Abstract
Liver transplantation (LT) is currently the only curative treatment option for selected patients with end stage liver disease or hepatocellular carcinoma. Improving waiting list-mortality, post-transplant morbidity and mortality and refining the selection of the patients remain our current central objectives. In this field, different concepts dealing with nutrition and the muscle such as sarcopenia, malnutrition, frailty or myosteatosis have emerged as possible game changers. For more than a decade, many prospective studies have demonstrated that sarcopenia and frailty are major predictive factors of mortality in the waiting list but also after LT. Malnutrition is also a well-known risk factor for morbidity and mor-tality. Muscle composition is a newer concept giving insight on muscle quality which has also been shown to be linked to poorer outcomes. Each of these terms has a precise definition as well as pathophysiological mechanisms. The bi-directional liver-muscle axis makes sense in this situation. Defining the best, easy to use in clinical practice tools to assess muscle quality, quantity, and function in this specific population and developing quality prospective studies to identify interventional strategies that could improve these parameters as well as evaluate the effect on mortality are among the important challenges of today.
Keywords: Muscle, Liver, Transplantation, Sarcopenia, Myosteatosis, Frailty
Core Tip: Patients suffering from end stage liver disease currently have liver transplantation as the only curative treatment. In order to improve the pre and post transplantation management of patients, muscle related concepts such as sarcopenia, myosteatosis, frailty and malnutrition could be important potential game changers. Considering a bidirectional axis between the muscle and the liver, it is therefore justified to characterize the condition of the muscles adequately and to identify interventional strategies that could improve both muscle parameters and patient survival.
INTRODUCTION
To date, despite medical developments in knowledge and drug treatments, liver transplantation (LT) remains the only curative treatment option for selected patients with acute liver failure, end-stage liver disease (ESLD), liver cancer and acquired or genetic metabolic liver disease[1]. ESLD is the most frequent indication for LT with alcohol-related liver disease as the main etiology[2]. Other common etiologies are metabolic dysfunction-associated fatty liver disease (MAFLD) and viral hepatitis[3,4]. Autoimmune related liver diseases and cholestatic diseases are rarer indications in Western countries. The epidemiology of LT has changed over the last 20 years since the selection of patients suffering from hepatocellular carcinoma (HCC) with the Milan criteria and the progressive eradication of hepatitis C virus since the universal use of direct-acting antivirals[5]. MAFLD is probably becoming one of the main indications for LT in parallel with the epidemic of obesity in Western countries. This disease can coexist with other causes and act as an important co-factor. This specific population represents a series of challenges in the pre-, peri- and post-transplant settings due to the presence of medical comorbidities that include obesity, type 2 diabetes and cardiovascular risk factors[6,7].
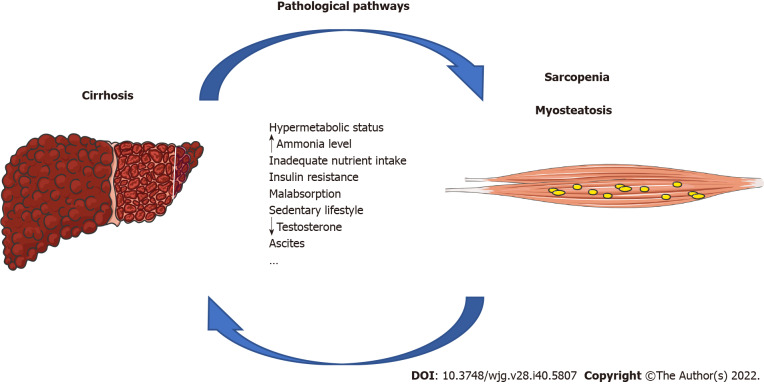
For years, graft allocation has been based on the model for end-stage liver disease (MELD) score that has been used to predict 3-mo mortality on the waiting list. The use of the MELD score has led to a better selection of patients requiring LT but also to a reduction in waiting time and a reduction in mortality on the waiting list[8]. However, the score suffers from several limitations: Patients with cholestatic liver diseases, severe portal hypertension as well as those with hepatic encephalopathy are disadvantaged due to a preserved synthesis function which does not reflect the severity of the disease and the related morbimortality. Another major limitation is the absence of assessment of malnutrition and more specifically of sarcopenia[8-10]. Abnormalities of body composition are frequently found in patients with chronic diseases such as cirrhosis. Interestingly, there is a close relationship between the skeletal muscle compartment and liver function (Figure 1)[11].
Figure 1.
Summary of pathways linking sarcopenia and myosteatosis to cirrhosis: A bi-directional communication. This figure was partly created using Servier Medical Art templates (https://smart.servier.com).
In the field of chronic liver disease (CLD) and particularly ESLD and LT, different concepts have emerged and are commonly used, such as sarcopenia, malnutrition, frailty or myosteatosis[12]. They affect between 40%-70% of cirrhotic patients with important clinical outcomes. They have been evaluated independently in different studies and it is confirmed that they are robust predictors of poor outcomes[13]. This fragile population is at increased risk of hepatic decompensation, reduced quality of life, increased risk of infection, and prolonged hospitalization. It leads to a higher morbidity and mortality[14,15]. Adding the concept of frailty on the waiting list prioritization, specifically helps a population that is listed with low priority based on a low MELD score (< 15). While adding muscle surface to the MELD score had limited added value for organ allocation in a global cirrhotic population, this measurement is highly correlated with waiting list mortality in patients with low MELD score (< 15)[16]. It is therefore important to define the best tools to evaluate these functional concepts in the field of liver diseases and LT[13].
Understanding these different concepts and their implications in our clinical practice is of major interest to improve the management of our patients. There is clearly a certain overlap in these defi-nitions, but it is important to understand them separately to develop tailored behavioral interventions and targeted pharmacotherapies for these conditions[17]. It is necessary to clearly define the gold standard of sarcopenia management with standardized cut-offs for this specific cirrhotic population. These clear definitions will allow us to evaluate the impact of interventions on patients’ outcome[13]. We then review the pathophysiology of cirrhosis-related sarcopenia and myosteatosis, provide a narrative review of the major studies on the subject and discuss the tools available for muscle assessment and treatment.
DEFINITIONS OF COMMONLY USED YET DISTINCT CONCEPTS
As explained above, various terms are now frequently used in the field of CLD, sometimes incorrectly or inappropriately. However, they each have a precise definition.
