Abstract
Purpose
Delay of elective surgeries, such as total joint replacement (TJR), is a common procedure in the current pandemic. In trauma surgery, postponement is associated with increased complication rates. This study aimed to evaluate the impact of postponement on surgical revision rates and postoperative complications after elective TJR.
Methods
In a retrospective analysis of 10,140 consecutive patients undergoing primary total hip replacement (THR) or total knee replacement (TKR) between 2011 and 2020, the effect of surgical delay on 90-day surgical revision rate, as well as internal and surgical complication rates, was investigated in a university high-volume arthroplasty center using the institute’s joint registry and data of the hospital administration. Moreover, multivariate logistic regression models were used to adjust for confounding variables.
Results
Two thousand four hundred and eighty TJRs patients were identified with a mean delay of 13.5 ± 29.6 days. Postponed TJR revealed a higher 90-day revision rate (7.1–4.5%, p < 0.001), surgical complications (3.2–1.9%, p < 0.001), internal complications (1.8–1.2% p < 0.041) and transfusion rate (2.6–1.8%, p < 0.023) than on-time TJR. Logistic regression analysis confirmed delay of TJRs as independent risk factor for 90-day revision rate [OR 1.42; 95% CI (1.18–1.72); p < 0.001] and surgical complication rates [OR 1.51; 95% CI (1.14–2.00); p = 0.04].
Conclusion
Alike trauma surgery, delay in elective primary TJR correlates with higher revision and complication rates. Therefore, scheduling should be performed under consideration of the current COVID-19 pandemic.
Level of evidence
Level III—retrospective cohort study.
Keywords: Surgical delay, Surgery postponement, Elective surgery, TJR, THA, TKA, Postoperative complications, Revision rate, COVID-19 pandemic
Introduction
Considering current statistical findings, the population is aging as a result of demographic change [1]. In the year 2019, about 16.5% of the US population was older than 65 years [2]. Some projections assume an increase in this generation to a level of 23.4% in the year 2060 [3]. Also from a more moderate point of view, it can be concluded consequently that the number of degenerative diseases and the number of necessary TJRs in the population will increase. According to the 2021 annual report of the American Academy of Orthopedic Surgeons (AAOS) in the year 2020, about 254,295 TJRs were recorded in the American Joint Registry [4]. However, these data may be not complete. Unreported cases can be assumed here. Other evaluations like the US Healthcare Cost and Utilization Project (H-CUP) recorded a larger number of total joint arthroplasty procedures (599,500 THR and 715,200 TKR) for the year 2018 in the USA [5]. Some studies anticipate a drastic increase in hip and knee arthroplasty and in revision procedures by the year 2030 [6] with rising postoperative complications [7] and an estimated cost to Medicare of 50 billion US $ per year [8]. This means a big burden for the patients and a huge effort for the healthcare systems.
During the COVID-19 pandemic, delays of planned surgeries and especially of elective total joint replacement surgeries are becoming more and more frequent [9, 10]. This postponement of elective orthopedic surgeries additionally causes a major organizational and economical challenge [11, 12]. With the spread of the COVID-19 pandemic, there is a need to relearn how to budget and distribute resources and restructure patient care [13]. Setting priorities in favor of emergency and trauma surgery a massive decline in elective primary TJR as well as in revision TJR services was observed [9, 14]. A survey from the European Hip Society (EHS) and the European Knee Associates (EKA) showed a drastic reduction in arthroplasty surgeries of 82.6% and TJR delay rates of 50.7% during the COVID-19 pandemic [15]. Studies report on the dropping of 30,000 primary TJR and 3000 revision arthroplasty procedures in the USA per week [16]. The consequences of these developments have been unknown so far.
In the literature delays, acute trauma surgery correlated with increased postoperative mortality and showed a trend toward higher postoperative complications [17, 18]. For elective surgeries, prolonged waiting time has demonstrated an adverse effect on the functional outcome of THR procedures [19]. To our knowledge, no correlation between delay after primary elective TJR and increased complications or increased revision rates has been described so far.
The objective of the presented paper was to assess the effect of postponing elective primary TJR on revision and complication rates in a university high-volume arthroplasty center. We first quantified the amount of delay after elective TJR. As the primary question of this study we asked, if there was a positive correlation of postponement of elective TJR procedures and a higher revision rate (90-day and 60-day revision rate). In addition, the correlation of delay in surgery and postoperative transfusion rate and surgical and internal complications was investigated using the institute’s joint registry and data of the hospital’s administration. Finally, we investigated possible confounders correlating with a higher revision rate after elective primary TJR.
