Abstract
Background:
Self-management interventions for adolescent and young adult survivors of childhood cancer (AYA) are needed. The present study reports on the acceptability and feasibility of delivering survivorship care plans (SCPs) and an accompanying app to AYA.
Procedure:
AYA (n=224) ages 15–29 who completed treatment for cancer were randomized and received a digital SCP only or an SCP plus a mobile app intended to enhance self-management. For 16 weeks, the app delivered 1–2 daily messages complementing information in their SCP and tailored based on age, treatment and health goal. Data are presented on feasibility, self-reported acceptability (including satisfaction and perceived benefits) and its relationship to app engagement (for those in app group), and feedback from qualitative interviews conducted with 10 AYA.
Results:
The SCP and app proved feasible as evidenced by high recruitment and retention, access to technology, time analysis, moderate app engagement, and minimal technical issues. However, 12% reported never reading the SCP and 8% never used the app. The App and SCP were acceptable to AYA and SCP acceptability ratings did not differ between groups. For those with the app, acceptability was positively related to message engagement. AYA recommended enhanced individualization and design features of the SCP and app.
Conclusions:
Results support the use of tailored SCPs and mobile health interventions for most AYA, as well as the need for further refinement and research. Delivery of SCPs and digital interventions are acceptable and feasible to AYA survivors and may help promote health-related knowledge and survivorship self-management.
Keywords: Survivorship care plan, cancer survivor, adolescents and young adults, self-management, digital health
Few interventions to improve self-management of adolescent and young adult (AYA) cancer survivors exist1. To address this gap, we combined two digital health interventions: 1) survivorship care plans (SCPs) and 2) a mobile health (mHealth) app with delivery of tailored mobile messages. The goal of this efficacy trial was to test the impact of the app and the SCP on self-management versus delivery of an SCP alone, via a randomized controlled trial (RCT) known as AYA Self-management via Texting, Education & Plans for Survivors (AYA STEPS). While we previously reported on the intervention development2, and with longer-term efficacy outcomes pending, we aim to provide generalizable knowledge on feasibility and acceptability of this digital health RCT to improve self-management of AYA survivors.
While SCPs have been integrated into adult oncology standard of care, few studies have described their use in pediatrics3,4. SCPs are documents that report on health risks (i.e., late effects) and recommendations for follow-up care, health promotion, and well-being5. SCPs for AYA may be especially important given AYA are assuming more responsibility for health care, may lack adequate knowledge of their childhood cancer history and possible late effects6–9, report reduced health-related quality of life10, and are at risk for suboptimal health behaviors11,12. Despite the potential value of SCPs for AYA, fewer than half of childhood cancer survivors receive an SCP13–16, and acceptability and feasibility of delivering and using SCPs with AYA has received little attention.
In addition to SCPs, mHealth interventions utilizing texting, app-based, or web-based platforms represent a promising strategy for delivering important information to AYA survivors17. Although there are increasing studies showing mHealth interventions for AYA survivors to be feasible and acceptable18, few have targeted health knowledge and self-management19,20, few are tailored to patient treatment history, and no RCTs have evaluated the feasibility and acceptability of incorporating SCPs into an app, which may have more appeal to AYA than a paper copy.
Taken together, there is a critical need to understand if AYA are receptive to SCPs and tailored mHealth interventions designed to deliver personalized health-related information and promote self-management, in addition to the feasibility of delivering such tailored interventions. We expected the AYA STEPS intervention to be feasible and acceptable for AYA survivors. We also expected SCP acceptability ratings to be greater for those randomized to receive the SCP plus app versus SCP alone due to the supportive text messages and ease of SCP access via the app-based platform. Given prior findings on the variability of engagement in the app21, we also explored whether acceptability ratings were associated with app engagement for those randomized to receive the app.
Methods
The study was IRB-approved from the two study sites-- a pediatric cancer center and the partnering adult academic cancer center--and was registered at clinicaltrials.gov (NCT03363711). Details of the intervention development were previously reported2. Informed consent was obtained from AYA or from parent/guardian (for AYA <18 years old).
Screening and Recruitment
Participants were screened through electronic health record (EHR) review and confirmed eligible by a member of their medical team. AYA were eligible if they were 15–29 years old, cognitively capable to complete study surveys/procedures, treated for pediatric cancer (and not just with surgery) and currently off treatment and in remission, and receiving follow-up care at the study sites. AYA who consented chose one of seven health goals (i.e., physical activity, smoking cessation, sleep, nutrition, social connection, school or work productivity) to consider for the duration of the study2. They then completed a baseline survey and were subsequently randomized to receive either the app and embedded SCP or SCP only.
SCP Creation
SCP-specific treatment summaries containing relevant treatment information (e.g., types and doses of chemotherapy, radiation location, etc.) were first created to later populate individualized digital SCP fields. For most patients followed in the Cancer Survivorship Program (CSP), consolidated clinic summaries of treatments already existed and additional relevant information was extracted to create the SCP-specific treatment summary. If there were no existing treatment summaries, they were created by study staff via EHR review and approved by providers. Treatments were then entered into the digital SCP generator (Smart Adult Living After Childhood Cancer; Smart-ALACC). Smart-ALACC (smartalacc.oncolink.org) was adapted for AYA survivors from OncoLife (Oncolink.org), a free Internet-based SCP generator for adult cancer survivors 3. The SCP was emailed and delivered in person (for those recruited in person) to all participants and housed in the app (for those in the app group).
Intervention Procedures
The 16-week intervention consisted of delivery of an SCP to all participants, as well as a mHealth app for those randomized to the app group. Once randomized, staff oriented AYA to their SCP (everyone) and downloaded and reviewed the app (app group only). The app was modified from an existing LifeScience Technologies (LST) HIPAA-compliant disease self-management app (m.Care).