Malnutrition
Malnutrition can be defined as a state resulting from an insufficient intake of nutrients or an imbalance in essential nutrients and/or in their utilization. This imbalance will have a deleterious impact on the body composition and body cell mass that could lead to diminished physical and mental function, as well as impaired clinical outcomes from disease. Malnutrition has multiple causes combined or take alone, which are starvation and diseases such as CLD and aging[18]. It is also important to note that malnutrition can affect the entire body mass index (BMI) spectrum from obese to anorexic[17]. Different clinical scores exist to estimate the presence of malnutrition such as the nutritional risk score or the Global Leadership Initiative on Malnutrition criteria. Malnutrition is associated with increased mortality in cirrhotic patients[19].
Sarcopenia
The term sarcopenia comes from Greek origin and literally means the “loss of flesh”. Sarcopenia is characterized by 3 components: Decreased muscle mass, decreased muscle strength as well as decreased physical performance[20]. Initially, sarcopenia was described as associated with aging. The term is now also used in association with chronic diseases such as cirrhosis[12]. Nevertheless, even today, the criteria to be included as well as the cut-off values are still discussed. The diagnosis of sarcopenia is still complicated today as the criteria can be so variable, especially in obese people[21]. Cutoffs for muscle mass depletion exist but are still currently under debate. Nevertheless, the use of muscle area measurement at the level of the third lumbar vertebra on a computed tomography (CT) slice is recognized as acceptable by relating the muscle area to the patient’s height squared [skeletal muscle index (SMI)]. By extension, the term sarcopenia is often used based on the sole criterion of low muscle area. Sarcopenia is then defined when SMI is < 41 cm2/m2 for a woman and < 53 cm2/m2 for a man in the field of obesity[22] or < 39 cm2/m2 for a woman and < 50 cm2/m2 for a man in the field of ESLD[23]. In the field of liver diseases, this measure is particularly interesting because it is minimally affected by hydro-sodium retention. Measurement of the brachial circumference (BC) or mid-arm muscle circumference and arm strength using the hand dynamometer are other frequently used techniques.
Myosteatosis
Myosteatosis can be defined as the ectopic accumulation of fat in the muscle. This increased accumulation around and within the myocyte can lead to an impairment of normal physiological function. We will therefore speak of intra and extra cellular fat. It can be estimated on the basis of the decrease in muscle density on an ultrasound image or a CT scan section for example[24,25]. A skeletal muscle radiation attenuation below 41 Hounsfield units (HU) in normal weight patients (BMI up to 24.9 kg/m²) and 33 HU in overweight patients (BMI ≥ 25 kg/m²) could be used[24]. Muscle density can also be related to the muscle surface to give an idea of the absolute amount of intramuscular fat[26]. This leads to the following parameters: The skeletal muscle density index (SMDI)[27] and the skeletal muscle fat index (SMFI) described in patients with MAFLD without ESLD[26,28]. Different groups of patients are compared in clinical studies, but pathological cut-offs for SMDI or SMFI are not yet defined[26-28]. Finally, imaging allows us to assess the homogeneous or heterogeneous distribution of fat in the muscle. This parameter can be associated with certain pathological conditions[29].
Frailty
Defined in the field of geriatrics, frailty is considered a metabolic syndrome associated with a decrease in physiological reserves and an increase in vulnerability to stress factors. In the case of cirrhosis, the stressors are variable, ranging from a dysfunction in protein synthesis to muscle toxicity. A reproducible and objective assessment of patients with liver disease is offered by several simple, non-invasive tests. For example, based on the results of handgrip, sit to stand and balance tests, the liver frailty index (LFI) can be calculated. A patient is considered frail if the score is between 4.5 and 6[15].
Physical exercise
Physical exercise is defined as activity requiring physical effort, performed specifically to maintain or improve health and fitness. The term is therefore relevant to physical activity interventions offered to patients with CLD to improve their condition. The data available so far concerns patients with compensated liver disease with no separate results for patients with ESLD[30]. An increase in functional capacity, strength and muscle mass is noted in the patients with compensated cirrhosis who are subjected to physical exercise for 12 wk and then compared to a group of patients with relaxation activity[31]. In patients awaiting LT, specific protocols are being evaluated (NCT04604860, NCT05061576, NCT05237583, etc). The type (endurance and/or resistance), duration and frequency should be determined, bearing in mind that these programs must be adapted to the patients’ situation (safety, absence of contraindications).
PATHOPHYSIOLOGICAL BASIS OF SARCOPENIA AND MYOSTEATOSIS IN END STAGE LIVER DISEASE
Several mechanisms exist that link sarcopenia to CLD and ESLD. Nevertheless, these exact mechanisms are particularly not well known. Sarcopenia is often a feature of malnutrition. The reasons for this malnutrition, in the case of cirrhosis, are multiple and often result from the combination of several factors (Figure 1)[32]. The first factor in the context of CLD and cirrhosis is the presence of a hypermetabolic status resulting from chronic inflammation and altered gut barrier function[33]. Low liver glycogen content induces muscle protein catabolism for blood glucose maintenance[34]. In addition, ascites present in cirrhotic patients may be responsible for an increase of energy expenditure and therefore increase the catabolism of protein[35]. Partly due to the pro-inflammatory environment, patients with cirrhosis and HCC showed accelerated sarcopenia[36]. Second, the hyperammonemia level is also increased due to its poor elimination because of a pathological architecture of the liver. The consequence of this increase will be the activation of myostatin and consequently the inactivation of protein synthesis which will lead to sarcopenia. Third, inadequate intake of micro and macronutrients can be due in cirrhotic patients to loss of appetite (dysgeusia, cytokines), prolonged gastric emptying or a restrictive diet (sodium and protein) for example. The sedentary lifestyle is probably the most obvious factor in sarcopenia. Indeed, a study showed that one of the causes of sarcopenia in the elderly was partly due to lack of physical exercise[20]. It is therefore easy to think that decompensated cirrhotic patients with high frailty and malnutrition may also suffer from a lack of physical activity aggravating their sarcopenia even more. Fourth, cirrhosis is associated with some degree of cholestasis. An increase in bile acids related to deregulation of the enterohepatic cycle (also due to the dysbiosis associated with cirrhosis) is observed. These have a potentially toxic effect, particularly on the muscle that expresses some bile acid receptors, inducing muscle atrophy[37]. Malabsorption in the context of cirrhosis also plays an important role. A decrease in bile excretion will result in a decrease in the reabsorption of lipids and certain lipo-soluble vitamins. Altered intestinal motility as well as changes in the composition of the gut microbiota will also affect nutrient absorption and utilization[33]. Finally, in cirrhotic patients, a decrease of testosterone levels has been associated with a decrease of muscle mass that could favor sarcopenia[34].
