Abstract
Objective:
The PreventionLink of Southern Maryland is a 5-year project to eliminate barriers to participation and retention in the National Diabetes Prevention Program (DPP) lifestyle change program to prevent or delay the onset of type 2 diabetes in adults with prediabetes. This is the study to identify the obstacles to participation and retention in the DPP lifestyle change program among high burden populations and learn how CHWs have reduced the identified barriers to participation and retention for high burden populations.
Methods:
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to conduct this literature review. We have used the Scopus and PubMed, including all types of studies and peer-reviewed documents published in English between 2010 and 2020.
Results:
From 131 identified articles, 18 articles were selected for qualitative synthesis. The reviewed literature documented following as main barriers to participate in a DPP lifestyle change program: time, cost, lack of transportation, cost of transportation, commute distance, technology access, access to facilities and community programs, caregiver responsibilities, lack of health literacy and awareness, and language. CHWs can address these barriers to participation and retention, they were involved in educating and supporting roles; they worked as bridges between healthcare providers and participants and as intervention team members.
Conclusions:
Diabetes prevention program participants with social determinant risk factors who most need CHW services are unlikely to have financial resources to pay for CHW services out-of-pocket. Hence, the public and private health plans that pay for their prediabetes care should consider paying for these CHW services and there is a need to trust more to CHW and have them as a “community health teams” member.
Keywords: community health workers, volunteers, diabetes, pre-diabetes, prevention, lifestyle, literature review
Introduction
Diabetes is a major public health problem in the US, with a prevalence rate of 10.5% and over 34.2 million people with diabetes in 2018.1 Approximately 88 million Americans have prediabetes, it is predicted that as many as 1 in 5 Americans could develop diabetes by 2025,2,3 lifestyle change interventions are key components to reduce the risk of developing type 2 diabetes. The Diabetes Prevention Program (DPP) demonstrated that people engaged in a structured lifestyle change program reduced their chance of developing type 2 diabetes by 16 percentage points per year.2,4 Congress authorized the CDC to establish the National Diabetes Prevention Program (National DPP) in 2010.4-9 The program is group-based, facilitated by a trained lifestyle coach, and uses a CDC-approved curriculum. Despite evidence that a structured lifestyle intervention can delay or prevent the development of type 2 diabetes,10-12 some organizations have had difficulty enrolling sufficient numbers of participants to sustain program services long-term.13,14 Identifying the barriers and facilitators to enrollment are crucial steps to improving recruitment and retention in CDC-recognized lifestyle change programs for type 2 diabetes prevention. The present paper seeks to: (1) examine the literature to understand how barriers or facilitators influence recruitment and retention (or lack thereof) in a lifestyle change program for type 2 diabetes prevention, and (2) identify Community Health Worker (CHW) interventions that can effectively address these barriers.
Prince George’s County Health Department (PGCHD) Approach
PreventionLink of Southern Maryland is a 5-year project funded by the CDC and led by the PGCHD. One of the strategies is “to explore and test innovative ways to eliminate barriers to participation and retention in CDC-recognized lifestyle change programs for type 2 diabetes prevention among high burden populations.” PreventionLink will implement a CHW intervention to eliminate barriers to participation and retention in the National DPP lifestyle change program. CHWs use the Evidence-Based Pathways Community Coordination model15 and Accountable Health Communities (AHC) Model16 to document the patients’ assessed needs and refer them to the community resources that respond to those needs. These pathways address problems with (1) transportation, (2) health literacy, (3) financial assistance, (4) social service support, (5) medication self-management, (6) self-monitoring, and (7) access to facilities.