Materials and methods
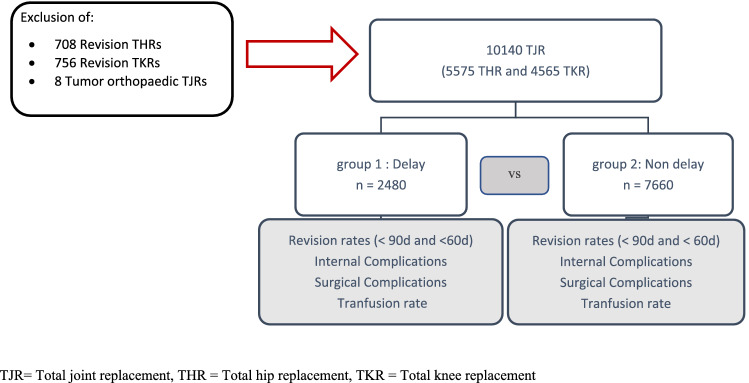
In a retrospective search, data of 10,140 consecutive patients undergoing elective primary total hip or knee replacement in a German Orthopedic University Hospital were identified. Patient data from the time period from January 2011 to December 2020 was retrieved from the in-house database (ORBIS; Agfa healthcare). Only elective primary THR or TKR surgeries were included in the study. Acute trauma cases, such as proximal femoral neck fractures, but also revision surgery or periprosthetic joint infections were excluded. From this population, 2480 patients with preoperative postponement of at least one day were selected, using the OPS-codes (Operation and Procedure Code) and individual case numbers. In contrast, 7660 patients could be identified who did not show preoperative delay, and the operation was performed as initially scheduled. If the surgery was performed at least one day later than initially scheduled, then this was defined as delay. Further patient data such as age, sex, BMI, ASA-Score (American Society of Anesthesiologists), operating time, hospital frailty risk score (HFRS) [20], internal and surgical complications, transfusion rates (yes/no), and reoperation rate < 90 days and < 60 days were evaluated using the institute’s joint registry and the data of the hospital’s administration system from 2011 until 2020 (Fig. 1). Complications were categorized in internal complications (cardiac complications: myocardial infarction and heart rhythm disorders; pulmonal complications: pneumonia and pulmonary edemas; renal complications: renal insufficiency and electrolyte derangement) and surgical complications (fractures, wound healing disturbance, and mechanical complications). The survey of the HFRS was conducted with the retrospective assignment of individual ICD-10 codes to each patient. These were matched with the 109 ICD-10 codes, which are characteristic for frailty and which are allocated to the respective severity of frailty in the form of point scores as defined by Gilbert et al. [20]. In summation, the maximal achievable score is 173.2 points [20].
Fig. 1.
Flowchart of the study population
All operations were performed in a single high-volume arthroplasty university center. All patients received the same standardized treatment protocol for THR or TKR, respectively. Cementless THR was performed in the lateral decubitus position. A minimally invasive anterolateral approach was used [21]. Press-fit acetabular components and cement-free stems of one single manufacturer (Pinnacle cup, Corail stem or Trilock stem; DePuy Synthes, J & J Medical Devices, Warsaw, IN) were used in all THR procedures. Cemented TKR was performed through a medial parapatellar approach. Cemented components of one single manufacturer (PFC Sigma; DePuy Synthes, J & J Medical Devices) were used in all TKRs. No patella resurfacing was performed.
For statistical analysis, continuous data are presented as mean (standard deviation). Group comparisons were performed by two-sided t tests. Absolute and relative frequencies were given for categorical data and compared between groups by Chi-square tests. The endpoints of the study were tested on 5% significance level. Multivariable logistic regression analyses were conducted to assess whether preoperative delay in primary elective total hip and knee arthroplasty independently correlates with postoperative revision rate while controlling for other variables such as operative time, type of surgery, sex, age, ASA classification, or frailty. IBM SPSS Statistics 26 (SPSS Inc, Chicago, IL, USA) was used for analysis.
