Highlights
-
•
After adjusting for age, sex, body size, and exercise time, we found population-level declines in 20-m shuttle run and sit-ups performance among Japanese children and adolescents during the COVID-19 pandemic.
-
•
The magnitude of these declines was 18- and 15-fold larger than improvements seen before the pandemic (2013–2019).
-
•
Declines in other physical fitness measures were smaller during the pandemic.
-
•
Declines in the 20-m shuttle run and sit-ups performance during the pandemic suggest corresponding declines in population health.
-
•
The pandemic provides an opportunity to reimagine physical activity by complementing structured physical activity with informal and unstructured physical activity.
Keywords: Census, Physical inactivity, Public health, Temporal trends, Youth
Abstract
Background
Limited nationally representative evidence is available on temporal trends in physical fitness (PF) for children and adolescents during the coronavirus disease 2019 (COVID-19) pandemic. The primary aim was to examine the temporal trends in PF for Japanese children and adolescents before and during the COVID-19 pandemic. The secondary aim was to estimate the concurrent trends in body size (measured as body mass and height) and movement behaviors (exercise, screen, and sleep time).
Methods
Census PF data for children in Grade 5 (aged 10–11 years) and adolescents in Grade 8 (aged 13–14 years) were obtained for the years 2013–2021 from the National Survey of Physical Fitness, Athletic Performance, and Exercise Habits in Japan (n = 16,647,699). PF and body size were objectively measured, and movement behaviors were self-reported. Using sample-weighted linear regression, temporal trends in mean PF were calculated before the pandemic (2013–2019) and during the pandemic (2019–2021) with adjustments for age, sex, body size, and exercise time.
Results
When adjusted for age, sex, body size, and exercise time, there were significant declines in PF during the pandemic, with the largest declines observed in 20-m shuttle run (standardized (Cohen's) effect size (ES) = −0.109 per annum (p.a.)) and sit-ups performance (ES = −0.133 p.a.). The magnitude of the declines in 20-m shuttle run and sit-ups performances were 18- and 15-fold larger, respectively, than the improvements seen before the pandemic (2013–2019), after adjusting for age, sex, body size, and exercise time. During the pandemic, both body mass and screen time significantly increased, and exercise time decreased.
Conclusion
Declines in 20-m shuttle run and sit-ups performances suggest corresponding declines in population health during the COVID-19 pandemic.
Graphical abstract
1. Introduction
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic.1 To mitigate the spread of COVID-19, the Japanese government declared a state of emergency on April 7, 2020. While Japan did not have mandatory lockdowns, the government encouraged residents to stay at home and reduce social contact by 70% to 80%.2 This caused significant reductions in physical activity (PA) among the Japanese population, particularly during the first state of emergency (April 7 through May 25, 2020).3 In particular, it was expected that the movement behaviors of children (PA, sedentary behavior, and sleep) would be adversely affected by a series of restrictions (e.g., cancelation of sporting events and organized sports participation) after the government declared a temporary closure of schools on March 2, 2020.2 Preliminary evidence indicated that PA levels declined and screen time increased among Japanese school-aged children during the pandemic (2021) as compared to before the pandemic (2019).4,5 Additionally, recent reviews summarizing the international evidence from the first year of COVID-19 found that lockdown restrictions led to reduced PA, increased screen time, and altered sleep patterns, with a shift to later bed and wake times among children and adolescents.6,7
Physical fitness (PF) is an important marker of current and future health.8, 9, 10 Preliminary evidence from small samples of youth suggested that lockdown measures had significant adverse effects on PF among children and adolescents.11, 12, 13, 14, 15, 16, 17, 18, 19 For example, Wahl-Alexander et al.14 reported significant declines in the 20-m shuttle run (–26.7%), sit-ups (–19.4%), and push-ups (–35.6%) performance of 264 children in the United States (mean age = 9.6 years) during lockdown. Similarly, Chambonnière et al.15 found a significant lockdown-related decline in the 20-m shuttle run, standing long jump, medicine ball throw, and motor skill performance of 206 French primary school children (mean age = 9.9 years). These findings, while important, are not generalizable to their respective country populations because of their small samples, which were identified using non-probability sampling procedures. To date, only a single study has used nationally representative data to identify declining PF levels. A Slovenian study found that after only 2 months of lockdown, PF had declined in 6- to 15-year-old Slovenian children by 13%; these were the lowest PF levels seen in 30 years of national monitoring.18 Unfortunately, the effect of lockdown restrictions on Slovenian children was only reported for a composite PF measure (comprising 8 distinct PF measures) rather than for individual components. Additionally, no study to date has examined the temporal trends in PF before and during the COVID-19 pandemic while adjusting for important covariates, such as age, sex, and PA. Furthermore, the effects of COVID-19-related restrictions on PF have only been reported for European11,12,15, 16, 17, 18, 19 and American children;13,14 no study has examined these effects in Asian children and adolescents.
Temporal trends in the PF levels of children and youth may help understand the impact of existing population-based intervention strategies, the impact of social change (e.g., the COVID-19 pandemic), and provides insight into current and future population health. This is particularly important since PF among children and adolescents tracks moderately well into adulthood and is associated with current and future health.8, 9, 10 In 2008, Japan launched its National Survey of Physical Fitness, Athletic Performance, and Exercise Habits (hereafter called the JP Fit Survey for Youth). While this survey is limited to students in Grades 5 and 8, nearly all students have completed PF testing annually (i.e., approximately 2 million per annum (p.a.)) with an average response rate between 2013 and 2021 of 97% at the school level.20 Therefore, unlike most studies using probability sampling, the JP Fit Survey for Youth recruited all students across Japan and so provided a complete annual picture of the PF levels among Japanese children and adolescents.20 Additionally, the JP Fit Survey for Youth includes 8 PF tests and provides detailed data on PF levels before and during the pandemic according to these individual components. The aim of this study, therefore, was to use the JP Fit Survey for Youth data to examine temporal trends in PF levels (adjusted for age, sex, body size, and exercise time) for Japanese children and adolescents before and during the COVID-19 pandemic. The secondary aim was to estimate concurrent trends in body size (height and body mass) and movement behaviors (exercise, screen, and sleep time).