The mechanism through which myosteatosis occurs is still not well understood. Myosteatosis is a well-known characteristic of patients with CLD due to MAFLD[27]. Cirrhotic patients are also characterized by muscle insulin resistance, regardless of the cause of the cirrhosis[34]. This insulin resistance status may also be responsible for myosteatosis[34]. Other proposed mechanisms include hyperammonemia (inducing impaired mitochondrial oxidative phosphorylation and decreased lipid oxidation in muscle), decreased lipid storage capacity within the subcutaneous adipose tissue and age-related differentiation of muscle stem cells into adipocytes[38].
WHY IS IT IMPORTANT TO CONSIDER THE MUSCLE IN A LIVER TRANSPLANT SETTING?
Screening and preventing sarcopenia and frailty is of major interest to patients with CLD. The challenge is big because muscle composition and muscle function have a direct impact on the prognosis of the cirrhotic patient. Sarcopenia and frailty will condition the prognosis of the cirrhotic patients awaiting LT, independently of the severity of the liver disease (MELD score)[39]. Table 1 summarizes the main studies investigating the deleterious role of sarcopenia, frailty and myosteatosis in the context of LT.
Table 1.
Main studies investigating the deleterious role of frailty, low muscle mass, sarcopenia and myosteatosis in patients undergoing pre-transplant assessment
|
Ref.
|
Patient selection
|
Patients, n
|
Sarcopenia, myosteatosis
|
Frailty parameters
|
Outcome
|
Results
|
| Lai et al[15], 2019 | Ambulatory cirrhotic patients awaiting LT | 1014 | Non applicable | LFI | Waiting list mortality | Frailty: 25%. HR = 1.82; 95%CI: 1.31-2.52; P < 0.001 |
| Fozouni et al[48], 2020 | LT recipients | 241 | Non applicable | LFI | Acute cellular rejection within 3 mo post-LT | Frailty: 19%. OR = 3.3; 95%CI: 1.2-9.3; P = 0.02 |
| Lai et al[47], 2022 | LT recipients | 1166 | Non applicable | LFI | LT LOS. ICU stay. Inpatient days within 3 mo post-LT. Overall survival (1-3 and 5-yr mortality) | Frailty: 21%. Prolonged LT LOS: OR = 2.00; 95%CI: 1.47-2.73. ICU stay: OR = 1.56; 95%CI: 1.12-2.14. Inpatient days within 3 mo. post-LT: OR = 1.72; 95%CI: 1.25-2.37. Overall survival: P = 0.02 |
| Bhanji et al[41], 2018 | Cirrhotic patients assessed for LT | 675 | L3-MA (HU). L3-SMI | Non applicable | HE. Mortality | Sarcopenia: 36%. HE: OR = 2.42; 95%CI: 1.43-4.10; P = 0.001. Mortality: Univariate HR = 2.02; 95%CI: 1.57-2.58; P < 0.001. Multivariate: HR = 2.15; 95%CI: 1.52-3.05; P < 0.001. Myosteatosis: 52%. HE: OR = 2.25; 95%CI: 1.32-3.85; P = 0.003. Mortality: Univariate: HR = 1.45; P = 0.004; 95%CI: 1.16-2.91. Multivariate: P = 0.69 |
| Van Vugt et al[42], 2016 | LT candidates/recipients | 3804. Meta-analysis | SMI. Total psoas area | Non applicable | Waiting list mortality. Post-LT mortality | Waiting list mortality: HR = 1.72; 95%CI: 0.99-3.00; P = 0.02. Post-LT mortality: HR = 1.84; 95%CI: 1.11-3.05; P = 0.05 |
| Bot et al[40], 2021 | ESLD patients awaiting LT | 262 | L3-SMI (cm2/m2). L3-MA (HU) | Non applicable | Waiting list mortality | Low SMI: HR = 2.580; 95%CI: 1.055-6.308. MA: HR = 9.124; 95%CI: 2.871-28.970 |
| Czigany et al[24], 2020 | LT recipients | 225 | L3-SMI. L3-MA (HU) | Non applicable | Major morbidity. ICU stay. LT LOS | Sarcopenia: 37%. Myosteatosis: 44%. Major morbidity: OR = 2.772; 95%CI: 1.516-5.066; P = 0.001. ICU stay: 18 ± 25 vs 11 ± 21 d, P < 0.001. LT LOS: 56 ± 55 vs 33 ± 24 d, P < 0.001 |
LFI: Liver frailty index; HR: Hazard ratio; CI: Confidence interval; LT: Liver transplantation; OR: Odds ratio; LT LOS: Liver transplantation length of stay; ICU: Intensive care unit; L3-MA: Lumbar 3-muscle attenuation; HU: Hounsfield unit; L3-SMI: Lumbar 3-skeletal muscle index; HE: Hepatic encephalopathy; SMI: Skeletal muscle index; ESLD: End stage liver disease.
For more than a decade, many prospective studies have demonstrated that low muscle mass is a major predictive factor of mortality in the waiting list but also after LT. In a study involving more than 200 patients on the waiting list, both low muscle quantity and quality were independent risk factors for mortality in patients with ESLD[40]. Low muscle mass is more frequent in patients with hepatic encephalopathy and associates with poor survival[41]. Two meta-analyses confirm these results, the first one includes more than 19 studies with 3800 patients awaiting LT. Sarcopenia was assessed by a wide range of CT-assessed skeletal muscle mass cut-points. Despite these limitations, the study described an independent association between low muscle mass and the post-LT and the waiting list mortality[42]. The second meta-analysis, although it has multiple biases, shows an association between sarcopenia in the pre-LT period and greater post-operative mortality, higher infection risk and post-operative complications, longer intensive care unit stay and ventilator dependency[43].
