A, Fekety F R, Werrin M, Ingraham N R. Field evaluation of a human anthrax vaccine. Am J Public Health. 1962;52:632–645. doi: 10.2105/ajph.52.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradley J V. Distribution-free statistical tests. Englewood Cliffs, N.J: Prentice-Hall Inc.; 1968. pp. 195–203. [Google Scholar]
- 5.Bron S, Luxen E, Swart P. Instability of recombinant pUB110 plasmids in Bacillus subtilis: plasmid-encoded stability function and effects of DNA inserts. Plasmid. 1988;19:231–241. doi: 10.1016/0147-619x(88)90041-8. [DOI] [PubMed] [Google Scholar]
- 6.Commission on the Care and Use of Laboratory Animals, Institute of Laboratory Animal Resources, National Research Council. Guide for the care and use of laboratory animals. Bethesda, Md: National Institutes of Health; 1996. [Google Scholar]
- 7.Coulson N M, Fulop M, Titball R W. Bacillus anthracis protective antigen, expressed in Salmonella typhimurium SL3261, affords protection against anthrax spore challenge. Vaccine. 1994;12:1395–1401. doi: 10.1016/0264-410x(94)90148-1. [DOI] [PubMed] [Google Scholar]
- 8.Dunny G M, Lee L N, LeBlanc D J. Improved electroporation and cloning vector system for gram-positive bacteria. Appl Environ Microbiol. 1991;57:1194–1201. doi: 10.1128/aem.57.4.1194-1201.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Escuyer V, Collier R J. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finkelstein A. Channels formed in phospholipid bilayer membranes by diphtheria, tetanus, botulinum and anthrax toxin. J Physiol (Paris) 1990;84:188–190. [PubMed] [Google Scholar]
- 11.Friedlander A M. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J Biol Chem. 1986;261:7123–7126. [PubMed] [Google Scholar]
- 12.Gordon V M, Leppla S H, Hewlett E L. Inhibitors of receptor mediated endocytosis block the entry of Bacillus anthracis adenylate cyclase toxin but not that of Bordetella pertussis adenylate cyclase toxin. Infect Immun. 1988;56:1066–1069. doi: 10.1128/iai.56.5.1066-1069.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green B D, Battisti L, Koehler T M, Thorne C B, Ivins B E. Demonstration of a capsule plasmid in Bacillus anthracis. Infect Immun. 1985;49:291–297. doi: 10.1128/iai.49.2.291-297.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hambleton P, Carman J A, Melling J. Anthrax: the disease in relation to vaccines. Vaccine. 1984;2:125–132. doi: 10.1016/0264-410x(84)90003-3. [DOI] [PubMed] [Google Scholar]
- 15.Horinouchi S, Weisblum B. Nucleotide sequence and functional map of pC194, a plasmid that specifies inducible chloramphenicol resistance. J Bacteriol. 1982;150:815–825. doi: 10.1128/jb.150.2.815-825.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hosmer D W, Lemeshow S. Applied logistic regression. New York, N.Y: John Wiley & Sons Inc.; 1989. [Google Scholar]
- 17.Iacono-Connors L C, Schmaljohn C S, Dalrymple J M. Expression of the Bacillus anthracis protective antigen gene by baculovirus and vaccinia virus recombinants. Infect Immun. 1990;58:366–372. doi: 10.1128/iai.58.2.366-372.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iacono-Connors L C, Welkos S L, Ivins B E, Dalrymple J M. Protection against anthrax with recombinant virus-expressed protective antigen in experimental animals. Infect Immun. 1991;59:1961–1965. doi: 10.1128/iai.59.6.1961-1965.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ivins B E, Ezzell J W, Jr, Jemski J, Hedlund K W, Ristroph J D, Leppla S H. Immunization studies with attenuated strains of Bacillus anthracis. Infect Immun. 1986;52:454–458. doi: 10.1128/iai.52.2.454-458.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ivins B E, Welkos S L. Cloning and expression of the Bacillus anthracis protective antigen gene in Bacillus subtilis. Infect Immun. 1986;54:537–542. doi: 10.1128/iai.54.2.537-542.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ivins B E, Welkos S L. Recent advances in the development of an improved, human anthrax vaccine. Eur J Epidemiol. 1988;4:12–19. doi: 10.1007/BF00152686. [DOI] [PubMed] [Google Scholar]
- 22.Ivins B E, Welkos S L, Knudson G B, Little S F. Immunization against anthrax with aromatic compound-dependent (Aro-) mutants of Bacillus anthracis and with recombinant strains of Bacillus subtilis that produce anthrax protective antigen. Infect Immun. 1990;58:303–308. doi: 10.1128/iai.58.2.303-308.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ivins B E, Welkos S L, Little S F, Crumrine M H, Nelson G O. Immunization against anthrax with Bacillus anthracis protective antigen combined with adjuvants. Infect Immun. 1992;60:662–668. doi: 10.1128/iai.60.2.662-668.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kado C I, Liu S-T. Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol. 1981;145:1365–1373. doi: 10.1128/jb.145.3.1365-1373.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaspar R L, Robertson D L. Purification and physical analysis of Bacillus anthracis plasmids pX01 and pX02. Biochem Biophys Res Commun. 1987;149:362–368. doi: 10.1016/0006-291x(87)90375-5. [DOI] [PubMed] [Google Scholar]