The intervention was tailored, in that SCPs were specific to a patient’s treatment history and daily mobile messages delivered through the app reflected tailored information relevant to the SCP and characteristics of the patients (e.g., age, health goal)2. The goal of the app was to improve knowledge and self-management, including uptake of SCP recommendations and health promotion. The app delivered 1–2 messages per day that were the main component of the mHealth intervention. These messages covered topics such as monitoring for late effects, general health and follow-up, social competence, emotional support, positive health behaviors, and survivorship stories. Some messages contained links to relevant online resources (e.g., American Cancer Society tips for being healthy after treatment, physical activity guidelines, etc.) or informational videos (e.g., beginner yoga, life after cancer, etc.). Approximately 40% were interactive and elicited participant engagement such as texting back responses to quiz and survey questions, or clicking “here” if wanting more information. If participants responded, the app sent an automated answer relevant to their response or request for more information. Participants earned points for responding to interactive messages and completing weekly surveys regarding goal progress and medication adherence if applicable, which could be redeemed for up to two $10 gift cards. The app also contained components for self-management that included the SCP and relevant applets (diet tracker, exercise tracker, step counter) for AYA to utilize and to refer back as desired. AYA could enter information (e.g., foods, exercises, steps) into the applets manually or sync them with a 3rd party application (i.e., FitBit, Apple Health). Staff attempted to contact all app group participants via phone, text, and/or email at two weeks to ensure that the app was functioning as expected. App engagement was monitored through the LST monitoring website. Participants who were inactive in the app for two consecutive weeks were contacted.
Measures
Via REDCap22, participants completed online questionnaires at baseline, 4 months (immediately post intervention) and 8 months.
Demographics and Electronic Health Record Review
At baseline, participants self-reported demographics (e.g., gender, race, ethnicity), smartphone ownership, and current data plan. EHR review ascertained age, cancer diagnosis, age at diagnosis, relapse or second cancer diagnosis, and date off treatment. Intensity of treatment was rated on a 4-point scale based on established guidelines23 by two oncologists.
Feasibility
Feasibility was assessed via tracking participant recruitment and retention at 4 and 8-month follow-ups, smartphone ownership and data plans, SCP time demand (time to create an SCP-specific treatment summary, build the SCP, review the SCP) as well as SCP engagement (self-reported reads). Additional indices for the app group included time to orient to the app, self-reported and objective engagement in the app, and logistical and technical difficulties. We examined three main objective measures of app engagement (percentage mobile messages read, number of SCP views and percentage of days active). Secondary app engagement outcomes included percentage of responses to weekly goal and adherence surveys and interactive messages, and number of participants making applet entries. App participants self-reported the extent to which they were able to access the app/messages and reason for any app interruptions. Logistical/technical difficulties reported to the study team were also noted.
Acceptability
Following theoretical frameworks informing AYA STEPS2,24,25 and recommended components of acceptability26, acceptability focused on participant satisfaction and perceived benefits, including ease of use; perceived gains of knowledge, health and quality of life; perceived efficacy; and impact on health motivation. App-specific acceptability included additional items pertaining to perceived benefits and desire to continue app access.
Quantitative.
Items were assessed on a 5-point scale from 1 (never/not at all, 0%) to 5 (completely, 100%). Consistent with our previous mHealth pilot27, endorsement was defined as agreeing at least somewhat (3, 50%), indicating at least moderate perceived benefit/satisfaction.
Qualitative.
The acceptability questionnaire elicited open-ended suggestions for SCP improvement. The app group received three additional open-ended questions asking for suggested improvements to the mobile app, the messages, and the applets. A convenience sample of 10 AYA from the app group also participated in semi-structured interviews to further assess acceptability.
Data Analysis
Sample size calculations were based on calculations of 80% power to detect change in the primary efficacy outcome of patient knowledge (to be reported in future paper). Those randomized to the app were compared to those in the SCP only group on demographic, treatment, and SCP engagement and acceptability ratings using t-tests and chi-squares. Feasibility outcomes were summarized descriptively, with app-specific outcomes summarized for the app group only. Self-reported indices of acceptability, as measured via questionnaire, were summarized as overall means and as the percentage of respondents who responded with a 3–5 (agreeing “somewhat” through “completely”). Qualitative responses to open-ended questions and interviews were coded into themes by two independent raters, with team members discussing final consensus. As app utilization was variable (0–100% engagement)21, exploratory analysis utilized Spearman’s non-parametric rank correlation to examine if acceptability ratings for the app group were associated with objective app engagement.
Results
Participants
A total of 224 AYA (see Table 1 for characteristics) completed baseline measures and were randomized. There were no significant demographic or treatment differences between groups. The qualitative app group subsample (n=10) was on average 19.7 (SD=3.3) years old, 50% male and 80% non-Hispanic white. Five had a blood cancer diagnosis, 4 had a solid tumor, and 1 had a brain tumor. Similar to the larger sample, this was a moderately engaged, yet variable, subsample, with 72.4% (SD=34.0, Range=11.5–100%) active app days, 60.4% (SD=42.3, Range=0–99.4%) messages read and 60.0% viewing their SCP in the app at least once.