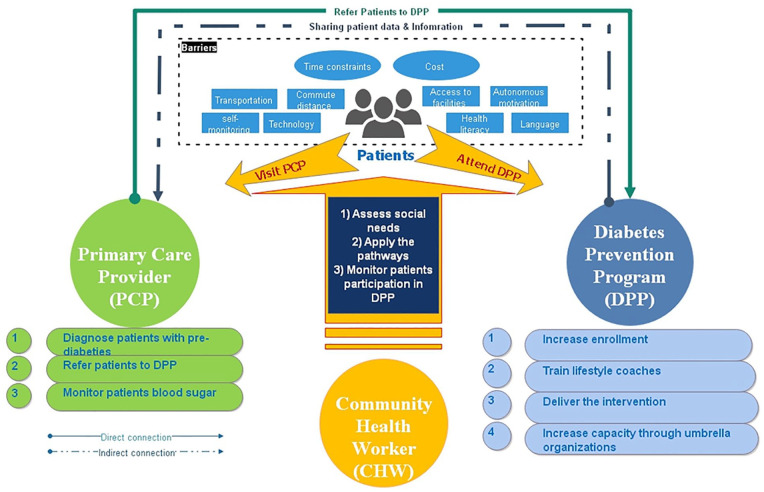
Figure 1 illustrates how the PreventionLink CHW intervention will work. Primary care providers in participating practices will refer patients with prediabetes to a CDC-recognized organization. Referred patients will be screened for unmet social needs using a screening tool adapted from the Accountable Health Communities Health-Related Social Needs Screening Tool,17 the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE),18 and the Health Literacy screener tool.19 Patients with unmet social needs20 will be referred to a CHW. The CHW will perform detailed social determinants of health assessment to determine what the patients’ needs are and then provide patients with the appropriate pathway services to address barriers to their participation in a CDC-recognized lifestyle change program for type 2 diabetes prevention and to meet Maryland’s unique Total Cost of Care Model.21
Figure 1.
The study conceptual framework.
Literature Review
Part A: Review of Barriers to Enrollment and Retention
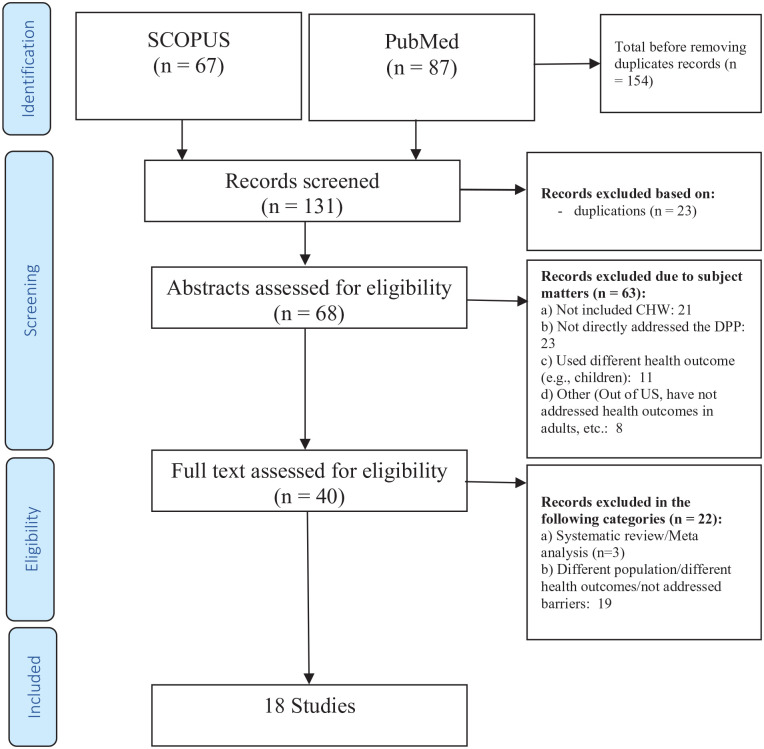
Research method: To conduct this review, we followed the steps suggested for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).21 The PRISMA Flowchart includes 4 main steps including identification, screening, eligibility, and including articles for analysis (see Figure 2). We conducted 2 literature reviews to assess the feasibility of using CHWs to effectively address the barriers to participation and retention in the National DPP lifestyle change program among high burden populations. The objective of the first review is to identify barriers to participation and retention. The second review assesses the evidence that CHWs can effectively reduce the identified barriers to participation and retention for high burden populations.
Figure 2.
PRISMA chart of the study.
Barriers and retention review criteria
The review included many types of studies (including but not limited to case-control, cross-sectional, and cohort studies), and all types of peer-reviewed documents (eg, original research articles, reviews, and reports) published in English between 2010 and 2020. The following were excluded from the review: articles published in languages other than English, articles that addressed type 2 diabetes prevention programs not utilized in the United States, non-peer-reviewed and systematic review articles, and articles focusing on interventions not related to diabetes prevention.
We conducted an electronic search using the databases Scopus and PubMed through March 28, 2020. We also conducted a citation search of selected articles to identify additional relevant studies. We obtained full-text reviews for studies that were initially selected and assessed whether the article met the eligibility criteria listed above. Our findings are discussed in the next section.