Results
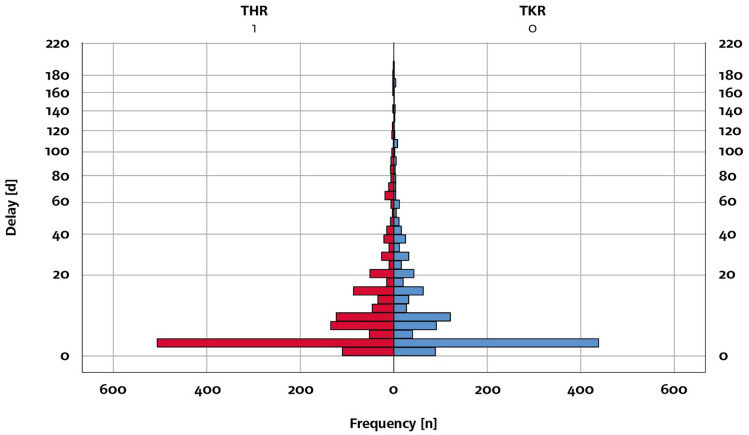
In the analysis of our in-house database (ORBIS; Agfa healthcare), we found data of 10,104 patients with condition after successful total joint arthroplasty in a time period from January 2011 to December 2020. Of these population, 55% (n = 5.575) people had undergone a hip replacement surgery and 45% (n = 4.565) a knee replacement surgery. The demographic characteristics of the study population are listed in Table 1. Among this population, there were 2480 patients with preoperative postponed elective surgeries, of which could be subdivided into 1335 delayed THR and 1145 delayed TKR surgeries. The mean of the delayed days until surgery for all TJRs was 13.5 days (SD: 29.6 days, THRs: 13.1 days, SD: 29.0; TKRs: 13.9 days, SD: 30.3, Fig. 2).
Table 1.
Demographics of the study group
| No delay n = 7660 | Delay n = 2480 | Total n = 10,140 | p value | |
|---|---|---|---|---|
| Sex | ||||
| Female | 57.2% | 58.9% | 57,6% | 0.12 |
| Male | 42.8% | 41.1% | 42,4% | |
| THA | 55.4% | 53.8% | 55% | 0.19 |
| TKA | 44.6% | 46.2% | 45% | |
| ASA | ||||
| I | 13.0% | 12.0% | 12.7% | 0.02 |
| II | 57.1% | 54.9% | 56.5% | |
| III | 29.7% | 32.6% | 30.5% | |
| IV | 0.2% | 0.4% | 0.3% | |
| Age (years) | 66.1 (10.7) | 66.0 (10.8) | 66.1 (10.7) | 0.54 |
| BMI (kg/m2) | 29.0 (5.5) | 29.1 (5.3) | 29.1 (5.4) | 0.70 |
| HFRS | 1.1 (2.0) | 1.1 (1.9) | 1.1 (2.0) | 0.89 |
| Operative time (min) | 76.2 (30.9) | 77.6 (28.7) | 76.5 (30.4) | 0.05 |
| Length of stay (days) | 8.9 (3.0) | 10.0 (5.0) | 9.1 (3.6) | < 0.001 |
Age, BMI, HFRS, operative time and length of stay are specified in mean (standard deviation)
THA total hip arthroplasty, TKA total knee arthroplasty, ASA American Society of Anesthesiologists, BMI body mass index, HFRS Hospital frailty risk score
Fig. 2.
Frequency of delay of elective TJR. The frequency (= n) of the delay of elective TJR (d = days)
In the univariate analysis, delay in elective primary TJR correlated with a higher revision rate < 90 days with 7.1% (175/2480) than on-time surgery with 4.5% (345/7660; p < 0.001). Similarly, the rate of revisions < 60 days was higher after delay in elective primary TJR with 6.6% (164/2480) compared to on-time surgery with 3.9% (300/7660; p < 0.001). Internal complications after delay in elective primary TJR were with 1.8% (44/2480) higher than on-time TJRs with 1.2% (94/7660) (p value < 0.001). Surgical complications after delay in elective primary TJR showed even higher percentages of 3.2% (79/2480) in contrast to the on-time TJRs of 1.9% (146/7660) (p value < 0.001). Postoperative transfusion was higher after postponed TJRs with 2.6% (64/2480) in comparison with TJRs without delay with 1.8% (141/7660) (p value < 0.001). In addition to this results, individual univariate analyses of delay in elective primary THR and TKR were also broken down (Table 2). Considering the time of delay in days, a longer delay did not correlate with higher complication rates (internal/surgical complications, revisions < 90 days, Fig. 3).
