Certain work locations and body postures of computer users working at home during COVID-19, were associated with higher risk of having musculoskeletal pain. Our results are highly relevant for employers encouraging continued work at home, and for individuals who work on computers, to recognise potential risks for musculoskeletal pain.
Keywords: musculoskeletal pain, working From home, computer user, SARS-2, corona virus, ergonomics, posture, depression
Objective
To understand the flexible work practices during the COVID-19 pandemic and their impact on work-related musculoskeletal disorders (MSDs) and depression in frequent computer users.
Methods
An e-survey determined the extent of workplace changes and MSD, and the relationships between them using descriptive-statistics and chi-squared tests.
Results
Of 700 who commenced the survey, 511 were analyzed. Since the pandemic commenced, 80% of respondents reported they were working more from home; and 89% reported some musculoskeletal pain. Compared with prepandemic, more people worked in nonergonomic environments, computer configurations and body postures. Work location was associated with upper back pain (P = 0.011); body posture with headache (P = 0.027) and low back pain (P = 0.003).
Conclusion
Nonergonomic work environments of frequent computer users during COVID-19 are related to having upper back pain, whereas nonergonomic postures are related to having headache and low back pain.
The COVID-19 pandemic has dramatically changed many aspects of individuals working life. Businesses across the world have had to unexpectantly pivot their work environment to embrace flexible work practices. Workers had to quickly adapt to working from home, often in nonergonomic workspaces and/or with atypical working hours to accommodate family commitments (e.g., homeschooling). The impact of these changes to the work environment on musculoskeletal complaints is largely unknown.
Musculoskeletal disorders (MSDs) include a wide range of inflammatory and degenerative conditions affecting musculoskeletal structures, mainly the muscles, tendons, ligaments and joints.1 Work-related injuries cost Australia $62 billion annually, with 77% of these costs borne by workers primarily in lost wages and the remainder being health care costs.2,3 Fifty-one percent of these costs are from MSD with the majority of MSD comprising neck and back pain.4 These costs are comparable to other countries. The United Kingdom has reported £7.5 billion of combined annual costs of new cases of work-related MSD and stress in 2013/14.4 US workers compensation costs for the most disabling, nonfatal workplace injuries being $55 billion.5 These figures suggest MSD are a large burden on governments, health care systems and individuals.
Working on computers or other electronic devices has been linked to MSD. Australian data before the COVID-19 pandemic identified that 80% of office workers (59% working flexibly) report MSD (neck pain 60%, shoulder pain 53%, back pain 47%).6 Data from Europe suggests 60% of people with a work-related health problem identify MSD as their most serious problem.7 MSD prevalence is also increasing in low- to middle-income countries.8 Posture is one risk factor possibly contributing to these MSD statistics as workplace ergonomics has been previously been linked to MSD.9 Contributing factors to work-related MSD are multifaceted. A body of literature suggests work-related MSD are associated with physical (e.g., nonneutral body postures either dynamic or static, rapid work pace, repetitive motion patterns and insufficient recovery time) and psychosocial risk factors (e.g., depression, employer/employee relationships and job autonomy).10–12 Established relationships between physical loads in the workplace and pain, impairment, and disability suggest that posture plays an important role in maintaining healthy ergonomics.10
The rapid shift to home working during the COVID-19 pandemic meant that many workers found themselves working in nonergonomic workspaces and using nonneutral postures. An ergonomic workstation supports the body in a neutral spinal posture, and has been shown to reduce musculoskeletal symptoms in office workers.13 One pilot study of 232 telecommunications workers in Croatia suggested that the work environment during COVID-19 may be related to musculoskeletal symptoms.14 Despite potential nonergonomic workspaces, the more relaxed environment at home, the ability to work at their own pace and take breaks as they choose and reduced commuting time may assist some workers. The effect of working at home on stress,15 fatigue or tiredness,16 and depression17 has been studied with mixed results.18 Whether a worker experiences stress or depression from working at home appears to be mediated by several factors including gender,19,20 organizational support,21 social connectedness,22 and voluntary versus mandated working from home.23 The extent of changes to the physical working environment during COVID-19 has not been elucidated, and whether these changes affect the frequency or severity of MSD is not established.
The aim of this study is to understand the flexible work practices that have proliferated during the COVID-19 pandemic and their impact on work-related MSD and depression levels in workers in flexible computer-based jobs. The specific research questions were:
How has COVID-19 changed the workplace and work-habits (location, computer type and body postures) of frequent computer users?
Are workplace and work-habits (location, computer type and body posture) related to having musculoskeletal pain or depression in computer users?
DESIGN AND METHODS
An online survey of computer users was open for completion between July 24, 2020, and 26 October 26, 2020, and accessible online using a computer or mobile device. It was administered using the Qualtrics platform (Qualtrics, Provo, UT). The questionnaire was in English only and thus participants had to be able to read and understand English to participate. Informed consent was obtained from all subjects. The survey and results are reported according to the Checklist for Reporting Results of Internet E-Surveys24 (Supplementary file, http://links.lww.com/JOM/B201).
Eligibility and Recruitment
Eligible participants were those who worked at least 75% of their working time on a computer or other mobile device (laptop, tablet, and/or smart phone). The eligibility threshold of “at least 75% of work time” was selected to represent workers who spent most of their working time on computers. Previous research has used this threshold to represent workers who do intensive computer work, and working a greater percentage of work time at a computer is associated with neck and shoulder symptoms.25 Participants were primarily recruited through social media, using platforms, such as Facebook, Twitter, and LinkedIn alongside sharing by the authors to their colleagues locally, nationally and internationally. Snowball sampling was used aiming to encourage sharing the social media posts among colleagues internationally, with posts originating from the authors, who were based in Australia, the United Kingdom or United States. Emails about the survey were circulated among the university workplaces of the authors, i.e., The University of Newcastle in Australia, the University of Birmingham in the United Kingdom, and Baylor University in Waco, TX.
Survey Structure, Content and Development
The adaptive survey contained a mix of multiple choice and text entry questions, with most items requiring a forced choice. The number of items per page varied, depending on the type of question and on the previous responses of a participant. Participants were directed to specific sections based on their responses, which allowed for efficient completion. Therefore, responses to individual questions do not consistently total 100%. Completeness checking was performed in the Qualtrics software by using the “force response” option, with an option for “other” responses where appropriate to allow participants to progress through the questionnaire. Respondents were allowed to finish their survey at a later time. Qualtrics uses cookies to assign a unique user identifier to each client computer so that respondents could return the survey from the point where they stopped, provided they used the same computer. Respondents were informed of this in the information distributed about the survey. Duplicate entries were handled via the unique user identifier in Qualtrics (i.e., IP address) and no duplicate entries were detected in the dataset.
