Abstract
Background
Depression is one of the most common mental illnesses. There are well-known deficiencies in the care of patients with depression, particularly at the interfaces between health service areas or sectors. The aim of this study was to analyze the characteristics and state of care of persons with a diagnosis of depression.
Methods
The analysis was based on diagnosis and billing data obtained from a statutory health insurance carrier in Germany. Patients carrying a diagnosis of depression in 2018 (ICD-10 F32, F33, F34.1) were identified and studied with respect to their utilization of care services for depression. Sociodemographic characteristics and the degree of severity of depression were also taken into account.
Results
More than 285 000 individuals with a diagnosis of depression were included in the analysis. Their mean age was 57.5 years, and 67.5% were female. About three-quarters had at least one comorbid mental disorder. Primary care physicians were involved in the treatment of depression for 82.8% of patients with severe depression; 41.1% of such patients had contact with a medical specialist, and 9.2% with a psychologist-psychotherapist. Antidepressants were prescribed for 60.3% of patients with severe depression, and 10.2% were receiving psychotherapeutic services in accordance with the psychotherapy directive.
Conclusion
Our findings point to existing deficiencies in the care of patients with depression, particularly in the establishment of the diagnosis and in the assessment of disease severity. These are essential matters for the initiation of guideline-oriented therapy and therefore deserve to be more strongly emphasized in continuing medical education.
Mental illness is one of the commonest causes of health impairment. Thus, depressive disorders and anxiety disorders are among the top ten disorders in adulthood that cause the highest global burden of disease (1). At the same time, and in addition to the health and social effects on those affected, mental illness results in considerable costs for health care systems (2).
In Germany and other industrial countries, depression is among the most common mental illnesses. According to the DEGS1-MH study conducted by the Robert Koch Institute (RKI; survey period: 2009–2012), the prevalence of unipolar depression is 8.2% and of dysthymia 1.7% (3, 4). If one compares the results of different health surveys in Germany, one sees that the prevalences of mental illness remain largely stable over time (5). In contrast, studies based on routine data from a German statutory health insurance (SHI) carrier (gesetzlichen Krankenversicherung) suggest a significant rise in the administrative prevalence over time (6, 7). The administrative prevalence describes the estimated disease incidence based on diagnoses medically established and documented in routine SHI data (8). Whereas in 2009 depression was diagnosed in 12.5% of individuals with statutory health insurance, this percentage had already risen to 15.7% by 2017 (6). At the same time, the number of absences among the working population due to illness have increased, as has the number of people undergoing rehabilitation and drawing reduced earning capacity pensions from the German Pension Insurance (Deutsche Rentenversicherung) due to mental illness (7). Why the number of affected individuals, according to data from the RKI, is stagnating in spite of the fact that the provision of care and its utilization have significantly increased in Germany in recent years (for example, psychiatric hospital beds and prescriptions of psychopharmacological drugs, rise in psychiatric inpatient treatment) is the subject of controversy. Explanations start by pointing out that specific and needs-oriented evidence-based prevention and care services are insufficiently implemented and utilized, morbidity is rising, and how society deals with mental illness is changing (9). Furthermore, changes in professional concepts of mental illness are contributing to more individuals being classified today as affected (10). The quality of care in Germany, as well as the extent to which it complies with guidelines, has been insufficiently investigated. For example, the results of the “Health Fact-Check” (Faktencheck Gesundheit) conducted by the Bertelsmann Foundation are based on routine SHI data from 2011. These show that a considerable proportion of patients with depression did not receive guideline-compliant care (11). A cross-sectional study found that patients with depressive disorders were undertreated in the primary care setting (12). More recent data on patients with depression reveal problems in the transition from inpatient to outpatient treatment (13).
The aim of the present study was to gather information on the state of care of patients with a diagnosis of depression. In addition to the frequency of the diagnosis as well as the characteristics and comorbidities of patients with depression, focus was also placed on depicting the utilization of specific serves, particularly in relation to the severity of depression.
Methods
Study design and data basis
The analyses are based on diagnosis and billing data from the German General Local Health Insurance Fund (Allgemeine Ortskrankenkasse, AOK) for the state of Lower Saxony. With 2.9 million insured persons, this insurance fund is one of the largest statutory health insurance funds in Germany and is similar to the overall German population in terms of its sex and age structure (14, 15).
Due to the nature of routine data from SHI, they are increasingly used to answer questions in (epidemiological) healthcare research (8). Routine data are also increasingly used in research on depressive disorders (6, 7, 16). The present study analyzed the diagnosis and services data for the outpatient and inpatient sectors, as well as for drug prescriptions.
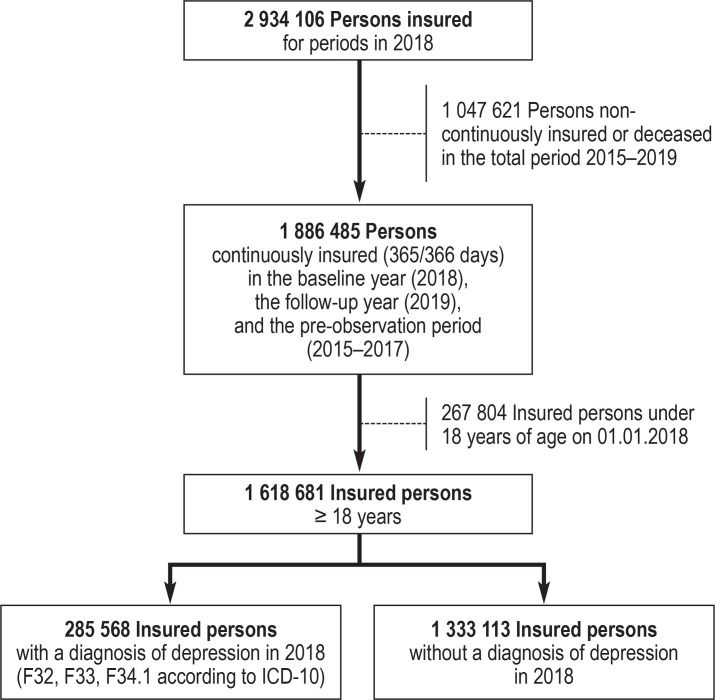
To this end, the state of care for patients with the diagnosis of depression was considered in a cross-sectional manner. Inclusion criteria were continuous insurance in the baseline year (2018), the pre-observation period (2015–2017), and the follow-up year (2019), as well as age 18 years or over (efigure 1). The pre-observation period served to differentiate between incident and prevalent cases. Using the follow-up period, it was possible to depict changes in diagnosis and/or severity in a year-on-year comparison.
eFigure 1.
