Abstract
Background
Important, but insufficient, gains have been achieved in access to and delivery of oral health care since the 2000 US surgeon general’s report on oral health in America. Access to care has increased for children and young adults, but considerable work remains to meet the oral health care needs of all people equitably. The National Institutes of Health report, Oral Health in America: Advances and Challenges, reviews the state of the US oral health care system, achievements made since 2000, and remaining challenges. In this article, the authors highlight key advances and continuing challenges regarding oral health status, access to care and the delivery system, integration of oral and systemic health, financing of oral health care, and the oral health workforce.
Results
Public insurance coverage has increased since 2000 but remains limited for many low-income, minority, and older adult populations. The oral health care workforce has expanded to include new dental specialties and allied professional models, increasing access to health promotion and preventive services. Practice gains made by women and Asian Americans have not extended to other minority demographic groups. Oral health integration models are improving access to and delivery of patient-centered care for some vulnerable populations.
Conclusions and Practical Implications
Coordinated policies and additional resources are needed to further improve access to care, develop dental insurance programs that reduce out-of-pocket costs to lower-income adults, and improve the integration of oral and medical health care delivery targeting a common set of patient-centered outcomes. Dental care professionals need to fully participate in meaningful and system-wide change to meet the needs of the population equitably.
Key Words: Oral Health in America, access, workforce, insurance, integration, dental practice, disparities
Abbreviation Key: ACA, Patient Protection and Affordable Care Act; CHIP, Children’s Health Insurance Program; DSO, Dental support organization; FQHC, Federally qualified health center; HPV, Human papillomavirus; HURE, Historically underrepresented races and ethnicities; MA, Medicare Advantage

The 2000 surgeon general’s report, Oral Health in America, revealed stark disparities and inequities in oral disease burden and health care access in the United States.1 In 2003, the surgeon general issued a call to action to address these challenges.2 Numerous federal and state government programs, professional organizations, and private practices created initiatives to increase the capabilities and diversity of the oral health care workforce, expand collaborations between dental and medical providers, expand dental science and technology, and improve access to care. The 2021 National Institutes of Health report, Oral Health in America: Advances and Challenges, 3 describes advances toward these goals over the past 20 years, along with challenges. The report details the unequal burden of oral health conditions across population groups and highlights promising new directions for health care delivery.
The purpose of the oral health care system is to meet the oral health needs of the entire population. Yet it does not meet the needs of the population at this time, despite advances made since the 2003 call to action. A 2018 guest editorial in The Journal of the American Dental Association described the US dental care system as stuck in a low-level equilibrium,4 in which the supply of oral health care services matches the effective demand for services, given existing service prices and available community income and financing. The equilibrium is low because there is substantial unmet demand among groups priced out of the system, and the system appears unable to accommodate this unmet demand. Populations with insufficient access to oral health care include adults with no private or public dental insurance; people who are frail or have complex health care needs; people who are lesbian, gay, bisexual, or transgender; people living in Health Professional Shortage Areas; and people living in long-term care facilities.3
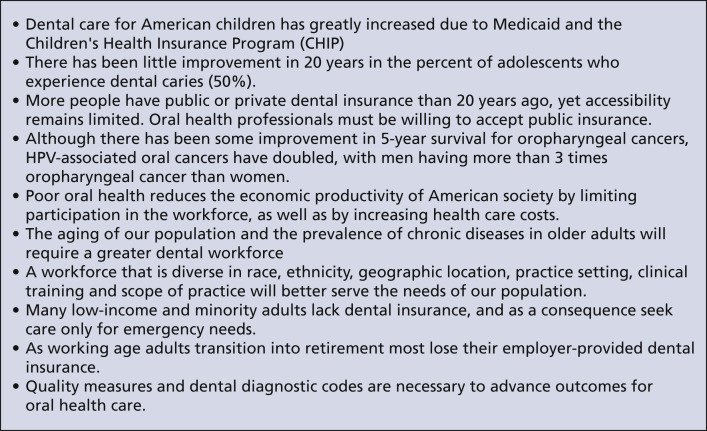
The report highlighted 10 messages that are critical to oral health care practice (Figure 1 ) and important changes in oral health and access to care, along with barriers that remain unaddressed. Our article highlights key elements of the report, including advances in funding and delivery of oral health care for children, strengthening of the insurance backbone allowing some additional Americans to get oral health care, efforts to improve integration with the medical system, some diversification of the workforce as well as additional practice models, and the continuing challenges in access to oral health care. Funding, medical care integration, workforce, and access are interrelated features of oral health care delivery, and addressing each of these is necessary to creating a well-designed system that equitably meets the needs of the population.
Figure 1.
Summary messages for dental practice. HPV: Human papillomavirus. Source: National Institutes of Health.3
Oral Health in America
Overall, oral health status has improved somewhat since 2000.5 The average number of missing permanent teeth has fallen from nearly 6 to less than 3.6 Edentulism has declined to 2% among working-age adults and 17% among adults aged 65 through 74 years.6 There has been no improvement in the prevalence of caries and untreated caries. Caries prevalence is similar across income and racial or ethnic groups. However, more than 40% of people who are in low-income groups have untreated caries compared with 9% among those in groups that are not low income, and untreated caries prevalence is 36% among Blacks and 23% among Hispanics compared with 18% among non-Hispanic Whites.7 Racial disparities persist even after controlling for income.
