Key Points
Question
What were the treatment times and in-hospital mortality among US patients with ST-segment elevation myocardial infarction (STEMI) between 2018 and 2021?
Findings
In this serial cross-sectional registry study that included 114 871 patients with STEMI, the median time to treatment was 86 minutes in the second quarter of 2018 and 91 minutes in the first quarter of 2021, a statistically significant difference. In-hospital mortality increased from 5.6% in the second quarter of 2018 to a peak of 8.7% in the first quarter of 2021, both statistically significant increases.
Meaning
This study provides registry data that inform understanding of the contemporary pattern of care and outcomes in US patients with STEMI.
Abstract
Importance
Recognizing the association between timely treatment and less myocardial injury for patients with ST-segment elevation myocardial infarction (STEMI), US national guidelines recommend specific treatment-time goals.
Objective
To describe these process measures and outcomes for a recent cohort of patients.
Design, Setting, and Participants
Cross-sectional study of a diagnosis-based registry between the second quarter of 2018 and the third quarter of 2021 for 114 871 patients with STEMI treated at 648 hospitals in the Get With The Guidelines–Coronary Artery Disease registry.
Exposures
STEMI or STEMI equivalent.
Main Outcomes and Measures
Treatment times, in-hospital mortality, and adherence to system goals (75% treated ≤90 minutes of first medical contact if the first hospital is percutaneous coronary intervention [PCI]-capable and ≤120 minutes if patients require transfer to a PCI-capable hospital).
Results
In the study population, median age was 63 (IQR, 54-72) years, 71% were men, and 29% were women. Median time from symptom onset to PCI was 148 minutes (IQR, 111-226) for patients presenting to PCI-capable hospitals by emergency medical service, 195 minutes (IQR, 127-349) for patients walking in, and 240 minutes (IQR, 166-402) for patients transferred from another hospital. Adjusted in-hospital mortality was lower for those treated within target times vs beyond time goals for patients transported via emergency medical services (first medical contact to laboratory activation ≤20 minutes [in-hospital mortality, 3.6 vs 9.2] adjusted OR, 0.54 [95% CI, 0.48-0.60], and first medical contact to device ≤90 minutes [in-hospital mortality, 3.3 vs 12.1] adjusted OR, 0.40 [95% CI, 0.36-0.44]), walk-in patients (hospital arrival to device ≤90 minutes [in-hospital mortality, 1.8 vs 4.7] adjusted OR, 0.47 [95% CI, 0.40-0.55]), and transferred patients (door-in to door-out time <30 minutes [in-hospital mortality, 2.9 vs 6.4] adjusted OR, 0.51 [95% CI, 0.32-0.78], and first hospital arrival to device ≤120 minutes [in-hospital mortality, 4.3 vs 14.2] adjusted OR, 0.44 [95% CI, 0.26-0.71]). Regardless of mode of presentation, system goals were not met in most quarters, with the most delayed system performance among patients requiring interhospital transfer (17% treated ≤120 minutes).
Conclusions and Relevance
This study of patients with STEMI included in a US national registry provides information on changes in process and outcomes between 2018 and 2021.
This cross-sectional study compares in-hospital mortality among patients with ST-segment elevation myocardial infarction receiving treatment within the US national guidelines–recommended target times vs later.
Introduction
Timely coronary artery perfusion remains the most important life-saving treatment for ST-segment elevation myocardial infarction (STEMI). Recognizing the relationship between treatment delays and morbidity and mortality, US national guidelines provide time-to-treatment goals starting at the time of first medical contact.1,2,3,4,5,6 In order to support the most effective treatment and provide data that bridge emergency medical systems (EMS) and hospitals, the American Heart Association established Mission: Lifeline and the Get With The Guidelines–Coronary Artery Disease (GWTG-CAD) registry. Since these data were last reported for patients treated between 2008 and 2012, quality programs have evolved and EMS agencies and hospitals have been subjected to the demands of a pandemic.7 This report describes process measures and outcomes for patients presenting with STEMI or STEMI equivalent (new left bundle branch block confirmed as a myocardial infarction [MI] or isolated posterior MI on electrocardiogram) between 2018 and 2021 as a benchmark. To consider the continued relevance of guideline-supported process times, the association between treatment goals and in-hospital mortality were examined during this time period.
Methods
Hospital participation in the registry is voluntary. Each participating hospital received either human research approval to enroll cases without individual patient consent under the common rule or a waiver of authorization and exemption from subsequent review by their institutional review board (IRB). Advarra, the IRB for the American Heart Association, determined that this study is exempt from IRB oversight. IQVIA served as the data collection and coordination center.