In patients with cirrhosis (decompensated or not), frailty, easily measured by the LFI, is an independent predictor of death, cirrhosis progression and unplanned hospitalizations (mainly due to infections)[44]. Frail cirrhotic patients also have an increased risk of acute kidney injury[45] and hepatorenal syndrome[46]. In cirrhotic patients awaiting LT, frailty is associated with a 2-fold increased risk of mortality, regardless of the presence of ascites or hepatic encephalopathy[15]. Frail cirrhotic LT recipients have increased postoperative morbidity with prolonged hospital stays[47] and an increased risk of acute rejection[48].
While the link between sarcopenia and mortality is well established, the long-term prognostic value of skeletal muscle quality is less clear. However, several studies tend to demonstrate that pre-transplant myosteatosis is an important prognostic marker for LT recipients in the post-operative period. The prognosis value of myosteatosis seems to be particularly important in the early post-operative phase with higher rates of deaths due to respiratory and septic complications[48]. Unfortunately, most studies are retrospective and the clinical impact of myosteatosis on the transplant waiting list still needs to be demonstrated with prospective studies.
In view of these results, the American Association for the Study of Liver Diseases guidance document suggests that all cirrhotic patients should be assessed for sarcopenia and frailty with standardized tools both at baseline and longitudinally[17]. These recommendations are consistent with the implementation of specific protocols such as “enhanced recovery after surgery” protocols to improve recovery after surgery, especially for LT candidates[49].
HOW TO EVALUATE THE MUSCLE IN ROUTINE PRACTICE?
To assess physical activity, muscle function, composition and mass, several tools exist. It is important to note that many tests, questionnaires and radiological methods are possible. A non-exhaustive list of these tools is presented in Table 2 with their advantages and disadvantages. Some of them have been included in a recent review manuscript[50]. It is interesting to note that patients’ baseline physical activity can be assessed by questionnaire or objective measurement (Table 2). Easy tests are possible in consultation or at the patient’s bedside, such as measuring BC or handgrip strength. Tests that are more complex to implement in routine practice are also available, such as the 6 min walk test, which correlates well with survival in patients awaiting LT[51], or isokinetic testing, the detailed results of which have given interesting information in other diseases such as type 2 diabetes[29]. Finally, among imaging techniques, the same dilemma exists between easier and less expensive techniques (such as ultrasound)[52,53] and time-consuming but probably more objective and reproducible techniques (such as CT or magnetic resonance imaging)[54] (Table 2).
Table 2.
Set of techniques to evaluate the physical activity as well as the quantity and quality of muscle
|
Technique
|
Goal
|
Advantages
|
Disadvantages
|
| Physical activity assessment | |||
| IPAQ | Reflects physical activity over the last 7 d | Easier to implement. Understandable for the patient. Representative over 7 d | Subjective. Poor estimation by the patient |
| Pedometer | Measures walking activity | Inexpensive and easy to set up. Represents the physical activity of walking | Reliability decreases with walking speed. Could induce changes in patient’s habits. Does not measure other physical activities |
| Accelerometer | Measures walking activity | Takes slope and weight carried in consideration | Long to wear for good representation. Not sensitive to the inclination of the walk or the load worn during the walk. Could induce changes in patient’s habits |
| Anthropometric measurement | |||
| BC | Gives information on arm circumference and stage of muscle mass depletion | Very easy to perform (requires only a tape measure) | User dependent |
| MAMC (BC-TSF) | Gives information on arm muscle volume | Well described and easy to perform. Assesses muscle volume better than BC alone | User dependent. Requires a caliper |
| BIA | Allows to assess the body composition | Simple. Non-invasive. Reproductible | Requires specific equipment. Varies with fluid retention (common in cirrhosis) |
| Function tests | |||
| Handgrip | Allows to measure the strength of the forearm and wrist muscles | Low cost. Easy to perform. Gold standard | Not representative of total body strength |
| 6MWT | Measures distance walked for 6 min | Easy to perform. Reflects endurance and general fitness | Caution in patients with cardiac and respiratory problems |
| LFI | Measures frailty of patients calculated with a score | Easy to perform. Little training | Not assessable in severe encephalopathy |
| Isokinetic | Measures the function and strength of a of group muscles | Gold standard. Reproducible | Cost. Requires training and collaboration. Caution in patients with cardiac and respiratory problems |
| Leg press | Measures the strength of the lower limbs | Simple device | Requires collaboration. Rougher assessment. Not well evaluated/used |
| Imaging techniques | |||
| US | Allows to measure the echogenicity of the muscle | Non-invasive. Not expensive | User dependent. Variability with fat thickness, position of the probe. Requires training |
| CT-scan | Allows to measure the surface of the muscle (easily) as well as its density | Clear image. Reproduceable | Radiation exposition |
| MRI | Can be used to evaluate the muscle surface. Measures the amount of fat within the muscle (PDFF) | Clear image. Reproduceable | Cost. Time consuming. Contra-indications (claustrophobia, pacemaker, etc) |
| DXA | Allows to measure the body composition (muscle, fat, water, etc) | Clear image. Reproduceable | Radiation exposition. Varies with fluid retention (common in cirrhosis) |
IPAQ: International physical activity questionnaire; BMI: Body mass index; BC: Brachial circumference; TSF: Tricipital skin fold; MAMC: Mid-arm muscle circumference; BIA: Bio-impedance analysis; 6MWT: 6 min walk test; LFI: Liver frailty index; US: Ultrasound; CT-Scan: Computed tomography scan; MRI: Magnetic resonance imaging; PDFF: Proton density fat fraction; DXA: Dual x-ray absorptiometry.
HOW TO IMPROVE THE MUSCLE IN CLINICAL PRACTICE?
It is well defined that malnutrition plays a major role in the prognosis of the cirrhotic patient and that the resulting loss of muscle mass is a real complication of cirrhotic disease with a significant impact on the morbidity and mortality of these patients. All patients with CLD should be evaluated for nutrition and sarcopenia at the time of diagnosis and then regularly at least annually for compensated cirrhosis and every 8-12 wk for decompensated cirrhosis[17]. The ultimate goal of the medical practitioner is the prevention of the occurrence of complications that may result from sarcopenia and undernutrition. Nevertheless, although there is no clear evidence for an appropriate guideline for patients at present, the current management in transplant centers is that patients with cirrhosis who are placed on the list benefit from efforts by the multidisciplinary team to try to preserve muscle mass and function, through the interventions of dieticians (screening for undernutrition, implementation of standard nutritional measures, early oral intake) and physical therapists (mobilization)[54]. However, it is not yet proven that we are able to slow down the progression of complications or reverse advanced situations via muscle targeted interventions[13]. There are two main options, non-exclusive: Dietary interventions and physical activity. Additional specific pharmacological measures are under investigation.
