Abstract
Background
Hand hygiene, facemask wearing, and physical distancing play a crucial role in the prevention of the COVID-19 pandemic. Identifying the key psychosocial determinants of these precautionary behaviors contributes to effective intervention and policymaking for COVID-19 and future pandemics.
Purpose
This study aimed to systematically review and meta-analyze available evidence on psychosocial determinants of the general population’s practice of three precautionary behaviors, based on the Risk, Attitudes, Norms, Abilities, and Self-regulation (RANAS) framework.
Methods
Literature was identified by searching seven databases and relevant review papers. Observational and experimental studies targeting the general population (≥18 years) published between January 2020 to September 2021 were included. Pooled effect sizes were calculated with the inverse-variance method using random-effects models.
Results
A total of 51 studies (64 samples) were included in the qualitative synthesis, of which 30 studies (42 samples) were included in the meta-analysis. RANAS-based constructs including knowledge, pros attitudes, and perceived norms were identified as significant determinants of all three behaviors in the meta-analysis. Perceived susceptibility and cons attitudes showed no significant associations with any behaviors. Perceived severity, perceived control, self-efficacy, and behavioral intention were significantly associated with one or two behaviors. Country (western vs. eastern hemispheres) significantly moderated the effects of certain risk and ability factors.
Conclusions
More research is needed with respect to the intention–behavior relationship, self-regulatory and reflexive factors of precautionary behaviors, as well as the exploration of the potential moderating effect of sociodemographic factors.
Keywords: COVID-19, Psychosocial determinants, Hand hygiene, Facemask wearing, Physical distancing, RANAS model
Adults who had more knowledge, positive behavioral attitudes, and better compliance with the norms, showed better practices of hand hygiene, facemask wearing, and physical distancing during the COVID-19 pandemic.
Introduction
The novel coronavirus disease (COVID-19) pandemic has continued for over 2 years and has had a devastating impact globally, with more than 543 million confirmed cases and over 6.3 million deaths as reported on June 30, 2022 [1]. Recently, several effective coronavirus vaccines have been developed. Universal vaccination cannot be achieved in the short term because of time constraints in the production and delivery of the vaccines, and vaccination mobilization for all populations (e.g., more than 30% of populations in some countries have not been fully vaccinated as of June 30, 2022) [1–3]. Most importantly, even following vaccination, there is no guarantee of full protection from COVID-19 [4, 5]. Therefore, prevention of COVID-19 infection is still important and continues to rely on non-pharmaceutical interventions, particularly individuals’ precautionary practices.
Performing individual precautionary behaviors including hand hygiene, facemask wearing, and physical distancing have been a straightforward way to prevent viral transmission and inhibit disease spread, with advocacy from many health authorities (e.g., World Health Organization, American Centers for Disease Control and Prevention, and National Health Commission of the People’s Republic of China) [6–10]. Recent policymaker’s guides of some countries also emphasized the effectiveness of compliance with the “3W” (Wash your hands, Wear a mask, and Watch your distance/keep social distancing) during the COVID-19 prevention campaign [10, 11]. Notwithstanding relevant recommendations and mass information campaigns, evidence from many countries has indicated that not all citizens were fully compliant with precautionary behaviors during the pandemic [12, 13]. Therefore, identifying psychosocial determinants of precautionary behaviors that are potentially modifiable by interventions is an efficacious approach to promote the enactment of such behaviors.
Based on previous psychosocial theories of behavioral change, such as the health belief model (HBM) [14], the theory of reasoned action (TRA) [15], the theory of planned behavior (TPB) [16], and the health action process approach (HAPA) [17], an integrated theoretical framework was proposed by Mosler (2012) [18], namely the Risk, Attitudes, Norms, Abilities, and Self-Regulation (RANAS) model. The RANAS model summarizes the psychosocial components of previous theories and recategorizes them into five blocks for designing and evaluating behavior change strategies (e.g., information interventions and persuasive interventions) [18, 19]. The risk factors block comprises all factors that reflect the individuals’ awareness, perception, and understanding of health risks (e.g., perceived susceptibility, perceived severity, and health knowledge) [14]. The attitudinal factors block includes the individuals’ positive (pros) or negative (cons) appraisals toward behavior and its consequences (e.g., perceived benefits and perceived barriers) [18, 20]. The normative block of factors describes the individuals’ convictions about the possibility of certain behaviors and their social networks’ perceptions of the behavior, thus creating social pressure to implement that behavior [21–23], while the ability factors block represents the individuals’ ability to perform a behavior and address target diseases (e.g., self-efficacies, perceived control, and health literacy) [24–27]. Finally, the fifth block consists of diverse self-regulatory factors ensuring behavioral execution and maintenance, such as self-monitoring (i.e., continuous evaluation of the behavioral execution with regard to a behavioral standard), action planning (i.e., when, where, and how she or he adherent to a behavior), and coping planning (i.e., what are the possible barriers of behavioral execution and what are the corresponding approaches to overcome these barriers) [18, 19, 28–30]. In addition, the RANAS model proposes that individual behaviors and behavioral intention are not determined only by psychosocial factors, social contextual factors (e.g., country and cultural differences) should also be considered for designing effective interventions [18, 19].
The five-block RANAS model has been examined in various health behaviors in diverse populations, providing an effective and pragmatic framework for designing and implementing behavioral interventions [19, 22, 28, 31, 32]. Further, studies examining the association of these modifiable factors with precautionary behaviors in the general population have been prevalent during the COVID-19 pandemic, yet available evidence has not been well summarized.
Most reviews have focused on the combination of diverse precautionary behaviors (e.g., overall practice of personal disinfection, avoidant behaviors, and nutrition supplement), whereas the diversity and distinction between these behaviors were comparatively ignored [9, 13, 33–37]. For instance, some researchers summarized the evidence on knowledge, attitudes, and practice (KAP) during the pandemic, providing preliminary support for a significant interrelationship between KAP concepts [13, 34, 35]. Another paper reviewing studies published between December 2019 and February 2021, focused on the social determinants of adherence to COVID-19 preventive guidelines [36] and identified the influential role of various demographic and social factors. However, the above reviews did not focus on specific precautionary behaviors (e.g., hand hygiene, facemask wearing, and physical distancing). To the best of our knowledge, only one scoping review has examined the determinants of physical distancing measures during the pandemic, whereas a systematic review and quantitative synthesis have not been undertaken [27].
In addition, some studies have shown that the practice of these three precautionary behaviors varied across eastern and western hemispheres [38–40]. For example, compared with people in eastern countries (e.g., China, Japan, and South Korea), people in western countries (e.g., European countries and USA) are more likely to wash hands frequently and less likely to wear facemasks in preventing the transmission of COVID-19 [39, 40]. A recent cross-cultural study also indicated that people in Europe had less knowledge and awareness of COVID-19 compared with those in the Asian regions as the pandemic began to unfold in 2020 [41]. However, the impact of cross-country differences on the association between COVID-19 precautionary behaviors and their psychosocial determinants has not been examined in a summary review and meta-analysis.
Taken together, a better understanding and systematic identification of the modifiable factors for the specific precautionary behaviors is needed in order to design effective and tailored interventions. This is also necessary and beneficial for governmental policymaking to support efficient organization, implementation, and evaluation of precautionary behaviors promotion programs [42]. Therefore, the current study aimed to systematically review and meta-analyze relevant evidence on the association of RANAS-based psychosocial constructs with each of the three precautionary behaviors (hand hygiene, facemask wearing, and physical distancing) during the COVID-19 pandemic in the general population (aged ≥ 18 years). Furthermore, the moderating role of country (eastern vs. western hemispheres) in the relationship between psychosocial determinants and precautionary behaviors was also examined.
Methods
Search Strategy and Study Selection
The present systematic review and meta-analysis were undertaken following the Cochrane guidelines and the results were reported according to the PRISMA statement [43]. The systematic review protocol has been prospectively registered on PROSPERO (Ref. CRD42020214966). According to a predefined literature search strategy (Supplementary Material 1), the following five databases were searched electronically: PsycINFO, PubMed, MEDLINE (using the EBSCOhost), EMBASE (using the Ovid platform), and Cochrane Library. Further, two databases were hand-searched, including the PROSPERO registry platform (COVID-19 theme) and ClinicalTrials.gov. In addition, the reference lists of relevant systematic reviews were also screened. Since the COVID-19 pandemic was first announced by the WHO on December 31, 2019 [1], the search span was limited from January 1, 2020 to September 30, 2021 (first-wave search was up to February 28, 2020 and second-wave search was by September 30, 2021). The literature search was limited to human participants and was not limited to specific publication languages.