Participants and Exposure
Consecutive patients enrolled in the registry (the supporting data collection instrument for Mission: Lifeline quality improvement activities) between the second quarter of 2018 and the third quarter of 2021 with rest myocardial ischemia symptoms and an electrocardiogram (ECG) showing STEMI or STEMI equivalent were evaluated. This period of time was selected according to availability of risk factors on admission most associated with in-hospital mortality, cardiac arrest, shock, and heart failure, and the most recent data available when the analyses were completed. The study population involved a complete case analysis and included patients identified as having reasons for delay. The data were collected using retrospective chart review by hospital and EMS quality improvement professionals.
Outcomes
The outcomes assessed were treatment times, in-hospital mortality, and adherence to system goals. First medical contact was defined according to the setting where patients first presented: for those presenting by EMS to a percutaneous coronary intervention (PCI)–capable hospital, it was defined as the time they were first evaluated by paramedics; for those who walked in to a PCI-capable hospital, it was defined as hospital arrival time; and for those requiring interhospital transfer for PCI, it was defined as the time they arrived at the first hospital. The primary objective of the quality program was to provide coronary artery reperfusion (device time) for 75% of patients within 90 minutes of first medical contact for patients initially presenting to PCI-capable hospitals (direct), and 120 minutes for patients requiring hospital transfer for PCI (transfer) (eTable 1 in Supplement 1). According to the mode of patient presentation (EMS, walk in, or interhospital transfer), additional time processes were followed including laboratory activation within 20 minutes for EMS-presenting patients, ECG time within 10 minutes for walk-in patients, and arrival at first hospital to departure (door-in door-out) times within 30 minutes for transferred patients. Process times are presented in a fashion similar to the corresponding quality improvement efforts, with the addition of box and whisker plots (median, IQR, absolute range) to more fully describe the time data.
Statistical Analyses
To balance comparison of in-hospital mortality according to process goal achievement and between quarters, multivariable logistic regression models were generated to calculate odds ratios (ORs) adjusting for demographics (age, sex, race, and ethnicity) on admission, and illness severity descriptors (cardiac arrest, shock, and heart failure) on presentation. Race and ethnicity were grouped according to registry-defined categories as obtained by chart review. These descriptors were included because prior work has indicated differences in treatment and outcome according to these categories.8 Statistical significance was assessed at a 2 sided α = .05. Patients with missing data were not included in the regression analyses of mortality. Data analysis was performed using the open-source software R (R Foundation for Statistical Computing) with the American Heart Association Precision Medicine Platform.9
Results
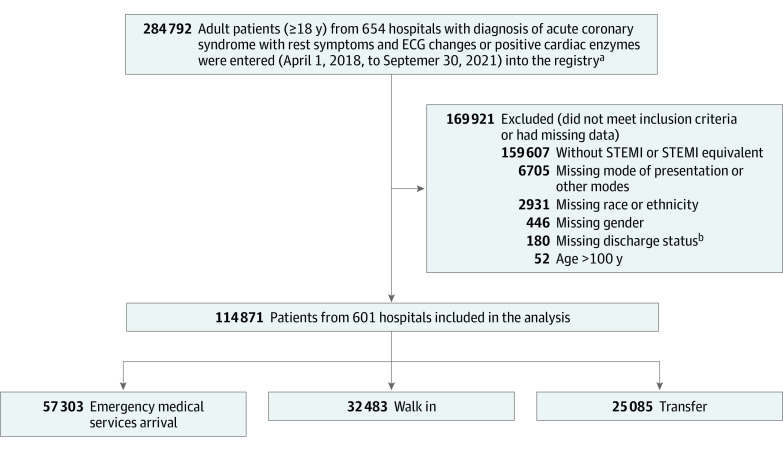
Between the second quarter of 2018 and the third quarter of 2021, 284 792 patients with a diagnosis of acute coronary syndrome (with rest symptoms and ECG changes or positive cardiac enzymes) were entered into the registry, of whom 114 871 patients with STEMI or STEMI equivalent on ECG were selected for this study (Figure 1). Among 601 participating hospitals in the registry, 505 were designated as STEMI receiving and 60 as STEMI referring, according to the quality improvement process terminology; 499 were urban and 63 rural, 102 hospitals had 500 or more beds, 496 were PCI capable on a 24-hour basis, and 294 had adult cardiac surgery (eTable 2 in Supplement 1). The median patient age was 63 (IQR, 54-72) years, 71% were men, and 29% were women. Demographic and clinical characteristics by mode of presentation are presented in Table 1. Risk factors present on admission included cardiogenic shock (7%) and heart failure (8%). In the second quarter of 2020, COVID-19 infection was added as a patient descriptor and was described as an active SARS-CoV-2 infection at admission or during hospitalization (range, 0.2% of patients treated in the second and third quarters of 2020, peaking at 0.7% of patients treated in the first quarter of 2021 [eTable 3 in Supplement 1]).