TABLE 1:
Participant characteristics
| App Group (n=110) | SCP only Group (n=114) | t | p | |
|---|---|---|---|---|
| Age (Mean(SD)) | 20.5(3.5) | 20.2 (3.0) | 0.7 | 0.48 |
| Age at Diagnosis | 9.8(6.5) | 9.5(6.1) | 0.31 | 0.75 |
| Months on Treatment M(SD) | 19.9(24.1) | 17.4(18.3) | 0.9 | 0.40 |
| Years off treatment M(SD) | 8.6(5.6) | 8.8(5.7) | 0.3 | 0.78 |
| χ2 | p | |||
| Female, n(%) | 47 (43%) | 58 (51%) | 0.5 | 0.22 |
| Racial or ethnic minority, n(%) | 33 (30%) | 29 (25%) | 0.6 | 0.45 |
| Primary cancer diagnosis | 1.1 | 0.58 | ||
| Leukemia/Lymphoma n(%) | 57 (52%) | 67 (59%) | ||
| Solid Tumor n(%) | 43 (39%) | 38 (33%) | ||
| Brain Tumor n(%) | 10 (9%) | 9 (8%) | ||
| Intensity of Treatment Rating | 1.9 | 0.59 | ||
| 1 n(%) | 1 (0.9%) | 0 (0%) | ||
| 2 n(%) | 36 (32.7%) | 34 (29.8%) | ||
| 3 n(%) | 41 (37.3%) | 50 (43.9%) | ||
| 4 n(%) | 32 (29.1%) | 30 (26.3%) | ||
| Had relapse or second cancer n(%) | 23(20.9%) | 15 (13.2%) | 2.4 | 0.09 |
SCP = survivorship care plan
Feasibility (Entire sample)
Recruitment and Retention (See Fig. 1)
Figure 1:
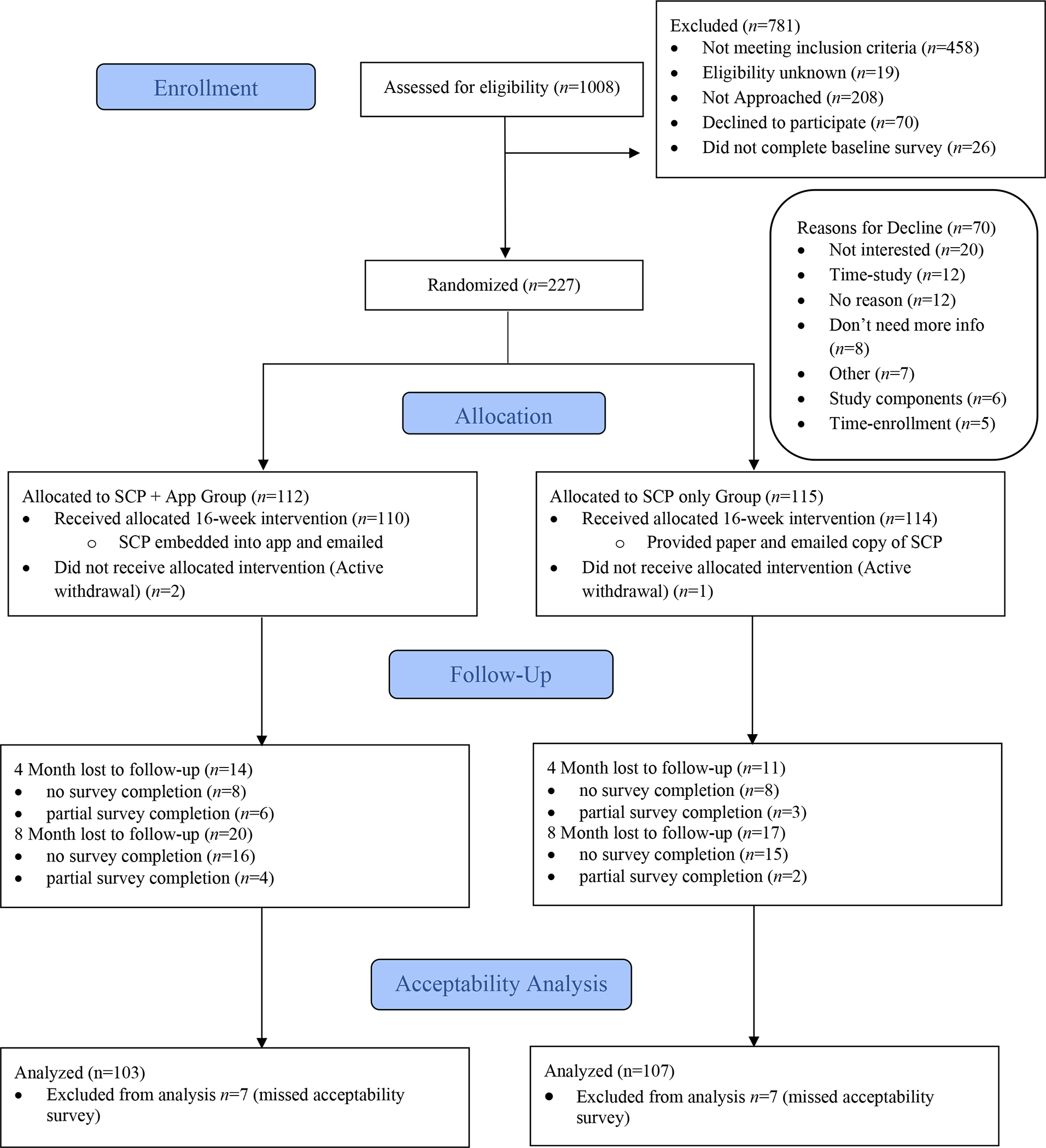
AYA STEPS CONSORT Flow Diagram
AYA STEPS = Adolescent and Young Adult Self-management via Texting, Education & Plans for Survivors; SCP = survivorship care plan
Of the 323 AYA approached, 253 (78%) consented and 227 (90% of those consented) completed baseline measures and were randomized to the app (n=112) or the SCP only (n=115). With three withdrawals after randomization, the final baseline sample was 224 (n=110 app group, n=114 SCP only group). Of this final sample, 199 (89%) and 187 (83%) completed follow-up surveys at 4 and 8 months, respectively.
Smart Phone Ownership/Data Plans.
All app participants downloaded the app and only one needed a phone to be provided. The majority (81%) owned an iPhone and 18% owned an Android. Forty percent had an unlimited data plan and only one participant did not have a data plan.
SCP Time demand.