2. Materials and methods
2.1. Description of the Japanese PF survey
The JP Fit Survey for Youth is a census survey, administered annually between May and July to approximately 2 million Japanese children (Grade 5; age = 10–11 years) and adolescents (Grade 8, age = 13–14 years). A detailed description of the survey has been published previously.20 Although data collection for the JP Fit Survey for Youth began in 2008, this study used data from 2013 onwards due to inconsistency in the sampling strategy during the 2008–2012 period.20 Additionally, the 2020 PF survey was canceled due to the COVID-19 pandemic. In total, PF data from 16,647,699 participants (Grade 5: 8,490,558 children (49% girls); Grade 8: 8,157,141 adolescents (49% girls)) were available between 2013 and 2021.20
The survey includes objectively measured PF, height, and body mass, plus self-reported movement behaviors (exercise, screen, and sleep time). In schools, PF was commonly measured by classroom or physical education teachers using standardized protocols21,22 for the following 8 tests: handgrip strength, sit-ups, sit-and-reach, side-step, 20-m shuttle run, 50-m sprint, standing long jump, and ball throw (softball for Grade 5 students and handball for Grade 8 students). Body mass was measured to the nearest 0.1 kg using a digital weighing scale, and standing height was measured to the nearest 0.1 cm using a stadiometer. All students were invited to participate in the PF tests, but some did not participate for the following reasons: (a) those who were prohibited or restricted from exercising by a medical doctor, and (b) those who were unwell (e.g., fever or undue fatigue) on the day of PF testing.
Questionnaires were also administered in school by classroom or physical education teachers. Self-reported exercise time was quantified using the following question: “Usually, how long do you play sports or exercise outside of physical education classes?” Participants quantified time spent participating in exercise for all days of the week (Monday through Sunday), and average daily exercise time was calculated by dividing total time by 7. Recreational screen time was quantified using the following question: “On school days, how long do you spend watching television, playing video games, or using your smartphone or computer, other than for homework?” As per the 24-h movement guidelines,23 recreational screen time was classified as “meeting” (<2 h/day) or “not meeting” (≥2 h/day) the recommendation. Sleep was quantified by asking participants the number of hours they sleep per day, with cut-points of ≥9 h for Grade 5 and ≥8 h for Grade 8 as per the 24-h movement guidelines.23
2.2. Data analyses
Descriptive results (e.g., sample sizes, means, standard deviation (SD), and percentage meeting 24-h guidelines) at the grade and sex levels were reported annually and used in our analysis. Temporal trends before (2013–2019) and during (2019–2021) the COVID-19 pandemic were analyzed using sample-weighted linear regression models relating the year of testing to mean PF (8 PF tests) and body size (height and body mass). Linear models were used because they naturally summarized the overall temporal trends. Temporal trends in PF and body size were estimated by adjusting for (a) age and sex (Model 1), and (b) age, sex, body size (height and body mass), and exercise time (Model 2).24 We expressed the overall linear trends in means as absolute trends (i.e., the regression coefficient), percent trends (i.e., the regression coefficient expressed as a percentage of the sample-weighted mean value for all means in the regression), and as standardized (Cohen's) effect sizes (ES) (i.e., the regression coefficient divided by the pooled SD for all values in the regression). Positive trends indicated temporal increases/improvements, and negative trends indicated temporal declines. Additionally, trends in mean exercise time and the percentage of children/adolescents meeting or not meeting the 24-h guidelines for sleep and sedentary behavior23 were also calculated.
Distributional variability was quantified as the coefficient of variation (CV) (i.e., the ratio of the SD to the mean). Trends in CVs were analyzed as the ratio of CVs by dividing the 2019 CV by the 2013 CV (before pandemic) and the 2021 CV by the 2019 CV (during pandemic) using the procedure described elsewhere.25,26 Ratios >1.1 indicated substantial increases in variability (i.e., the magnitude of variability in relation to the mean increased over time), ratios < 0.9 indicated substantial declines in variability (i.e., the magnitude of variability in relation to the mean decreased over time), and ratios between 0.9 and 1.1 indicated negligible trends in variability (i.e., the magnitude of variability in relation to the mean did not change substantially over time).27
3. Results
Age- and sex-adjusted temporal trends in PF and body size before and during the COVID-19 pandemic are shown in Table 1. There were significant trends for all PF measures before and during the pandemic. Some trended upward through 2019 before declining sharply in 2021. For example, the 20-m shuttle run performance improved steadily before the pandemic (ES = 0.005 p.a.) but declined at a 16-fold larger rate during the pandemic (ES = −0.081 p.a.). Similarly, the sit-ups performance was improving before the pandemic (ES = 0.012 p.a.) but then declined at a 7-fold larger rate during the pandemic (ES = –0.086 p.a.). Similar trends were observed for all age–sex groups (Supplementary Tables 1–4). For other PF measures, the before- and during-pandemic temporal differences were considerably smaller (<3-fold). Body mass increased before and during the pandemic, with a 10-fold larger increase during the pandemic. There were negligible trends in variability for all PF and body size measures before and during the pandemic.
Table 1.