Figure 1. Flowchart of Cohort Selection for Patients With STEMI or STEMI Equivalent on Electrogram.
aRegistry refers to the Get With the Guidelines–Coronary Artery Disease registry.
bMissing discharge status refers to patient death or discharged to home, hospice, or other health care facilities.
STEMI indicates ST-segment elevation myocardial infarction.
Table 1. Selected Characteristics of Patients With STEMI or STEMI Equivalent by Mode of Presentation.
| Characteristics | Patients, No. (%)a | ||
|---|---|---|---|
| EMS arrival (n = 57 303) | Walk in (n = 32 483) | Transfer (n = 25 085) | |
| Age, median (IQR), y | 64 (55-73) | 61 (53-70) | 62 (54-71) |
| Men | 39 468 (68.9) | 24 177 (74.4) | 18 003 (71.8) |
| Women | 17 835 (31.1) | 8306 (25.6) | 7082 (28.2) |
| Race and ethnicity | |||
| American Indian/Alaska Native | 233 (0.4) | 153 (0.5) | 234 (0.9) |
| Asian | 2210 (3.9) | 1507 (4.6) | 562 (2.2) |
| Black | 7085 (12.4) | 3311 (10.2) | 2101 (8.4) |
| Hispanic | 4071 (7.1) | 3183 (9.8) | 1976 (7.9) |
| Native Hawaiian/Pacific Islander | 169 (0.3) | 88 (0.3) | 49 (0.2) |
| Non-Hispanic White | 41 690 (72.8) | 23 315 (71.8) | 19 520 (77.8) |
| Not specified | 1845 (3.2) | 926 (2.9) | 643 (2.6) |
| Heart rate documented on first medical contact, median (IQR), /min | 78 (63-94) | 81 (69-96) | 80 (67-95) |
| Systolic blood pressure on first medical contact, median (IQR), mm Hg | 138 (113-161) | 151 (131-172) | 147 (125-168) |
| Cardiac arrest prior to arrival, No./total No. (%) | 5551/53 293 (10.4) | NA | NA |
| Heart failure documented on first medical contact, No./total No. (%) | 4378/52 226 (8.4) | 1884/29 731 (6.3) | 1830/22 437 (8.2) |
| Cardiogenic shock documented on first medical contact, No./total No. (%) | 5277/52 196 (10.1) | 918/29 705 (3.1) | 1435/22 431 (6.4) |
| History of smoking, No./total No. (%) | 21 771/54 822 (39.7)b | 11 632/31 187 (37.3)b | 10 059/24 131 (41.7)b |
| Destination prearrival alert or notificationc | 41 620 (72.6) | NA | NA |
Abbreviations: EMS, emergency medical services; NA, not applicable; STEMI, ST-segment elevation myocardial infarction.
Numeric values are reported as No. (%) unless otherwise specified.
Regarding history of smoking, data were missing for 2481 (4.3%) patients who arrived by EMS, 1296 (4.0%) who walked in, and 954 (3.8%) who were transferred.
EMS notified hospital of incoming STEMI patient prior to arrival.
Among the 75% of patients directly presenting to PCI-capable hospitals, 63% arrived by EMS, 35% walked in, and 1.6% arrived by air transport. For the remaining patients who were transferred from another hospital for primary PCI, 70% were transferred by ground transport and 30% by air. During the study period, 84.6% of patients underwent primary PCI, 4.5% received thrombolytics, and 9.3% did not have a reperfusion method recorded. Overall, 20% of patients undergoing primary PCI were flagged as having a registry-defined hospital-specified reasons for delay, most commonly cardiac arrest and/or need for intubation (6.8%), other reasons (5.8%), and difficulty crossing the culprit lesion (3.8%) (Table 2). In 2020, a new reason for delay was added to the registry, “need for additional personal protective equipment for suspected/confirmed infectious disease.” This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters (eTable 4 in Supplement 1). The proportion of patients noted to have delays increased over time, from 17% in the second quarter of 2018, peaking at 25% in the second quarter of 2020 (difference, 8.4% [95% CI, 7.2%-9.7%]), and falling to 20% in the final quarter of data (difference, 3.8% [95% CI, 2.6%-5.1%]). This increase was observed in many categories of delay rather than solely in the personal protective equipment category.
