Abstract
A CD8+ cytolytic T-lymphocyte (CTL) response to antigen-presenting cells generally requires intracellular delivery or synthesis of antigens in order to access the major histocompatibility complex (MHC) class I processing and presentation pathway. To test the ability of pertussis toxin (PT) to deliver peptides to the class I pathway for CTL recognition, we constructed fusions of CTL epitope peptides with a genetically detoxified derivative of PT (PT9K/129G). Two sites on the A (S1) subunit of PT9K/129G tolerated the insertion of peptides, allowing efficient assembly and secretion of the holotoxin fusion by Bordetella pertussis. Target cells incubated with these fusion proteins were specifically lysed by CTLs in vitro, and this activity was shown to be MHC class I restricted. The activity was inhibited by brefeldin A, suggesting a dependence on intracellular trafficking events, but was not inhibited by the proteasome inhibitors lactacystin and N-acetyl-l-leucyl-l-leucyl-l-norleucinal (LLnL). Furthermore, the activity was present in mutant antigen-presenting cells lacking the transporter associated with antigen processing, which transports peptides from the cytosol to the endoplasmic reticulum for association with MHC class I molecules. PT may therefore bypass the proteasome-dependent cytosolic pathway for antigen presentation and deliver epitopes to class I molecules via an alternative route.
CD8+ cytolytic T lymphocytes (CTL) are a subset of T cells that can recognize and kill host cells expressing foreign antigens and that can protect experimental animals from lethal viral or parasitic infections (26, 28). CTL recognize antigens as short peptides of 8 to 11 amino acids (aa) in association with major histocompatibility complex (MHC) class I molecules on the surfaces of infected cells (2). These peptide epitopes are generally derived from cytosolic proteins that are proteolytically processed by proteasomes and transported by the transporter associated with antigen processing (TAP) proteins to the endoplasmic reticulum (ER), where they associate with class I molecules (13). While this endogenous pathway accounts for the majority of class I-restricted CTL responses, alternative pathways for class I presentation of exogenous antigens have been described but are poorly characterized (for reviews, see references 17 and 23). For peptide-based vaccines intended to prime specific CTL, peptides must be delivered to an MHC class I presentation pathway for recognition by the CTL. Here we describe the initial development and characterization of a detoxified bacterial toxin as the delivery molecule.
Pertussis toxin (PT), a major virulence factor of Bordetella pertussis, consists of five different subunits (S1 through S5) that are assembled into the holotoxin in the bacterial periplasm and then secreted into the external medium (49). The A subunit of PT (S1) ADP-ribosylates the α subunits of several membrane-associated G proteins in eukaryotic cells (30, 57), and the B oligomer (S2 through S5) binds glycoconjugate receptors on cells (40). The intracellular trafficking of PT between surface binding and target protein modification appears to involve a retrograde transport through endosomes and the Golgi apparatus (7, 8, 57, 58), and possibly also the ER (19, 20), before transport of at least S1 across the plasma membrane. A genetically detoxified PT molecule called PT9K/129G (referred to below as PT*), with mutations in two active site residues of S1, was completely deficient in enzymatic and toxic activities but retained B oligomer-associated properties and immunogenicity in mice (31, 36). It was protective for mice challenged with virulent B. pertussis (36), and an acellular pertussis vaccine including this molecule was safe and highly efficacious in a phase III trial (15). As a first step in the development of PT* as a possible vaccine vector molecule for epitope delivery and stimulation of CTL responses, we report here the construction of toxin-peptide fusion molecules that are stably assembled and secreted by B. pertussis and the ability of these fusion molecules to sensitize target cells to MHC class I-restricted CTL lysis in vitro.
MATERIALS AND METHODS
Bacterial growth.
B. pertussis was grown on Bordet-Gengou agar supplemented with 15% sheep blood or in Stainer-Scholte medium (45) with 0.1% heptakis(2,6-O-dimethyl)-β-cyclodextrin (Sigma). When necessary, antibiotics were added to the following final concentrations: streptomycin, 400 μg/ml; nalidixic acid, 20 μg/ml; gentamicin, 10 μg/ml; and kanamycin, 50 μg/ml, Escherichia coli was grown on Luria-Bertani agar, with the addition of 100 μg of ampicillin/ml when necessary.
Reagents.
Restriction endonucleases and DNA-modifying enzymes were from New England Biolabs or Stratagene. Oligonucleotides were synthesized on an Applied Biosystems DNA Synthesizer, model 380B, and automated DNA sequencing was performed on an Applied Biosystems DNA Sequencer, model 373A. Peptides were synthesized on a Rainin/Protein Technologies Symphony multiplex peptide synthesizer. Fetuin-agarose, brefeldin A (BFA), and N-acetyl-l-leucyl-l-leucyl-l-norleucinal (LLnL) were from Sigma, and lactacystin was purchased from E. J. Corey (Harvard University).
Construction of PT*-peptide fusions.
Fusions with insertions of peptides at specific locations on the S1 subunit of PT* were constructed genetically by overlap extension PCR (21). Oligonucleotides were designed to encode the epitope by using B. pertussis codon preference (53). PCR-generated fusion fragments were ligated into KpnI/XbaI-digested pS-PT (a 4.7-kb EcoRI fragment containing the ptx genes inserted into the allelic exchange vector pSS1129 [48]), transformed into E. coli S17.1 (43), and introduced into the chromosome of B. pertussis W28 by conjugation and allelic exchange as previously described (16, 47). DNA sequencing of the fusion-containing plasmid was performed to confirm the correct insertion of the peptide-encoding sequence, and PCR was used to confirm the correct insertion of the fusion into the chromosome of B. pertussis.
Assay for secretion of PT*-peptide fusions by B. pertussis.
