Abstract
Introduction:
Perceived Stress Scale (PSS), developed in 1983, is one among the widely used global scales to assess the perceived psychological stress status. Hence, our study aimed at developing a Tamil version of THE 10-item PSS (TPSS-10) and assess its construct validity and internal consistency among patients with diabetes in Puducherry, South India.
Methods:
We translated the TPSS-10 by language experts and pilot-tested the sample with a subsample of diabetes patients. The finalized version of TPSS-10 was administered to 117 Tamil-speaking diabetic patients availing services from the rural health center in Puducherry, South India. Construct validity was assessed using the exploratory factor analysis (EFA) and the principal component analysis (PCA). A confirmatory factor analysis (CFA) was also done to obtain the goodness-of-fit. Reliability of questionnaire was evaluated by Cronbach’s alpha.
Results:
Two factors were obtained with Eigenvalues of 4.61 and 2.16. Both factors explained 67.8% of the total variance. The two-factor model assessed by CFA found a χ2 value of 714.99 (P < 0.001). Goodness-of-fit revealed acceptable comparative fit indices (0.93). The reliability coefficient (Cronbach’s alpha) for complete TPSS-10 was 0.86, indicating good internal consistency.
Discussion:
Our study concludes that the TPSS-10 questionnaire is internally valid and consistent with good reliability coefficient after its administration to Tamil-speaking urban diabetic patients in order to measure perceived stress. However, further research is warranted to content-validate the tool with a standard diagnostic instrument.
Keywords: Diabetes, Perceived Stress Scale, stress, validation studies
Introduction
Cardiovascular diseases (CVDs) and diabetes account for the majority of non-communicable deaths worldwide.[1] Diabetes mellitus (DM) alone affects about one in ten adults globally, and almost four-fifth of people with DM hail from low- and middle-income countries (“LMIC”).[2,3] It is estimated that the global prevalence of DM in 2015 will be around 415 million as reported by the International Diabetes Federation (IDF), and it is speculated that it might even reach 642 million by 2040.[4] India has the second-highest burden of DM cases in the world (5%-17%), next to China, with higher prevalence observed among the Southern states.[4,5,6] DM, a disease characterized by changes in blood sugar levels, is often associated with deviations in mood, anxiety, feeling fatigued, problems in decision-making, and other unrecognized mental health disorders.[7,8] The IDF has also highlighted the need for an integrated approach that adds psychological care to DM management.[9] DM patients’ coexisting challenges such as depression, anxiety, and stress are often associated with poor diabetes outcomes.[10,11] Worldwide estimates on the prevalence of stress among diabetic patients vary widely by location, for example, studies from Asia, including India, report wide-ranging prevalence of stress among diabetics, from 20% to 60%.[12,13,14] Stress and anxiety among the diabetic population is a growing concern globally, which could hamper their quality of living and medication adherence.
Various scales are in place to quantify stress levels. The Perceived Stress Scale (PSS) is one of the widely utilized stress scales developed by Cohen et al.[15] in 1983 to quantify the level of perceived stress. PSS is particularly useful to evaluate the effect of interventions to decrease stress, and it is also used as a reference tool for examining the validity of new measures of stress.[16]
Most studies to validate PSS, however, were carried out in adult populations who were generally depressed and who were planning to quit tobacco, for example. Very few attempts have been made to validate PSS among individuals with diabetes, and little data on stress levels among these specific people groups have been reported. PSS has earlier been translated into many languages, like Japanese,[17] Swedish,[18] French,[19] Arabic,[20] and Chinese,[21] to generate population-specific data and study cross-cultural variations. We observed a lacuna in the validation of PSS in local languages of India, especially Tamil, focusing on DM patients. Hence, our study aimed at developing a Tamil version of the 10-item PSS (TPSS-10), focusing on assessment of the psychometric properties, such as construct validity and internal consistency, among patients with DM in Puducherry, South India.