Table 2. Hospital-Specified Reasons for Delay From First Medical Contact to Device by Mode of Presentation.
| Reasons | Patients, No. (%) | |||
|---|---|---|---|---|
| EMS arrival | Walk in | Transfer | All | |
| Cardiac arrest and/or need for intubation | 5417 (9.5) | 1197 (3.7) | 1182 (4.7) | 7796 (6.8) |
| Other reasons not specifieda | 3608 (6.3) | 1729 (5.3) | 1338 (5.3) | 6675 (5.8) |
| Difficulty crossing the culprit lesion | 2238 (3.9) | 1291 (4.0) | 874 (3.5) | 4403 (3.8) |
| Difficult vascular access diseaseb | 1554 (2.7) | 743 (2.3) | 565 (2.3) | 2862 (2.5) |
| Need for additional PPE for suspected or confirmed infectious diseasec | 746 (3.2) | 394 (3.2) | 255 (2.5) | 1395 (3.0) |
| Patient delays in providing consent | 576 (1.0) | 225 (0.7) | 160 (0.6) | 961 (0.8) |
| Emergent placement of LV support deviced | 562 (1.3) | 207 (0.8) | 190 (1) | 959 (1.1) |
| One or more reasons for delay | 13 175 (23.0) | 5234 (16.1) | 4171(16.6) | 22 580 (19.7) |
Abbreviations: EMS, emergency medical services; LV, left ventricular; PPE, personal protective equipment.
The other reasons category was not defined within the database. The main purpose of these exclusions was to allow for consistency of cohorts across hospitals.
Delay in percutaneous coronary intervention due to difficulty in passing catheters to the coronary artery ostia through available arterial access points including radial and femoral arteries.
The need for additional PPE for suspected or confirmed infectious disease only included individuals after the second quarter of 2020. This field refers to specific additional measures that delayed treatment, primarily related to cardiac catheterization laboratory delays.
The emergent placement of LV support device included individuals after the first quarter of 2019 since this variable started in 2019.
Process Times
Among patients presenting to PCI-capable hospitals, median time from symptom onset (identified by medical record review of patient report) to first medical contact was shorter for those presenting by EMS (52 minutes [IQR, 25-126]) as compared with walk-in patients (118 minutes [IQR, 58-267]). First medical contact to hospital time was 30 minutes (IQR, 23-39) for EMS patients. Over time, symptom onset to first medical contact increased from 50 to 54 minutes for EMS-presenting patients and from 114 to 120 minutes for walk-in patients.
Stratifying patients according to whether hospitals achieved target treatment times, adjusted in-hospital mortality was lower for those treated within target times (Table 3). For patients presenting to PCI-capable hospitals by EMS, the target was for first medical contact to laboratory activation within 20 minutes (in-hospital mortality, 3.6% vs 9.2%; adjusted OR, 0.54 [95% CI, 0.48-0.60]; P < .001), emergency department wait time 15 minutes or less (in-hospital mortality, 4.0% vs 10.9%; adjusted OR, 0.50 [95% CI, 0.44-0.57]; P < .001), and first medical contact to device within 90 minutes (in-hospital mortality, 3.3% vs 12.1%; adjusted OR, 0.40 [95% CI, 0.36-0.44]; P < .001) were all associated with significantly lower mortality. For walk-in patients, the target was for ECG within 10 minutes of arrival (in-hospital mortality, 2.4% vs 5.7%; adjusted OR, 0.52 [95% CI, 0.45-0.60]; P < .001), and hospital arrival to device within 90 minutes (in-hospital mortality, 1.8% vs 4.7%; adjusted OR, 0.47 [95% CI, 0.40-0.55]; P < .001) had lower in-hospital mortality. For patients transferred to a PCI-capable hospital, the target was for door-in to door-out time less than 30 minutes (in-hospital mortality 2.9% vs 6.4%; adjusted OR, 0.51 [95% CI, 0.32-0.78]; P < .05), and first hospital arrival to device within 120 minutes (in-hospital mortality, 4.3% vs 14.2%; adjusted OR, 0.44 [95% CI, 0.26-0.71]; P < .01) were associated with lower in-hospital mortality. Comparing adjusted in-hospital mortality by quarter for the entire cohort, mortality was significantly higher for patients treated in the second and fourth quarters of 2020 and the first and second quarters of 2021 (adjusted OR, 1.22 [95% CI, 1.01-1.47]); adjusted OR, 1.29 [95% CI, 1.08-1.55]; adjusted OR, 1.38 [95% CI, 1.15-1.65]; and adjusted OR, 1.26 [95% CI, 1.05-1.51]) relative to those treated in the second quarter of 2018.
