Abstract
Problems in mental health and socioeconomic health inequalities during childhood and adolescence are receiving important scientific and political attention. This in mind, we study how current family income and parental education are associated with psychiatric disorders among children in a well-developed welfare state, Finland. To gain a deeper understanding of how these disparities develop through early life course, we study the differences between genders, age groups, types of mental disorders, and also take into account the role of parental mental disorders. We exploit high-quality Finnish register data containing the whole population aged 4–17 with information on their families and parents. Our results of linear probability models show that lower parental education is consistently associated with higher probability of mental disorders throughout childhood, although some gender and disorder-specific differences are also identified. Interestingly, household income is related to mental health in more complex ways, having both negative and positive associations with psychiatric disorders. Inequalities are stronger among boys than girls, and the strongest associations are found among boys aged 7–12 and girls aged 13–17. Parental mental disorders increase the risk of children's psychiatric disorders but do not explain socioeconomic disparities. Considering the negative effects of mental problems on socioeconomic outcomes, inequalities in childhood mental health can be expected to reinforce other social inequalities in later life and should therefore be a focus of interventions.
Keywords: Adolescence, Childhood, Finland, Inequality, Mental disorders, Socioeconomic background, Psychiatric diagnosis, Register data
Highlights
-
•
Inequalities in psychiatric disorders throughout childhood were examined using unique register data from Finland.
-
•
Inequalities according to parental education were stronger and more consistent than according to family income.
-
•
Parents' psychiatric disorders did not explain socioeconomic disparities.
1. Introduction
Problems in mental health and socioeconomic health disparities during childhood and adolescence have received a lot of attention, especially since the Covid-19 pandemic. As health problems in childhood can have long-lasting effects, the trend of rising mental health issues warrants a serious consideration. Evidence on mental health disparities is needed to design effective policies and to understand how social inequalities are created.
There is plenty of evidence on socioeconomic inequalities in health using various indicators for both health and socioeconomic status (Kivimäki et al., 2020). Importantly, these disparities have been found also among children and adolescents (Case, Lubotsky, & Paxson, 2002; Kruk, 2013), as well as for mental health among children (Hakulinen, Mok, et al., 2020; Paananen, Ristikari, Merikukka, & Gissler, 2013). Less is known about the mechanisms explaining the early start for inequalities and how they develop throughout childhood. For example, parental health can directly affect the socioeconomic status of the family and health of the child.
In this article, we examine mental health disparities in childhood across socioeconomic classes exploiting high-quality Finnish register data that provides us rich information on the entire population. Our main research question is what socioeconomic inequalities exist in the prevalence of mental disorders among children aged 4–17 in Finland. Second, we investigate whether the same pattern of inequality is found when looking at parental education and income as the measure of socioeconomic status. Third, we describe differences in the level of inequality between boys and girls, age groups, and psychiatric disorder groups. Fourth, we further contribute to the existing literature on mental health inequalities by examining whether parental mental disorders explain inequality among children. Fifth, we further examine whether the association between parental mental health and child's mental health is moderated by socioeconomic status of the parent.
Mental health problems in childhood and youth have many negative social and economic consequences. They have been shown to have an association with noncompletion and choice of study track in Finnish upper secondary education (Mikkonen, Remes, Moustgaard, & Martikainen, 2020, 2021) and with the likelihood and duration of receipt of social assistance in young adulthood (Haula & Vaalavuo, 2021; Vaalavuo & Bakkum, 2021). Autism spectrum and psychotic disorders during adolescence have a strong association with not being in education, employment or training (NEET) in early adulthood (Ringbom et al., 2021). A Swedish study found that children with conduct problems had an increased risk of developing both mental disorders and other problems such as criminal behaviour and substance and alcohol misuse in emerging adulthood (Lichtenstein et al., 2020). In addition, mental disorders of Swedish male adolescents were associated with poorer labour market outcomes such as lower earnings, higher unemployment, and higher welfare benefit receipt (Lundborg, Nilsson, & Rooth, 2014). Psychological problems in childhood were associated also with reduced family income and lower educational attainments in adulthood in the US (Smith & Smith, 2010). Consequently, socioeconomic inequalities in mental health in early life course may perpetuate other social inequalities in life. Therefore, tackling mental health inequalities should be among the priorities of public health as well as social policy.
2. Background & literature review
2.1. Theoretical framework
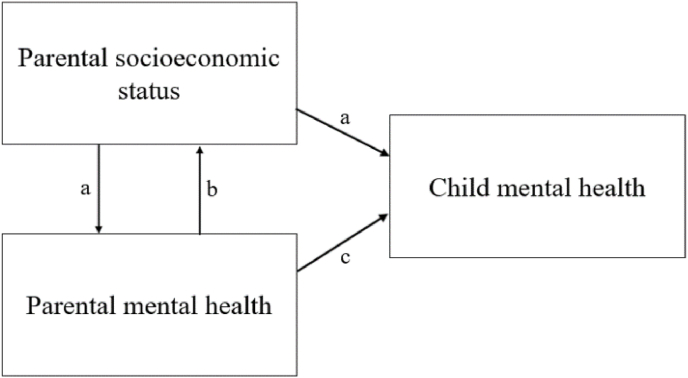
Socioeconomic health inequalities have been studied widely with consistent results (Kröger, Pakpahan, & Hoffmann, 2015). There are two main hypotheses, that offer possible explanations for the social gradient in health: social causation and social selection hypotheses. Social causation theory argues that people with lower socioeconomic status have worse life circumstances, such as less resources, poorer health behaviour and higher levels of stress, which contribute to poorer health (a in Fig. 1). Social selection thesis, on the other hand, claims that people with poorer health have worse possibilities and abilities to achieve higher socioeconomic status and to invest in their education and career (b in Fig. 1). (E.g., Hoffmann, Kröger, & Pakpahan, 2018; Kröger et al., 2015; Reiss, 2013.)
Fig. 1.
Associations between parental and child mental health and socioeconomic status.
However, these hypotheses are not exclusive. A systematic review of evidence found that both theories are quite equally supported by research (Kröger et al., 2015). However, the choice of SES indicators influenced the results and the support for the alternative theories. Another possible explanation for the association is indirect selection, where both SES and (mental) health are assumed to be caused by common background factors, for example genetic, cognitive and physical characteristics, or risk taking behaviour (Hoffmann et al., 2018).
The relevant mechanisms at play might be different when we look at health inequalities in childhood. In addition, it might be impossible to disentangle the different mechanisms. For example, through social selection, parental health affects the socioeconomic status of the family that, consequently, through social causation, affects childhood health, or the other way around. Furthermore, it should not be excluded that a child's health affects parental well-being as has been demonstrated by Vaalavuo, Salokangas, and Tahvonen (2022) regarding the impact of child cancer on parental labour market outcomes (mechanism not shown in Fig. 1). Arrow c in Fig. 1 also illustrates the socio-genetic mechanisms from parental mental health to a child's mental health: psychiatric problems among parents can be risk factors for offspring mental health both genetically as well as through social and familial mechanisms (Mortensen, Pedersen, Melbye, Mors, & Ewald, 2003; Tienari et al., 2004).
Age is an important factor in understanding health inequalities, because the relationship of socioeconomic status and health varies by age (Dupre, 2007). For example, the health differences of educational and occupational groups widened by age in a Swedish study (Leopold, 2016). However, a study from the US found that association of lower SES and poorer health did not change with age throughout childhood (Chen, Martin, & Matthews, 2006). Another US-based study found that financial problems in childhood family had a stronger association with mental disorder onsets in ages 4–12 than onsets in adolescence and early adulthood, although the association was found in all ages (McLaughlin et al., 2011).
2.2. Mental disorders in childhood
Many mental disorders typically first appear in childhood and adolescence. Age of onset is the earliest in autism spectrum and impulse-control disorders. Some of the anxiety disorders also appear early. Mood disorders and substance use disorders often first occur in adolescence, but the median age of onsets has larger ranges (Kessler et al., 2007.). According to Kessler, Berglund, Demler, Jin, and Walters (2005), the majority of psychiatric disorders start by the age of 24. Prevalence for childhood mental disorder was 12.7 percent in a systematic review of studies from high-income countries (Barican et al., 2022). Most common disorders were anxiety and ADHD.
In Finland, the use of health services for mental disorders has increased among adolescents in recent years. The largest absolute increases were found for depression, anxiety, and ADHD, while the pattern in disorders between genders varied (Gyllenberg et al., 2018.). Also the age-specific prevalence of diagnoses for autism spectrum disorder, childhood autism, hyperkinetic disorder, obsessive compulsive disorder and Tourette syndrome has risen in Finland, Sweden and Denmark between years 1990 and 2007 (Atladottir et al., 2015).
Parental mental disorders are risk factors for child's mental disorders (Dean et al., 2010). They might also mediate or moderate the association between parental SES and offspring mental health. More research is needed on the topic as the associations are complex. For example, schizophrenia has an association with both low parental SES and psychiatric disorders in the family (Agerbo et al., 2015). Another study found that Finnish children aged 0–12 years, whose mothers had psychiatric disorders and substance abuse problems, had a higher risk of developing emotional, behavioural, and psychological development mental health disorders than other children. The risks were higher for boys than for girls and for children, whose mothers were socioeconomically disadvantaged (Ranta & Raitasalo, 2015.).