Effectiveness of CHWs review criteria
Using the inclusion and exclusion criteria described above, we conducted another search including “CHW” OR “Community Health Workers.” We identified 154 articles from the initial electronic search and 4 articles from the manual citation search. We excluded 114 articles by screening the titles and abstracts using the study eligibility criteria. After removing duplicates, 40 articles were selected for full-text review of eligibility. Finally, we selected 18 articles with the most relevant studies regarding CHW roles in addressing barriers for patients in diabetes prevention programs.
Results
Barriers reported in similar studies
Multiple barriers to participation and retention in diabetes prevention programs were identified in the thirteen (13) articles (see Table 1) that were reviewed, as follows:
Table 1.
Reported Barriers to Diabetes Prevention Program Participant Enrollment and Retention Based on the Reviewed Publications: 2010 to 2020.
| Article | Barriers identified |
|---|---|
| Albright and Gregg,2 Gary-Webb et al,22 Griauzde et al,23 and Venditti et al24 | Time |
| Gary-Webb et al,22 Griauzde et al,23 Reddy et al,25 and Thomas et al26 | Cost |
| Gary-Webb et al,22 Dyer et al,27 and Jiang et al28 | Transportation and cost of transportation |
| Reddy et al25 and Dyer et al27 | Commute distance |
| Reddy et al25 | Self-monitoring |
| Griauzde et al,23 Dyer et al,27 and Bian et al29 | Technology access |
| Albright and Gregg,2 Reddy et al,25 and Thomas et al26 | Access to facilities and community programs |
| Griauzde et al,23 Venditti et al,24 and Thomas et al26 | Autonomous motivation |
| Thomas et al26 and Jiang et al28 | Caregiver responsibilities |
| Albright and Gregg2 | Health literacy and awareness |
| Nhim et al30 | Language |
Source: Study findings based on literature review (2010-March 2020).
Time constraints: The time constraints of potential program participants were identified as a common barrier in multiple research articles.22,25 Setting aside time to attend the 16 weekly sessions was a barrier for some participants, particularly those with low socioeconomic status.2 Time constraints were also a barrier when program sessions were extended beyond the scheduled time frame.22 Among diabetes prevention programs that utilized technology to engage participants, lengthy and time-consuming apps resulted in loss of interest and participant disengagement.23 Last, participants’ time management and planning was identified as a barrier to program adherence and participation.24
Cost: The out-of-pocket costs participants incur for various program components, for example, recreational center fees so that they can engage in exercise, are a barrier to participant engagement and retention.22,23 The cost barrier was even more significant for uninsured individuals who were unable to pay the entire program cost out-of-pocket.26 To lessen these financial burdens, some programs have offered scholarships for participants who commit to complete a minimum of 75% of the sessions.25
Transportation: Lack of transportation and transportation costs to attend weekly program sessions emerged as a barrier in multiple studies.22,27 Although in some studies, short-term retention was not affected by transportation, long-time retention was difficult to achieve and resulted in participant attrition.28 Some program delivery organizations have addressed the transportation barrier by giving participants limited value transit passes22; however, this approach is of limited utility in rural areas that generally lack public transportation options.
