Abstract
The aim of this study was to create an overview on the COVID-associated burdens faced by the oral and maxillofacial surgery (OMS) workforce during 1 year of the pandemic.
OMS hospitals and private practices nationwide were surveyed regarding health care worker (HCW) screening, infection status, pre-interventional testing, personal protective equipment (PPE), and economic impact. Participants were recruited via the German Society for Oral and Maxillofacial Surgery.
A total of 11 hospitals (416 employees) and 55 private practices (744 employees) participated. The HCW infection rate was significantly higher in private practices than in clinics (4.7% vs. 1.4%, p<0.01), although most infections in HCW occurred in private environment (hospitals 88.2%, private practice 66.7%). Pre-interventional testing was performed significantly less for outpatients in private practices than in hospitals (90.7% vs. 36.4%, p<0.01). Polymerase chain reaction (PCR) was used significantly more for inpatients in hospitals than in private practices (100.0% vs. 27.3%, p<0.01). FFP2/3 use rose significantly in hospitals (0% in second quarter vs. 46% in fourth quarter, p<0.05) and private practices (15% in second quarter vs. 38% in fourth quarter, p<0.01). The decrease in procedures (≤50%) was significantly higher in hospitals than in private practices (90.9% vs. 40.0%, p<0.01). Despite higher infection rates in private practices, declining procedures and revenue affected hospitals more.
Future COVID-related measures must adjust the infrastructure especially for hospitals to prevent further straining of staff and finances.
Keywords: COVID-19, Oral and maxillofacial surgery, Aerosol, Personal protective equipment, Pre-interventional testing, Healthcare workers
1. Introduction
With its origin reportedly in Wuhan, China, severe acute respiratory syndrome corona virus 2, or SARS-CoV-2, is a beta coronavirus that has caused a global pandemic. By now, more than 158 million infected and over 3.2 million fatalities worldwide have been documented, mostly due to respiratory failure or thromboembolism (Huang et al., 2020; Robert-Koch-Institut, Germany, 2021a, Robert-Koch-Institut, Germany, 2021b; Joint WHO-China Study, 2021; WHO, 2021; Ackermann et al., 2020). Health care systems worldwide are struggling with enormous numbers of infected patients as well as thinning numbers of health care workers (HCW) due to disease transmission (Erdem et al., 2021). HCWs could be at higher risk for becoming infected with SARS-CoV-2 because of working in COVID-19 hospital wards but also during routine clinical interventions (Bielicki et al., 2020).
The nature of the virus’s transmission seems to increase the risk of infection with SARS-CoV-2 during aerosol and droplet-generating procedures (AGP) (Gallagher et al., 2020). These AGP, for example, dental surgeries such as tooth extractions, are carried out routinely by HCWs in oral and maxillofacial surgery (OMS) facilities (Gallagher et al., 2020; Zimmermann and Nkenke, 2020).
Recommendations on personal protective equipment (PPE) use protecting against potentially infectious material existed before the COVID-19 pandemic. These included the use of gloves, masks, and goggles (Nejatidanesh et al., 2013). Because of the COVID-19 outbreak, an expansion was established containing FFP2/3 masks and gowns (Altermann et al., 2021, Robert-Koch-Institut, Germany, 2021a, Robert-Koch-Institut, Germany, 2021b; Bundesministerium für Arzneimittel und Medizinprodukte, 2021). However, data regarding the infection rates of HCWs as well as use and benefit of PPE in OMS facilities are sparse.
With hospitals managing high numbers of incoming and longtime COVID-19 patients, medical staff were shifted to establish COVID-19 wards as well as further intensive care capacities. By adding this to newly placed government implementations, a reduction in elective surgeries and diagnostics as well as bed capacities occurred (Zimmermann and Nkenke, 2020; Stöß et al., 2020). Long-term economic consequences can only be suspected currently and may keep health care systems occupied for several years to come.
As a part of the collaborative project “Bundesweites Forschungsnetz Angewandte Surveillance und Testung” (B-FAST) of the Network of University Medicine (NUM), Augsburg University Hospital was commissioned to acquire data on aerosol-producing medical fields including OMS. The study was supported by the German Society of Oral and Maxillofacial Surgery (DGMKG).
This study aims to present data from a nationwide survey of Oral and Maxillofacial Surgery hospitals and private practices regarding the impact of the COVID-19 pandemic on health care workers and on the economic situation of health care facilities.