2.3. Mental disorders and childhood living conditions
According to a systematic literature review (Reiss, 2013), children and adolescents aged 4–18 from low SES families are two to three times more likely to have mental health issues than their peers with high SES. Out of SES indicators, low levels of household income and parental education had the best predictive power. There were no big gender differences between SES and mental health, and the association was found in all ages. Moreover, Torikka et al. (2014) found that the prevalence of self-reported depression has risen in Finland especially among adolescents who have unemployed and lower educated parents. Consequently, disparities between socioeconomic groups have widened.
Several studies have shown that poor family income is associated with higher amount of all mental disorders among children (e.g., Bøe, Øverland, Lundervold, & Hysing, 2012; Najman et al., 2010). A Norwegian register-based study of 5–17-year-old children by Kinge et al. (2021) found that the prevalence of mental disorder differed by parental income as poorer children had notably more mental disorders than children from high-earning families. Similarly, family poverty in childhood and adolescence had an association with higher levels of anxiety and depression in adolescence and young adulthood in an Australian study. Recurring exposures to poverty over early life course led to stronger associations (Najman et al., 2010.). The consequences of childhood conditions can also be long-lasting. For example, a Danish study found that lower level of family income in childhood was associated with a higher risk of developing mental disorders and getting a diagnosis during ages 15–37 (Hakulinen, Mok, et al., 2020). Also, parental separation or divorce is associated with a higher risk of child's mental health problems, but socioeconomic factors explain part of the effect (Lucas, Nicholson, & Erbas, 2013; Strohschein, 2005).
In addition, children from low SES families have been found to be more likely to have more than one disorder at the same time (comorbidity) than their peers with a high SES. As for specific disorders, a stronger association with low SES and externalizing disorders has been identified in many studies compared with internalizing disorders, although not all results are consistent (Reiss, 2013.). On the other hand, Sariaslan et al. (2021) found no causal effects between changing family income during childhood and adolescence and severe mental health diagnoses among young adults in Finland, when sibling-comparison models were employed. This study however received critic for its use of a sibling design as a tool to study causality of family income (Rod, Lange, & Petersen, 2021). While causal studies on the topic are difficult to conduct, Costello, Compton, Keeler, and Angold (2003) were able to examine the effects of a policy intervention in the US. They studied poverty and mental health and found support for the social causation theory. After a poverty intervention, American Indian children, whose families left poverty, had fewer (behavioural) mental health symptoms.
3. Data and methods
3.1. Data and analysis sample
We use individual-level register data of the total population in Finland. Our data on psychiatric health information is obtained from the Care Register for Health Care (Hilmo), which is provided by the Finnish Institute of Health and Welfare. It contains information on the use of public specialized health care services and ICD-10 codes (International Classification for Diseases) for diagnoses. We also exploit Statistics Finland's register data that allow linking family members and include various socioeconomic information on annual level. The data is anonymized, and it is analysed in a remote system provided by Statistics Finland.
Our analysis sample consists of children aged 4–17 years in 2018. Children below 4 years old were omitted due to low incidence of mental disorders in the public record. Children and biological and adoptive parents were linked to each other with individual identification numbers. We also utilise household level data, which is used for information about children's living environment, for example, household income, whether they live with their parents, and the number of siblings. Parental mental disorder information was included from years 2014–2018, all other information refers to year 2018.
In year 2018 there were 849,233 children aged 4–17 years living in Finland. However, we excluded from the analysis sample children for whom one or both parent identification numbers were missing (n = 21,245) and children who were not living in the same household with neither of their biological or adoptive parents (n = 13,818). For the former group no parental information could be found and the latter consist of special groups of children living for example in foster homes, custody and adolescents living on their own. After these exclusions our analysis sample consist of 815,616 children.
3.2. Dependent variable
Our dependent variable is a binary variable indicating a mental disorder based on ICD-10 F-class diagnosis in public special health care. If a child had a treatment contact in specialized health care with any mental disorder diagnosis during 2018, the variable has a value of 1, otherwise it has a value of 0. All F-class disorders were included except for organic, including symptomatic, mental disorders (F00–F09), intellectual disability (F70–F79) and developmental disorder of speech, language, learning and motor coordination (F80–F83). These conditions are often congenital or caused by a serious medical illness during childhood, and are mostly diagnosed and treated in pediatric, neurological and disability services, not in psychiatric services. The frequencies of different diagnosis groups are presented in Table 1.
Table 1.
12-month prevalence of psychiatric disorder groups by gender and age group (2018).
| All | Gender |
Age |
N | ||||
|---|---|---|---|---|---|---|---|
| Boy | Girl | 4–6 | 7–12 | 13–17 | |||
| No mental disorder | 95.3% | 95.9% | 95.7% | 98.3% | 95.6% | 93.0% | 777,212 |
| Alcohol and other substance use disorders (F10–F19) | 0.1% | 0.1% | 0.1% | 0.0% | 0.01% | 0.3% | 802 |
| Schizophrenia spectrum disorders (F20–F29) | 0.04% | 0.03% | 0.04% | 0.0% | 0.01% | 0.1% | 301 |
| Bipolar disorders (F30, F31, F34.0) | 0.02% | 0.01% | 0.02% | 0.0% | 0.0% | 0.04% | 138 |
| Depressive disorders (F32, F33, F34.1) | 0.7% | 0.4% | 1.02% | 0.0% | 0.2% | 1.8% | 5509 |
| Anxiety disorders (F40, F41, F42) | 0.6% | 0.3% | 0.87% | 0.02% | 0.2% | 1.5% | 4820 |
| Trauma- and stress-related disorders (F43) | 0.2% | 0.1% | 0.21% | 0.03% | 0.1% | 0.3% | 1435 |
| Eating disorders (F50) | 0.2% | 0.03% | 0.27% | 0.0% | 0.03% | 0.4% | 1193 |
| Autism spectrum disorders and other disorders of psychological development (F85, F88, F89) | 0.5% | 0.8% | 0.25% | 0.4% | 0.6% | 0.5% | 4438 |
| ADHD/Hyperkinetic disorders (F90) | 1.0% | 1.6% | 0.39% | 0.3% | 1.4% | 0.9% | 8065 |
| Conduct disorders (F91, F92) | 0.3% | 0.5% | 0.18% | 0.1% | 0.4% | 0.4% | 2765 |
| Emotional disorder with onset specific to childhood (F93) | 0.5% | 0.5% | 0.48% | 0.1% | 0.6% | 0.6% | 3788 |
| Other childhood onset disorders (F94–F98) | 0.6% | 0.7% | 0.44% | 0.5% | 0.8% | 0.4% | 4699 |
| Total number of observations | 100.0% | 417,786 | 397,830 | 175,041 | 361,031 | 279,544 | 815,616 |
In addition, if a child had a treatment contact in the specialized field of psychiatry, child psychiatry or youth psychiatry without any ICD-10 diagnosis or had a Z-class diagnosis, the child is categorised as having a mental disorder. Z-class refers to factors that have an impact on the state of health or contacts to service providers. These visits often indicate that the patient had an evaluation period for psychiatric symptoms, for which a diagnosis is not yet given. We also use similar variables for different psychiatric diagnostic groups.
3.3. Independent and control variables
Our main explanatory variables are indicators of socioeconomic status of the child's family: income and parental education. We use household income to describe childhood living environment. Household income is defined as household's disposable income in year 2018, more specifically income after taxes and income transfers, divided by the OECD consumption unit. Incomes are presented as quintiles that are formed based on the analysis sample. 1.7 percent had a missing value for household income.
Parental education refers to the highest completed degree, separately for mothers and fathers, and it is split to three categories: lower secondary or less, upper secondary education, and tertiary education. In the models we use maternal educational level but also include a robustness check for paternal education.
We control for child's age, as a categorical variable (4–6, 7–12 and 13–17 years), and gender. Information on child's family structure, i.e., whether the child lives with both parents, only mother or only father, is also used. This variable indicates parental separation status, which is two-sided. On one hand, parental separation creates family instability, which might account for mental disorders, and on the other hand, parental separation often leads to lower income level. In addition, we controlled for maternal age at birth, urbanization of municipality of child's residence, immigration background, where child was classified as having an immigrant background when both parents were born outside Finland, and the number of siblings. Parental mental disorder is controlled for both mother and father and coded as a binary variable like our main dependent variable. It contains all F-class disorders, but neither empty nor Z-class main diagnosis visits in psychiatric units of specialized health care.
Independent and control variables and their prevalence in the analysis sample are presented in Table 2.
Table 2.