Informed by a review of existing evidence and literature, the questionnaire included four sections: (1) demographics including employment, education, household size to describe the participant sample; (2) work practices including work habits, locations, computer types (i.e., workstation set-up), and body postures; (3) prevalence, intensity and impact of MSD (via a Nordic questionnaire modified to include head pain)26 with validated questionnaires to quantify physical disability related to a respondent’s specific symptoms; and (4) general health including physical activity (Godin Leisure-time Physical Activity Questionnaire) and a depression screen (Center for Epidemiologic Studies Short Depression Scale [CESD-10]). The CESD-10 is a validated 10-question screening tool for symptoms of depression. While it is not a diagnostic tool for depression, a score of ≥10 is generally accepted as an indication of depressive symptoms.27
Work locations were defined as any physical space used for work; selections included office desk at work, office desk at home, dining room table, kitchen bench/counter, couch, bed, hotel room, park bench, one that moves (e.g., train), waiting at child’s activity, other. These categories were suggested to capture some of the potentially nonergonomic work settings respondents might use by assisting them to identify any location within or outside their home that they might have used for work. For the location where they worked most often before the pandemic, and the locations (up to three) where they worked most often since the onset of the pandemic, respondents selected their computer type (desktop computer; laptop with external keyboard, monitor and mouse; laptop with external monitor and mouse; laptop with external mouse only; and laptop without external equipment) and body posture. For body posture, respondents selected a posture from five validated illustrations28 that they believed they used most commonly, also described with text: trunk a little bent forward, straight up, back against backrest; straight up, back NOT against backrest; bottom dropped, lower back not against backrest; and variable, alter at least once per ½ hour (Fig. 1).6,28
FIGURE 1.
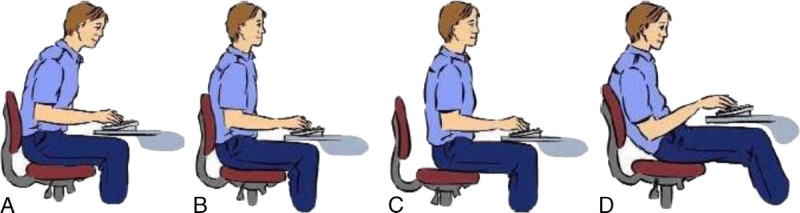
Illustrations of body posture used by respondents to select the body posture they used most often while working before and during the COVID-19 pandemic (trunk a little bent forward (A), straight up, back against backrest (B); straight up, back NOT against backrest (C); bottom dropped, lower back not against backrest (D); and variable, alter at least once per ½ hour (no illustration). Reproduced with permission from James et al. Applied Ergonomics,6 and originally published by IJmker et al. Applied Ergonomics.26
Intensity of MSD was quantified with a pain visual analog scale (VAS), and questions about whether they had sought treatment or taken medications. The VAS, anchored by no pain on the left and worst pain imaginable on the right, was generated using the Qualtrics slider bar tool; by default, it included numbering above the scale at 10-point intervals, though participants could place the bar anywhere along the scale. Participants were also asked if they believed their pain had worsened during the pandemic. To quantify physical disability, participants completed one of the following, based on the body area they selected as their most problematic: Headache Impact Tool,29 Neck Disability Index,30 Disabilities of the Shoulder, Arm and Hand Questionnaire,31 the Oswestry Disability Index,32 and the Lower Extremity Functional Scale.33 All are scored out of 100% with a higher number representing more disability. The Lower Extremity Functional Scale, scored with a lower number representing more disability, is presented as reversed, to allow better comparisons with the other scales. See supplementary files for a copy of the questionnaire items (Supplementary Digital Content, http://links.lww.com/JOM/B201).
Before participant recruitment, the questionnaire was piloted with a convenience sample of office workers (n = 13) from Australia and the United Kingdom, some with and others without MSDs. Minor modifications were made after piloting to improve the clarity of wording of some questions. Pilot data were excluded from the analysis.
Data Management and Analysis
Data were exported from Qualtrics survey software and analyzed using R (Version 4, The R Foundation, www.r-project.org) and SPSS (Version 27.0; IBM Statistics, Armonk, NY) software. Chi-squared tests were used to determine if completers of the survey were different to noncompleters with respect to the included demographic variables. A completer was defined as a participant who answered the question matrix in section two about their workplace environment (locations, computer types and body postures), regardless of whether they completed the remainder of the questionnaire. Descriptive statistics were calculated and tabulated for those who completed the survey. Data are reported as collected without imputation for missing data, and numbers responding are reported for each question. As work location included many categories, they were collapsed for reporting descriptive statistics based on the common selections of respondents.
For research question one, changes in work locations, computer types and body postures were examined with chi-squared, comparing these variables prepandemic with those used most often postpandemic. For research question two, chi-squared was used to determine relationships between work locations and presence of MSD or depression, and between body posture and presence of MSD or depression. For these analyses, categories were collapsed as follows: work locations (office desk at work, office desk at home, dining room table, kitchen bench/counter, couch/bed, other location), computer types (desktop + laptop with all peripherals; laptop with minimal or no peripherals), body posture (trunk bent forwards, straight up against a backrest, straight up not against a back rest, bottom dropped, and variable). Relationships with significant chi-squared values were further examined using adjusted standardized residuals ≥2 to determine the category pairs where the assumption of independence between variables in the table is likely to be false. The cells with large residuals signify significant differences in the distribution of locations worked or body postures with respect to the presence or absence of pain.
As pain responses differ by gender and proportions of respondents with pain differed by gender for some pain conditions in our sample, we explored the effect of gender on our main outcomes (work location and body posture) using multinomial logistic regression. The models contained a main effect for pain condition, gender and their interaction. The interaction term provides the test as to whether the effect of gender modifies the relationship between pain condition and the outcomes (work location or body posture). Separate models were constructed for each pain condition and for depression. Because of the additional testing using gender above our original research questions we chose to adjust for multiple testing (7 conditions) to reduce the chance of false positives. For each outcome (location and body posture), we applied the Bonferroni correction and set the significance at P ≤ 0.007 for the interaction term (pain*gender).
RESULTS
Participants
Of 700 who commenced the survey, 25 (3.6%) did not work at least 75% of working hours at a computer and were excluded; 27 (3.9%) did not answer this screening question or any further questions; 137 (19.6%) answered one or more demographics questions but did not complete the question about where they worked, so were not included in this analysis. Thus, 511 surveys were considered complete. Completers and noncompleters did not differ in terms of demographics, e.g., age, gender. However, a higher proportion of respondents who completed the survey were working full time (71%, n = 420 of 593 who provided their work status) than those who commenced the survey but did not complete it (10%, n = 61, chi-squared = 3.66, P = 0.056). For completers, the percentage of missing data from any one question was ≤7%, most often <5%.
The 511 completing respondents had a mean age of 42.6 ± 11.5 years and included 70% (n = 359) females. Demographics of the respondents are reported in Table 1. A majority (89%, n = 452) reported musculoskeletal pain in at least one body area in the previous 4 weeks. Respondents were mainly from Australia (55%, n = 281), UK (20%, n = 100) and US (7%, n = 36). Eighty-six percent held a university degree or higher and 75.7% were full-time paid employees. Over 70% (n = 367) were categorized as physically active (Godin score).34 Forty percent (n = 204) had self-reported depressive symptoms and 88.5% (n = 452) had experienced musculoskeletal discomfort in the previous 12 months (Table 1).
TABLE 1.