On average, it took approximately half an hour for study staff to create, build, and review the SCPs with each participant (see Table 2). Of note, creating the SCP-specific treatment summaries took approximately half the time for patients from the CSP with existing consolidated treatment summaries compared to those from other clinics that required a more lengthy EHR review to extract all SCP-relevant treatment information.
TABLE 2:
Survivorship care plan time demand
| M | SD | Range | n | |
| SCP-specific treatment summary creation (min) | 15.1 | 11.0 | 2–50 | 164 |
| CSP (min) | 10.8 | 9.4 | 2–50 | 102 |
| Non-CSP (min) | 22.1 | 9.7 | 7–48 | 62 |
| SCP build (min) | 9.7 | 7.6 | 1–60 | 198 |
| SCP review (min) | 5.8 | 3.8 | 2–25 | 188 |
| Total SCP time demand (min) | 32.7 | 14.9 | 6–112 | 124 |
SCP = survivorship care plan.
CSP = cancer survivorship program
SCP Engagement.
Twenty-four (11.6%) participants reported never reading their SCP during the intervention, 151 (72.9%) reported reading it once or twice, 21 (10.1%) read it once a month, 10 (4.8%) read it once a week and one read it once per day. Participants in the app group self-reported reading their SCP more than the SCP only group (t=2.4, p=.02).
Feasibility (App group only)
App Orientation Time Demand.
Orienting participants to the app took an additional 6.7 minutes on average (SD=5.1, Range=0–35 min).
Self-reported App Engagement.
Eight (8%) AYA reported not using the app. Half (50%) of the participants reported ignoring a message sometimes or more. Of those who self-reported reading any of the messages (92%), 66% reported clicking on the links/resources in the messages at least sometimes. Applets were less utilized, with only 18% of participants reporting using them at least sometimes.
Objective App Engagement.
As previously reported21, objective app data showed that participants were active in the app an average of 59.8% days (SD=37.2, Range=0–100%), and read an average of 63.1% of the messages (SD=39.9, Range=0–100%). SCP components were viewed in the app on average 3.3 times (SD=4.4, Range=0–20) and on an average of 1.5 days (SD=1.9, Range=0–8), with 61.9% viewing the SCP in the app at least once. Percent messages read and percent active app days were significantly associated with SCP view days in the app (rs=0.49, p<0.01, and rs=0.38, p<0.01, respectively). On average, participants responded to 50.7% (SD=38.8, Range=0–100%) of interactive mobile messages, 41.5% (SD=35.9, Range=0–100%) of weekly adherence surveys, and 41.6% (SD=36.0, Range=0–100%) of weekly goal surveys. This engagement resulted in 32 participants (29.1%) earning both gift cards and 17 (15.5%) earning one gift card. The applets were underutilized with only 12 (10.9%) and 13 (11.8%) AYA making nutrition or physical activity entries, respectively.
App Issues and Interruptions
Fifty (45%) participants in the app group had at least 2 weeks of inactivity and were attempted to be contacted. In the post-intervention survey, 25 participants reported that they did not have access to the app for the whole study. Self-reported reasons for app interruptions included losing the app (n=11, 11%), deleting the app (n=1, 1%), technical problems (n=6, 6%), or not wanting to use it anymore (n=7, 7%).
Acceptability
Most AYA [n=207 (92%); 101 app group, 106 SCP only group] completed acceptability questions at 4 months. Three participants completed acceptability items at the 8-month time point due to missing the 4-month acceptability survey, leaving a final sample of 210 (94%; 103 app group, 107 SCP only group) included in the acceptability analyses.
SCP Acceptability
Quantitative Survey Feedback.
AYA were satisfied with the SCP, with no difference between acceptability ratings or health related motivations found between groups (see Table 3). The most common reported reasons for using SCPs were to remind participants of their own risks and ways to be healthy, and less so for sharing information with others (providers, friends, school/work).
TABLE 3:
Survivorship care plan acceptability and health-related motivations: Total and comparison between those in SCP only group versus SCP plus app group.
| Item | Total sample | App group | SCP only group | ||
|---|---|---|---|---|---|
| SCP Acceptability | Endorsementa | M(SD) | M(SD) | t | p |
| Improved knowledge of health | 85.5% | 3.8 (1.1) | 3.8 (1.2) | 0.1 | 0.96 |
| Easy to find | 84.9% | 4.0 (1.2) | 3.8 (1.2) | 1.3 | 0.21 |
| Increased awareness of ways to be more healthy | 74.6% | 3.4 (1.2) | 3.2 (1.3) | 1.0 | 0.32 |
| Positive impact on QOL | 68.9% | 3.1 (1.2) | 3.3 (1.2) | 0.7 | 0.46 |
| Helped achieve health goal | 50.5% | 2.6 (1.3) | 2.5 (1.1) | 0.6 | 0.53 |
| Improved physical health | 47.4% | 2.7 (1.2) | 2.4 (1.3) | 1.4 | 0.16 |
| Information in SCP made me feel overwhelmed/scared | 24.1% | 2.0 (1.2) | 1.7 (0.9) | 2.0 | 0.05 |
| Reported Reasons for using SCP | % selected | % selected | % selected | χ2 | p |
| Remind what to do to stay healthy | 51.2% | 48.0% | 54.2% | 0.8 | 0.41 |
| Remind of risks for other diseases | 50.2% | 52.0% | 48.6% | 0.2 | 0.68 |
| Lower stress/worry about health | 28.2% | 32.4% | 24.3% | 1.7 | 0.22 |
| Share information with providers | 23.9% | 23.5% | 24.3% | <0.1 | 0.99 |
| Share information with friends/family | 23.0% | 20.6% | 25.2% | 0.6 | 0.51 |
| Prepare for doctor’s appointment | 19.1% | 20.6% | 17.8% | 0.3 | 0.73 |
| Did not use SCP | 14.4% | 14.7% | 14.0% | <0.1 | 0.99 |
| Share information with school/work | 10.5% | 9.8% | 11.2% | 0.1 | 0.82 |
| Health-Related Motivations | Endorsementa | M(SD) | M(SD) | t | p |
| Motivated to improve general health behaviors | 79.7% | 3.4 (1.1) | 3.5 (1.1) | 0.8 | 0.41 |
| Motivated to follow recommendations in SCP | 76.0% | 3.3 (1.2) | 3.4 (1.2) | 0.2 | 0.87 |
| Motivated to improve medical habits | 76.0% | 3.4 (1.2) | 3.6 (1.2) | 1.3 | 0.20 |
| Motivated to seek more information about health/well-being | 73.9% | 3.1 (1.4) | 3.4 (1.2) | 1.8 | 0.07 |
| Motivated to find/use supportive services | 52.7% | 2.8 (1.3) | 2.6 (1.4) | 1.2 | 0.22 |
SCP = Survivorship care plan; QOL = quality of life;
Endorsement represents agreeing “somewhat” (3, 50%) through “completely” (5, 100%)
Qualitative Survey Feedback.