Table 2.
Results of univariate analysis with Pearson’s Chi-quadrat test of delayed TJR
| TJRs | No delay n = 7660 |
Delay n = 2480 |
Population n = 10,140 |
p value |
|---|---|---|---|---|
| Univariate analysis with Pearson’s Chi-Quadrat-Test of TJR | ||||
| THRs | No delay n = 4240 |
Delay n = 1335 |
Total n = 5575 |
p value |
|---|---|---|---|---|
| Total hip replacements | ||||
| Revisions < 90 days | 4.5% (191) | 7.0% (93) | 5.1% (284) | < 0.001 |
| Revisions < 60 days | 4.1% (173) | 6.4% (86) | 4.6% (259) | < 0.001 |
| Internal complications | 1.1% (47) | 2.3% (31) | 1.4% (78) | < 0.001 |
| Surgical complications | 2.2% (92) | 3.9% (52) | 2.6% (144) | < 0.001 |
| Transfusion rate (yes/no) | 2.0% (83) | 2.7% (36) | 2.1% (119) | 0.103 |
| TKRs | No delay n = 3420 |
Delay n = 1145 |
Total n = 4565 |
p value |
|---|---|---|---|---|
| Total knee replacements | ||||
| Revisions < 90 days | 4.5% (154) | 7.2% (82) | 5.2% (236) | < 0.001 |
| Revisions < 60 days | 3.7% (127) | 6.8% (78) | 4.5% (205) | < 0.001 |
| Internal complications | 1.4% (47) | 1,1% (13) | 1.3% (60) | 0.539 |
| Surgical complications | 1.6% (54) | 2.4% (27) | 1.8% (81) | 0.840 |
| Transfusion rate (yes/no) | 1.7% (58) | 2.4% (28) | 1.9% (86) | 0.106 |
The bold values highlight the significant data
Internal complications: cardiac complications like myocardial infarction and heart rhythm disorders, pulmonal complications like pneumonia and pulmonary edemas, renal complications like renal insufficiency or electrolyte derangement. Surgical complications: fractures, wound healing disturbance and mechanical complications. Transfusion rate (yes/no). The data of the sections no delay, delay and total are presented in percentage (%) and number (n)
TJR total joint replacement, THR total hip replacement, TKR total knee replacement
Fig. 3.
Adverse events in correlation to preoperative delay of elective TJR. Means of adverse events in correlation to delay of elective TJR in days
Even in multivariable analyses, delay in elective primary TJR showed a significant higher correlation with revision surgeries < 90 days [OR 1.42; CI (1.18–1.72); p < 0.001] and < 60 days [OR 1.59; CI (1.30–1.94); p < 0.001] than non-delayed surgeries. Other parameters such as ASA [OR 1.58; CI (1.34–1.85): p < 0.001], operative time [OR 1.01; CI (1.01–1.02): p < 0.001], and HFRS [OR 2.19; CI (1.61–2.97): p < 0.001] revealed an additional effect on the probability of occurrence of required revision surgery < 90 days. The results held true for 60-day revision rates (Table 3).
Table 3.
Multivariate analysis showing the effect of preoperative delay of elective TJR on operative revision rate < 90 and < 60 days
| OR (CI 95%) | p value | |
|---|---|---|
| Multivariate analysis with logistic regression | ||
| Revisions < 90 days | ||
| Delay | 1.42 (1.18 – 1.72) | < 0.001 |
| ASA | 1.58 (1.34 – 1.85) | < 0.001 |
| Age | 1.01 (0.99 – 1.02) | 0.191 |
| Sex | 0.89 (0.73 – 1.08) | 0.220 |
| Operative time | 1.01 (1.01 – 1.02) | < 0.001 |
| TKR | 0.92 (0.76 – 1.11) | 0.390 |
| HFRS | 2.19 (1.61 – 2.97) | < 0.001 |
| Revision < 60 days | ||
| Delay | 1.59 (1.30 – 1.94) | < 0.001 |
| ASA | 1.58 (1.33 – 1.87) | < 0.001 |
| Age | 1.01 (0.99 – 1.02) | 0.071 |
| Sex | 0.87 (0.71 – 1.07) | 0.185 |
| Operative time | 1.01 (1.01 – 1.02) | < 0.001 |
| TKR | 0.88 (0.72 – 1.08) | 0.210 |
| HFRS | 2.35 (1.72 – 3.22) | < 0.001 |
Multivariate calculations via logistic regression analyses to be aware of confounding variables
The bold values highlight the significant data
OR odds ratio, CI confidence interval, ASA American Society of Anesthesiologists, TKR total knee replacement, HFRS Hospital frailty risk score
In summary, the present study found a correlation between delay in elective primary TJR and increased 90-day revision rates, internal and surgical complications, and transfusion rates.