Age- and sex-adjusted temporal trends in PF and body size for Japanese children and adolescents before (2013–2019) and during (2019–2021) the COVID-19 pandemic.
| Change in means (95%CI) |
Ratio of CVs (95%CI) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| PF test | n | Standardized (ES) |
Absolute |
Percent (%) |
Before pandemic | During pandemic | |||
| Before pandemic | During pandemic | Before pandemic | During pandemic | Before pandemic | During pandemic | ||||
| Handgrip strength (kg) | 16,398,970 | –0.005 | –0.009 | –0.022 | –0.044 | –0.10 | –0.21 | 1.02 | 1.02 |
| (–0.005 to –0.004) | (–0.010 to –0.008) | (–0.023 to –0.021) | (–0.049 to –0.039) | (–0.11 to –0.10) | (–0.23 to –0.19) | (1.02 to 1.02) | (1.02 to 1.02) | ||
| Sit-ups (number) | 16,203,745 | 0.012 | –0.086 | 0.072 | –0.511 | 0.32 | –2.30 | 1.01 | 1.03 |
| (0.012 to 0.012) | (–0.087 to –0.085) | (0.070 to 0.073) | (–0.517 to –0.505) | (0.32 to 0.33) | (–2.32 to –2.27) | (1.01 to 1.02) | (1.03 to 1.03) | ||
| Sit-and-reach (cm) | 16,327,071 | 0.012 | 0.008 | 0.117 | 0.079 | 0.29 | 0.20 | 1.02 | 1.03 |
| (0.012 to 0.013) | (0.007 to 0.009) | (0.114 to 0.119) | (0.070 to 0.088) | (0.29 to 0.30) | (0.18 to 0.22) | (1.02 to 1.02) | (1.03 to 1.03) | ||
| Side-steps (number) | 16,234,599 | 0.026 | –0.074 | 0.196 | –0.565 | 0.43 | –1.25 | 1.01 | 1.07 |
| (0.026 to 0.026) | (–0.075 to –0.073) | (0.194 to 0.198) | (–0.573 to –0.558) | (0.43 to 0.44) | (–1.27 to –1.23) | (1.01 to 1.01) | (1.07 to 1.07) | ||
| 20-m shuttle run (lap) | 13,282,199 | 0.005 | –0.081 | 0.095 | –1.683 | 0.17 | –3.05 | 1.01 | 1.06 |
| (0.004 to 0.005) | (–0.082 to –0.080) | (0.089 to 0.101) | (–1.706 to –1.661) | (0.16 to 0.18) | (–3.09 to –3.01) | (1.01 to 1.02) | (1.06 to 1.06) | ||
| 50-m sprint (s) | 16,156,563 | –0.005 | 0.014 | –0.005 | 0.012 | –0.05 | 0.14 | 1.05 | 1.03 |
| (–0.006 to –0.005) | (0.013 to 0.014) | (–0.005 to –0.005) | (0.011 to 0.013) | (–0.06 to –0.05) | (0.13 to 0.14) | (1.05 to 1.06 | (1.03 to 1.03) | ||
| Standing broad jump (cm) | 16,202,434 | 0.012 | –0.004 | 0.292 | –0.106 | 0.18 | –0.06 | 1.01 | 1.05 |
| (0.012 to 0.013) | (–0.005 to –0.003) | (0.286 to 0.298) | (–0.130 to –0.083) | (0.17 to 0.18) | (–0.08 to –0.05) | (1.01 to 1.02) | (1.05 to 1.05) | ||
| Ball throw (m) | 16,223,284 | –0.014 | –0.037 | –0.080 | –0.213 | –0.46 | –1.24 | 1.06 | 1.03 |
| (–0.014 to –0.014) | (–0.038 to –0.036) | (–0.081 to –0.078) | (–0.218 to –0.207) | (–0.47 to –0.46) | (–1.27 to –1.20) | (1.06 to 1.06) | (1.02 to 1.03) | ||
| Height (cm) | 16,354,253 | 0.004 | 0.034 | 0.030 | 0.231 | 0.02 | 0.16 | 1.01 | 0.99 |
| (0.004 to 0.005) | (0.033 to 0.035) | (0.028 to 0.032) | (0.224 to 0.237) | (0.02 to 0.02) | (0.15 to 0.16) | (1.01 to 1.01) | (0.99 to 1.00) | ||
| Body mass (kg) | 16,259,017 | 0.004 | 0.041 | 0.031 | 0.322 | 0.08 | 0.83 | 1.01 | 1.01 |
| (0.004 to 0.004) | (0.040 to 0.042) | (0.029 to 0.033) | (0.314 to 0.330) | (0.08 to 0.09) | (0.81 to 0.85) | (1.01 to 1.01) | (1.00 to 1.01) | ||
Notes: Temporal trends in PF and body size were adjusted for age and sex. Positive trends in means indicated temporal increases/improvements, and negative trends in means indicated temporal declines. Ratio of CVs >1.1 indicated substantial temporal increases in variability, and ratios <0.9 indicated substantial temporal declines.
Abbreviations: 95%CI = 95% confidence interval; COVID-19 = coronavirus disease 2019; CV = coefficient of variation; ES = effect size; PF = physical fitness.
Age-, sex-, body size-, and exercise time-adjusted PF trends before and during the COVID-19 are shown in Table 2. Similar trends emerged as with the age- and sex-adjusted trends, which reversed from pre-pandemic increases to decline sharply during the pandemic. Both 20-m shuttle run (ES = 0.006 p.a.) and sit-ups (ES = 0.009 p.a.) performance improved before the pandemic but afterward declined at considerably higher rates (18-fold (ES = −0.109 p.a.) and 15-fold (ES = −0.133 p.a.), respectively). Temporal differences before and during the pandemic were <4-fold for other PF measures.
Table 2.