Following the PICOS principles, the study selection criteria included: (a) Population: studies targeting the general population (≥18 years) of any gender were eligible for inclusion. Considering that health professionals (e.g., frontline nurses, medical staff, and healthcare workers) directly participated in the control of the COVID-19 pandemic and were presumed to be better equipped with self-protective measures, the target population in the present study excluded health professionals. (b) Intervention/exposure: studies targeting the individual precautionary behaviors in response to the COVID-19 pandemic were included. (c) Comparison: not applicable in the present study. (d) Outcomes of interest: studies focusing on the practice of three individual precautionary behaviors (i.e., hand hygiene, facemask wearing, or physical distancing) toward the COVID-19 pandemic and RANAS-based psychosocial determinants of these precautionary behaviors were included. In our study, hand hygiene refers to washing hands with soap, water, or alcohol-based hand rub, and other hand disinfection behaviors, while facemasks included surgical masks, N95 respirators, and other cloth face covering. Physical distancing denotes diverse physical avoidant behaviors (e.g., staying out of crowded places and avoiding mass gatherings), and keeping at least 1-m space between people, while excessive physical distancing behaviors (e.g., avoided hospitals or clinics) and self-isolation/mandatory quarantine due to inflection of the COVID-19 were excluded. Studies that measured the combined preventive practice (e.g., KAP) without data for each single precautionary behavior were excluded. (e) Study types: observational studies (e.g., cross-sectional and cohort) and experimental/quasi-experimental studies (e.g., randomized controlled trial) were eligible for inclusion, while editorials and pure qualitative assessments were excluded. In addition, we only included full-text articles that contained primary data and could be retrieved through online databases, library requests, or email correspondence with the authors.
All identified publications were exported into reference management software (Mendeley) for duplication checking and further screening. Following the de-duplication, the titles and abstracts of all identified publications were initially screened by three reviewers (W.L., D.P., and J.J.), where clearly irrelevant publications were excluded. At the stage of the full-text eligibility screen, two reviewers (W.L. and D.P.) independently reviewed the publications remaining after the initial screen. Disagreements during the review process were resolved by consensus or by involving a third reviewer.
Data Extraction
Based on the study selection criteria, data from all eligible publications were exported to Microsoft Excel 2016. DP/XW extracted the information, including authors, publication date, study design, region, sample characteristics (age, gender), precautionary behavior measured, RANAS-based psychosocial components, theories reported, and the main results on the association between RANAS-based constructs and precautionary behavior (e.g., effect estimates, associated 95% confidence intervals [CI], and standardized errors [SE]).
Study Quality Assessment
Two reviewers (W.L. and F.L.) independently evaluated the quality of each included study using the National Institute of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies [44]. The NIH quality assessment tool determines study quality using 14 criteria (e.g., clarity of research questions, appropriateness of study population, sample size justification, quality of outcome measures, and accuracy of statistical analysis). Overall study quality was judged using four categories: “high = satisfying all assessed parameters,” “good = did not satisfy one parameter,” “moderate = did not satisfy two to four parameters,” and “poor = did not satisfy more than four parameters” [45]. In addition, we planned to use the Cochrane risk of bias tool (Version 2) for randomized controlled trials [46]; however, no eligible randomized trials were identified in our search.
Data Synthesis and Meta-analysis
Meta-analyses were conducted if at least three samples provided effect sizes of the association for the same parameters [47]. Otherwise, a narrative synthesis was conducted. In the meta-analysis, the adjusted odds ratio (OR) was used as the effect size measure. Several studies used multivariate linear regression, so the regression coefficients (beta) and their standard errors (SE) were extracted to calculate the ORs with 95% CI (beta = logOR) [48]. For studies reporting other adjusted effect sizes (e.g., Cohen’s f2), the data was arithmetically converted to OR using a spreadsheet [49]. For studies with multiple effect sizes in a particular scope of outcomes (e.g., different physical distancing behaviors), the weighted arithmetic averaging approach was used to pool the effect sizes in a synthesized size [50]. The pooled effect size with 95% CI was estimated using the inverse-variance method under the random-effects model assumption. The percentage of total variation across the studies due to heterogeneity (Cochran’s Q-statistic) was used to calculate the I2 statistics, with I2 values of 25%, 50%, and 75% indicating small, moderate, and large degrees of heterogeneity, respectively [51].
Publication bias was identified using funnel plots and Egger’s regression tests [52]. Sensitivity analyses were conducted on study quality and study design to evaluate the robustness of the summary estimates and determine whether a particular study accounted for the heterogeneity. In addition, we examined the potential sources of heterogeneity by stratifying the meta-analyses for different subgroups (i.e., country: western vs. eastern hemispheres) in case the number of included samples is ≥10 [53]. The analyses were conducted using Review Manager 5.4 and R (R Core Team, 2013), with a statistical significance threshold of p value <.05 for overall effect examination, and <.10 for tests of heterogeneity and publication bias [24, 52].
Results
Study Selection and Characteristics
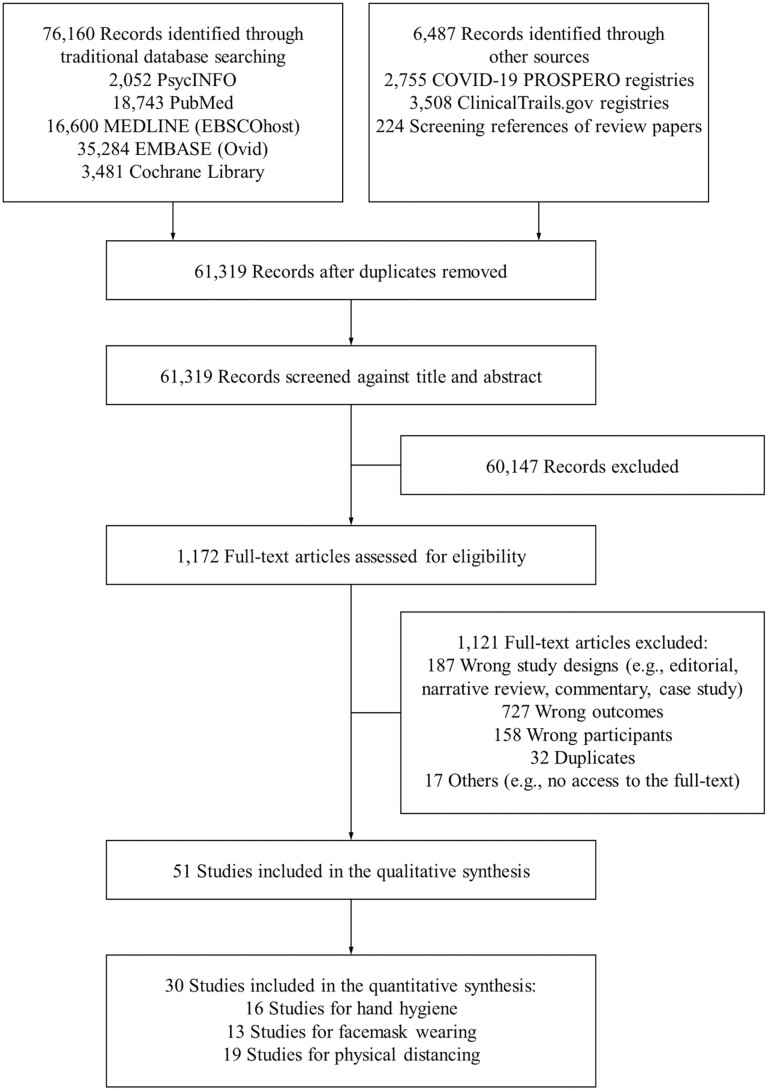
The search resulted in 61,319 potentially relevant records (Figure 1). A total of 51 studies (k) with 191,772 general adults (n) were included in the systematic review (47 cross-sectional and 4 longitudinal), among which 30 studies (n = 118,986) provided eligible data for the meta-analysis (references are attached in Supplementary Material 2). As shown in Table 1, these 51 studies contained 64 different samples (42 samples were included in the meta-analysis), most of which were in the western countries (62.5%; e.g., the USA, Canada, UK, France, and Australia). For individual precautionary behaviors, physical distancing raised the most interest (k = 39), while many studies also focused on hand hygiene (k = 24) and facemask wearing (k = 22). Among the included studies, the rate of participants practicing hand hygiene, facemask wearing, and physical distancing was 26.3%–96.6%, 18.5%–96.4%, and 18.0%–98.0%, respectively (i.e., answering “Yes” in the binary 1/0 scale, and scoring 4–5 in the 5-point Likert scale, and 3–4 in the 4-point Likert scale for behaviors). For the RANAS-based psychosocial constructs, most of the studies focused on the risk factors (k = 44), followed by the attitudinal factors (k = 26), while only two studies examined the self-regulatory factors, and six studies examined the intention–behavior relationship. About 76.5% of included studies explicitly indicated the theoretical frame for the examination, where the top two theories were the HBM (k = 14) and the TPB (k = 10) (Supplementary Material 2).