Discussion
In the present study, we evaluated the effect of postponed elective surgery on revision and complication rates in elective TJR in a high-volume arthroplasty center. Analyzing a consecutive cohort of over 10,000 patients, delay in elective primary TJR correlated with increased revision rates within the first 90 days and similarly with higher internal and surgical complications and transfusion rates.
As described in the literature, it is recommended that surgical treatment of femoral neck fractures should be performed as early as possible within a range of 6–24 h in acute trauma care [22–24]. Looking at the postoperative mortality, morbidity, and postoperative complication rates, there is a significant correlation with a surgical delay of more than 24 h [17, 18, 22–26, 31–34]. There are even reports that the relative risk of death is up to 4.5-fold higher, if surgery does not occur until 24 h after admission [35]. Several studies confirm especially the rise of internal and surgical complication rates with a surgical delay of traumatic proximal femoral fractures of more than 24 h [26, 29, 36, 37]. One study even showed an increase in the relative risk of lethality and early revision by about one third in case of delay of more than 24 h [29]. Another study showed that patients with proximal femur fracture and a longer preoperative waiting time for surgery had an increased rate of early needed surgical revision with 6.4% [29]. It can be seen that our elective outcomes regarding revision rates are comparable to these values.
In the field of elective surgery, to our knowledge, there are only few studies showing an association of surgery postponement and complication rates. A study group in the sector of elective spine surgery found that patients with concomitant diseases and surgical delays showed an increased coherence with postoperative complications, like deep venous thrombosis and pulmonary embolism, return to the operating room, sepsis, cerebrovascular accident, progressive renal insufficiency, prolonged ventilator time, urinary tract infection, pneumonia, and wound infections. The deep wound infections in this paper were for example significantly higher for postponed surgeries with 3.2% compared with 1.0% for on-time surgeries. [38]. In elective spine surgery, a correlation between delays and negative patient outcomes could also be observed [39]. Looking at the above-mentioned rates of deep wound infections in delayed elective spine surgery, the rates are also comparable to our results concerning the revision rates of delayed surgeries, although there were slightly higher rates in our data. This shows that postponement of elective surgeries has negative effects.
As the number of elective total joint arthroplasty has risen even before the COVID-19 pandemic [6], a pronounced waiting time for elective joint replacement surgery could be observed due to an increasing demand [9]. With the developments and necessary measures in the context of the pandemic, the waiting time for elective total joint replacement surgery is reaching a peak. Even patients with severe symptoms have to be postponed due to limited resources for elective surgery. A study by Pietrzak et al. confirmed that patients whose elective TJA surgery was postponed during the COVID-19 pandemic experienced more pain and worse function [40]. Additionally, considering the costs for the healthcare system in the literature demonstrated that a postponement of elective operations causes a high financial burden [41, 42]. Furthermore, there is research showing that end-stage osteoarthritis causes a higher postoperative need for opioid analgesia and results in a worse outcome in terms of revisions and readmission rates after TJA [43]. In particular, even psychosocial consequences are to be expected in this context [44].
Given the current evolution of the COVID-19 pandemic, the primary need is to properly allocate resources (staff, beds, ICU beds, economic resources, post-discharge care, etc.) [45] and contain the pandemic spread. However, given the continuing and recurring constraints, secondarily in the long term, it is also necessary to find strategies and ways to allow elective surgery to avoid the far-reaching consequences that arise from surgical delays. Plans and models must be drawn up to deal with these consequences from a medical and financial point of view. Meanwhile, there are already research foci dealing with the perioperative management of elective surgery in times of the COVID-19 pandemic [46, 47]. Perhaps, this study can help to initiate more research in this area of elective surgery to minimize the risk of surgical revisions and postoperative complications.