Flowchart of study population selection
ICD-10, International Statistical Classification of Diseases and Related Health Problems
Classification of patients with depression and severity classification
Insured persons were included in the analysis if they received a diagnosis in 2018 of a depressive episode (F32), a recurrent depressive disorder (F33), or dysthymia (F34.1), either as a confirmed outpatient diagnosis or as an inpatient principal discharge/secondary diagnosis. When classifying the disease into different levels of severity, as explicitly provided for in the International Statistical Classification of Diseases and Related Health Problems (ICD-10), and the specificity of the diagnoses, we were guided by the approach of the Bertelsmann Foundation and the Central Institute of the Association of Statutory Health Insurance Physicians (Zentralinstitut für die kassenärztlichen Versorgung, ZI) (6, 11). Patients were assigned to the highest-coded level of severity in the year of the analysis, 2018. If the same patient was coded with both specific and nonspecific diagnoses, the specific diagnosis was used for the classification. Specific diagnoses include the following severity levels: mild (F32.0, F33.0, F34.1), moderate (F32.1, F33.1), and severe (F32.2, F33.2, F32.3, F33.3). Diagnoses of other, or not otherwise specified, depressive disorders (F32.8, F33.8, F33.4, F32.9, F33.9) were grouped together as nonspecific. Somatic and psychological comorbidities were also defined using ICD-10 diagnoses from the outpatient and inpatient setting.
The state of care and its utilization
The state of care and utilization of services were depicted using outpatient treatments in which a diagnosis of depression was coded, inpatient treatments with mental health diagnoses, as well as specific drug prescriptions. In outpatient care, treatments were differentiated according to the following specialties:
Primary care physicians
Medical specialists (specialists in neurology and psychiatry, neurology, psychiatry and psychotherapy, psychosomatic medicine and psychotherapy, physicians practicing psychotherapy)
Psychological psychotherapists.
Furthermore, the extent to which services were utilized in line with the psychotherapy guideline was investigated (etable 1). These services were identified using the specific codes of the uniform evaluation scale (Einheitlicher Bewertungsmaßstab, EBM). A distinction was made between the following services:
eTable 1. Overview of services according to the psychotherapy guideline in the German Uniform Evaluation Standard (EBM) catalog.
| EBM No. | Description |
| Services not subject to an application process | |
| 35100 | Differential diagnostic investigation of psychosomatic disease states |
| 35110 | Verbal intervention in psychosomatic disease states |
| 35111 | Exercise interventions, individual therapy |
| 35112 | Exercise interventions, group therapy |
| 35120 | Hypnosis |
| 35130 | Report to the assessor (STT 1 or 2) |
| 35131 | Report to the assessor (LTT) |
| 35140 | Biographical history of the patient |
| 35141 | In-depth exploration |
| 35142 | Surcharge for assessing neurological and psychiatric findings |
| 35150 | Trial session |
| 35151 | Psychotherapeutic consultation hours |
| 35152 | Acute psychotherapeutic treatment |
| Services subject to an application process | |
| 35401 | Depth psychology-based psychotherapy (STT 1, individual therapy) |
| 35402 | Depth psychology-based psychotherapy (STT 2, individual therapy) |
| 35405 | Depth psychology-based psychotherapy (LTT, individual therapy) |
| 35411 | Analytical psychotherapy (STT 1, individual therapy) |
| 35412 | Analytical psychotherapy (STT 2, individual therapy) |
| 35415 | Analytical psychotherapy (LTT, individual therapy) |
| 35421 | Behavioral therapy (STT 1, individual therapy) |
| 35422 | Behavioral therapy (STT 2, individual therapy) |
| 35425 | Behavioral therapy (LTT, individual therapy) |
| 35503 | Psychodynamic psychotherapy (STT), 3 Ps |
| 35504 | Psychodynamic psychotherapy (STT), 4 Ps |
| 35505 | Psychodynamic psychotherapy (STT), 5 Ps |
| 35506 | Psychodynamic psychotherapy (STT), 6 Ps |
| 35507 | Psychodynamic psychotherapy (STT), 7 Ps |
| 35508 | Psychodynamic psychotherapy (STT), 8 Ps |
| 35509 | Psychodynamic psychotherapy (STT), 9 Ps |
| 35513 | Psychodynamic psychotherapy (LTT), 3 Ps |
| 35514 | Psychodynamic psychotherapy (LTT), 4 Ps |
| 35515 | Psychodynamic psychotherapy (LTT), 5 Ps |