Table 3. In-Hospital Mortality by Process Time Goalsa.
| Process and time goal | In-hospital death, No./total No. (%) | Met vs did not meet time goal, adjusted odds ratio (95% CI) | |
|---|---|---|---|
| Met time goal | Did not meet time goal | ||
| Directly presented to PCI-capable hospital by emergency medical services | |||
| First evaluated by paramedics time to cardiac catheterization laboratory activation time ≤20 min | 518/14 524 (3.6) | 2242/24 448 (9.2) | 0.54 (0.48-0.60) |
| Emergency department wait time ≤15 min | 377/9382 (4.0) | 4206/38 593 (10.9) | 0.50 (0.44-0.57) |
| Hospital arrival time to PCI device deployment time ≤90 min | 868/26 699 (3.3) | 2584/21 289 (12.1) | 0.40 (0.36-0.44) |
| Directly presented to PCI-capable hospital by walk inb | |||
| Hospital arrival time to electrocardiogram time ≤10 min | 509/21 622 (2.4) | 454/7907 (5.7) | 0.52 (0.45-0.60) |
| Hospital arrival time to PCI device deployment time ≤90 min | 367/20 307 (1.8) | 384/8140 (4.7) | 0.47 (0.40-0.55) |
| Presented to PCI-capable hospital via transfer from another hospital | |||
| Arrival at first hospital to departure ≤30 min | 77/2662 (2.9) | 1304/20 292 (6.4) | 0.51 (0.32-0.78) |
| First hospital arrival time to PCI device deployment time ≤120 min | 22/517 (4.3) | 291/2056 (14.2) | 0.44 (0.26-0.71) |
Abbreviation: PCI, percutaneous coronary intervention.
Adjusted models were adjusted for age, race and ethnicity, sex, cardiac arrest, cardiogenic shock, and heart failure on presentation. Model area under receiver operating characteristic curves and median of deviance residuals are provided in eTable 5 in Supplement 1.
Walk-in patients did not have cardiac arrest prior to arrival.
Figure 2 shows treatment times according to mode of presentation and study quarter for patients undergoing primary PCI. The quality initiative targeted treating 75% of patients within 90 minutes of first medical contact for those presenting to PCI-capable hospitals and within 120 minutes for those requiring interhospital transfer. Examining process time goal components, first medical contact to catheterization laboratory activation was more than 20 minutes for most EMS-presenting patients for all quarters, and first hospital door-in to door-out time was more than 30 minutes for most transferred patients for all quarters. Median time from symptom onset to PCI device deployment was 148 minutes (IQR, 111-226) for EMS-presenting patients, 195 minutes (IQR, 127-349) for walk-in patients, and 240 minutes (IQR, 166-402) for transferred patients.
Figure 2. Process Time Measures by Year, Quarter, and Mode of Presentation.
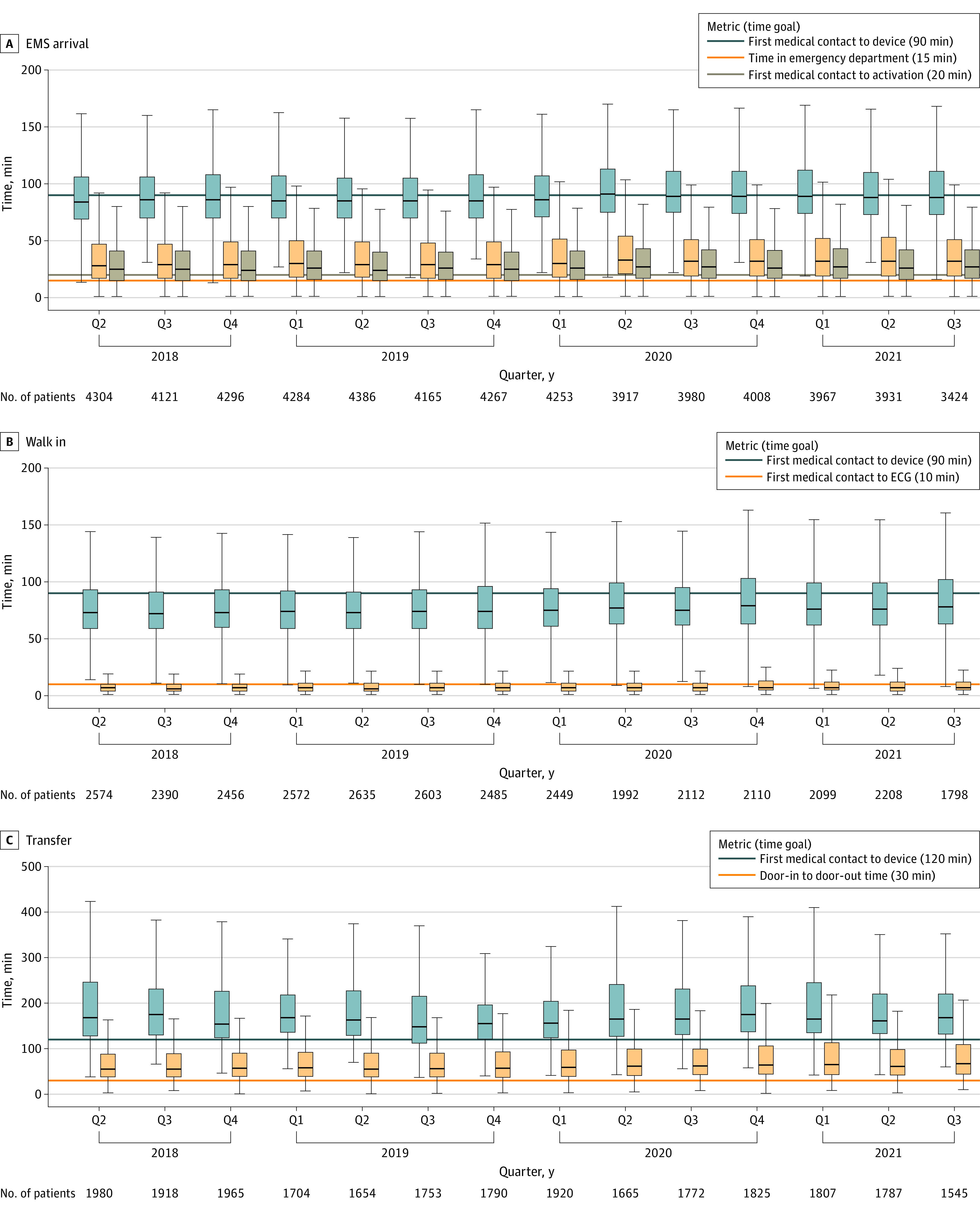
The horizontal line in each box indicates the median, the top and bottom of the boxes indicate the IQR, and the whiskers indicate the absolute range. The horizontal lines indicate the quality initiative for time goals for treating 75% of patients. EMS indicates emergency medical services.
Discussion
These data provide an overview of recent care for patients presenting with STEMI. The data continue to illustrate significantly lower mortality for patients treated within guideline-recommended time goals put forth more than a decade prior and reaffirmed in subsequent policy statements.1,2,3,4,5,6 While comparisons according to treatment time are confounded, as patients experiencing complications are more likely to be delayed in treatment, mortality remains substantially lower in those achieving guideline time goals after adjustment for patient characteristics most associated with mortality. Thus, some portion of the relationship is likely a reflection of the importance of time in achieving coronary reperfusion, an association that has remained constant since the time-dependent wave of myocardial necrosis initially documented by Reimer and Jennings.10
