Abstract
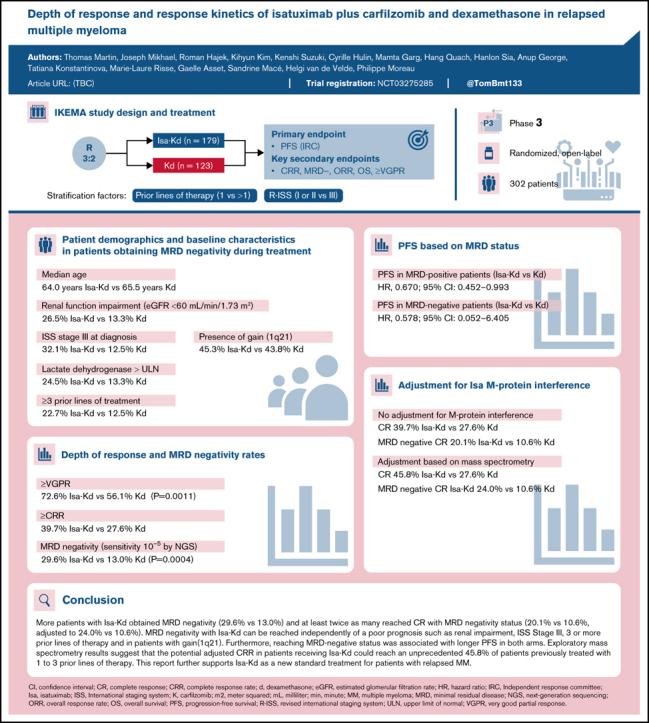
The IKEMA study (Randomized, Open Label, Multicenter Study Assessing the Clinical Benefit of Isatuximab Combined With Carfilzomib [Kyprolis®] and Dexamethasone Versus Carfilzomib With Dexamethasone in Patients With Relapse and/or Refractory Multiple Myeloma Previously Treated With 1 to 3 Prior Lines; #NCT03275285) was a randomized, open-label, multicenter phase 3 study investigating isatuximab plus carfilzomib and dexamethasone (Isa-Kd) vs Kd in patients with relapsed multiple myeloma. This subanalysis analyzed the depth of response of Isa-Kd vs Kd. The primary end point was progression-free survival (PFS); secondary end points included overall response rate, very good partial response or better (≥VGPR) rate, complete response (CR) rate, and minimal residual disease (MRD) negativity rate (assessed in patients with ≥VGPR by next-generation sequencing at a 10−5 sensitivity level). At a median follow-up of 20.7 months, deeper responses were observed in the Isa-Kd arm vs the Kd arm, with ≥VGPR 72.6% vs 56.1% and CR of 39.7% vs 27.6%, respectively. MRD negativity occurred in 53 (29.6%) of 179 patients in the Isa-Kd arm vs 16 (13.0%) of 123 patients in the Kd arm, with 20.1% (Isa-Kd, 36 of 179 patients) vs 10.6% (Kd, 13 of 123 patients) reaching MRD-negative CR status. Achieving MRD negativity resulted in better PFS in both arms. A positive PFS treatment effect was seen with Isa-Kd in both MRD-negative patients (hazard ratio, 0.578; 95% CI, 0.052-6.405) and MRD-positive patients (hazard ratio, 0.670; 95% CI, 0.452-0.993). Exploratory analysis indicates that both current CR and MRD-negative CR rates are underestimated due to M-protein interference (potential adjusted CR rate, 45.8%; potential adjusted MRD-negative CR rate, 24.0%). In conclusion, there was a clinically meaningful improvement in depth of response with Isa-Kd. The CR rate in Isa-Kd was 39.7%. Mass spectrometry suggests that the potential adjusted CR rate could reach an unprecedented 45.8% of patients treated with Isa-Kd.
Key Points
-
•
This report analyzed the depth of response of Isa-Kd vs Kd in relapsed multiple myeloma.
-
•
Deeper responses were observed with Isa-Kd, including a CR rate of 39.7% (increased to 45.8% when adjusted).
Introduction
Over the past 10 years, the development of several novel treatments with different mechanisms of action has improved the survival of patients with multiple myeloma (MM).1 Consequently, an increasing proportion of patients with MM expect to achieve deep responses utilizing the novel treatments currently available.2 However, despite these therapeutic advances to date, MM remains incurable, and new potent treatment regimens are required to bridge this unmet clinical need.
Deep response to MM treatment is associated with improved progression-free survival (PFS) and overall survival (OS).3,4 Minimal residual disease (MRD) is an important prognostic factor in MM, and achievement of MRD-negative status is associated with improved survival outcomes.2,5 Importantly, use of MRD assessment to measure response to MM treatment and predict survival outcomes in clinical practice may allow early utilization of the most effective targeted therapies.