Nearly 60% of adults 65 years and older have periodontal disease.8 The prevalence of any periodontitis is higher among low-income and racial or ethnic minority populations than higher-income or White and non-Hispanic populations. Older Americans also have higher prevalence than younger people of medical comorbidities that affect oral health, including hypertension, heart disease, and dementia.9 , 10 Oropharyngeal cancer prevalence is also increasing, despite reductions in cigarette smoking, primarily owing to the increasing prevalence of human papillomavirus infection.11
Access to Care and Oral Care Delivery
The percentage of Americans with an annual oral health care visit increased from 2000 through 2018, particularly among children younger than 18 years (from 74% in 2000 to 86% in 2018).12 Race or ethnicity and income-level differences seen in 2000 were largely erased by 2018. Annual visit rates among older adults increased from 57% in 2000 to 66% in 2018, but rates did not change among adults aged 18 through 64 years (66% in 2018). Differences also persisted across race or ethnicity and income groups for all adults older than 18 years: in 2018, less than one-half of older adults living below 200% of a federal poverty guideline had a dental visit.
Access to comprehensive oral health care continues to be one of the biggest challenges within the oral health care system and a key driver of oral health care inequity. Many Americans regularly seek care for nontraumatic dental conditions in hospital emergency departments that are not equipped to provide comprehensive or definitive oral health care.13 Most patients seeking care in the emergency department are uninsured, qualify for Medicaid,14 or are unable to find a dental office that accommodates their work schedule.15 Others simply cannot afford the high deductibles and co-payments of private dental insurance programs.16 , 17
During the first year of the COVID-19 pandemic, it became evident that dentistry was not viewed as an essential health care service. Dental practices were largely closed to nonemergency care. The American Dental Association leadership responded, assuring Americans, “Dentistry is an essential health care service because of its role in evaluating, diagnosing, preventing or treating oral diseases, which can affect systemic health.”18 As of 2018, 75% of oral health care services were diagnostic or preventive, and 12% were restorative.19
Practice setting
As of 2018, 91% of active dentists worked in private practice settings. The remainder practiced in dental schools, military and Veterans Administration clinics, community and other public health practices, and hospitals (Health Policy Institute, American Dental Association, unpublished data, August 26, 2019). As of 2021, 46% of private practice dentists were in solo practice. Although solo practice remains the most common setting, group and corporate practices are becoming more common, with over 10% of dentists affiliated with a dental support organization (DSO).20
Private Practices
Private practices typically serve patients who are privately insured or able to self-pay for care; less than 40% of dentists accept Medicaid or Children’s Health Insurance Program (CHIP) payments. Private practices are located predominantly in highly populated, affluent regions. This results in more than 600 Health Resources and Services Administration–designated dental Health Professional Shortage Areas nationwide; many are rural areas with a combined population of more than 34 million people.21 , 22 Rural populations also have longer travel times to providers and lower rates of insurance coverage22; together, these factors make rural residents less likely to use preventive services and more likely to use emergency care. Racial or ethnic disparities in dental outcomes are also larger in rural areas.23, 24, 25
Safety Net Clinics
Safety net clinics, including dental schools and federally qualified health centers (FQHCs), serve as care delivery sites for millions of adults and children who are uninsured or enrolled in public insurance. From 2001 through 2020, the number of people obtaining oral health care at FQHCs increased from 1.4 million to 5.2 million; in 2017, one-third of these patients were younger than 18 years.26 Of these, 88.5% were Medicaid or CHIP beneficiaries. Although all FQHCs are required to provide dental services, some rely on referral mechanisms.27
DSOs
DSOs provide centralized practice management and group-purchasing services to affiliated dentists. A 2017 survey of 47 DSOs found that 61% of affiliated dentists had patients who were Medicaid or CHIP beneficiaries, and 43% cared exclusively or almost exclusively for Medicaid and CHIP beneficiaries.28 Thus, DSOs have become a substantial contributor to the dental safety net.
School-Based Oral Health Programs
School-based oral health programs, whether stand-alone or integrated with other health services, improve access to oral health care for students, deliver preventive services, improve oral health literacy, and connect students and families to a dental home. However, scope-of-practice laws in many states limit the effectiveness of school-based programs by requiring either an on-site dentist or a dentist’s prior examination for students to receive services in these efficient settings. Other challenges for these programs include getting consent forms signed and returned and avoiding interference with existing dentist-patient relationships.
