The COVID-19 pandemic accelerated the transition to working from home for many people. Our results suggest that this represents an opportunity for increased flexibility and inclusion of people with chronic conditions and caregivers in the workplace without impacting productivity. Our findings also emphasize the importance of considering sociodemographic differences.
Keywords: working from home, work productivity loss, absenteeism, presenteeism, caregiver, patient
Objective
The aim of this study was to measure the association of working from home (WFH) with work productivity loss due to caregiving responsibilities or health problems during the COVID-19 pandemic.
Methods
We conducted an online survey of family/friend caregivers (n = 150 WFH/75 non-WFH) and patients (n = 95/91) who worked during the past 7 days in May and July 2020, respectively. Absenteeism and presenteeism were measured using the Valuation of Lost Productivity questionnaire.
Results
Working from home was associated with higher odds of absenteeism (odds ratio, 2.53; 95% confidence interval, 1.11 to 5.77) and presenteeism (2.79; 1.26 to 6.18) among caregivers and higher odds of presenteeism among patients (2.78; 1.13 to 6.84). However, among caregivers with absenteeism more than 0 days, WFH was significantly associated with fewer absent workdays.
Conclusions
Working from home was not associated with overall absenteeism and presenteeism in caregivers or patients. Working from home allows a more flexible and inclusive workplace without impacting productivity, although further research is needed.
Working from home (WFH) has been researched since the 1980s under a broader term “telework.”1 The term “telework” was first coined by Nilles1 as “includes all work-related substitutions of telecommunications and related information technologies for travel (from substation of telephone calls or electronic mail for personal visits to the use of full-motion videoconferencing as a substitute for executive travel).” Early studies in the 1970s and 1980s focused on telecommuting-induced travel impacts by measuring WFH time and commute distance and time.1 In more recent studies (2000–2020) systematically reviewed by Athanasiadou and Theriou,2 there was a lack of universally accepted definition of telework, and terms, such as “telework,” “homeworking,” “telehomeworking,” “working from home,” “telecommuting,” “remote working,” “virtual work,” and “e-work,” have been used interchangeably in the literature. However, researchers have commonly distinguished and studied three main types of telework: a) home-based work or WFH; b) group-based teleworking in a satellite office or neighborhood office centers that are remote from the main office but close to employees; and c) mobile telework that “usually involves travel and/or spending time at the customers' premises.”2,3
Work productivity is one of the main telework outcomes in recent studies.2,4 According to Athanasiadou and Theriou2 and a review of national studies from 15 countries conducted by Messenger et al,4 most studies suggested teleworking improves individual work productivity. A meta-analysis also found a small but positive association between teleworking and perceptions of increased productivity.5 However, there were a few exceptions. Dutcher6 demonstrated that teleworking had a positive effect on productivity for creative tasks but a negative effect on productivity for dull tasks. Perez et al7 showed a negative relationship between telework and productivity when the teleworker has a dual role, including raising children.
Working from home became a more common or only option for many workplaces because of the public health measures at the beginning of the COVID-19 pandemic. Studies have been conducted to measure the impact of WFH on work productivity among working populations during the pandemic. These results were mixed depending on the setting, population, occupation, and time of the survey.8–18 Smite et al8 reviewed 13 surveys conducted in different countries to measure the changes in perceived productivity among the software engineers during the pandemic; in four surveys, most respondents reported decreased productivity; in six surveys, most respondents reported no changes; and in three surveys, most respondents reported increased productivity. Based on the Labour Force Survey conducted by Statistics Canada, 90% of employees who usually worked outside the home before the pandemic but worked most of their hours at home during February 14 to 20, 2021, reported being at least as productive as they were in their usual workplace (58% the same and 32% more productive).19 Awada et al9 found that the overall perception of productivity did not change compared with in-office productivity before the pandemic among survey respondents who were WFH in the United States. However, the number of hours spent at a workstation increased by 1.5 hours during a typical WFH day. In contrast, Huls et al10 found that survey respondents from the Netherlands, who had paid work for at least 24 hours per week and worked at home at least 4 hours per week because of lockdown, spent 4.8 less hours per week (14%) on paid work, and their productivity decreased by 5.5%.