Monoclonal antibody–based therapies have substantially improved clinical outcomes for patients with MM. Isatuximab (Sarclisa, sanofi-aventis US LLC, Bridgewater, NJ) is an immunoglobulin-G1 (IgG1) monoclonal antibody that targets a specific epitope on the CD38 receptor, which is uniformly expressed on MM cells. Isatuximab's modes of action include inhibition of CD38 ectoenzymatic activity and immediate tumor cell lysis through antibody-dependent cellular cytotoxicity, antibody-dependent cellular phagocytosis, complement-dependent cytotoxicity, and direct apoptosis. Isatuximab modulates the activity of immune effector cells, including natural killer cells, through the binding of the CD38 receptor. Isatuximab also elicits longer term immunomodulation, which includes an increase in CD3+ T cells, a decrease in regulatory T cells, and the induction of myeloma-specific antitumor immunity.6,7,8,9,10,11 Based on the phase 3 ICARIA-MM (A Phase 3 Randomized, Open-label, Multicenter Study Comparing Isatuximab [SAR650984] in Combination With Pomalidomide and Low-Dose Dexamethasone Versus Pomalidomide and Low-Dose Dexamethasone in Patients With Refractory or Relapsed and Refractory Multiple Myeloma) study, isatuximab is approved in several countries, including Japan and the Republic of Korea, in combination with pomalidomide and dexamethasone for the treatment of adult patients with relapsed/refractory MM who have received at least 2 prior therapies, including lenalidomide and a proteasome inhibitor.12,13 To date, based on the phase 3 IKEMA study (Randomized, Open Label, Multicenter Study Assessing the Clinical Benefit of Isatuximab Combined With Carfilzomib [Kyprolis®] and Dexamethasone Versus Carfilzomib With Dexamethasone in Patients With Relapse and/or Refractory Multiple Myeloma Previously Treated With 1 to 3 Prior Lines; #NCT03275285), isatuximab in combination with carfilzomib (an irreversible second-generation proteasome inhibitor) and dexamethasone (ie, Isa-Kd) is approved in the United States for the treatment of adult patients with relapsed/refractory MM who have received 1 to 3 prior lines of therapy, in the European Union for the treatment of adult patients with relapsed MM who have received at least 1 prior therapy, and in Japan for the treatment of adult patients with relapsed or refractory MM who have received 1 prior treatment.12,13,14 Carfilzomib is a proteasome inhibitor approved for use in combination with dexamethasone for patients with relapsed/refractory MM based on the phase 3 ENDEAVOR (A Randomized, Open-label, Phase 3 Study of Carfilzomib Plus Dexamethasone vs. Bortezomib Plus Dexamethasone in Patients With Relapsed Multiple Myeloma) study15,16,17 showing superior efficacy of carfilzomib combined with dexamethasone compared with bortezomib combined with dexamethasone (median PFS and OS, 18.7 and 47.6 months vs 9.4 and 40.0 months, respectively; hazard ratios [HRs], 0.53 and 0.79; P < .0001 and .010, respectively). These results were the basis for the control treatment used in the IKEMA study.
The current analysis explored the depth of response, including MRD-negativity long-term survival outcomes, and kinetics of disease response in the IKEMA study, a randomized, open-label, multicenter phase 3 study that investigated Isa-Kd (n = 179) vs carfilzomib and dexamethasone (ie, Kd; n = 123) in patients with relapsed MM and 1 to 3 prior lines of therapy.18 At the prespecified interim analysis, at a median follow-up of 20.7 months, the median PFS was not reached in the isatuximab arm vs 19.2 months in the control arm (HR, 0.531; 99% confidence interval [CI], 0.318-0.889; one-sided P = .0007), corresponding to a 47% reduction in the risk of progression or death.19
Isatuximab, being a monoclonal IgG antibody, can be detected on immunofixation electrophoresis (IFE) and conventional serum protein electrophoresis (SPEP) assays that monitor patients for residual M-protein. This interference may lead to false-positive immunofixation results and thus underestimation of a patient's response to treatment according to International Myeloma Working Group (IMWG) criteria.1 Immuno-capture and liquid chromatography coupled to high-resolution mass spectrometry of serum M-protein was performed to overcome the interference with isatuximab in the standard IFE assay. This paper also reports the impact on depth of response with Isa-Kd, considering adjustment with mass spectrometry.
Methods
IKEMA study design and participants
The IKEMA phase 3 study design has been published previously.18 Briefly, patients were randomized in a 3:2 ratio to receive Isa-Kd or Kd. Randomization was stratified according to number of prior lines of treatment (1 vs >1) and revised international Staging System (R-ISS) (Stage I or II vs III vs not classified).
The study was approved by local independent ethics committees and/or institutional review boards for review, and written approval was obtained from patients before enrollment into the study. The study was conducted in accordance with consensus ethics principles derived from international ethics guidelines, including the Declaration of Helsinki and the International Conference on Harmonisation guidelines for Good Clinical Practice, as well as all applicable laws, rules, and regulations.
End points
The primary end point was PFS, and key secondary end points were overall response rate,18 very good partial response or better (≥VGPR) rate, MRD negativity rate, complete response rate, and OS. Disease response and date of progression were determined by a blinded Independent Response Committee (IRC) based on central data for M-protein, central imaging review, and local bone marrow for plasma cell infiltration according to IMWG criteria.1 Exploratory end points included the impact of M-protein measurement without interference on best overall response assessment.
Procedures
MRD was assessed in bone marrow aspirates by using next-generation sequencing (NGS) by clonoSEQ at a 10−5 sensitivity level from patients who achieved ≥VGPR. Immuno-capture and liquid chromatography coupled to high-resolution mass spectrometry analyses were performed on the 27 patients with near or potential CR20 (only those with serum immunofixation [IF] positive for IgG κ) or potential CR (serum remaining M-protein ≤0.5 g/dL with IF-positive IgG κ) in the Isa-Kd arm to measure serum M-protein without isatuximab interference. M-protein analyses were performed either by a central laboratory or Sanofi TMED Department (Montpellier Cedex, France) using a validated mass spectrometry test. The M-protein detection limit varied between 0.012 and 0.025 g/dL. In publications, the lower limit for detection of M-protein or of therapeutic monoclonal antibodies by immunofixation has been reported as 0.025 g/dL.21,22 The threshold for M-protein positivity in the mass spectrometry assay was determined at 0.025 g/dL.
Statistical analyses
The interim analysis of PFS was preplanned when 65% of the 159 PFS events (103 events) were observed. For PFS, comparison between arms was conducted through a log-rank test procedure by stratification factors at randomization. HRs and corresponding CIs were estimated by using the stratified Cox proportional hazards model. Secondary end points were compared between treatment arms by using the stratified Cochran-Mantel-Haenszel test and a hierarchical procedure.
MRD negativity rate analysis was performed in the intention-to-treat population. For this analysis, patients in the intention-to-treat population with no MRD assessment were considered MRD positive. Analyses on the MRD negativity rate were also performed on patients with ≥VGPR as per IRC. MRD status according to best overall response as per IRC was also assessed.