Looking at the covariates in the multivariable correlation calculations, we could see that ASA, HFRS, and operative time also had an effect on revision rates < 90 days and < 60 days. While operative time and ASA showed a significant effect on surgical complications, ASA, age, and HFRS had a significant effect on internal medicine complications. In addition, there was a statistically significant effect of ASA, age, operative time, and HFRS on postoperative transfusion rates. These results are not surprising and confirm data from the known literature.
The present study certainly has some limitations. One of them is the model of a database study and the related retrospective design, which might favor a potential bias. We tried to reduce this analyzing a consecutive series of patients over a period of almost 10 years. Second, the current available data are limited to the data entered in our joint registry and coding program. Consequently, the resulting quality of information may be inherently limited. Other interesting parameters were not assessed and therefore not available. In particular, it would be interesting to know which complications occur more frequently and have the highest relevance when surgery is postponed. In this regard, our data were also limited, so we had to pool the individual complications to prove an effect. Another interesting point would be the detection of the different preoperative reasons for the postponement of surgeries. Unfortunately, this information was not collected in our database, so that it could not be utilized. However, it might have an impact on the results whether the scheduled surgery was delayed due to administrative or medical reasons. This subject could be content of further research projects.
The strengths of the present study are the big study cohort with over 10,000 patients and the monocentric design including a highly standardized surgical procedure with a standardized postoperative physiotherapeutic rehabilitation program avoiding potential confounders.
Conclusion
The initial study objective could be successfully confirmed by demonstrating that there is a significant association of preoperative delay of elective TJR with revision surgery rates < 90 and < 60 days and also with internal and surgical complications and transfusion rates. This context is an important factor in long-term assessment and organization of elective surgeries with respect to changing demographics and the current COVID-19 pandemic.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by DEH, MM, MW, MT, SP, and FvonK. The first draft of the manuscript was written by DEH, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no funding, grants or other support.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Conflict of interest
There are no conflicts of interest among the authors.
Ethics approval
The study was approved by the local ethic commission of University of Regensburg, Germany (20-1821-104). It was performed in line with the principles of the Declaration of Helsinki.
Consent to participate
For this type of study, consent to participate is not required.
Consent to publish
For this type of study, consent for publication is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kanasi E, Ayilavarapu S, Jones J. The aging population: demographics and the biology of aging. Periodontol 2000. 2016;72:13–18. doi: 10.1111/prd.12126. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Census Bureau. 2019 American Community Survey 1-Year Estimates. TABLE ID: DP05. https://data.census.gov/cedsci/table?tid=ACSDP1Y2019.DP05. Accessed 04 July 2022
- 3.Demographic Turning Points for the United States: Population Projections for 2020 to 2060. U.S. Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf. Accessed 04 Jan 2022
- 4.American Joint Replacement Registry (AJRR) (2021) 2021 Annual Report. American Academy of Orthopaedics Surgeons (AAOS), Rosemont
- 5.US Health Care Cost and Utilization Project (HCUP). Overview of Operating Room Procedures During Inpatient Stays in U.S. Hospitals, 2018. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb281-Operating-Room-Procedures-During-Hospitalization-2018.pdf. Accessed 04July 2022
- 6.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 7.Acuña AJ, Do MT, Samuel LT, et al. Periprosthetic joint infection rates across primary total hip arthroplasty surgical approaches: a systematic review and meta-analysis of 653,633 procedures. Arch Orthop Trauma Surg. 2021;142:2965–2977. doi: 10.1007/s00402-021-04186-3. [DOI] [PubMed] [Google Scholar]