Decreased work productivity was also observed among a working population in Austria,14 workers in manufacturing firms in Japan,12 and a representative sample of employees and employers in Japan.18 On the other hand, increased work productivity was observed among certain professions who worked from home only part time in the United States,11 vocational counseling psychologists in Switzerland,13 inpatient and infusion pharmacists at a US comprehensive cancer center,15 pediatric neuroradiologists in a US quaternary pediatric academic hospital,16 and public health workers from a large local health district in Australia.17
In the working-age population, there is a high proportion of people who are living with at least one chronic condition (ie, patients) or who are providing care or help family members or friends with a chronic condition, a physical or mental disability, or problems related to aging (ie, caregivers who are family members or friends instead of paid professionals). In Canada, the percentage of population that reports having been diagnosed with at least 1 of 10 common chronic conditions is 23.8% in the age group of 20 to 34 years, 31.0% in the age group of 35 to 49 years, and 51.6% in the age group of 50 to 64 years.20 The proportion of people who are caregivers by age group is 16.8% for 25 to 34 years, 20.4% for 35 to 44 years, 32.9% for 45 to 54 years, and 33.9% for 55 to 64 years.21 Studies have demonstrated the higher work productivity loss due to health problems among patients22–25 or caregiving responsibilities among caregivers.25–27
Only a few studies measured the impact of WFH on work productivity loss due to health problems during the pandemic. One study among a random sample of employees working in the Austrian finance, insurance, and IT sectors suggested that WFH was not directly associated with increased sickness presenteeism propensity (defined as the probability that an employee chooses presence at work over absence from work when sick).28 Shimura et al29 found that remote working 5 days a week was associated with higher odds of worsening health-related presenteeism (defined as work productivity loss at work) compared with 0-day remote working among a sample of workers from 23 companies from tertiary industries in Japan.
The impact of WFH on work productivity loss among patients and caregivers during the COVID-19 pandemic remains unclear. Our objectives were to measure the associations of WFH with having work productivity loss (absenteeism or presenteeism), work productivity loss among those with absenteeism or presenteeism, and total absenteeism and total presenteeism due to a) caregiving responsibilities among caregivers who were caring for a family member or friend living with a chronic condition, and b) health problems among patients.
METHODS
Study Design and Population
Both caregivers and patients were recruited from online panel of Ipsos, a market research company, with predefined quota to represent the age (25 to 64 years), sex, and province/region distribution of Canada's caregiver population30 and patient population.20 We targeted a sample of 400 caregivers, at least 200 of whom had worked in the past 7 days before completing the survey, and a sample of 200 patients who had worked in the past 7 days. The online survey was conducted among caregivers on May 15, 2020, to June 2, 2020, and among patients on July 11, 2020, to July 17, 2020.
At our screening stage, we defined caregivers as individuals who were “currently caring for a family member or friend living with a chronic condition (a long-term condition diagnosed by a health professional lasting 6 months or longer).” Patients were defined as individuals who were currently living with any of 25 chronic conditions (a long-term condition diagnosed by a health professional lasting 6 months or longer), including allergies; Alzheimer's disease or any dementia; anxiety disorder; arthritis; asthma; autism; bowel disorders; cancer; chronic bronchitis, emphysema, or chronic obstructive pulmonary disease; chronic pain; diabetes; Down syndrome; fibromyalgia; heart disease; high blood cholesterol or lipids; high blood pressure; kidney disease; migraines; mood disorder; multiple sclerosis; osteoporosis; sleep apnea; stomach ulcers; stroke; and urinary incontinence.
This study was approved by the University of British Columbia–Providence Health Care Research Ethics Board (Ethics Certificate No. H19-00329). The online survey participants provided their consent online to continue the survey.