Results
Depth of response and MRD negativity rates
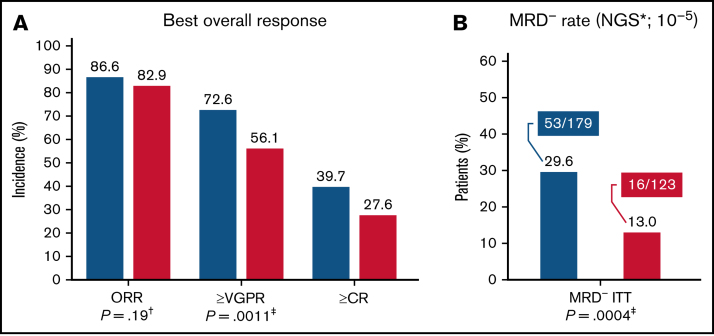
At the positive PFS interim analysis with median follow-up of 20.7 months, deeper responses were observed in the Isa-Kd arm vs the Kd arm, with ≥VGPR 72.6% vs 56.1% (nominal P value = .0011) and ≥CR 39.7% vs 27.6%, respectively (Figure 1A). Consistent with the IRC assessment, the rate of ≥VGPR based on the investigator assessment was 71.5% and 56.9% in the Isa-Kd and Kd arms, respectively. MRD negativity (sensitivity 10−5 by NGS) in the intention-to-treat population occurred in 53 (29.6%) of 179 patients in the Isa-Kd arm vs 16 (13.0%) of 123 in the Kd arm (nominal P = .0004) (Figure 1B), with 20.1% (36 of 179 patients in the Isa-Kd arm) vs 10.6% (13 of 123 patients in the Kd arm) reaching both CR as per IRC and MRD negativity (Figure 1A). The MRD negativity rate at 12 months was 26.8% (95% CI, 0.20-0.34) in Isa-Kd and 12.2% (95% CI, 0.07-0.19) in the Kd arm; the CR MRD negativity rate at 12 months was 17.3% in Isa-Kd (95% CI, 0.06-0.17) vs 10.6% (95% CI, 0.12-0.24) in Kd. The CR MRD-negative CR rate at 12 months was 17.3% in Isa-Kd (95% CI, 0.06-0.17) vs 10.6% (95% CI, 0.12-0.24) in Kd.
Figure 1.
Depth of response. Best overall response (A) and MRD negativity rate (B). *Adaptive Biotechnologies NGS, MRD testing performed at time of VGPR or CR. Per protocol, the CR was not tested at the time of the interim analysis because the Hydrashift M-protein interference assay38 was not yet available at that time. †Stratified Cochran-Mantel-Haenszel test. One-sided significance level is .025. ‡Provided for descriptive purposes only. ITT, intention-to-treat; ORR, overall response rate.
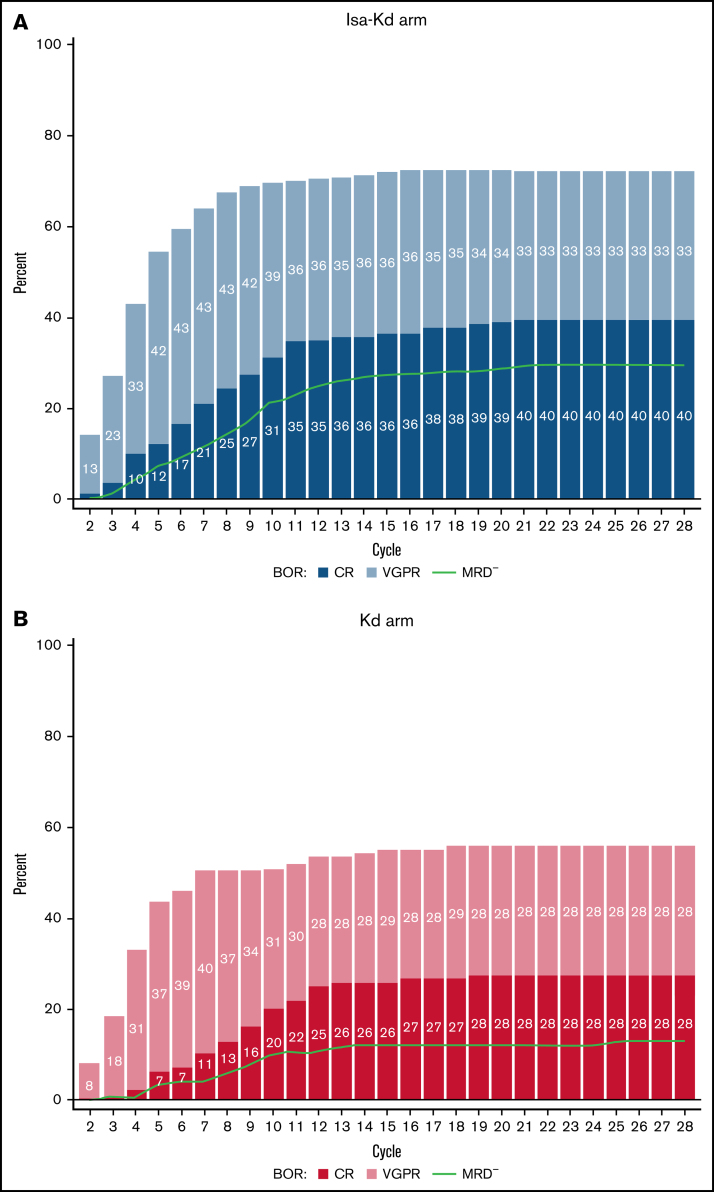
Responses occurred quickly in both treatment arms, with similar median times to first response (32.0 days in the Isa-Kd arm vs 33.0 days in the Kd arm), but median time to the first CR occurred earlier with Isa-Kd vs Kd (median, 184.0 days vs 229.5 days). Analysis of response over time in the Isa-Kd arm showed that all responding patients obtained at least a partial response by cycle 5 and ≥VGPR was obtained by cycle 12 (Figure 2A). Furthermore, most patients in the Isa-Kd arm who achieved CR and MRD negativity obtained the best response by cycle 12 (12 months), although some patients still obtained CR and MRD negativity between cycle 12 and cycle 24 (12 and 24 months), indicating a maturation of depth of response over time. Substantially fewer patients in the Kd arm achieved CR and MRD-negative status (Figure 2B).
Figure 2.
Cumulative best overall response based on IRC according to cycle. Patients who received Isa-Kd (A) compared with those who received Kd (B) (intention-to-treat population). BOR, best overall response.