Secretion of PT*-peptide fusions by B. pertussis was assessed by Western immunoblotting of trichloroacetic acid (TCA)-precipitated supernatant proteins. Detection of the S1 subunit in B. pertussis culture supernatants represents a convenient method of assaying for holotoxin assembly and secretion, since S1 is never secreted alone, and subtle changes in S1 that may disrupt correct assembly of the holotoxin result in the absence of detectable S1 in the supernatant (35). B. pertussis strains carrying the fusions were grown in 10-ml cultures for 24 h (to an A600 of 1.0 to 1.5). The supernatant was collected by centrifugation and filter sterilization, and proteins were precipitated by the addition of 200 μl of 2% sodium deoxycholate and 4 ml of 24% TCA. Precipitated protein was pelleted by centrifugation and resuspended in 1 M Tris-HCl (pH 7)–0.5 N NaOH in a volume standardized against the A600 of the overnight culture (100 μl × A600). Sample buffer was added, and samples were run on a sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gel (15% polyacrylamide) and transferred to nitrocellulose by Western blotting. The S1 subunit was detected with an S1-specific monoclonal antibody, either X2X5 or 3CX4 (both kindly provided by Drusilla Burns, U.S. Food and Drug Administration) or 6G7 (kindly provided by Rino Rappuoli, Istituto Richerche Immunobiologiche Siena), a peroxidase-conjugated secondary antibody (Boehringer Mannheim), and ECL development (Amersham).
Purification of PT*-peptide fusions.
Three-liter cultures of B. pertussis strains secreting the fusion proteins were grown in shake flasks at 35°C for approximately 65 h to an A600 of 2 to 3. PT*-peptide fusion proteins were purified from the culture supernatants by batch chromatography with fetuin-agarose according to the method of Kimura et al. (27). The concentration of protein in purified samples was determined by a Bradford assay (3), and the purity was assessed by Coomassie blue staining of SDS-PAGE gels.
Cell lines.
The CTL clone HD8 (56) was obtained from Michael Oldstone (Scripps Research Institute). HD8 was maintained in RPMI 1640 medium supplemented with 10% fetal bovine serum, 2 mM glutamine, 50 μM 2-mercaptoethanol, 1 mM sodium pyruvate, 50 μg of gentamicin sulfate/ml, 40 U of interleukin 2/ml, 200 μM nucleoprotein (NP) 118-126 peptide, and 1.5 × 106 irradiated (3,000 rads) BALB/c splenocytes/ml, and cells were split 1:2 every 7 days. Target cells for CTL lysis assays were DBA/2 mouse mastocytoma P815 cells (H-2d) (American Type Culture Collection [ATCC]), mouse thymoma EL4 cells (H-2b) (ATCC), and RMAS-Ld (24, 50) and T2-Ld cells (5, 38), TAP-deficient mouse and human cell lines, respectively, transfected with Ld (kindly provided by Jonathan Schneck, Johns Hopkins University). Target cells were maintained in RPMI 1640 medium supplemented with 10% fetal bovine serum, 2 mM glutamine, 50 μM 2-mercaptoethanol, 1 mM sodium pyruvate, and 50 μg of gentamicin sulfate/ml.
CTL lysis assay.
Target cells (5 × 106) were labelled with 200 μCi of 51Cr (DuPont, NEN) in 200 μl of fetal bovine serum for 1 h at 37°C. Cells were washed and resuspended in complete medium at a final concentration of 1 × 105 cells/ml. HD8 CTL clones were harvested, washed three times, and resuspended to give the desired effector-to-target (E/T) ratio in a final volume of 200 μl. Peptide, fusion protein, and/or inhibitor was added, and the samples were incubated for 6 h at 37°C in 6% CO2. After incubation, 100 μl of each sample supernatant was removed and counted in a Beckman gamma counter. Percent specific lysis was calculated as [(experimental release − spontaneous release)/(maximum release − spontaneous release)] × 100. All data are means of triplicate samples.
Flow cytometry.
Flow cytometry was carried out as previously described (50) by using a FACS Calibur (Becton Dickinson Immunocytometry Services, San Jose, Calif.) flow cytometer. Ld was detected with monoclonal antibody 30-5-7 (34). Where appropriate, peptides were titrated in 1/2 log dilutions between 0.1 and 1,000 ng/ml. Data were acquired on 5,000 cells as judged by light scatter and analyzed by CellQuest (BDIS) or FlowJo (Treestar, Inc., San Carlos, Calif.).
RESULTS
Two sites on S1 tolerate insertion of peptides for assembly and secretion of PT*-peptide holotoxin fusions by B. pertussis.
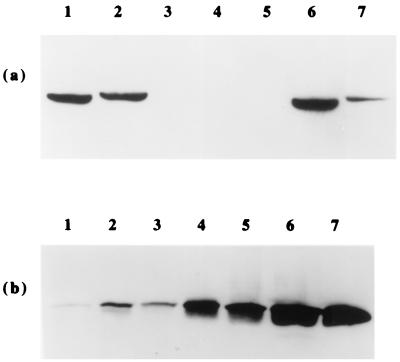
Examination of the crystal structure of PT (46) allowed the identification of external, potentially flexible loops on S1 as candidate tolerant sites for insertion of peptides. These sites were between aa 1 and 2, 28 and 29, 45 and 46, 134 and 135, and 180 and 181. The locations of the aa 1-to-2 and 180-to-181 sites are shown in Fig. 1. We inserted the sequence encoding the 9-aa lymphocytic choriomeningitis virus (LCMV) NP118-126 epitope (Table 1) at each of these sites on S1. In addition, we inserted two other CTL epitope peptides (Table 1) at one or more of these sites. To determine whether assembly and secretion of holotoxin were maintained after insertion of the peptides into S1, we assayed for the presence of S1 in B. pertussis culture supernatants. Insertion of the LCMV NP118-126 peptide was tolerated between aa 1 and 2 and between aa 180 and 181, giving reasonable yields of secreted fusion protein (Fig. 2a). However, the other sites did not tolerate insertion of this peptide, resulting in the absence of S1 in the supernatant (Fig. 2a). To confirm that the lack of detectable S1 was due to nonsecretion rather than loss of the X2X5 epitope after insertion of the peptide, we repeated the immunoblotting with two other S1-specific monoclonal antibodies that recognize different epitopes and obtained the same results (data not shown). In addition, the aa 28-to-29 and 134-to-135 sites did not tolerate the insertion of the Plasmodium yoelii CSP281-289 peptide, demonstrating that insertions into some external locations are still disruptive for the assembly and secretion of holotoxin. The yield of secreted fusion protein with the peptide inserted between aa 180 and 181 was relatively low (Fig. 2a). To test this site further, we inserted the P. yoelii CSP281-289 and LCMV GP33-41 peptide epitopes between aa 180 and 181. Both peptides were tolerated extremely well, allowing high-yield secretion of the fusion proteins (Fig. 2b). These peptides were also inserted between aa 1 and 2 (at the N terminus of the mature S1 subunit), resulting in high-yield secretion of the fusion proteins (data not shown). These sites therefore represent generally tolerant insertion sites, although the yield of fusion protein depends on the peptide sequence inserted.