Descriptive statistics: 12-month distribution and prevalence of children with a mental disorder (2018).
| Distribution of background characteristic among all children | Distribution of background characteristic among children with a mental disorder | Prevalence of mental disorders | |
|---|---|---|---|
| Observations | n = 815,616/100% | n = 38,404/100% | 4.7% |
| Gender | |||
| Male | 51.2% | 55.3% | 5.1% |
| Female | 48.8% | 44.7% | 4.3% |
| Age group | |||
| 4–6 | 21.5% | 7.8% | 1.7% |
| 7–12 | 44.3% | 41.5% | 4.4% |
| 13–17 | 34.3% | 50.7% | 7.0% |
| Family structure: lives with | |||
| Both parents | 71.6% | 50.0% | 3.3% |
| Mother | 24.1% | 42.1% | 8.2% |
| Father | 4.3% | 7.9% | 8.6% |
| Urbanization of municipality | |||
| Urban | 69.5% | 71.8% | 4.9% |
| Semi-urban | 17.1% | 15.9% | 4.4% |
| Rural | 13.3% | 12.4% | 4.4% |
| Immigration background | |||
| At least one parent born in Finland | 93.1% | 95.5% | 4.8% |
| Both parents born outside Finland | 6.9% | 4.5% | 3.1% |
| Number of siblings | |||
| Only child | 23.9% | 34.2% | 6.7% |
| One | 43.8% | 40.7% | 4.4% |
| Two | 20.6% | 16.6% | 3.8% |
| Three or more | 11.8% | 8.5% | 3.4% |
| Maternal age at birth | |||
| −20 | 3.3% | 5.8% | 8.3% |
| 21–39 | 92.3% | 89.6% | 4.6% |
| 40 or more | 4.4% | 4.6% | 4.9% |
| Parental mental health | |||
| Maternal | |||
| No diagnosis | 92.1% | 80.0% | 4.1% |
| Any diagnosis | 7.9% | 20.0% | 12.0% |
| Paternal | |||
| No diagnosis | 94.6% | 88.3% | 4.4% |
| Any diagnosis | 5.4% | 11.7% | 10.2% |
| Maternal education | |||
| Lower secondary or less | 9.4% | 12.5% | 6.3% |
| Upper secondary | 38.6% | 45.1% | 5.5% |
| Post-secondary or tertiary | 52.0% | 42.5% | 3.8% |
| Paternal education | |||
| Lower secondary or less | 15.7% | 21.8% | 6.5% |
| Upper secondary | 46.3% | 48.5% | 4.9% |
| Post-secondary or tertiary | 38.0% | 29.8% | 3.7% |
| Household income quintile | |||
| 1 The lowest | 20.0% | 22.8% | 5.4% |
| 2 | 20.0% | 24.2% | 5.7% |
| 3 | 20.0% | 20.3% | 4.7% |
| 4 | 20.0% | 17.6% | 4.2% |
| 5 The highest | 20.0% | 15.1% | 3.6% |
Mental disorder: child had a visit in specialized health care with an ICD-10 F-class main diagnosis (excluding groups F00–F09, F70–F79 & F80–F83) or had a visit with an empty or a Z-class main diagnosis in a specialized field of psychiatry in 2018.
3.4. Methods
We use linear probability models to estimate the association between child's mental disorder and parental socioeconomic status. Linear probability method allows comparing between different models and is easier to interpret than logistic regression models (Hellevik, 2009). The models are conducted separately for boys and girls due to important gender differences in the prevalence of psychiatric diagnoses.
The modelling procedure begins by testing separately the association between maternal education or income quintile and any psychiatric disorder of the child. The first model includes child's age group, maternal birth age and maternal education level as independent factors. In model 2, we add family structure, type of municipality, immigration background, and number of siblings as control variables. Then we enter both maternal and paternal psychiatric disorders in model 3. Same procedure is repeated, but instead of maternal education we test household income quintile as the main independent variable . Finally, we have both income quintile and education level in same model.
We also conduct the full model with maternal education, household income quintile and all control variables separately for age groups and genders. Thereafter, models are conducted for different diagnostic groups of psychiatric disorders using maternal education and control variables as independent factors.
4. Results
4.1. Descriptive statistics
Table 2 describes the study population by mental disorder. Based on our analysis sample, 4.7 percent (n = 38,404) of all children (n = 815,616) had a mental disorder or treatment contact in a psychiatric unit in specialized health care in 2018.
The patterns between mental disorders and background variables are in line with the previous research. Boys (prevalence of 5.1%) and older children (7.0% for ages 13–17) have an elevated risk for mental disorders compared to girls (4.3%) and younger children (1.7% for ages 4–6, 4.4% for ages 7–12). Parental mental disorders are strong risk factors (12.0% for maternal, 10.2% for paternal) for child mental disorder compared to children whose parents were not treated for mental disorders recently (4.1% for maternal, 4.4% for paternal). Children whose parents have the lowest level of education have almost twice as high a risk for mental disorders compared to children of higher educated parents. In the two poorest income quintiles the risks for mental disorder are also greater (5.4% for 1st quintile, 5.7% for 2nd quintile) than in the richest quintile (3.6%). For other control variables, the prevalence is greater among children who live with only one parent, are the only child and have young mothers.
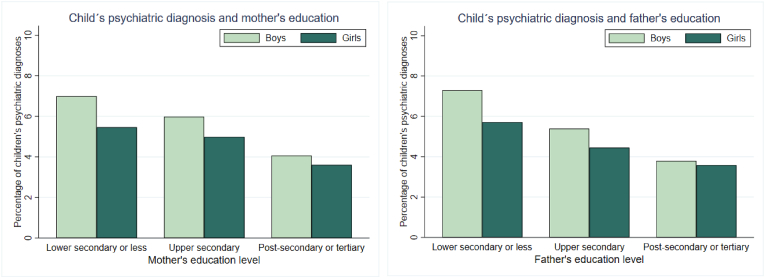
We move on to describe the prevalence of mental disorders by socioeconomic background. First, Fig. 2A and B illustrate the differences in prevalence between parental education levels. There is a clear gradient according to both maternal and paternal education for both girls and boys, although the gradient seems to be slightly steeper among boys.
Fig. 2.
A and B. 12-month prevalence of mental disorders and parental education by gender.
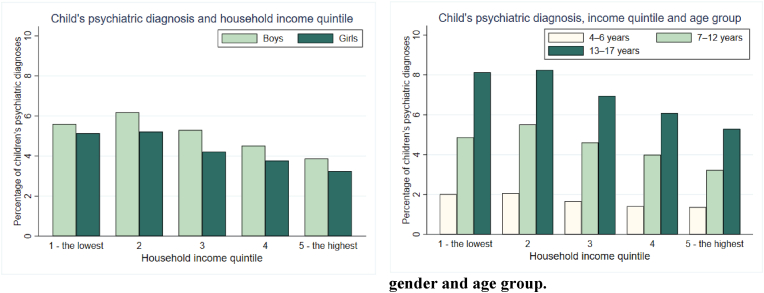
The prevalence of mental disorders is lower in the three richest income quintiles than in the two poorest ones (Fig. 3A). However, the bottom income quintile diverts from the linear pattern for boys. The gradient is found in all age groups, while it appears somewhat stronger in the oldest age group (Fig. 3B).
Fig. 3.
A and B. 12-month prevalence of mental disorders and household income quintile by gender and age group.
Fig. 4A, B & 4C visualize the prevalence of mental disorders among children and parents over socioeconomic classes. We see a strong correlation between parental mental disorders and family income and parental education. It is noteworthy that the correlation is much stronger for parents than for children.
Fig. 4.
AB & 4C. 12-month prevalence of mental disorders among children and parents over parental education and household income.
4.2. Results from regression models
We start by discussing the results regarding mental disorder gradient by mother's education and then move on to results showing income gradient. The results of linear probability models are shown for genders separately in Table 3, Table 4. Dependent variable is a dummy indicating whether the child has any mental disorder in specialized health care during 2018.
Table 3.
Results from linear probability model. Association between mother's education and child's mental disorder, by gender.
| Boys |
Model 2a | Model 3a | Girls |
Model 2b | Model 3b | |
|---|---|---|---|---|---|---|
| Model 1a | Model 1b | |||||
| Maternal education Ref. Lower secondary or less | ||||||
| Upper Secondary | −0.009*** | −0.012*** | −0.008*** | −0.003** | −0.007*** | −0.004** |
| (0.0013) | (0.0013) | (0.0013) | (0.0012) | (0.0013) | (0.0012) | |
| Post-secondary or tertiary | −0.027*** | −0.026*** | −0.020*** | −0.017*** | −0.016*** | −0.011*** |
| (0.0012) | (0.0013) | (0.0013) | (0.0012) | (0.0013) | (0.0013) | |
| Maternal mental health disorder Ref. no mental health disorder | ||||||
| 0.071*** | 0.059*** | |||||
| (0.0013) | (0.0012) | |||||
| Paternal mental health disorder Ref. no mental health disorder | ||||||
| 0.040*** | 0.031*** | |||||
| (0.0015) | (0.0014) | |||||
| Constant | 0.039*** | 0.041*** | 0.029*** | 0.021*** | 0.027*** | 0.017*** |
| (0.0013) | (0.0016) | (0.0016) | (0.0012) | (0.0015) | (0.0015) | |
| N | 415,961 | 415,961 | 415,961 | 396,247 | 396,247 | 396,247 |
Standard errors in parentheses.