Methods
Participants
To conduct this validation study, we recruited DM patients availing treatment from the non-communicable disease (NCD) clinic of the selected urban health center in Puducherry, Southern India. The center provides services to 10,000 people living in four urban wards, namely, Kurusukuppam, Chinnayapuram, Vazhaikulam, and Vaithikuppam.[22] The center holds weekly special clinics for NCD, antenatal, under-five, and adolescent care. There were 150–200 DM patients availing their monthly medications from the center. A sample of 117 diabetic patients was enrolled for the study through consecutive sampling technique. We excluded patients who failed to attend the clinic on two consecutive occasions. The study recruitment was done for a period of 3 months between December 2017 and February 2018. Reviewed by the department review committee on 03rd January 2018.
Study tool
Cohen’s PSS is widely used to assess the perceived psychological stress status. It is a self-reporting scale used to measure the level and intensity of perceived stress, and it is used to find out the stressful situations in the daily life. Items included in the scale intended to apprehend how overloaded, uncontainable, and unpredictable participants perceived their lives. This is a 10-item scale that includes questions regarding positive and negative aspects of stress. Scoring was done based on a 5-point Likert-type scale ranging from 0 to 4. Scores were valued as follows: 4 = never, 3 = rarely, 2 = sometimes, 1 = often, and 0 = always. It should be noted that the questions 4, 5, 7, and 8 have to be positively calculated. Based on the overall score, stress levels were further classified as follows: “low” (score 0–11), “average” (score 12–15), “high” (score “16–20”), and “very high” (score ≥21).
Translation
We adopted this PSS questionnaire, and translation process was as done as in other studies.[17,18,19] We adopted a two-step process where the English version was translated into Tamil by two independent language experts (who were native Tamil speakers with English skills). They had no prior knowledge regarding the purpose, content, or interpretation of the questionnaire. The English and Tamil versions were paralleled for any discrepancy of information. Later, it was translated back to English to check the content, and the final draft was obtained. This was further verified by an expert in the local language, and the final version was constructed after rectifying the language and grammatical errors. TPSS-10 also has 10 items as does the original 10-item English version of PSS, of which 4 items are positively worded (e.g., how often have you felt that things were going your way?) and the rest six are negatively worded (e.g., how often have you been upset because of something that happened unexpectedly?). The final Tamil version was then piloted with a subsample of diabetic individuals (n = 15) for assessing the difficulty in comprehending the questions. Finally, the questionnaire was again modified based on the feedback.
Data collection
Three trained doctors who are confident and familiar with the language were assigned as data collectors after sensitization regarding the study objectives. The patients were enrolled after informed consent, and confidentiality of the information was assured. Data collection was done using a semi-structured questionnaire that was administered during the patients’ monthly clinic visits. The questionnaire had two sections: sociodemographic characteristics like age, gender, education, occupation, and duration of diabetes, and the Tamil version of the PSS.
Ethical approval
The study was done as a component of NCD care services delivered in the urban health center toward chronic disease clinics. Any query arising from the participants were clarified after obtaining written consent. The study was reviewed and approved by the department review committee.
Statistical analysis
Data were entered into Epidata, version 3.01 (EpiData Association, Odense, Denmark) and analyzed using Stata version 14.2 (StataCorp, College Station, TX, USA). Continuous variables were summarized depending on their distribution as mean (±SD) or median (IQR). Categorical variables were summarized as proportions. Bartlett’s test of sphericity was used for checking the intercorrelation between the PSS items, and Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was utilized to check the sample adequacy and suitability for factor analysis. Once the adequacy was achieved, we further employed exploratory factor analysis (EFA) using principal component analysis (PCA) with varimax rotation to obtain the list of factors along with their factor loadings. Factors having an Eigen value of more than 1 were taken as factor models. Factor loadings with values >0.4 were taken for the characterization of the factor model.[20,21] To test the results of EFA, we ran a confirmatory factor analysis (CFA) and determined the goodness-of-fit for the existing factor models using the χ2 statistic. Indices such as root mean square error of approximation (RMSEA), comparative fit indices (CFIs), standardized root mean square residual (SRMR), and Tucker–Lewis’s index (TLI) were considered for the evaluation and comparison of descriptive goodness-of-fit. We took an acceptable cut-off of CFI ≥0.90, TFI ≥0.90, SRMR ≤0.10, and the RMSEA ≤0.08 for evaluating the fit indices.[23] We also determined the Cronbach’s alpha coefficient for determining the internal consistency of TPSS-10.