Age-, sex-, body size-, and exercise time-adjusted temporal trends in PF for Japanese children and adolescents before (2013–2019) and during (2019–2021) the COVID-19 pandemic.
| Change in means (95%CI) |
Ratio of CVs (95%CI) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| PF test | n | Standardized (ES) |
Absolute |
Percent (%) |
Before pandemic | During pandemic | |||
| Before pandemic | During pandemic | Before pandemic | During pandemic | Before pandemic | During pandemic | ||||
| Handgrip strength (kg) | 16,398,970 | –0.010 | –0.020 | –0.050 | –0.094 | –0.24 | –0.45 | 1.01 | 1.01 |
| (–0.011 to –0.010) | (–0.024 to –0.015) | (–0.051 to –0.048) | (–0.114 to –0.074) | (–0.24 to –0.23) | (–0.54 to –0.35) | (1.01 to 1.01) | (1.01 to 1.01) | ||
| Sit-ups (number) | 16,203,745 | 0.009 | –0.133 | 0.055 | –0.792 | 0.25 | –3.56 | 1.01 | 1.06 |
| (0.009 to 0.010) | (–0.137 to –0.129) | (0.054 to 0.057) | (–0.815 to –0.768) | (0.24 to 0.26) | (–3.66 to –3.45) | (1.01 to 1.01) | (1.06 to 1.06) | ||
| Sit-and-reach (cm) | 16,327,071 | 0.013 | –0.018 | 0.123 | –0.167 | 0.31 | –0.42 | 1.02 | 0.98 |
| (0.013 to 0.013) | (–0.022 to –0.014) | (0.120 to 0.126) | (–0.204 to –0.130) | (0.30 to 0.31) | (–0.51 to –0.33) | (1.01 to 1.02) | (0.98 to 0.99) | ||
| Side-steps (number) | 16,234,599 | 0.030 | –0.009 | 0.226 | –0.071 | 0.50 | –0.16 | 0.99 | 0.99 |
| (0.030 to 0.030) | (–0.013 to –0.005) | (0.224 to 0.229) | (–0.101 to –0.040) | (0.50 to 0.51) | (–0.22 to –0.09) | (0.99 to 1.00) | (0.98 to 0.99) | ||
| 20-m shuttle run (lap) | 13,282,199 | 0.006 | –0.109 | 0.121 | –2.258 | 0.22 | –4.09 | 0.99 | 1.06 |
| (0.005 to 0.006) | (–0.113 to –0.104) | (0.113 to 0.128) | (–2.355 to –2.161) | (0.20 to 0.23) | (–4.26 to –3.91) | (0.99 to 1.00) | (1.05 to 1.06) | ||
| 50-m sprint (s) | 16,156,563 | –0.007 | 0.030 | –0.006 | 0.027 | –0.07 | 0.30 | 1.05 | 1.05 |
| (–0.007 to –0.006) | (0.026 to 0.034) | (–0.006 to –0.006) | (0.024 to 0.031) | (–0.07 to –0.06) | (0.26 to 0.34) | (1.04 to 1.05) | (1.05 to 1.05) | ||
| Standing broad jump (cm) | 16,202,434 | 0.012 | –0.014 | 0.278 | –0.322 | 0.17 | –0.19 | 1.01 | 1.02 |
| (0.011 to 0.012) | (–0.018 to –0.010) | (0.270 to 0.285) | (–0.418 to –0.227) | (0.16 to 0.17) | (–0.25 to –0.14) | (1.01 to 1.01) | (1.01 to 1.02) | ||
| Ball throw (m) | 16,223,284 | –0.009 | 0.035 | –0.053 | 0.200 | –0.31 | 1.17 | 1.05 | 1.01 |
| (–0.010 to –0.009) | (0.031 to 0.039) | (–0.055 to –0.052) | (0.177 to 0.224) | (–0.32 to –0.30) | (1.03 to 1.30) | (1.05 to 1.05) | (1.01 to 1.01) | ||
Notes: Temporal trends in PF were adjusted for age, sex, body size (height and mass), and sport/exercise participation. Positive trends in means indicated temporal increases/improvements, and negative trends in means indicated temporal declines. Ratio of CVs >1.1 indicated substantial temporal increases in variability, and ratios <0.9 indicated substantial temporal declines.
Abbreviations: 95%CI = 95% confidence interval; COVID-19 = coronavirus disease 2019; CV = coefficient of variation; ES = effect size; PF = physical fitness.
In Fig. 1, trends in mean exercise time between 2013 and 2021 are shown as trends in absolute values (min/day) because SD and sample size data were unavailable. There was a decline in exercise time among children and adolescents (except for Grade 8 girls), with grade- and sex-specific rates of decline ranging from −5.5% to −19.6% during the pandemic (2019–2021). There were negligible trends in variability for all adjusted PF measures before and during the pandemic.
Fig. 1.
Temporal trends in mean exercise time for Japanese children and adolescents before (2013–2019) and during (2019–2021) the COVID-19 pandemic. Exercise time was self-reported. The 2020 PF survey was canceled due to the COVID-19 pandemic. COVID-19 = coronavirus disease 2019; PF = physical fitness.
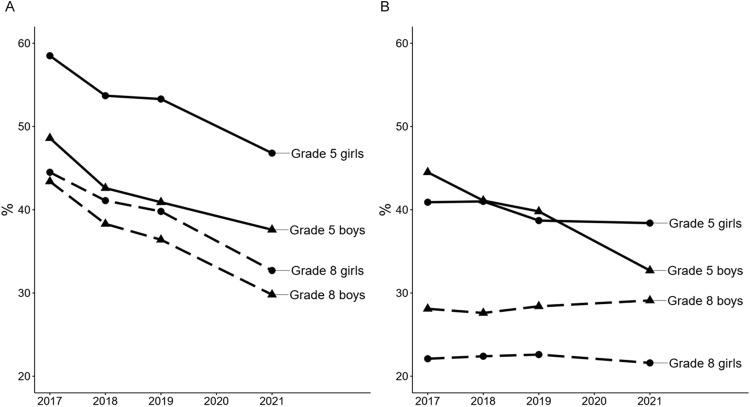
The percentages of children and adolescents who met the screen time (<2 h/day) and the sleep time guidelines (≥9 h/day for Grade 5, ≥8 h/day for Grade 8) are shown in Fig. 2. Collectively, there was a steady decline in the percentage of children and adolescents who met the screen time guideline, with grade- and sex-specific rates of decline ranging from −1.7% to −3.5% during the pandemic (2019–2021) and from −2.5% to −3.9% before the pandemic (2017–2019). The percentage of children and adolescents meeting the recommended sleep guidelines remained steady from 2017 to 2021. Descriptive statistics for PF by grade and sex between 2013 and 2021 are shown in Supplementary Table 5.