Top suggestions for SCP improvement included: no changes (37%), SCP content (32%), and accessibility (12%). More tailored/personalized information relating to their diagnosis, treatment, health risks and/or goals (16%) was the most endorsed content update.
App Acceptability
Quantitative Survey Feedback.
The majority (>50%) of participants found the app and messages to be at least moderately acceptable with varying perceived benefits (see Table 4). The items with the greatest endorsement (>75%) pertained to satisfaction with app use and message content, perceived knowledge benefits, and desire to continue use and/or recommend to other survivors. Acceptability ratings with <50% endorsement related to perceived social benefits of the app, satisfaction with the applets, and feelings of being overwhelmed or scared. For those reporting that the app helped them achieve their health goal at least a little (n=77, 83%), top reasons why included: obtained useful information about being healthy (n=48), reminded to take care of health (n=37), and increased motivation to be healthy (n=36). Among those that read the messages, the majority (60%) reported that the number of messages was “just the right amount”, 14% wanted more and 26% felt there were too many.
TABLE 4:
App acceptability ratings post-intervention (App group reporting on app)
| Item | Endorsementa | Mean (SD) |
|---|---|---|
| App Acceptability | ||
| Would recommend to other survivorsb | 86.0% | 3.9 (1.1) |
| Increased awareness of ways to be more healthy | 83.0% | 3.7 (1.1) |
| Improved knowledge of health | 81.7% | 3.6 (1.2) |
| Perceived obtained more knowledge than others | 78.9% | 3.5 (1.3) |
| Would continue app use in futureb | 78.0% | 3.4 (1.2) |
| Ease of app use | 77.1% | 3.4 (1.3) |
| Related to my own experiences | 72.3% | 3.2 (1.2) |
| Provided new information not discussed with providers | 71.3% | 3.4 (1.3) |
| Felt like others had similar experiences | 69.5% | 3.2 (1.3) |
| Positive impact on quality of life | 68.8% | 3.1 (1.3) |
| Helped achieve health goal | 62.4% | 3.0 (1.3) |
| Perceived better physical health than others | 57.6% | 2.9 (1.4) |
| Perceived better emotional health others | 55.4% | 2.9 (1 4) |
| Improved emotional health | 51.1% | 2.6 (1.3) |
| Improved physical health | 50.0% | 2.6 (1.3) |
| Felt connected to others | 47.4% | 2.6 (1.4) |
| Improved social life | 25.5% | 1.9 (1.2) |
| Information in app made feel overwhelmed/scared | 21.3% | 1.8 (1.3) |
| Acceptability Specific to Messages in App | ||
| Messages easy to understand | 90.3% | 4.2 (1.0) |
| Satisfied with message content variety | 87.9% | 3.7 (1.0) |
| Easy to access messages | 78.5% | 3.8 (1.3) |
| Easy to make time to read messages | 76.3% | 3.6 (1.3) |
| Messages were useful | 75.3% | 3.4 (1.2) |
| Links/resources in messages helpful/interesting | 74.2% | 3.3 (1.0) |
| Looked forward to messages | 55.9% | 2.8 (1.3) |
| Acceptability Specific to Applets in App | ||
| Applets helpful/interesting | 34.7% | 2.1 (1.2) |
Endorsement represents agreeing “somewhat” (3, 50%) through “completely” (5, 100%)
scale was from “definitely not” (1) to “definitely yes” (5), endorsement represents at least maybe (3)
Qualitative Survey Feedback.
Suggested app improvements included: improving user interface (e.g., navigation, layout; 42%) and fixing technical issues (e.g., notifications, loading delays, app crashes; 21%). Suggested message improvements were varied, but requests for updated message content (28%), particularly more personalized content, was the most frequent recommendation. Regarding applets, for those that used them and provided feedback (9%), improvements to the user interface were most common (20%), with an additional 12% indicating integration with external apps could be improved.
Qualitative Interviews.
The 10 participants were generally satisfied with the app and felt that it helped to motivate them to achieve their health goal and gain new knowledge or remember forgotten information. Eight AYA reported regular app use, two indicated declining engagement over time and one participant only used it to seek out information. Engagement was best facilitated by notifications/prompts and trivia-style messages, whereas barriers included technical issues and competing priorities. Although 80% indicated they would continue using the app in the future, the general preference was to use it less than daily.
Association Between Objective App Engagement and Acceptability Ratings
App engagement (particularly percent messages read) was generally positively correlated with app acceptability ratings (see Table 5). Specifically, percent messages read was associated with message acceptability (e.g., easy to access/understand the messages) (rs=0.29 to 0.48, p<0.001), continuing to use the app in the future (rs=0.42, p<0.001) and likelihood to recommend the app to other cancer survivors (rs=0.37, p<0.001). The associations between active app days and acceptability were more varied. App engagement was not associated with SCP acceptability, with the exception of those who read more messages rated their SCP as easier to find (rs=0.24, p=0.02).