FIG. 1.
Alpha carbon drawings of the crystal structure of PT, with the S1 subunit on top of the B oligomer. (a) Side view, with aa 180 and 181 of S1 highlighted as spheres. (b) Side view rotated 90° with respect to the view in panel a, showing aa 2 (the N-terminal amino acid is absent from the crystal structure) of S1 highlighted as spheres.
TABLE 1.
CTL epitopes inserted into PT*
| Epitope | Amino acid sequence | DNA sequence (5′→3′)a | MHC class I element | Reference(s) |
|---|---|---|---|---|
| LCMV NP118-126 | RPQASGVYM | CGCCCGCAGGCCAGCGGCGTGTACATG | Ld | 12, 33 |
| LCMV GP33-41 | KAVYNFATC | AAGGCCGTGTACAACTTCGCCACCTGC | Dd | 12 |
| P. yoelii CSP281-289 | SYVPSAEQI | AGCTACGTACCGAGCGCGGAGCAGATC | Kd | 54 |
Synthetically derived epitope-encoding sequence inserted into the S1 gene by overlap extension PCR.
FIG. 2.
Western immunoblots showing the secretion of PT*-peptide fusion proteins by B. pertussis W28, by detection of the S1 subunit with monoclonal antibody X2X5. (a) Twenty percent of total TCA-precipitated supernatant proteins were loaded in each well. Lanes: 1, PT* (no insertion); 2, PT*-NP/N; 3, PT*-NP/28; 4, PT*-NP/45; 5, PT*-NP/134; 6, PT* (no insertion); 7, PT*-NP/180. (b) The percentage of total TCA-precipitated supernatant proteins loaded in each well is as follows. Lanes: 1, PT*-NP/180 (5%); 2, PT*-NP/180 (20%); 3, PT*-CSP/180 (5%); 4, PT*-CSP/180 (20%); 5, PT*-GP/180 (5%); 6, PT*-GP/180 (20%); 7, PT* (no insertion) (20%).
We purified the fusion proteins with the NP118-126 peptide inserted either at the N terminus (PT*-NP/N) or between aa 180 and 181 (PT*-NP/180) from B. pertussis culture supernatants. The yields of fusion protein were approximately 80 and 30 μg per liter of culture, respectively. SDS-PAGE analysis revealed that the S1 subunit of the fusion proteins was correspondingly larger (about 1 kDa) than the S1 subunit of PT*, and there appeared to be the same stoichiometry of subunits as in PT* (data not shown), suggesting that there was little free B oligomer in the preparation and that the holotoxin structure was stable.
Target cells incubated with PT*-NP/N fusion protein are sensitized to lysis by NP-specific CTL.
51Cr-labelled P815 target cells were incubated with peptide or fusion protein and HD8 (NP118-126-specific, Ld-restricted) CTL at various E/T ratios in a 6-h 51Cr release assay. Target cells incubated with NP118-126 peptide were efficiently lysed by the CTL (Fig. 3), whereas incubation with the CSP281-289 peptide gave background levels of lysis (<5%) (data not shown), demonstrating the specificity of the CTL clone. Target cells incubated with the PT*-NP/N fusion protein were also efficiently lysed by the CTL (Fig. 3). Incubation with PT* or buffer alone (Fig. 3), or without CTL added (data not shown), resulted in negligible lysis of target cells, demonstrating that the presence of the epitope on the fusion protein was necessary for the activity and that the fusion protein itself was not lysing target cells. When the fusion protein was boiled for 20 min (which denatures the holotoxin into its separate subunits) prior to addition to the target cells, no lysis by the CTL was observed (Fig. 3). Boiling of the NP118-126 peptide had no significant effect on its ability to sensitize target cells to lysis (data not shown). This demonstrates that intact holotoxin is necessary for sensitization of targets to CTL lysis. In addition, when EL4 (H-2b) target cells were used in similar assays, negligible lysis (<5%) was observed after incubation with NP118-126 peptide or PT*-NP/N protein (data not shown), demonstrating that the response is MHC restricted, occurring in H-2d but not H-2b cells.
FIG. 3.
Lysis by the NP-specific CTL clone HD8 of 51Cr-labelled P815 target cells incubated with PT*-NP/N (or control protein or peptide). Protein or peptide additions included the indicated amounts of PT*-NP/N, 200 ng of boiled PT*-NP/N, 200 ng of PT*, or 10 ng of NP118-126 peptide. See the text for experimental details. Data are means of triplicate samples and are representative of several experiments with similar results.
Sensitization of target cells by PT*-NP/N to CTL lysis is inhibited by BFA but not by proteasome inhibitors.