Commuting time: In multiple studies, the time involved in traveling to facilities to attend in-person sessions was identified as a barrier by participants commuting from rural areas in multiple studies.25,27 To address this barrier, participation outside of the class through small groups was encouraged.27 Alternative options included programs delivered online or through distance learning where participants could attend without needing to travel.27,31
Self-monitoring: Self-monitoring of food intake is well-established as a crucial behavioral change strategy for weight loss. Lower household income and low educational attainment were significantly associated with less frequent dietary self-monitoring among diabetes prevention program participants.24
Technology access: Some organizations have used technology to increase participants’ access to the program via online service delivery with the premise that this mode of service delivery may allow a larger number of persons to participate, may increase geographic access to this service, and may reduce the per participant cost, and thus improve the cost effectiveness of the intervention.32 However, despite the finding that online programs have proven to be as effective as in-person models, some participants were challenged by the online technology.29 Limited computer literacy or access, especially among older populations, has been a cause for online participant dissatisfaction.27,31 In addition, participants lacking internet access or smart devices are unable to participate meaningfully in online programs.23 Additionally, some older participants prefer to have in-person services.33 Furthermore, for an online program to operate efficiently, it needs the full-time support of professional online coaches; not all programs have such resources.32
Accessibility of digital technology allows users to initiate interventions effortlessly but also allows users to disengage easily, so online programs need to define elements that make their programs successful.34,35
Access to facilities and community programs: Access to community-based exercise facilities are another identified barrier.2 Multiple program participants experienced challenges accessing the necessary space and equipment to engage in exercise.25 Lack of support from community programs and exercise facilities such as fitness centers may negatively impact participant retention.26
Lack of motivation: Participants who lacked motivation to change their lifestyle tended to either not enroll or to not complete the program.24 Conversely, participants who were highly motivated to make the necessary changes tended to remain engaged and complete the program.23
Caregiver responsibilities: Participants who were caregivers reported that caregiving responsibilities negatively impacted their ability to enroll and remain in a diabetes prevention program.26 Although, in some studies, short-term retention was not affected by care-giving responsibilities, long-term retention was difficult to achieve.28
Health literacy: Among individuals with multiple type 2 diabetes risk factors, studies have found that an overall lack of awareness may further increase risk. For these patients, brief education or consulting about how they can influence their risk may help to reduce progression to higher levels of risk.2
Language: Language difficulties have been identified as barriers to diabetes prevention program enrollment and retention among vulnerable and disadvantaged groups.30 While the information is conveyed to participants, there are barriers to a successful delivery. Some online programs are available only in English, thus limiting access to non-English speakers.36 To address the language barrier, some organizations have opted to use native speaker facilitators with experience in community outreach to deliver the program.22
Part B: The Role of CHWs in Facilitating Retention in Diabetes Prevention Programs
As summarized in Table 2, CHWs have been involved in diabetes prevention programs to support patients. Among the selected articles and referenced citations reviewed, the main roles and responsibilities of CHWs are summarized in 3 main categories: (1) educating and supporting roles of CHWs, (2) CHWs as bridges between healthcare providers and participant, and (3) CHWs roles as intervention team members.
Table 2.
CHW Roles in Addressing Diabetes Prevention Program Recruitment and Retention Barriers.
| Article | Barriers | CHW role/intervention to address the barriers |
|---|---|---|
| Ruggiero et al37 | Time | Providing participants with the option to meet in small CHW-facilitated groups with flexible scheduling |
| Katula et al,38 Lawlor et al,39 and Perez et al40 | Cost | Reducing direct cost of the program; for example, in some CHW models, the direct cost has been as low as one-third of the original DPP intervention ($850 vs $2631). |
| It may be due to using more-costly medical professionals to deliver lifestyle intervention or delivering group-based services in comparison with individual-based service. | ||
| Wagner et al41 | Lack of transportation | Providing transportation |
| Lorig et al,42 Van der Wees et al,43 and Islam et al44 | Self-monitoring | - Providing self-monitoring training. |
| - Lifestyle strategies for glycemic control including physical activity, prevention of diabetes complications, healthy food, and diabetes care. | ||
| - Glucose self-monitoring training | ||
| Kim et al45 | Autonomous motivation | Motivational counseling |
| Kim et al45 | Health literacy | Using a literacy-enhancing approach that addresses the strong need to enhance essential health literacy skills |
| Wagner et al,41 Islam et al,44 and Kim et al45 | Language | A CHW who speaks the native language, helps a non-English speaker to understand their culture and to overcome language barriers for them. |
Source: Study findings based on Literature Review (2010-March 2020).
Educating and supporting roles of CHWs
CHWs are engaged in patient care and support, outreach, and patient education.46 They play a major role in training and counseling participants.8,42,47 They mitigate the barrier of time constraints by facilitating small groups of participants who met on a flexible schedule.27,46 They also provide practical support, such as offering transportation to diabetes prevention program sessions, so that participants are able to attend to the program to reach program goals.41 Additionally, they maintain regular contact with participants and provide them with ongoing support and information.48 In one program, the CHWs employed a computer-based mapping system to locate healthcare resources for patients.43 In another program, the CHWs engaged participants in teach-backs, role playing, and group discussions designed to improve the participants’ health literacy.45 Therefore, CHWs play a role in educating and counseling participants.8,47
CHWs assist non-native English-speaking participants to understand their culture and to overcome language barriers for them.41,44,45 In addition, evidence has shown that CHWs have great potential to reduce costs and increase accessibility to lifestyle behavioral change interventions and provide a cost-effective alternative to professional healthcare providers.38,47 In the Healthy Living Partnerships to Prevent Diabetes (HELP PD), CHWs delivered a cost-effective intervention by reducing direct medical and non-medical program costs.39 Huang et al49 used an incremental cost effectiveness ratio method, and concluded that CHW intervention was highly cost-effective.