- 26.Klimpel K R, Molloy S S, Thomas G, Leppla S H. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc Natl Acad Sci USA. 1992;89:10277–10281. doi: 10.1073/pnas.89.21.10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koehler T M, Dai Z, Kaufman-Yarbray M. Regulation of the Bacillus anthracis protective antigen gene: CO2 and a trans-acting element activate transcription from one of two promoters. J Bacteriol. 1994;176:586–595. doi: 10.1128/jb.176.3.586-595.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leppla S H. Production and purification of anthrax toxin. Methods Enzymol. 1988;165:103–116. doi: 10.1016/s0076-6879(88)65019-1. [DOI] [PubMed] [Google Scholar]
- 29.Little S F, Knudson G B. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect Immun. 1986;52:509–512. doi: 10.1128/iai.52.2.509-512.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Little S F, Lowe J R. Location of the receptor-binding region of protective antigen from Bacillus anthracis. Biochem Biophys Res Commun. 1991;180:531–537. doi: 10.1016/s0006-291x(05)81097-6. [DOI] [PubMed] [Google Scholar]
- 31.Maniatis T, Fritsch E F, Sambrook J. Molecular cloning: a laboratory manual. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1982. [Google Scholar]
- 32.McKenzie T, Hoshino T, Tanaka T, Sueoka N. The nucleotide sequence of pUB110: some salient features in relation to replication and its regulation. Plasmid. 1986;15:93–103. doi: 10.1016/0147-619x(86)90046-6. [DOI] [PubMed] [Google Scholar]
- 33.McKenzie T, Hoshino T, Tanaka T, Sueoka N. A revision of the nucleotide sequence and functional map of pUB110. Plasmid. 1987;17:83–85. doi: 10.1016/0147-619x(87)90015-1. [DOI] [PubMed] [Google Scholar]
- 34.Mikesell P, Ivins B E, Ristroph J D, Dreier T M. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect Immun. 1983;39:371–376. doi: 10.1128/iai.39.1.371-376.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34a.Novak, J. M., and A. M. Friedlander. Unpublished data.
- 35.Pezard C, Berche P, Mock M. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect Immun. 1991;59:3472–3477. doi: 10.1128/iai.59.10.3472-3477.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pezard C, Weber M, Sirard J-C, Berche P, Mock M. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect Immun. 1995;63:1369–1372. doi: 10.1128/iai.63.4.1369-1372.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Puziss M, Manning L C, Lynch L W, Barclay E, Abelow I, Wright G G. Large-scale production of protective antigen of Bacillus anthracis anaerobic cultures. Appl Microbiol. 1963;11:330–334. doi: 10.1128/am.11.4.330-334.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quinn C P, Singh Y, Klimpel K R, Leppla S H. Functional mapping of anthrax toxin lethal factor by in-frame insertional mutagenesis. J Biol Chem. 1991;266:20124–20130. [PubMed] [Google Scholar]
- 39.Shlyakhov E N, Rubinstein E. Human live anthrax vaccine in the former USSR. Vaccine. 1994;12:727–730. doi: 10.1016/0264-410x(94)90223-2. [DOI] [PubMed] [Google Scholar]
- 40.Singh Y, Leppla S H, Bhatnagar R, Friedlander A M. Internalization and processing of Bacillus anthracis lethal toxin by toxin-sensitive and toxin-resistant cells. J Biol Chem. 1989;264:11099–11102. [PubMed] [Google Scholar]
- 41.Singh Y, Klimpel K R, Quinn C P, Chaudhary V K, Leppla S H. The carboxyl-terminal end of protective antigen is required for receptor binding and anthrax toxin activity. J Biol Chem. 1991;266:15493–15497. [PubMed] [Google Scholar]
- 42.Stepanov A V, Marinin L I, Pomerantsev A P, Staritsin N A. Development of novel vaccines against anthrax in man. J Biotechnol. 1996;44:155–160. doi: 10.1016/0168-1656(95)00092-5. [DOI] [PubMed] [Google Scholar]
- 43.Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci USA. 1979;76:4350–4354. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turnbull P C. Anthrax vaccines: past, present and future. Vaccine. 1986;9:533–539. doi: 10.1016/0264-410x(91)90237-z. [DOI] [PubMed] [Google Scholar]
- 45.Turnbull P C, Broster M G, Carman J A, Manchee R J, Melling J. Development of antibodies to protective antigen and lethal factor components of anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Infect Immun. 1986;52:356–363. doi: 10.1128/iai.52.2.356-363.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Uchida I, Hashimoto K, Terakado N. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J Gen Microbiol. 1986;132:557–559. doi: 10.1099/00221287-132-2-557. [DOI] [PubMed] [Google Scholar]
- 47.Uchida I, Hornung J M, Thorne C B, Klimpel K R, Leppla S H. Cloning and characterization of a gene whose product is a trans-activator of anthrax toxin synthesis. J Bacteriol. 1993;175:5329–5338. doi: 10.1128/jb.175.17.5329-5338.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uchida I, Sekizaki T, Hashimoto K, Terakado N. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J Gen Microbiol. 1985;131:363–367. doi: 10.1099/00221287-131-2-363. [DOI] [PubMed] [Google Scholar]
- 49.Welkos S L, Friedlander A M. Comparative safety and efficacy against Bacillus anthracis of protective antigen and live vaccines in mice. Microb Pathog. 1988;5:127–139. doi: 10.1016/0882-4010(88)90015-0. [DOI] [PubMed] [Google Scholar]
- 50.Welkos S L, Vietri N J, Gibbs P H. Non-toxigenic derivatives of Bacillus anthracis are fully virulent for mice: role of plasmid pX02 and chromosome in strain dependent virulence. Microb Pathog. 1993;14:381–388. doi: 10.1006/mpat.1993.1037. [DOI] [PubMed] [Google Scholar]