2. Materials and methods
The present cross-sectional, explorative study was conducted using an online questionnaire created with Unipark, comprising 64 items designed by a panel of experts and based on review of the latest scientific publications. Hospitals and private practices were asked to participate in this survey inquiring about the application of PPE, HCW infection rates, pre-interventional testing, and economic development during the pandemic (Supplement 1).
Department heads of the OMS hospitals and practice owners were addressed in this nationwide questionnaire. Clinical departments as well as private practice owners were recruited via the DGMKG. The online questionnaire could be answered from December 16, 2020, to January 24, 2021.
Data management and statistical analysis were performed using SPSS IBM version 27.0. Categorical variables such as type of medical facility, presumed source of infection, pre-interventional testing of patients, and HCW screening are presented as absolute frequencies and percentages. HCW status was calculated as the proportion of the SARS-Cov-2−positive infections among HCW to the underlying total population and is expressed as percentage. Association between categorial variables was assessed using the χ2 test or Fisher exact test when appropriate. Also applied was the Friedmann test for related samples. The significance level was set as p<0.05.
The study was conducted in accordance with the Declaration of Helsinki and the Good Clinical Practice (GCP) guidelines. A positive ethical evaluation of the study was obtained from the Ethics Committee of the Faculty of Medicine of the Technical University Munich under accession number 713/20 S-SR.
3. Results
3.1. Study sample
A total of 11 hospitals (16.7%, 416 employees) and 55 private practices (83.3%, 744 employees) for OMS participated in the study. The majorities of hospitals had more than 800 beds, whereas most private practices treated 600 to 1199 patients per quarter (Table 1 ).
Table 1.
Participation hospitals and private practices for Oral and Maxillofacial Surgery. Distribution by numbers of beds and patients per quarter in private practices and hospital-based departments.
| Number of facilities | % | ||
|---|---|---|---|
| Total | 66 | 100.0 | |
| Hospital | 11 | 16.7 | |
| 100-199 beds | 1 | 9.1 | |
| 200-499 beds | 1 | 9.1 | |
| 500-799 beds | 1 | 9.1 | |
| >800 beds | 8 | 72.7 | |
| Private practice | 55 | 83.3 | |
| Less than 600 patients per quarter | 17 | 30.9 | |
| 600-1,199 patients per quarter | 21 | 38.2 | |
| 1,200–1,799 patients per quarter | 9 | 16.4 | |
| 1,800–2,399 patients per quarter | 5 | 9.1 | |
| 2400 or more patients per quarter | 3 | 5.5 |
3.2. Spectrum of operative interventions
Although implantology was performed in all participating private practices (98.1%), only half of the hospitals reported implants to be placed regularly. However, most hospitals performed cancer surgeries (compared to only 20.4% of private practices), orthognathic surgery, and traumatological reconstruction (Table 2 ).
Table 2.
Overview distribution of operative interventions.
| Private Practice | Clinic | |||
|---|---|---|---|---|
| Implantology | 53 | 98.1% | 6 | 54.5% |
| Orthognatic surgery | 9 | 16.7% | 10 | 90.0% |
| Traumatology | 5 | 9.3% | 10 | 90.9% |
| Cancer surgery | 11 | 20.4% | 11 | 100% |
3.3. Health care worker status
Overall, 3.5% of HCWs had a SARS-CoV-2- infection (Table 3 ). The rate of infected HCW was significantly higher in private practices than in hospital-based departments (p<0.01).
Table 3.
Distribution of COVID-19 positive healthcare workers in private practices and hospitals.
| Employees (in total) |
Employees (SARS-CoV-2 positive) |
p-value | ||||
|---|---|---|---|---|---|---|
| Number of facilities | Number of HCW | Number of facilities | Number of HCW | Rate of SARS-CoV-2 positive HCW (%) | ||
| Private Practice | 55 | 744 | 17 | 35 | 4.7 | <0.01 |
| Hospital | 11 | 416 | 6 | 6 | 1.4 | |
| Overall | 66 | 1160 | 23 | 41 | 3.5 | |
3.4. Source of infection
The survey showed social contacts in the private environment, not the workplace, as the primary source of infection of HCWs (Table 4 ). This is reflected in private practices (88.2%, n = 15) as well as in hospitals (66.7%, n = 4).