The current nutrition guidelines for patients with CLD recommend a weight-based daily caloric intake of at least 35 kcal/kg/d with a protein intake of 1.2-1.5 g/kg/d[18]. These recommendations are derived from data assessing energy expenditure (indirect calorimetry). They are difficult to achieve in routine practice. Protein intake is easily found in staple foods such as meat and vegetables. Several studies have analyzed the benefit of branched-chain amino acid (BCAA) supplementation but the results of these data are contradictory. While some authors suggest that BCAA improve hepatic encephalopathy and muscle mass[55], a meta-analysis shows that there is no effect on mortality and nutritional parameters[56]. Because of these contradictions and the limitations of clinical studies, BCAA supplementation is not currently recommended. Prolonged periods of fasting should be avoided in cirrhosis and it is important to favor split meals associated with a late evening snack or an early morning breakfast[17]. Oral nutritional supplements given before bedtime showed a muscle benefit in Child A patients but not Child B or C[57]. If not achieved via oral route, energy intake via enteral nutritional supplementation may be considered to achieve targets.
Besides these nutritional recommendations, physical activity improvement is also important. The latest recommendations propose to assess frailty and/or sarcopenia with standardized tools in order to define a personalized approach for the sarcopenic patient. This personalized activity prescription is guided by the principles of frequency-intensity-time-type: A combination of aerobic exercise that improves cardiorespiratory endurance and resistance exercise that improves strength and skeletal muscle mass[17]. Personalized physical activity allows patients to improve their cardiopulmonary capacity and quality of life. Unfortunately, current randomized controlled data are limited by small samples of well-compensated cirrhosis patients (mean MELD = 10)[31,58]. Despite these promising results, there are no randomized controlled studies with patients with ESLD or a waiting list for LT. It is therefore not currently possible to conclude whether a personalized physical activity program would improve the outcomes in the waiting list and post-LT surgery.
Several randomized controlled trials evaluating the benefit of nutritional and/or physical exercise on muscle mass (SMI) and frailty (LFI) pre- and post-LT would help to answer these uncertainties. Finally, pharmacological treatments are being studied to treat sarcopenia (hormone replacement therapy such as testosterone or growth hormone, ammonia reduction and myostatin inhibition)[59].
CONCLUSION
Malnutrition, sarcopenia and frailty are very common in patients with cirrhosis, especially in cases of disease requiring organ transplantation. Bi-directional pathophysiological links exist between muscle and liver that underlie this association. This highlights the interest of prospective studies comparing the different tools at our disposal to evaluate the cirrhotic patient as well as translational studies to understand these mechanisms and find a possible therapeutic or diagnostic target. Through a better understanding of mechanistic links, the muscle can become a game changer. A better understanding of the situation will also allow us to prioritize fragile patients who need a faster LT or to identify negative factors in certain recipients in whom the situation would be irreversible post-LT and deleterious to the graft. Interventional strategies (nutritional, physical exercise and pharmacological treatments) are also being evaluated. The rationale for their efficacy is clear, even if at this ESLD, evidence of their impact on reducing pre-LT and post-LT mortality is lacking, as well as a precise characterization of the protocols to be implemented. Again, quality prospective studies will be able to answer this question.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: European Association for the Study of the Liver; Belgian Association for the Study of the Liver; Société Royale Belge de Gastro-Entérologie.
Peer-review started: July 8, 2022
First decision: August 19, 2022
Article in press: October 11, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Belgium
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Srpcic M, Slovenia; Tsoulfas G, Greece S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
Contributor Information
Alexis Goffaux, Laboratory of Hepato-Gastroenterology, Institut de Recherche Expérimentale et Clinique, Université catholique de Louvain, Brussels 1200, Belgium; Service d’Hépato-Gastroentérologie, Cliniques universitaires Saint-Luc, Université catholique de Louvain, Brussels 1200, Belgium.
Alicia Delorme, Service d’Hépato-Gastroentérologie, Cliniques universitaires Saint-Luc, Université catholique de Louvain, Brussels 1200, Belgium.
Géraldine Dahlqvist, Service d’Hépato-Gastroentérologie, Cliniques universitaires Saint-Luc, Université catholique de Louvain, Brussels 1200, Belgium.
Nicolas Lanthier, Laboratory of Hepato-Gastroenterology, Institut de Recherche Expérimentale et Clinique, Université catholique de Louvain, Brussels 1200, Belgium; Service d’Hépato-Gastroentérologie, Cliniques universitaires Saint-Luc, Université catholique de Louvain, Brussels 1200, Belgium. nicolas.lanthier@saintluc.uclouvain.be.