| 35516 | Psychodynamic psychotherapy (LTT), 6 Ps |
| 35517 | Psychodynamic psychotherapy (LTT), 7 Ps |
| 35518 | Psychodynamic psychotherapy (LTT), 8 Ps |
| 35519 | Psychodynamic psychotherapy (LTT), 9 Ps |
| 35523 | Analytical psychotherapy (STT), 3 Ps |
| 35524 | Analytical psychotherapy (STT), 4 Ps |
| 35525 | Analytical psychotherapy (STT), 5 Ps |
| 35526 | Analytical psychotherapy (STT), 6 Ps |
| 35527 | Analytical psychotherapy (STT), 7 Ps |
| 35528 | Analytical psychotherapy (STT), 8 Ps |
| 35529 | Analytical psychotherapy (STT), 9 Ps |
| 35533 | Analytical psychotherapy (LTT), 3 Ps |
| 35534 | Analytical psychotherapy (LTT), 4 Ps |
| 35535 | Analytical psychotherapy (LTT), 5 Ps |
| 35536 | Analytical psychotherapy (LTT), 6 Ps |
| 35537 | Analytical psychotherapy (LTT), 7 Ps |
| 35538 | Analytical psychotherapy (LTT), 8 Ps |
| 35539 | Analytical psychotherapy (LTT), 9 Ps |
| 35543 | Behavioral therapy (STT), 3 Ps |
| 35544 | Behavioral therapy (STT), 4 Ps |
| 35545 | Behavioral therapy (STT), 5 Ps |
| 35546 | Behavioral therapy (STT), 6 Ps |
| 35547 | Behavioral therapy (STT), 7 Ps |
| 35548 | Behavioral therapy (STT), 8 Ps |
| 35549 | Behavioral therapy (STT), 9 Ps |
| 35553 | Behavioral therapy (LTT), 3 Ps |
| 35554 | Behavioral therapy (LTT), 4 Ps |
| 35555 | Behavioral therapy (LTT), 5 Ps |
| 35556 | Behavioral therapy (LTT), 6 Ps |
| 35557 | Behavioral therapy (LTT), 7 Ps |
| 35558 | Behavioral therapy (LTT), 8 Ps |
| 35559 | Behavioral therapy (LTT), 9 Ps |
| Psychodiagnostic testing methods | |
| 35600 | Testing methods, standardized |
| 35601 | Testing methods, psychometric |
| 35602 | Methods, projective |
EBM, German Uniform Evaluation Standard (Einheitlicher Bewertungsmaßstab); STT, short-term therapy; LTT, long-term therapy, Ps, participants
Services not subject to an application process (for example, trial session, psychotherapeutic consultation hours)
Services subject to an application process (for example, individual or group behavioral therapy)
In order to depict inpatient care, all hospitalizations involving depression as the principal discharge diagnosis, as well as additionally with a diagnosis in the F chapter, were investigated. With regard to the provision of drugs, prescriptions in the active substance classes of antidepressants (N06A) were considered according to the Anatomical Therapeutic Chemical (ATC) classification, as well as supplementary lithium (N05AN), antipsychotics (N05A), and benzodiazepines (N05BA), since these are sometimes used for certain forms of depression (19).
Statistical analysis
Data analysis was performed using IBM SPSS Statistics 25 software. Analyses were carried out primarily descriptively. Group comparisons were carried out using appropriate test methods (chi square test or t-test). Statistical significance was set at p ≤ 0.05.
Results
Frequency of depression diagnoses and patient characteristics
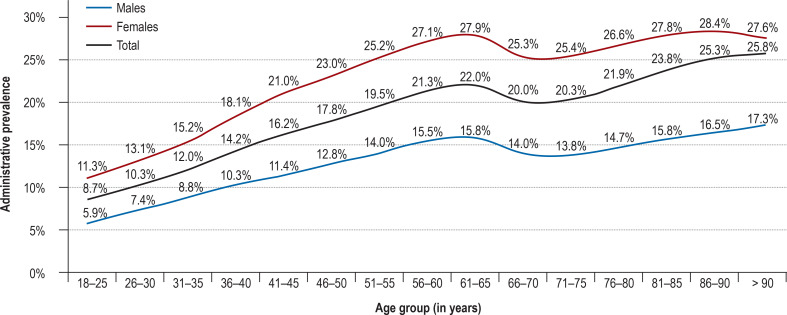
A total of 1,618,681 insured persons were included in the analysis. A diagnosis of depression was coded for 285,568 of these insured persons in 2018. Thus, the administrative 1-year prevalence in 2018 was 17.6%, whereas the administrative 1-year incidence was 2.6%. The former was almost twice as high in females compared to males (22.4% vs. 12.3%) (p < 0.001). It increased with age for both sexes, reaching its highest level in the 61–65 age group, then initially declining only to rise again (figure 1).
Figure 1.
Administrative 1-year prevalence of depressive disorders according to age
The figure shows the frequency of diagnoses of depression (codes F32, F33, and F34.1 of the International Statistical Classification of Diseases and Related Health Problems [ICD-10]) depending on age. The data basis consists of diagnoses in the outpatient medical sector as well as the inpatient care sector.
The mean age of patients diagnosed with depression was 57.5 years, and 67.5% were female. Approximately three out of four patients (73.8%) had at least one other mental health comorbidity. The most frequent comorbidities belonged to the group of neurotic, stress-related, and somatoform disorders (F40–F48) (57.1%) as well as the group of mental and behavioral disorders due to psychoactive substance use (F10-F19) (20.1%). Mental health comorbidities became more frequent with increasing severity of the depressive disorder (p < 0.001). Table 1 provides an overview of mental health and somatic comorbidities.