The observation that denatured (boiled) PT*-NP/N was unable to sensitize target cells to CTL lysis suggests that intracellular events, after the binding and entry of holotoxin, are necessary for this activity, rather than extracellular release of the peptide for binding to surface class I molecules. To investigate this hypothesis further, we repeated the lysis assay in the presence of the inhibitor BFA, which disrupts the Golgi apparatus and inhibits both the trafficking of PT in cells (7, 8, 57, 58) and the secretion of nascent class I molecule-peptide complexes to the cell surface (32, 59). As shown in Fig. 4, the addition of 10 μg of BFA/ml to target cells incubated with PT*-NP/N greatly reduced CTL lysis. BFA had no significant effect on CTL lysis of target cells incubated with NP118-126 peptide (Fig. 4), demonstrating that the inhibitory effect was not exerted directly on the activity of the CTL. This strongly suggests that sensitization of target cells by PT*-NP/N to CTL lysis depends on internalization of the fusion protein for delivery of the peptide to class I molecules. To determine whether peptide delivery to class I molecules occurred by the cytosolic pathway of antigen processing, we repeated the lysis assay in the presence of the proteasome inhibitor lactacystin (11), which can prevent class I presentation of peptides derived from this pathway (4, 52). As shown in Fig. 4, addition of 10 μM lactacystin did not inhibit the sensitization of target cells incubated with either NP118-126 peptide or PT*-NP/N fusion protein. The same effect was observed with an alternative proteasome inhibitor, LLnL (100 μM) (37), in the lysis assay ( data not shown). Lactacystin and BFA both reduced surface expression of Ld class I molecules on P815 cells, as measured by flow cytometry using the anti-Ld mouse immunoglobulin G2a monoclonal antibody 30-5-7 (34), with 72 and 52% decreases, respectively, in median channel fluorescence after 4 h of culture (data not shown), demonstrating their efficacy in inhibition of MHC class I processing and presentation. We conclude from these data that the proteasome is not involved in the processing of PT*-NP/N for class I presentation of the peptide.
FIG. 4.
Lysis by the NP-specific CTL clone HD8 of 51Cr-labelled P815 target cells incubated with PT*-NP/N (200 ng) or NP118-126 peptide (10 ng) in the presence or absence of inhibitors. Inhibitors were BFA (10 μg/ml) and lactacystin (10 μM). See the text for experimental details. Data are means of triplicate samples and are representative of several experiments with similar results.
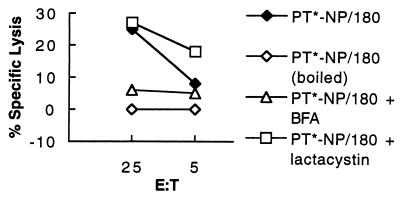
PT*-NP/180 sensitizes target cells to CTL lysis in the same manner as PT*-NP/N.
To determine whether the effects seen with PT*-NP/N were due to the location of the peptide at the N terminus of S1, we repeated the lysis assays with the PT*-NP/180 fusion protein and HD8 CTL. As shown in Fig. 5, PT*-NP/180 was also able to sensitize P815 target cells to specific CTL lysis. Boiling of PT*-NP/180 abolished this activity (Fig. 5), and the same pattern of effects was observed with the inhibitors: the activity was significantly reduced by BFA but insensitive to lactacystin (Fig. 5). This demonstrates that insertion of the peptide at an alternative location in S1 maintains the ability of the fusion protein to sensitize target cells to CTL lysis (although the efficiency may be affected) and that processing of the two fusion proteins apparently occurs by the same BFA-sensitive and proteasome-independent pathway.
FIG. 5.
Lysis by the NP-specific CTL clone HD8 of 51Cr-labelled P815 target cells incubated with PT*-NP/180 (200 ng) in the presence or absence of inhibitors. Inhibitors were BFA used at 10 μg/ml and lactacystin used at 10 μM. See the text for experimental details. Data are means of triplicate samples and are representative of several experiments with similar results.
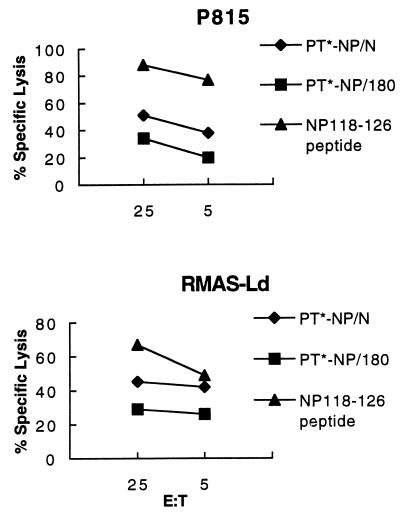
Sensitization of target cells by PT*-NP fusion proteins to CTL lysis is independent of the TAP peptide transporter.
The previous data suggest that a noncytosolic pathway of antigen processing may be utilized by the PT*-NP fusion proteins for intracellular delivery of peptides to class I molecules. A prediction of this hypothesis is that processing of the fusion proteins, and subsequent sensitization of target cells to CTL lysis, would be independent of the TAP peptide transporter, which mediates transport of proteasome-generated class I-restricted peptides from the cytosol to the ER (25, 44). To test this prediction, we used in the CTL lysis assay a TAP-deficient target cell line, RMAS, transfected with the class I molecule Ld (which presents the NP118-126 peptide). As shown in Fig. 6, the ability of both PT*-NP/N and PT*-NP/180 to sensitize the TAP-deficient target cells to CTL lysis was similar to their activity on target cells with functional TAP (P815 cells). The activity was inhibited by BFA (data not shown), and no specific lysis was observed in the absence of peptide or fusion protein or in the absence of CTL (data not shown). The same level of activity was observed when a second TAP-deficient target cell line (T2-Ld) was used in the lysis assay (data not shown). To confirm the phenotype of the TAP-deficient target cells, we analyzed by flow cytometry the surface expression of Ld on these cells when they were incubated with and without NP118-126 peptide (1 μg) for 6 h at 37°C. Addition of peptide significantly increased the low level of surface Ld on the TAP-deficient cells (a 5.7-fold increase in median channel fluorescence) (data not shown) but did not increase the higher level on P815 cells, confirming their TAP-deficient phenotype. From these data we conclude that processing of the PT*-NP fusion proteins for delivery of the peptide to class I molecules occurs via a TAP-independent pathway.
FIG. 6.