Patient demographic and baseline characteristics based on MRD status
When comparing baseline characteristics of patients reaching MRD negativity in the Isa-Kd arm (53 patients) vs the Kd arm (16 patients) (Table 1), more patients in the Isa-Kd arm reaching MRD-negative status had adverse prognostic markers such as renal function impairment (estimated glomerular filtration rate <60 mL/min/1.73 m2, 26.5% vs 13.3%), high-stage disease (ISS Stage III at diagnosis, 32.1% vs 12.5%), lactate dehydrogenase levels more than the upper limit of normal (24.5% vs 13.3%), or were heavily pretreated (≥3 prior lines, 22.7% vs 12.5%). Median age (64.0 years vs 65.5 years) and presence of gain(1q21) (45.3% vs 43.8%) were similar between arms in patients reaching MRD negativity. In the patients achieving MRD negativity, high-risk cytogenetic abnormalities were less frequent in the Isa-Kd arm (17.0%) than in the Kd arm (43.8%), resulting in a high proportion of standard-risk patients reaching MRD negativity in the Isa-Kd arm.
Table 1.
Key patient demographic and baseline characteristics according to treatment group and MRD status (randomized population)
| Characteristic | MRD negative (n = 69) | MRD positive (n = 233) | ||
|---|---|---|---|---|
| Isa-Kd (n = 53) | Kd (n = 16) | Isa-Kd (n = 126) | Kd (n = 107) | |
| Age, y | ||||
| Median | 64.0 | 65.5 | 65.0 | 63.0 |
| Range | 37-83 | 33-78 | 38-86 | 38-90 |
| Age by category | ||||
| <65 y | 29 (54.7) | 8 (50.0) | 59 (46.8) | 58 (54.2) |
| ≥65-74 y | 20 (37.7) | 6 (37.5) | 54 (42.9) | 41 (38.3) |
| ≥75 y | 4 (7.5) | 2 (12.5) | 13 (10.3) | 8 (7.5) |
| eGFR (MDRD* formula) | ||||
| No. of evaluable patients | 49 | 15 | 116 | 96 |
| <60 mL/min/1.73 m2 | 13 (26.5) | 2 (13.3) | 30 (25.9) | 16 (16.7) |
| ≥60 mL/min/1.73 m2 | 36 (73.5) | 13 (86.7) | 86 (74.1) | 80 (83.3) |
| ISS stage at initial diagnosis | ||||
| Stage I | 10 (18.9) | 8 (50.0) | 30 (23.8) | 25 (23.4) |
| Stage II | 13 (24.5) | 6 (37.5) | 40 (31.7) | 42 (39.3) |
| Stage III | 17 (32.1) | 2 (12.5) | 35 (27.8) | 23 (21.5) |
| Unknown | 13 (24.5) | 0 | 21 (16.7) | 17 (15.9) |
| LDH more than the ULN | 13 (24.5) | 2/15 (13.3) | 31/123 (25.2) | 15 (14.0) |
| Prior lines of therapy | ||||
| Median | 1 | 1 | 2 | 2 |
| Range | 1-4 | 1-3 | 1-4 | 1-4 |
| 1 line | 28 (52.8) | 10 (62.5) | 51 (40.5) | 45 (42.1) |
| 2 lines | 13 (24.5) | 4 (25.0) | 51 (40.5) | 32 (29.9) |
| ≥3 lines | 12 (22.7) | 2 (12.5) | 24 (19.1) | 30 (28.1) |
| Patients refractory to | ||||
| Lenalidomide | 14 (26.4) | 4 (25.0) | 43 (34.1) | 38 (35.5) |
| IMiD and PI | 6 (11.3) | 2 (12.5) | 29 (23.0) | 25 (23.4) |
| Refractory to last regimen | 25 (47.2) | 5 (31.3) | 64 (50.8) | 68 (63.6) |
| Lenalidomide | 10 (18.9) | 3 (18.8) | 26 (20.6) | 28 (26.2) |
| Bortezomib | 8 (15.1) | 2 (12.5) | 24 (19.0) | 21 (19.6) |
| Cytogenetic risk† | ||||
| High risk | 9 (17.0) | 7 (43.8) | 33 (26.2) | 24 (22.4) |
| Standard risk | 41 (77.4) | 9 (56.3) | 73 (57.9) | 69 (64.5) |
| Unknown or missing | 3 (5.7) | 0 | 20 (15.9) | 14 (13.1) |
| Gain(1q21) present‡ | 24 (45.3) | 7 (43.8) | 51 (40.5) | 45 (42.1) |
Data are presented as No. (%) unless otherwise indicated. CRF, chronic renal failure; eGFR, estimated glomerular filtration rate, IMiD, immunomodulatory drug; LDH, lactate dehydrogenase; MDRD, Modification of Diet in Renal Disease; PI, proteasome inhibitor; ULN, upper limit of normal.
Incidence calculated in patients with reported CRF: 165 patients in the Isa-Kd arm and 111 patients in the Kd arm.
Cytogenetics by central laboratory: cutoff 50% for del17p, 30% for t(4;14) and t(14;16).
Gain(1q21) is defined as the presence of at least 3 copies with a cutoff of 30%.
Comparing baseline characteristics in patients within the Isa-Kd arm reaching MRD negativity (n = 53) vs MRD-positive status (n = 126), similar percentages of patients had renal function impairment (estimated glomerular filtration rate <60 mL/min/1.73 m2), high-stage disease (ISS Stage III at diagnosis), presence of gain(1q21), were refractory to lenalidomide in the last regimen, and were heavily pretreated (≥3 prior lines).