References
- 1.Mahmud N. Selection for Liver Transplantation: Indications and Evaluation. Curr Hepatol Rep. 2020;19:203–212. doi: 10.1007/s11901-020-00527-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singal AK, Kwo P, Kwong A, Liangpunsakul S, Louvet A, Mandrekar P, McClain C, Mellinger J, Szabo G, Terrault N, Thursz M, Winder GS, Kim WR, Shah VH. Research methodologies to address clinical unmet needs and challenges in alcohol-associated liver disease. Hepatology. 2022;75:1026–1037. doi: 10.1002/hep.32143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lanthier N, Vanuytsel T. Metabolic dysfunction-associated fatty liver disease: a new clearer nomenclature with positive diagnostic criteria. Acta Gastroenterol Belg. 2020;83:513–515. [PubMed] [Google Scholar]
- 4.Hamoir C, Horsmans Y, Stärkel P, Dahlqvist G, Negrin Dastis S, Lanthier N. Risk of hepatocellular carcinoma and fibrosis evolution in hepatitis C patients with severe fibrosis or cirrhosis treated with direct acting antiviral agents. Acta Gastroenterol Belg. 2021;84:25–32. doi: 10.51821/84.1.420. [DOI] [PubMed] [Google Scholar]
- 5.Dahlqvist G, Moreno C, Starkel P, Detry O, Coubeau L, Jochmans I. Innovations in liver transplantation in 2020, position of the Belgian Liver Intestine Advisory Committee (BeLIAC) Acta Gastroenterol Belg. 2021;84:347–359. doi: 10.51821/84.2.347. [DOI] [PubMed] [Google Scholar]
- 6.Gill MG, Majumdar A. Metabolic associated fatty liver disease: Addressing a new era in liver transplantation. World J Hepatol. 2020;12:1168–1181. doi: 10.4254/wjh.v12.i12.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanthier N. Les nouveaux traitements de la stéatohépatite non-alcooliqueNew therapies in non-alcoholic steatohepatitis. Nutr Clin Metab. 2020;34:216–222. [Google Scholar]
- 8.Durand F, Buyse S, Francoz C, Laouénan C, Bruno O, Belghiti J, Moreau R, Vilgrain V, Valla D. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography. J Hepatol. 2014;60:1151–1157. doi: 10.1016/j.jhep.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Ebadi M, Montano-Loza AJ. Sarcopenia and Frailty in the Prognosis of Patients on the Liver Transplant Waiting List. Liver Transpl. 2019;25:7–9. doi: 10.1002/lt.25386. [DOI] [PubMed] [Google Scholar]
- 10.Artru F, le Goffic C, Pageaux GP, Saliba F, Louvet A. Sarcopenia should be evaluated in patients with acute-on-chronic liver failure and candidates for liver transplantation. J Hepatol. 2022;76:983–985. doi: 10.1016/j.jhep.2021.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Sinclair M, Gow PJ, Grossmann M, Angus PW. Review article: sarcopenia in cirrhosis--aetiology, implications and potential therapeutic interventions. Aliment Pharmacol Ther. 2016;43:765–777. doi: 10.1111/apt.13549. [DOI] [PubMed] [Google Scholar]
- 12.Lanthier N, Stärkel P, Dahlqvist G. Muscle mass depletion in chronic liver diseases: An accelerated model of aging or a distinct entity? Clin Res Hepatol Gastroenterol. 2021;45:101721. doi: 10.1016/j.clinre.2021.101721. [DOI] [PubMed] [Google Scholar]
- 13.Lanthier N, Stärkel P, Dahlqvist G. Frailty, sarcopenia and mortality in cirrhosis: what is the best assessment, how to interpret the data correctly and what interventions are possible? Clin Res Hepatol Gastroenterol. 2021;45:101661. doi: 10.1016/j.clinre.2021.101661. [DOI] [PubMed] [Google Scholar]
- 14.Mazumder N, Rinella M. Editorial: sarcopenia in liver transplantation-our weakest patients may need the strongest push. Aliment Pharmacol Ther. 2019;49:1100–1101. doi: 10.1111/apt.15204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai JC, Rahimi RS, Verna EC, Kappus MR, Dunn MA, McAdams-DeMarco M, Haugen CE, Volk ML, Duarte-Rojo A, Ganger DR, O'Leary JG, Dodge JL, Ladner D, Segev DL. Frailty Associated With Waitlist Mortality Independent of Ascites and Hepatic Encephalopathy in a Multicenter Study. Gastroenterology. 2019;156:1675–1682. doi: 10.1053/j.gastro.2019.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Vugt JLA, Alferink LJM, Buettner S, Gaspersz MP, Bot D, Darwish Murad S, Feshtali S, van Ooijen PMA, Polak WG, Porte RJ, van Hoek B, van den Berg AP, Metselaar HJ, IJzermans JNM. A model including sarcopenia surpasses the MELD score in predicting waiting list mortality in cirrhotic liver transplant candidates: A competing risk analysis in a national cohort. J Hepatol. 2018;68:707–714. doi: 10.1016/j.jhep.2017.11.030. [DOI] [PubMed] [Google Scholar]
- 17.Lai JC, Tandon P, Bernal W, Tapper EB, Ekong U, Dasarathy S, Carey EJ. Malnutrition, Frailty, and Sarcopenia in Patients With Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1611–1644. doi: 10.1002/hep.32049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Association for the Study of the Liver. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70:172–193. doi: 10.1016/j.jhep.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumont C, Wuestenberghs F, Lanthier N, Piessevaux H, Dahlqvist G. Malnutrition is highly prevalent in hospitalized cirrhotic patients and associates with a poor outcome. Acta Gastroenterol Belg. 2022;85:311–319. doi: 10.51821/85.2.9016. [DOI] [PubMed] [Google Scholar]
- 20.Dhillon RJ, Hasni S. Pathogenesis and Management of Sarcopenia. Clin Geriatr Med. 2017;33:17–26. doi: 10.1016/j.cger.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–2646. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 22.Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–1547. doi: 10.1200/JCO.2012.45.2722. [DOI] [PubMed] [Google Scholar]