Results
Sociodemographic characteristics
A total of 117 patients with DM consented to participate in the study. The mean (±SD) age of the study participants was found to be 57.1 (±10.9) years. Table 1 explains the sociodemographic characteristics of the participants. Briefly, the majority of participants were females (72.6%), almost half of them belonged to the 46–60 years age group, more than three-fourth had a family income of less than 10,000, about 80.4% were employed during the time of interview, and 39.3% had diabetes for more than 5 years [Table 1].
Table 1.
Sociodemographic characteristics of the study participants (n=117)
| Characteristics | Frequency (%) |
|---|---|
| Gender | |
| Female | 85 (72.6) |
| Male | 32 (27.4) |
| Age category (in years) | |
| ≤45 | 7 (11.1) |
| 46-60 | 66 (51.3) |
| >61 | 44 (37.6) |
| Total family income (Indian Rupees - INR) | |
| ≤10,000 | 103 (88.0) |
| >10,000 | 14 (12.0) |
| Duration of diabetes (in years) | |
| ≤5 | 71 (60.7) |
| >5 | 46 (39.3) |
| Employment status | |
| Unemployed | 94 (80.4) |
| Employed | 23 (19.6) |
| Presence of hypertension | |
| Yes | 81 (69.3) |
| No | 36 (30.7) |
Psychometric properties
Construct validity
Before conducting EFA, Bartlett’s test was used to evaluate the intercorrelation level of the items, which showed high significance (χ2 = 683.420, P < 0.001) and a KMO value of 0.836, proving very good intercorrelation between the items of TPSS-10 thereby fulfilling the prerequisites for performing EFA.
Table 2 shows the pattern of EFA conducted using a PCA method. Two factors (factors 1 and 2) had an eigenvalue of 4.61 and 2.16 (more than 1) and thus were retained. Factor 1 had 6 items explaining 43.05% of variance, whereas factor 2 with the remaining 4 items explained 24.75% of variance, thus making the two-factor model to explain 67.8% of the variance. We did not observe any double loadings in the pattern matrix, with all item loadings having values of more than 0.5.
Table 2.
Results from exploratory factor analysis (EFA) using principal component analysis (PCA) with varimax rotation on the Tamil version of the 10-item Perceived Stress Scale (TPSS-10; n=117)
| Factor 1 | Factor 2 | |
|---|---|---|
| The 10 items of TPSS-10 | ||
| Item 1: In the last month, how often have you been upset because of something that happened unexpectedly? | 0.8707 | -0.0485 |
| Item 2: In the last month, how often have you felt that you were unable to control the important things in your life? | 0.8980 | -0.1096 |
| Item 3: In the last month, how often have you felt nervous and “stressed”? | 0.8880 | -0.0106 |
| Item 4: In the last month, how often have you felt confident about your ability to handle your personal problems? | -0.0512 | 0.8700 |
| Item 5: In the last month, how often have you felt that things were going your way? | -0.0458 | 0.7939 |
| Item 6: In the last month, how often have you found that you could not cope with all the things that you had to do? | 0.8054 | -0.1434 |
| Item 7: In the last month, how often have you been able to control irritations in your life? | -0.1514 | 0.6435 |
| Item 8: In the last month, how often have you felt that you were on top of things? | -0.1909 | 0.7726 |
| Item 9: In the last month, how often have you been angered because of things that were outside of your control? | 0.7748 | -0.1449 |
| Item 10: In the last month, how often have you felt difficulties were piling up so high that you could not overcome them? | 0.7992 | -0.1464 |
| Eigenvalue | 4.61 | 2.16 |
| Percentage of variance explained | 43.05% | 24.75% |
| Cronbach’s alpha | 0.86 | |
| Interfactor Pearson correlation (two-tailed significance value) | <0.001 | |
Factor 1 consisted of item 1, item 2, item 3, item 6, item 9, and item 10, having negatively worded questions, whereas factor 2 consisted of item 4, item 5, item 7, and item 8 which were positively worded questions. The observed correlation between factor 1 and factor 2 was 0.69 with a P value < 0.001.