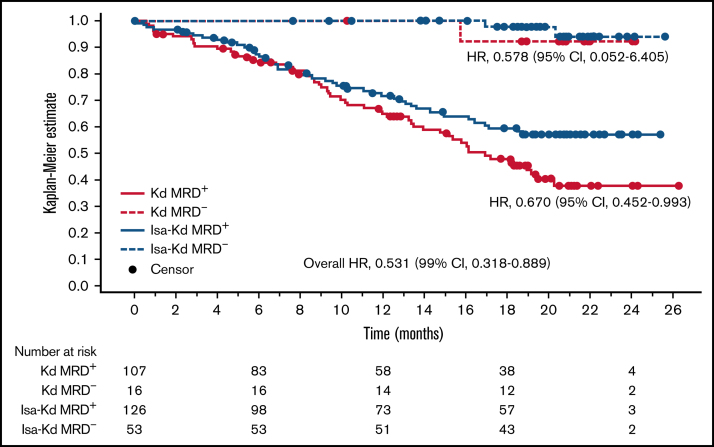
PFS based on MRD status
PFS according to MRD status is shown in Figure 3. MRD-negative patients had a longer PFS compared with MRD-positive patients. The very low PFS event rate and the plateau aspect of the Kaplan-Meier curves in the MRD-negative patients support the prognostic relevance for long-term outcomes of the MRD-negative observation. Isa-Kd clearly improved PFS in MRD-positive patients (HR, 0.670; 95% CI, 0.452-0.993). In MRD-negative patients, a similar PFS HR of 0.578 (95% CI, 0.052-6.405) in favor of Isa-Kd was observed but should be interpreted with caution due to the low PFS rate observed at current follow-up.
Figure 3.
PFS according to MRD status.
Adjustment for isatuximab M-protein interference
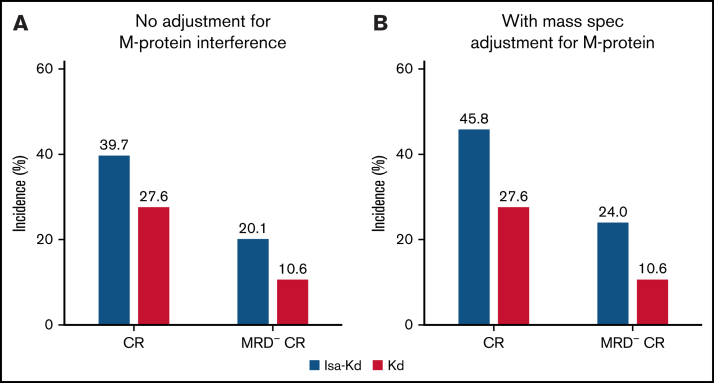
The interference of isatuximab with M-protein assessment was tested by using mass spectrometry in 153 samples from 27 patients with near-CR (no serum M-protein by SPEP and serum IF-positive for IgG κ) or potential CR (serum M-protein ≤0.5 g/dL by SPEP with IF-positive IgG κ) in the Isa-Kd arm. In 15 patients, there was no residual M-protein detectable in multiple samples at the sensitivity level of the central laboratory immunofixation test (below 0.025 g/dL). Among these 15 patients, 11 had documented <5% plasma cells in bone marrow, indicating these patients could have CR as best response (no residual serum M-protein above the threshold for IFE positivity in the study). This supports the premise that the current CR rate is underestimated and that the adjusted CR rate could be 45.8% (82 of 179).
Of the 11 patients who were negative according to mass spectrometry testing with ≤5% bone marrow plasma cells, 7 patients were also MRD-negative, supporting that the current MRD-negative CR rate is also underestimated and that the adjusted MRD-negative CR rate could be 24.0% (43 of 179) (Figure 4).
Figure 4.
Depth of response subgroup. With no adjustment for isatuximab interference with M-protein measurement (A) and mass spectrometry (Mass Spec) adjustment for M-protein value (B). Adaptive Biotechnologies NGS, MRD testing performed at time of VGPR or CR.
Discussion
IKEMA is the first phase 3 study to evaluate the triplet regimen Isa-Kd, previous studies of Kd having already shown that this doublet regimen is effective, and the first to show PFS and OS superiority over bortezomib-dexamethasone in relapsed/refractory MM.16 The results from IKEMA showed that the addition of isatuximab to Kd was associated with a significant benefit in PFS in patients with relapsed MM compared with Kd alone.19 The risk of disease progression or death was 47% lower in the Isa-Kd arm, indicated by the very low HR at the time of the prespecified interim analysis (0.531; 99% CI, 0.318-0.889; P = .0007). A similar response rate was reported in both arms due to a very high response rate of 82.9% in the control arm, which is the highest response rate ever reported for Kd (77% in ENDEAVOR and 75% in CANDOR (A Randomized, Open-label, Phase 3 Study Comparing Carfilzomib, Dexamethasone, and Daratumumab to Carfilzomib and Dexamethasone for the Treatment of Patients With Relapsed or Refractory Multiple Myeloma]). However, the quality of response was better in the Isa-Kd arm vs Kd arm, with a clinically meaningful improvement in ≥VGPR (72.6% vs 56.1%) and CR rate (39.7% vs 27.6%) despite lack of a test accounting for interference between M-protein and isatuximab.
In this study, an unprecedented MRD-negative rate was reported in patients with relapsed MM treated with a proteasome inhibitor–based regimen (Isa-Kd, 29.6%; Kd, 13.0%). Also, twice as many patients in the CR group reached MRD negativity status (20.1% vs 10.0%) in the Isa-Kd arm vs the Kd arm.