These data also identify concerning patterns and opportunities for improvement across the entire episode of care for patients presenting with STEMI. While a number of hospitals participating in this registry received quality recognition awards for having met national treatment time goals for 75% of patients, from the perspective of the overall system, many patients did not receive timely care.11 For patients presenting by EMS, the most readily identified process warranting additional focus involves catheterization laboratory activation prior to hospital arrival for patients diagnosed with STEMI by paramedics. When this process occurs within 20 minutes, emergency department wait times decrease, and there is less time for a catastrophic cardiac event to occur prior to coronary artery reperfusion.12,13
The most pressing opportunities appear to involve the processes for transferring patients from an initial hospital to one that is PCI capable, a scenario in which only 17% of patients were treated within 120 minutes of arrival to the first hospital. There are many actions that must take place in a coordinated and parallel fashion to diagnose STEMI and arrange rapid transfer, and the door-in to door-out time likely reflects the efficiency of these steps. Recommended processes include prespecified algorithms for diagnosis and treatment, assessing patients’ symptoms before hospital registration, ECG acquisition in a dedicated space within 10 minutes of arrival, immediate ECG interpretation by a physician or physician extender, enabling the transferring clinician to activate cardiac catheterization lab teams at the receiving hospital with a single contact, predetermined methods for rapid transfer including contingencies for weather unsuitable for air transport, simple transfer regimens that avoid continuous intravenous infusions, and the acceptance by PCI-capable hospitals of all patients requiring coronary reperfusion regardless of bed availability.5,6,13,14,15,16
The second quarter of 2020 represented the first full quarter of data during the COVID-19 pandemic. Less than 1% of STEMI patients were identified as having COVID-19, and delays related to personal protective equipment fell from 5.4% in the first quarter of the pandemic to 1.3% and 1.2% in the final 2 quarters. Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes. Rather, the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system. For 4 of the quarters during the pandemic, in-hospital mortality was significantly higher than the reference period (second quarter of 2018). The registry data in this study only capture patients who were diagnosed early in their course of illness and who survived until hospital presentation and registry enrollment; thus, these data only provide limited insight into the estimated 116 000 excess cardiovascular deaths observed during the first 2 years of the pandemic.17,18 These observational data did not identify a substantial increase in presenting illness severity that could account for the higher mortality.