Table 1. Frequency of comorbidities.
| Diagnostic category | Level of severity | Total | |||
| Mild | Moderate | Severe | Nonspecific | ||
| A: Mental health comorbidities | |||||
| F00–F09: Organic, including symptomatic mental disorders | 9.9% | 9.2% | 10.9% | 9.4% | 9.6% |
| F10–F19: Mental and behavioral disorders due to psychoactive substances | 17.2% | 21.1% | 26.6% | 17.7% | 20.1% |
| F20–F29: Schizophrenia, schizotypal, and delusional disorders | 3.0% | 3.7% | 7.7% | 3.5% | 4.1% |
| F40–F48: Neurotic. stress-related. and somatoform disorders | 55.2% | 62.4% | 68.2% | 48.7% | 57.1% |
| F50–F59: Abnormal behaviors associated with physiological disturbances and physical factors | 9.0% | 11.0% | 13.1% | 7.5% | 9.7% |
| F60–F69: Personality and behavioral disorders | 8.2% | 10.5% | 16.1% | 5.8% | 9.3% |
| B: Somatic comorbidities | |||||
| I10: Essential (primary) hypertension | 55.8% | ||||
| I50: Heart failure | 11.9% | ||||
| I25: Chronic ischemic heart disease | 15.2% | ||||
| E78: Disorders of lipoprotein metabolism and other lipidemias | 35.1% | ||||
| E11: Type 2 diabetes mellitus | 20.0% | ||||
| E10: Type 1 diabetes mellitus | 3.2% | ||||
| J44: Chronic obstructive pulmonary disease | 14.0% | ||||
| J45: Asthma | 13.0% | ||||
A: Mental health comorbidities according to severity level:
The table shows the frequency of mental health comorbidities according to the level of severity of the depressive disorder in line with the International Statistical Classification of Diseases and Related Health Problems (ICD-10). The data basis consists of diagnoses in the outpatient medical sector as well as the inpatient care sector.
B: Somatic comorbidities:
The table shows the frequency of common somatic comorbidities according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10).
The data basis consists of diagnoses in the outpatient medical sector as well as the inpatient care sector
Diagnosis and severity of the disorder
A total of 1.28 million confirmed diagnoses of depression in the study population were made in the outpatient sector. Almost half of all coded diagnoses of depression were nonspecific (47.2%). Mild depression accounted for 11.2%, moderate for 25.7%, and severe for 11.2% of all diagnoses. Dysthymia was comparatively rarely identified (4.7%).
A total of 64.2% of all outpatient diagnoses of depression were made by primary care providers (53.6% of which were nonspecific). In all, 15.8% were made by specialists in mental health disorders or psychological psychotherapists (of which 14.4% were nonspecific), and 20.0% of diagnoses were made in other specialties, such as gynecology and orthopedics (of which 52.8% were nonspecific).
According to the differentiation of severity of illness at the patient level, 16.1% of those affected suffered from a mild, 30.3% from a moderate, and 16.2% from a severe form of depression. In 37.5% of cases, it was not possible to assign a level of severity, since only nonspecific diagnoses of depression were available for these cases. The analysis according to sex revealed a similar severity distribution between males and females. With increasing age, the proportion of diagnoses of moderate or severe depression declined, while nonspecific diagnoses simultaneously rose (table 2).
Table 2. Specificity and severity of the disorder.
| Level of severity | ||||
| Mild | Moderate | Severe | Nonspecific | |
| Sex | ||||
| All | 16.1% | 30.3% | 16.2% | 37.5% |
| Males (n = 93,190) | 15.8% | 29.9% | 16.9% | 37.3% |
| Females (n = 192,378) | 16.2% | 30.4% | 15.8% | 37.6% |
| Age group | ||||
| 18–29 Years (n = 22,200) | 14.2% | 34.0% | 17.6% | 34.2% |
| 30–39 Years (n = 26,808) | 14.3% | 33.3% | 16.7% | 35.7% |
| 40–49 Years (n = 40,628) | 14.3% | 33.0% | 18.5% | 34.2% |
| 50–59 Years (n = 64,928) | 14.6% | 32.5% | 19.0% | 34.0% |
| 60–69 Years (n = 53,824) | 17.0% | 29.5% | 15.6% | 38.0% |
| 70–79 Years (n = 42,532) | 19.2% | 25.9% | 12.8% | 42.2% |
| 80–89 Years (n = 30,462) | 18.3% | 25.2% | 11.9% | 44.6% |
| ≥ 90 Years (n = 4186) | 16.7% | 22.8% | 11.0% | 49.5% |
The table subdivides the patient population (n = 285,568) according to level of severity of the depressive disorder. This subdivision additionally differentiates between sex and age groups. Patients were assigned to the highest-coded level of severity in the year of the analysis, 2018. If the same patient was coded with both specific and nonspecific diagnoses, the specific diagnosis was used as the basis for the classification. The data basis consists of diagnoses in the outpatient medical sector as well as the inpatient care sector.
The state of care and its utilization
Depression was diagnosed in the primary care setting in 78.3% of all patients, making primary care physicians the most common diagnosing doctor. Of all those with a finding of depression, 18.7% had contact with a medical specialist due to their depression, and 5.1% had contact with a psychological psychotherapist (table 3). Overall in 2018, 50.7% of insured persons with a diagnosis of depression utilized a psychotherapeutic service that was not subject to an application process according to the psychotherapy guideline, and 6.2% utilized a service that was not subject to an application process (details on services in eTables 2 and 3). In all, 42% of diagnosed persons were prescribed antidepressants (ATC Classification: N06A), making a total of 465 992 prescriptions issued for these drugs (information on pharmacological treatment in eTable 4 and eFigure 2). The percentage of affected individuals admitted to hospital for a mental disorder (F diagnosis) was 4.7%. Hospitalization due to a depressive disorder was coded in 2.2% of cases.