Table 5:
Association between objective app engagement and acceptability ratings for participants in the app group
| App Acceptability | r s | r s |
|---|---|---|
| Would continue app use in future | 0.42 ** | 0.19 |
| Would recommend to other survivors | 0.37 ** | 0.19 |
| Feel like others had similar experiences | 0.34 ** | 0.23 * |
| Perceived obtained more knowledge than others | 0.33 ** | 0.12 |
| Ease of app use | 0.32 ** | 0.23 * |
| Related to my own experiences | 0.30 ** | 0.21 * |
| Improved awareness of new healthy habits | 0.30 ** | 0.14 |
| Information in app made feel overwhelmed/scared | −0.26 * | −0.04 |
| Positive impact on quality of life | 0.23 * | 0.16 |
| Improved knowledge of health | 0.21 * | 0.17 |
| Perceived better emotional health others | 0.21 * | −0.03 |
| Perceived better physical health than others | 0.20 | −0.04 |
| Feel connected to others | 0.18 | 0.12 |
| Helped achieve health goal | 0.15 | 0.09 |
| Improved social life | −0.08 | −0.01 |
| Improved emotional health | 0.06 | 0.14 |
| Improved physical health | −0.04 | 0.07 |
| Provided new information not discussed with providers | 0.04 | 0.06 |
| Message Acceptability | ||
| Messages easy to understand | 0.48 ** | 0.26 * |
| Messages were useful | 0.41 ** | 0.27 * |
| Easy to access messages | 0.40 ** | 0.25 * |
| Easy to make time for messages | 0.40 ** | 0.17 |
| Satisfied with message content variety | 0.36 ** | 0.35 ** |
| Links/resources in messages helpful/interesting | 0.36 ** | 0.36 ** |
| Looked forward to messages | 0.29 ** | 0.17 |
| Applet Acceptability | ||
| Applets helpful/interesting | 0.22 | 0.27 * |
| SCP Acceptability | ||
| Easy to find | 0.24 * | 0.14 |
| Information made me feel overwhelmed/scared | −0.17 | 0.03 |
| Improved knowledge of health | 0.11 | 0.15 |
| Positive impact on QOL | 0.06 | 0.05 |
| Improved awareness of new ways to be healthy | 0.06 | 0.04 |
| Helped achieve my health goal | 0.02 | 0.09 |
| Improved Physical Health | −0.02 | 0.03 |
| Health-related Motivations | ||
| Motivated to improve medical habits | 0.22 * | 0.21 * |
| Motivated to follow recommendations in SCP | 0.21 * | 0.17 |
| Motivated to improve my general health behaviors | 0.17 | 0.16 |
| Motivated to seek more information about health/well-being | 0.16 | 0.25 * |
| Motivated to find/use supportive services | 0.04 | 0.14 |
SCP = Survivorship care plan; QOL = quality of life
=p<0.05
p<0.01
Discussion
This study filled an important gap, addressing the paucity of evidence related to the feasibility and acceptability of SCPs or accompanying mHealth interventions targeting self-management among AYA survivors of childhood cancer. This RCT successfully delivered SCPs to a relatively large sample of AYA either in a stand-alone format or through a tailored mobile app with daily supporting messages. The trial was feasible and both the SCP and accompanying AYA STEPS app and messages were an acceptable way to receive health information.
The AYA STEPS intervention had high retention (>85%) and high SCP uptake (88% read at least once). Further, this study demonstrated that SCP delivery to AYA survivors by non-clinical staff using a digital SCP generator is feasible with an average time of 32 minutes, thus challenging prior arguments of time being a barrier to SCP use. 15,28–30 As demonstrated, having a complete and accessible treatment summary as part of clinical care, as recommended by the Institutes of Medicine and American Society of Clinical Oncology31,32, should significantly reduce the time to create an SCP. The use of an app to support SCP uptake was also highly feasible with AYA having virtually ubiquitous smartphone ownership, all willing and able to download the app, and minimal time required for app orientation. App engagement was variable, with the average views of the app and percent of messages read around 60%. Less than half of our participants earned a gift card for engagement, suggesting that more variable amounts or types of incentives may be more effective. Engagement is a common challenge in mHealth research33, and increasingly recognized as an important determinant of efficacy34,35.
The positive relationship between engagement and acceptability was more robust for percentage of messages read than active app days. This is consistent with our intention for messages to be the most prominent and important intervention component and supports the intention for AYA to benefit more with increasing attention to the mobile messages. It is also plausible that those who found the messages more impactful at the onset were more likely to continue reading them throughout the intervention. The app group self-reported engaging with their SCP slightly more than the SCP only group, which may have been facilitated through app notifications or ease of access. As SCP engagement may be an important predictor of SCP effectiveness, delivering SCPs through an app with appropriate notifications may be a feasible way to increase the intended efficacy of SCPs and track actual usage. Forthcoming results from this trial will determine if levels of engagement with the app, messages and/or SCP impact efficacy.
In line with our study pilot2, participants were satisfied with the app and messages, found the app to be valuable and helpful, and would recommend it to other survivors. An updated user interface and resolving technical glitches would further improve app satisfaction. Social connectedness was the least endorsed benefit of the app. Although some tips and resources to enhance social connectedness were provided through the messages, the app did not facilitate peer connections, thus limiting perceived social benefits. Contrary to expectations, the app did not enhance SCP acceptability. This may be because both groups received a digital SCP via email which could have reduced accessibility barriers for the SCP only group. Although both the SCP and message content were tailored to each participant, AYA desired further personalization and customization.