Lysis by the NP-specific CTL clone HD8 of 51Cr-labelled target cells with functional or nonfunctional TAP proteins incubated with PT*-NP fusion proteins (200 ng) or NP118-126 peptide (10 ng). See the text for experimental details. Data are means of triplicate samples and are representative of several experiments with similar results.
DISCUSSION
The results of this study demonstrate that fusions of minimal CTL epitope peptides with the S1 subunit of PT* can be stably assembled and secreted as holotoxin by B. pertussis and that these fusion molecules can sensitize target cells to lysis by peptide-specific CTL in vitro. This activity is (i) MHC class I restricted, (ii) dependent on the presence of intact holotoxin, (iii) sensitive to the inhibitor (of Golgi-associated trafficking) BFA, (iv) resistant to the proteasome inhibitors lactacystin and LLnL, and (v) independent of the TAP peptide transporter proteins. Our CTL lysis assay protocol of coincubation of fusion protein (or peptide), target cells, and CTL may underestimate the efficiency of the sensitizing activity of our fusion proteins, since the proteins may also enter and sensitize the CTL to lysis. We are currently attempting alternative protocols involving preincubation of target cells with fusion proteins to address this issue.
The BFA-sensitive nature of the epitope delivery activity by the fusion proteins (but not by control peptide) suggests that the pathway that PT* uses to deliver peptides to MHC class I molecules in target cells involves retrograde movement of the fusion molecules beyond the endosomal compartment, at least as far as the Golgi apparatus, but does not involve the proteasome- and TAP-dependent cytosolic pathway. These properties may distinguish this pathway from previously described alternative pathways for exogenous antigen processing and presentation by MHC class I molecules. For example, a proposed “phagosome-to-cytosol” pathway is dependent on proteasome and TAP functions (29), whereas the noncytosolic “vacuolar” pathway is insensitive to BFA (18). The processing pathway used by our PT*-peptide fusion proteins may simply be an inherent property of the intracellular trafficking of PT. PT is thought to be taken up by receptor-mediated endocytosis and then to move in a retrograde pathway through endosomes to the Golgi apparatus (7, 8, 57, 58). One group has proposed further retrograde transport to the ER, where ATP binding to the B oligomer alters the conformation and activates the enzymatic activity of the toxin (19, 20). The S1 subunit is then proposed to traverse the membrane, possibly utilizing an ER-associated protein degradation pathway for the removal of misfolded proteins, which are transported back to the cytosol for proteasome degradation (20, 55). The active S1 subunit, which may remain membrane associated (57), then ADP-ribosylates its target proteins, which include the α subunits of several membrane-associated G proteins (30, 57, 58). Our data are consistent with the idea of PT trafficking to the ER, where proteolysis of the fusion protein to release the class I-binding peptide may occur. The ER is known to contain proteases that can contribute to processing of proteins for class I presentation (9, 22). If S1 ultimately enters the cytosol, why is there no apparent cytosolic processing of the fusion protein? One possibility is that complete proteolytic release of the peptide has already occurred in the ER (or a previous compartment). Alternatively, the lack of lysines on S1 may allow it to avoid ubiquitination (ubiquitin attachment requires lysine residues) and therefore escape proteasome-dependent proteolysis and the cytosolic processing pathway (20). Further analyses with these fusion molecules may shed additional light on the cellular trafficking pathway used by PT.
Other bacterial toxins have been utilized as carriers for eliciting CTL responses. Epitopes fused to the binding and translocation domains of Pseudomonas exotoxin A sensitized cells to specific CTL lysis in vitro (6), but this activity was BFA resistant and TAP independent (51), suggesting a vacuolar processing pathway for class I presentation. Peptides fused to B. pertussis adenylate cyclase toxin also sensitized cells to specific CTL lysis in vitro (41), but the processing pathway of these fusion molecules was not investigated. However, the induction of efficient CTL responses in vivo by these fusions was dependent on the coadministration of alum (10), suggesting that a particulate nature of the fusion protein, and therefore an alternative processing pathway, was required. A fusion of a polypeptide to a truncated lethal factor component (LFn) of anthrax toxin also sensitized cells (in the presence of the cell-binding protective antigen component of the toxin) to in vitro lysis by CTL specific for an epitope on the polypeptide (14), and the sensitivity of this activity to lactacystin suggested that the cytosolic pathway of MHC class I antigen processing was used. The different properties of the MHC class I delivery activity of these various bacterial toxin-peptide fusions are most probably a reflection of the different pathways adopted by the toxins for cellular intoxication.
The relationship between the pathway of MHC class I processing and presentation for an antigen and its ability to stimulate protective immune responses is still unclear. Recombinant Listeria monocytogenes strains expressing either a secreted or a nonsecreted form of an LCMV NP118-126-containing fusion protein (which would presumably be processed by different pathways) were equally able to elicit protective CD8+ T-cell responses against LCMV infection (42). Fusions of peptides with both B. pertussis adenylate cyclase toxin and anthrax toxin LFn, which may follow different processing pathways, elicited CTL responses in mice and could protect mice against infection by the pathogen from which the peptide was derived (1, 39). This suggests that foreign carrier antigen delivery of peptides for class I presentation in vivo by either the cytosolic pathway or an alternative pathway can lead to protective CTL responses. We have preliminary data showing that two different PT*-peptide fusions elicit a strong CTL response in mice after a single immunization without adjuvant. Further investigation will determine whether this is a consistent property of PT*-peptide fusions and whether such responses are protective against challenge with the pathogen.
ACKNOWLEDGMENTS
We thank Rino Rappuoli for the opportunity to initiate this project and for reagents; Drusilla Burns, Michael Oldstone and Jonathan Schneck for reagents and cells; and Elena Rostapshova and Wei Dong for technical assistance. We also thank Antoinette Tishon and Michael Oldstone for help with some early experiments, Dave Maneval for advice on protein purification, and Jonathan Yewdell for advice on BFA.
This work was supported by an award from the University of Maryland School of Medicine and NIH grants AI38979 and AI42681 to N.H.C. and AI38192 to G.K.L.