Table 4.
Distribution of infection sources in private practices and hospital-based departments.
| Private Practice |
Hospital based |
p-value | ||||
|---|---|---|---|---|---|---|
| Number of facilities | % | Number of facilities | % | |||
| No infected HCW | 38 | 69.1 | 5 | 45.5 | 0.171 | |
| Infected HCW | 17 | 30.9 | 6 | 55.5 | ||
| Private life | 15 | 88.2 | 4 | 66.7 | 0.716 | |
| At work | 0 | 0.0 | 1 | 16.7 | 1.00 | |
| During Interventions | 3 | 17.6 | 0 | 0.0 | 0.176 | |
| Without patient contact | 1 | 5.9 | 0 | 0.0 | 1.00 | |
| Unclear origin | 2 | 11.8 | 1 | 16.7 | 0.427 | |
3.5. Health care worker screening
There was no significant difference in the frequency of HCW screening between hospitals and private practices (Table 5 ). Nevertheless, a significant difference was observed regarding the type of testing. Hospitals have tested their employees significantly more often using polymerase chain reaction (PCR) (57.1%, n = 4 vs. 16.7%, n = 5, p<0.05) compared with private practices, whereas the latter was using preferably antigen testing for HCW screening (70.0%, n = 21 vs. 28.6%, n = 2, p<0.05).
Table 5.
Screening of healthcare workers with distribution of testing methods between private practice and hospitals.
| Private Practice |
Hospital based |
p-value | |||||
|---|---|---|---|---|---|---|---|
| Number of facilities | % | Number of facilities | % | ||||
| HCW screening | 55 | 100.0 | 11 | 100.0 | |||
| No testing | 25 | 45.6 | 4 | 36.4 | 0.753 | ||
| Testing | 30 | 54.4 | 7 | 63.6 | 0.061 | ||
| Antibody test | 4 | 13.3 | 1 | 14.3 | 0.920 | ||
| PCR | 5 | 16.7 | 4 | 57.1 | 0.028 | ||
| Antigen test | 21 | 70.0 | 2 | 28.6 | 0.046 | ||
HCW: healthcare worker.
3.6. Pre-interventional testing
Significantly more outpatients were tested pre-intervention in hospitals compared to private practices (63.6.% vs. 9.3%, p<0.01) (Table 6 ). A significantly higher number of inpatients were tested in hospitals than in private practices, with the most frequently used method of testing being PCR in hospitals and antigen testing in private practices.
Table 6.
Methods and distribution of pre-interventional testing of out- and inpatients comparing hospitals and private practices.
| Private Practice |
Hospital based |
p-value | |||||
|---|---|---|---|---|---|---|---|
| Number of facilities | % | Number of facilities | % | ||||
| Outpatients | 54 | 100.0 | 11 | 100.0 | <0.01 | ||
| No testing | 49 | 90.7 | 4 | 36.4 | |||
| Testing | 5 | 9.3 | 7 | 63.6 | <0.01 | ||
| PCR | 2 | 3.7 | 7 | 63.6 | <0.01 | ||
| Antigen test | 3 | 5.6 | 0 | 0.0 | <0.01 | ||
| Inpatients | 55 | 100 | 11 | 100.0 | |||
| No testing | 20 | 36.4 | 0 | 0.0 | <0.05 | ||
| Testing | 35 | 63.6 | 11 | 100.0 | <0.01 | ||
| PCR | 15 | 27.3 | 11 | 100.0 | <0.01 | ||
| Antigen test | 20 | 36.4 | 0 | 0.0 | <0.01 | ||
3.7. Personal protective equipment
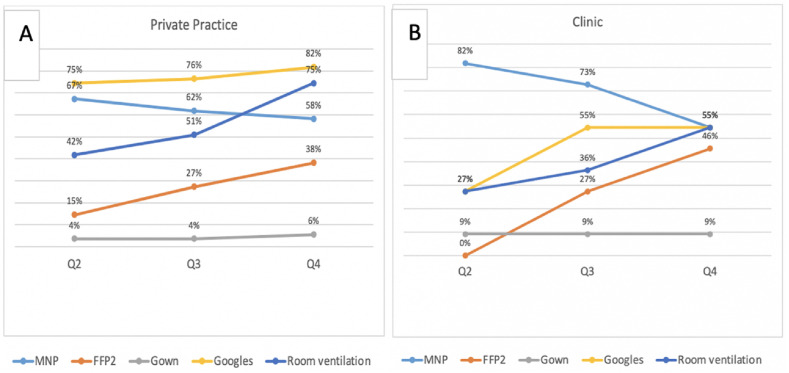
Considering quarterly data, a significant increasing tendency in PPE use can be seen in the use of FFP2/3 masks in private practices and hospitals (Figure 1 ). An opposite trend is shown in the use of conventional surgical masks with a decrease in private practices and even more prominently in hospitals.