Fig. 2.
Temporal trends in the percentage of Japanese children and adolescents who met the (A) screen time and (B) sleep guidelines before (2017–2019) and during (2019–2021) the COVID-19 pandemic. Screen time and sleep were self-reported. Annual trends in the percentage of Japanese children and adolescents meeting (A) the recreational screen time guideline of <2 h/day and (B) sleep guidelines (≥9 h/day for Grade 5 and ≥8 h/day for Grade 8).23 COVID-19 = coronavirus disease 2019.
4. Discussion
We examined trends in the PF levels of a census sample of 16,647,699 Japanese children and adolescents before (2013–2019) and during (2019–2021) the COVID-19 pandemic. The principal findings were (a) that PF generally declined during the pandemic and at larger rates than before, and (b) the 20-m shuttle run and sit-ups performance declined at rates considerably higher (>15-fold) than before the pandemic after adjusting for age, sex, body size, and exercise time. Declines in 20-m shuttle run and sit-ups performance are of concern to public health given these measures are significantly associated with present and future health outcomes among children and adolescents.8, 9, 10,28, 29, 30
4.1. Explanation of main findings
Declines in 20-m shuttle run and sit-ups performance during the pandemic were considerable when compared to before the pandemic levels, and when compared to international trends. For example, the decline in 20-m shuttle run performance during the pandemic was 18-fold larger than the improvement seen before the pandemic when adjusted for age, sex, body size, and exercise time. Among Japanese children and adolescents, the decline in 20-m shuttle run performance during the pandemic was 27-fold larger than the international decline of −0.004 ES p.a. that took place between 2010 and 2014.31 Similarly, the age-, sex-, body size-, and exercise time-adjusted decline in sit-ups performance during the pandemic was 15-fold larger than the before-pandemic improvement, and 11-fold larger than the international decline of −0.012 ES p.a. that occurred between 2010 and 2017.32 In contrast, the decline in standing long jump performance during the pandemic was 2-fold smaller than the international decline of −0.03 ES p.a. between 2010 and 2017.33 These results suggest that declines in 20-m shuttle run and sit-ups performance among Japanese youth were considerable during the pandemic, which is cause for concern. Similar findings were observed in Slovenian children during the pandemic, with endurance performance (long distance running) showing the largest declines and muscle power performance (standing long jump) showing the smallest.18 Also consistent with these findings are the results from a study of children living in the Miyagi prefecture after the 2011 Great East Japan Earthquake (this prefecture was one of the most affected areas34). Researchers saw larger declines in the 20-m shuttle run (ES = –0.09 p.a.) and sit-ups performance (ES = –0.07 p.a.) compared to other PF performance tests (ES: handgrip strength = –0.01 p.a.; sit-and-reach = –0.05 p.a.; side-steps = –0.02 p.a.; 50-m sprint = –0.03 p.a.; standing broad jump = –0.03 p.a.; and ball throw = –0.05 p.a.).35
It is a challenge to explain why performances on endurance PF (longer duration) tests, such as the 20-m shuttle run and sit-ups, were more affected during the pandemic than other PF (short duration) tests, such as the standing long jump and handgrip strength. We have previously argued that temporal trends in PF performance are probably caused by a network of environmental, social, behavioral, psychosocial, and/or physiological factors.31,36 Several recent studies have found declines in body-size adjusted 20-m shuttle run37 and sit-ups38 performances, which suggest that declines in PA levels have influenced the declines in PF. No study to our knowledge has examined temporal trends in 20-m shuttle run and sit-ups performance while statistically adjusting for trends in PA levels. Our novel finding of declines in age-, sex-, body size-, and exercise time-adjusted 20-m shuttle run and sit-ups performance indicate that factors other than increased body size and reduced exercise time are probably at play. Systematic reviews have found consistent positive associations between vigorous PA and both cardiorespiratory fitness (CRF)39 and muscular endurance.40 Given that only the duration, not the intensity, of exercise time was self-reported in the JP Fit Survey for Youth, it is possible that long duration vigorous PA levels among Japanese schoolchildren declined during, but not before, the pandemic. It is also possible that pandemic-related restrictions (e.g., school/recreation facility closures and organized sports cancellations/restrictions) impacted the quantity and intensity of physical education, active play, active transportation, and/or muscle strengthening activities, resulting in larger declines in 20-m shuttle run and sit-ups performance during the pandemic compared to beforehand. For example, in Japan, unlike in other countries, organized sport in school settings is highly popular, and the majority of Japanese children and adolescents participate in organized sport at school.41 However, after the outbreak of the pandemic, most organized sports activities were cancelled for several months. The restrictions, such as reduced practice time, continued for more than a year. This starved children and adolescents of PA opportunities, including vigorous intensity and continuous types of PA (both maximal and sub-maximal PA).42 In contrast, since children's PA patterns are generally intermittent (as opposed to continuous) in nature,43 pandemic-related changes in intermittent PA may have been minimal compared to changes in endurance (aerobic) PA. This may help explain why other PF measures were less affected during the COVID-19 pandemic compared to 20-m shuttle run and sit-ups performance.
4.2. Comparisons with other studies
Previous studies examining the effects of the COVID-19 pandemic on PF among children and adolescents have also found a negative effect, although the magnitude of the declines in PF varied between studies.11, 12, 13, 14, 15, 16, 17, 18, 19 We do note that all studies,11, 12, 13, 14, 15, 16, 17,19 with the exception of one,18 recruited small non-probability samples of youth, ranging from 10 to 764 children and adolescents, which may explain the between-study differences. Such between-study differences could also be due to differences in participant pools, policy decisions on school and sport closures, timing of testing, test methodologies, as well as changes in movement behaviors during the pandemic. Our study builds on previous findings by providing the most complete national picture of the COVID-19 pandemic-related impact on PF, using annual census PF data on Japanese children and adolescents since 2013. Our study found significant declines in PF, which along with declines in exercise time and percentage of school children meeting screen time guidelines, suggest an overall decline in population health during the COVID-19 pandemic.