CHWs as bridges between healthcare providers and participants
CHWs play other supportive roles in diabetes prevention programs, including serving as liaisons between participants and their medical providers and following up with participants to ensure they adhere to their care plan including accessing needed services,50 and providing instrumental support to healthcare professionals in the delivery of care and educational programs.37 They can assist participants with low health literacy by clarifying healthcare providers’ instructions so that participants are able to follow the instructions.51
CHWs roles as intervention team members
CHWs participate in data collection such as recording of family attendance in program activities.52 As a team member, CHWs improve participants knowledge and behavior regarding diabetes53 self-care practice and glucose self-monitoring, diet, and physical activities.46
Discussion and Conclusion
PreventionLink offers a viable approach to address barriers to enrollment and retention in diabetes prevention programs. Evidence shows that CHWs can help program participants overcome most of the barriers to enrollment and retention. Although technology challenges and caregiving responsibilities were identified as barriers to participant retention, no studies presented ways in which CHWs can help mitigate these barriers. Nonetheless, it is quite plausible for CHWs to facilitate participants’ access to online diabetes prevention programs by training them on how to use the technology. CHWs can also help program participants obtain child care,54 adult daycare, and home health aide services. They have been shown to be an effective bridge between providers and community-based services.50,55 CHWs can serve as agents for program participants, helping to make the most of their interactions with their primary care providers and their diabetes prevention programs.
A major challenge for providing any support services is how to sustain the services financially. The second is AccessHealth, which employs CHWs to provide several services. PGCHD contracts with PGHA and AccessHealth to provide these services as a part of PreventionLink. However, the ability to bill for CHW services is crucial to sustain this needed support. Diabetes prevention program participants with social determinant risk factors who most need CHW services are unlikely to have financial resources to pay for CHW services out-of-pocket. Hence, the public and private health plans that pay for their prediabetes care should consider paying for these CHW services.
Under the Medicare Diabetes Prevention Program (MDPP) Expanded Model, CMS reimburses MDPP suppliers for enrolled Medicare beneficiaries, based on a pay-for-performance model linked to attendance and weight loss goals in New Mexico.56 Creating a sustainable statewide model for CHW’s reimbursement needs more collaboration from local and statewide policymakers to defining type and qualifications for reimbursement, and sustainable funding and mechanisms to reimburse CHWs.57,58 States may develop policies and programs to “adopt a statewide CHW training curriculum” and “develop statewide certification/licensing process for CHWs”56 to facilitate a sustainable statewide model or shifting value-based reimbursement models similar to other health professionals.59
The Centers for Medicare and Medicaid Services (CMS) reimbursement for CHW services is not unprecedented. CMS currently pays for CHW services under the Medicaid program. CMS allows states to pay for preventative care services recommended by a physician provided by a CHW, including coordinating care, addressing health literacy, supporting home-based self-management, and providing health education and promotion services. Typically, these services are offered to dually eligible beneficiaries who are high utilizers and children with special healthcare needs, such as those with asthma. PreventionLink is evaluating this strategy of using CHWs to address the barriers to participation and retention in diabetes prevention programs. If it proves to cost effective, then CMS should consider adding payment for CHW services to the MDDP Expanded Model. CHWs have great potential to save more money by providing cost-effective services38,47 to patients and communities. Their awareness of the community needs and their similarity with participants in culture and language make them powerful agents for promoting community health, this is a great investment with a significant return.60 However, there is a general understanding lack of full capacity of CHWs in promoting the health of the communities. It is a 2-sided barrier at health system and professional providers and CHW (by themselves). There is a need to “trust” more in CHW-capacity at the health system and professional provider by helping CHWs to build their collaboration and integration58 it is also crucial for CHWs to develop their strengths to join the “community health teams” and work as a “crucial connection between the team and the community; they can also play a vital role in building community capacity and promoting patient empowerment.”61
Acknowledgments
The research was supported through cooperative agreement NU58DP006626-01-00 (Prince George’s County Health Department) from the U.S. Department of Health and Human Services (DHHS, Centers for Disease Control and Prevention). Dr. Ernest L. Carter, MD, PhD, the Health Officer, Prince George’s County, Maryland is the Principal Investigator. Lori Werrell, MPH, MCHES is the Co-Principal Investigator. Rigorous evaluation will be conducted by a team headed by Darrell J. Gaskin, PhD, the William C. and Nancy F. Richardson Professor in Health Policy and Director of the Center for Health Disparities Solutions, Johns Hopkins Bloomberg School of Public Health. The Hopkins team, consisting of Darrell J. Gaskin, PhD; Hossein Zare, PhD; Roland J. Thorpe, Jr., PhD; Michelle Spencer, MS; and Laurine Thomas, PhD, an independent health services research consultant with expertise in qualitative methods. The PGHCD Evaluation team consists of Donna Perkins, MPH and Christina Gray, MS.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research was supported through grants #:1 NU58DP006626-01-00 (Prince George’s County Health Department) from the U.S. Department of Health and Human Services (DHHS, Centers for Disease Control and Prevention). Dr. Ernest Carter, MD, PhD, the Acting Health Officer, Prince George’s County, Maryland is the Principal Investigator.