Other opportunities identified by the registry involve the 9.3% of STEMI patients who did not receive any type of coronary reperfusion. For comparison, corresponding data from 2008 through 2012 reported a decline in the rate of untreated eligible patients falling from 6.2% to 3.3% during the study period.7
This study involved all patients regardless of reason for delay designation. Over the study period, the number of patients with 1 or more reasons for delays increased from 17% to 21%, partly related for the need to employ protective protocols for the SARS-CoV-2 virus, particularly during the first quarter of the pandemic when 6% of cases were delayed for this reason. The rates of delays were substantially higher than the 9% to 15% of patients with delays observed in prior registry reports of patients undergoing primary PCI and are similar to the 28% rate reported from a corresponding Centers for Medicare & Medicaid Services quality measurement initiative.19,20,21 Patients with hospital-specified reasons for delay were included in the analyses to provide the broadest overview of the STEMI reperfusion and because patients designated to have such delays historically have the highest mortality.
Limitations
This study has several limitations. The first involves the self-reported nature of the registry data. The registry is a voluntary quality improvement project with the objective of assisting participating hospitals to improve their processes of care and does not include data quality audits. A second related limitation involves missing data for approximately 8% of patients. The data were primarily collected from chart review, limiting the ability to identify important conditions or processes that were not recorded. Furthermore, many of the data fields were not required to be completed as a condition of submission, resulting in missing data. The regression analyses in this study include only patients for whom full data were available, rather than impute missing data fields, as the ability of available fields to predict missing data for highly prognostic terms such as cardiac arrest was quite limited. To the extent that missing data were not a random occurrence, these observations may be biased by the factors that led to data not being reported. A third limitation involves the use of logistic models that did not account for clustering or the lack of independence between patients treated at the same hospital. Thus, the models potentially overestimated the significance of associations between treatment time and mortality but not to a degree likely to account for the very large observed mortality differences. Despite these significant limitations, these data represent 1 of 2 available contemporary registries of STEMI care in the United States that provides an overview of recent practice.
Conclusions
This study of patients with STEMI included in a US national registry provides information on changes in process and outcomes between 2018 and 2021.
eTable 1. Process Time Goals From Select Mission: Lifeline Quality Improvement Programs
eTable 2. Characteristics of GWTG-CAD Registry Hospitals
eTable 3. Selected Characteristics of Patients With STEMI or STEMI Equivalent by Year Quarter
eTable 4. Hospital-Specified Reasons for Delay by Year Quarter
eTable 5. Model Diagnostics for Multivariate Logistic Regression
Data Sharing Statement
References
- 1.Gersh BJ, Stone GW, White HD, Holmes DR Jr. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA. 2005;293(8):979-986. doi: 10.1001/jama.293.8.979 [DOI] [PubMed] [Google Scholar]
- 2.Henry TD, Sharkey SW, Burke MN, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116(7):721-728. doi: 10.1161/CIRCULATIONAHA.107.694141 [DOI] [PubMed] [Google Scholar]
- 3.Jollis JG, Roettig ML, Aluko AO, et al. ; Reperfusion of Acute Myocardial Infarction in North Carolina Emergency Departments (RACE) Investigators . Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298(20):2371-2380. doi: 10.1001/jama.298.20.joc70124 [DOI] [PubMed] [Google Scholar]
- 4.Antman EM, Hand M, Armstrong PW, et al. 2007 Focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;117(2):296-329. doi: 10.1161/CIRCULATIONAHA.107.188209 [DOI] [PubMed] [Google Scholar]
- 5.O’Gara PT, Kushner FG, Ascheim DD, et al. ; CF/AHA Task Force . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. Circulation. 2013;127(4):529-555. doi: 10.1161/CIR.0b013e3182742c84 [DOI] [PubMed] [Google Scholar]