Within the constraints of cross-trial comparison, an MRD negativity rate of 29.6% with Isa-Kd after a median follow-up of 20.7 months seems superior to other proteasome inhibitor–based regimens in relapsed MM. In the CANDOR study of patients with relapsed MM with 1 to 3 prior lines of therapy, an MRD negativity rate of 22.8% was achieved in the daratumumab-Kd arm.1,18,23 In the TOURMALINE-MM1 (A Phase 3, Randomized, Double-Blind, Multicenter Study Comparing Oral Ixazomib [MLN9708] Plus Lenalidomide and Dexamethasone Versus Placebo Plus Lenalidomide and Dexamethasone in Adult Patients With Relapsed and/or Refractory Multiple Myeloma) study of patients with newly diagnosed MM, an MRD negativity rate of 12.5% was achieved in the ixazomib, lenalidomide, and dexamethasone arm at a median follow-up of 55 months.24 In the POLLUX (Phase 3 Study Comparing Daratumumab, Lenalidomide, and Dexamethasone [DRd] vs Lenalidomide and Dexamethasone [Rd] in Subjects With Relapsed or Refractory Multiple Myeloma) study of patients with MM who had received at least 1 prior line of therapy, an MRD negativity rate of 22% was achieved in the daratumumab, lenalidomide, and dexamethasone arm.25
It is recognized that patients who achieve ≥VGPR and MRD negativity status at a sensitivity of 1 tumor cell per 105 cells have an improved PFS and OS compared with those who are MRD positive, and that NGS assays such as clonoSEQ are credible assays for the assessment of MRD status.1,26 In our study, PFS was better for patients reaching MRD negativity vs patients who remained MRD positive, which is consistent with the literature. Although the association between MRD negativity and prolonged long-term outcomes has by now been well established in newly diagnosed MM, data from large randomized trials on the predictive significance of MRD negativity in relapsed MM are more scarce.20,27 Our study adds to the body of evidence that obtaining MRD negativity is a desired outcome with longer term benefit in relapsed MM.28 A similar observation has been made with isatuximab in combination with pomalidomide-dexamethasone in the ICARIA study in a more refractory population.29 Similar observations have also been made in studies with daratumumab when used in combination with pomalidomide and dexamethasone (APOLLO: Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma), or in combination with lenalidomide and dexamethasone (POLLUX), or in combination with carfilzomib and dexamethasone (CANDOR).23,25,30
In the current study, the addition of isatuximab to Kd increased the potential to reach MRD-negative status independently of adverse prognostic characteristics such as renal impairment, ISS Stage III, ≥3 prior lines of treatment, gain(1q21), or being refractory to lenalidomide in the last regimen, indicating that Isa-Kd treatment is independent of these adverse prognostic characteristics. Fewer patients were refractory to prior immunomodulatory drug and proteasome inhibitor treatment among patients who were MRD negative vs patients who were MRD positive, but this was observed in both arms of the study, indicating that MRD negativity remains difficult to achieve in this population. The percentage of patients with high-risk cytogenetics at baseline and obtaining MRD negativity was lower in the Isa-Kd arm compared with the Kd arm. As there was clear PFS benefit (HR, 0.72) in the high-risk cytogenetic subgroup,19 this result should be interpreted with caution due to the low number of high-risk patients obtaining MRD negativity in each arm.
Analysis of patients in the Isa-Kd arm showed that all responding patients obtained at least a ≥VGPR by cycle 12 (12 months). Although most patients in the Isa-Kd arm who achieved CR and MRD negativity obtained the best response by 12 months, some patients obtained CR and MRD negativity between cycle 12 and cycle 24 (12 and 24 months), indicating a maturation of depth of response over time. Substantially fewer patients in the Kd arm achieved MRD-negative CR status. Similar late achievement of CR and/or MRD negativity has been reported with daratumumab-Kd in the CANDOR study.18 An update on late CR and MRD negativity, as well as more mature data on the PFS results in patients achieving MRD negativity in each treatment arm, is expected during further follow-up of the IKEMA study.
Therapeutic monoclonal antibodies such as isatuximab may interfere with IFE and SPEP assays, rendering false-positive results for the detection of M-protein.31,32 Consequently, more sensitive and specific assays have been introduced to detect M-protein.33,34,35,36,37 An isatuximab-specific antibody-capture assay to mitigate M-protein interference on immunofixation is now Conformité Européenne marked in the European Union, US Food and Drug Administration 510(k) approved,38 and submitted for regulatory clearance in other regions.39 However, at the time of the interim analysis of the IKEMA study, the isatuximab-specific assay was not available for use; therefore, M-protein interference was analyzed through high-resolution mass spectrometry, preceded by immuno-capture and liquid chromatography. Recent recommendations from the IMWG Mass Spectrometry Committee have endorsed the use of mass spectrometry to aid in distinguishing therapeutic antibodies from endogenous M-protein.40 Although mass spectrometry has not yet been incorporated in the IMWG response criteria, the mass spectrometry results in the IKEMA study suggest that conventional disease assessments using IFE have led to an ∼6% underestimation of CR rate (adjusted CR rate, 45.8%) and an ∼4% underestimation of MRD-negative CR rate (adjusted MRD-negative CR rate, 24%) in the Isa-Kd arm.
In conclusion, treatment options for relapsed MM have improved significantly over the past decade resulting in increases in CR rates and life expectancy. However, with many patients experiencing relapses following multiple therapies there is a continual need for new molecules and novel combinations of treatments to improve patient outcomes. More patients in Isa-Kd vs Kd reached MRD-negative status (29.6% vs 13.0%) and at least twice as many reached CR with MRD negativity status (20.1% vs 10.6%, adjusted to 24.0% vs 10.6%). MRD negativity with Isa-Kd can be reached independently of bad prognosis such as renal impairment, ISS Stage III, ≥3 prior lines of therapy, and in patients with gain(1q21). Furthermore, reaching MRD-negative status was associated with longer PFS in both arms. The mass spectrometry results suggest that the potential adjusted CR rate in patients receiving Isa-Kd could reach an unprecedented 45.8% of patients previously treated with 1 to 3 prior lines of therapy. The high incidence of patients with at least 1 prior line of treatment reaching MRD-negative CR in the Isa-Kd arm further supports Isa-Kd as a new standard treatment for patients with relapsed MM.
Acknowledgments
The authors thank the participating patients and their families, and the study centers and investigators, for their contributions to the study. Medical writing support was provided by John Clarke of Elevate Medical Affairs, contracted by Sanofi Genzyme for publication support services.
The IKEMA study was funded by Sanofi.
Footnotes
Presented in abstract form at the 62nd annual meeting of the American Society of Hematology, Virtual Meeting, 5-8 December 2020.
Qualified researchers can request access to patient-level data and related study documents, including the clinical study report, study protocol with any amendments, blank case report forms, statistical analysis plan, and data set specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi's data-sharing criteria, eligible studies, and process for requesting access are provided at: https://protect-de.mimecast.com/s/R_McC28yBDTk0jLglhnULrH?domain=vivli.org.
Authorship
Contribution: All authors were involved in the validation, formal analysis, writing, review, and editing of the manuscript; M.-L.R., G.A., S.M., and H.v.d.V. were involved in the conceptualization, project administration, and supervision of the study; and all authors approved the final version of the manuscript and take responsibility for the accuracy of the data.