REFERENCES
- 1.Ballard J D, Collier R J, Starnbach M N. Anthrax toxin-mediated delivery of a cytotoxic T-cell epitope in vivo. Proc Natl Acad Sci USA. 1996;93:12531–12534. doi: 10.1073/pnas.93.22.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barber L D, Parham P. Peptide binding to major histocompatibility molecules. Annu Rev Cell Biol. 1993;9:163–198. doi: 10.1146/annurev.cb.09.110193.001115. [DOI] [PubMed] [Google Scholar]
- 3.Bradford M M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 4.Craiu A, Gaczynska M, Akopian T, Gramm C, Fenteany G, Goldberg A L, Rock K L. Lactacystin and clasto-lactacystin beta-lactone modify multiple proteasome β subunits and inhibit intracellular protein degradation and major histocompatibility class I antigen processing. J Biol Chem. 1997;272:13437–13445. doi: 10.1074/jbc.272.20.13437. [DOI] [PubMed] [Google Scholar]
- 5.DeMars R, Rudersdorf R, Chang C, Petersen J, Strandtmann J, Korn N, Sidwell B, Orr H T. Mutations that impair a posttranscriptional step in expression of HLA-A and -B antigens. Proc Natl Acad Sci USA. 1985;82:8183–8187. doi: 10.1073/pnas.82.23.8183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly J J, Ulmer J B, Hawe L A, Friedman A, Shi X-P, Leander K R, Shiver J W, Oliff A I, Martinez D, Montgomery D, Liu M A. Targeted delivery of peptide epitopes to class I major histocompatibility molecules by a modified Pseudomonas exotoxin. Proc Natl Acad Sci USA. 1993;90:3530–3534. doi: 10.1073/pnas.90.8.3530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.el Baya A, Linnermann R, von Olleschik-Elbheim L, Schmidt M A. Pertussis toxin: entry into cells and enzymatic activity. Adv Exp Med Biol. 1997;419:83–86. [PubMed] [Google Scholar]
- 8.el Baya A, Linnermann R, von Olleschik-Elbheim L, Robenek H, Schmidt M A. Endocytosis and retrograde transport of pertussis toxin to the Golgi complex as a prerequisite for cellular intoxication. Eur J Cell Biol. 1997;73:40–48. [PubMed] [Google Scholar]
- 9.Elliott T, Willis A, Cerundolo V, Townsend A. Processing of major histocompatibility class I-restricted antigens in the endoplasmic reticulum. J Exp Med. 1995;181:1481–1491. doi: 10.1084/jem.181.4.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fayolle C, Sebo P, Ladant D, Ullmann A, Leclerc C. In vivo induction of CTL responses by recombinant adenylate cyclase of Bordetella pertussis carrying viral CD8+ T cell epitopes. J Immunol. 1996;156:4697–4706. [PubMed] [Google Scholar]
- 11.Fenteany G, Standaert R F, Lane W S, Choi S, Corey E J, Schreiber S L. Inhibition of proteasome activities and subunit-specific amino-terminal threonine modification by lactacystin. Science. 1995;268:726–731. doi: 10.1126/science.7732382. [DOI] [PubMed] [Google Scholar]
- 12.Gairin J E, Mazarguil H, Hudrisier D, Oldstone M B A. Optimal lymphocytic choriomeningitis virus sequences restricted by H-2Db-MHC class I molecules and presented to cytotoxic T lymphocytes. J Virol. 1995;69:2297–2305. doi: 10.1128/jvi.69.4.2297-2305.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Germain R N, Margulies D H. The biochemistry and cell biology of antigen processing and presentation. Annu Rev Immunol. 1993;11:403–450. doi: 10.1146/annurev.iy.11.040193.002155. [DOI] [PubMed] [Google Scholar]
- 14.Goletz T J, Klimpel K R, Arora N, Leppla S H, Keith J M, Berzofsky J A. Targeting HIV proteins to the major histocompatibility complex class I processing pathway with a novel gp120-anthrax toxin fusion protein. Proc Natl Acad Sci USA. 1997;94:12059–12064. doi: 10.1073/pnas.94.22.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greco D, Salmaso S, Mastrantonio P, Giuliano M, Tozzi A E, Anemona A, Ciofi degli Atti M L, Giammanco A, Panei P, Blackwelder W C, Klein D L, Wassilak S G the Progetto Pertosse Working Group. A controlled trial of two acellular vaccines and one whole-cell vaccine against pertussis. N Engl J Med. 1996;334:341–348. doi: 10.1056/NEJM199602083340601. [DOI] [PubMed] [Google Scholar]
- 16.Gross R, Rappuoli R. Positive regulation of pertussis toxin expression. Proc Natl Acad Sci USA. 1988;85:3913–3917. doi: 10.1073/pnas.85.11.3913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harding C V. Alternate pathways of MHC-I antigen processing. In: Kaufmann S H E, editor. Host response to intracellular pathogens. R. G. Georgetown, Tex: Landes Company; 1997. pp. 37–45. [Google Scholar]
- 18.Harding C V, Song R. Phagocytic processing of exogenous particulate antigens by macrophages for presentation by class I MHC molecules. J Immunol. 1994;53:4925–4933. [PubMed] [Google Scholar]
- 19.Hazes B, Boodhoo A, Cockle S A, Read R J. Crystal structure of the pertussis toxin-ATP complex: a molecular sensor. J Mol Biol. 1996;258:661–671. doi: 10.1006/jmbi.1996.0277. [DOI] [PubMed] [Google Scholar]
- 20.Hazes B, Read R J. Accumulating evidence suggests that several A-B toxins subvert the endoplasmic reticulum-associated protein degradation pathway to enter target cells. Biochemistry. 1997;36:11051–11054. doi: 10.1021/bi971383p. [DOI] [PubMed] [Google Scholar]
- 21.Ho S N, Hunt H D, Horton R M, Pullen J K, Pease L R. Site-directed mutagenesis by overlap extension using the polymerase chain reaction. Gene. 1989;77:51–59. doi: 10.1016/0378-1119(89)90358-2. [DOI] [PubMed] [Google Scholar]