Fig. 1.
Personal protective equipment (PPE). Use over the second to fourth quarter (Q2- Q4) with comparison between private practice (A) and clinics (B).
A significant increase in room ventilation can be observed in private practices and marginally not significant in hospitals. Except for FFP2/3-use and protective gowns, the percentage of PPE such as conventional surgical masks and safety goggles, as well as room ventilation, were higher in private practice than in hospitals.
3.8. Procedures, revenue, and employee development
Looking at the numbers of procedures performed during the coronavirus pandemic, significantly more hospitals than private practices have experienced a decrease of less than 50% (90.9% vs. 40%, p<0.01), with the majority of private practices seeing no change regarding the number of procedures at all (Table 7 ). On the contrary, a significantly smaller share of hospitals reported a stable level of procedures during the COVID-19-pandemic.
Table 7.
Comparison of procedures between private practices and hospitals.
| Private Practice |
Hospital based |
p-value | ||||
|---|---|---|---|---|---|---|
| Number of facilities | % | Number of facilities | % | |||
| Procedures | 55 | 100.0 | 11 | 100.0 | 0.074 | |
| Increase less than 50% | 2 | 3.6 | 0 | 0.0 | 0.549 | |
| Increase more than 50% | 1 | 1.8 | 0 | 0.0 | 0.617 | |
| Stable | 29 | 52.7 | 1 | 9.1 | <0.01 | |
| Decrease less than 50% | 22 | 40.0 | 10 | 90.9 | <0.01 | |
| Decrease more than 50% | 1 | 1.8 | 0 | 0.0 | 0.617 | |
| Revenue | 55 | 100.0 | 11 | 100.0 | <0.05 | |
| Increase less than 50% | 6 | 10.9 | 0 | 0.0 | 0.271 | |
| Stable | 25 | 45.5 | 1 | 9.1 | <0.05 | |
| Decrease less than 50% | 23 | 41.8 | 10 | 90.9 | <0.01 | |
| Decrease more than 50% | 1 | 1.8 | 0 | 0.0 | 0.617 | |
| Employees | 55 | 100.0 | 11 | 100.0 | 0.367 | |
| Increase | 7 | 12.7 | 1 | 9.1 | 0.764 | |
| Stable | 38 | 69.1 | 10 | 90.9 | 0.134 | |
| Decrease | 10 | 18.2 | 0 | 0.0 | 0.134 | |
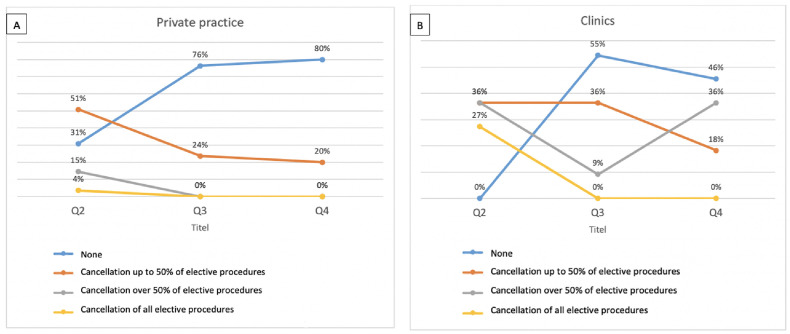
Comparing the quarterly numbers of cancelled elective procedures, a varying situation can be seen between private practices and hospitals (Fig. 2 ). Some private practices initially had to cancel over 50% of their elective procedures but soon returned to a relatively normal routine in Q4, whereas hospitals had a reduced elective surgical program for a longer period of time.
Fig. 2.
Cancellation of procedures over the course of the pandemic for private practices (A) and clinics (B).