Perceived gains to knowledge, health awareness, and motivation to improve health were the most endorsed benefits of both the app and SCP. The literature on the knowledge benefits of SCPs has been largely inconclusive30, and we plan to provide further objective data on knowledge gains with our pending post-intervention efficacy data. Regardless, these preliminary findings are promising as increasing knowledge, awareness, and motivation may be a precursor to better health behaviors and outcomes24, including better indices of self-management, for AYA survivors. Indeed, we plan to evaluate further efficacy outcomes to ascertain if these self-reported benefits translated to better self-management at 14 months post enrollment.
Despite the promising results, there are limitations to note. For one, there was not a true control group, as both groups received tailored SCPs. Second, despite a pilot phase, unanticipated technical problems remained and were a barrier to engagement, thus impacting feasibility and, possibly, acceptability. Third, brain tumor survivors were slightly underrepresented due to higher rates of cognitive impairment excluding them from participation. Finally, most of the AYA enrolled were participants already engaged in survivorship care, and it is possible the benefits of the SCP and app may differ for cancer survivors who are disengaged from follow-up care. Existing evidence suggests that those engaged in survivorship care tend to have greater knowledge of their cancer history and health risks9. The perceived and actual benefits of digital delivery of SCPs and/or mobile health apps may therefore be greater for disengaged AYA with lower baseline knowledge and more barriers to engaging in the health care system.
Results provide support for the use of digital tailored AYA SCPs, especially the open-access Smart-ALACC and related mHealth interventions to enhance uptake, as well as the need for further refinement and research. The creation and delivery of SCPs is only feasible if the integration into clinical care is supported within the local clinic “culture” and treatment summaries needed to create digital SCPs become more readily available and/or automated through the EHR. Although the app is not publicly available, Smart-Alacc is open-access and can be used by anyone (patient, lay person, provider) to quickly populate and create an SCP. In the absence of an available app, more accessible text message platforms can be used to deliver text messages to reinforce SCP content.
Further implementation research is needed to determine facilitators and barriers of incorporating SCPs into standard of care in pediatric cancer. To address mHealth disengagement and/or habituation, it will be important for future research to be agile in terms of improving upon technology, algorithms and platforms, and incentivization strategies tailored to AYA. Results from the current AYA STEPS trial will demonstrate the impact of SCPs and the related self-management app intervention on important outcomes for AYA survivors, such as knowledge of heath and adherence to SCP recommendations. Future research should determine the benefits of digital health interventions on longer-term survivorship health outcomes (e.g., sustained engagement in follow-up care, adherence to screening and preventative health behaviors), as well as extend such research to those disengaged from follow-up care.
Acknowledgements:
The trial was supported by a Centers for Disease Control and Prevention Special Interest Project grant (Award #: U48DP005053, SIP #: 15–001). The authors would like to sincerely thank the adolescent and young adults and their caregivers who participated in the study and our technology partners at LifeScience Technologies.
Abbreviations Key
- AYA
Adolescent and young adult
- AYA STEPS
Adolescent and Young Adult Self-management via Texting, Education & Plans for Survivors
- CSP
Cancer Survivorship Program
- EHR
Electronic health record
- LST
LifeScience Technologies
- mHealth
Mobile health
- RCT
Randomized controlled trial
- SCP
Survivorship care plan
- Smart-ALACC
Smart Adult Living After Childhood Cancer
Footnotes
Conflict of Interest Statement: The authors declare that they have no conflict of interest.
Data Availability Statement:
Data is available upon request from the corresponding author.
References
- 1.Kobe CM, Turcotte LM, Sadak KT. A Narrative Literature Review and Environmental Scan of Self-management Education Programs for Adolescent and Young Adult Survivors of Childhood Cancer. J Cancer Educ Off J Am Assoc Cancer Educ. 2020;35(4):731–735. doi: 10.1007/s13187-019-01520-7 [DOI] [PubMed] [Google Scholar]
- 2.Schwartz LA, Psihogios AM, Henry-Moss D, et al. Iterative development of a tailored mHealth intervention for adolescent and young adult survivors of childhood cancer. Clin Pract Pediatr Psychol. 2019;7(1):31–43. doi: 10.1037/cpp0000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szalda D, Schwartz L, Schapira MM, et al. Internet-Based Survivorship Care Plans for Adult Survivors of Childhood Cancer: A Pilot Study. J Adolesc Young Adult Oncol. 2016;5(4):351–354. doi: 10.1089/jayao.2016.0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szalda D, Schapira MM, Jacobs LA, et al. Survivorship Care Planning for Young Adults After Cancer Treatment: Understanding Care Patterns and Patient-Reported Outcomes. J Adolesc Young Adult Oncol. 2018;7(4):430–437. doi: 10.1089/jayao.2017.0112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Earle CC. Failing to plan is planning to fail: improving the quality of care with survivorship care plans. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(32):5112–5116. doi: 10.1200/JCO.2006.06.5284 [DOI] [PubMed] [Google Scholar]
- 6.Henderson TO, Friedman DL, Meadows AT. Childhood cancer survivors: transition to adult-focused risk-based care. Pediatrics. 2010;126(1):129–136. doi: 10.1542/peds.2009-2802 [DOI] [PubMed] [Google Scholar]
- 7.Kadan-Lottick NS, Robison LL, Gurney JG, et al. Childhood cancer survivors’ knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. JAMA. 2002;287(14):1832–1839. [DOI] [PubMed] [Google Scholar]
- 8.Quillen J, Li Y, Demski M, et al. Comparing the Knowledge of Parents and Survivors Who Attend a Survivorship Clinic. J Pediatr Oncol Nurs. 2018;35(1):56–64. doi: 10.1177/1043454217735828 [DOI] [PubMed] [Google Scholar]