**p < 0.01, ***p < 0.001.
Model 1: Maternal education level and adjusted for age group and maternal birth age.
Model 2: Model 1 + adjusted for family structure, number of siblings, type of municipality, immigrant background.
Model 3: Model 2 + parental mental health disorders.
Table 4.
Results from linear probability model. Association between family income and child's mental disorder, by gender.
| Boys |
Model 2a | Model 3a | Model 4a | Girls |
Model 2b | Model 3b | Model 4b | |
|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 1b | |||||||
| Income quintile Ref. 1. quintile – lowest | ||||||||
| 2. quintile | 0.006*** | 0.008*** | 0.010*** | 0.012*** | 0.0009 | 0.001 | 0.002* | 0.004*** |
| (0.0011) | (0.0011) | (0.0011) | (0.0011) | (0.0010) | (0.0010) | (0.0010) | (0.0010) | |
| 3. quintile | −0.002* | 0.006*** | 0.010*** | 0.013*** | −0.008*** | −0.004** | −0.0003 | 0.001 |
| (0.0011) | (0.0012) | (0.0012) | (0.0012) | (0.0010) | (0.0011) | (0.0011) | (0.001) | |
| 4. quintile | −0.010*** | 0.001 | 0.006*** | 0.011*** | −0.012*** | −0.006*** | −0.002 | 0.001 |
| (0.0011) | (0.0012) | (0.0012) | (0.0012) | (0.0010) | (0.0011) | (0.0011) | (0.0012) | |
| 5. quintile – highest | −0.017*** | −0.005*** | 0.002 | 0.009*** | −0.017*** | −0.014*** | −0.006*** | −0.002 |
| (0.0011) | (0.0012) | (0.0012) | (0.0013) | (0.0010) | (0.0012) | (0.0012) | (0.0012) | |
| Maternal mental health disorder Ref. no mental health disorder | ||||||||
| 0.072*** | 0.071*** | 0.060*** | 0.060*** | |||||
| (0.0013) | (0.0013) | (0.0012) | (0.0012) | |||||
| Paternal mental health disorder Ref. no mental health disorder | ||||||||
| 0.041*** | 0.040*** | 0.031*** | 0.031*** | |||||
| (0.0015) | (0.0015) | (0.0014) | (0.0014) | |||||
| Maternal education Ref. Lower secondary or less | ||||||||
| Upper Secondary | −0.011*** | −0.005*** | ||||||
| (0.0014) | (0.0013) | |||||||
| Post-secondary or tertiary | −0.023*** | −0.011*** | ||||||
| (0.0014) | (0.0013) | |||||||
| Constant | 0.025*** | 0.020*** | 0.009*** | 0.020*** | 0.018*** | 0.022*** | 0.012*** | 0.017*** |
| (0.0010) | (0.0014) | (0.0014) | (0.0018) | (0.0009) | (0.0013) | (0.0014) | (0.0017) | |
| N | 409,022 | 409,022 | 409,022 | 409,022 | 389,567 | 389,567 | 389,567 | 389,567 |
Standard errors in parentheses.
**p < 0.01, ***p < 0.001.
Model 4: Household income quintile and adjusted for age group and maternal birth age.
Model 5: Model 4 + adjusted for family structure, number of siblings, type of municipality, immigrant background.
Model 6: Model 5 + parental psychiatric disorders.
Model 7: Model 6 + maternal education.
Maternal education had a slightly stronger association with mental disorders among boys than girls (Table 3). Having a mother with a post-secondary or tertiary education decreased the probability of having a mental disorder for boys by 2.7 percentage points and for girls by 1.7 percentage points compared to children whose mothers had the lowest level of education (models 1a and 1b). This can be considered as a large effect size as the prevalence of mental disorders overall was 4.7 percent in the study population. After adjusting for control variables, coefficients remained similar (models 2a and 2b).
Children whose mothers had a recent mental disorder diagnosis had an increased probability for having a mental disorder (models 3a and 3b). An increased risk of 7.1 percentage points for boys and 5.9. percentage points is important and societally relevant. Coefficients for paternal mental disorder were in line with the pattern, but smaller. However, accounting for parental mental disorders in the models did not greatly affect the association between mother's education and child's mental disorder.
A robustness check, where the dependent variable was measured over a longer observation period, namely indicating a child's psychiatric disorder during 2014–2018 (Appendix A, Table A1), was also conducted. The results were similar, but stronger associations were found compared to the results in Table 3. Another robustness check with paternal education as the main independent variable (Appendix A, Table A2) demonstrated similar results as with maternal education. Paternal education was more strongly associated with mental disorders of boys before controlling than maternal education, but after controlling no real differences were observed.
Next, we compare the results when using household income quintile as the main independent variable (Table 4). For boys, belonging to the richest income quintile decreased the probability of having a psychiatric disorder by 1.7 percentage points and in the 4th quintile by 1.0 percentage point when compared to the poorest income quintile (model 1a). However, when models were adjusted for control variables, only the richest quintile was associated with a decreased probability of mental disorders, and other income quintiles were reversely associated with a mental disorder or coefficients were statistically unsignificant (model 2a) compared to the poorest quintile. As for girls, the results were similar (model 1b), but when control variables were included, the coefficients for the three highest income groups remained negative, while the associations weakened a bit (model 2b). Effect sizes were much smaller than for maternal education (Table 3).
For boys, the addition of parental mental disorders led to a stronger reversed association in middle quintiles. For girls, only in the richest income quintile the coefficient remained statistically significant (models 3a and 3b).
Interestingly, when maternal education was included, its coefficients remained negative and higher education was associated with a lower probability for a child's mental disorder even when controlling for other factors and seemed to be a stronger determinant than income especially among boys (models 4a and 4b). In other words, the association between higher family income and child's mental disorder disappeared for girls and turned reverse for boys, when other family background variables, parental mental disorders and maternal education were included in the models.
We further studied the association by age groups using the full model with both income and maternal education (Table 5). Higher income was associated with a slightly increased risk for mental disorder among boys in all ages and for girls aged 4–12 (models 1a–1e). Higher income was associated with a lower risk for mental disorder only for girls aged 13–17 in the two richest quintiles (model 1f). The effect sizes were around 1 percentage point for boys, but smaller for girls. These results were against our expectations.
Table 5.
Results from linear probability model. Association between mother's education, family income and child's mental disorder, by gender and age group.
| Boys |
Girls |
|||||
|---|---|---|---|---|---|---|
| 4–6 years |
7–12 years |
13–17 years |
4–6 years |
7–12 years |
13–17 years |
|
| Model 1a | Model 1b | Model 1c | Model 1d | Model 1e | Model 1f | |
| Income quintile Ref. 1. quintile - lowest | ||||||
| 2. quintile | 0.007*** | 0.015*** | 0.010*** | 0.001 | 0.005*** | 0.003 |
| (0.0016) | (0.0018) | (0.0020) | (0.0012) | (0.0013) | (0.0024) | |
| 3. quintile | 0.008*** | 0.017*** | 0.011*** | 0.002 | 0.005*** | −0.004 |
| (0.0017) | (0.0019) | (0.0021) | (0.0013) | (0.0013) | (0.0025) | |
| 4. quintile | 0.007*** | 0.017*** | 0.006** | 0.002 | 0.004** | −0.005* |
| (0.0018) | (0.0020) | (0.0022) | (0.0014) | (0.0014) | (0.0027) | |
| 5. quintile – highest | 0.010*** | 0.013*** | 0.003 | 0.001 | 0.003* | −0.011*** |
| (0.0019) | (0.0021) | (0.0022) | (0.0014) | (0.0015) | (0.0028) | |
| Maternal education Ref. Lower secondary or less | ||||||
| Upper Secondary | −0.009*** | −0.013*** | −0.010*** | −0.001 | −0.007*** | −0.007* |
| (0.0019) | (0.0022) | (0.0025) | (0.0014) | (0.0016) | (0.0031) | |
| Post-secondary or tertiary | −0.015*** | −0.030*** | −0.020*** | −0.004* | −0.012*** | −0.018*** |
| (0.0020) | (0.0023) | (0.0025) | (0.0015) | (0.0016) | (0.0031) | |
| Maternal mental health disorder Ref. no mental health disorder | ||||||
| Has disorder | 0.034*** | 0.084*** | 0.079*** | 0.024*** | 0.055*** | 0.093*** |
| (0.0019) | (0.0021) | (0.0023) | (0.0014) | (0.0015) | (0.0029) | |
| Paternal mental health disorder Ref. no mental health disorder | ||||||
| Has disorder | 0.022*** | 0.053*** | 0.037*** | 0.013*** | 0.025*** | 0.053*** |
| (0.0023) | (0.0025) | (0.0027) | (0.0017) | (0.0017) | (0.0034) | |
| Constant | 0.023*** | 0.063*** | 0.047*** | 0.010*** | 0.029*** | 0.093*** |
| (0.0025) | (0.0029) | (0.0030) | (0.0018) | (0.0020) | (0.0037) | |
| N | 87,599 | 180,686 | 140,737 | 83,489 | 172,845 | 133,233 |
Standard errors in parentheses.