The development of revenue showed a significant decrease of less than 50% in the majority of hospitals, whereas only about half of private practices reported the same (90.9% vs. 41.8%, p<0.01) (Table 7). Significantly more private practices experienced no change at all in economic revenue compared to hospitals (45.5% vs. 9.1%, p<0.05). In all, 10.9% of private practices even reported enhancement of their economic revenue during the pandemic.
Regarding employee number fluctuation, hospitals have been shown to be stable employers during this pandemic, with constant employee numbers. No decrease in staff size was reported by any hospital questioned (Table 7). In private practices, the greatest share reportedly maintained a stable number of employees as well.
4. Discussion
This nationwide study shows data on SARS-CoV-2 infection of HCW and its origin, use of preventive measures such as pre-interventional testing of patients, HCW screening, and use of PPE, as well as economic development over three quarters (Q2 to Q4) of the COVID-19 pandemic in hospital-based departments and private practices for OMS in Germany. This scientific work presents survey data of 55 private practices with 744 employees and 11 hospitals with 416 employees for OMS in Germany.
Our study aimed at a closer inspection of specialties with higher exposure to aerosols and droplets, as they are presumed to be a risk factors for infection transmission. AGP can be found especially in the fields of gastroenterology, otolaryngology, dentistry and oral and maxillofacial surgery. With evidence suggesting that a substantial viral load can be found in the oropharyngeal cavities, the spread of particles during medical procedures may expose oral and maxillofacial surgeons to a higher risk of infection (Kerawala and Riva, 2020). Looking at the data collected, a total of 3.5% HCW were reported to have had SARS-CoV-2 infection, which is comparable with infection rates found for AGP-related specialties excluding gastrointestinal endoscopy. Furthermore, private practices questioned reported having a significantly higher rate of HCW infection, with 4.7% of cases, compared with clinics, for which the reported percentage of HCW infection was only 1.4%. The paper focusing on four AGP-related specialties has shown an opposite trend, with clinics having a significantly higher rate of SARS-CoV-2 infection than private practices.
Because of their professional activity, HCW are at a double risk of infection, which can be acquired at the workplace and in the private environment. Looking at the data collected, private practices (17.6%) had a higher percentage regarding infection during interventions than hospitals (0.0%), with more hospitals (16.7%) reporting the workplace overall as a source of transmission compared with private practices (0.0%). The highest percentage (88.2% for private practices, 66.7% for hospitals) saw a correlation between COVID-19 infection and private life. Studies discussing the possibility of heightened risk during aerosol-generating procedures compared to transmission via human exhalation have been conducted, with no clear result thus far (Tang, 2021; Gallagher et al., 2020).
Indeed, HCW themselves can represent a potential risk of infection for their colleagues. Although only a minority of study participants named the workplace as a source of infection in private practices and hospitals, no clear conclusion can be drawn in this study as to whether infected HCW are responsible for transmission of the virus within collective. Some studies show that infected HCW were a risk factor for nosocomial outbreaks, having broken protective protocols by insufficient use of face masks and social distancing (Schneider et al., 2020). HCW screening is a measure aiming at preventing an infection outbreak within a medical facility. In particular, to ensure the safety of staff and patients, 63.6% of hospitals and 54.4% of private practices carried out employee screenings. The most frequently used form of testing in private practices was antigen testing (70.0%), whereas PCR was the chosen method in 57.1% and antigen testing in 28.6% of hospitals. Considering the poor performance of antigen testing in terms of its sensitivity, its massive use in private practices is to be critically questioned, as the reverse transcription−polymerase chain reaction (RT-PCR) remains the most precise form of testing currently available (Kahn et al., 2021).
Another measure preventing transmission of SARS-CoV-2 infection in health care institutions is pre-interventional testing of patients. In this regard, our study showed a low testing rate for outpatients in private practices (9.0%), whereas inpatients were tested substantially more frequently (63.6%). In hospitals, pre-interventional testing was conducted for 63.6% of outpatients, whereas 100.0% of hospitals reported having tested all inpatients. Moreover, clinics were testing their patients preferably using PCR, whereas private practices were testing their patients mainly with antigen testing. Therefore, the higher infection rate among HCW in private practices might be related to insufficient pre-interventional testing, especially of outpatients, as well as frequent use of antigen tests instead of PCR. A strict separation of inpatients and outpatients is advised, especially with untested patients involved, to reduce the risk of cross-infection (Zimmermann and Nkenke, 2020). As seen in nosocomial outbreaks especially in the beginning of the pandemic, the spread of the disease must be thoroughly examined, and safety protocols initiated (Höring et al., 2020).