Fig. 1.
PRISMA flow diagram.
Table 1.
Study Characteristics
| Characteristics | No. of studies | Percentages (%) |
|---|---|---|
| 51 | 100.00 | |
| Publication year | ||
| 2020 | 24 | 47.1 |
| 2021 | 27 | 52.9 |
| Region of samples (s = 64) | ||
| Western culture | 40 | 62.5 |
| America (i.e., USA, Canada, Columbia, Mexico) | 20 | 50.0 |
| Europe (i.e., UK, Belgium, France, Switzerland, etc.) | 14 | 35.0 |
| Oceania (i.e., Australia and New Zealand) | 2 | 5.0 |
| Africa (i.e., Ethiopia, Sierra Leone and South Africa) | 4 | 10.0 |
| Eastern culture | 24 | 37.5 |
| Middle east (i.e., Qatar and Saudi Arabia) | 2 | 3.1 |
| Southeast Asia (i.e., China, Korea, Indonesia, etc.) | 22 | 33.8 |
| Study design | ||
| Cross-sectional | 47 | 92.2 |
| Longitudinal | 4 | 7.8 |
| Behavioral outcome measures | ||
| Hand hygiene | 24 | 47.1 |
| Facemask wearing | 22 | 43.1 |
| Physical distancing | 39 | 76.5 |
| RANAS-based psychosocial constructs | ||
| Risk factor block | 44 | 86.3 |
| Knowledge | 20 | 45.5 |
| Perceived severity | 22 | 50.0 |
| Perceived susceptibility | 25 | 56.8 |
| Overall risk perception/awareness/threat | 7 | 15.9 |
| Attitudinal factor block | 26 | 51.0 |
| Pros (e.g., perceived effectiveness, benefits) | 23 | 88.5 |
| Cons (e.g., perceived barriers) | 5 | 19.2 |
| Overall (pros + cons) | 3 | 11.5 |
| Normative factor block | 14 | 26.9 |
| Perceived norms | 14 | 26.9 |
| Others (e.g., moral) | 1 | 1.9 |
| Ability factor block | 21 | 41.2 |
| Perceived control | 8 | 38.1 |
| Self-efficacy | 15 | 71.4 |
| Health literacy (actional knowledge) | 1 | 4.8 |
| Self-regulation factor block | 2 | 3.8 |
| Action planning | 2 | 3.8 |
| Coping planning | 2 | 3.8 |
| Action control | 1 | 1.9 |
| Theoretical backdrop reported | ||
| Not reported | 12 | 23.5 |
| Reported (e.g., HBM, TPB, KAP, PMT) | 39 | 76.5 |
| Study quality | ||
| High | 8 | 15.7 |
| Good | 26 | 51.0 |
| Moderate | 17 | 33.3 |
| Poor | 0 | 0 |
HBM health belief model; TPB theory of planned behavior; KAP knowledge, attitude, and practice framework; PMT protection motivation theory.
Study Quality Assessment
As presented in Table 1, 34 studies (66.7%) were rated as high (k = 8) and good quality (k = 26), while 16 studies (33.3%) were assessed as moderate quality with no poor-quality studies. Among studies with good and moderate quality (k = 43), the major weakness included (a) no/inadequate description/justification for the sample size estimate (k = 36, 83.7%), (b) no/inadequate statement for the definition, reliability, and validity of outcome measures (k = 17, 39.5%), (c) no adjustment/analysis or justification for the covariates and confounders (k = 8, 18.6%), and (d) no clearly stated inclusion/exclusion criteria of participant recruitment (k = 6, 14.0%). Complete details for study quality are presented in Supplementary Material 3.
Psychosocial Determinants of Hand Hygiene
A total of 24 studies (k) describing 32 samples (s) with 148,192 participants examined the psychosocial factors of hand hygiene, covering the intention–behavior relationship and four components of the RANAS model (i.e., risk factors, attitudinal factors, normative factors, and ability factors). Of these, 16 studies (s = 24) reported data for the effect size synthesis (n = 102,030). Forest plots can be found in Supplementary Material 4 (Supplementary Fig. SA1–SA7).
Intention–behavior relationship for hand hygiene
One study examined the association between behavioral intention and hand hygiene behavior, supporting a significant positive intention–behavior relationship (OR = 1.91, 95% CI = [1.17–3.13]) [54].
Risk factors for hand hygiene
A total of 23 studies investigated the risk factors of hand hygiene, including knowledge (k = 11), perceived susceptibility (k = 14), perceived severity (k = 13), and overall risk perception (k = 2). For the meta-analysis, 13 studies (s = 21) provided eligible data. As shown in Table 2, the pooled effect size was statistically significant for knowledge (OR = 1.25, p = .008), while the association was not statistically significant for perceived severity (OR = 1.06, p = .06) and perceived susceptibility (OR = 1.02, p = .57). There was large heterogeneity in the magnitude of effect sizes for these risk factors across the included samples (I2 = 86%–92%, all p < .001). Two studies measured the overall risk perception (susceptibility + severity) and were included only in the narrative analysis. A consistent and significant positive association between overall risk perception and hand hygiene practice was indicated in these two studies [55, 56].
Table 2.
Meta-analysis on the Association of RANAS-Based Psychosocial Constructs With Hand Hygiene
| Psychosocial constructs | k | s | n | OR | [95% CI] | Z | Q | I 2 (%) | Egger’s test |
|---|---|---|---|---|---|---|---|---|---|
| Risk factors | |||||||||
| Knowledge | 5 | 5 | 6,741 | 1.25** | [1.06, 1.48] | 2.66 | 49.11 | 92 | 0.85 |
| Perceived susceptibility | 9 | 17 | 90,857 | 1.02 | [0.94, 1.12] | 0.57 | 176.36 | 91 | −0.44 |
| Perceived severity | 7 | 15 | 90,001 | 1.06† | [1.00, 1.13] | 1.88 | 97.36 | 86 | −1.56 |
| Attitudinal factors | |||||||||
| Pros | 10 | 13 | 85,609 | 1.35*** | [1.21, 1.52] | 5.27 | 183.51 | 93 | 2.95 |
| Cons | 3 | 6 | 73,363 | 0.87† | [0.76, 1.00] | 1.94 | 14.87 | 66 | −0.17 |
| Normative factors | |||||||||
| Perceived norms | 3 | 3 | 4,623 | 1.28* | [1.06, 1.55] | 2.58 | 7.58 | 74 | 0.14 |
| Ability factors | |||||||||
| Self-efficacy | 3 | 6 | 72,621 | 1.66** | [1.16, 2.37] | 2.76 | 136.13 | 96 | −1.52 |
***p < .001
**p < .01
*p < .05
† p < .10.
Subgroup analyses revealed that country (western vs. eastern hemispheres) significantly modified the effects of perceived susceptibility on the behavioral practice, while no significant subgroup effect was found for perceived severity (Qsubgroup difference = 0.51, I2 = 0%, p = .47). In particular, the contribution of perceived susceptibility on hand hygiene was significant and stronger among western samples (OR = 1.16 [1.01, 1.33], p = .04; Q = 53.89, I2 = 85%, p < .001), while the relationship with this behavioral practice was negative and nonsignificant among eastern samples (OR = 0.92 [0.83, 1.02], p = .11; Q = 93.45, I2 = 93%, p < .001; Qsubgroup difference = 6.93, I2 = 85.6%, p = .008).
Attitudinal factors for hand hygiene
Seventeen studies examined the attitudinal correlates of hand hygiene, covering pros (e.g., perceived benefits, perceived effectiveness; k = 15), cons (e.g., perceived barriers; k = 3), and overall attitudes (pros + cons; k = 1). Ten studies (s = 13) provided data for the quantitative synthesis. A pooled analysis revealed that the association with hand hygiene was statistically significant for pros (OR = 1.35, p < .001), while marginally significant for cons (OR = 0.87, p = .05; Table 2). Moderate-to-large heterogeneity of effect sizes was found between samples (I2 = 66%–93%, all p < .001). A positive significant association between overall attitudes and hand washing was reported in one study which was excluded from the meta-analysis [57]. For subgroup analyses, we found that country did not show a significant moderating role in the association between pros attitudes and hand hygiene (Qsubgroup difference = 0.63, I2 = 0%, p = .43).
Normative factors for hand hygiene
Four studies examined the contribution of perceived norms on hand hygiene [19, 54, 57, 58]. The quantitative synthesis of three studies (s = 3) indicated a statistically significant association between perceived norms and behavioral practice (OR = 1.28, p = .01), with a moderate-to-high heterogeneity of effect sizes (I2 = 74%, p = .02). Subgroup analyses were not applicable due to lack of sufficient samples.