Oral Health Integration
The separation of oral health care from the broader health care system began with the compartmentalization of dental and medical education, which led to distinct delivery, coding, and payment systems.29 Recognizing the relationships between many oral and systemic health conditions and their treatment, in 2003 the surgeon general called for integration of oral and general health care to meet the needs of the population.2 After this call to action, numerous models were developed, many following the road map provided by the federal Oral Health Strategic Framework, with financial support from the Health Resources and Services Administration.30 , 31
The Integration of Oral Health and Primary Care Practice32 and the Oral Health Delivery Framework33 models focus on improving access to care by providing risk assessment, caries prevention, patient education, and referrals for patients in smaller towns receiving services in safety net settings, using interprofessional practice collaborations.27 , 34, 35, 36 Oral Health Delivery Framework sites successfully integrated oral health screenings and fluoride varnish application into medical visits, followed by a dentist referral.
Commercial insurers and health systems have used integration to provide patient-centered care, improve patient health, and reduce costs.34 , 37 Insurers have used integration to provide dental examinations and prophylaxis to pregnant women, children, and adults with medical comorbidities.38, 39, 40 Health systems that combine care delivery and coverage have used clinic colocation, shared clinic workflows, and fully integrated electronic health records to facilitate integration of care and improved quality measures41; fully integrated dental offices were found to double care-gap closure for older adults compared with nonintegrated offices.42
Despite progress, barriers at multiple levels limit more widespread integration of oral and medical health care delivery.34 , 43 Clinical barriers include perceived limits to scope of practice between dental and medical providers, inadequate cross-discipline training, concerns about patient acceptance, and limited demonstration of clinical effectiveness.34 Technical barriers include lack of time and facility space and incompatibility of electronic records systems.34 Federal policies to increase access to care and implement quality measures associated with integration of oral and general health care for children were set in place by the Patient Protection and Affordable Care Act (ACA),44 but integration and access to care efforts for adults have lagged owing to the exclusion of comprehensive adult dental benefits in most Medicaid programs and absence of a universal, comprehensive Medicare dental benefit.45 , 46
Insurance Coverage and Financing
The percentage of Americans covered by dental insurance grew from 55% in 2009 to 80% in 2019. These increases in coverage resulted primarily from the expansion of Medicaid and CHIP and benefits extension for young adults to age 26 years in 2010 after the passage of the ACA.47
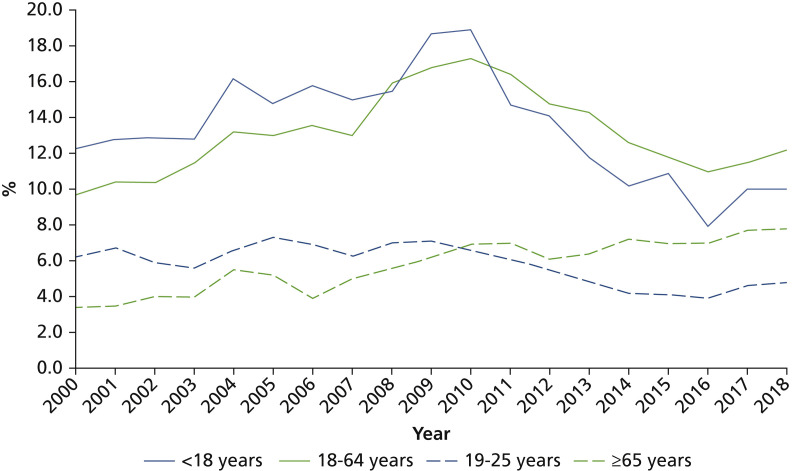
From 2011 through 2014, 56% of people with private dental insurance had a dental visit in the past 12 months compared with 33% of those with public insurance and 26% of those with no insurance. Among children with Medicaid and CHIP coverage, use of dental services nearly doubled from 2009 (28%) through 2020 (50%).48 However, the ACA’s successes have not reached all underserved populations.49 Extending benefits to young adults (aged 19-25 years) in 2010 accounted for most of the increase in annual dental visits.50 Use increases may have been limited by dentist supply constraints, low rates of Medicaid acceptance, and poor oral health literacy.49 Furthermore, many of the improvements since 2010 largely reversed negative trends seen from 2000 through 2010. For example, data show improvements in rates of delayed or nonreceipt of needed oral health care from 2000 through 2018 for children and young adults, but rates have not improved for adults overall and have doubled for older adults (Figure 2 ).
Figure 2.
Delay or nonreceipt of needed oral health care during the past 12 months due to cost, by selected age group: United States, 2000-2018. Source: National Center for Health Statistics.12
Cost continues to be a major barrier to receiving oral health care. Unlike medical insurance, under which 89% of costs are covered by insurance and preventive services are fully covered, dental out-of-pocket costs can exceed 40% for insured patients.51 Financial barriers play a larger role in access to oral health care than for any other type of health care; almost 25% of adults with incomes below the federal poverty guideline deferred needed oral health care because of cost in 2014 and 2015.16 Furthermore, the Centers for Medicare & Medicaid Services accounted for 37% of medical care spending but only 10% of dental care spending in 2019.51 This stark difference suggests that the oral health care needs of many vulnerable populations are not addressed adequately by current programs.