To prevent a high number HCW becoming COVID-19 positive, the implementation of personal protective protocols was essential. Although universal rules of social distancing (1,5 m) could be followed only to an extent in the context of close patient care, the wearing of masks, room ventilation, and sanitation protocols had to be strictly ensured (Altermann et al., 2021; Jeffrey et al., 2020; Chu et al., 2020).
Concerning medical specialties with AGP, the use of PPE such as MNP, FFP2-masks, protective goggles and gowns was surveyed in this study. Except for MNP, all PPE showed a steady rise in use in private practices as well as hospitals. Studies show FFP2-masks to be an important protective measure for persons working in medical fields with aerosol-generating procedures (Lepelletier et al., 2020). Regarding the airborne pathway of COVID-19 infection, frequent room ventilation was shown to be incorporated in clinical settings. To further enhance this strategy, studies suggest particle filtration and air disinfection, as well as circulation systems (Morawska et al., 2020; Bhagat et al., 2020). Furthermore, measures for patients such as triage or special COVID paths were introduced into everyday clinical work (Giovanditto et al., 2022). To ensure the continuation of patient care while limiting the chances of the disease spreading, programs were developed using telemedicine and video consultation (Robiony et al., 2021)
Insights regarding the economic development of medical facilities in Germany during the COVID-19 pandemic are sparse so far. Our study presents data regarding economic revenue, cancellation of interventions, and employee development. The shift in staff and resources to support the challenges of overflowing intensive care units and COVID-19 hospital wards may explain the higher cancellation rates for elective interventions in hospitals compared with private practices. With 90.9% of hospitals reporting a decline in procedures, an association with these circumstances could be assumed. Following this trend, a decrease in revenue is also described in 90.9% of hospitals. Another factor seemed to be the hesitation of patients to enter medical care during the peak of the pandemic, which can be noticed in private practices as well (Jeffrey et al., 2020). About 40% reported about a decline in procedures and a decrease in revenue, a noticeably smaller number than in hospitals. Compensations for clinicians and private practitioners were being discussed with the Bundesministerium für Gesundheit (BMG) issuing a statement on March 27, 2020, to alleviate the COVID-19−related economic impact for German health care institutions (Waitzberg et al., 2020; Bundesministerium für Gesundheit, 2021).
With these financial difficulties and decrease in procedures, another issue arising could be the quality of the training of OMS interns, which was evaluated in a study from 2022 (Pabst et al., 2022); this study did show an impact of the clinical work because of the COVID-19 pandemic but found the training situation still to be positive overall.
It must be mentioned that the present cross-sectional study has some limitations, such as that selection bias cannot be ruled out due to the nature of recruitment via e-mail through the DGMKG. No definitive statement can be made regarding the authenticity of the information transferred back by practice owners or heads of departments.
5. Conclusion
Future COVID-related measures must adjust the infrastructure especially for hospitals to prevent further straining of staff and finances.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and the Good Clinical Practice (GCP) guidelines. A positive ethical evaluation was obtained from the Ethics Committee of the Faculty of Medicine of the Technical University of Munich under the accession number 713/20 S-SR.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgements
This study received public funds by B-FAST of the Network of University Medicine (NUM)
(award/grant number: 01KCX2021) and Bavarian State Ministry for Science and Arts (award/grant number: 152820012).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcms.2022.10.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ackermann M., Verleden S., Kuehnel M., et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman M., Nassar M., Rushinek H., et al. The efficacy of protective protocol for oral and maxillofacial surgery procedures in a COVID-19 pandemic area─results from 147 patients. Clin. Oral Invest. 2021:1–8. doi: 10.1007/s00784-021-03809-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhagat R., Wykes M.S., Dalziel S., Linden P.F. Effect on ventilation on the indoor spread of COVID-19. J. Fluid Mech. 2020;903:F1. doi: 10.1017/jfm.2020.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bielicki J., Duval X., Gobat N., et al. Monitoring approaches for health-care workers during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20:e261–e267. doi: 10.1016/S1473-3099(20)30458-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundesinstitut für Arzneimittel und Medizinprodukte, Germany. Accessed May 12, 2021.https://www.bfarm.de/SharedDocs/Risikoinformationen/Medizinprodukte/DE/schutzmasken.html.