Table 3. Depression-specific utilization of services according to sex, age, and severity.
| Care sector | ||||||||
| Primary care physician*1 | Medical specialist*2 | Psychological psychotherapist*3 | Other specialist*4 | Services not subject to an application process | Services subject to an application process | Antidepressant prescriptions (ATC: N06A) | Inpatient treatment (depression) | |
| Patient group | ||||||||
| All | 78.3% | 18.7% | 5.1% | 33.7% | 50.7% | 6.2% | 42.0% | 2.2% |
| Sex | n. s. | *** | *** | *** | *** | *** | *** | *** |
| Males (n = 93 190) | 78.1% | 19.5% | 4.5% | 30.0% | 47.2% | 5.2% | 39.5% | 2.5% |
| Females (n = 192 378) | 78.4% | 18.3% | 5.4% | 36.2% | 52.4% | 6.7% | 43.2% | 2.0% |
| Severity | *** | *** | *** | *** | *** | *** | *** | *** |
| Mild (n = 45 850) | 69.5% | 16.4% | 3.9% | 38.3% | 48.0% | 4.6% | 33.2% | 0.0% |
| Moderate (n = 86 438) | 79.2% | 25.8% | 9.7% | 33.0% | 55.7% | 10.6% | 48.1% | 1.4% |
| Severe (n = 46 126) | 82.8% | 41.1% | 9.2% | 39.9% | 59.0% | 10.2% | 60.3% | 10.7% |
| Nonspecific (n = 107 154) | 79.5% | 4.3% | 0.2% | 29.6% | 44.3% | 1.6% | 32.9% | 0.0% |
| Age group | *** | *** | *** | *** | *** | *** | *** | *** |
| 18–29 Years (n = 22 200) | 75.5% | 18.3% | 10.6% | 27.1% | 66.6% | 13.2% | 32.2% | 5.6% |
| 30–39 Years (n = 26 808) | 76.1% | 19.8% | 10.0% | 27.9% | 61.1% | 11.7% | 36.8% | 3.0% |
| 40–49 Years (n = 40 628) | 79.0% | 22.1% | 8.1% | 31.0% | 57.6% | 9.7% | 43.0% | 2.9% |
| 50–59 Years (n = 64 928) | 78.8% | 23.4% | 6.9% | 35.4% | 54.6% | 8.4% | 45.3% | 2.5% |
| 60–69 Years (n = 53 824) | 79.7% | 18.0% | 2.7% | 36.5% | 44.9% | 3.5% | 41.6% | 1.3% |
| 70–79 Years (n = 42 532) | 77.4% | 13.9% | 0.7% | 37.6% | 42.3% | 0.9% | 42.6% | 1.0% |
| 80–89 Years (n = 30 462) | 78.9% | 12.4% | 0.2% | 33.9% | 37.6% | 0.2% | 44.8% | 0.8% |
| ≥ 90 Years (n = 4186) | 81.3% | 10.1% | 0.0% | 27.8% | 28.4% | 0.0% | 44.3% | 0.4% |
*** p < 0.001; n. s. = Not significant
*1 Diagnosis of depression made by a primary care physician (physician groups 1, 2, 3)
*2 Diagnosis of depression made by a medical specialist in a field such as psychiatry or neurology (physician groups 51, 53, 58, 60, 61)
*3 Diagnosis of depression made by a psychological psychotherapist (physician group 68)
*4 Diagnosis of depression made by another medical specialist (other physician groups)
ATC; Anatomical Therapeutic Chemical Classification System
eTable 2. Overview of billed-for services not subject to an application process.
| EBM No. | Description | Share of all services not subject to an application process (n = 525 271) | Share of patients receiving a service (n = 285 568) |
| 35100 | Differential diagnostic investigation of psychosomatic disease states | 27.3% | 29.9% |
| 35110 | Verbal intervention in psychosomatic disease states | 51.8% | 34.9% |
| 35111 | Exercise interventions, individual therapy | 0.5% | 0.3% |
| 35112 | Exercise interventions, group therapy | 0.2% | 0.0% |
| 35120 | Hypnosis | 0.4% | 0.2% |
| 35130 | Report to the assessor (STT 1 or 2) | 0.1% | 0.2% |
| 35131 | Report to the assessor (LTT) | 0.4% | 0.8% |
| 35140 | Biographical history of the patient | 2.1% | 3.7% |
| 35141 | In-depth exploration | 1.6% | 2.4% |
| 35142 | Surcharge for assessing neurological and psychiatric findings | 0.2% | 0.4% |
| 35150 | Trial session | 4.8% | 3.6% |
| 35151 | Psychotherapeutic consultation hours | 7.4% | 5.9% |
| 35152 | Acute psychotherapeutic treatment | 3.1% | 0.9% |
A total of 525 271 psychotherapeutic services not subject to an application process were billed for according to the EBM in the study population in 2018.
These primarily comprised the differential diagnostic investigation of psychosomatic disease states and verbal intervention in psychosomatic disease states. The percentage of patients receiving the respective service is also shown.
EBM, German Uniform Evaluation Standard (Einheitlicher Bewertungsmaßstab); STT, short-term therapy; LTT, long-term therapy
eTable 4. Drugs prescribed*.
| Drug/active substance class | Share of patients with a prescription in the respective active substance class (n = 285 568) | Share of allantidepressant prescriptions (n = 465 992) |
| Antidepressants: N06A | 42.0% | |
| Other antidepressants: N06AX | 17.1% | 36.9% |
| Selective serotonin reuptake inhibitors: N06AB | 17.7% | 32.4% |
| Non-selective monoamine reuptake inhibitors: N06AA | 14.7% | 29.4% |
| Plant-based antidepressants: N06AP | 0.8% | 0.9% |
| Monoamine oxidase A inhibitors: N06AG | 0.1% | 0.3% |
| Non-selective monoamine oxidase inhibitors: N06AF | < 0.1% | 0.1% |
| Homeopathic/anthroposophic antidepressants: N06AH | < 0.1% | 0.01% |
| Benzodiazepine derivatives: N05BA | 5.8% | Not applicable |
| Antipsychotics: N05A (lithium: N05AN) | 11.3% (0.4%) | Not applicable |
| Combination of antidepressants and antipsychotics: N05A and N06A | 7.6% | Not applicable |
*This overview is based on the codes and designations of the Anatomical Therapeutic Chemical Classification system.