Dependent Variables
The Valuation of Lost Productivity (VOLP) questionnaire was the main component of the online survey. The VOLP, measuring productivity loss due to health problems among patients, has been validated and used for different diseases such as rheumatoid arthritis, asthma, systemic autoimmune rheumatic disease, cardiovascular disease/risk, and multiple sclerosis.31–39 The VOLP was then adapted and validated to measure work productivity loss due to caregiving responsibilities among caregivers.40 The dependent variables of this study were absenteeism and presenteeism. Absenteeism was defined as the number of absent work days due to caregiving responsibilities for caregivers or due to health for patients in the past 3 months. Presenteeism, indicating reduced work productivity while working, was measured by the percentage time loss while working in the past 7 days due to caregiving responsibilities for caregivers or due to health for patients. The percentage time loss was derived from the following formula: , where A is the total hours survey respondents took to complete all work in the past 7 days, and B is the total hours survey respondents would take to complete the same work if they did not have caregiving responsibilities or did not experience any health problems.32,40
Key Independent Variable
Among those who answered yes to “In the past 7 days, have you worked” in the VOLP, we further asked whether they worked from home (yes vs no). The survey respondents were then categorized into WFH and non-WFH groups.
Potential Confounders
We considered the following potential confounders: 1) demographic characteristics including age as a categorical variable (25 to 34, 35 to 44, 45 to 54, or 55 to 64), sex (male or female), ethnicity (Asian, European, or others), marital status (currently married or common law vs widowed, divorced, separated, or never married), and province; 2) socioeconomic status including personal income as a categorical variable (<$50,000, $50,000 to $99,999, and $100,000 or more) and highest education completed (high school or under, college or technical/trade, university, and postgraduate or professional designation); 3) health status including self-rated health status (excellent or very good, good, or fair or poor), patient self-rated chronic condition severity level (mild, moderate, or severe), and care receiver's chronic condition severity level as rated by caregivers; and 4) work-related characteristics including current employment status (full time, part time, or self-employed) and occupation (management; business, finance, and administration; natural and applied sciences and related; education, law and social, community and government services; sales and service; or other), which was categorized based on the National Occupation Classification 2016 version 1.1.41
For patient respondents, we also measured their work habits (usually sit; stand or walk quite a lot; or often have to climb stairs or hills, usually lift or carry light loads, or do heavy work or carry very heavy loads) and the frequency of working within a team (none or a little of the time, some of the time, or most or all of the time). For caregiver respondents, we measured caregiver respondents including caregiving length (less than 1 year, 1 to 3 years, 3 to 5 years, or more than 5 years), caregiving hours (total hours spent on all caregiving responsibilities including household activities and tasks, personal care, practical support, emotional support, and other responsibilities) in the past 7 days, whether they were compensated for their caregiving time (yes or no), and whether their care receivers received care from other informal or professional caregivers at home in the past 7 days (yes or no). The categorization of each variable above ensured at least five respondents for each category by WFH status.
Statistical Analysis
Descriptive statistics of the WFH and non-WFH groups among caregivers and patients were reported. Categorical variables were compared using Pearson chi-square or Fisher exact tests, whereas continuous variables were compared using the Wilcoxon rank sum test. Because of inflated zeros and highly skewed data distribution, we used two-part models as suggested from previous studies42–44 to measure the association between WFH and work productivity loss (absenteeism or presenteeism) among patients and caregivers separately. Logistic regression models were used for the first part to measure the probabilities of having any absenteeism or having any presenteeism. Gamma regression was used for the second part of absenteeism >0 because of the skewed data distribution,42–44 whereas Beta regression was used for presenteeism >0 because of the presenteeism outcome range of 0 to 1.42,45 The average marginal effects of WFH on overall absenteeism and presenteeism and 95% confidence interval (CI) were then calculated using Bootstrap methods with 5000 replications.