- Bundesministerium für Gesundheit. Accessed May 13, 2021.https://www.bundesgesundheitsministerium.de/presse/pressemitteilungen/2020/1-quartal/corona-gesetzespaket-im-bundesrat.html.
- Chu D., Akl E., Duda S., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdem H., Lucey D.R. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239–241. doi: 10.1016/j.ijid.2020.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher J., Sukriti K.C., Johnson I.G., et al. A systematic review of contamination (aerosol splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open. 2020;6:25. doi: 10.1038/s41405-020-00053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovanditto F., Soma D., Vaira L.A., et al. Recommendations for a safe restart of elective aerosol-generating oral surgery procedures following the COVID-19 pandemic outbreak: an Italian multicenter study. J. Cranio-Maxillo-Fac. Surg. 2022;50:462–467. doi: 10.1016/j.jcms.2022.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höring S., Fussen R., Neusser J., et al. Managment of a hospital-wide COVID-19 outbreak affecting patients and healthcare workers. SN Comp Clin Med. 2020;2:2540–2545. doi: 10.1007/s42399-020-00597-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffrey M., D'Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern. Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint WHO-China Study . 2021. WHO-Convened Global Study of Origins of SARS-CoV-2: China Part. Joint Report. 14 January – 10 February. [Google Scholar]
- Kahn M., et al. Performance of antigen testing for diagnosis of COVID-19: a direct comparison of a lateral flow device to nucleic acid amplification based tests. BMC Infect. Dis. 2021;21(1):798. doi: 10.1186/s12879-021-06524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerawala C., Riva F. Aerosol generating procedures in head and neck surgery─can we improve practice fter COVID-19? Br. J. Oral Maxillofac. Surg. 2020;58:704–707. doi: 10.1016/j.bjoms.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepelletier D., Grandbastien B., Romano-Bertrand S., et al. What face mask for what use in the context of the COVID-19 pandemic? The French guideline. J. Hosp. Infect. 2020;105:414–418. doi: 10.1016/j.jhin.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Tang J., Bahnfleth W., et al. How can airborne transmission of COVID-19 indoors be minimized? Environ. Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nejatidanesh F., Khosravi Z., Goroohi H., Badrian H., Savabi O. Risk of contamination of different areas of dentist's face during dental practice. Int. J. Prev. Med. 2013;4:611–615. [PMC free article] [PubMed] [Google Scholar]
- Pabst A., et al. An update on the current training situation of German interns in oral and maxillofacial surgery at special times in 2021. J Craniomaxillofac Surg. 2022;April(50(4)):380–387. doi: 10.1016/j.jcms.2022.02.005. [DOI] [PubMed] [Google Scholar]
- Robert-Koch-Institut, Germany https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Hygiene.html
- Robert-Koch-Institut, Germany. Accessed May 11, 2021..https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Virologische_Basisdaten.html.
- Robiony M., Bocin E., Sembronio S., et al. Working in the era of COVID-19: an organization model for maxillofacial surgery based on telemedicine and video consultation. J. Cranio-Maxillo-Fac. Surg. 2021;49:323–328. doi: 10.1016/j.jcms.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S., Piening B., Nouri-Pasovksy P., et al. SARS-Coronavirus-2 cases in healthcare workers may not regularly originate from patient care: lessons from a university hospital on the underestimated risk of healthcare worker to healthcare worker transmission. Antimicrob. Resist. Infect. Control. 2020;9:192. doi: 10.1186/s13756-020-00848-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stöß C., Steffani M., Kohlhaw K., et al. The COVID-19 pandemic: impact on surgical departments of non-university hospitals. BMC Surg. 2020;20:313. doi: 10.1186/s12893-020-00970-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J. SARS-CoV-2 and aerosols─arguing over the evidence. J. Virol. Methods. 2021;289 doi: 10.1016/j.jviromet.2020.114033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waitzberg R., Aissat D., Habicht T., et al. Compensating healthcare professionals for income losses and extra expenses during COVID-19. Eurohealth. 2020;26:2. [Google Scholar]
- World Health Organization https://covid19.who.int
- Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J. Cranio-Maxillo-Fac. Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.