Ability factors for hand hygiene
Six studies investigated the association of hand hygiene with ability factors, including self-efficacy (k = 4), perceived control (k = 3), and health literacy (k = 1). For self-efficacy, a pooled analysis of three studies (s = 6) revealed a significant association with behavior practice (OR = 1.66, p = .006), showing a large heterogeneity of effect sizes (I2 = 74%, p < .001). Three studies that were excluded from the meta-analysis due to lack of eligible data, showed mixed results in terms of the association between perceived control and hand hygiene [54, 57, 58]. One study indicated a significantly inverse association of health literacy with hand hygiene (PR = 0.76, 95% CI = [0.68, 0.86], p < .001) [59]. Subgroup analyses were not applicable due to lack of enough samples.
Psychosocial Determinants of Facemask Wearing
A total of 24 studies (k) describing 28 samples (s) with 37,201 participants examined the psychosocial correlates of facemask wearing, containing the intention–behavior association and four components of the RANAS model (i.e., risk factors, attitudinal factors, normative factors, and ability factors). Of these, 13 studies (s = 19) were included in the meta-analysis (n = 21,137). Forest plots can be found in Supplementary Material 4 (Supplementary Fig. SB1–SB6).
Intention–behavior relationship for facemask wearing
One study examined the association between behavioral intention and facemask wearing, indicating a nonsignificant intention–behavior relationship (OR = 1.38, p = .13) [60].
Risk factors for facemask wearing
Seventeen studies examined the association of facemask wearing with three risk factors, specifically, knowledge (k = 10), perceived susceptibility (k = 11), and perceived severity (k = 12), among which, 9 studies (s = 15) reported available data for the quantitative synthesis. The pooled analysis revealed that facemask wearing was significantly associated with knowledge (OR = 1.34, p = .01), yet not with perceived susceptibility (OR = 1.04, p = .30) or perceived severity (OR = 1.02, p = .28). The heterogeneity in the magnitude of effect sizes for these risk factors between the included samples ranged from moderate-to-large (I2 = 68%–88%, all p < .001; see Table 3).
Table 3.
Meta-analysis on the Association of RANAS-Based Psychosocial Constructs With Facemask Wearing
| Psychosocial constructs | k | s | n | OR | [95% CI] | Z | Q | I 2 (%) | Egger’s test |
|---|---|---|---|---|---|---|---|---|---|
| Risk factors | |||||||||
| Knowledge | 4 | 4 | 4,162 | 1.34** | [1.07, 1.69] | 2.54 | 9.24 | 68 | 0.46 |
| Perceived susceptibility | 8 | 14 | 13,415 | 1.04 | [0.97, 1.11] | 1.03 | 106.54 | 88 | −0.44 |
| Perceived severity | 8 | 14 | 13,415 | 1.02 | [0.98, 1.07] | 1.07 | 42.11 | 69 | 0.73 |
| Attitudinal factors | |||||||||
| Pros | 8 | 9 | 13,686 | 1.27*** | [1.13, 1.43] | 3.97 | 109.25 | 93 | 0.41 |
| Normative factors | |||||||||
| Perceived norms | 3 | 4 | 3,850 | 1.30** | [1.10, 1.54] | 3.04 | 35.55 | 92 | −0.54 |
| Ability factors | |||||||||
| Perceived control | 2 | 3 | 2,846 | 1.33 | [0.93, 1.90] | 1.54 | 92.93 | 98 | 10.83 |
***p < .001
**p < .01.
Subgroup analyses were conducted on perceived susceptibility and severity. We found that the associations between perceived susceptibility (OR = 1.04 [1.01, 1.08], p = .01; Q = 2.92, I2 = 0%, p = .57) and perceived severity (OR = 1.04 [1.01, 1.07], p = .02; Q = 4.21, I2 = 5%, p = .38) with facemask wearing were significant in western samples, with heterogeneity decreasing to nonsignificance. Among eastern samples, the overall effect sizes were still nonsignificant. By contrast, the associations between this behavioral practice and perceived susceptibility (Qsubgroup difference = 0.01, I2 = 0%, p = .98) and perceived severity (Qsubgroup difference = 0.08, I2 = 0%, p = .78) were not moderated by country.
Attitudinal factors for facemask wearing
Fourteen studies examined the association between facemask wearing and attitudinal factors, where the positive aspects of attitudes (e.g., perceived importance, benefits, and effectiveness of preventive behavior) were measured in all included studies, while the negative aspect (i.e., perceived barriers) was only evaluated in one study [54]. For the positive aspect, a pooled analysis of eight studies (s = 9) revealed a significant association with facemask wearing practice (OR = 1.27, p < .001), showing a large heterogeneity of effect sizes across the included samples (I2 = 93%, p < .001). A nonsignificant correlation of behavior and perceived barriers was identified (β = −0.04, 95% CI = −0.12 to 0.04, p = .28) [61]. Subgroup analyses were not applicable due to the limited samples.
Normative factors for facemask wearing
Five studies examined the contribution of perceived norms on the practice of facemask wearing. A pooled analysis of three studies (s = 4) indicated a significant association (OR = 1.30, p = .002), with large heterogeneity (I2 = 92%, p < .001). Subgroup analyses were not applicable due to the limited samples.
Ability factors for facemask wearing
Five studies investigated the association between facemask wearing and ability factors, including perceived control (k = 2) and self-efficacy (k =3). For perceived control, the meta-analysis with three samples indicated a nonsignificant association (OR = 1.33, p = .12), with a large level of heterogeneity (I2 = 98%, p < .001). For self-efficacy, three studies in the narrative synthesis indicated inconsistent findings on the association with behavioral practice (two nonsignificant and one positive significant) [60, 62, 63].
Psychosocial Determinants of Physical Distancing
For physical distancing, 38 studies (k) describing 45 samples (s) with 142,129 participants were examined, covering the intention–behavior relationship and all blocks of RANAS-based psychosocial correlates. Of these, 19 studies (s = 23) were included in the meta-analysis (n = 102,500). Forest plots can be found in Supplementary Material 4 (Supplementary Fig. SC1–SC8).
Intention–behavior relationship for physical distancing
Five studies examined the association between behavioral intention and physical distancing, and a significant positive intention–behavior relationship was found in four of these studies [64–67]. The remaining study indicated mixed results, where the intention was significantly associated with keeping >2m outside and not visiting friends/family, yet not with limiting leave home and keeping > 2m inside [47].
Risk factors for physical distancing
Thirty-three studies examined the contribution of risk factors on physical distancing, covering knowledge (k = 14), perceived susceptibility (k = 19), perceived severity (k = 15), and overall risk perception (k = 5). Sixteen studies (s = 21) were included in the meta-analysis and showed a statistically significant association of physical distancing with knowledge (OR = 1.14, p = .02) and perceived severity (OR = 1.20, p < .001), yet not with perceived susceptibility (OR = 1.04, p = .28). The heterogeneity of the effect sizes was large across the included samples (I2 = 80%–89%, all p < .001; see Table 3). A higher overall risk perception/perceived threat was found to be positively associated with the practice of physical distancing in five studies, which did not offer adjusted effect estimates and thus were excluded from the quantitative synthesis [56, 65, 68–70].
For subgroup analyses, we found that country was a significant moderator of the effect of perceived severity on physical distancing, yet not in perceived susceptibility (Qsubgroup difference = 2.14, I2 = 53.2%, p = .14). Particularly, the contribution of perceived severity on physical distancing was stronger in western samples (OR = 1.31 [1.16, 1.48], p < .001; Q = 68.57, I2 = 91%, p < .001) compared with eastern samples (OR = 1.13 [1.12, 1.27], p < .001; Q = 47.86, I2 = 85%, p < .001; Qsubgroup difference = 4.13, I2 = 75.8%, p = .04).
Attitudinal factors for physical distancing
Seventeen studies examined the association of physical distancing with attitudinal factors, including pros (k = 16), cons (k = 5), and overall attitudes (k = 1). For the meta-analysis, the pooled effect was found to be significant for pros (OR = 1.32, p < .001), yet not for cons (OR = 0.96, p = .31; see Table 3). There was large heterogeneity in the effect sizes for pros (I2 = 94%, p < .001), however, the cons had a nonsignificant estimate (I2 = 44%, p = .10). One study indicated significant correlations between overall attitudes and the practice of diverse physical distancing behaviors (r = .16 to .32, all p < .01) [57]. Nonsignificant subgroup differences were identified in the post hoc test, indicating that country did not significantly modify the effects of pros (Qsubgroup difference = 0.90, I2 = 0%, p = .34) and cons (Qsubgroup difference = 0.02, I2 = 0%, p = .90) on the practice of physical distancing.
Normative factors for physical distancing
Nine studies examined the contribution of perceived norms on physical distancing. A pooled analysis of five studies (s = 5) with effect size information indicated a significant norm-behavioral relationship (OR = 1.05, p = .03), with nonsignificant heterogeneity of effect sizes across the samples (I2 = 15%, p = .32; see Table 3). Subgroup analyses were not undertaken due to inadequate samples.