- 8.Wilson NA, Schneller ES, Montgomery K, Bozic KJ. Hip and knee implants: current trends and policy considerations. Health Aff (Millwood) 2008;27:1587–1598. doi: 10.1377/hlthaff.27.6.1587. [DOI] [PubMed] [Google Scholar]
- 9.Brown TS, Bedard NA, Rojas EO, et al. The effect of the COVID-19 pandemic on hip and knee arthroplasty patients in the United States: a multicenter update to the previous survey. Arthroplasty Today. 2021;7:268–272. doi: 10.1016/j.artd.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hunger R, König V, Stillger R, Mantke R. Impact of the COVID-19 pandemic on delays in surgical procedures in Germany: a multi-center analysis of an administrative registry of 176,783 patients. Patient Saf Surg. 2022;16:22. doi: 10.1186/s13037-022-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor CM, Anoushiravani AA, DiCaprio MR, et al. Economic recovery after the COVID-19 pandemic: resuming elective orthopedic surgery and total joint arthroplasty. J Arthroplasty. 2020;35:S32–S36. doi: 10.1016/j.arth.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tu Y, Ning Y, Li K, et al. After-hour elective total knee arthroplasty does not affect clinical outcomes but negatively affects alignment. Arch Orthop Trauma Surg. 2022 doi: 10.1007/s00402-022-04490-6. [DOI] [PubMed] [Google Scholar]
- 13.Zagra L, Faraldi M, Pregliasco F, et al. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020;44:1591–1598. doi: 10.1007/s00264-020-04590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reichert M, Sartelli M, Weigand MA, et al. Two years later: Is the SARS-CoV-2 pandemic still having an impact on emergency surgery? An international cross-sectional survey among WSES members. World J Emerg Surg. 2022;17:34. doi: 10.1186/s13017-022-00424-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thaler M, Khosravi I, Hirschmann MT, et al. Disruption of joint arthroplasty services in Europe during the COVID-19 pandemic: an online survey within the European Hip Society (EHS) and the European Knee Associates (EKA) Knee Surg Sports Traumatol Arthrosc. 2020;28:1712–1719. doi: 10.1007/s00167-020-06033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parvizi J, Gehrke T, Krueger CA, et al. Resuming elective orthopaedic surgery during the COVID-19 pandemic: guidelines developed by the International Consensus Group (ICM) J Bone Jt Surg. 2020;102:1205–1212. doi: 10.2106/JBJS.20.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verbeek DOF, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32:13–18. doi: 10.1007/s00264-006-0290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anesth Can Anesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 19.Garbuz DS, Xu M, Duncan CP, et al. Delays worsen quality of life outcome of primary total hip arthroplasty. Clin Orthop. 2006;447:79–84. doi: 10.1097/01.blo.0000203477.19421.ed. [DOI] [PubMed] [Google Scholar]
- 20.Gilbert T, Neuburger J, Kraindler J, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391:1775–1782. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michel MC, Witschger P. MicroHip: a minimally invasive procedure for total hip replacement surgery using a modified Smith-Peterson approach. Ortop Traumatol Rehabil. 2007;9(1):46–51. [PubMed] [Google Scholar]
- 22.Bonnaire FA, Weber AT. The influence of haemarthrosis on the development of femoral head necrosis following intracapsular femoral neck fractures. Injury. 2002;33:33–40. doi: 10.1016/S0020-1383(02)00329-7. [DOI] [PubMed] [Google Scholar]
- 23.Manninger J, Kazar G, Fekete G, et al. Significance of urgent (within 6 h) internal fixation in the management of fractures of the neck of the femur. Injury. 1989;20:101–105. doi: 10.1016/0020-1383(89)90152-6. [DOI] [PubMed] [Google Scholar]
- 24.Beringer TR, Crawford VL, Brown JG. Audit of surgical delay in relationship to outcome after proximal femoral fracture. Ulster Med J. 1996;65:32–38. [PMC free article] [PubMed] [Google Scholar]
- 25.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Jt Surg. 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 26.Alvi HM, Thompson RM, Krishnan V, et al. Time-to-surgery for definitive fixation of hip fractures. A look at outcomes based upon delay. Am J Orthop. 2018 doi: 10.12788/ajo.2018.0071. [DOI] [PubMed] [Google Scholar]
- 27.Davis FM, Woolner DF, Frampton C, et al. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br J Anaesth. 1987;59:1080–1088. doi: 10.1093/bja/59.9.1080. [DOI] [PubMed] [Google Scholar]