Most adults who qualify for Medicare and Medicaid lack dental insurance. Medicare offers essentially no dental benefit, although Medicare recipients may purchase dental benefits from a Medicare Advantage (MA) plan, if one is available. In the past 20 years, enrollment in MA plans increased from approximately 7% to 34% (covering ≈ 22 million people).52 Approximately two-thirds of MA enrollees have a dental benefit; this increased coverage and access has benefited primarily higher-income older adults, increasing disparities in oral health care delivery.53 As of 2019, 19 states and the District of Columbia provided extensive adult dental benefits under Medicaid, 15 provided limited benefits, 12 provided emergency-only benefits, and 4 offered no benefits.54 Lack of dental insurance has been shown to transfer unmet oral health care costs to the medical system through patients’ higher use of emergency and urgent-care services.
The Dental Workforce
In 2022 in the United States, there are more than 200,000 active dentists, or approximately 61 dentists per 100,000 residents, ranging by state from 41 per 100,000 in Alabama through 104 per 100,000 in the District of Columbia.55 There are also approximately 194,000 dental hygienists, 312,000 dental assistants, and 30,000 dental laboratory technicians.56, 57, 58 Most dentists (80%) are in general practice, with the remainder spread between 12 dental specialties, including new specialties of dental anesthesiology (2019), oral medicine (2020), and orofacial pain (2020).55 Since 2000, the supply of dentists has increased by 23%. The largest increases have been among pediatric dentists (103%) and endodontists (42%), whereas the number of dental public health specialists fell by 14%.
The 2003 surgeon general call to action sought efforts to increase the diversity of the dental workforce to better reflect the demographics of dental patients.2 Such efforts have had some success over the past 20 years. The number of women enrolling in dental schools has increased substantially; women now make up approximately one-half of dental school graduates and are expected to make up one-half of active dentists by 2040.59 Efforts to increase the racial and ethnic diversity of the dental workforce have had less success. There is a higher percentage of practicing dentists who are White or Asian than in the general population, whereas Black and Hispanic dentists are underrepresented.60 Since 2000, there have been modest increases in dental school enrollments among Hispanics. Enrollment rates from other historically underrepresented races and ethnicities (HURE) have remained stagnant, despite increases in the number of applicants. HURE graduates also incur higher educational debt on average than non-HURE graduates; thus, education costs may be a disincentive to apply or enroll.61
The call to action identified the need for improved access to primary oral health care for low-income and racial or ethnic minority populations.2 Allied dental care professionals, such as hygienists and dental therapists, can facilitate care for vulnerable populations who face barriers in seeking care.62 , 63 In many states, scope-of-practice laws restrict these providers from caring for patients in accessible settings.64 Efforts to change these laws have had limited success. Thirteen states now allow dental therapists to practice, but they are active only in 5 states.62
Moving Forward
The 2021 Oral Health in America report showed that although important advances were made in oral health care workforce development, delivery, and financing over the past 20 years, these advances have been insufficient to solve the problems of cost and access to oral health care services.3 We highlight 3 strategies discussed in the report that could help advance dental practice toward equitably meeting the oral health care needs of the US population.
Strategy 1. Make dental care services an essential benefit for private and public insurance
The dental financing model does not afford all Americans equal access to oral health care and diminishes oral health’s value in the overall health care system; payment reform is necessary to increase access and quality of care and reduce health disparities.4 Although there have been improvements for children, increases in dental insurance coverage over the past 20 years have largely bypassed Medicare beneficiaries, Medicaid-eligible adults, and insured people who cannot afford the high out-of-pocket costs of their plans. Including oral health care in comprehensive health coverage can increase oral health care access and reduce overall health costs.65 The US economic recovery depends on a healthy workforce, and oral health is an essential component of health.
Major financing reform of medicine in the United States has come largely through publicly funded programs. To bring about insurance reform in oral health care, insurers, working with public and private purchasers, dental and dental hygiene groups, and public health professionals at the state and federal levels, must identify and implement payment reform pilot programs to show the value of such reforms for improving the US population’s oral and general health.
Many have supported integrating a Medicare dental benefit into Medicare Part B outpatient medical coverage53 , 66 to further promote the integration of medical and oral health care, adoption of oral health care quality measures, and participation of dental practitioners in accountable care organizations. Means testing could be used to reach at least low-income enrollees. However, a means-tested benefit, beyond existing tests to set premiums and co-payments, could leave services unaffordable to some enrollees and could limit dentists’ enrollment as Medicare providers, thereby increasing the burden on resource-constrained safety net providers.53
In addition to establishing an essential dental benefit for adults, federal and state policy makers could support patient demand and provider acceptance and reduce out-of-pocket costs by increasing reimbursement rates for publicly funded dental benefits.
Strategy 2. Incorporate dental or oral health care services demand into workforce planning
The 2003 call to action suggested incorporating the future demand for oral health care services into workforce planning. Others have repeated these calls.67 , 68 There is no estimate of the optimal number of general dentists, specialists, or allied dental providers for the population. It is not known whether the current workforce size meets the current demand for care, but it is clear that expanding dental coverage will increase demand for services and exacerbate any existing supply constraints, particularly for primary oral health care.