Ability factors for physical distancing
Sixteen studies investigated the association between ability factors and physical distancing, including perceived control (k = 6) and self-efficacy (k = 12). For perceived control, the meta-analysis of four studies (s = 4) indicated a significant overall effect (OR = 1.23, p = .007), with a large level of heterogeneity (I2 = 92%, p < .001). For self-efficacy, similar findings were found in seven studies (s = 10; OR = 2.01, p < .001; I2 = 95%, p < .001).
Results of subgroup analyses revealed that country was a significant moderator of the effect of self-efficacy on physical distancing. Specifically, the relationship between self-efficacy and physical distancing was weaker in western samples (OR = 1.76 [1.50, 2.07], p < .001; Q = 42.46, I2 = 86%, p < .001) relative to eastern samples (OR = 2.56 [2.39, 2.75], p < .001; Q = 2.56, I2 = 22%, p = .28; Qsubgroup difference = 17.46, I2 = 94.3%, p < .001).
Self-regulation factors for physical distancing
Three articles, describing two studies, focused on the self-regulation factors of physical distancing (i.e., action planning, coping planning, and self-monitoring) [65, 66, 71]. Beeckman et al. (2020) conducted a cross-sectional survey among Belgian adults and found that both action planning (β = 0.50–0.84, p < .001) and coping planning (β = 0.30–0.59, p < .001) showed a significant association with adhering to “keep a 1.5 m physical distance” in the multiple regression models [65]. However, mixed findings were presented in another two-wave prospective study with Australian and US adults [66, 71]. The researchers found that although action planning, coping planning, and self-monitoring showed a significant zero-order correlation with physical distancing (r = .24–.67, p < .001), their direct effects on physical distancing were not significant when adding other HAPA-based variables in the structural equation model (|β| < 0.17, p = .15–.97) [71].
Publication Bias and Sensitivity Tests
Publication bias was assessed for all psychosocial determinants. Based on the inspection of funnel plots and Egger’s tests, we found no evidence of significant publication bias (all p > .10; see Tables 2–4; Supplementary Material 5). Consistent findings without apparent fluctuation were revealed in sensitivity tests on study quality and study design, supporting the stability of the results.
Table 4.
Meta-analysis on the Association of RANAS-Based Psychosocial Constructs With Physical Distancing
| Psychosocial constructs | k | s | n | OR | [95% CI] | Z | Q | I 2 (%) | Egger’s test |
|---|---|---|---|---|---|---|---|---|---|
| Risk factors | |||||||||
| Knowledge | 5 | 5 | 7,484 | 1.14* | [1.02, 1.28] | 2.29 | 19.91 | 80 | 0.52 |
| Perceived susceptibility | 13 | 17 | 95,016 | 1.04 | [0.97, 1.10] | 1.08 | 91.32 | 82 | 1.03 |
| Perceived severity | 11 | 15 | 91,884 | 1.20*** | [1.13, 1.27] | 5.76 | 126.12 | 89 | 1.99 |
| Attitudinal factors | |||||||||
| Pros | 12 | 15 | 86,769 | 1.32*** | [1.18, 1.47] | 4.99 | 231.29 | 94 | 3.33 |
| Cons | 4 | 7 | 73,763 | 0.96 | [0.88, 1.04] | 1.01 | 10.79 | 44 | −1.84 |
| Normative factors | |||||||||
| Perceived norms | 5 | 5 | 5,426 | 1.05* | [1.01, 1.10] | 2.21 | 4.70 | 15 | 1.41 |
| Ability factors | |||||||||
| Perceived control | 4 | 4 | 5,636 | 1.23** | [1.06, 1.42] | 2.68 | 35.60 | 92 | 4.25 |
| Self-efficacy | 7 | 10 | 79,044 | 2.01*** | [1.67, 2.41] | 7.47 | 185.85 | 95 | −2.56 |
***p < .001
**p < .01
*p < .05.
Discussion
The purpose of this large international systematic review and meta-analysis was to examine the relationship between RANAS-based psychosocial determinants and the general population’s practice of hand hygiene, facemask wearing, and physical distancing during the COVID-19 pandemic. We found that RANAS-based constructs varied in the relationship with the three precautionary behaviors, and country (western vs. eastern) showed a moderating role in the effects of specific psychosocial determinants on behavioral practice. A summary of the overall findings is presented in Table 5.
Table 5.
A Summary of the Quantitative and Qualitative Synthesis
| RANAS-based constructs | Hand hygiene adherence | Facemask wearing adherence | Physical distancing adherence |
|---|---|---|---|
| Behavioral intention | sig+ (narrative) | ns (narrative) | sig+ (narrative) |
| Risk factor block | |||
| Knowledge | sig+ | sig+ | sig+ |
| Perceived susceptibility | nsa | ns | ns |
| Perceived severity | ns | ns | sig+a |
| Attitudinal factor block | |||
| Pros | sig+ | sig+ | sig+ |
| Cons | ns | ns (narrative) | ns |
| Normative factor block | |||
| Perceived norms | sig+ | sig+ | sig+ |
| Ability factor block | |||
| Perceived control | Mixed (narrative) | ns | sig+ |
| Self-efficacy | sig+ | Mixed (narrative) | sig+b |
| Self-regulation factor block | |||
| Action planning | n/a | n/a | Mixed (narrative) |
| Coping planning | n/a | n/a | Mixed (narrative) |
| Action control | n/a | n/a | Mixed (narrative) |
ns nonsignificant association; sig+ positive significant association; n/a not applicable.
aThe association with the precautionary behavior may be weaker among eastern samples compared with western samples.
bThe association with the precautionary behavior may be stronger among eastern samples compared with western samples.
Collectively, this review compiled data from 191,772 participants (aged ≥ 18 years) in 64 samples across 51 studies, covering all continents. The majority of studies were assessed as good and high quality. Thus, the available sample of studies represents a rich dataset to appraise the state of current evidence in an attempt to organize the findings and propose areas for future research [72]. Importantly, there was no evidence of significant publication bias among the included studies and the sensitivity test indicated no statistically significant relationships between the magnitude of effects and study quality, allowing for robust generalization of the findings.
Interestingly, unlike physical activity and other health behaviors, the intention–behavior relationship was only examined in a few studies on precautionary behaviors. We found that the behavioral intention was significantly associated with hand hygiene (k = 1) and physical distancing (k = 4/5), but not with facemask wearing (k = 1). More research on the intention–behavior relationship targeting precautionary behaviors is needed.
Risk factors were the most frequently investigated constructs among the included studies. Knowledge was identified as a consistent correlate of all three behaviors, providing quantitative support to earlier reviews that found a “convincing” positive association between knowledge and preventive practices [13, 34–36]. The above findings imply the usefulness of information campaigns on promoting preventive behaviors during the COVID-19 pandemic. Knowledge-enhancing strategies [73], such as presenting information about the circumstances and possibilities of contracting the disease, would be appropriate and essential.
Interestingly, perceived susceptibility did not show a significant relationship with any of these behaviors, and perceived severity was only associated with physical distancing. Similar findings have also been found in previous review papers, where perceived susceptibility and severity showed weak and indirect impacts on the behavioral changes, especially with the inclusion of other psychosocial determinants (e.g., attitudes and self-efficacy) [74, 75]. It has been suggested that the relationship between precautionary practices and susceptibility and severity beliefs might be moderated or hindered by various factors (e.g., type of target behaviors, demographics, other covariates, and measurement period) [14, 74].
Some researchers have also suggested that after individuals have adopted certain preventive behavior, they should logically perceive themselves as less susceptible to negative health outcomes. This process would result in a negative association between susceptibility and the likelihood of adopting the target behavior [14]. The same could be true for severity if the target behavior reduced the severity of the illness or pandemics [14, 74]. Taken together, our findings suggest that such “threat” components could be used sparingly in interventions, especially compared with knowledge.
Aligning with earlier reviews and meta-analyses, pros attitudes (e.g., perceived effectiveness and benefits of behavior) showed a stable and significant association with all studied precautionary behaviors [13, 36]. It is worth noting that cons attitude (e.g., perceived barriers) was not a salient determinant with any behaviors in our study. For hand hygiene and physical distancing, the behavioral practice might not be perceived as too challenging, particularly considering the situation that communities and societies have taken strict sanitization measures (e.g., provision of hand sanitizers in public and implementation of physical distancing policy) [76, 77]. For facemask wearing, only one study provided evidence for a nonsignificant association between perceived barriers and behavioral practice. More studies on this relationship are needed (e.g., perceived shortage of mask supply may affect the behavioral practice). Overall, our findings are commensurate with communication theories that highlight an emphasis on pros over cons [78]. When combined with knowledge, this suggests a focus on causal explanations/persuasive arguments of high positive expectancies and appropriate persuasive peripheral cues [18], when designing the intervention content.