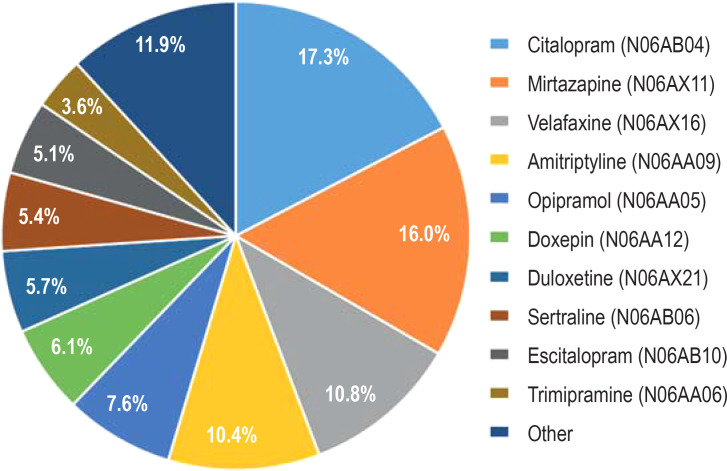
eFigure 2.
Proportion of the respective active substance in all antidepressant prescriptions (ATC code: N06A)
A total of 465 992 antidepressant prescriptions (ATC code: N06A) were documented in the study population in 2018. The most frequently prescribed drugs were citalopram, mirtazapine, and venlafaxine. In all, 59.5% of prescriptions were accounted for by a primary care physician (physician groups 1, 2, 3), 33.0% by medical specialties such as psychiatry or neurology (physician groups 51, 53, 58, 60, 61), and 7.5% by other specialties.
ATC, Anatomical Therapeutic Classification System
Due to the frequent diagnostic vagueness in patients with nonspecific or mild depression, the present analyses focus on patients with moderate or severe depression. Although approximately four out of five patients with moderate (79.2%) or severe depression (82.5%) received treatment in the primary care setting, the proportion of patients receiving treatment from a specialist significantly increased with the severity of the disorder (moderate depression: 25.8%; severe depression: 41.1%). In contrast, there was virtually no difference in the frequencies of treatment by a psychological psychotherapist (moderate depression: 9.7%; severe depression: 9.2%) and the utilization of services not subject to an application process (moderate depression: 55.7%; severe depression: 59.0%) and subject to an application process (moderate depression: 10.6%; severe depression: 10.2%) according to the psychotherapy directive. Furthermore, pharmacological treatment increased with severity. Of those with moderate depression, 48.1% were prescribed an antidepressant at least once, versus 60.3% of patients with severe depression. Primarily patients with severe depression accounted for patients treated for mental illness in the inpatient setting. Thus, of the severely affected patients, 15.7% were treated as inpatients for mental illness and 10.7% for depression. The figures for patients with moderate symptoms were 4.5% (F diagnosis) and 1.4% (depression diagnosis).
Overall, one can be seen that there was a significant difference between genders in terms of how often which services were utilized. While men were more frequently treated by a specialist (p < 0.001), women had more contact with psychological psychotherapists (p < 0.001) and more frequently received services subject to an application process (p < 0.001) as well as not subject to an application process (p < 0.001) according to the psychotherapy directive. Furthermore, it was apparent, as discussed above, that utilization increases in line with severity (all p < 0.001).
Year-on-year change in diagnosis and severity
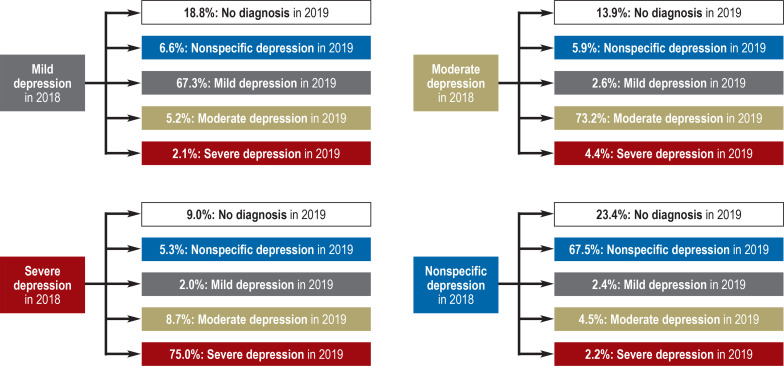
Figure 2 shows the changes in diagnosis and highest-coded disorder severity in the baseline year (2018) compared to the follow-up year (2019).
Figure 2.
Changes in diagnosis or severity in a year-on-year comparison between 2018 and 2019
The figure shows the percentages of patients according to disease severity in 2018 and the changes in diagnosis in 2019. Patients were assigned to the highest-coded level of severity in each year. If the same patient was coded with both specific and nonspecific diagnoses, the specific diagnosis was used as a basis for the classification in the year under consideration. The data basis consists of diagnoses in the outpatient medical sector as well as the inpatient care sector. Example interpretation: Of the patients with mild severity in 2018, 18.8% were diagnosed with no depression in 2019. A total of 67.3% of patients were still coded with a mild depressive disorder. Moderate or severe depression was found in 5.2% and 2.1%, respectively, of patients whose severity level was originally mild; 6.6% of patients received only a nonspecific diagnosis in 2019. The percentage of patients that were affected in 2018 but received no diagnosis in 2019 declined with increasing severity.
Discussion
The present study investigated the characteristics and state of care for patients with a diagnosis of depression on the basis of routine SHI data. Thus, the study complements the current literature with regard to important aspects that need to be taken into consideration in the further development of care. The analysis found an administrative prevalence for depression in 2018 of 17.6%. This is largely in line with other analyses of routine SHI data. For example, the ZI analysis found an administrative prevalence of 15.7% based on outpatient data for the overall German population (6). According to older data, the frequency with which depressive episodes (F32/F33) were diagnosed was 16.3% (7). The analyses also confirmed considerable comorbidity with regard to psychological and somatic disorders.