Conflict-of-interest disclosure: T.M. reports receiving research funding from Sanofi, Amgen, Seattle Genetics, Johnson & Johnson, and Janssen; and consultancy fees from Legend Biotech. J.M. reports receiving honoraria from Amgen, Celgene, GSK, Janssen, Karyopharm, Sanofi, and Takeda. R.H. reports receiving consultancy fees from Janssen, Amgen, Celgene, AbbVie, BMS, Pharma MAR, Takeda, and Novartis; research funding from Janssen, Amgen, Celgene, and Novartis; being a member of the Board of Directors or advisory committees for Amgen and Takeda; and receiving honoraria from AbbVie, BMS, Celgene, and Takeda. K.K. received consultancy fees, honoraria and research funding from Amgen, BMS, Janssen, Sanofi, and Takeda. K.S. received honoraria from Takeda, Celgene, ONO, Amgen, Novartis, Sanofi, BMS, AbbVie, and Janssen; consultancy fees from Takeda, Amgen, Janssen, and Celgene; and research funding from BMS, Celgene, and Amgen. H.Q. received research funding from Amgen, Sanofi, Celgene, Karyopharm, and GSK; was a member of the board of directors or advisory committee for Amgen, Celgene, Karyopharm, Janssen, and Sanofi; received consultancy fees from GSK, Karyopharm, Amgen, Celgene, and Janssen; and honoraria from GSK, Karyopharm, Amgen, Celgene, and Janssen. P.M. received consultancy fees and honoraria from Janssen, BMS, Celgene, Amgen, Sanofi, and AbbVie. M.-L.R., G.A., S.M., and H.v.d.V. are employees of Sanofi and may hold shares and/or stock options in the company. The remaining authors declare no competing financial interests.
References
- 1.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–e346. doi: 10.1016/S1470-2045(16)30206-6. [DOI] [PubMed] [Google Scholar]
- 2.Munshi NC, Avet-Loiseau H, Rawstron AC, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2017;3(1):28–35. doi: 10.1001/jamaoncol.2016.3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gay F, Larocca A, Wijermans P, et al. Complete response correlates with long-term progression-free and overall survival in elderly myeloma treated with novel agents: analysis of 1175 patients. Blood. 2011;117(11):3025–3031. doi: 10.1182/blood-2010-09-307645. [DOI] [PubMed] [Google Scholar]
- 4.van de Velde HJ, Liu X, Chen G, Cakana A, Deraedt W, Bayssas M. Complete response correlates with long-term survival and progression-free survival in high-dose therapy in multiple myeloma. Haematologica. 2007;92(10):1399–1406. doi: 10.3324/haematol.11534. [DOI] [PubMed] [Google Scholar]
- 5.Paiva B, van Dongen JJ, Orfao A. New criteria for response assessment: role of minimal residual disease in multiple myeloma. Blood. 2015;125(20):3059–3068. doi: 10.1182/blood-2014-11-568907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atanackovic D, Yousef S, Shorter C, et al. In vivo vaccination effect in multiple myeloma patients treated with the monoclonal antibody isatuximab. Leukemia. 2020;34(1):317–321. doi: 10.1038/s41375-019-0536-3. [DOI] [PubMed] [Google Scholar]
- 7.Deckert J, Wetzel MC, Bartle LM, et al. SAR650984, a novel humanized CD38-targeting antibody, demonstrates potent antitumor activity in models of multiple myeloma and other CD38+ hematologic malignancies. Clin Cancer Res. 2014;20(17):4574–4583. doi: 10.1158/1078-0432.CCR-14-0695. [DOI] [PubMed] [Google Scholar]
- 8.Feng X, Zhang L, Acharya C, et al. Targeting CD38 suppresses induction and function of T regulatory cells to mitigate immunosuppression in multiple myeloma. Clin Cancer Res. 2017;23(15):4290–4300. doi: 10.1158/1078-0432.CCR-16-3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang H, Acharya C, An G, et al. SAR650984 directly induces multiple myeloma cell death via lysosomal-associated and apoptotic pathways, which is further enhanced by pomalidomide. Leukemia. 2016;30(2):399–408. doi: 10.1038/leu.2015.240. [DOI] [PubMed] [Google Scholar]
- 10.Martin TG, Corzo K, Chiron M, et al. Therapeutic opportunities with pharmacological inhibition of CD38 with isatuximab. Cells. 2019;8(12):E1522. doi: 10.3390/cells8121522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moreno L, Perez C, Zabaleta A, et al. The mechanism of action of the anti-CD38 monoclonal antibody isatuximab in multiple myeloma. Clin Cancer Res. 2019;25(10):3176–3187. doi: 10.1158/1078-0432.CCR-18-1597. [DOI] [PubMed] [Google Scholar]
- 12.Sanofi-Aventis. Sarclisa (isatuximab-irfc) [package insert]. Bridgewater, NJ. https://products.sanofi.us/Sarclisa/Sarclisa.pdf. Accessed 10 February 2022.
- 13.European Medicines Agency. Medicines. Sarclisa. https://www.ema.europa.eu/en/medicines/human/summaries-opinion/sarclisa-0. Accessed 10 February 2022.
- 14.Sanofi Japan. Sarclisa [package insert]. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/780069_4291454A1021_1_02. Accessed 10 February 2022.
- 15.Amgen. Kyprolis (carfilzomib) [package insert]. Thousand Oaks, CA. https://www.pi.amgen.com/∼/media/amgen/repositorysites/pi-amgen-com/kyprolis/kyprolis_pi.pdf. Accessed 10 February 2022.
- 16.Dimopoulos MA, Goldschmidt H, Niesvizky R, et al. Carfilzomib or bortezomib in relapsed or refractory multiple myeloma (ENDEAVOR): an interim overall survival analysis of an open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18(10):1327–1337. doi: 10.1016/S1470-2045(17)30578-8. [DOI] [PubMed] [Google Scholar]
- 17.Dimopoulos MA, Moreau P, Palumbo A, et al. ENDEAVOR Investigators Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol. 2016;17(1):27–38. doi: 10.1016/S1470-2045(15)00464-7. [DOI] [PubMed] [Google Scholar]
- 18.Landgren O, Weisel K, Rosinol L, et al Evaluation of minimal residual disease (MRD) negativity in patients with relapsed or refractory multiple myeloma treated in the Candor study. Abstract presented at the Virtual Meeting of the American Society of Hematology. Abstract 2282, 5-8 December 2020.