For final model selection, we started by including all potential confounders that differed between the WFH group and the non-WFH group with P < 0.2 among caregivers or patients.46 In our final multivariable regressions, we adjusted for all possible confounders except income for four reasons: 1) its associations with the outcomes were not significant at α = .05 in all the multivariable logistic regressions; 2) removing the variable from the regression models did not change the coefficient size of the association of WFH with all the outcomes; 3) removing the variable improved the model fit in terms of the Bayesian Information Criterion from all logistic regression models; and 4) removing the variable increased sample size for both patients and caregivers because a higher proportion of survey participants preferred not to report their income. We performed all analyses using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Among the targeted 400 caregivers, we excluded respondents who did not work in the past 7 days (n = 159), reported total caregiving hours deemed too long (ie, more than 126 hours in the past 7 days assuming the average individual would get 6 hours of sleep) (n = 9), or did not provide valid answers for confounders (n = 7). The final sample size included for analysis was 225 caregivers. Among the targeted 200 patients, after excluding respondents who did not have at least one chronic condition (n = 1) or did not work in the past 7 days (n = 13), we ended up with a sample size of 186 patients.
Sample Characteristics by WFH Status
Table 1 and Table S1 (in Supplemental Digital Content 1, http://links.lww.com/JOM/B176) present caregiver and patient characteristics by WFH status. There were 150 caregivers and 95 patients WFH and 75 caregivers and 91 patients not WFH in the past 7 days. There was a higher proportion of WFH caregivers who had higher education levels, higher incomes, occupations in management, business, finance and administration, and natural and applied sciences, had fair or poor health status, who were not compensated for their caregiving time, and who received help from other informal or professional caregivers than non-WFH caregivers. Working from home patients had higher education levels and incomes and occupations in management and natural and applied sciences, were more likely to work full-time or be self-employed, usually sat during the work day, and worked less frequently within a team than non-WFH patients.
TABLE 1.
Study Sample Characteristics by WFH Status
| Caregivers | Patients | |||||
|---|---|---|---|---|---|---|
| Variable | WFH (n = 150) | Non-WFH (n = 75) | P | WFH (n = 95) | Non-WFH (n = 91) | P |
| Age | 0.125 | 0.199 | ||||
| 25–34 y | 32 (21.3%) | 25 (33.3%) | 14 (14.7%) | 13 (14.3%) | ||
| 35–44 y | 31 (20.7%) | 14 (18.7%) | 25 (26.3%) | 13 (14.3%) | ||
| 45–54 y | 60 (40.0%) | 20 (26.7%) | 24 (25.3%) | 25 (27.5%) | ||
| 55–64 y | 27 (18.0%) | 16 (21.3%) | 32 (33.7%) | 40 (44.0%) | ||
| Female | 75 (50.0%) | 31 (41.3%) | 0.220 | 57 (60.0%) | 46 (50.5%) | 0.195 |
| Married/common lawa | 93 (62.0%) | 47 (62.7%) | 0.923 | 56 (59.6%) | 57 (62.6%) | 0.669 |
| Ethnicitya | 0.417 | 0.799 | ||||
| Asian | 41 (27.7%) | 14 (19.7%) | 19 (20.7%) | 19 (21.6%) | ||
| European | 94 (63.5%) | 49 (69.0%) | 63 (68.5%) | 62 (70.5%) | ||