The US population is aging and becoming more urban and racially and ethnically diverse.69 These trends are likely to exacerbate existing inequities in access to oral health care services associated with inadequate insurance coverage, place-based limits on dental services, and lack of diversity in the oral health care workforce. Policy makers and dental education administrators will need to be forward thinking to align the capabilities and demographic characteristics of the oral health care system workforce with the future demand for care. The complex care needs of an aging population would support the establishment of federally supported dental specialty and hygiene training programs in geriatric oral health and patients with special health care needs with clinical training incorporated into assisted living and other long-term care facilities.
Strategy 3. Increase the integration of oral and medical care delivery
Oral health integration is a key strategy for improving oral health care access, quality, and outcomes. Increasing prevalence of medical comorbidities will increase the importance of medical-dental integration to effectively manage patient care needs. A newly established partnership between the Centers for Disease Control and Prevention and the National Association of Chronic Disease Directors should help create a national medical-dental integration framework.70 2019 updates to the patient-centered dental home concept include integration of standardized definitions and performance measures, which may help integrate care for defined populations.71 Additional models of care delivery, even in rural settings, are showing promise.72
To achieve the promise of oral health integration and better align oral and medical health care delivery, interprofessional partnerships between dental and medical practitioners are needed. In addition, the long-standing system-level barriers that perpetuate the separation of dental and medical professions, education, care, and payment systems need to be addressed.73 Dental and medical education share a common scientific foundation. Integrating dental and medical education programs and internships could improve cross-disciplinary knowledge and create champions for oral health integration into primary care.74, 75, 76 Oral health care and payment systems also need to focus more on oral health outcomes and less on procedures.4 Some integrated health systems already have adopted quality measures for oral health, but change is slow among independent dental providers.77 The use of a common dental and medical diagnostic coding system would support the extension of quality measures.
The lack of interoperability of electronic dental and medical records is a major barrier to communication and integration.41 , 78 Independent dental practices depend primarily on patient self-reported health status and treatment history. A 2019 comparison of parent-reported health information in children’s dental records and their actual medical records showed substantial reporting errors.79 Enabling web-based access to patient medical charts, such as through the Care Everywhere website,80 would improve the accuracy of information available to dental providers, informing treatment decisions. It also may improve communication between dental and medical providers. Policy makers should support efforts to provide online access to patients’ medical charts.
Conclusions
The US oral health care system requires major changes to meet the needs of the population equitably. The opportunities described in the Oral Health in America report and highlighted above are mutually dependent. Public and private stakeholders need to coordinate a meaningful and systemwide approach to eliminating barriers and inequities in oral health care access, reducing costs, and improving oral health outcomes for Americans.
Biographies
Dr. Fellows is a senior investigator, Kaiser Permanente Center for Health Research, Portland, OR.
Dr. Atchison is a professor, School of Dentistry and Fielding School of Public Health, University of California, Los Angeles, Los Angeles, CA.
Dr. Chaffin is the chief dental officer, Delta Dental of Iowa, Johnston, IA.
Dr. Chávez is the director, Pacific Center for Equity in Oral Health Care, and a professor, Department of Diagnostic Sciences, University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco, CA.
Dr. Tinanoff is a professor, Department of Orthodontics and Pediatric Dentistry, University of Maryland School of Dentistry, Baltimore, MD.
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
Footnotes
Disclosures. None of the authors reported any disclosures.
ORCID Numbers. Jeffrey L. Fellows: 0000-0001-8839-2851; Norman Tinanoff: 0000-0002-6810-7432.
The authors thank Neon Brooks for her substantive and timely editing of manuscript drafts and Kelly Jewell for her administrative help organizing citations.
Any statements or conclusions presented in this article are those of the authors.
References
- 1.Oral Health in America: A Report of the Surgeon General. US Department of Health and Human Services; 2000. [Google Scholar]
- 2.Office of the Surgeon General . National Institute of Dental and Craniofacial Research (US); 2003. National Call to Action to Promote Oral Health. [PubMed] [Google Scholar]
- 3.Oral Health in America: Advances and Challenges. National Institutes of Health; 2021. [Google Scholar]