- 22.Hughes E A, Ortmann B, Surman M, Cresswell P. The protease inhibitor, N-acetyl-l-leucyl-l-leucyl-l-norleucinal, decreases the pool of major histocompatibility complex class I-binding peptides and inhibits peptide trimming in the endoplasmic reticulum. J Exp Med. 1996;183:1569–1578. doi: 10.1084/jem.183.4.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jondal M, Schirmbeck R, Reimann J. MHC class I-restricted CTL responses to exogenous antigens. Immunity. 1996;5:295–302. doi: 10.1016/s1074-7613(00)80255-1. [DOI] [PubMed] [Google Scholar]
- 24.Karre K, Ljunggren H G, Piontek G, Kiessling R. Selective rejection of H-2-deficient lymphoma variants suggests alternative immune defence strategy. Nature. 1986;319:675–678. doi: 10.1038/319675a0. [DOI] [PubMed] [Google Scholar]
- 25.Kelly A, Powis S H, Kerr L-A, Mockridge I, Elliott T, Bastin J, Uchanska-Ziegler B, Ziegler A, Trowsdale J, Townsend A. Assembly and function of the two ABC transporter proteins encoded in the human major histocompatibility complex. Nature. 1992;355:641–644. doi: 10.1038/355641a0. [DOI] [PubMed] [Google Scholar]
- 26.Khusmith S, Sedegah M, Hoffman S L. Complete protection against Plasmodium yoelii by adoptive transfer of a CD8+ cytotoxic T-cell clone recognizing sporozoite surface protein 2. Infect Immun. 1994;62:2979–2983. doi: 10.1128/iai.62.7.2979-2983.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kimura A, Mountzouros K T, Schad P A, Cieplak W, Cowell J L. Pertussis toxin analog with reduced enzymatic and biological activities is a protective immunogen. Infect Immun. 1990;58:3337–3347. doi: 10.1128/iai.58.10.3337-3347.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klavinskis L S, Whitton J L, Oldstone M B A. Molecularly engineered vaccine which expresses an immunodominant T-cell epitope induces cytotoxic T lymphocytes that confer protection from lethal virus infection. J Virol. 1989;63:4311–4316. doi: 10.1128/jvi.63.10.4311-4316.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kovacsovics-Bankowski M, Rock K L. A phagosome-to-cytosol pathway for exogenous antigens presented on MHC class I molecules. Science. 1995;267:243–246. doi: 10.1126/science.7809629. [DOI] [PubMed] [Google Scholar]
- 30.Moss J, Stanley S J, Watkins P A, Burns D L, Manclark C R, Kaslow H R, Hewlett E L. Stimulation of the thiol-dependent ADP ribosyltransferase and NAD glycohydrolase activities of Bordetella pertussis toxin by adenine nucleotides, phospholipids and detergents. Biochemistry. 1986;25:2720–2725. doi: 10.1021/bi00357a066. [DOI] [PubMed] [Google Scholar]
- 31.Nencioni L, Pizza M, Bugnoli M, De Magistris T, Di Tommaso A, Giovannoni F, Manetti R, Marsili I, Matteucci G, Nucci D, Olivieri R, Pileri P, Presentini R, Villa L, Kreeftenberg J G, Silvestri S, Tagliabue A, Rappuoli R. Characterization of genetically inactivated pertussis toxin mutants: candidates for a new vaccine against whooping cough. Infect Immun. 1990;58:1308–1315. doi: 10.1128/iai.58.5.1308-1315.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nuchtern J G, Bonifacino J S, Biddison W E, Klausner R D. Brefeldin A implicates egress from endoplasmic reticulum in class I restricted antigen presentation. Nature. 1989;339:223–226. doi: 10.1038/339223a0. [DOI] [PubMed] [Google Scholar]
- 33.Oldstone M B A, Tishon A, Geckeler R, Lewicki H, Whitton J L. A common antiviral cytotoxic T-lymphocyte epitope for diverse major histocompatibility complex haplotypes: implications for vaccination. Proc Natl Acad Sci USA. 1992;89:2752–2755. doi: 10.1073/pnas.89.7.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ozato K, Hansen T H, Sachs D H. Monoclonal antibodies to mouse MHC antigens. II. Antibodies to the H-2Ld antigen, the products of a third polymorphic locus of the mouse major histocompatibility complex. J Immunol. 1980;125:2473–2477. [PubMed] [Google Scholar]
- 35.Pizza M, Bugnoli M, Manetti R, Rappuoli R. A correct folding of the S1 subunit is required for pertussis toxin secretion. J Biol Chem. 1990;265:17759–17763. [PubMed] [Google Scholar]
- 36.Pizza M, Covacci A, Bartoloni A, Perugini M, Nencioni L, DeMagistris M T, Villa L, Nucci D, Manetti R, Bugnoli M, Giovannoni F, Olivieri R, Barbieri J T, Sato H, Rappuoli R. Mutants of pertussis toxin suitable for vaccine development. Science. 1989;246:497–500. doi: 10.1126/science.2683073. [DOI] [PubMed] [Google Scholar]
- 37.Rock K L, Gramm C, Rothstein L, Clark K, Stein R, Dick L, Hwang D, Goldberg A L. Inhibitors of the proteasome block the degradation of most cell proteins and the generation of peptides presented on MHC class I molecules. Cell. 1994;78:761–771. doi: 10.1016/s0092-8674(94)90462-6. [DOI] [PubMed] [Google Scholar]