**p < 0.01, ***p < 0.001.
Model 8: Household income quintile, maternal education, parental MHDs and adjusted for maternal birth age, family structure, number of siblings, type of municipality and immigrant background.
However, higher maternal education was associated with a lower risk for child's mental disorder in all age groups and for both genders. In addition, we can see that among girls, the negative association strengthened with age (model 1d–1f). For boys the association of education and mental disorder peaked at ages 7–12 (model 1b).
Genders also differed by age in terms of the association between parental mental disorder and child's mental disorder. For maternal and paternal mental disorders, the associations were strongest for boys aged 7–12 and for girls aged 13–17. The associations of maternal disorder were stronger than those of paternal disorder.
In conclusion, parental education seems to be a more robust socioeconomic indicator for inequality in childhood mental disorders even when controlling for family income. Therefore, the next analyses are only conducted with education.
In addition, we run a model, where interaction between maternal mental disorder and maternal education was included. The idea was to study whether higher maternal education would protect from the effect of maternal mental disorder discussed earlier. These results are shown in Fig. 5A and B as plots of average marginals effects, where the black line indicates children with a maternal mental disorder and those without it are the reference group.
Fig. 5.
Aand B. Average marginal effects of maternal mental disorder by maternal education.
For boys (Fig. 5A), the highest probabilities compared to the reference were among the lowest education level, and the probability decreased when education level was higher. Hence, higher maternal education protected boys from the association between maternal mental disorder and child's mental disorder as was expected. For girls (Fig. 5B) the results were not linear as the greatest probability for mental disorder was among those girls whose mothers had a middle education level, while the difference between the lowest and the highest education was small. However, these differences between maternal education levels were limited in size, less than one percentage point, and confidence intervals of the lowest and highest education level overlapped.
The difference between age groups and genders are expected because of differences in the specific diagnoses. Therefore, we conducted separate analyses for different diagnostic groups with mother's education as the main independent variable. The maternal education coefficients of these models are shown in Table 6. The highest level of maternal education associated with a lower probability of alcohol and other substance use disorders and depressive disorders for girls and trauma- and stress-related disorders for boys when compared to the lowest education level. The risk for ADHD/hyperkinetic and conduct disorders, emotional disorders with onset in childhood and other psychiatric disorders with onset in childhood also declined for both genders with a higher maternal education. Exceptions to this pattern were eating disorders, with which higher maternal education was associated with increased risk for girls and bipolar disorders, with which maternal education level was associated with increased risk for boys.
Table 6.
Results from linear probability models. Association between maternal education and child's mental disorder by gender and psychiatric diagnostic groups.
| Diagnostic group | Maternal education ref. Lower secondary or less |
Coefficient | |
|---|---|---|---|
| Boys | Girls | ||
| Alcohol and other substance use disorders | Upper secondary | −0.0001 | −0.0003 |
| Post-secondary or tertiary | −0.0004 | −0.0006** | |
| Schizophrenia spectrum disorders |
Upper secondary | 0.0001 | −0.00003 |
| Post-secondary or tertiary | 0.0002 | −0.00001 | |
| Bipolar disorders | Upper secondary | 0.0002** | 0.0002 |
| Post-secondary or tertiary | 0.0001 | 0.0001 | |
| Depressive disorders | Upper secondary | −0.0003 | −0.0005 |
| Post-secondary or tertiary | −0.0004 | −0.0022*** | |
| Anxiety disorders | Upper secondary | −0.0003 | −0.0003 |
| Post-secondary or tertiary | −0.0001 | −0.0008 | |
| Trauma- and stress-related disorders |
Upper secondary | −0.0011*** | 0.0002 |
| Post-secondary or tertiary | −0.0015*** | −0.0005 | |
| Eating disorders | Upper secondary | −0.00009 | 0.0005 |
| Post-secondary or tertiary | 0.00003 | 0.0016*** | |
| Autism spectrum and other disorders of psychological development | Upper secondary | −0.0005 | 0.0002 |
| Post-secondary or tertiary | −0.0013* | −0.00007 | |
| ADHD/Hyperkinetic disorders | Upper secondary | −0.0033*** | −0.0014*** |
| Post-secondary or tertiary | −0.0102*** | −0.0034*** | |
| Conduct disorders | Upper secondary | −0.0016*** | −0.0009*** |
| Post-secondary or tertiary | −0.0037*** | −0.0015*** | |
| Emotional disorders with onset specific to childhood | Upper secondary | −0.0009* | −0.0013** |
| Post-secondary or tertiary | −0.0015*** | −0.0017*** | |
| Other childhood onset disorders | Upper secondary | −0.0016** | −0.0006 |
| Post-secondary or tertiary | −0.0021*** | −0.0012** | |
*p < 0.1, **p < 0.01, ***p < 0.001.
Models adjusted for age group, maternal birth age, family structure, number of siblings, parental MHDs, type of municipality and immigrant background.
Only schizophrenia spectrum disorders had no statistically significant associations with maternal education. However, the prevalence of these disorders was low, which may have contributed to the unsignificant associations in our models. Parental mental disorders increased the probability of children's disorders in almost all diagnostic groups. It should be said that the effect sizes in all cases are quite small even in relation to the diagnosis-specific prevalence.
As an additional analysis we run the full model with maternal education separately for groups based on children's parents' country of origin. The coefficients of maternal education of these models are presented in Appendix A Table A3. All the groups of children with two foreign-born parents (where mother is from either Western countries, Eastern Europe, Africa/Middle East or Asia) had no statistically significant associations with maternal education and the coefficients were very close to zero.
5. Conclusions
Rising rates of mental health disorders among children and adolescents are rightly gaining attention from policymakers, researchers as well as the wider public. The increase has in some cases been accompanied with widening inequality between socioeconomic groups (e.g., Torikka et al., 2014). In the Nordic welfare states, aiming for equality of opportunity, this is a serious challenge as mental health problems have been shown to associate with social disadvantage later in life (e.g., Lundborg et al., 2014; Hakulinen, Musliner, & Agerbo, 2019; Haula & Vaalavuo, 2021).
We utilized unique Finnish register data on the total population to study how mental disorders and family's socioeconomic status are linked during early life course. We compared two measures of SES, household income and parental education level, and studied also whether parental mental disorders explain mental health disparities among children. The focus of this study was on how current income level, recent parental mental disorders and attained parental education level are associated with mental disorders and treatment contacts in public specialized health care of children aged 4–17 in year 2018. In addition, we contributed to existing evidence on the topic by examining differences between genders, age groups, and types of psychiatric diagnostic groups.
Our results illustrate that the association between any psychiatric disorder and socioeconomic status persisted through childhood, but complexity emerged when models included control variables. In the case of parents' education, children with lower SES had a higher probability for mental disorders than children with socioeconomic advantage. In contrast, after adjusting for control variables in our models, higher income was only partly associated with an increased risk for mental disorders. Importantly, the association between mental health and SES was stronger for education than for household income. In general, mental health disparities were clearer for boys than for girls. Parental mental disorders were strongly associated with a child's mental disorders, especially among older children, but they did not explain the SES differences, against our expectations. However, we did find an interaction effect between parental mental health disorders and mother's educational level showing that the risk of mental health disorders was higher especially among boys with low SES and parental disorders. This could mean that high SES families are able to protect their children from the negative effects of their own mental health problems. It should be noted, though, that important differences exist in the specific disorders experienced by boys, girls, and parents. More detailed analysis on parental disorders and offspring outcomes could be warranted to target policy interventions.
We further investigated whether the socioeconomic pattern can be found for immigrant children as well, but we did not identify statistically significant differences in mental health disorders by maternal education among children with parents born abroad. However, these results are uncertain, since register information on higher education of immigrants is shown to be unreliable due to a high amount of missingness in education degrees attained abroad (Sutela & Larja, 2015). In general, prior research on mental health among immigrants has found that immigrants use health services less than the native population (e.g., Kieseppä et al., 2020; Markkula, Lehti, Gissler, & Suvisaari, 2017). This could be due to many reasons, for example, the healthy immigrant effect (see Kennedy et al., 2015), stigma, or unequal access to treatment and services. Related to socioeconomic disparities in mental health, it could be that determinants of mental health disorders vary across ethnic groups (Beiser, Hou, Hyman, & Tousignant, 2002), and these determinants should be studied more in the immigrant population.
We do not provide causal evidence on the association between childhood mental health and parental background. However, these results are significant for depicting the early onset of health disparities. The differences found for education and income could mean that rather than just economic resources at home, the social environment, parenting skills and social networks associated with higher human capital could explain the social gradient in mental health (see Pichler & Wallace, 2009, on the social stratification of social capital, and Hoff & Laursen, 2019, on socioeconomic differences in parenting behaviour).