- 4.Vujicic M. Our dental care system is stuck: and here is what to do about it. JADA. 2018;149(3):167–169. doi: 10.1016/j.adaj.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Rozier R.G., White B.A., Slade G.D. Trends in oral diseases in the U.S. population. J Dent Educ. 2017;81(8):eS97–eS109. doi: 10.21815/JDE.017.016. [DOI] [PubMed] [Google Scholar]
- 6.Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2019. [Google Scholar]
- 7.Bashir N.Z. Update on the prevalence of untreated caries in the US adult population, 2017-2020. JADA. 2022;153(4):300–308. doi: 10.1016/j.adaj.2021.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Eke P.I., Thornton-Evans G.O., Wei L., Borgnakke W.S., Dye B.A., Genco R.J. Periodontitis in US adults: National Health and Nutrition Examination Survey 2009-2014. JADA. 2018;149(7):576–588, e6. doi: 10.1016/j.adaj.2018.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.2019 Profile of Older Americans. Administration on Aging; 2020. [Google Scholar]
- 10.Delwel S., Binnekade T.T., Perez R., Hertogh C.M.P.M., Scherder E.J.A., Lobbezoo F. Oral hygiene and oral health in older people with dementia: a comprehensive review with focus on oral soft tissues. Clin Oral Investig. 2018;22(1):93–108. doi: 10.1007/s00784-017-2264-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cancer stat facts: oral cavity and pharynx cancer National Cancer Institute, National Instututes of Health. https://seer.cancer.gov/statfacts/html/oralcav.html
- 12.Health, United States, 2019, selected tables. Centers for Disease Control and Prevention. Accessed January 10, 2022. 10.15620/cdc:100685 [DOI]
- 13.Allareddy V., Rampa S., Lee M.K., Allareddy V., Nalliah R.P. Hospital-based emergency department visits involving dental conditions: profile and predictors of poor outcomes and resource utilization. JADA. 2014;145(4):331–337. doi: 10.14219/jada.2014.7. [DOI] [PubMed] [Google Scholar]
- 14.Rampa S., Wilson F.A., Allareddy V. Trends in dental-related emergency department visits in the State of California from 2005 to 2011. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(4):426–433. doi: 10.1016/j.oooo.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Koziol-McLain J., Price D.W., Weiss B., Quinn A.A., Honigman B. Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J Emerg Nurs. 2000;26(6):554–563. doi: 10.1067/men.2000.110904. [DOI] [PubMed] [Google Scholar]
- 16.Vujicic M., Buchmueller T., Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff (Millwood) 2016;35(12):2176–2182. doi: 10.1377/hlthaff.2016.0800. [DOI] [PubMed] [Google Scholar]
- 17.National Health Expenditure Data Table 08: Dental Services Expenditures 2020. Centers for Medicare and Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
- 18.Statement on dentistry as essential health care American Dental Association. https://www.ada.org/about/press-releases/2020-archives/statement-on-dentistry-as-essential-health-care#:∼:text=CHICAGO%2C%20August%2010%2C%202020%20%E2%80%94,integral%20part%20of%20overall%20health
- 19.Guay A.H., Blatz A., Harrison B. Health Police Institute research brief: demand for restorative dental care varies by patient age. American Dental Association. https://www.ada.org/- /media/project/ada-organization/ada/adaorg/files/resources/research/hpi/hpibrief_restorative_care_demand_patient_age.pdf
- 20.The dentist workforce American Dental Association. https://www.ada.org/resources/research/health-policy-institute/dentist-workforce
- 21.What is shortage designation? Health Resources and Services Administration. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation
- 22.Barnett S., Belanger K., Borders T., et al. National Advisory Committee on Rural Health and Human Services; 2018. Improving Oral Health Care Services in Rural America. Policy Brief and Recommendations. [Google Scholar]
- 23.Geiger C.K., Kranz A.M., Dick A.W., Duffy E., Sorbero M., Stein B.D. Delivery of preventive oral health services by rurality: a cross-sectional analysis. J Rural Health. 2019;35(1):3–11. doi: 10.1111/jrh.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quandt S.A., Chen H., Bell R.A., et al. Disparities in oral health status between older adults in a multiethnic rural community: the rural nutrition and oral health study. J Am Geriatr Soc. 2009;57(8):1369–1375. doi: 10.1111/j.1532-5415.2009.02367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schroeder S., Adamsen C., Ward C. Dental care utilization and service needs among American Indian/Alaska Native/Native Hawaiian elders: 2008 to 2017. J Aging Health. 2019;31(10):1917–1940. doi: 10.1177/0898264318800598. [DOI] [PubMed] [Google Scholar]
- 26.National Health Center Program Uniform Data System (UDS) awardee data. https://data.hrsa.gov/tools/data-reporting/program-data/national
- 27.Crall J.J., Pourat N., Inkelas M., Lampron C., Scoville R. Improving the oral health care capacity of federally qualified health centers. Health Aff (Millwood) 2016;35(12):2216–2223. doi: 10.1377/hlthaff.2016.0880. [DOI] [PubMed] [Google Scholar]
- 28.Langelier M.W.S., Surdu S., Mertz E., Wides C. Oral Health Workforce Research Center; 2017. Trends in the Development of the Dental Service Organization Model: Implications for the Oral Health Workforce and Access to Services. [Google Scholar]
- 29.Mertz E.A. The dental-medical divide. Health Aff (Millwood) 2016;35(12):2168–2175. doi: 10.1377/hlthaff.2016.0886. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen V., Daniel M., Joskow R., et al. Impact of oral health service expansion funding at health centers in the United States. J Public Health Dent. 2020;80(4):304–312. doi: 10.1111/jphd.12385. [DOI] [PubMed] [Google Scholar]