The current guideline recommends treatment according to severity. Specific principal and secondary symptoms support diagnosis and severity classification. Furthermore, the guideline recommends deploying simple, low-threshold diagnostic tools to assess severity and disease course (19). As severity increases, care intensifies and becomes ever more specialized, as measured by the proportion of patients having contact to specialized treatment providers as well as by the frequency of medication. Nevertheless, care appears to be overall insufficient. For example, only 10% of patients with severe depression receive services that are subject to an application process in line with the psychotherapy guideline, and only 60% of patients were prescribed antidepressants. However, one needs to bear in mind here that some patients refuse pharmacological treatment. The analysis provides evidence that a significant proportion of patients are not treated in accordance with the national treatment guideline (19), which confirms the conclusions drawn in previous studies (11, 12). It is not possible to determine the causes for this on the basis of routine SHI data, but it may be care-related (for example, insufficient diagnostic measures, lack of time), patient-related (for example, refusal of medical or psychotherapeutic treatment), or structural (for example, lack of access to specialists, waiting times). Further studies are required in order to analyze this more closely.
The present study has strengths and weaknesses associated with the use of routine SHI data (8, 20, 21). Its strengths lie in particular in the high case number and the exclusion of the sort of selection effects that occur in surveys. One disadvantage is the lack of information on patient-reported aspects of care, such as the symptoms they experience and their treatment preferences. It is well known that prevalence estimates can differ significantly from systematic surveys, depending on whether they are based on patient-reported medical diagnoses, diagnoses based on standardized instruments, or on routine SHI diagnosis data (22). Furthermore, the validity of depression diagnoses in billing data is judged critically—particularly in the primary care sector—and this needs to be taken into consideration when interpreting the results (11, 22, 23). It is also important to note that the use and appropriateness of the strategy of watchful waiting or low-threshold psychosocial interventions cannot be assessed on the basis of SHI data and may be sufficient for many patients with a mild course. For the outpatient sector, the present study took into account only diagnoses and services provided by office-based physicians, psychotherapists, and institutions that bill using the EBM catalog. Outpatient treatments in hospitals that use a different billing method, such as outpatient departments in psychiatric institutes or university hospitals, were not included. However, this leads to only a slight underestimation of how often services were utilized, since the route to these specialized forms of care is usually via the office-based sector. Likewise, no substances obtained by private prescriptions, most notably no plant-based or homeopathic products, were taken into consideration. SHI data are only able to approximately depict changes in disease severity over time, thereby failing to take into account the episodic nature of the disorder. For more precise results, other research approaches are needed.
The analyses provide insights into the characteristics of and utilization of services by patients with a diagnosis of depression. The results indicate that patients do not always receive treatment in line with guideline recommendations. Therefore, more intensive training needs to be provided in continuing medical education on important aspects such as correct diagnosis, severity estimation, as well as the initiation of guideline-oriented therapy, especially in the primary care sector.
eTable 3. Overview of billed-for services subject to an application process.
| Area | EBM No. | Share of all services subject to an application process (n = 216 089) | Share of patients receiving a service (n = 285 568) |
| Depth psychology-basedpsychotherapy: individual therapy (STT, LTT) | 35100, 35110, 35111 | 39.7% | 2.5% |
| Analytical psychotherapy: individual therapy (STT, LTT) | 35411, 35412, 35415 | 8.8% | 0.2% |
| Behavioral therapy: individual therapy (STT, LTT) | 35421, 35422, 35152 | 46.4% | 3.4% |
| Depth psychology-basedpsychotherapy: group therapy (STT, LTT) | 35503, 35504, 35505, 35506, 35507, 35508, 35509, 35513, 35514, 35515, 35516, 35517, 35518, 35519 | 2.7% | 0.1% |
| Analytical psychotherapy:group therapy (STT, LTT) | 35523, 35524, 35525, 35526, 35527, 35528, 35529, 35533, 35534, 35535, 35536, 35537, 35538, 35539 | 0.6% | 0.02% |
| Behavioral therapy: group therapy(STT, LTT) | 35543, 35544, 35545, 35546, 35547, 35548, 35549, 35553, 35554, 35555, 35556, 35557, 35558, 35559 | 1.9% | 0.1% |
A total of 216 089 services subject to an application process were billed for according to the EBM in the study population in 2018.
These primarily comprised depth psychology-based psychotherapy as individual therapy and behavioral therapy as individual therapy. The percentageof patients receiving the respective service is also shown.
EBM, German Uniform Evaluation Standard (Einheitlicher Bewertungsmaßstab); STT, short-term therapy; LTT, long-term therapy
Acknowledgments
Translated from the original German by Christine Rye.
Footnotes
Conflict of interest statement
Prof. Kahl is a member of the Advisory Board at Janssen/J&J, neuraxpharm, and Takeda. He received lecture fees from Servier, Eli Lilly, Dr. Schwabe, Alexion, Aristo, Berlin Chemie, Janssen, Johnson& Johnson, Otsuka, neuraxpharm, and Takeda. He received study support (third-party funding) from Sevier and Tromsdorff/Ferrer.
The remaining authors declare that no conflict of interests exists.