Characteristics of Respondents (n = 511)
| Characteristics | Mean (SD) or n (%) |
|---|---|
| Age (yr), mean (SD) | 42.6 (11.47) |
| Sex (female), n (%) | 359 (70.3) |
| Country, n (%) | |
| Australia | 281 (55) |
| UK | 100 (19.6) |
| US | 36 (7.0) |
| Other | 94 (18.4) |
| Highest level of educational qualification | |
| Higher university degree | 272 (53.2) |
| Bachelor's degree | 170 (33.3) |
| Certificate, high school or trade | 63 (12.3) |
| Year 10 or lower qualification | 6 (1.2) |
| Household size, n (%) | |
| Number of adults | |
| 1 | 86.0 (16.9) |
| 2 | 321 (62.8) |
| 3–4 | 94 (18.4) |
| 5 or more | 10 (2.0) |
| Number of dependent children, n (%) (missing, n = 1) | |
| 0 | 318 (62.2) |
| 1 | 65 (12.7) |
| 2 | 100 (19.6) |
| 3 or more | 27 (5.3) |
| Employment status, n (%) | |
| Full time paid | 387 (75.7) |
| Part time paid | 73 (14.3) |
| Self-employed full time | 15 (2.9) |
| Self-employed part time | 11 (2.2) |
| Contract/temporary full time | 18 (3.5) |
| Casual/temporary part-time | 6 (1.2) |
| Employer | 1 (0.2) |
| Employment industry, n (%) | |
| Agriculture, mining, manufacturing, electricity/gas/water services, construction | 18 (3.6) |
| Retail/transport | 7 (1.4) |
| Media/telecommunications | 23 (4.5) |
| Financial/insurance | 33 (6.5) |
| Professional/technical | 96 (18.8) |
| Public administration | 23 (4.5) |
| Education | 194 (38.0) |
| Health care | 80 (15.7) |
| Other | 37 (7.2) |
| Physical activity (category), n (%) | |
| Insufficiently active | 73 (14.3) |
| Moderately active | 70 (13.7) |
| Active | 367 (71.8) |
| Mental well-being: CES-D 10* (category), n (%) | |
| Depressed (“having depressive symptoms”) | 204 (40.0) |
| Not depressed (not ‘having depressive symptoms’) | 231 (45.2) |
| Experienced musculoskeletal discomfort in previous 12 months; all also reported discomfort in the previous 4 weeks, n (%) | 452 (88.5) |
| Reported pain in the last 4 weeks, by body area (respondents could choose multiple body areas) | |
| Headache | 122 (27) |
| Neck pain | 322 (71) |
| Shoulder pain | 297 (66) |
| Elbow pain | 61 (14) |
| Wrist/hand pain | 138 (31) |
| Upper back pain | 159 (35) |
| Lower back pain | 280 (62) |
| Hip pain | 146 (32) |
| Knee pain | 105 (24) |
| Ankle pain | 69 (15) |
*Center for Epidemiologic Studies Short Depression Scale.
Working From Home Habits
Table 2 summarizes working habits before and during the COVID pandemic in 2020. While more than half of the respondents (54%, n = 276) indicated that their workplace offered flexible work before COVID, 81% (n = 413) reported the amount of time they worked at home had increased during the pandemic, from 28% (SD, 29) of work time on average to 48% (SD, 28). Most were working at home due to employer requirements (47%, n = 198) or government restrictions (39%, n = 241). Seventy-five respondents spent time homeschooling during the pandemic (40% of those with dependent children). Of these, 65% reported that homeschooling affected their work productivity (Table 2).
TABLE 2.
Working From Home Habits before and During the Covid-19 Pandemic 2020 in Workers Who Spend ≥75% of Work Time on Computers (n = 511)
| Workplace Offered Flexible Work Before COVID, n (%) | |
|---|---|
| Yes | 276 (54) |
| No | 235 (46) |
| Worked from home before COVID, n (%) | |
| Yes | 272 (53.2) |
| No | 239 (46.8) |
| Percentage of time (average per week) worked at home before COVID, mean (SD) | 28.4 (29.3) |
| Work at home during the previous 4 weeks, n (%) | |
| Some hours | 204 (39.9) |
| All hours | 257 (50.3) |
| No | 50 (9.8) |
| Percentage of work time at home in the previous 4 weeks, mean (SD) | 47.4 (27.9) |
| How work at home changed since COVID, n (%) | |
| Increased | 413 (80.8) |
| Decreased | 12 (2.3) |
| Stayed the same | 35 (6.8%) |
| Reason currently working at home, n (%) | |
| Government restrictions | 198 (38.7) |
| Employer requirements | 241 (47.2) |
| Carer's responsibilities | 28 (5.5) |
| Health issues | 42 (8.2) |
| General fear of contracting COVID | 65 (12.7) |
| Other | 92 (18.0) |
| Reason not working at home, n (%) | |
| COVID restrictions lifted | 8 (1.6) |
| Home/family situation not conducive to working at home | 3 (0.6) |
| Home does not have access to Internet or proper equipment | 1 (0.2) |
| Other | 4 (0.8) |
| Spent additional time on computer to help children, n (%) of n = 192 with dependent children | |
| Yes | 75 (39.1) |
| No | 117 (60.9) |
| Of n = 75 who spent additional time on computer to help children | |
| Homeschooling affected ability to work usual work hours | |
| Never | 6 (8.0) |
| Rarely | 14 (18.7) |
| Sometimes | 25 (33.3) |
| Often | 19 (25.3) |
| Always | 11 (14.7) |
| Homeschooling affected work productivity | |
| Never | 10 (13.3) |
| Rarely | 16 (21.3) |
| Sometimes | 23 (30.7) |
| Often | 18 (24.0) |
| Always | 8 (10.6) |
| Number of different locations worked ≥ 6 hours in the last 4 weeks, n (%) | |
| 1 | 225 (44.0) |
| 2 | 204 (39.9) |
| 3 | 53 (20.4) |
| Greater than 3 | 29 (5.7) |
| Hours per week, on average, using computerized devices for activities outside of work, mean (SD) | 19.54 (13.7) |
Work Locations and Body Postures
Work locations used most frequently, type of computer used, and body postures were reported before and during the COVID-19 pandemic (Table 3). If respondents used more than one work location, they prioritized their locations as the most, second most and third most often used. Table 3 shows that compared with before the pandemic, during the pandemic a greater number of respondents used locations, computer types and postures that were less likely to be ergonomic, and they used these more often. Chi-squared tests comparing pre-pandemic to setting used most during the pandemic showed significant changes in work location (fewer people working at an office desk (chi-squared = 57.50; df, 4; P < 0.001), computer type (fewer people using a desktop or laptop with external monitor, keyboard and mouse (chi-squared = 96.89, df 1, P < 0.001), and body posture (fewer people sitting straight up (chi-squared = 392.92, df 4, P < 0.001).
TABLE 3.