- 31.US Public Health Service Oral Health Coordinating Committee . US Department of Health and Human Services, Health Resources and Services Administration; 2014. Oral Health Strategic Framework, 2014–2017. [Google Scholar]
- 32.Health Resources and Services Administration. Integration of Oral Health and Primary Care Practice. Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration; 2014. Accessed January 10, 2022. https://www.hrsa.gov/sites/default/files/hrsa/oralhealth/integrationoforalhealth.pdf
- 33.Hummel J, Phillips KE, Holt B, Hayes C. Oral Health: an Essential Component of Primary Care. Seattle WA: Qualis Health; June 2015. Accessed January 10, 2022. https://oralhealth.hsdm.harvard.edu/publications/oral-health-essential-component-primary-care
- 34.Harnagea H., Couturier Y., Shrivastava R., et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ Open. 2017;7(9) doi: 10.1136/bmjopen-2017-016078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dalal M., Clark M., Quiñonez R.B. Part 1: how to integrate oral health into pediatric primary care. Contemporary Pediatr J. 2019;36(1):29–33. [Google Scholar]
- 36.Harnagea H, Lamothe L, Couturier Y, et al. From theoretical concepts to policies and applied programmes: the landscape of integration of oral health in primary care. BMC Oral Health. 2018;18(1):23. doi: 10.1186/s12903-018-0484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Institute of Medicine . National Academies Press; 2011. Advancing Oral Health in America. [Google Scholar]
- 38.Albert D.A., Sadowsky D., Papapanou P., Conicella M.L., Ward A. An examination of periodontal treatment and per member per month (PMPM) medical costs in an insured population. BMC Health Serv Res. 2006;6:103. doi: 10.1186/1472-6963-6-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United Healthcare Insurance Company Medical Dental Integration Study. United Healthcare; 2013. [Google Scholar]
- 40.Nasseh K., Vujicic M. Health Policy Institute Research Brief: dental care utilization steady among working-age adults and children, up slightly among the elderly. American Dental Association. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_1016_1.pdf
- 41.Jones J.A., Snyder J.J., Gesko D.S., Helgeson M.J. Integrated medical-dental delivery systems: models in a changing environment and their implications for dental education. J Dent Educ. 2017;81(9):eS21–eS29. doi: 10.21815/JDE.017.029. [DOI] [PubMed] [Google Scholar]
- 42.Mosen D.M., Banegas M.P., Dickerson J.F., et al. Examining the association of medical-dental integration with closure of medical care gaps among the elderly population. JADA. 2021;152(4):302–308. doi: 10.1016/j.adaj.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Atchison K.A., Weintraub J.A., Rozier R.G. Bridging the dental-medical divide: case studies integrating oral health care and primary health care. JADA. 2018;149(10):850–858. doi: 10.1016/j.adaj.2018.05.030. [DOI] [PubMed] [Google Scholar]
- 44.Rosenbaum S. The Patient Protection and Affordable Care Act: implications for public health policy and practice. Public Health Rep. 2011;126(1):130–135. doi: 10.1177/003335491112600118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Donoff B., McDonough J.E., Riedy C.A. Integrating oral and general health care. N Engl J Med. 2014;371(24):2247–2249. doi: 10.1056/NEJMp1410824. [DOI] [PubMed] [Google Scholar]
- 46.McDonough J. Might oral health be the next big thing? Milbank Q. 2016;94(4):720–723. doi: 10.1111/1468-0009.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.2019 Dental Benefits Report: Enrollment. National Association of Dental Plans; 2020. [Google Scholar]
- 48.Medicaid Payment Policy for Federally Qualified Health Center. Medicaid and CHIP Payment and Access Commission; 2017. [Google Scholar]
- 49.Song J., Kim J.N., Tomar S., Wong L.N. The impact of the Affordable Care Act on dental care: an integrative literature review. Int J Environ Res Public Health. 2021;18(15):7865. doi: 10.3390/ijerph18157865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lau J.S., Adams S.H., Park M.J., Boscardin W.J., Irwin C.E., Jr. Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatr. 2014;168(12):1101–1106. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- 51.National health expenditure data. Centers for Medicare and Medicaid Services. www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData
- 52.Jacobson G, Freed M, Damico A, Neuman T. A dozen facts about Medicare Advantage in 2019. Kaiser Family Foundation. Accessed December 28, 2021. https://www.kff.org/medicare/issue-brief/a-dozen-facts-about-medicare-advantage-in-2019
- 53.Simon L., Giannobile W.V. Is it finally time for a Medicare dental benefit? N Engl J Med. 2021;385(23):e80. doi: 10.1056/NEJMp2115048. [DOI] [PubMed] [Google Scholar]
- 54.Medicaid adult dental benefits: an overview. Center for Health Care Strategies. https://www.chcs.org/resource/medicaid-adult-dental-benefits-overview
- 55.Supply of dentists in the U.S.: 2001-2021. American Dental Association. https://www.ada.org/resources/research/health-policy-institute/dentist-workforce
- 56.Occupational employment and wages, May 2021: 29-1292 dental hygienists. https://www.bls.gov/oes/current/oes291292.htm