References
- 1.GBD 2019 Diseases and Injuries Collaborators. global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eden J-L, Konnopka A, König HH. [Costs of depression in Germany— systematic review] Psychiatr Prax. 2021;48:290–300. doi: 10.1055/a-1399-4430. [DOI] [PubMed] [Google Scholar]
- 3.Jacobi F, Höfler M, Siegert J, et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the mental health module of the German health interview and examination survey for adults (DEGS1-MH) Int J Methods Psychiatr Res. 2014;23:304–319. doi: 10.1002/mpr.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobi F, Höfler M, Strehle J, et al. Twelve-months prevalence of mental disorders in the German health interview and examination survey for adults - mental health module (DEGS1-MH): a methodological addendum and correction. Int J Methods Psychiatr Res. 2015;24:305–313. doi: 10.1002/mpr.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bretschneider J, Janitza S, Jacobi F, et al. Time trends in depression prevalence and health-related correlates: results from population-based surveys in Germany 1997-1999 vs 2009 2012. BMC Psychiatry. 2018;18 doi: 10.1186/s12888-018-1973-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steffen A, Thom J, Jacobi F, Holstiege J, Bätzing J. Trends in prevalence of depression in Germany between 2009 and 2017 based on nationwide ambulatory claims data. J Affect Disord. 2020;271:239–247. doi: 10.1016/j.jad.2020.03.082. [DOI] [PubMed] [Google Scholar]
- 7.Stahmeyer JT, Kuhlmann K, Eberhard S. [The frequency of depression diagnoses in different groups of insured persons—a routine data analysis of the years 2006 to 2015] Psychother Psychosom Med Psychol. 2019;69:72–80. doi: 10.1055/a-0581-4785. [DOI] [PubMed] [Google Scholar]
- 8.Ohlmeier C, Frick J, Prütz F, et al. [Use of routine data from statutory health insurances for federal health monitoring purposes] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:464–472. doi: 10.1007/s00103-013-1912-1. [DOI] [PubMed] [Google Scholar]
- 9.Thom J, Bretschneider J, Kraus N, Handerer J, Jacobi F. [Healthcare epidemiology of mental disorders: why is the prevalence not declining despite growing provision of care?] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62:128–139. doi: 10.1007/s00103-018-2867-z. [DOI] [PubMed] [Google Scholar]
- 10.Richter D. [The supposed increase of mental illness—social change and mental health] Psychiatr Prax. 2020;47:349–351. doi: 10.1055/a-1228-9503. [DOI] [PubMed] [Google Scholar]
- 11.Bertelsmann Stiftung (eds.) Faktencheck Gesundheit: Regionale Unterschiede in der Diagnostik und Behandlung von Depressionen. Gütersloh: Bertelsmann Stiftung. 2014 [Google Scholar]
- 12.Trautmann S, Beesdo-Baum K. The treatment of depression in primary care. Dtsch Arztebl Int. 2017;114:721–728. doi: 10.3238/arztebl.2017.0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiegand HF, Saam J, Marschall U, et al. Challenges in the transition from in-patient to out-patient treatment in depression. Dtsch Arztebl Int. 2020;117:472–479. doi: 10.3238/arztebl.2020.0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jaunzeme J, Eberhard S, Geyer S. [How „representative“ are SHI (statutory health insurance) data? Demographic and social differences and similarities between an SHI-insured population, the population of Lower Saxony, and that of the Federal Republic of Germany using the example of the AOK in Lower Saxony] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:447–454. doi: 10.1007/s00103-012-1626-9. [DOI] [PubMed] [Google Scholar]
- 15.Epping J, Geyer S, Eberhard S, Tetzlaff J. [Completely different or quite similar? The sociodemographic structure of the AOK Lower Saxony in comparison to the general and working population in Lower Saxony and the Federal Republic of Germany] Gesundheitswesen. 2021;83:77–86. doi: 10.1055/a-1553-3565. [DOI] [PubMed] [Google Scholar]
- 16.Kleine-Budde K, Müller R, Kawohl W, Bramesfeld A, Moock J, Rössler W. The cost of depression—a cost analysis from a large database. J Affect Disord. 2013;147:137–143. doi: 10.1016/j.jad.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 17.Kassenärztliche Bundesvereinigung. Online-Version des EBM. www.kbv.de/html/ebm.php (last accessed on 11 January 2022) [Google Scholar]
- 18.Gemeinsamer Bundesausschuss. Richtlinie des Gemeinsamen Bundesausschusses über die Durchführung der Psychotherapie. www.g-ba.de/richtlinien/20/ (last accessed on 11 January) [Google Scholar]
- 19.DGPPN, BÄK, KBV, AWMF (eds.) für die Leitliniengruppe Unipolare Depression. Ärztliches Zentrum für Qualität in der Medizin (ÄZQ) Vol. 238. Berlin: 2015. S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression - Langfassung 2nd edition. Version 5. [Google Scholar]
- 20.Neubauer S, Zeidler J, Lange A, von der Schulenburg J-M. Nomos. Baden-Baden: 2017. Prozessorientierter Leitfaden für die Analyse und Nutzung von Routinedaten der Gesetzlichen Krankenversicherung. 1st edition. [Google Scholar]
- 21.Kreis K, Neubauer S, Klora M, Lange A, Zeidler J. Status and perspectives of claims data analyses in German—a systematic review. Health Policy. 2016;120:213–226. doi: 10.1016/j.healthpol.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Grobe TG, Kleine-Budde K, Bramesfeld A, Thom J, Bretschneider J, Hapke U. [Prevalences of depression among adults: comparative analysis of a nationwide survey and routine data] Gesundheitswesen. 2019;81:1011–1017. doi: 10.1055/a-0652-5424. [DOI] [PubMed] [Google Scholar]
- 23.IGES Institut. www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/aerztliche_versorgung/verguetung_und_leistungen/klassifikationsverfahren/9_Endbericht_Kodierqualitaet_Hauptstudie_2012_12-19.pdf (last accessed on 11 January 2022) Berlin: Bewertung der Kodierqualität von vertragsärztlichen Diagnosen. Eine Studie im Auftrag des GKV-Spitzenverbands in Kooperation mit der BARMER GEK. [Google Scholar]