4.3. Future efforts to restore pre-pandemic PF levels
While the long-term effects of COVID-19-related restrictions are unknown and need further investigation, declines in PF during the COVID-19 pandemic, particularly with respect to CRF, may negatively impact population health. Low CRF, specifically, tracks moderately well from childhood into adulthood44, 45, 46 and is significantly associated with all-cause mortality in later life.10,47 Therefore, there is a pressing need to help Japanese children and adolescents return to pre-pandemic PF levels. Japan was succeeding in its approach to improving population PF levels, as demonstrated by the pre-pandemic improvements we found in most PF components, including CRF (measured as 20-m shuttle run performance in this study). Therefore, relaxing pandemic restrictions may help restore pre-pandemic PF levels. On the other hand, the COVID-19-related restrictions provide an opportunity for Japan to reimagine PA by complementing structured PA with informal and unstructured PA. Although Japan's unique culture of organized school sport activities should be maintained, international experts also recommend increasing PA opportunities by promoting informal and unstructured PA activities at home, in the community, and in non-school settings.48 Such an approach may improve population PF levels, especially among those not currently involved in organized sport.49
4.4. Strengths and limitations
This study has several strengths. First, we used annual census PF data from the annual JP Fit Survey for Youth surveillance system for all Grades 5 and 8 Japanese students between 2013 and 2021. The school-level participation rate in the PF surveillance system has been consistently near perfect since 2013 (average = 97.0%). These data allowed us to estimate national trends in PF for Japanese children and adolescents before and during the COVID-19 pandemic with very high statistical power. Additionally, our analytical approach enabled us to examine trends in PF while statistically adjusting for important covariates, including age, sex, body size, and exercise time. While we used only summary statistics (since raw data were not available), our trends (and corresponding 95% confidence intervals (95%CIs)) were not biased compared to those based on individual-level regression.24
The limitations of this study include missing data from 2020 due to COVID-19 lockdowns. This lack of data meant we could not determine continuous trends between May–July 2019 (before pandemic) and May–July 2021 (during pandemic). Therefore, while the time course of the trends in PF during the pandemic is unclear (e.g., Did PF steadily decline or drastically decline and then plateau/improve?), our linear regression approach did provide an overall summary. Second, our trends may not be generalizable to all Japanese children and adolescents (i.e., those not in Grades 5 and 8). Understanding whether trends in PF during the pandemic differed for those at different developmental stages would help determine whether targeted or generalized initiatives are required. Third, movement behaviors were self-reported and may be inaccurate. For example, the exercise time question used in the JP Fit Survey for Youth reportedly overestimates PA levels when compared to accelerometry.50 Additionally, only the duration of each movement behavior was estimated (exercise, screen, and sleep time) with neither the type nor the content evaluated (e.g., intensity (moderate, vigorous) and domain (school vs. non-school PA, weekday vs. weekend)). Trends in self-reported measures may also suffer from recall or response bias.51 Furthermore, since only the mean exercise time statistics were presented in the surveillance report (no SD and sample size data were available), we were unable to determine the statistical significance of such trends. Nonetheless, it is important to note that the JP Fit Survey for Youth has used the same questions every year since 2013 (for exercise) and 2017 (for screen time and sleep).
5. Conclusion
We found general declines in PF levels for Japanese children and adolescents during the COVID-19 pandemic, with the largest declines occurring in 20-m shuttle run and sit-ups performance. Given that these PF measures are significantly associated with present and future health, these declines suggest corresponding declines in population health due to the pandemic-related restrictions implemented in Japan. Japan's annual national surveillance of PF for children and adolescents is unique. It not only provides insight into the negative effects of COVID-19-related restrictions on PF, it also predicts future disease burden and highlights potential opportunities to engage cost-effective public health surveillance strategies. Moving forward, efforts must be made to help Japanese children and adolescents return to pre-pandemic PF levels.
Acknowledgments
Data availability statement
The datasets analyzed in this study are available from the corresponding author on reasonable request.
Acknowledgment
Supported in part by JSPS KAKENHI Scientific Research (C) (20K11450 to KS) and by Institute of Health and Sports Science & Medicine, Juntendo University.
Authors' contributions
TK developed the research question, designed the study, led the statistical analysis, and drafted the manuscript; GRT designed the study, led the statistical analysis, and helped draft the manuscript; JJL led the statistical analysis and helped draft the manuscript; and KS developed the research question, designed the study, and helped draft the manuscript. All authors had full access to the data and takes responsibility for the integrity of the data. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2022.11.002.
Contributor Information
Tetsuhiro Kidokoro, Email: kidokoro@nittai.ac.jp.
Koya Suzuki, Email: ko-suzuki@juntendo.ac.jp.