Work Locations, Computer Types and Body Postures Most Often Used for Work Before and During the COVID-19 Pandemic 2020 in Workers Who Spent ≥75% of Work Time on Computers (n = 511)
| Pre-COVID | During COVID | |||
|---|---|---|---|---|
| Most* | Second Most* | Third Most* | ||
| n (%) | n (%) | n (%) | n (%) | |
| Location | ||||
| Office desk at work | 400 (78.3) | 166 (32.5) | 83 (29.1) | 17 (21.0) |
| Office desk at home | 79 (15.5) | 241 (47.2) | 71 (24.9) | 7 (8.6) |
| Dining room table | 15 (2.9) | 61 (11.9) | 48 (16.8) | 7 (8.6) |
| Kitchen bench/counter | 2 (0.4) | 10 (2.0) | 12 (4.2) | 6 (7.4) |
| Couch | 2 (0.4) | 19 (3.7) | 35 (12.3) | 20 (24.7) |
| Bed | 2 (0.4) | 7 (1.4) | 13 (4.6) | 5 (6.2) |
| Other | 11 (2.2) | 7 (1.4) | 23 (8.2) | 19 (23.4) |
| Computer type† | ||||
| Desktop computer | 213 (41.7) | 139 (27.2) | 47 (16.5) | 9 (11.1) |
| Laptop, external monitor, keyboard, mouse | 236 (46.2) | 234 (45.8) | 84 (29.5) | 6 (7.4) |
| Laptop, external keyboard, mouse | 6 (1.2) | 29 (5.7) | 16 (5.6) | 4 (4.9) |
| Laptop, external mouse only | 26 (5.1) | 38 (7.4) | 38 (13.3) | 12 (14.8) |
| Laptop, no external equipment | 30 (5.9) | 71 (13.9) | 100 (35.1) | 50 (61.7) |
| Body posture† | ||||
| Trunk a little bent forward (A) | 183 (35.8) | 202 (39.5) | 93 (32.6) | 21 (25.9) |
| Straight up, back against backrest (B) | 163 (31.9) | 122 (23.9) | 53 (18.6) | 8 (9.9) |
| Straight up, back NOT against backrest (C) | 56 (11.0) | 53 (10.4) | 42 (14.7) | 7 (8.6) |
| Bottom dropped, lower back not against backrest (D) | 35 (6.8) | 50 (9.8) | 44 (15.4) | 21 (25.9) |
| Variable: alter at least once per 1/2 hr | 74 (14.5) | 84 (16.4) | 53 (18.6) | 24 (29.6) |
*Most often used, second most often used, third most often used; respondents only provided answers for second most/third most if they worked in more than one location for ≥6 hr/wk.
†Respondents provided computer type and body posture for each location where they worked; responses for computer type and body posture are summed, regardless of location.
Musculoskeletal Pain and Disability
Reported discomfort in each body area during last 4 weeks, pain intensity, level of disability, and treatment seeking behavior including medications are tabulated in Table 4. Except for headache, pain intensities and disability were somewhat low (range of means: VAS, 37–42 mm; disability, 14–23%). Depending on the pain location, 30% to 50% of respondents indicated their musculoskeletal problem had worsened during the pandemic.
TABLE 4.
Number of Respondents Reporting Discomfort in each Body Area in the Last 4 Weeks, With Pain and Disability Scores for Each Body Region for Preceding 4 Weeks
| Pain Area | Number of Respondents (%) | Visual Analogue Scale | Number Who Sought Treatment* | Number Who Have Taken Medications* | Number Reporting Pain Worsened During COVID* | Level of Disability (Mean, SD)† |
|---|---|---|---|---|---|---|
| Headache | 122 (23.9) | 42.97 (25.60) | 29 (40.3) | 9 (12.5) | 29 (40.3) | 61.48 (7.62) |
| Neck | 322 (63.0) | 35.65 (22.50) | 132 (52.2) | 153 (60.5) | 97 (38.3) | 17.49 (11.43) |
| Shoulder | 297 (58.1) | 36.88 (23.56) | 108 (50.2) | 144 (67.0) | 73 (34.0) | 19.29 (16.65) |
| Elbow | 61 (11.9) | 42.78 (25.34) | 16 (61.5) | 17 (65.4) | 11 (42.3) | 21.59 (16.81) |
| Wrist/hand | 138 (27.0) | 37.68 (23.93) | 53 (63.9) | 63 (75.9) | 22 (26.5) | 21.05 (15.67) |
| Upper back | 159 (31.1) | 36.95 (21.48) | 50 (51.5) | 71 (73.2) | 29 (29.9) | — |
| Lower back | 280 (54.8) | 39.24 (22.84) | 115 (56.4) | 135 (66.2) | 87 (42.6) | 14.08 (11.45) |
| Hip/thigh | 146 (28.6) | 39.23 (22.77) | 37 (45.1) | 53 (64.6) | 30 (36.6) | 24.22 (23.40)‡ |
| Knee | 106 (20.7) | 36.74 (22.38) | 26 (49.1) | 33 (62.3) | 25 (47.2) | 24.93 (14.90)‡ |
| Ankle/foot | 69 (13.5) | 36.83 (25.85) | 19 (55.9) | 23 (67.6) | 20 (58.8) | 20.27 (21.95)‡ |
*Columns 4, 5, and 6 only include those who selected the specific body area as their most, second most, third most or fourth most discomfort (head n = 72, neck n = 253, shoulder n = 215, elbow n = 26, wrist/hand n = 83, upper back n = 97, lower back n = 204, hip/thigh n = 82, knee n = 53, ankle/foot n = 34) and % are calculated from these totals.
†Column 7 only includes those who selected the body area as their area with most discomfort (head n = 33, neck n = 104, shoulder n = 78, elbow n = 6, wrist/hand n = 20, upper back n = 26 no disability questionnaire for this group, low back n = 100, hip/thigh n = 31, knee n = 18, ankle/foot n = 14. Disability scales were: Headache Impact Tool (headache), Neck Disability Index (neck pain), short version Disabilities of the Shoulder, Arm and Hand Questionnaire (shoulder, elbow and wrist/hand), the Oswestry Disability Index (low back pain), and the Lower Extremity Functional Scale (hip/thigh, knee, ankle/foot).
‡Lower Extremity Functional Scale score has been reversed to allow easier comparison to the other disability scores, i.e., LEFS normally assigns a lower score to lower function, i.e., more disability, but in this table we have reported it in reverse: a higher number representing more disability.
Relationships Between MSD and Work Location or Body Posture
Table 5 reports relationships between MSDs and work locations. There was a statistically significant association between the work location and self-reporting upper back pain (chi-squared (5) = 14.8, P = 0.011). Analysis of the adjusted residuals indicated that the categories where significant differences occurred between the pain and no pain groups were the kitchen bench/counter (adjusted residual ±2.0) and the couch/bed (±3.1). For the kitchen bench/counter category, a higher proportion of people reported upper back pain (4%) than would have been expected under the assumption of independence, i.e., no association, compared with those with no upper back pain who used the kitchen bench/counter less than expected (1%). Similarly, for the couch/bed, the pain group reported higher levels of use than the no pain group (9% vs 2%, Table 5).
TABLE 5.