ORCID iD: Hossein Zare  https://orcid.org/0000-0002-5832-0854
https://orcid.org/0000-0002-5832-0854
References
- 1. CDC. National diabetes statistics report 2020: estimates of diabetes and its burden in the United States. 2020. Accessed August 28, 2022. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- 2. Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med. 2013;44:S346-S351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lin J, Thompson TJ, Cheng YJ, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr. 2018;16(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015;3(11):866-875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cannon MJ, Masalovich S, Ng BP, et al. Retention among participants in the National Diabetes Prevention Program lifestyle change program, 2012–2017. Diabetes Care. 2020;43(9):2042-2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gruss SM, Nhim K, Gregg E, Bell M, Luman E, Albright A. Public health approaches to type 2 diabetes prevention: the US National Diabetes Prevention Program and beyond. Curr Diab Rep. 2019;19(9):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the diabetes prevention program into the community: the DEPLOY pilot study. Am J Prev Med. 2008;35(4):357-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP) description of lifestyle intervention. Diabetes Care. 2002;25(12):2165-2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ely EK, Gruss SM, Luman ET, et al. A national effort to prevent type 2 diabetes: participant-level evaluation of CDC’s National Diabetes Prevention Program. Diabetes Care. 2017;40(10):1331-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med. 2015;163(6):437-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Task Force. Diabetes prevention and control: combined diet and physical activity promotion programs to prevent type 2 diabetes among people at increased risk: task force finding and rationale statement. 2015. Accessed August 28, 2022. https://www.thecommunityguide.org/sites/default/files/assets/Diabetes-Diet-and-PA_1.pdf
- 13. DiBenedetto JC, Blum NM, O’Brian CA, Kolb LE, Lipman RD. Achievement of weight loss and other requirements of the diabetes prevention and recognition program: a National Diabetes Prevention Program network based on nationally certified diabetes. Diabetes Educ. 2016;42(6):678-685. [DOI] [PubMed] [Google Scholar]
- 14. Zigmont VA, Shoben AB, Kaye GL, et al. An evaluation of reach for a work site implementation of the National Diabetes Prevention Program focusing on diet and exercise. Am J Health Promot. 2018;32(6):1417-1424. [DOI] [PubMed] [Google Scholar]
- 15. Redding S, Conrey E, Porter K, Paulson J, Hughes K, Redding M. Pathways community care coordination in low birth weight prevention. Matern Child Health J. 2015;19(3):643-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. CMS. Accountable health communities model. The U.S. Centers for Medicare & Medicaid Services. 2020. Updated 4 September 2020. Accessed August 28, 2022. https://innovation.cms.gov/innovation-models/ahcm
- 17. CMS. Centers for Medicare & Medicaid Services. The accountable health communities health-related social needs screening tool. 2017. Accessed August 28, 2022. https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf
- 18. NACHC. PRAPARE: Protocol for Responding to and Assessing Patient Assets, Risks, and Experiences. National Association of Community Health Centers, Inc., Association of Asian Pacific Community Health Organizations, and Oregon Primary Care Association; 2016. Accessed August 28, 2022. https://prapare.org/prapare-toolkit
- 19. Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. MDH. Maryland Department of Health. Health enterprise zones (HEZs). 2020. Accessed August 28, 2022. https://health.maryland.gov/healthenterprisezones/Pages/home.aspx
- 21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-269. [DOI] [PubMed] [Google Scholar]