- 23.Carey EJ, Lai JC, Wang CW, Dasarathy S, Lobach I, Montano-Loza AJ, Dunn MA Fitness, Life Enhancement, and Exercise in Liver Transplantation Consortium. A multicenter study to define sarcopenia in patients with end-stage liver disease. Liver Transpl. 2017;23:625–633. doi: 10.1002/lt.24750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Czigany Z, Kramp W, Bednarsch J, van der Kroft G, Boecker J, Strnad P, Zimmermann M, Koek G, Neumann UP, Lurje G. Myosteatosis to predict inferior perioperative outcome in patients undergoing orthotopic liver transplantation. Am J Transplant. 2020;20:493–503. doi: 10.1111/ajt.15577. [DOI] [PubMed] [Google Scholar]
- 25.Czigany Z, Kramp W, Lurje I, Miller H, Bednarsch J, Lang SA, Ulmer TF, Bruners P, Strnad P, Trautwein C, von Websky MW, Tacke F, Neumann UP, Lurje G. The role of recipient myosteatosis in graft and patient survival after deceased donor liver transplantation. J Cachexia Sarcopenia Muscle. 2021;12:358–367. doi: 10.1002/jcsm.12669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nachit M, Lanthier N, Rodriguez J, Neyrinck AM, Cani PD, Bindels LB, Hiel S, Pachikian BD, Trefois P, Thissen JP, Delzenne NM. A dynamic association between myosteatosis and liver stiffness: Results from a prospective interventional study in obese patients. JHEP Rep. 2021;3:100323. doi: 10.1016/j.jhepr.2021.100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lanthier N, Rodriguez J, Nachit M, Hiel S, Trefois P, Neyrinck AM, Cani PD, Bindels LB, Thissen JP, Delzenne NM. Microbiota analysis and transient elastography reveal new extra-hepatic components of liver steatosis and fibrosis in obese patients. Sci Rep. 2021;11:659. doi: 10.1038/s41598-020-79718-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nachit M, Kwanten WJ, Thissen JP, Op De Beeck B, Van Gaal L, Vonghia L, Verrijken A, Driessen A, Horsmans Y, Francque S, Leclercq IA. Muscle fat content is strongly associated with NASH: A longitudinal study in patients with morbid obesity. J Hepatol. 2021;75:292–301. doi: 10.1016/j.jhep.2021.02.037. [DOI] [PubMed] [Google Scholar]
- 29.Bell KE, Paris MT, Avrutin E, Mourtzakis M. Altered features of body composition in older adults with type 2 diabetes and prediabetes compared with matched controls. J Cachexia Sarcopenia Muscle. 2022;13:1087–1099. doi: 10.1002/jcsm.12957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tandon P, Montano-Loza AJ, Lai JC, Dasarathy S, Merli M. Sarcopenia and frailty in decompensated cirrhosis. J Hepatol. 2021;75 Suppl 1:S147–S162. doi: 10.1016/j.jhep.2021.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Román E, García-Galcerán C, Torrades T, Herrera S, Marín A, Doñate M, Alvarado-Tapias E, Malouf J, Nácher L, Serra-Grima R, Guarner C, Cordoba J, Soriano G. Effects of an Exercise Programme on Functional Capacity, Body Composition and Risk of Falls in Patients with Cirrhosis: A Randomized Clinical Trial. PLoS One. 2016;11:e0151652. doi: 10.1371/journal.pone.0151652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mazurak VC, Tandon P, Montano-Loza AJ. Nutrition and the transplant candidate. Liver Transpl. 2017;23:1451–1464. doi: 10.1002/lt.24848. [DOI] [PubMed] [Google Scholar]
- 33.Quigley EM, Stanton C, Murphy EF. The gut microbiota and the liver. Pathophysiological and clinical implications. J Hepatol. 2013;58:1020–1027. doi: 10.1016/j.jhep.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 34.Clarembeau F, Bale G, Lanthier N. Cirrhosis and insulin resistance: current knowledge, pathophysiological mechanisms, complications and potential treatments. Clin Sci (Lond) 2020;134:2117–2135. doi: 10.1042/CS20200022. [DOI] [PubMed] [Google Scholar]
- 35.Dolz C, Raurich JM, Ibáñez J, Obrador A, Marsé P, Gayá J. Ascites increases the resting energy expenditure in liver cirrhosis. Gastroenterology. 1991;100:738–744. doi: 10.1016/0016-5085(91)80019-6. [DOI] [PubMed] [Google Scholar]
- 36.Perisetti A, Goyal H, Yendala R, Chandan S, Tharian B, Thandassery RB. Sarcopenia in hepatocellular carcinoma: Current knowledge and future directions. World J Gastroenterol. 2022;28:432–448. doi: 10.3748/wjg.v28.i4.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abrigo J, Gonzalez F, Aguirre F, Tacchi F, Gonzalez A, Meza MP, Simon F, Cabrera D, Arrese M, Karpen S, Cabello-Verrugio C. Cholic acid and deoxycholic acid induce skeletal muscle atrophy through a mechanism dependent on TGR5 receptor. J Cell Physiol. 2021;236:260–272. doi: 10.1002/jcp.29839. [DOI] [PubMed] [Google Scholar]
- 38.Ebadi M, Tsien C, Bhanji RA, Dunichand-Hoedl AR, Rider E, Motamedrad M, Mazurak VC, Baracos V, Montano-Loza AJ. Myosteatosis in Cirrhosis: A Review of Diagnosis, Pathophysiological Mechanisms and Potential Interventions. Cells. 2022;11 doi: 10.3390/cells11071216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai JC, Feng S, Terrault NA, Lizaola B, Hayssen H, Covinsky K. Frailty predicts waitlist mortality in liver transplant candidates. Am J Transplant. 2014;14:1870–1879. doi: 10.1111/ajt.12762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bot D, Droop A, Lucassen CJ, van Veen ME, van Vugt JLA, Shahbazi Feshtali S, Leistra E, Tushuizen ME, van Hoek B. Both muscle quantity and quality are predictors of waiting list mortality in patients with end-stage liver disease. Clin Nutr ESPEN. 2021;42:272–279. doi: 10.1016/j.clnesp.2021.01.022. [DOI] [PubMed] [Google Scholar]
- 41.Bhanji RA, Moctezuma-Velazquez C, Duarte-Rojo A, Ebadi M, Ghosh S, Rose C, Montano-Loza AJ. Myosteatosis and sarcopenia are associated with hepatic encephalopathy in patients with cirrhosis. Hepatol Int. 2018;12:377–386. doi: 10.1007/s12072-018-9875-9. [DOI] [PubMed] [Google Scholar]
- 42.van Vugt JL, Levolger S, de Bruin RW, van Rosmalen J, Metselaar HJ, IJzermans JN. Systematic Review and Meta-Analysis of the Impact of Computed Tomography-Assessed Skeletal Muscle Mass on Outcome in Patients Awaiting or Undergoing Liver Transplantation. Am J Transplant. 2016;16:2277–2292. doi: 10.1111/ajt.13732. [DOI] [PubMed] [Google Scholar]