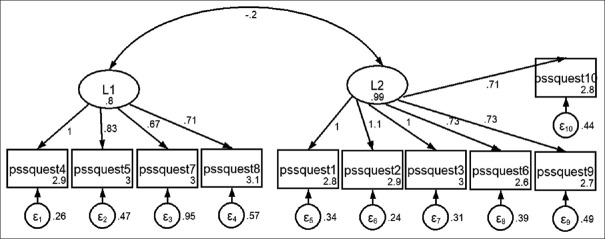
After EFA, the model was further analyzed by CFA. Figure 1 explains the model generated by our two-factor models using the structural equation modelling (SEM). CFA showed that the two-factor model had a χ2 value of 714.99 and P value < 0.001. Goodness-of-fit indices showed good CFI at 0.93, SRMR at 0.07, TLI at 0.90, and an acceptable RMSEA at 0.10.
Figure 1.
Evaluated model of the Tamil version of the Perceived Stress Scale (PSS) structure generated through structural equation modelling (SEM). L1: latent variable 1 (factor 1), L2: latent variable 2 (factor 2), pssquest1–pssquest1o: PSS item 1–10
Reliability (Internal consistency)
The Cronbach’s alpha value for TPSS-10 was found to be 0.86, indicating very good internal consistency.
Discussion
PSS, a widely used stress scale, has an added advantage of determining an individual’s behavior even before a stressful situation. Existing literature on the use of PSS in India focused on nonspecific samples, such as medical personnel,[21] school students,[24] occupational workers, teachers, and medical students.[25,26,27] Transferability of these findings to a broader disease spectrum involving a regional language is challenging. Attempts to translate and validate PSS in regional languages of India is not new, as efforts have been made earlier to validate PSS in Punjabi[25] and Hindi speakers.[28] Tamil, being a native language of Tamil Nadu and Puducherry, is also one of the official languages of Singapore and Sri Lanka with around 77 million native speakers globally.[29] A Tamil version of PSS that assesses the levels of stress among patients with chronic diseases conditions like diabetes is currently not in use. Thus, we undertook this study to evaluate the construct validity and reliability of TPSS-10 among DM patients in South India.
Hewitt et al.[29] in 1992 had labelled the final two-factor model that evolved as “Perceived distress,” as it included negative items tapping the general feelings of lack of control, and “perceived coping” with positively framed items reflecting the perception of ability to cope with increased stress. Our results also indicate a similar two-factor model for TPSS-10, such as factor 1 (perceived distress) having 6 negative items and factor 2 (perceived coping) having 4 positive items. These results were also found to be in line with other studies that attempted to validate the PSS.[17,20,21]
In our two-factor model, we found that all the factor loadings had statistically significant values. In addition, CFA findings also showed good CFI, TFI, and SRMR values. Our reliability assessment also showed a good overall Cronbach’s alpha of 0.86. This finding was also comparable with the previous regionally translated versions of PSS in India and other countries of the world.[17,20,21,30,31] This highlights the scale’s good internal consistency just like the other regional versions of the questionnaire, despite the lingual, regional, and cultural differences.[30,31]
Our study had many strengths. To the best of our knowledge, ours was the first attempt to validate the Tamil version of PSS among DM patients from India. A brief understanding regarding the homogeneity among the study participants with respect to their cultural, economic, and social contexts might help in better generalization of study results. Despite these strengths, our study had certain limitations. We did not assess the test and retest reliability, since our study was done at a single cross-sectional point of time. Moreover, the patients were recruited from the NCD clinics, and, therefore, our sample may not be representative of all the diabetic individuals present in the community. Hence, we encourage further research to explore the external validity of the questionnaire for determining fix cut-off points for the diagnosis of perceived stress among DM patients.