For example, a review by McPherson et al. (2014) found that parent–child relations, extended family support, social support networks, religiosity, and neighbourhood and school quality are linked with better mental health outcomes among children. Similarly, Rothon, Goodwin, and Stansfeld (2012) show that good relationships with parents, high parental surveillance and regular evening meals at home are associated with positive mental health. Both studies indicate that reinforcing these aspects of childhood environments could be ways to improve mental health also among lower SES families. In the future, intervention studies focusing on improving parent-child interaction and parenting practices could be a way to investigate effective ways to reduce inequalities in childhood mental health. Some randomized controlled trials on the topic already exist, and a review of evidence shows that they have been effective, but the positive impact fades away over time (Kjøbli et al., 2022).
While we found weaker SES gradient for household income, we cannot exclude that it would not have a causal impact on mental health. Causal evidence on the topic is scarce and policy changes could be used to study the topic in a quasi-experimental setting. Understanding better the reasons behind the findings of our study necessitates further research, which is fundamental for designing better policies for improving childhood mental health. The Finnish context is likely to play an important role too: a comprehensive social protection, school and service system helps in avoiding severe hardship. This could explain why parental education is more strongly than income associated with mental health outcomes in children. A recent study comparing the UK and Australia also showed that socioeconomic differences were more marked based on education in Australia, while income was a stronger SES predictor in the UK (Terhaag et al., 2021).
Previous research evidence suggests that differences in the relation of inequality and the type of mental health illness also exist. Therefore, in addition to general association between any psychiatric disorder and socioeconomic status, we also studied different disorder groups and found differences in the strength of the SES-disorder association. In the case of most disorders with onset in childhood, higher maternal education was associated with lower probability compared to the lowest education level. The associations were strongest for externalizing disorders and substance use disorders, while the effect sizes were quite small overall. This is consistent with previous studies (Ormel et al., 2015; Torvik et al., 2020). A notable exception for this pattern is eating disorders among girls as they were more common among girls with high maternal education. Previous studies have found this association especially in anorexia nervosa, while the association is less pronounced in other eating disorders (Koch et al., 2022).
The findings related to schizophrenia spectrum and bipolar disorders are consistent with previous literature suggesting that in early onset cases, the contribution of childhood socioeconomic factors is smaller whereas the contribution of genetic factors, including de novo rare variants, is more pronounced (Giannitelli et al., 2018; Kalman et al., 2021; O'Connell & Coombes, 2021). Nevertheless, childhood socioeconomic disadvantage as a risk factor for schizophrenia spectrum disorders is also documented (Agerbo et al., 2015; Schofield et al., 2021).
According to our findings as well as previous literature, adverse socioeconomic conditions and parental mental disorders have mostly independent effects on children's risk of developing mental disorders. On the other hand, these problems often co-occur and reinforce each other (Stolper et al., 2021). This underscores the importance of treating the whole family with a multi-agency approach, based on each family's individual vulnerabilities, when a child or a parent has a mental disorder.
To better understand these results, it is good to put them in context. Finland is a Nordic welfare state, where comprehensive public health care is offered to all citizens. Specialized health care services are provided in public hospitals and psychiatric specialized care is offered to children and adolescents when symptoms are severe and when primary or school health care are not able to offer adequate help. Expenses of health care are mainly paid by the home municipalities of citizens and specialized services are organized by hospital districts. User fees in hospitals are modest and have an annual payment ceiling, hence individual's or family's income should not strongly impact seeking treatment for illness. In addition, the services are mostly free for children under 18 years. Furthermore, comprehensive child health clinics and school health care system with regular health checks for all children ensure that identifying mental health disorders is not based only on parents' own activity and knowledge (see Nikander, Kosola, Vahlberg, Kaila, & Hermanson, 2022; Poutiainen, Hakulinen, Mäki, & Laatikainen, 2016).
While we used unique register data with massive amount of information, the data also has some limitations: it contained mainly the more severe psychiatric cases, because primary, school, and private health care were excluded. Another aspect about data coverage is that a large amount, about a half of Finnish children, have a supplementary health insurance and take-up is higher among high SES families (Valtonen, Kempers, & Karttunen, 2014). Therefore, it is possible that our data is missing psychiatric disorders of children who have highly educated parents and mainly use private services. However, Valtonen et al. (2014) demonstrate that both children with and without health insurance use public health care, and therefore children with health insurance are not necessarily completely left out of public records.
Ethical statement
The study is based on Finnish register data for which no ethical approvement is necessary. The data used is pseudonymized and no single individuals can be identified according to the rules by Statistics Finland.
The researchers follow the guidelines of TENK (Finnish National Board on Research Integrity): https://tenk.fi/en/research-misconduct/responsible-conduct-research-rcr.
Author statement
Maria Vaalavuo acquired funding for the research, conceptualised the study, designed the analytical strategy, participated in writing the article, and supervised Ripsa Niemi in her tasks; Ripsa Niemi was in charge of data management, literature review and empirical analyses; Jaana Suvisaari advised from psychiatry perspective and participated in interpreting the results and writing the conclusions. All participated in reviewing and editing the article.
Financial disclosure statement
This study has received funding from the Academy of Finland (decision number 342605).
Declaration of competing interest
No conflict of interest to declare.
Contributor Information
Maria Vaalavuo, Email: maria.vaalavuo@thl.fi.
Ripsa Niemi, Email: ripsa.niemi@thl.fi.
Jaana Suvisaari, Email: jaana.suvisaari@thl.fi.
Appendix A.
Table A1.
Results from linear probability model. Association between mother's education and child's mental disorder during 2014–2018, by gender.
| Boys |
Model 10a | Model 11a | Girls |
Model 10b | Model 11b | |
|---|---|---|---|---|---|---|
| Model 9a | Model 9b | |||||
| Maternal education Ref. Lower secondary or less | ||||||
| Upper Secondary | −0.017*** | −0.020*** | −0.014*** | −0.008** | −0.012*** | −0.008*** |
| (0.0016) | (0.0017) | (0.0017) | (0.0015) | (0.0016) | (0.0016) | |
| Post-secondary or tertiary | −0.048*** | −0.043*** | −0.033*** | −0.030*** | −0.028*** | −0.020*** |
| (0.0016) | (0.0017) | (0.0017) | (0.0015) | (0.0016) | (0.0016) | |
| Maternal mental health disorder Ref. no mental health disorder | ||||||
| Has disorder | 0.110*** | 0.092*** | ||||
| (0.0017) | (0.0015) | |||||
| Paternal mental health disorderRef. no mental health disorder | ||||||
| Has disorder | 0.060*** | 0.044*** | ||||
| (0.0020) | (0.0018) | |||||
| Constant | 0.068*** | 0.067*** | 0.048*** | 0.043*** | 0.050*** | 0.035*** |
| (0.0017) | (0.0021) | (0.0021) | (0.0015) | (0.0019) | (0.0019) | |
| N | 415,961 | 415,961 | 415,961 | 396,247 | 396,247 | 396,247 |
Standard errors in parentheses.
**p < 0.01, ***p < 0.001.
Model 1: Maternal education level and adjusted for age group and maternal birth age.
Model 2: Model 1 + adjusted for family structure, number of siblings, type of municipality, immigrant background.
Model 3: Model 2 + parental psychiatric disorders.
Table A2.
Results from linear probability model. Association between father's education and child's mental disorder during 2018, by gender.
| Boys |
Model 13a | Model 14a | Girls |
Model 13b | Model 141b | |
|---|---|---|---|---|---|---|
| Model 12a | Model 12b | |||||
| Paternal education Ref. Lower secondary or less | ||||||
| Upper Secondary | −0.017*** | −0.013*** | −0.011*** | −0.010** | −0.007*** | −0.005*** |
| (0.0010) | (0.0010) | (0.0010) | (0.0009) | (0.0010) | (0.0010) | |
| Post-secondary or tertiary | −0.033*** | −0.024*** | −0.020*** | −0.019*** | −0.011*** | −0.008*** |
| (0.0010) | (0.0011) | (0.0011) | (0.0010) | (0.0010) | (0.0010) | |
| Maternal mental health disorder Ref. no mental health disorder | ||||||
| Has disorder | 0.071*** | 0.060*** | ||||
| (0.0013) | (0.0012) | |||||
|
Paternal mental health disorder Ref. no mental health disorder |
||||||
| Has disorder | 0.040*** | 0.031*** | ||||
| (0.0015) | (0.0014) | |||||
| Constant | 0.042*** | 0.038*** | 0.028*** | 0.022*** | 0.024*** | 0.016*** |
| (0.0011) | (0.0014) | (0.0014) | (0.0010) | (0.0013) | (0.0013) | |
| N | 415,961 | 415,961 | 415,961 | 396,247 | 396,247 | 396,247 |
Standard errors in parentheses.
**p < 0.01, ***p < 0.001.
Model 1: Paternal education level and adjusted for age group and maternal birth age.
Model 2: Model 1 + adjusted for family structure, number of siblings, type of municipality, immigrant background.
Model 3: Model 2 + parental psychiatric disorders.
Table A3.