It should be noted that some theories (e.g., multi-process action control and reasoned action approach) emphasize attitudes as containing effective (e.g., “pleasant, enjoyable”) and cognitive/instrumental dimensions (e.g., “beneficial, useful”) [79] and several studies have demonstrated how the effective dimension may have superior predictive utility [80, 81]. While our meta-analysis did not contain enough studies using these attitudinal dimensions to explore these potential distinctions, they may distinguish COVID-19 precautionary behaviors (e.g., mask-wearing practices may be explained by variability in affective attitude). These components of attitude should be examined in future research.
Perceived norms were also identified as a prominent determinant of all three precautionary behaviors in our study. Considering the special societal context of these precautionary behaviors (i.e., others depend on the behaviors to reduce infection during the COVID-19 pandemic), it is not surprising that these behaviors were found to be associated with norms. This is different than other individual health behaviors, such as exercise, dietary behavior, and alcohol, where norms are often less associated with behavioral change [82]. It is noteworthy that we focused on the general concept of norms (e.g., social normative pressure) rather than the subcomponents (e.g., descriptive and injunctive norms) in our study [83–85]. Further studies identifying the distinctive impact of each subtype of norms are needed. Overall, our findings underline the importance of appropriate strategies for enhancing normative factors, such as reinforcing a public commitment by showing that most people perform these behaviors or by encouraging individuals to imagine how they would feel after they behaved in a way that is inconsistent with their personal norms [18].
For ability factors, self-efficacy and perceived control were identified as significant correlates of one or two preventive behaviors. Self-efficacy showed a strong association with hand hygiene and physical distancing. This is not surprising, as numerous review papers have demonstrated similar findings in relation to the indispensable role of self-efficacy in behavioral initiation and maintenance [24, 27, 75]. However, mixed results were found on facemask wearing in the narrative synthesis of three studies. For perceived control, a salient association was only found for physical distancing, yet not for hand hygiene or facemask wearing. Previous reviews and meta-analyses have shown similar findings that the effect of perceived behavioral control was trivial and nonsignificant for certain health behaviors (e.g., alcohol) [83]. These precautionary behaviors are not particularly difficult to perform and thus may not require much agency (e.g., perceived behavioral control and self-efficacy) [86]. By contrast, these behaviors are more normative, knowledge dependent, and attitudinal. The applied recommendation is that brief instructions on how to perform each behavior may be helpful but intensive intervention on personal abilities seems unneeded.
For self-regulation factors, only two studies (three samples) conducted a relevant investigation on physical distancing and showed mixed results. Our study could not provide strong evidence on the critical role of these regulatory components in promoting the three precautionary behaviors, which contrasts the strong relationship between these factors and the maintenance of other health behaviors (e.g., physical activity, healthy eating, and smoking ceasing) [20]. More empirical evidence contributing to quantitative analysis is needed before any recommendations can be rendered.
In the current review, we also identified the moderating role of country on the effects of RANAS-based psychosocial determinants on the three precautionary behaviors. Interestingly, we found that certain risk factors (i.e., perceived susceptibility and perceived severity) showed stronger effects on the behavioral practices among western samples compared with those within the eastern countries. More specifically, western samples who have a higher level of perceived susceptibility were more likely to comply with hand hygiene recommendations. Similarly, western countries also had a stronger relationship between perceived severity and physical distancing than eastern countries. In contrast, the effect of the ability factor (i.e., self-efficacy) on physical distancing favored eastern samples in comparison with western samples. In other words, eastern samples who had more confidence on their ability were more likely to keep a secure physical distance relative to western samples. The above findings to some extent provide a potential explanation for the results of previous review papers, where compliance with preventive behaviors was found to vary prominently across different ethnicities and countries [33, 36]. While country/culture-related mechanisms seem to exist, our findings underline the generic importance of modifiable factors and addressing them through interventions, especially in a resource-oriented way considering the characteristics of different precautionary behaviors.
Despite the important findings and implications of this review, several limitations should be noted. First, although we implemented a thorough literature search of relevant databases and resources, we may have omitted suitable studies due to missing key terms over the time span that was searched. Second, we had to exclude some of the identified articles due to lack of reporting statistics that could be used to estimate the adjusted OR. Our use of specific terms (e.g., limited to the RANAS-based constructs) and low return rate from authors who had missing statistical information has likely narrowed the available studies for the quantitative synthesis. Moreover, a high degree of heterogeneity, and the small number of included studies could result in cautious interpretations of the synthesized results. Although we conducted moderating analyses on country, the heterogeneity was not fully resolved. Other potential sources of heterogeneity may be due to differences in outcome measures. In our review, all the included studies used self-reported items for measuring precautionary behaviors. Self-report measures are feasible, economic, and time-saving for data collection, but they have limitations of high subjectivity and low accuracy caused by measurement and response biases (e.g., recall bias and social desirability) [87, 88]. This may also lead to the heterogeneity of effect size estimates. Furthermore, public health messaging was changing over time and varied across different countries and regions, which could also affect individuals’ practice of precautionary behaviors during the pandemic [89]. Due to the limited data, these potential sources of heterogeneity have not been systematically examined in our study. As the relevant evidence continues to increase, future research syntheses may be able to detect the effects of the additional moderators (e.g., demographic information, personality, psychological well-being, outcome measures, and public health messaging) on relevant associations. In addition, our findings and suggestions come with the caveat that the current study focused on behavioral prediction rather than behavior change. Future reviews that summarize relevant evidence on behavioral change and maintenance are needed. Finally, the RANAS framework includes largely reflective and regulatory aspects of behavior and not reflexive factors, such as habits, implicit associations, emotion, or identity. As research incorporating such constructs accumulates, sufficient data might be available in the future to include all these constructs in the meta-analytic analyses.
Conclusion
To the best of our knowledge, the current study is the first to provide a comprehensive review and cumulative estimates of the effect sizes and variability among RANAS-based psychosocial constructs as determinants of COVID-19 precautionary behaviors. Our findings showed that knowledge, pros attitude, and perceived norms were salient determinants of the general population’s practice of hand hygiene, facemask wearing, and physical distancing during the COVID-19 pandemic. Other RANAS-based constructs varied in their relationships with the three precautionary behaviors. We also found a prominent moderating role of country in the effects of certain risk and ability factors on these behavioral practices. The overall findings add new knowledge and understanding of modifiable determinants for specific precautionary behaviors. The current review is also expected to provide important information and make a unique contribution to designing effective tailored interventions and making efficient policy strategies in the battle with COVID-19 and future pandemics.
Supplementary Material
Contributor Information
Wei Liang, School of Competitive Sport, Shandong Sport University, Shandong, China; Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Yanping Duan, Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Feifei Li, Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Ryan E Rhodes, School of Exercise Science, Physical and Health Education, University of Victoria, Victoria, Canada.
Xiang Wang, Department of Curriculum and Instruction, the Education University of Hong Kong, Hong Kong, China.
Dehiwala Liyanage Ishanka Harshani Kusum Peiris, Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Lin Zhou, Lab of Measurement and Evaluation in Health Sciences, Hebei Normal University, Hebei, China.
Borui Shang, Department of Social Sciences, Hebei Sport University, Hebei, China.
Yide Yang, School of Medicine, Hunan Normal University, Hunan, China.
Julien S Baker, Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Jiao Jiao, Center for Health and Exercise Science Research, Hong Kong Baptist University, Hong Kong, China.
Wei Han, School of Competitive Sport, Shandong Sport University, Shandong, China.
Funding
This study was funded by the Faculty Research Funding of Emerging Industries of Modern Sport, Shandong Sport University (JNSX2021068).
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards All authors declared no conflict of interest.
Transparency Statement A review protocol has been also prospectively registered on PROSPERO (CRD42020214966). Data used in the analysis has been attached in the supplementary files. Analytic code used in this study are available by emailing the first and corresponding authors.
Authors’ Contributions W.L. was responsible for conceptualization, data curation, formal analysis, investigation, methodology, and writing the original draft; Y.D. contributed to the methodology, reviewing, and editing the original draft; F.L. contributed to the investigation, methodology, reviewing, and editing the original draft; R.R. contributed to the methodology, reviewing, and editing the original draft; X.W. contributed to the formal analysis and investigation; D.P. contributed to the investigation and data curation; L.Z. contributed to the investigation and validation; B.S. contributed to the data validation and reviewing the original manuscript; Y.Y. contributed to the data curation, software, and reviewing the original manuscript; J.S.B. contributed to the validation, reviewing, and editing the manuscript; J.J. contributed to the methodology, investigation, and reviewing the original manuscript; W.H. was responsible for funding acquisition, supervision, reviewing, and editing the original manuscript; All authors have reviewed and approved the final version of the manuscript.