| Others | 13 (8.8%) | 8 (11.3%) | 10 (10.9%) | 7 (8.0%) | ||
| Highest level of education completed | <0.001 | 0.026 | ||||
| High school or less | 21 (14.0%) | 16 (21.3%) | 12 (12.6%) | 21 (23.1%) | ||
| College or technical/trade | 25 (16.7%) | 28 (37.3%) | 27 (28.4%) | 36 (39.6%) | ||
| University | 68 (45.3%) | 19 (25.3%) | 42 (44.2%) | 27 (29.7%) | ||
| Postgraduation or professional designation | 36 (24.0%) | 12 (16.0%) | 14 (14.7%) | 7 (7.7%) | ||
| Personal incomea | <0.001 | 0.004 | ||||
| Less than $50,000 | 32 (21.9%) | 34 (47.2%) | 21 (23.6%) | 42 (47.2%) | ||
| $50,000–$99,999 | 74 (50.7%) | 26 (36.1%) | 53 (59.6%) | 39 (43.8%) | ||
| $100,000 or more | 40 (27.4%) | 12 (16.7%) | 15 (16.9%) | 8 (9.0%) | ||
| Current employment status | 0.443 | 0.002 | ||||
| Employed full time | 110 (73.3%) | 54 (72.0%) | 71 (74.7%) | 64 (70.3%) | ||
| Employed part time | 22 (14.7%) | 15 (20.0%) | 8 (8.4%) | 22 (24.2%) | ||
| Self-employed | 18 (12.0%) | 6 (8.0%) | 16 (16.8%) | 5 (5.5%) | ||
| Occupation | 0.005 | < 0.001 | ||||
| Management | 66 (44.0%) | 20 (26.7%) | 33 (34.7%) | 15 (16.5%) | ||
| Business, finance, and administration | 17 (11.3%) | 5 (6.7%) | 22 (23.2%) | 20 (22.0%) | ||
| Natural and applied sciences and related | 22 (14.7%) | 7 (9.3%) | 18 (18.9%) | 5 (5.5%) | ||
| Education, law and social, community and government services | 13 (8.7%) | 11 (14.7%) | 7 (7.4%) | 7 (7.7%) | ||
| Sales and service | 18 (12.0%) | 14 (18.7%) | 8 (8.4%) | 19 (20.9%) | ||
| Others | 14 (9.3%) | 18 (24.0%) | 7 (7.4%) | 25 (27.5%) | ||
| Self-rated health status | 0.090 | 0.478 | ||||
| Excellent or very good | 65 (43.3%) | 39 (52.0%) | 32 (33.7%) | 24 (26.4%) | ||
| Good | 51 (34.0%) | 28 (37.3%) | 46 (48.4%) | 46 (50.5%) | ||
| Fair or poor | 34 (22.7%) | 8 (10.7%) | 17 (17.9%) | 21 (23.1%) | ||
Chi-square or Fisher exact test was used for categorical variables.
aWith respondents who did not provide valid answers.
Caregivers and patients were asked to select any chronic conditions that their care receivers or they had (a full list can be found in Tables S2 and S3, Supplemental Digital Content 1, http://links.lww.com/JOM/B176). Among all caregivers, the most common chronic conditions care receivers had were diabetes (27.1%), arthritis (26.2%), high blood pressure (24.9%), chronic pain (23.1%), anxiety disorder (15.6%), and high blood cholesterol or lipids (15.6%) (Table S2). For patients, the common chronic conditions were allergies (39.2%), high blood pressure (25.3%), asthma (18.8%), high blood cholesterol or lipids (18.8%), and anxiety disorder (17.2%) (Table S3).
Absenteeism and Presenteeism by WFH Status
More caregivers were absent from work in the past 3 months in the WFH group compared with the non-WFH group (50.0% vs 33.3%; Table 2). Among those with absenteeism, the median number of absent workdays was similar among WFH caregivers (4 days; Q1–Q3, 2 to 6) and non-WFH caregivers (4 days; 2 to 10 days). More caregivers also had presenteeism in the past 7 days in the WFH group compared with the non-WFH group (42.7% vs 22.7%). Among those with presenteeism, the median percentage time loss while working was 20% (13% to 33%) in WFH caregivers compared with 25% (11% to 38%) in non-WFH caregivers.
TABLE 2.