Supplementary materials
References
- 1.World Health Organization. Coronavirus disease (COVID-19) pandemic: WHO characterizes COVID-19 as a pandemic. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [accessed 08.07.2022]
- 2.Looi MK. COVID-19: Japan declares state of emergency as Tokyo cases soar. BMJ. 2020;369:m1447. doi: 10.1136/bmj.m1447. [DOI] [PubMed] [Google Scholar]
- 3.Yamada Y, Yoshida T, Nakagata T, Nanri H, Miyachi M. Letter to the editor: Age, sex, and regional differences in the effect of COVID-19 pandemic on objective physical activity in Japan: A 2-year nationwide longitudinal study. J Nutr Health Aging. 2021;25:1032–1033. doi: 10.1007/s12603-021-1662-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim H, Ma J, Kim J, Xu D, Lee S. Changes in adherence to the 24-hour movement guidelines and overweight and obesity among children in northeastern Japan: A longitudinal study before and during the COVID-19 pandemic. Obesities. 2021;1:167–177. [Google Scholar]
- 5.Hyunshik K, Jiameng M, Sunkyoung L, Ying G. Change in Japanese children's 24-hour movement guidelines and mental health during the COVID-19 pandemic. Sci Rep. 2021;11:22972. doi: 10.1038/s41598-021-01803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson DC, Ramage K, Moore SA, Riazi N, Tremblay MS, Faulkner G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: A scoping review of evidence after the first year. J Sport Health Sci. 2021;10:675–689. doi: 10.1016/j.jshs.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc Med. 2021;7 doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the American Heart Association. Circulation. 2016;134:e653–99. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 9.Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: A powerful marker of health. Int J Obes (Lond) 2008;32:1–11. doi: 10.1038/sj.ijo.0803774. [DOI] [PubMed] [Google Scholar]
- 10.Sato M, Kodama S, Sugawara A, Saito K, Sone H. Physical fitness during adolescence and adult mortality. Epidemiology. 2009;20:463–464. doi: 10.1097/EDE.0b013e31819ed09f. [DOI] [PubMed] [Google Scholar]
- 11.López-Bueno R, Calatayud J, Andersen LL, et al. Cardiorespiratory fitness in adolescents before and after the COVID-19 confinement: A prospective cohort study. Eur J Pediatr. 2021;180:2287–2293. doi: 10.1007/s00431-021-04029-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jarnig G, Jaunig J, van Poppel MNM. Association of COVID-19 mitigation measures with changes in cardiorespiratory fitness and body mass index among children aged 7 to 10 years in Austria. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.21675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dayton JD, Ford K, Carroll SJ, Flynn PA, Kourtidou S, Holzer RJ. The deconditioning effect of the COVID-19 pandemic on unaffected healthy children. Pediatr Cardiol. 2021;42:554–559. doi: 10.1007/s00246-020-02513-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wahl-Alexander Z, Camic CL. Impact of COVID-19 on school-aged male and female health-related fitness markers. Pediatr Exerc Sci. 2021;33:61–64. doi: 10.1123/pes.2020-0208. [DOI] [PubMed] [Google Scholar]
- 15.Chambonnière C, Fearnbach N, Pelissier L, et al. Adverse collateral effects of COVID-19 public health restrictions on physical fitness and cognitive performance in primary school children. Int J Environ Res Public Health. 2021;18:11099. doi: 10.3390/ijerph182111099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramos Álvarez O, Arufe Giráldez V, Cantarero Prieto D, Ibáñez García A. Changes in physical fitness, dietary habits and family habits for Spanish children during SARS-CoV lockdown. Int J Environ Res Public Health. 2021;18:13293. doi: 10.3390/ijerph182413293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrison SA, Meh K, Sember V, Starc G, Jurak G. The effect of pandemic movement restriction policies on children's physical fitness, activity, screen time, and sleep. Front Public Health. 2021;9:785679. doi: 10.3389/fpubh.2021.785679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jurak G, Morrison SA, Kovač M, et al. A COVID-19 crisis in child physical fitness: Creating a barometric tool of public health engagement for the republic of Slovenia. Front Public Health. 2021;9:644235. doi: 10.3389/fpubh.2021.644235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basterfield L, Burn NL, Galna B, et al. Changes in children's physical fitness, BMI and health-related quality of life after the first 2020 COVID-19 lockdown in England: A longitudinal study. J Sports Sci. 2022;40:1088–1096. doi: 10.1080/02640414.2022.2047504. [DOI] [PubMed] [Google Scholar]
- 20.Kidokoro T, Tomkinson GR, Noi S, Suzuki K. Japanese physical fitness surveillance: A greater need for international publications that utilize the world's best physical fitness database. J Phys Fitness Sports Med. 2022;11:161–167. [Google Scholar]
- 21.Ministry of Education, Culture, Sports, Science, and Technology. Implementation guidelines for the new physical fitness test (6–11 years). Available at: https://www.mext.go.jp/a_menu/sports/stamina/05030101/001.pdf. [accessed 08.07.2022] [in Japanese]
- 22.Ministry of Education, Culture, Sports, Science, and Technology. Implementation guidelines for the new physical fitness test (12–19 years). Available at: https://www.mext.go.jp/a_menu/sports/stamina/05030101/002.pdf. [accessed 08.07.2022] [in Japanese]
- 23.Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S311–S327. doi: 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- 24.Moineddin R, Urquia ML. Regression analysis of aggregate continuous data. Epidemiology. 2014;25:929–930. doi: 10.1097/EDE.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 25.Tomkinson GR, Kidokoro T, Dufner T, Noi S, Fitzgerald JS, McGrath RP. Temporal trends in handgrip strength for older Japanese adults between 1998 and 2017. Age Ageing. 2020;49:634–639. doi: 10.1093/ageing/afaa021. [DOI] [PubMed] [Google Scholar]