- 43.Ooi PH, Hager A, Mazurak VC, Dajani K, Bhargava R, Gilmour SM, Mager DR. Sarcopenia in Chronic Liver Disease: Impact on Outcomes. Liver Transpl. 2019;25:1422–1438. doi: 10.1002/lt.25591. [DOI] [PubMed] [Google Scholar]
- 44.Wang S, Whitlock R, Xu C, Taneja S, Singh S, Abraldes JG, Burak KW, Bailey RJ, Lai JC, Tandon P. Frailty is associated with increased risk of cirrhosis disease progression and death. Hepatology. 2022;75:600–609. doi: 10.1002/hep.32157. [DOI] [PubMed] [Google Scholar]
- 45.Cullaro G, Verna EC, Duarte-Rojo A, Kappus MR, Ganger DR, Rahimi RS, Boyarsky B, Segev DL, McAdams-DeMarco M, Ladner DP, Volk ML, Hsu CY, Lai JC. Frailty and the Risk of Acute Kidney Injury Among Patients With Cirrhosis. Hepatol Commun. 2022;6:910–919. doi: 10.1002/hep4.1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schleicher EM, Kremer WM, Kalampoka V, Gairing SJ, Kaps L, Schattenberg JM, Galle PR, Wörns MA, Nagel M, Weinmann-Menke J, Labenz C. Frailty as Tested by the Clinical Frailty Scale Is a Risk Factor for Hepatorenal Syndrome in Patients With Liver Cirrhosis. Clin Transl Gastroenterol. 2022;13:e00512. doi: 10.14309/ctg.0000000000000512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lai JC, Shui AM, Duarte-Rojo A, Ganger DR, Rahimi RS, Huang CY, Yao F, Kappus M, Boyarsky B, McAdams-Demarco M, Volk ML, Dunn MA, Ladner DP, Segev DL, Verna EC, Feng S from the Multi-Center Functional Assessment in Liver Transplantation (FrAILT) Study. Frailty, mortality, and health care utilization after liver transplantation: From the Multicenter Functional Assessment in Liver Transplantation (FrAILT) Study. Hepatology. 2022;75:1471–1479. doi: 10.1002/hep.32268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fozouni L, Mohamad Y, Lebsack A, Freise C, Stock P, Lai JC. Frailty Is Associated With Increased Rates of Acute Cellular Rejection Within 3 Months After Liver Transplantation. Liver Transpl. 2020;26:390–396. doi: 10.1002/lt.25669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crespo G, Hessheimer AJ, Armstrong MJ, Berzigotti A, Monbaliu D, Spiro M, Rapti DA, Lai JC. Which preoperative assessment modalities best identify patients who are suitable for enhanced recovery after liver transplantation? Clin Transplant. 2022:e14644. doi: 10.1111/ctr.14644. [DOI] [PubMed] [Google Scholar]
- 50.Hari A. Muscular abnormalities in liver cirrhosis. World J Gastroenterol. 2021;27:4862–4878. doi: 10.3748/wjg.v27.i29.4862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carey EJ, Steidley DE, Aqel BA, Byrne TJ, Mekeel KL, Rakela J, Vargas HE, Douglas DD. Six-minute walk distance predicts mortality in liver transplant candidates. Liver Transpl. 2010;16:1373–1378. doi: 10.1002/lt.22167. [DOI] [PubMed] [Google Scholar]
- 52.Kara M, Kaymak B, Ata AM, Özkal Ö, Kara Ö, Baki A, Şengül Ayçiçek G, Topuz S, Karahan S, Soylu AR, Çakır B, Halil M, Özçakar L. STAR-Sonographic Thigh Adjustment Ratio: A Golden Formula for the Diagnosis of Sarcopenia. Am J Phys Med Rehabil. 2020;99:902–908. doi: 10.1097/PHM.0000000000001439. [DOI] [PubMed] [Google Scholar]
- 53.Razaq S, Kara M, Özçakar L. Measure grip strength, gait speed and quadriceps muscle in cirrhosis. Comment to "Frailty, sarcopenia and mortality in cirrhosis: What is the best assessment, how to interpret the data correctly and what interventions are possible? Clin Res Hepatol Gastroenterol. 2021;45:101727. doi: 10.1016/j.clinre.2021.101727. [DOI] [PubMed] [Google Scholar]
- 54.Brustia R, Monsel A, Skurzak S, Schiffer E, Carrier FM, Patrono D, Kaba A, Detry O, Malbouisson L, Andraus W, Vandenbroucke-Menu F, Biancofiore G, Kaido T, Compagnon P, Uemoto S, Rodriguez Laiz G, De Boer M, Orloff S, Melgar P, Buis C, Zeillemaker-Hoekstra M, Usher H, Reyntjens K, Baird E, Demartines N, Wigmore S, Scatton O. Guidelines for Perioperative Care for Liver Transplantation: Enhanced Recovery After Surgery (ERAS) Recommendations. Transplantation. 2022;106:552–561. doi: 10.1097/TP.0000000000003808. [DOI] [PubMed] [Google Scholar]
- 55.Hernández-Conde M, Llop E, Gómez-Pimpollo L, Fernández Carrillo C, Rodríguez L, Van Den Brule E, Perelló C, López-Gómez M, Abad J, Martínez-Porras JL, Fernández-Puga N, Ferre C, Trapero M, Fraga E, Calleja JL. Adding Branched-Chain Amino Acids to an Enhanced Standard-of-Care Treatment Improves Muscle Mass of Cirrhotic Patients With Sarcopenia: A Placebo-Controlled Trial. Am J Gastroenterol. 2021;116:2241–2249. doi: 10.14309/ajg.0000000000001301. [DOI] [PubMed] [Google Scholar]
- 56.Gluud LL, Dam G, Les I, Marchesini G, Borre M, Aagaard NK, Vilstrup H. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;5:CD001939. doi: 10.1002/14651858.CD001939.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Plank LD, Gane EJ, Peng S, Muthu C, Mathur S, Gillanders L, McIlroy K, Donaghy AJ, McCall JL. Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology. 2008;48:557–566. doi: 10.1002/hep.22367. [DOI] [PubMed] [Google Scholar]
- 58.Aamann L, Dam G, Borre M, Drljevic-Nielsen A, Overgaard K, Andersen H, Vilstrup H, Aagaard NK. Resistance Training Increases Muscle Strength and Muscle Size in Patients With Liver Cirrhosis. Clin Gastroenterol Hepatol. 2020;18:1179–1187.e6. doi: 10.1016/j.cgh.2019.07.058. [DOI] [PubMed] [Google Scholar]
- 59.Allen SL, Quinlan JI, Dhaliwal A, Armstrong MJ, Elsharkawy AM, Greig CA, Lord JM, Lavery GG, Breen L. Sarcopenia in chronic liver disease: mechanisms and countermeasures. Am J Physiol Gastrointest Liver Physiol. 2021;320:G241–G257. doi: 10.1152/ajpgi.00373.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]