- 9.Signorelli C, Wakefield CE, Fardell JE, et al. The impact of long-term follow-up care for childhood cancer survivors: A systematic review. Crit Rev Oncol Hematol. 2017;114:131–138. doi: 10.1016/j.critrevonc.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 10.Quinn GP, Gonçalves V, Sehovic I, Bowman ML, Reed DR. Quality of life in adolescent and young adult cancer patients: a systematic review of the literature. Patient Relat Outcome Meas. 2015;6:19–51. doi: 10.2147/PROM.S51658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arroyave WD, Clipp EC, Miller PE, et al. Childhood cancer survivors’ perceived barriers to improving exercise and dietary behaviors. Oncol Nurs Forum. 2008;35(1):121–130. doi: 10.1188/08.ONF.121-130 [DOI] [PubMed] [Google Scholar]
- 12.Badr H, Chandra J, Paxton RJ, et al. Health-related quality of life, lifestyle behaviors, and intervention preferences of survivors of childhood cancer. J Cancer Surviv Res Pract. 2013;7(4):523–534. doi: 10.1007/s11764-013-0289-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berg CJ, Stratton E, Esiashvili N, Mertens A. Young Adult Cancer Survivors’ Experience with Cancer Treatment and Follow-Up Care and Perceptions of Barriers to Engaging in Recommended Care. J Cancer Educ Off J Am Assoc Cancer Educ. 2016;31(3):430–442. doi: 10.1007/s13187-015-0853-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casillas J, Syrjala KL, Ganz PA, et al. How confident are young adult cancer survivors in managing their survivorship care? A report from the LIVESTRONGTM Survivorship Center of Excellence Network. J Cancer Surviv Res Pract. 2011;5(4):371–381. doi: 10.1007/s11764-011-0199-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62(2):101–117. doi: 10.3322/caac.20142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirchhoff AC, Montenegro RE, Warner EL, et al. Childhood cancer survivors’ primary care and follow-up experiences. Support Care Cancer. 2014;22(6):1629–1635. doi: 10.1007/s00520-014-2130-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karlson CW, Palermo TM. eHealth and mHealth in Pediatric Oncology. In: Abrams AN, Muriel AC, Wiener L, eds. Pediatric Psychosocial Oncology: Textbook for Multidisciplinary Care. Springer International Publishing; 2016:351–365. doi: 10.1007/978-3-319-21374-3_20 [DOI] [Google Scholar]
- 18.Devine KA, Viola AS, Coups EJ, Wu YP. Digital Health Interventions for Adolescent and Young Adult Cancer Survivors. JCO Clin Cancer Inform. 2018;2:1–15. doi: 10.1200/CCI.17.00138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Casillas JN, Schwartz LF, Crespi CM, et al. The use of mobile technology and peer navigation to promote adolescent and young adult (AYA) cancer survivorship care: results of a randomized controlled trial. J Cancer Surviv. 2019;13(4):580–592. doi: 10.1007/s11764-019-00777-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kunin-Batson A, Steele J, Mertens A, Neglia JP. A randomized controlled pilot trial of a web-based resource to improve cancer knowledge in adolescent and young adult survivors of childhood cancer. Psychooncology. 2016;25(11):1308–1316. doi: 10.1002/pon.3956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Psihogios AM, King-Dowling S, O’Hagan B, et al. Contextual Predictors of Engagement in a tailored mHealth Intervention for Adolescent and Young Adult Cancer Survivors. In Press. Ann Behav Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kazak AE, Hocking MC, Ittenbach RF, et al. A Revision of the Intensity of Treatment Rating Scale: Classifying the Intensity of Pediatric Cancer Treatment. Pediatr Blood Cancer. 2012;59(1):96–99. doi: 10.1002/pbc.23320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rimer BK, Glanz K. Theory at a Glance: A Guide for Health Promotion Practice. 2nd ed. U.S. Dept. of Health and Human Services, National Institutes of Health, National Cancer Institute; 2005. [Google Scholar]
- 25.Naar-King S, Suarez M. Motivational Interviewing with Adolescents and Young Adults. Guilford Press; 2011. [Google Scholar]
- 26.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwartz LA, Daniel LC, Henry-Moss D, et al. Feasibility and acceptability of a pilot tailored text messaging intervention for adolescents and young adults completing cancer treatment. Psychooncology. 2020;29(1):164–172. doi: 10.1002/pon.5287 [DOI] [PubMed] [Google Scholar]
- 28.Klemp JR. Survivorship care planning: one size does not fit all. Semin Oncol Nurs. 2015;31(1):67–72. doi: 10.1016/j.soncn.2014.11.008 [DOI] [PubMed] [Google Scholar]
- 29.Brennan ME, Gormally JF, Butow P, Boyle FM, Spillane AJ. Survivorship care plans in cancer: a systematic review of care plan outcomes. Br J Cancer. 2014;111(10):1899–1908. doi: 10.1038/bjc.2014.505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hill RE, Wakefield CE, Cohn RJ, et al. Survivorship Care Plans in Cancer: A Meta-Analysis and Systematic Review of Care Plan Outcomes. The Oncologist. 2020;25(2):e351–e372. doi: 10.1634/theoncologist.2019-0184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology Statement: Achieving High-Quality Cancer Survivorship Care. J Clin Oncol. 2013;31(5):631–640. doi: 10.1200/JCO.2012.46.6854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Society of Clinical Oncology. Institute of Medicine. From cancer patient to cancer survivor: lost in transition. Published online 2005.
- 33.Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and Evaluating Digital Interventions to Promote Behavior Change in Health and Health Care: Recommendations Resulting From an International Workshop. J Med Internet Res. 2017;19(6):e232. doi: 10.2196/jmir.7126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evans W, Nielsen PE, Szekely DR, et al. Dose-Response Effects of the Text4baby Mobile Health Program: Randomized Controlled Trial. JMIR MHealth UHealth. 2015;3(1):e12. doi: 10.2196/mhealth.3909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Short CE, DeSmet A, Woods C, et al. Measuring Engagement in eHealth and mHealth Behavior Change Interventions: Viewpoint of Methodologies. J Med Internet Res. 2018;20(11):e292. doi: 10.2196/jmir.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon request from the corresponding author.