Number (%) of Respondents (n = 511) With and Without Pain in Specific Body Areas and the Locations Where They Work Most Often, With Associations Between Presence of Pain and Work Location Determined Using Chi-Squared
| Pain Area (n) | Office Desk at Work | Office Desk at Home | Dining Room Table | Kitchen Bench/Counter | Couch/Bed | Other | Significance (P) |
|---|---|---|---|---|---|---|---|
| Headache | |||||||
| Males* | |||||||
| Pain (21) | 8 (38) | 11 | 1 (52) | 0 (0) | 1 (5) | 0 (0) | |
| No pain (104) | 28 (27) | 58 (56) | 13 (13) | 0 (0) | 4 (4) | 1 (1) | |
| Females* | |||||||
| Pain (101) | 38 (38) | 44 (44) | 10 (10) | 4 (4) | 4 (4) | 1 (1) | |
| No pain (224) | 76 (34) | 99 (44) | 29 (13) | 5 (2) | 12 (5) | 3 (1) | |
| Total | |||||||
| Pain (122) | 46 (38) | 55 (45) | 11 (9) | 4 (3) | 5 (4) | 1 (1) | 0.587 |
| No pain (330) | 105 (32) | 158 (48) | 42 (13) | 5 (2) | 16 (5) | 4 (1) | |
| Neck | |||||||
| Males | |||||||
| Pain (70) | 20 (29) | 44 (63) | 3 (4) | 0 (0) | 2 (3) | 1 (1) | |
| No pain (55) | 16 (29) | 25 (46) | 11 (20) | 0 (0) | 3 (6) | 0 (0) | |
| Females | |||||||
| Pain (251) | 84 (34) | 112 (45) | 33 (13) | 8 (3) | 11 (4) | 3 (1) | |
| No pain (74) | 30 (41) | 31 (42) | 6 (8) | 1 (1) | 5 (7) | 1 (1) | |
| Total | |||||||
| Pain (322) | 104 (32) | 157 (49) | 36 (11) | 8 (3) | 13 (4) | 4 (1) | 0.582 |
| No pain (130) | 47 (36) | 56 (43) | 17 (13) | 1 (1) | 8 (6) | 1 (1) | |
| Shoulder | |||||||
| Males | |||||||
| Pain (61) | 15 (25) | 33 (54) | 9 (15) | 0 (0) | 3 (5) | 1 (2) | |
| No pain (64) | 21 (33) | 36 (56) | 5 (8) | 0 (0) | 2 (3) | 0 (0) | |
| Females | |||||||
| Pain (235) | 85 (36) | 97 (41) | 31 (13) | 7 (3) | 13 (6) | 2 (1) | |
| No pain (90) | 29 (32) | 46 (51) | 8 (9) | 2 (2) | 3 (3) | 2 (2) | |
| Total | |||||||
| Pain (297) | 100 (34) | 131 (44) | 40 (14) | 7 (2) | 16 (5) | 3 (1) | 0.346 |
| No pain (155) | 51 (33) | 82 (53) | 13 (8) | 2 (1) | 5 (3) | 2 (1) | |
| Upper back | |||||||
| Males | |||||||
| Pain (36) | 8 (22) | 21 (58) | 1 (3) | 0 (0) | 5 (14) | 1 (3) | |
| No pain (89) | 28 (32) | 48 (54) | 13 (15) | 0 (0) | 0 (0) | 0 (0) | |
| Females | |||||||
| Pain (123) | 39 (32) | 53 (43) | 15 (12) | 6 (5) | 7 (4) | 1 (1) | |
| No pain (202) | 75 (37) | 90 (45) | 24 (12) | 3 (2) | 16 (5) | 3 (2) | |
| Total | |||||||
| Pain (159) | 47 (30) | 74 (47) | 16 (10) | 6 (4)† | 14 (9)† | 2 (1) | 0.011‡ |
| No pain (293) | 104 (36) | 139 (47) | 37 (13) | 3 (1) | 7 (2) | 3 (1) | |
| Lower back | |||||||
| Males | |||||||
| Pain (84) | 29 (35) | 45 (54) | 7 (8) | 0 (0) | 3 (4) | 0 (0) | |
| No pain (41) | 7 (17) | 24 (59) | 7 (17.1) | 0 (0) | 2 (5) | 1 (2) | |
| Females | |||||||
| Pain (195) | 63 (32) | 88 (45) | 21 (11) | 6 (3) | 14 (7) | 3 (2) | |
| No pain (130) | 51 (39) | 55 (42) | 18 (14) | 3 (2) | 2 (2) | 1 (1) | |
| Total | |||||||
| Pain (280) | 92 (33) | 134 (48) | 28 (10) | 6 (2) | 17 (6) | 3 (1) | 0.377 |
| No pain (172) | 59 (34) | 79 (46) | 25 (15) | 3 (2) | 4 (2) | 2 (1) | |
| Hip/thigh | |||||||
| Males | |||||||
| Pain (33) | 9 (27) | 20 (61) | 4 (12) | 0 (0) | 0 (0) | 0 (0) | |
| No pain (92) | 27 (29) | 49 (53) | 10 (11) | 0 (0) | 5 (5) | 1 (1) | |
| Females | |||||||
| Pain (113) | 33 (29) | 54 (48) | 14 (12) | 5 (4) | 6 (5) | 1 (1) | |
| No pain (212) | 81 (38) | 89 (42) | 25 (12) | 4 (2) | 10 (5) | 3 (1) | |
| Total | |||||||
| Pain (146) | 42 (29) | 74 (51) | 18 (12) | 5 (3) | 6 (4) | 1 (1) | 0.448 |
| No pain (306) | 109 (36) | 139 (45) | 35 (11) | 4 (1) | 15 (5) | 4 (1) | |
| CES-D 10 | |||||||
| Males | |||||||
| Depressed (45) | 17 (38) | 23 (51) | 4 (9) | 0 (0) | 1 (2) | 1 (2) | |
| Not depressed (84) | 21 (25) | 50 (60) | 8 (10) | 0 (0) | 3 (4) | 3 (4) | |
| Females | |||||||
| Depressed (159) | 59 (37) | 61 (38) | 20 (13) | 4 (3) | 11 (7) | 11 (7) | |
| Not depressed (145) | 51 (35) | 71 (49) | 15 (10) | 3 (2) | 4 (3) | ||
| Total | 4 (3) | ||||||
| Depressed (204) | 76 (37) | 84 (41) | 24 (12) | 4 (2) | 9 (4) | 4 (2) | 0.416 |
| Not depressed (231) | 73 (32) | 122 (53) | 23 (10) | 3 (1) | 5 (2) | 3 (1) |
*Male and female numbers do not sum to totals, as some participants did not identify as male or female or chose not to answer.
†The category pairs contributing most to the chi-squared statistic, defined by adjusted standardized residual of ≥2.
‡P < 0.05, therefore the relationship is statistically significant.