- 19.Moreau P, Dimopoulos MA, Mikhael J, et al. IKEMA study group Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open-label, randomised phase 3 trial. Lancet. 2021;397(10292):2361–2371. doi: 10.1016/S0140-6736(21)00592-4. [DOI] [PubMed] [Google Scholar]
- 20.Paiva B, Puig N, Cedena MT, et al. GEM (Grupo Español de Mieloma)/PETHEMA (Programa Para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group Measurable residual disease by next-generation flow cytometry in multiple myeloma. J Clin Oncol. 2020;38(8):784–792. doi: 10.1200/JCO.19.01231. [DOI] [PubMed] [Google Scholar]
- 21.Howard SC, Jones DP, Pui CH. The tumor lysis syndrome. N Engl J Med. 2011;364(19):1844–1854. doi: 10.1056/NEJMra0904569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for Multiple Myeloma: a report from International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863–2869. doi: 10.1200/JCO.2015.61.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dimopoulos M, Quach H, Mateos MV, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomised, multicentre, open-label, phase 3 study. Lancet. 2020;396(10245):186–197. doi: 10.1016/S0140-6736(20)30734-0. [DOI] [PubMed] [Google Scholar]
- 24.Kumar SK, Berdeja JG, Niesvizky R, et al. Ixazomib, lenalidomide, and dexamethasone in patients with newly diagnosed multiple myeloma: long-term follow-up including ixazomib maintenance. Leukemia. 2019;33(7):1736–1746. doi: 10.1038/s41375-019-0384-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dimopoulos MA, Oriol A, Nahi H, et al. POLLUX Investigators Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(14):1319–1331. doi: 10.1056/NEJMoa1607751. [DOI] [PubMed] [Google Scholar]
- 26.Martinez-Lopez J, Lahuerta JJ, Pepin F, et al. Prognostic value of deep sequencing method for minimal residual disease detection in multiple myeloma. Blood. 2014;123(20):3073–3079. doi: 10.1182/blood-2014-01-550020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munshi NC, Avet-Loiseau H, Anderson KC, et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 2020;4(23):5988–5999. doi: 10.1182/bloodadvances.2020002827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avet-Loiseau H, San-Miguel J, Casneuf T, et al. Evaluation of sustained minimal residual disease negativity with daratumumab-combination regimens in relapsed and/or refractory multiple myeloma: analysis of POLLUX and CASTOR. J Clin Oncol. 2021;39(10):1139–1149. doi: 10.1200/JCO.20.01814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hulin C, Richardson PC, Attal M, et al. Depth of response and response kinetics in the ICARIA-MM study of isatuximab with pomalidomide/dexamethasone in relapsed/refractory multiple myeloma. Blood. 2019;134:3185. suppl 1. [Google Scholar]
- 30.Dimopoulos MA, Terpos E, Boccadoro M, et al. APOLLO Trial Investigators Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(6):801–812. doi: 10.1016/S1470-2045(21)00128-5. [DOI] [PubMed] [Google Scholar]
- 31.McCudden C, Axel AE, Slaets D, et al. Monitoring multiple myeloma patients treated with daratumumab: teasing out monoclonal antibody interference. Clin Chem Lab Med. 2016;54(6):1095–1104. doi: 10.1515/cclm-2015-1031. [DOI] [PubMed] [Google Scholar]
- 32.Tang F, Malek E, Math S, Schmotzer CL, Beck RC. Interference of therapeutic monoclonal antibodies with routine serum protein electrophoresis and immunofixation in patients with myeloma: frequency and duration of detection of daratumumab and elotuzumab. Am J Clin Pathol. 2018;150(2):121–129. doi: 10.1093/ajcp/aqy037. [DOI] [PubMed] [Google Scholar]
- 33.Finn G, Mace S, Campana F, et al. Evaluating isatuximab interference with monoclonal protein detection by immuno-capture and liquid chromatography coupled to high resolution mass spectrometry in the pivotal phase 3 multiple myeloma trial, ICARIA-MM. Blood. 2019;134:3143. suppl 1. [Google Scholar]
- 34.Mills JR, Barnidge DR, Dispenzieri A, Murray DL. High sensitivity blood-based M-protein detection in sCR patients with multiple myeloma. Blood Cancer J. 2017;7(8):e590. doi: 10.1038/bcj.2017.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moore LM, Cho S, Thoren KL. MALDI-TOF mass spectrometry distinguishes daratumumab from M-proteins. Clin Chim Acta. 2019;492:91–94. doi: 10.1016/j.cca.2019.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muccio S, Tavernier A, Rouchon M-C, et al. M-protein semi quantification in MM serum patients based on immuno-capture and liquid chromatography coupled to high resolution mass spectrometry. Clin Lymphoma Myeloma Leuk. 2019;19:E149–E150. 10 suppl. [Google Scholar]
- 37.Thoren KL, Pianko MJ, Maakaroun Y, Landgren CO, Ramanathan LV. Distinguishing drug from disease by use of the Hydrashift 2/4 daratumumab assay. J Appl Lab Med. 2019;3(5):857–863. doi: 10.1373/jalm.2018.026476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.US Food and Drug Administration. November 2021 501(K) clearances. https://www.fda.gov/medical-devices/510k-clearances/november-2021-510k-clearances. Accessed 10 February 2022.
- 39.Finn G, Mace S, Chu R, et al Development of a Hydrashift 2/4 isatuximab assay to mitigate interference with monoclonal protein detection on immunofixation electrophoresis in vitro diagnostic tests in multiple myeloma. Poster presented at the Virtual Scientific Meeting of the American Society of Hematology. 5-8 December 2020. Poster 1562.
- 40.Murray DL, Puig N, Kristinsson S, et al. Mass spectrometry for the evaluation of monoclonal proteins in multiple myeloma and related disorders: an International Myeloma Working Group Mass Spectrometry Committee Report. Blood Cancer J. 2021;11(2):24. doi: 10.1038/s41408-021-00408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]