- 6.Jacobs AK, Ali MJ, Best PJ, et al. Systems of care for ST-segment–elevation myocardial infarction: a policy statement from the American Heart Association. Circulation. 2021;144(20):e310-e327. doi: 10.1161/CIR.0000000000001025 [DOI] [PubMed] [Google Scholar]
- 7.Granger CB, Bates ER, Jollis JG, et al. Improving care of STEMI in the United States 2008 to 2012. J Am Heart Assoc. 2019;8(1):e008096. doi: 10.1161/JAHA.118.008096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McNamara RL, Kennedy KF, Cohen DJ, et al. Predicting in-hospital mortality in patients with acute myocardial infarction. J Am Coll Cardiol. 2016;68(6):626-635. doi: 10.1016/j.jacc.2016.05.049 [DOI] [PubMed] [Google Scholar]
- 9.American Heart Association . Precision Medicine Platform. Accessed November 1, 2022. https://precision.heart.org
- 10.Reimer KA, Lowe JE, Rasmussen MM, Jennings RB. The wavefront phenomenon of ischemic cell death. Circulation. 1977;56(5):786-794. doi: 10.1161/01.CIR.56.5.786 [DOI] [PubMed] [Google Scholar]
- 11.American Heart Association . How to find heart and stroke care near you, measured by the American Heart Association. Accessed September 16, 2022. https://www.usnewsbrandfuse.com/AmericanHeartAssociation
- 12.Bagai A, Al-Khalidi HR, Muñoz D, et al. Bypassing the emergency department and time to reperfusion in patients with prehospital ST-segment-elevation: findings from the reperfusion in acute myocardial infarction in Carolina Emergency Departments project. Circ Cardiovasc Interv. 2013;6(4):399-406. doi: 10.1161/CIRCINTERVENTIONS.112.000136 [DOI] [PubMed] [Google Scholar]
- 13.Glickman SW, Lytle BL, Ou FS, et al. Care processes associated with quicker door-in-door-out times for patients with ST-elevation-myocardial infarction requiring transfer: results from a statewide regionalization program. Circ Cardiovasc Qual Outcomes. 2011;4(4):382-388. doi: 10.1161/CIRCOUTCOMES.110.959643 [DOI] [PubMed] [Google Scholar]
- 14.Fordyce CB, Al-Khalidi HR, Jollis JG, et al. ; STEMI Systems Accelerator Project . Association of rapid care process implementation on reperfusion times across multiple ST-segment-elevation myocardial infarction networks. Circ Cardiovasc Interv. 2017;10(1):e004061. doi: 10.1161/CIRCINTERVENTIONS.116.004061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeitouni M, Al-Khalidi HR, Roettig ML, et al. Catheterization laboratory activation time in patients transferred with ST-segment-elevation myocardial infarction: insights from the Mission: Lifeline STEMI Accelerator-2 Project. Circ Cardiovasc Qual Outcomes. 2020;13(7):e006204. doi: 10.1161/CIRCOUTCOMES.119.006204 [DOI] [PubMed] [Google Scholar]
- 16.Jollis JG, Al-Khalidi HR, Roettig ML, et al. Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: Mission: Lifeline Accelerator-2. Circulation. 2018;137(4):376-387. doi: 10.1161/CIRCULATIONAHA.117.032446 [DOI] [PubMed] [Google Scholar]
- 17.Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021;6(3):296-303. doi: 10.1001/jamacardio.2020.6210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uy-Evanado A, Chugh HS, Sargsyan A, et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol. 2021;7(1):6-11. doi: 10.1016/j.jacep.2020.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swaminathan RV, Wang TY, Kaltenbach LA, et al. Nonsystem reasons for delay in door-to-balloon time and associated in-hospital mortality: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2013;61(16):1688-1695. doi: 10.1016/j.jacc.2012.11.073 [DOI] [PubMed] [Google Scholar]
- 20.McCabe JM, Kennedy KF, Yeh RW. Defining unavoidable delays in primary percutaneous coronary intervention: discordance among patients excluded from National Cardiovascular Quality Registries. J Am Heart Assoc. 2014;3(3):e000944. doi: 10.1161/JAHA.114.000944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cotoni DA, Roe MT, Li S, Kontos MC. Frequency of nonsystem delays in ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention and implications for door-to-balloon time reporting (from the American Heart Association Mission: Lifeline program). Am J Cardiol. 2014;114(1):24-28. doi: 10.1016/j.amjcard.2014.04.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Process Time Goals From Select Mission: Lifeline Quality Improvement Programs
eTable 2. Characteristics of GWTG-CAD Registry Hospitals
eTable 3. Selected Characteristics of Patients With STEMI or STEMI Equivalent by Year Quarter
eTable 4. Hospital-Specified Reasons for Delay by Year Quarter
eTable 5. Model Diagnostics for Multivariate Logistic Regression
Data Sharing Statement