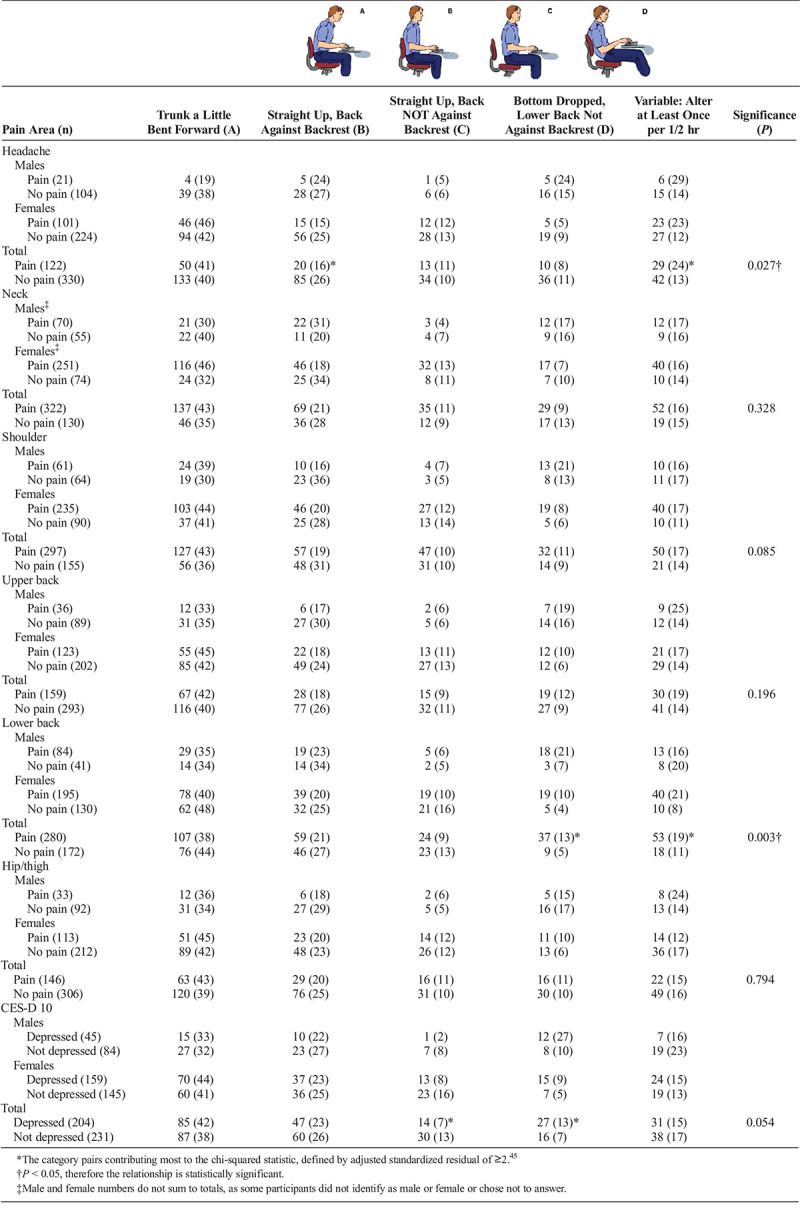
Table 6 reports relationships between MSD and reported body postures commonly used. Body posture was associated with having headache (chi-squared (4) = 10.9, P = 0.027) and with having lower back pain (chi-squared (4) = 16.3, P = 0.003). The categories where significant differences occurred between the headache and no headache groups were the straight up, back against backrest posture (adjusted residuals ±2.1) and the variable posture (±2.9). A lower proportion of people reporting headache sat with their back straight up, against the backrest (16%) compared with those with no headache (26%), whereas this was reversed for variable postures where a higher proportion with headache (24%) used variable postures compared with those without headache (13%). For the low back pain analysis, the significant differences between pain and no pain groups were for the bottom dropped posture (adjusted residual ±2.7) and the variable posture (±2.4). A higher proportion of people with lower back pain compared with no low back pain reported they sat most often with their bottom dropped, lower back not against backrest (13 vs 5%) or used variable postures (19 vs 11%, Table 6). Approaching significance (chi-squared (4) = 9.3, P = 0.054) was a relationship between having depression and body posture, with the categories contributing most to this relationship being sitting straight up, back not against a backrest (adjusted residual ±2.1) and bottom dropped (±2.2). A lower proportion with depression compared with not depressed sat straight up, back not against a backrest (7 vs 13%) and a higher proportion sat with bottom dropped (13 vs 7%). Nonsignificant interaction effects between gender and pain in the multinomial logistic regression models suggested that gender did not affect the relationships between condition and location or body posture.
TABLE 6.
Number (%) of Respondents (n = 511) With and Without Pain in Specific Body Areas and the Body Posture They Reported They Used Most Often, With Associations Between Presence of Pain and Body Posture Determined Using Chi-Squared
DISCUSSION
This survey reports the impact of work practices on work-related MSDs and depressive symptoms during the COVID-19 pandemic in 2020 when flexible work practices initially proliferated. It is the first study to quantify pain disability using standardized outcome measures. We surveyed 511 frequent computer users (≥75% of working time). Most respondents (88%, n = 452) had work-related pain. The most common painful areas were neck (63%, n = 322), shoulder (58%, n = 297), low back (55%, n = 280), and upper back (31%, n = 159). Forty percent (n = 204) were categorized as depressed based on the CESD-10. Eighty percent (n = 413) reported they had increased the amount of time they worked at home since the onset of the pandemic. Compared to before the pandemic, more respondents reported working in locations less likely to be ergonomic, e.g., dining room table, couch/bed; fewer used a desktop computer most of the time. Chi-squared analysis suggested respondents with upper back pain worked more often at the kitchen bench/counter or on the couch or bed than those without upper back pain. Those with headache used more variable postures and fewer sat straight up back against a backrest than those without headache. Respondents with lower back pain sat more often in a leaned back posture, with bottom dropped or used variable postures. Approaching significance at P = 0.054, respondents with depression tended to sit more often in the leaned back, bottom dropped posture and less often straight up back against a back rest compared to those without depression. Gender did not significantly affect the relationships between pain and location or body posture. Together these results suggest COVID-19 has changed work habits, and many work from home habits appear to exacerbate MSD, particularly back pain and headache.
Changes in Work Environments and Postures During COVID-19 Pandemic
Respondents spent more time working at home during the COVID-19 pandemic in 2020, and they reported using nonergonomic work environments and postures more often than before pandemic. This is similar to a survey of 51 Italian computer users working at home during the pandemic, where a majority reported using nonergonomic workstation components (e.g., nonadjustable chairs without casters, dining tables) and for 50%, it exacerbated their neck and shoulder pain.35 In the current study, during the pandemic fewer people used an office desk (either at work or home), and fewer used a desktop computer or laptop with monitor, keyboard and mouse as compared with before the pandemic. Alternative, less ergonomic work configurations were used more often, such as a laptop on its own without peripherals, or sitting on the couch. These ergonomic practices may contribute to postures that place greater loads on musculoskeletal structures, leading to MSD. Studies measuring three-dimensional postures show that less ergonomic workstation configurations lead to increased muscle activity36 and poor postures (e.g., greater head and neck flexion) in individuals with and without MSD.37,38 Indeed, compared with before the pandemic, during the pandemic fewer respondents reported their most common body posture while working was sitting straight up with their back against a backrest. Poor postures may contribute to MSD39,40 and may be reflected in the high numbers of participants reporting MSD in the current study. These findings suggest that during the pandemic, working at home led to work practices that may have placed workers at risk for MSD.