- 38.Salter R D, Cresswell P. Impaired assembly and transport of HLA-A and -B antigens in a mutant T×B hybrid. EMBO J. 1986;5:943–949. doi: 10.1002/j.1460-2075.1986.tb04307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saron M F, Fayolle C, Sebo P, Ladant D, Ullmann A, Leclerc C. Antiviral protection conferred by recombinant adenylate cyclase toxins from Bordetella pertussis carrying a CD8+ T cell epitope from lymphocytic choriomeningitis virus. Proc Natl Acad Sci USA. 1997;94:3314–3319. doi: 10.1073/pnas.94.7.3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saukkonen K, Burnette W N, Mar V L, Masure H R, Tuomanen E I. Pertussis toxin has eukaryotic-like carbohydrate recognition domains. Proc Natl Acad Sci USA. 1992;89:118–122. doi: 10.1073/pnas.89.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sebo P, Fayolle C, d’Andria O, Ladant D, Leclerc C, Ullmann A. Cell-invasive activity of epitope-tagged adenylate cyclase of Bordetella pertussis allows in vitro presentation of a foreign epitope to CD8+ cytotoxic T cells. Infect Immun. 1995;63:3851–3857. doi: 10.1128/iai.63.10.3851-3857.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shen H, Miller J F, Fan X, Kolwyck D, Ahmed R, Harty J T. Compartmentalization of bacterial antigens: differential effects on priming of CD8 T cells and protective immunity. Cell. 1998;92:535–545. doi: 10.1016/s0092-8674(00)80946-0. [DOI] [PubMed] [Google Scholar]
- 43.Simon R, Priefer U, Pühler A. A broad host range mobilization system for in vivo genetic engineering: transposon mutagenesis in gram negative bacteria. Bio/Technology. 1983;1:784–791. [Google Scholar]
- 44.Spies T, Cerundolo V, Colonna M, Cresswell P, Townsend A, DeMars R. Presentation of viral antigen by MHC class I molecules is dependent on a putative peptide transporter heterodimer. Nature. 1992;355:644–646. doi: 10.1038/355644a0. [DOI] [PubMed] [Google Scholar]
- 45.Stainer D W, Scholte M J. A simple chemically defined medium for the production of phase I Bordetella pertussis. J Gen Microbiol. 1970;63:211–220. doi: 10.1099/00221287-63-2-211. [DOI] [PubMed] [Google Scholar]
- 46.Stein P E, Boodhoo A, Armstrong G D, Cockle S A, Klein M H, Read R J. The crystal structure of pertussis toxin. Structure. 1994;2:45–57. doi: 10.1016/s0969-2126(00)00007-1. [DOI] [PubMed] [Google Scholar]
- 47.Stibitz S, Black W, Falkow S. The construction of a cloning vector designed for gene replacement in Bordetella pertussis. Gene. 1986;50:133–140. doi: 10.1016/0378-1119(86)90318-5. [DOI] [PubMed] [Google Scholar]
- 48.Stibitz S, Yang M-S. Subcellular location and immunological detection of proteins encoded by the vir locus of Bordetella pertussis. J Bacteriol. 1991;173:4288–4296. doi: 10.1128/jb.173.14.4288-4296.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tamura M, Nogimori L, Murai S, Yajima M, Itio K, Katada T, Ui M, Ishii S. Subunit structure of the islet-activating protein, pertussis toxin, in conformity with the A-B model. Biochemistry. 1982;21:5516–5522. doi: 10.1021/bi00265a021. [DOI] [PubMed] [Google Scholar]
- 50.Townsend A, Ohlen C, Bastin J, Ljunggren H-G, Foster L, Karre K. Association of class I major histocompatibility heavy and light chains induced by viral peptides. Nature. 1989;340:443–448. doi: 10.1038/340443a0. [DOI] [PubMed] [Google Scholar]
- 51.Ulmer J B, Donnelly J J, Liu M A. Presentation of an exogenous antigen by major histocompatibility complex class I molecules. Eur J Immunol. 1994;24:1590–1596. doi: 10.1002/eji.1830240721. [DOI] [PubMed] [Google Scholar]
- 52.Vinitsky A, Anton L C, Snyder H L, Orlowski M, Bennink J R, Yewdell J W. The generation of MHC class I-associated peptides is only partially inhibited by proteasome inhibitors. J Immunol. 1997;159:554–564. [PubMed] [Google Scholar]
- 53.Wada, K., Y. Wada, F. Ishibashi, T. Gojobori, and T. Ikemura. 1992. Codon usage tabulated from the GenBank genetic sequence data. Nucleic Acids Res. 20(Suppl.):2111–2118. [DOI] [PMC free article] [PubMed]
- 54.Weiss W R, Berzofsky J A, Houghten R A, Sedegah M, Hollindale M, Hoffman S L. A T cell clone directed at the circumsporozoite protein which protects mice against both Plasmodium yoelii and Plasmodium berghei. J Immunol. 1992;149:2103–2109. [PubMed] [Google Scholar]
- 55.Werner E D, Brodsky J L, McCracken A A. Proteasome-dependent endoplasmic reticulum-associated protein degradation: an unconventional route to a familiar fate. Proc Natl Acad Sci USA. 1996;93:13797–13801. doi: 10.1073/pnas.93.24.13797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Whitton J L, Tishon A, Lewicki H, Gebhard J, Cook T, Salvato M, Joly E, Oldstone M B A. Molecular analyses of a five-amino-acid cytotoxic T-lymphocyte (CTL) epitope: an immunodominant region which induces nonreciprocal CTL cross-reactivity. J Virol. 1989;63:4303–4310. doi: 10.1128/jvi.63.10.4303-4310.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xu Y, Barbieri J T. Pertussis toxin-mediated ADP ribosylation of target proteins in Chinese hamster ovary cells involves a vesicle trafficking mechanism. Infect Immun. 1995;63:825–832. doi: 10.1128/iai.63.3.825-832.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu Y, Barbieri J T. Pertussis toxin-catalyzed ADP-ribosylation of Gi-2 and Gi-3 in CHO cells is modulated by inhibitors of intracellular trafficking. Infect Immun. 1996;64:593–599. doi: 10.1128/iai.64.2.593-599.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yewdell J W, Bennink J R. Brefeldin A specifically inhibits presentation of protein antigens to cytotoxic T lymphocytes. Science. 1989;244:1072–1075. doi: 10.1126/science.2471266. [DOI] [PubMed] [Google Scholar]