Our study findings have certain programmatic implications at a primary care level. Efforts to translate the questionnaire into the local Tamil language and validate it adds emphasis to the scientific basis for applying this scale among Tamil-speaking DM patients and capturing their level of perceived stress. It also emphasizes the application of simple instruments such as TPSS-10 at routine NCD clinics in the primary health center, at least once a year. This could help the primary care physicians to identify those with high stress levels at the earliest and refer them for necessary specialist counselling and treatment, train them regarding various methods of relaxation, and advocate lifestyle changes. Further research is necessary for the establishment of the construct validity of this instrument, as it is often a continuous process of refinement, evaluation, re-evaluation, and development. We recommend that future research consider cross-cultural invariance observed among diabetic individuals to arrive at additional significant findings.
Summary and Conclusion
This study concludes that the TPSS-10 is internally valid with a two-factor model (explaining 67.8% of the variance, correlation between factor 1 and factor 2 was 0.69, P value < 0.001.) and very good internal consistency (Cronbach’s alpha value of 0.86) among study participants. Hence, we conclude that our translated TPSS-10 could serve as a vital tool for primary care physicians to use to assess perceived stress among native Tamil-speaking DM patients across the globe.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. World Health Organization. 2011;155 Available from: https://apps.who.int/iris/handle/10665/44701 . [Google Scholar]
- 2.World Health Organization. Global Report on Diabetes. France: World Health Organization; 2016. [Google Scholar]
- 3.Rehman T, Rajaa S, Kumar G, Jayalakshmy R. Prevalence and factors influencing diabesity among persons with type 2 diabetes mellitus in urban Puducherry: A cross-sectional analytical study. Indian J Community Med. 2020;45:315–9. doi: 10.4103/ijcm.IJCM_324_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Diabetes Federation. IDF Diabetic Atlas. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Google Scholar]
- 5.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 6.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 8.Rajput R, Gehlawat P, Gehlan D, Gupta R, Rajput M. Prevalence and predictors of depression and anxiety in patients of diabetes mellitus in a tertiary care center. Indian J Endocrinol Metab. 2016;20:746–751. doi: 10.4103/2230-8210.192924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.IDF Clinical Guidelines Task Force: Global Guideline for Type 2 Diabetes. Brussels: International Diabetes Federation. 2005. [Last accessed on2016 Jul 22]. Available from: https://www.idf.org/sites/default/files/IDF%20T2DM%20Guideline.pdf .