Relationships Between Work Environments, Postures and Pain Disability
The work locations and body postures that respondents used most often during the pandemic were related to having MSD in specific body areas. Having upper back pain was more common in people who used the dining table or couch/bed most often for work. Using a couch or bed is likely to result in greater upper back, head, and neck flexion, which would be expected to increase stress on back and neck structures. Indeed, flexed postures at a desk have been shown to be associated with MSD.40 A previous study also suggested not using an ergonomic office chair or desk at home was associated with reporting greater work-related musculoskeletal pain when working at home compared with the office.14 Related to posture, a greater number of people with low back pain reported they sat most often with their bottom dropped, lower back not against the backrest. Similar postures on a couch or bed have been shown to cause pain in normally asymptomatic individuals.41 Those with headache were less likely to report their most common body posture was sitting straight up, and more likely to use variable body postures. Using variable body postures may be a coping mechanism, as previous studies have shown that having less variability in spinal posture is related to having headache.42,43 It is possible the body postures associated with low back pain or headache contributed to symptoms, or respondents used certain postures to ameliorate their symptoms. As this survey was cross-sectional, we cannot determine the cause or effect.
Relationships Between Work Environments, Postures and Depression
Forty percent of respondents had depressive symptoms as classified by the CESD-10. This is higher than the 20% office workers previously reported in a Turkish study who were all working at home during the pandemic,44 and lower than the 63% of a New Zealand general population classified as depressed during the pandemic. Both of these other studies used different scales than the current study to classify depression, the Depression Anxiety Stress Questionnaire-Short Form in the Turkish study and the Patient Health Questionnaire in the New Zealand one, which may be one reason for differences. A previous study of workers in a shared office space found that satisfaction related to the workspace itself (e.g., furniture, acoustics) was associated with a number of well-being outcomes.46 Our study did not find any links between the physical work location and having depressive symptoms, but we found a weak relationship (chi-squared P value = 0.054) between the body posture most often used for work and having depressive symptoms. More people with depressive symptoms used a leant back, bottom dropped posture and fewer sat straight up compared with those without depressive symptoms. These postures may have been a result of having depressive symptoms, rather than a cause of it, however longitudinal studies would be required to determine this. Nevertheless, the observed relationship between depressive symptoms and postures suggests that interventions to change postures may possibly have an incidental effect on depression and could be explored in future research.
Strengths and Limitations
With over 500 responses to our survey from 42 countries, this study provides broad perspectives on work practices across the globe. However, 75% of respondents were from Australia or the United Kingdom, and 85% had a university degree, limiting generalizability to these populations. A strength of this study was the use of validated questionnaires to quantify disability due to pain. A large proportion of our respondents (89%) reported having MSD, potentially suggesting recruitment methods contributed and prevalence of MSD in this population may be over-estimated. However, similarly high prevalence of MSD (71%) was also reported in another survey of computer users working at home35 during the pandemic. Due to the nature of recruitment using social media and snowball sampling, an exact survey response rate could not be calculated. A larger sample size may have produced different results.
IMPLICATIONS
With the observed relationships between MSD and work environments and postures in the current study, it is important that practitioners who treat patients with MSD consider the work environment and assess whether changes to the patient’s work environment may assist their condition. Interventions to alter the work environment have included ergonomic workstation assessments,47 posture education,48 and activity prompts.49 While the evidence for individual interventions is weak,50,51 they are more effective in the context of a worker’s specific tasks.52 Employers, human resources, and health and safety professionals who oversee employee health should consider the ergonomics of work from home and potentially intervene to prevent or reduce MSD. Future longitudinal and intervention studies are needed to determine if MSD changes over time in response to changes in work environments or postures, and the effects of any interventions.
CONCLUSION
COVID-19 has changed the work environments and postures of frequent computer users. MSD and depression are commonly reported. Nonergonomic work environments are related to having upper back pain, and nonergonomic postures are related to having headache, lower back pain and approaching significance, depression. These results support the development of interventions to improve work from home practices that may ultimately provide recommendations for preventing or reducing work-related MSD in the new working normal.
ACKNOWLEDGMENTS
The authors would like to acknowledge Kim Colyvas, statistician, for his assistance.
Footnotes
Ethics approval: Ethics approval was obtained from Human Ethics Committee of The University of Newcastle [H-2020-2224]. All methods were performed in accordance with the relevant guidelines and regulations.
Author contributions: S.S., S.E., N.H., E.P., C.J. participated in the study concept and design. S.S., S.E., C.J. participated in the acquisition of data. S.S., S.E., C.J. participated in the design of data analysis plan. S.S., S.E., N.H., E.P., C.J. participated in the analysis and interpretation. S.S. I.W. participated in the drafting of the article. S.S. I.W. S.E. N.H. E.P. C.J. participated in the critical review and final approval of the article.
Competing Interests Statement: There are no competing interests to report.
Source(s) of support: No external sources of funding support.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
Contributor Information
Ishanka Weerasekara, Email: ishanka.weerasekara@uon.edu.au.
Suzi Edwards, Email: suzi.edwards@sydney.edu.au.
Nicola R. Heneghan, Email: n.heneghan@bham.ac.uk.
Emilio J. Puentedura, Email: louie_puentedura@baylor.edu.
Carole James, Email: carole.james@newcastle.edu.au.
REFERENCES
- 1.World Health Organisation . Musculoskeletal conditions. 2019. Available at: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions. Accessed September 20, 2022.
- 2.Pezzullo L, Crook A. NOHSAC Technical Report 4: The economic and social costs of occupational disease and injury in New Zealand. Wellington; 2006. [Google Scholar]
- 3.Safe work Australia . Cost injury and illness statistics 2021. Available at: https://www.safeworkaustralia.gov.au/resources-and-publications/statistical-reports/cost-work-related-injury-and-illness-australian-employers-workers-and-community-2012-13. Accessed September 20, 2022.
- 4.Safe Work Australia . Canberra: Australian Government. 2021. Available at: https://www.safeworkaustralia.gov.au/doc/australian-workers-compensation-statistics-2018-19. Accessed September 20, 2022.