- 22. Gary-Webb TL, Walker EA, Realmuto L, et al. Translation of the National Diabetes Prevention Program to engage men in disadvantaged neighborhoods in New York City: a description of power up for health. Am J Mens Health. 2018;12(4):998-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Griauzde D, Kullgren JT, Liestenfeltz B, et al. A mobile phone-based program to promote healthy behaviors among adults with prediabetes who declined participation in free diabetes prevention programs: mixed-methods pilot randomized controlled trial. JMIR mHealth and uHealth. 2019;7:e11267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Venditti EM, Wylie-Rosett J, Delahanty LM, Mele L, Hoskin MA, Edelstein SL. Short and long-term lifestyle coaching approaches used to address diverse participant barriers to weight loss and physical activity adherence. Int J Behav Nutr Phys Act. 2014;11(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Reddy P, Hernan AL, Vanderwood KK, et al. Implementation of diabetes prevention programs in rural areas: Montana and south-eastern Australia compared. Aust J Rural Health. 2011;19(3):125-134. [DOI] [PubMed] [Google Scholar]
- 26. Thomas T, Samuel-Hodge CD, Porterfield DS, Alva ML, Leeman J. Scaling up diabetes prevention programs in North Carolina: perceptions of demand from potential program recipients and providers. Diabetes Educ. 2019;45(1):116-124. [DOI] [PubMed] [Google Scholar]
- 27. Dyer KE, Moreau JL, Finley E, et al. Tailoring an evidence-based lifestyle intervention to meet the needs of women veterans with prediabetes. Women Health. 2020;60:748-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jiang L, Manson SM, Dill EJ, et al. Participant and site characteristics related to participant retention in a diabetes prevention translational project. Prev Sci. 2015;16(1):41-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bian RR, Piatt GA, Sen A, et al. The effect of technology-mediated diabetes prevention interventions on weight: a meta-analysis. J Med Internet Res. 2017;19:e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nhim K, Gruss SM, Porterfield DS, et al. Using a RE-AIM framework to identify promising practices in National Diabetes Prevention Program implementation. Implement Sci. 2019;14(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moin T, Ertl K, Schneider J, et al. Women veterans’ experience with a web-based diabetes prevention program: a qualitative study to inform future practice. J Med Internet Res. 2015;17(5):e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sepah SC, Jiang L, Peters AL. Translating the diabetes prevention program into an online social network: validation against CDC standards. Diabetes Educ. 2014;40(4):435-443. [DOI] [PubMed] [Google Scholar]
- 33. Rutledge T, Skoyen JA, Wiese JA, Ober KM, Woods GN. A comparison of MOVE! versus TeleMOVE programs for weight loss in veterans with obesity. Obes Res Clin Pract. 2017;11(3):344-351. [DOI] [PubMed] [Google Scholar]
- 34. Grock S, Ku JH, Kim J, Moin T. A review of technology-assisted interventions for diabetes prevention. Curr Diab Rep. 2017;17(11):107. [DOI] [PubMed] [Google Scholar]
- 35. McLean V. Motivating patients to use smartphone health apps. PR Web. 2011;113. [Google Scholar]
- 36. Coughlin SS, Hardy D, Caplan LS. The need for culturally-tailored smartphone applications for weight control. J Ga Public Health Assoc. 2016;5(3):228-232. [PMC free article] [PubMed] [Google Scholar]
- 37. Ruggiero L, Oros S, Choi YK. Community-based translation of the diabetes prevention program’s lifestyle intervention in an underserved Latino population. Diabetes Educ. 2011;37(4):564-572. [DOI] [PubMed] [Google Scholar]
- 38. Katula JA, Kirk JK, Pedley CF, et al. The lifestyle intervention for the treatment of Diabetes study (LIFT Diabetes): design and baseline characteristics for a randomized translational trial to improve control of cardiovascular disease risk factors. Contemp Clin Trials. 2017;53:89-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lawlor MS, Blackwell CS, Isom SP, et al. Cost of a group translation of the diabetes prevention program: healthy living partnerships to prevent diabetes. Am J Prev Med. 2013;44(4):S381-S389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Perez A, Alos VA, Scanlan A, et al. The rationale, design, and baseline characteristics of PREVENT-DM: a community-based comparative effectiveness trial of lifestyle intervention and metformin among Latinas with prediabetes. Contemp Clin Trials. 2015;45:320-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wagner J, Bermudez-Millan A, Damio G, et al. Community health workers assisting Latinos manage stress and diabetes (CALMS-D): rationale, intervention design, implementation, and process outcomes. Transl Behav Med. 2015;5(4):415-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35(4):641-651. [DOI] [PubMed] [Google Scholar]