- 57.Occupational employment and wages, May 2021: 31-9091 dental assistants. https://www.bls.gov/oes/current/oes319091.htm
- 58.Occupational employment and wages, May 2021: 51-9081 dental laboratory technicians. https://www.bls.gov/oes/current/oes519081.htm
- 59.Munson B., Vujicic M. Projected supply of dentists in the United States, 2020–2040. Health Policy Institute Research Brief. American Dental Association. https://www.ada.org/-/media/project/adaorganization/ada/ada-org/files/resources/research/hpi/hpibrief_0521_1.pdf
- 60.Mertz E.A., Wides C.D., Kottek A.M., Calvo J.M., Gates P.E. Underrepresented minority dentists: quantifying their numbers and characterizing the communities they serve. Health Aff (Millwood) 2016;35(12):2190–2199. doi: 10.1377/hlthaff.2016.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mertz E., Calvo J., Wides C., Gates P. The Black dentist workforce in the United States. J Public Health Dent. 2017;77(2):136–147. doi: 10.1111/jphd.12187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Expanding access to care through dental therapy. American Dental Hygienists’ Association. https://www.adha.org/resources-docs/Expanding_Access_to_Dental_Therapy.pdf
- 63.Health Resources and Services Administration . National Advisory Committee on Rural Health and Human Services; 2018. Improving Oral Health Care Services in Rural America. [Google Scholar]
- 64.Cripe KM. Ohio State Dental Board implements teledentistry rules. BMD Alerts. May 26, 2020. Accessed January 10, 2022. https://www.bmdllc.com/resources/blog/ohio-state-dental-board-implements-teledentistry-rules
- 65.Listl S., Quiñonez C., Vujicic M. Including oral diseases and conditions in universal health coverage. Bull World Health Organ. 2021;99(6):407. doi: 10.2471/BLT.21.285530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Valachovic R. A dental benefit in Medicare: a matter of when and how. NYU Dentistry Center for Oral Health Policy and Management. https://wp.nyu.edu/collegeofdentistry-prohmotion/a-dental-benefit-in-medicare-a-matter-of-when-and-how
- 67.Ahern S., Woods N., Kalmus O., Birch S., Listl S. Needs-based planning for the oral health workforce: development and application of a simulation model. Hum Resour Health. 2019;17(1):55. doi: 10.1186/s12960-019-0394-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Birch S., Ahern S., Brocklehurst P., et al. Planning the oral health workforce: time for innovation. Community Dent Oral Epidemiol. 2021;49(1):17–22. doi: 10.1111/cdoe.12604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Annual estimates of the resident population for selected age groups by sex for the United States: April 1, 2010 to July 1, 2019. US Census Bureau. Accessed January 10, 2022. https://www.census.gov/newsroom/press-kits/2020/population-estimates-detailed.html
- 70.CDC announces medical-dental integration partnership. Centers for Disease Control and Prevention. https://www.cdc.gov/oralhealth/about/md-integration.html
- 71.Damiano P., Reynolds J., Herndon J.B., McKernan S., Kuthy R. The patient-centered dental home: a standardized definition for quality assessment, improvement, and integration. Health Serv Res. 2019;54(2):446–454. doi: 10.1111/1475-6773.13067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pawloski C, Hilgert J, Senturia K, Davis S, Koday M, Cunha-Cruz J. Medical-dental integration in a rural community health center: a qualitative program evaluation. Health Promot Pract. Published online April 14, 2021. https://doi.org/10.1177/15248399211002832 [DOI] [PubMed]
- 73.Valentijn P.P., Boesveld I.C., van der Klauw D.M., et al. Towards a taxonomy for integrated care: a mixed-methods study. Int J Integr Care. 2015;15:e003. doi: 10.5334/ijic.1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Park S.E., Donoff R.B., Saldana F. The impact of integrating oral health education into a medical curriculum. Med Princ Pract. 2017;26(1):61–65. doi: 10.1159/000452275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hartnett E., Haber J., Catapano P., et al. The impact of an interprofessional pediatric oral health clerkship on advancing interprofessional education outcomes. J Dent Educ. 2019;83(8):878–886. doi: 10.21815/JDE.019.088. [DOI] [PubMed] [Google Scholar]
- 76.Haber J., Hartnett E., Allen K., et al. The impact of oral-systemic health on advancing interprofessional education outcomes. J Dent Educ. 2017;81(2):140–148. [PubMed] [Google Scholar]
- 77.Glassman P., Harrington M., Namakian M. The virtual ental home: improving the oral health of vulnerable and underserved populations using geographically distributed telehealth-enabled teams. University of the Pacific Dugoni School of Dentistry. https://dental.pacific.edu/sites/default/files/users/user244/VirtualDentalHome_PolicyBrief_Aug_2014_HD_ForPrintOnly.pdf
- 78.Atchison K.A., Rozier R.G., Weintraub J.A. National Academy of Medicine; 2018. Integration of Oral Health and Primary Care: Communication, Coordination, and Referral. [Google Scholar]
- 79.Kovalesky M.B., Unkel J.H., Reinhartz J., Reinhartz D. Discrepancies between dental parent-derived health histories and medical electronic health records. Pediatr Dent. 2019;41(5):371–375. [PubMed] [Google Scholar]
- 80.Ruley M., Walker V., Studeny J., Coustasse A. The Nationwide Health Information Network: the case of the expansion of health information exchanges in the United States. Health Care Manag (Frederick) 2018;37(4):333–338. doi: 10.1097/HCM.0000000000000231. [DOI] [PubMed] [Google Scholar]