- 28.Bredahl C, Nyholm B, Hindsholm KB, et al. Mortality after hip fracture: results of operation within 12 h of admission. Injury. 1992;23:83–86. doi: 10.1016/0020-1383(92)90037-S. [DOI] [PubMed] [Google Scholar]
- 29.Müller-Mai CM, Schulze Raestrup US, Kostuj T, et al. Einjahresverläufe nach proximalen Femurfrakturen: Poststationäre Analyse von Letalität und Pflegestufen durch Kassendaten. Unfallchirurg. 2015;118:780–794. doi: 10.1007/s00113-013-2534-7. [DOI] [PubMed] [Google Scholar]
- 30.Holt EM, Evans RA, Hindley CJ, Metcalfe JW. 1000 femoral neck fractures: the effect of pre-injury mobility and surgical experience on outcome. Injury. 1994;25:91–95. doi: 10.1016/0020-1383(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 31.Laberge A, Bernard PM, Lamarche PA. Relationship between preoperative delay in hip fractures, postoperative complications and risk of death. Rev Epidemiol Sante Publ. 1997;45:5–12. [PubMed] [Google Scholar]
- 32.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–951. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zuckerman JD, Skovron ML, Koval KJ, et al. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Jt Surg. 1995;77:1551–1556. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Yosef D, Tauber C, Cohen D, Gdalevich M. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004;124:334–340. doi: 10.1007/s00402-004-0662-9. [DOI] [PubMed] [Google Scholar]
- 35.Hamlet WP, Lieberman JR, Freedman EL, et al. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop Belle Mead NJ. 1997;26:621–627. [PubMed] [Google Scholar]
- 36.Lefaivre KA, Macadam SA, Davidson DJ, et al. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Jt Surg Br. 2009;91-B:922–927. doi: 10.1302/0301-620X.91B7.22446. [DOI] [PubMed] [Google Scholar]
- 37.Kostuj T, Smektala R, Schulze-Raestrup U, Müller-Mai C. Einfluss des Operationszeitpunkts und -verfahrens auf Mortalität und Frühkomplikationen der Schenkelhalsfraktur: Eine Analyse von 22.566 Fällen der verpflichtenden externen Qualitätssicherung. Unfallchirurg. 2013;116:131–137. doi: 10.1007/s00113-011-2071-1. [DOI] [PubMed] [Google Scholar]
- 38.Wagner SC, Butler JS, Kaye ID, et al. Risk factors for and complications after surgical delay in elective single-level lumbar fusion. Spine. 2018;43:228–233. doi: 10.1097/BRS.0000000000002282. [DOI] [PubMed] [Google Scholar]
- 39.Wade SM, Fredericks DR, Elsenbeck MJ, et al. The incidence, risk factors, and complications associated with surgical delay in multilevel fusion for adult spinal deformity. Glob Spine J. 2020 doi: 10.1177/2192568220954395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pietrzak JRT, Maharaj Z, Erasmus M, et al. Pain and function deteriorate in patients awaiting total joint arthroplasty that has been postponed due to the COVID-19 pandemic. World J Orthop. 2021;12:152–168. doi: 10.5312/wjo.v12.i3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vogel TR, Dombrovskiy VY, Lowry SF. In-hospital delay of elective surgery for high volume procedures: the impact on infectious complications. J Am Coll Surg. 2010;211:784–790. doi: 10.1016/j.jamcollsurg.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weber M, Renkawitz T, Voellner F, et al. Revision surgery in total joint replacement is cost-intensive. Biomed Res Int. 2018;2018:1–8. doi: 10.1155/2018/8987104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Malik AT, Alexander JH, Li DD, et al. What are the costs of hip osteoarthritis in the year prior to a total hip arthroplasty? J Arthroplasty. 2020;35:313–317.e1. doi: 10.1016/j.arth.2019.09.020. [DOI] [PubMed] [Google Scholar]
- 44.Sequeira SB, Novicoff WM, McVey ED, et al. Patient perspectives on the cancellation of elective primary hip and knee arthroplasty during the COVID-19 pandemic. J Am Acad Orthop Surg. 2021;29:e1321–e1327. doi: 10.5435/JAAOS-D-20-00765. [DOI] [PubMed] [Google Scholar]
- 45.Ong CB, Cororaton AD, Westrich GH, et al. COVID-19 disruptions to elective postoperative care did not adversely affect early complications or patient reported outcomes of primary TKA. Arch Orthop Trauma Surg. 2022 doi: 10.1007/s00402-022-04422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vaidya S, Berluti D, Irving JF, et al. A COVID-19 pivot plan to resume elective surgeries at the Hartford Healthcare Connecticut Orthopaedic Institute. Cureus. 2021 doi: 10.7759/cureus.15077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iyengar KP, Jain VK, Vaish A, et al. Post COVID-19: planning strategies to resume orthopaedic surgery—challenges and considerations. J Clin Orthop Trauma. 2020;11:S291–S295. doi: 10.1016/j.jcot.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.