Results from linear probability models. Association between maternal education and child's mental disorder by immigration status.
| Immigration status | Maternal education ref. Lower secondary or less |
Coefficient |
|---|---|---|
| Both parents born in Finland (n = 688,878) | Upper secondary | −0.012*** |
| Post-secondary or tertiary | −0.022*** | |
| One parent born in Finland; another parent foreign-born (n = 67,366) | Upper secondary | −0.0003 |
| Post-secondary or tertiary | −0.006* | |
| Both parents foreign-born, mother from: | ||
| Western countries (n = 2379) | Upper secondary | 0.003 |
| Post-secondary or tertiary | 0.004 | |
| Eastern Europe (n = 22,626) | Upper secondary | 0.005 |
| Post-secondary or tertiary | −0.00002 | |
| Africa or Middle East (n = 22,773) | Upper secondary | 0.004 |
| Post-secondary or tertiary | 0.003 | |
| Asia (n = 6599) | Upper secondary | 0.007 |
| Post-secondary or tertiary | 0.001 | |
*p < 0.1, **p < 0.01, ***p < 0.001.
Models adjusted for gender, age group, maternal birth age, family structure, number of siblings, parental MHDs and type of municipality.
Data availability
The authors do not have permission to share data.
References
- Agerbo E., Sullivan P.F., Vilhjálmsson B.J., Pedersen C.B., Mors O., Børglum A.D., et al. Polygenic risk score, parental socioeconomic status, family history of psychiatric disorders, and the risk for schizophrenia: A Danish population-based study and meta-analysis. JAMA Psychiatry. 2015;72(7):635–641. doi: 10.1001/jamapsychiatry.2015.0346. [DOI] [PubMed] [Google Scholar]
- Atladottir H., Gyllenberg D., Langridge A., Sandin S., Hansen S., Leonard H., et al. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: A descriptive multinational comparison. European Child & Adolescent Psychiatry. 2015;24(2):173–183. doi: 10.1007/s00787-014-0553-8. [DOI] [PubMed] [Google Scholar]
- Barican J.L., Yung D., Schwartz C., Zheng Y., Georgiades K., Waddell C. Prevalence of childhood mental disorders in high-income countries: A systematic review and meta-analysis to inform policymaking. Evidence-Based Mental Health. 2022;25(1):36–44. doi: 10.1136/ebmental-2021-300277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiser M., Hou F., Hyman I., Tousignant M. Poverty, family process, and the mental health of immigrant children in Canada. American Journal of Public Health. 2002;92(2):220–227. doi: 10.2105/ajph.92.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøe T., Øverland S., Lundervold A.J., Hysing M. Socioeconomic status and children's mental health: Results from the Bergen Child Study. Social Psychiatry and Psychiatric Epidemiology. 2012;47(10):1557–1566. doi: 10.1007/s00127-011-0462-9. [DOI] [PubMed] [Google Scholar]
- Case A., Lubotsky D., Paxson C. Economic status and health in childhood: The origins of the gradient. The American Economic Review. 2002;92(5):1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Chen E., Martin A.D., Matthews K.A. Socioeconomic status and health: Do gradients differ within childhood and adolescence? Social Science & Medicine. 2006;62(9):2161–2170. doi: 10.1016/j.socscimed.2005.08.054. 1982. [DOI] [PubMed] [Google Scholar]
- Costello E., Compton S., Keeler G., Angold A. Relationships between poverty and psychopathology: A natural experiment. JAMA, the Journal of the American Medical Association. 2003;290(15):2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- Dean K., Stevens H., Mortensen P.B., Murray R.M., Walsh E., Pedersen C.B. Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Archives of General Psychiatry. 2010;67(8):822–829. doi: 10.1001/archgenpsychiatry.2010.86. [DOI] [PubMed] [Google Scholar]
- Dupre M.E. Educational differences in age-related patterns of disease: Reconsidering the cumulative disadvantage and age-as-leveler hypotheses. Journal of Health and Social Behavior. 2007;48(1):1–15. doi: 10.1177/002214650704800101. [DOI] [PubMed] [Google Scholar]
- Giannitelli M., Consoli A., Raffin M., Jardri R., Levinson D.F., Cohen D., et al. An overview of medical risk factors for childhood psychosis: Implications for research and treatment. Schizophrenia Research. 2018;192:39–49. doi: 10.1016/j.schres.2017.05.011. [DOI] [PubMed] [Google Scholar]
- Gyllenberg D., Marttila M., Sund R., Jokiranta-Olkoniemi E., Sourander A., Gissler M., et al. Temporal changes in the incidence of treated psychiatric and neurodevelopmental disorders during adolescence: An analysis of two national Finnish birth cohorts. The Lancet Psychiatry. 2018;5(3):227–236. doi: 10.1016/S2215-0366(18)30038-5. [DOI] [PubMed] [Google Scholar]
- Hakulinen C., Mok P.L.H., Horsdal H.T., Pedersen C.B., Mortensen P.B., Agerbo E., et al. Parental income as a marker for socioeconomic position during childhood and later risk of developing a secondary care-diagnosed mental disorder examined across the full diagnostic spectrum: A national cohort study. BMC Medicine. 2020;18(1):1–11. doi: 10.1186/s12916-020-01794-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakulinen C., Musliner K.L., Agerbo E. Bipolar disorder and depression in early adulthood and long-term employment, income, and educational attainment: A nationwide cohort study of 2,390,127 individuals. Depression and Anxiety. 2019;36(11):1080–1088. doi: 10.1002/da.22956. [DOI] [PubMed] [Google Scholar]
- Haula T., Vaalavuo M. Mental health problems in youth and later receipt of social assistance: Do parental resources matter? Journal of Youth Studies. 2021;25(7):877–896. doi: 10.1080/13676261.2021.1923676. [DOI] [Google Scholar]
- Hellevik O. Linear versus logistic regression when the dependent variable is a dichotomy. Quality and Quantity. 2009;43(1):59–74. doi: 10.1007/s11135-007-9077-3. [DOI] [Google Scholar]
- Hoff E., Laursen B. In: Handbook of parenting. Bornstein M.H., editor. Routledge; New York: 2019. Socioeconomic status and parenting. [Google Scholar]
- Hoffmann R., Kröger H., Pakpahan E. Pathways between socioeconomic status and health: Does health selection or social causation dominate in Europe? Advances in Life Course Research. 2018;36:23–36. doi: 10.1016/j.alcr.2018.02.002. [DOI] [Google Scholar]
- Kalman J.L., Olde Loohuis L.M., Vreeker A., et al. Characterisation of age and polarity at onset in bipolar disorder. British Journal of Psychiatry. 2021;219(6):659–669. doi: 10.1192/bjp.2021.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy S., Kidd M.P., McDonald J.T., et al. The healthy immigrant effect: Patterns and evidence from four countries. Journal of International Migration and Integration. 2015;16:317–332. doi: 10.1007/s12134-014-0340-x. [DOI] [Google Scholar]
- Kessler R.C., Amminger G.P., Aguilar‐Gaxiola S., Alonso J., Lee S., Ustun T.B. Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry. 2007;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kieseppä V., Torniainen-Holm M., Jokela M., et al. Immigrants' mental health service use compared to that of native Finns: A register study. Social Psychiatry and Psychiatric Epidemiology. 2020;55:487–496. doi: 10.1007/s00127-019-01774-y. [DOI] [PubMed] [Google Scholar]
- Kinge J.M., Øverland S., Flatø M., Dieleman J., Røgeberg O., Magnus M.C., et al. Parental income and mental disorders in children and adolescents: Prospective register-based study. International Journal of Epidemiology. 2021;50(5):1615–1627. doi: 10.1093/ije/dyab066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki M., Batty G.D., Pentti J., Shipley M.J., Sipilä P.N., Nyberg S.T., et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: A multi-cohort study. The Lancet Public Health. 2020;5(3):e140–e149. doi: 10.1016/S2468-2667(19)30248-8. [DOI] [PubMed] [Google Scholar]
- Kjøbli J., Melendez-Torres G.J., Gardner F., Backhaus S., Linnerud S., Leijten P. Research review: Effects of parenting programs for children's conduct problems on children's emotional problems - a network meta-analysis. Journal of Child Psychology and Psychiatry. 2022 doi: 10.1111/jcpp.13697. 2022 Sep. 13. Epub ahead of print. PMID: 36097742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch S.V., Larsen J.T., Plessen K.J., Thornton L.M., Bulik C.M., Petersen L.V. Associations between parental socioeconomic-, family-, and sibling status and risk of eating disorders in offspring in a Danish national female cohort. International Journal of Eating Disorders. 2022 doi: 10.1002/eat.23771. 2022 July 9. Epub ahead of print. PMID: 35809040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kröger H., Pakpahan E., Hoffmann R. What causes health inequality? A systematic review on the relative importance of social causation and health selection. The European Journal of Public Health. 2015;25(6):951–960. doi: 10.1093/eurpub/ckv111. [DOI] [PubMed] [Google Scholar]
- Kruk K.E. Parental income and the dynamics of health inequality in early childhood—evidence from the UK. Health Economics. 2013;22(10):1199–1214. doi: 10.1002/hec.2876. [DOI] [PubMed] [Google Scholar]