References
- 1. World Health Organization. Coronavirus disease (COVID-19) pandemic. Available at http://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessibility verified July 18, 2022.
- 2. Usher AD. COVID-19 vaccines for all? Lancet. 2020; 395:1822–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wouters OJ, Shadlen KC, Salcher-Konrad M, et al. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet. 2021; 397:1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bernal JL, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B. 1.617. 2 (Delta) variant. New Engl J Med. 2021; 385:585–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chin ET, Leidner D, Zhang Y, et al. Effectiveness of the mRNA-1273 Vaccine during a SARS-CoV-2 delta outbreak in a prison. New Engl J Med. 2021; 385:2300–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. Advice on the use of masks in the context of COVID-interim guidance. Available at https://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak. Accessibility verified July 18, 2022.
- 7. Centers for Disease Control and Prevention. How to protect yourself & others. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessibility verified July 18, 2022.
- 8. Chiu NC, Chi H, Tai YL, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. J Med Internet Res. 2020; 22:e21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li F, Liang W, Rhodes RE, et al. A systematic review and meta-analysis on the preventive behaviors in response to the COVID-19 pandemic among children and adolescents. BMC Public Health 2022; 22:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fakhira AD, Pawitra AS, Diyanah KC, Wikurendra EA, Nagy I, Abdeljawad NS.. Awareness of doing 3M (wearing mask, physical distancing, washing hands) during pandemic era in rural and urban families. J Kesehatan Lingkungan. 2021; 13:94–101. [Google Scholar]
- 11. Promoting mask-wearing during the COVID-19 pandemic: A policy-maker’s guide [Internet]. Available at https://africacdc.org/download/promoting-mask-wearing-during-the-covid-19-pandemic-a-policymakers-guide/. Accessibility verified July 18, 2022.
- 12. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet. 2020; 395:1973–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siddiquea BN, Shetty A, Bhattacharya O, Afroz A, Billah B.. Global epidemiology of COVID-19 knowledge, attitude and practice: A systematic review and meta-analysis. BMJ Open. 2021; 11:e051447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Janz NK, Becker MH.. The health belief model: A decade later. Health Edu Quart. 1984; 11:1–47. [DOI] [PubMed] [Google Scholar]
- 15. Fishbein M, Ajzen I.. Attitudes and voting behavior: An application of the theory of reasoned action. Prog Appl Soc Psycho. 1981; 1:253–313. [Google Scholar]
- 16. Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, eds. Action Control. SSSP Springer Series in Social Psychology. Berlin, Heidelberg: Springer. doi: 10.1007/978-3-642-69746-3_2. [DOI] [Google Scholar]
- 17. Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psycho. 2008; 57:1–29. [Google Scholar]
- 18. Mosler HA. Systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. Int J Environ Health Res. 2012; 22:431–449. [DOI] [PubMed] [Google Scholar]
- 19. Gamma AE, Slekiene J, von Medeazza G, Asplund F, Cardoso P, Mosler HJ.. Contextual and psychosocial factors predicting Ebola prevention behaviors using the RANAS approach to behavior change in Guinea-Bissau. BMC Public Health 2017; 17:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang CQ, Zhang R, Schwarzer R, Hagger MS.. A meta-analysis of the health action process approach. Health Psycho. 2019; 38:623. [DOI] [PubMed] [Google Scholar]
- 21. Dwipayanti NM, Lubis DS, Harjana NP.. Public perception and hand hygiene behavior during COVID-19 pandemic in Indonesia. Front Public Health. 2021; 9:543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gamma AE, Slekiene J, Mosler HJ.. The impact of various promotional activities on Ebola prevention behaviors and psychosocial factors predicting Ebola prevention behaviors in the Gambia evaluation of Ebola prevention promotions. Int J Environ Res Public Health. 2019; 16:2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Latkin CA, Dayton L, Kaufman MR, Schneider KE, Strickland JC, Konstantopoulos A.. Social norms and prevention behaviors in the United States early in the COVID-19 pandemic. Psycho, Health Med. 2021; 27:1–6. [DOI] [PubMed] [Google Scholar]
- 24. Amireault S, Godin G, Vézina-Im LA.. Determinants of physical activity maintenance: A systematic review and meta-analyses. Health Psych Rev. 2013; 7:55–91. [Google Scholar]
- 25. Duan Y, Shang B, Liang W, et al. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the covid-19 pandemic: An integrated social cognition model. BMC Geriatr. 2022; 22:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu HX, Chow BC, Liang W, Hassel H, Huang YW.. Measuring a broad spectrum of eHealth skills in the Web 3.0 context using an eHealth Literacy Scale: Development and validation study. J Med Internet Res. 2021; 23:e31627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Noone C, Warner NZ, Byrne M, et al. A scoping review of research on the determinants of adherence to social distancing measures during the COVID-19 pandemic. Health Psycho Rev. 2021; 15:350–370. [DOI] [PubMed] [Google Scholar]
- 28. Contzen N, Meili IH, Mosler HJ.. Changing handwashing behavior in southern Ethiopia: A longitudinal study on infrastructural and commitment interventions. Soc Sci Med. 2015; 124:103–114. [DOI] [PubMed] [Google Scholar]
- 29. Duan Y, Li X, Guo L, Liang W, Shang B, Lippke S.. A WeChat mini program-based intervention for physical activity, fruit and vegetable consumption among Chinese cardiovascular patients in home-based rehabilitation: A study protocol. Front Public Health. 2022; 10:739100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Duan Y, Hu C, Lin Z, et al. Individual preventive behaviors of COVID-19 and associated psychological factors among Chinese older adults: A cross-sectional online survey. Front Psycho. 2022; 13:827152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Inauen J, Lilje J, Mosler HJ.. Refining hand washing interventions by identifying active ingredients: A cluster-randomized controlled trial in rural Zimbabwe. Soc Sci Med. 2020; 245:112712. [DOI] [PubMed] [Google Scholar]
- 32. Seimetz E, Slekiene J, Friedrich MN, Mosler HJ.. Identifying behavioral determinants for interventions to increase handwashing practices among primary school children in rural Burundi and urban Zimbabwe. BMC Res Notes 2017; 10:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. AlAmodi AA, Al-Kattan K, Shareef MA.. The current global perspective of the knowledge-attitude-behavior of the general public towards the corona virus disease-19 pandemic: Systematic review and meta-analysis on 67,143 participants. PLoS One. 2021; 16:e0260240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rincón Uribe FA, Godinho RC, Machado MA, et al. Health knowledge, health behaviors and attitudes during pandemic emergencies: A systematic review. PLoS One. 2021; 16:e0256731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sarria-Guzmán Y, Fusaro C, Bernal JE, Mosso-González C, González-Jiménez FE, Serrano-Silva N.. Knowledge, Attitude and Practices (KAP) towards COVID-19 pandemic in America: A preliminary systematic review. J Infect Dev Ctries. 2021; 15:9–21. [DOI] [PubMed] [Google Scholar]
- 36. Shushtari ZJ, Salimi Y, Ahmadi S, et al. Social determinants of adherence to COVID-19 preventive guidelines: A comprehensive review. Osong Public Health Res Perspect. 2021; 12:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Regmi K, Lwin CM.. Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): A systematic review. Int J Environ Res Public Health. 2021; 18:4274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Duan Y, Lippke S, Liang W, et al. Association of social-cognitive factors with individual preventive behaviors of Covid-19 among a mixed-sample of older adults from China and Germany. Int J Environ Res Public Health. 2022; 19:6364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kumar S, Loughnan L, Luyendijk R, et al. Handwashing in 51 countries: Analysis of proxy measures of handwashing behavior in multiple indicator cluster surveys and demographic and health surveys, 2010–2013. Am J Trop Med Hyg. 2017; 97:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pogrebna G, Kharlamov A.. The impact of cross-cultural differences in handwashing patterns on the COVID-19 outbreak magnitude. Regul Gov. 2020; 10:1–8. [Google Scholar]
- 41. Ali M, Uddin Z, Banik PC, et al. Knowledge, attitude, practice, and fear of COVID-19: An online-based cross-cultural study. Int J Ment Health Addict. 2021; 30:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bacon SL, Revenson TA.. Introduction to the special section: The importance of behavioral medicine in the COVID-19 pandemic response. Ann Behav Med. 2022; 56:321–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst Rev. 2021; 10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Janz National Institute of Health. Quality assessment tool for observational cohort and cross-sectional studies. Bethesda, MD: The National Heart, Lung, and Blood Institute. Available at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessibility verified July 18, 2022. [Google Scholar]
- 45. Okoli GN, Lam OL, Racovitan F, et al. Seasonal influenza vaccination in older people: A systematic review and meta-analysis of the determining factors. PLoS One. 2020; 15:e0234702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R.. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol. 2020; 126:37–44. [DOI] [PubMed] [Google Scholar]
- 47. Williams G, Hamm MP, Shulhan J, Vandermeer B, Hartling L.. Social media interventions for diet and exercise behaviours: A systematic review and meta-analysis of randomized controlled trials. BMJ Open 2014; 4:e003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Austin PC, Steyerberg EW.. Interpreting the concordance statistic of a logistic regression model: Relation to the variance and odds ratio of a continuous explanatory variable. BMC Med Res Methodol. 2012; 12:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. DeCoster J. Converting effect sizes Microsoft Excel Spreadsheets. Stat-Help, 2012. Available at http://www.stat-help.com/spreadsheets.html. Accessibility verified July 18, 2022.