- 43. Van der Wees PJ, Friedberg MW, Guzman EA, Ayanian JZ, Rodriguez HP. Comparing the implementation of team approaches for improving diabetes care in community health centers. BMC Health Serv Res. 2014;14(1):608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Islam NS, Zanowiak JM, Wyatt LC, et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health. 2013;38(6):1030-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kim MT, Kim KB, Huh B, et al. The effect of a community-based self-help intervention: Korean Americans with type 2 diabetes. Am J Prev Med. 2015;49(5):726-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ruggiero L, Castillo A, Quinn L, Hochwert M. Translation of the diabetes prevention program’s lifestyle intervention: role of community health workers. Curr Diab Rep. 2012;12(2):127-137. [DOI] [PubMed] [Google Scholar]
- 47. Katula JA, Vitolins MZ, Rosenberger EL, et al. One-year results of a community-based translation of the Diabetes Prevention Program: Healthy-Living Partnerships to Prevent Diabetes (HELP PD) Project. Diabetes Care. 2011;34(7):1451-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wilson MG, DeJoy DM, Vandenberg R, Padilla H, Davis M. Fuel your life: a translation of the diabetes prevention program to worksites. Am J Health Promot. 2016;30(3):188-197. [DOI] [PubMed] [Google Scholar]
- 49. Huang SJ, Galárraga O, Smith KA, Fuimaono S, McGarvey ST. Cost-effectiveness analysis of a cluster-randomized, culturally tailored, community health worker home-visiting diabetes intervention versus standard care in American Samoa. Hum Resour Health. 2019;17(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Whittemore R, Rosenberg A, Gilmore L, Withey M, Breault A. Implementation of a diabetes prevention program in public housing communities. Public Health Nurs. 2014;31(4):317-326. [DOI] [PubMed] [Google Scholar]
- 51. Gerber BS, Cano AI, Caceres ML, et al. A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. Ann Pharmacother. 2010;44(1):70-79. [DOI] [PubMed] [Google Scholar]
- 52. Reinschmidt KM, Teufel-Shone NI, Bradford G, et al. Taking a broad approach to public health program adaptation: adapting a family-based diabetes education program. J Prim Prev. 2010;31(1-2):69-83. [DOI] [PubMed] [Google Scholar]
- 53. Castillo A, Giachello A, Bates R, et al. Community-based diabetes education for Latinos: the Diabetes Empowerment Education Program. Diabetes Educ. 2010;36(4):586-594. [DOI] [PubMed] [Google Scholar]
- 54. Costich MA, Peretz PJ, Davis JA, Stockwell MS, Matiz LA. Impact of a community health worker program to support caregivers of children with special health care needs and address social determinants of health. Clin Pediatr. 2019;58(11-12):1315-1320. [DOI] [PubMed] [Google Scholar]
- 55. Islam N, Gepts T, Lief I, et al. Protocol for the CHORD project (community health outreach to reduce diabetes): a cluster-randomized community health worker trial to prevent diabetes. BMC Public Health. 2018;18(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rodriguez B. The role of Community Health Workers (CHWs) in Diabetes Prevention and Control: lessons learned from states and cities. American Association of Diabetes Educators. AADE18, Passion into action. 2018. Accessed August 28, 2022. https://www.diabeteseducator.org/docs/default-source/annual-meetings/AADE18/presentation-slides/m07.pdf?sfvrsn=0
- 57. Alvisurez J, Clopper B, Felix C, Gibson C, Harpe J. Funding community health workers: best practices and the way forward. 2013. Accessed August 28, 2022. http://www.healthreform.ct.gov/ohri/lib/ohri/sim/care_delivery_work_group/funding_chw_best_practices.pdf
- 58. Alvisurez J, Clopper B, Felix C, et al. Funding community health workers: best practices and the way forward. 2013. [Google Scholar]
- 59. Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93(7):1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mehra R, Boyd LM, Lewis JB, Cunningham SD. Considerations for building sustainable community health worker programs to improve maternal health. J Prim Care Community Health. 2020;11:2150132720953673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Balcazar H, Rosenthal EL, Brownstein JN, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for change in the United States: three actions for a new paradigm. Am J Public Health. 2011;101(12):2199-2203. [DOI] [PMC free article] [PubMed] [Google Scholar]