- Leopold L. Cumulative advantage in an egalitarian country? Socioeconomic health disparities over the life course in Sweden. Journal of Health and Social Behavior. 2016;57(2):257–273. doi: 10.1177/0022146516645926. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P., Cederlof M., Lundstrom S., D'Onofrio B.M., Anckarsater H., Larsson H., et al. Associations between conduct problems in childhood and adverse outcomes in emerging adulthood: A longitudinal Swedish nationwide twin cohort. Journal of Child Psychology and Psychiatry. 2020;61(7):798–806. doi: 10.1111/jcpp.13169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas N., Nicholson J.M., Erbas B. Child mental health after parental separation: The impact of resident/non-resident parenting, parent mental health, conflict and socioeconomics. Journal of Family Studies. 2013;19(1):53–69. doi: 10.5172/jfs.2013.19.1.53. [DOI] [Google Scholar]
- Lundborg P., Nilsson A., Rooth D.O. Adolescent health and adult labor market outcomes. Journal of Health Economics. 2014;37:25–40. doi: 10.1016/j.jhealeco.2014.05.003. [DOI] [PubMed] [Google Scholar]
- Markkula N., Lehti V., Gissler M., Suvisaari J. Incidence and prevalence of mental disorders among immigrants and native Finns: A register-based study. Social Psychiatry and Psychiatric Epidemiology. 2017;52(12):1523–1540. doi: 10.1007/s00127-017-1432-7. [DOI] [PubMed] [Google Scholar]
- McLaughlin K.A., Breslau J., Green J.G., Lakoma M.D., Sampson N.A., Zaslavsky A.M., et al. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Social Science & Medicine. 2011;73(7):1088–1096. doi: 10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson K.E., Kerr S., McGee E., et al. The association between social capital and mental health and behavioural problems in children and adolescents: An integrative systematic review. BMC Psychology. 2014;2:7. doi: 10.1186/2050-7283-2-7. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkonen J., Remes H., Moustgaard H., Martikainen P. Evaluating the role of parental education and adolescent health problems in educational attainment. Demography. 2020;57(6):2245–2267. doi: 10.1007/s13524-020-00919-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkonen J., Remes H., Moustgaard H., Martikainen P. Early adolescent health problems, school performance, and upper secondary educational pathways: A counterfactual-based mediation analysis. Social Forces. 2021;99(3):1146–1175. doi: 10.1093/sf/soaa048. [DOI] [Google Scholar]
- Mortensen P.B., Pedersen C.B., Melbye M., Mors O., Ewald H. Individual and familial risk factors for bipolar affective disorders in Denmark. Archives of General Psychiatry. 2003;60(12):1209–1215. doi: 10.1001/archpsyc.60.12.1209. [DOI] [PubMed] [Google Scholar]
- Najman J.M., Hayatbakhsh M.R., Clavarino A., Bor W., O’callaghan M.J., Williams G.M. Family poverty over the early life course and recurrent adolescent and young adult anxiety and depression: A longitudinal study. American Journal of Public Health. 2010;100(9):1719–1723. doi: 10.2105/AJPH.2009.180943. 1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikander K., Kosola S., Vahlberg T., Kaila M., Hermanson E. Associating school doctor interventions with the benefit of the health check: An observational study. BMJ Paediatric Open. 2022;6(1) doi: 10.1136/bmjpo-2021-001394. 2022 Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell K.S., Coombes B.J. Genetic contributions to bipolar disorder: Current status and future directions. Psychological Medicine. 2021;51(13):2156–2167. doi: 10.1017/S0033291721001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J., Raven D., van Oort F., Hartman C.A., Reijneveld S.A., Veenstra R., et al. Mental health in Dutch adolescents: A TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychological Medicine. 2015;45(2):345–360. doi: 10.1017/S0033291714001469. [DOI] [PubMed] [Google Scholar]
- Paananen R., Ristikari T., Merikukka M., Gissler M. Social determinants of mental health: A Finnish nationwide follow-up study on mental disorders. Journal of Epidemiology & Community Health. 2013;67(12):1025–1031. doi: 10.1136/jech-2013-202768. 1979. [DOI] [PubMed] [Google Scholar]
- Pichler F., Wallace C. Social capital and social class in Europe: The role of social networks in social stratification. European Sociological Review. 2009;25(3):319–332. doi: 10.1093/esr/jcn050. June 2009. [DOI] [Google Scholar]
- Poutiainen H., Hakulinen T., Mäki P., Laatikainen T. Family characteristics and parents' and children's health behaviour are associated with public health nurses' concerns at children's health examinations. International Journal of Nursing Practice. 2016;22(6):584–595. doi: 10.1111/ijn.12478. 2016 Dec. Epub 2016 Aug 31. [DOI] [PubMed] [Google Scholar]
- Ranta J., Raitasalo K. Disorders of cognitive and emotional development in children of mothers with substance abuse and psychiatric disorders. Nordic Studies on Alcohol and Drugs. 2015;32(6):591–604. doi: 10.1515/nsad-2015-0056. [DOI] [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. 1982. [DOI] [PubMed] [Google Scholar]
- Ringbom I., Suvisaari J., Kääriälä A., Sourander A., Gissler M., Ristikari T., et al. Psychiatric disorders diagnosed in adolescence and subsequent long-term exclusion from education, employment or training: Longitudinal national birth cohort study. British Journal of Psychiatry. 2021;220(3):148–153. doi: 10.1192/bjp.2021.146. [DOI] [PubMed] [Google Scholar]
- Rod N.H., Lange T., Petersen A.H. Do sibling comparisons answer the causal question? In response to ‘No causal associations between childhood family income and subsequent psychiatric disorders, substance misuse and violent crime arrests. International Journal of Epidemiology. 2021:1–2. doi: 10.1093/ije/dyab235. [DOI] [PubMed] [Google Scholar]
- Rothon C., Goodwin L., Stansfeld S. Family social support, community “social capital” and adolescents’ mental health and educational outcomes: A longitudinal study in england. Social Psychiatry and Psychiatric Epidemiology. 2012;47:697–709. doi: 10.1007/s00127-011-0391-7. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sariaslan A., Mikkonen J., Aaltonen M., Hiilamo H., Martikainen P., Fazel S. No causal associations between childhood family income and subsequent psychiatric disorders, substance misuse and violent crime arrests: A nationwide Finnish study of >650 000 individuals and their siblings. International Journal of Epidemiology. 2021;50(5):1628–1638. doi: 10.1093/ije/dyab099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield P., Das-Munshi J., Webb R.T., Horsdal H.T., Pedersen C.B., Agerbo E. Lack of fit with the neighbourhood social environment as a risk factor for psychosis - a national cohort study. Psychological Medicine. 2021:1–9. doi: 10.1017/S0033291721002233. Epub ahead of print. PMID: 34140057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.P., Smith G.C. Long-term economic costs of psychological problems during childhood. Social Science & Medicine. 2010;71(1):110–115. doi: 10.1016/j.socscimed.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohschein L. Parental divorce and child mental health trajectories. Journal of Marriage and Family. 2005;67(5):1286–1300. doi: 10.1111/j.1741-3737.2005.00217.x. [DOI] [Google Scholar]
- Sutela H., Larja L. Tilastokeskus; Helsinki: 2015. Ulkomaalaistaustaisessa väestössä paljon korkeasti ja paljon matalasti koulutettuja.www.stat.fi/tup/maahanmuutto/art_2015-11-02_001.htmlStolper [internet publication]. 2.11.2015. Accessed. [Google Scholar]
- Tienari P., Wynne L.C., Sorri A., Lahti I., Läksy K., Moring J., et al. Genotype–environment interaction in schizophrenia-spectrum disorder: Long-term follow-up study of Finnish adoptees. The British Journal of Psychiatry. 2004;184(3):216–222. doi: 10.1192/bjp.184.3.216. [DOI] [PubMed] [Google Scholar]
- Torikka A., Kaltiala-Heino R., Rimpelä A., Marttunen M., Luukkaala T., Rimpelä M. Self-reported depression is increasing among socio-economically disadvantaged adolescents – repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. 2014;14:408. doi: 10.1186/1471-2458-14-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torvik F.A., Eilertsen E.M., McAdams T.A., Gustavson K., Zachrisson H.D., Brandlistuen R., et al. Mechanisms linking parental educational attainment with child ADHD, depression, and academic problems: A study of extended families in the Norwegian mother, father and child cohort study. Journal of Child Psychology and Psychiatry. 2020;61(9):1009–1018. doi: 10.1111/jcpp.13197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaalavuo M., Bakkum B. Mental health problems at a critical juncture: Exit from social assistance among young Finns. Journal of Social Policy. 2021;50(4):764–787. doi: 10.1017/S0047279420000501. [DOI] [Google Scholar]
- Vaalavuo M., Salokangas H., Tahvonen O. Gender inequality reinforced: The impact of a child's health shock on parents' labor market trajectories. INVEST working. 2022 doi: 10.31235/osf.io/wx83z. paper 51/2022. [DOI] [PubMed] [Google Scholar]
- Valtonen H., Kempers J., Karttunen A. Supplementary health insurance in Finland. Consumer preferences and behaviour. Kela Working papers 65. 2014 http://hdl.handle.net/10138/135958 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.