- 10.Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care. 2000;23:934–42. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- 11.Vasanth R, Ganesh A, Shanker R. Impact of stress on type 2 diabetes mellitus management. Psychiatr Danub. 2017;29(Suppl 3):416–21. [PubMed] [Google Scholar]
- 12.Tan KC, Chan GC, Eric H, Maria AI, Norliza MJ, Oun BH, et al. Depression, anxiety and stress among patients with diabetes in primary care: A cross-sectional study. Malays Fam Physician. 2015;10:9–21. [PMC free article] [PubMed] [Google Scholar]
- 13.Sendhilkumar M, Tripathy JP, Harries AD, Dongre AR, Deepa M, Vidyulatha A, et al. Factors associated with high stress levels in adults with diabetes mellitus attending a tertiary diabetes care center, Chennai, Tamil Nadu, India. Indian J Endocrinol Metab. 2017;21:56–63. doi: 10.4103/2230-8210.196006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rehman A, Farhana KS. Prevalence and level of depression, anxiety and stress among patients with type-2 diabetes mellitus. Ann Pak Inst Med Sci. 2015;11:81–6. [Google Scholar]
- 15.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 16.Chen CH, Tseng YF, Chou FH, Wang SY. Effects of support group intervention in postnatally distressed women: A controlled study in Taiwan. J Psychosom Res. 2000;49:395–9. doi: 10.1016/s0022-3999(00)00180-x. [DOI] [PubMed] [Google Scholar]
- 17.Mimura C, Griffiths P. A Japanese version of the Perceived Stress Scale: Translation and preliminary test. Int J Nursing Stud. 2004;41:379–85. doi: 10.1016/j.ijnurstu.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Eskin M, Parr D. Introducing a Swedish Version of an Instrument Measuring Mental Stress. Open J Nursing: University of Stockholm. 1996;3:1–9. [Google Scholar]
- 19.Razurel C, Kaiser B, Dupuis M, Antonietti JP, Sellenet C, Epiney M. Validation of the postnatal perceived stress inventory in a French speaking population of primiparous women. J Obstet Gynecol Neonatal Nurs. 2013;42:685–96. doi: 10.1111/1552-6909.12251. [DOI] [PubMed] [Google Scholar]
- 20.Mimura C, Griffiths P. A Japanese version of the Perceived Stress Scale: Cross cultural translation and equivalence assessment. BMC Psychiatry. 2008;8:85–91. doi: 10.1186/1471-244X-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Dubai SA, Aishagga MA, Rampal KG, Sulaiman NA. Factor structure and reliability of the Malay version of the Perceived Stress Scale among Malaysian medical students. Malays J Med Sci. 2012;19:43–9. [PMC free article] [PubMed] [Google Scholar]
- 22.Rajaa S, Priyan S, Lakshminarayanan S, Kumar G. Health information needs assessment among self-help groups and willingness for involvement in health promotion in a rural setting in Puducherry: A mixed-method study. J Edu Health Promot. 2019;8:186. doi: 10.4103/jehp.jehp_35_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schermelleh-Engel K, Moosbrugger H, Muller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness of fit measures. MPR Online. 2003;8:23–74. [Google Scholar]
- 24.Augustine LF, Vazir S, Rao SF, Rao MV, Laxmaiah A, Nair KM. Perceived stress, life events &coping among higher secondary students of Hyderabad, India: A pilot study. Indian J Med Res. 2011;134:61. [PMC free article] [PubMed] [Google Scholar]
- 25.Chawla JK, Shweta S, Sandhu JS. Assessment of occupational stress using Punjabi version of Perceived Stress Scale (PSS-10) in Punjabi population. Int J Med Health Sci. 2014;3:163–71. [Google Scholar]
- 26.Limone P, Zefferino R, Toto GA, Tomei G. Work stress, mental health and validation of Professional Stress Scale (PSS) in an Italian-speaking teachers sample. Healthcare. 2021;9:1434. doi: 10.3390/healthcare9111434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen JY, Chin WY, Tiwari A, Wong J, Wong IC, Worsley A, et al. Validation of the Perceived Stress Scale (PSS-10) in medical and health sciences students in Hong Kong. Asia Pac Sch. 2021;6:31–7. [Google Scholar]
- 28.Pangtey R, Basu S, Meena GS, Banerjee B. Perceived stress and its epidemiological and behavioral correlates in an Urban Area of Delhi, India: A community-based cross-sectional study. Indian J Psychol Med. 2020;42:80–6. doi: 10.4103/IJPSYM.IJPSYM_528_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hewitt PL, Flett GL, Mosher SW. The Perceived Stress Scale: Factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess. 1992;14:247–257. [Google Scholar]
- 30.Lee EH. Review of the psychometric evidence of the Perceived Stress Scale. Asian Nurs Res. 2012;6:121–7. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 31.Ng S-M. Validation of the 10-item Chinese Perceived Stress Scale in elderly service workers: One-factor versus two-factor structure. BMC Psychol. 2013;1:9. doi: 10.1186/2050-7283-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]