- 26.Tomkinson GR, Kidokoro T, Dufner TJ, Noi S, Fitzgerald JS, Brown-Borg HM. Temporal trends in 6-minute walking distance for older Japanese adults between 1998 and 2017. J Sport Health Sci. 2021;10:462–469. doi: 10.1016/j.jshs.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Drinkwater EJ, Hopkins WG, McKenna MJ, Hunt PH, Pyne DB. Modelling age and secular differences in fitness between basketball players. J Sports Sci. 2007;25:869–878. doi: 10.1080/02640410600907870. [DOI] [PubMed] [Google Scholar]
- 28.Smith JJ, Eather N, Morgan PJ, Plotnikoff RC, Faigenbaum AD, Lubans DR. The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sports Med. 2014;44:1209–1223. doi: 10.1007/s40279-014-0196-4. [DOI] [PubMed] [Google Scholar]
- 29.Katzmarzyk PT, Craig CL. Musculoskeletal fitness and risk of mortality. Med Sci Sports Exerc. 2002;34:740–744. doi: 10.1097/00005768-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 30.García-Hermoso A, Ramírez-Campillo R, Izquierdo M. Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and meta-analysis of longitudinal studies. Sports Med. 2019;49:1079–1094. doi: 10.1007/s40279-019-01098-6. [DOI] [PubMed] [Google Scholar]
- 31.Tomkinson GR, Lang JJ, Tremblay MS. Temporal trends in the cardiorespiratory fitness of children and adolescents representing 19 high-income and upper middle-income countries between 1981 and 2014. Br J Sports Med. 2019;53:478–486. doi: 10.1136/bjsports-2017-097982. [DOI] [PubMed] [Google Scholar]
- 32.Kaster T, Dooley FL, Fitzgerald JS, et al. Temporal trends in the sit-ups performance of 9,939,289 children and adolescents between 1964 and 2017. J Sports Sci. 2020;38:1913–1923. doi: 10.1080/02640414.2020.1763764. [DOI] [PubMed] [Google Scholar]
- 33.Tomkinson GR, Kaster T, Dooley FL, et al. Temporal trends in the standing broad jump performance of 10,940,801 children and adolescents between 1960 and 2017. Sports Med. 2021;51:531–548. doi: 10.1007/s40279-020-01394-6. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization . 2011. The great east Japan earthquake.https://apps.who.int/iris/bitstream/handle/10665/207516/9789290615682_eng.pdf Available at: [accessed 08.07.2022] [Google Scholar]
- 35.Miyagi Board of Education . Miyagi Board of Education; Miyagi prefecture: 2010. Report book on the survey of physical fitness and athletic ability. –2011. [in Japanese] [Google Scholar]
- 36.Tomkinson GR, Olds TS. Secular changes in pediatric aerobic fitness test performance: The global picture. Med Sport Sci. 2007;50:46–66. doi: 10.1159/000101075. [DOI] [PubMed] [Google Scholar]
- 37.Sandercock GR, Ogunleye A, Voss C. Six-year changes in body mass index and cardiorespiratory fitness of English schoolchildren from an affluent area. Int J Obes (Lond) 2015;39:1504–1507. doi: 10.1038/ijo.2015.105. [DOI] [PubMed] [Google Scholar]
- 38.Sandercock GRH, Cohen DD. Temporal trends in muscular fitness of English 10-year-olds 1998–2014: An allometric approach. J Sci Med Sport. 2019;22:201–205. doi: 10.1016/j.jsams.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 39.Gralla MH, McDonald SM, Breneman C, Beets MW, Moore JB. Associations of objectively measured vigorous physical activity with body composition, cardiorespiratory fitness, and cardiometabolic health in youth: A review. Am J Lifestyle Med. 2019;13:61–97. doi: 10.1177/1559827615624417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith JJ, Eather N, Weaver RG, Riley N, Beets MW, Lubans DR. Behavioral correlates of muscular fitness in children and adolescents: A systematic review. Sports Med. 2019;49:887–904. doi: 10.1007/s40279-019-01089-7. [DOI] [PubMed] [Google Scholar]
- 41.Uchiumi K. Extra-curricular school sport (bukatsu) and corporal punishment in Japan. Asia Pac J Soc Work. 2014;3:108–114. [Google Scholar]
- 42.Schmidt SCE, Anedda B, Burchartz A, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: A natural experiment. Sci Rep. 2020;10:21780. doi: 10.1038/s41598-020-78438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomes TN, Katzmarzyk PT, Pereira S, Thuany M, Standage M, Maia J. A systematic review of children's physical activity patterns: Concept, operational definitions, instruments, statistical analyses, and health implications. Int J Environ Res Public Health. 2020;17:5837. doi: 10.3390/ijerph17165837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ortega FB, Ruiz JR, Labayen I, et al. Role of socio-cultural factors on changes in fitness and adiposity in youth: A 6-year follow-up study. Nutr Metab Cardiovasc Dis. 2013;23:883–890. doi: 10.1016/j.numecd.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 45.Ruiz JR, Castro-Piñero J, Artero EG, et al. Predictive validity of health-related fitness in youth: A systematic review. Br J Sports Med. 2009;43:909–923. doi: 10.1136/bjsm.2008.056499. [DOI] [PubMed] [Google Scholar]
- 46.Malina RM. Physical activity and fitness: Pathways from childhood to adulthood. Am J Hum Biol. 2001;13:162–172. doi: 10.1002/1520-6300(200102/03)13:2<162::AID-AJHB1025>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 47.Högström G, Nordström A, Nordström P. Aerobic fitness in late adolescence and the risk of early death: A prospective cohort study of 1.3 million Swedish men. Int J Epidemiol. 2016;45:1159–1168. doi: 10.1093/ije/dyv321. [DOI] [PubMed] [Google Scholar]
- 48.Straker L, Booth V, Cleland V, et al. Reimagining physical activity for children following the systemic disruptions from the COVID-19 pandemic in Australia. Br J Sports Med. 2022;56:5–6. doi: 10.1136/bjsports-2021-105277. [DOI] [PubMed] [Google Scholar]
- 49.Vella SA, Schranz NK, Davern M, et al. The contribution of organised sports to physical activity in Australia: Results and directions from the Active Healthy Kids Australia 2014 report card on physical activity for children and young people. J Sci Med Sport. 2016;19:407–412. doi: 10.1016/j.jsams.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 50.Sasayama K, Adachi M. Comparison of physical activity using questionnaire and accelerometer in 4th grade children. Jpn J Phys Fitness Sports Med. 2019;68:91–96. [Google Scholar]
- 51.Durante R, Ainsworth BE. The recall of physical activity: Using a cognitive model of the question-answering process. Med Sci Sports Exerc. 1996;28:1282–1291. doi: 10.1097/00005768-199610000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed in this study are available from the corresponding author on reasonable request.