- 50. Duan Y, Shang B, Liang W, Du G, Yang M, Rhodes RE.. Effects of eHealth-based multiple health behavior change interventions on physical activity, healthy diet, and weight in people with noncommunicable diseases: Systematic review and meta-analysis. J Med Internet Res. 2021; 23:e23786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Higgins JP, Thompson SG, Deeks JJ, Altman DG.. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Egger M, Smith GD, Schneider M, Minder C.. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cochrane Library. Chapter 10: Analyzing data and undertaking meta-analyses. Cochrane Training. Available at https://training.cochrane.org/handbook/current/chapter-10. Accessibility verified July 18, 2022.
- 54. Norman P, Wilding S, Conner M.. Reasoned action approach and compliance with recommended behaviours to prevent the transmission of the SARS-CoV-2 virus in the UK. Br J Health Psychol. 2020; 25:1006–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Barrett C, Cheung KL.. Knowledge, socio-cognitive perceptions and the practice of hand hygiene and social distancing during the COVID-19 pandemic: A cross-sectional study of UK university students. BMC Public Health 2021; 21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lu P, Kong D, Shelley M.. Risk Perception, preventive behavior, and medical care avoidance among American older adults during the COVID-19 pandemic. J Aging Health. 2021; 33:577–584. [DOI] [PubMed] [Google Scholar]
- 57. Bogg T, Milad E.. Demographic, personality, and social cognition correlates of coronavirus guideline adherence in a US sample. Health Psycho. 2020; 39:1026. [DOI] [PubMed] [Google Scholar]
- 58. Aschwanden D, Strickhouser JE, Sesker AA, et al. Preventive behaviors during the COVID-19 pandemic: Associations with perceived behavioral control, attitudes, and subjective norm. Front Public Health. 2021; 9:492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hermans L, Van den Broucke S, Gisle L, Demarest S, Charafeddine R.. Mental health, compliance with measures and health prospects during the COVID-19 epidemic: The role of health literacy. BMC Public Health 2021; 21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Barile JP, Guerin RJ, Fisher KA, et al. Theory-based behavioral predictors of self-reported use of face coverings in public settings during the COVID-19 pandemic in the United States. Ann Behav Med. 2021; 55:82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tong KK, Chen JH, Yu EW, Wu AM.. Adherence to COVID-19 precautionary measures: Applying the health belief model and generalized social beliefs to a probability community sample. Appl Psychol Health Well-Being. 2020; 12:1205–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kwan RY, Lee PH, Cheung DS, Lam SC.. Face mask wearing behaviors, depressive symptoms, and health beliefs among older people during the COVID-19 pandemic. Front Med. 2021; 8:590936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ozdemir S, Ng S, Chaudhry I, Finkelstein EA.. Adoption of preventive behavior strategies and public perceptions about COVID-19 in Singapore. Int J Health Policy Manage. 2020; 11:579–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gibson LP, Magnan RE, Kramer EB, Bryan AD.. Theory of planned behavior analysis of social distancing during the COVID-19 pandemic: Focusing on the intention–behavior gap. Ann Behav Med. 2021; 55:805–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hagger MS, Smith SR, Keech JJ, Moyers SA, Hamilton K.. Predicting social distancing intention and behavior during the COVID-19 pandemic: An integrated social cognition model. Ann Behav Med. 2020; 54:713–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Beeckman M, De Paepe A, Van Alboom M, et al. Adherence to the physical distancing measures during the covid-19 pandemic: A HAPA-based perspective. Appl Psychol Health Well-Being. 2020; 12:1224–1243. [DOI] [PubMed] [Google Scholar]
- 67. Hills S, Eraso Y.. Factors associated with non-adherence to social distancing rules during the COVID-19 pandemic: A logistic regression analysis. BMC Public Health 2021; 21:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Badr H, Oluyomi A, Woodard L, et al. Sociodemographic and health belief model factors associated with nonadherence to COVID-19 mitigation strategies in the United States. Ann Behav Med. 2021; 55:677–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Gratz KL, Richmond JR, Woods SE, et al. Adherence to social distancing guidelines throughout the COVID-19 pandemic: The roles of pseudoscientific beliefs, trust, political party affiliation, and risk perceptions. Ann Behav Med. 2021; 55:399–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lithopoulos A, Liu S, Zhang CQ, Rhodes RE.. Predicting physical distancing in the context of COVID-19: A test of the extended parallel process model among Canadian adults. Can Psychol. 2021; 62:56. [Google Scholar]
- 71. Hamilton K, Smith SR, Keech JJ, Moyers SA, Hagger MS.. Application of the health action process approach to social distancing behavior during COVID-19. Appl Psychol Health Well-Being. 2020; 12:1244–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Rhodes RE, Boudreau P, Josefsson KW, Ivarsson A.. Mediators of physical activity behaviour change interventions among adults: A systematic review and meta-analysis. Health Psycho Rev. 2021; 15:272–286. [DOI] [PubMed] [Google Scholar]
- 73. Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH.. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005; 131:856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Carpenter CA. meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010; 25:661–669. [DOI] [PubMed] [Google Scholar]
- 75. Noar SM, Benac CN, Harris MS.. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007; 133:673. [DOI] [PubMed] [Google Scholar]
- 76. Abdullahi L, Onyango JJ, Mukiira C, et al. Community interventions in low—and middle-income Countries to inform COVID-19 control implementation decisions in Kenya: A rapid systematic review. PLoS One. 2020; 15:e0242403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sridhar S, Ho PL.. COVID-19 outbreak in Hong Kong: Public health, surgical masks, and hand hygiene. Am J Public Health. 2020; 110:941–942. [Google Scholar]
- 78. Severin WJ, Tankard JW.. Communication Theories: Origins, Methods, and Uses in the Mass Media. New York: Longman; 1997. [Google Scholar]
- 79. Rhodes RE. Chapter Five - The evolving understanding of physical activity behavior: A multi-process action control approach. In: Elliot AJ, ed. Advances in Motivation Science, Vol. 4. Elsevier; 2017:171–205. ISSN ; ISBN 9780128121238. doi: 10.1016/bs.adms.2016.11.001. [DOI] [Google Scholar]
- 80. Phipps DJ, Hannan TE, Rhodes RE, Hamilton K.. A dual-process model of affective and instrumental attitudes in predicting physical activity. Psychol Sport Exerc. 2021; 54:101899. [Google Scholar]
- 81. Rhodes RE, McEwan D, Rebar AL.. Theories of physical activity behavior change: A history and synthesis of approaches. Psychol Sport Exerc. 2019; 42:100–109. [Google Scholar]
- 82. McEachan RR, Conner M, Taylor NJ, Lawton RJ.. Prospective prediction of health-related behavoirs with the theory of planned behavior: A meta-analysis. Health Psychol Rev. 2011; 5:97–144. [Google Scholar]
- 83. Hagger MS, Chan DK, Protogerou C, Chatzisarantis NL.. Using meta-analytic path analysis to test theoretical predictions in health behavior: An illustration based on meta-analyses of the theory of planned behavior. Prev Med. 2016; 89:154–161. [DOI] [PubMed] [Google Scholar]
- 84. Lin N, Roberts KR.. Using the theory of planned behavior to predict food safety behavioral intention: A systematic review and meta-analysis. Int J Hosp Manag. 2020; 90:102612. [Google Scholar]
- 85. Niemiec RM, Champine V, Vaske JJ, Mertens A.. Does the impact of norms vary by type of norm and type of conservation behavior? A meta-analysis. Soc Nat Resour. 2020; 33:1024–1040. [Google Scholar]
- 86. Williams DM, Rhodes RE.. The confounded self-efficacy construct: Conceptual analysis and recommendations for future research. Health Psychol Rev. 2016; 10:113–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Annett J. Subjective rating scales: Science or art? Ergonomics 2002; 45:966–987. [DOI] [PubMed] [Google Scholar]
- 88. Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990; 43:87–91. [DOI] [PubMed] [Google Scholar]
- 89. Lee M, You M.. Effects of COVID-19 emergency alert text messages on practicing preventive behaviors: Cross-sectional web-based survey in South Korea. J Med Internet Res. 2021; 23:e24165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.