- 5.In Workplace (Liberty Mutual Workplace Safety Index). Hopkinton, MA: Liberty Mutual Research Institute for Safety; 2016. [Google Scholar]
- 6.James C, et al. Musculoskeletal discomfort and use of computers in the university environment. Appl Ergon. 2018;69:128–135. [DOI] [PubMed] [Google Scholar]
- 7.Isusi I. Work-related musculoskeletal disorders: facts and figures—synthesis report of 10 EU member states reports. European Agency for Safety and Health at Work, Luxembourg: Publications Office of the European Union; 2020. [Google Scholar]
- 8.Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain—where to from here? Am J Public Health. 2019;109:35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaliniene G, Ustinaviciene R, Skemiene L, Vaiciulis V, Vasilavicius P. Associations between musculoskeletal pain and work-related factors among public service sector computer workers in Kaunas County, Lithuania. BMC Musculoskelet Disord. 2016;17:420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Musculoskeletal Disorders and the Workplace . National Research Council (US) and Institute of Medicine (US) Panel on Musculoskeletal Disorders and the Workplace. Washington (DC): National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 11.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14:13–23. [DOI] [PubMed] [Google Scholar]
- 12.Aytutuldu GK, Birinci T, Tarakcı E. Musculoskeletal pain and its relation to individual and work-related factors: a cross-sectional study among Turkish office workers who work using computers. Int J Occup Saf Ergon. 2020;28:790–797. [DOI] [PubMed] [Google Scholar]
- 13.Lee S, De Barros FC, De Castro CSM, DE Oliveira Sato T. Effect of an ergonomic intervention involving workstation adjustments on musculoskeletal pain in office workers—a randomized controlled clinical trial. Ind Health. 2021;59:78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radulović AH Žaja R Milošević M, et al. Work from home and musculoskeletal pain in telecommunications workers during COVID-19 pandemic: a pilot study. Arh Hig Rada Toksikol. 2021;72:232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazekami S. Mechanisms to improve labor productivity by performing telework. Telecommun Policy. 2020;44:101868. [Google Scholar]
- 16.Giménez-Nadal JI, Molina JA, Velilla J. Work time and well-being for workers at home: evidence from the American Time Use Survey. Int J Manpow. 2020;41:184–206. [Google Scholar]
- 17.Henke RM Benevent R Schulte P, et al. The effects of telecommuting intensity on employee health. Am J Health Promot. 2016;30:604–612. [DOI] [PubMed] [Google Scholar]
- 18.Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health. 2020;20:1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hornung S, Glaser J. Home-based telecommuting and quality of life: further evidence on an employee-oriented human resource practice. Psychol Rep. 2009;104:395–402. [DOI] [PubMed] [Google Scholar]
- 20.Windeler JB, Chudoba KM, Sundrup RZ. Getting away from them all: managing exhaustion from social interaction with telework. J Organ Behav. 2017;38:977–995. [Google Scholar]
- 21.Bosua R, Gloet M, Kurnia S, Mendoza A, Yong J. Telework, productivity and wellbeing: an Australian perspective. Telecommunications Journal of Australia. 2013;63. [Google Scholar]
- 22.Anderson AJ, Kaplan SA, Vega RP. The impact of telework on emotional experience: when, and for whom, does telework improve daily affective well-being? Eur J Work Organ Psy. 2015;24:882–897. [Google Scholar]
- 23.Kaduk A, Genadek K, Kelly EL, Moen P. Involuntary vs. voluntary flexible work: insights for scholars and stakeholders. Community Work Fam. 2019;22:412–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen C, Finsen L, Søgaard K, Christensen H. Musculoskeletal symptoms and duration of computer and mouse use. Int J Ind Ergon. 2002;30:265–275. [Google Scholar]
- 26.Crawford JO. The Nordic musculoskeletal questionnaire. Occup Med. 2007;57:300–301. [Google Scholar]
- 27.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 28.IJmker S Mikkers J Blatter BM, et al. Test-retest reliability and concurrent validity of a web-based questionnaire measuring workstation and individual correlates of work postures during computer work. Appl Ergon. 2008;39:685–696. [DOI] [PubMed] [Google Scholar]
- 29.Kosinski M Bayliss MS Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12:963–974. [DOI] [PubMed] [Google Scholar]
- 30.Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manip Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 31.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. [DOI] [PubMed] [Google Scholar]
- 33.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (lefs): scale development, measurement properties, and clinical application. Phys Ther. 1999;79:371–383. [PubMed] [Google Scholar]
- 34.Amireault S, Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept Mot Skills. 2015;120:604–622. [DOI] [PubMed] [Google Scholar]
- 35.Moretti A Menna F Aulicino M, et al. Characterization of home working population during covid-19 emergency: a cross-sectional analysis. Int J Environ Res Public Health. 2020;17:6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seghers J, Jochem A, Spaepen A. Posture, muscle activity and muscle fatigue in prolonged VDT work at different screen height settings. Ergonomics. 2003;46:714–730. [DOI] [PubMed] [Google Scholar]
- 37.Yu Z, James C, Edwards S, Snodgrass SJ. Differences in posture kinematics between using a tablet, a laptop, and a desktop computer in sitting and in standing. Work. 2018;61:57–266. [DOI] [PubMed] [Google Scholar]
- 38.Lee R, James C, Edwards S, Snodgrass SJ. Posture During the use of electronic devices in people with chronic neck pain: a 3D motion analysis project. Work. 2021;68:491–505. [DOI] [PubMed] [Google Scholar]
- 39.Dolphens M Vansteelandt S Cagnie B, et al. Multivariable modeling of factors associated with spinal pain in young adolescence. Eur Spine J. 2016;25:2809–2821. [DOI] [PubMed] [Google Scholar]
- 40.Brink Y, Louw Q, Grimmer K, Jordaan E. The relationship between sitting posture and seated-related upper quadrant musculoskeletal pain in computing South African adolescents: a prospective study. Man Ther. 2015;20:820–826. [DOI] [PubMed] [Google Scholar]
- 41.Gold JE, Driban JB, Yingling VR, Komaroff E. Characterization of posture and comfort in laptop users in non-desk settings. Appl Ergon. 2012;43:392–399. [DOI] [PubMed] [Google Scholar]
- 42.Mingels S, Dankaerts W, van Etten L, Bruckers L, Granitzer M. Spinal postural variability relates to biopsychosocial variables in patients with cervicogenic headache. Sci Rep. 2021;11:13783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mingels S, Dankaerts W, van Etten L, Bruckers L, Granitzer M. Lower spinal postural variability during laptop-work in subjects with cervicogenic headache compared to healthy controls. Sci Rep. 2021;11:5159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Şentürk E, Sağaltıcı E, Geniş B, Günday Toker Ö. Predictors of depression, anxiety and stress among remote workers during the COVID-19 pandemic. Work. 2021;70:41–51. [DOI] [PubMed] [Google Scholar]
- 45.Agresti A. Categorical Data Analysis, 3rd ed. Hoboken, New Jersey: John Wiley & Sons; 2013. [Google Scholar]
- 46.Lusa S, Käpykangas SM, Ansio H, Houni P, Uitti J. Employee satisfaction with working space and its association with well-being-a cross-sectional study in a multi-space office. Front Public Health. 2019;7:358–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Esmaeilzadeh S, Ozcan E, Capan N. Effects of ergonomic intervention on work-related upper extremity musculoskeletal disorders among computer workers: a randomized controlled trial. Int Arch Occup Environ Health. 2014;87:73–83. [DOI] [PubMed] [Google Scholar]
- 48.Pillastrini P de Lima E Sá Resende F Banchelli F, et al. Effectiveness of global postural re-education in patients with chronic nonspecific neck pain: randomized controlled trial. Phys Ther. 2016;96:1408–1416. [DOI] [PubMed] [Google Scholar]
- 49.Waongenngarm P, Areerak K, Janwantanakul P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: a systematic review of randomized and non-randomized controlled trials. Appl Ergon. 2018;68:230–239. [DOI] [PubMed] [Google Scholar]
- 50.Hoe VC, Urquhart DM, Kelsall HL, Zamri EN, Sim MR. Ergonomic interventions for preventing work-related musculoskeletal disorders of the upper limb and neck among office workers. Cochrane Database Syst Rev. 2018;10:CD008570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luger T, Maher CG, Rieger MA, Steinhilber B. Work-break schedules for preventing musculoskeletal symptoms and disorders in healthy workers. Cochrane Database Syst Rev. 2019;7:CD012886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Robertson MM, Huang YH, Lee J. Improvements in musculoskeletal health and computing behaviors: effects of a macroergonomics office workplace and training intervention. Appl Ergon. 2017;62:182–196. [DOI] [PubMed] [Google Scholar]