Absenteeism and Presenteeism by WFH Status
| Caregivers | Patients | |||||
|---|---|---|---|---|---|---|
| Variable | WFH (n = 150) | Non-WFH (n = 75) | P | WFH (n = 95) | Non-WFH (n = 91) | P |
| Absenteeism in the past 3 mo | ||||||
| Absent from work | 0.018 | 0.600 | ||||
| No | 75 (50.00%) | 50 (66.67%) | 63 (66.32%) | 57 (62.64%) | ||
| Yes | 75 (50.00%) | 25 (33.33%) | 32 (33.68%) | 34 (37.36%) | ||
| No. absent workdays | ||||||
| Mean (SD) | 3.66 (8.97) | 4.03 (13.60) | 0.833 | 1.65 (4.16) | 2.09 (9.50) | 0.689 |
| Median (Q1–Q3) | 0.50 (0.00–4.00) | 0.00 (0.00–2.00) | 0.037 | 0.00 (0.00–1.00) | 0.00 (0.00–2.00) | 0.621 |
| No. of absent workdays >0 | ||||||
| Mean (SD) | 7.32 (11.61) | 12.08 (21.66) | 0.303 | 4.91 (6.00) | 5.59 (15.04) | 0.808 |
| Median (Q1–Q3) | 4.00 (2.00–6.00) | 4.00 (2.00–10.00) | 0.651 | 3.00 (1.00–5.00) | 2.50 (1.00–5.00) | 0.974 |
| Presenteeism in the past 7 d | ||||||
| Time lost while working | 0.003 | 0.020 | ||||
| No | 86 (57.33%) | 58 (77.33%) | 58 (61.05%) | 70 (76.92%) | ||
| Yes | 64 (42.67%) | 17 (22.67%) | 37 (38.95%) | 21 (23.08%) | ||
| Percentage time loss while working | ||||||
| Mean (SD) | 0.11 (0.17) | 0.06 (0.16) | 0.078 | 0.10 (0.18) | 0.06 (0.17) | 0.161 |
| Median (Q1–Q3) | 0.00 (0.00–0.19) | 0.00 (0.00–0.00) | 0.005 | 0.00 (0.00–0.17) | 0.00 (0.00–0.00) | 0.027 |
| Percentage time loss while working >0 | ||||||
| Mean (SD) | 0.25 (0.17) | 0.28 (0.25) | 0.587 | 0.26 (0.21) | 0.28 (0.25) | 0.729 |
| Median (Q1–Q3) | 0.20 (0.13–0.33) | 0.25 (0.11–0.38) | 0.871 | 0.20 (0.13–0.38) | 0.20 (0.13–0.33) | 0.821 |
Fisher exact test was used for binary variables; t test and Wilcoxon rank sum test were used for continuous variables.
A similar proportion of patients was absent from work in the past 3 months between the WFH and non-WFH groups (33.7% vs 37.4%). Working from home patients were more likely to have time loss while working than non-WFH patients (38.9% vs 23.1%). Among those with presenteeism, the percentage time loss while working was similar between WFH and non-WFH patients (median, 20% [13% to 38%] vs 20% [13% to 33%]).
Association of WFH With Absenteeism and Presenteeism
After adjusting for the confounders, the first part of the two-part models using a logistic regression model showed that WFH was significantly associated with a higher odds of being absent from work in the past 3 months (odds ratio, 2.53; 95% CI, 1.11 to 5.77) as well as having time loss while working in the past 7 days (2.79; 1.26–6.18) among caregivers (Fig. 1). Working from home patients were not significantly more likely to be absent from work (1.36; 0.57–3.23) but were more likely to have time loss while working (2.78; 1.13–6.84).
FIGURE 1.
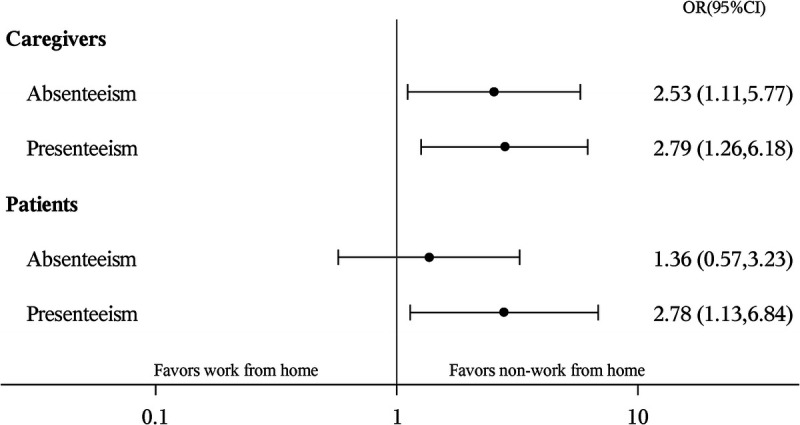
Logistic regression results for the association between WFH and absenteeism and presenteeism. OR, odds ratio.
Among those with absenteeism >0 days, WFH was associated with fewer absent work days in both caregivers (n = 75 WFH vs 25 non-WFH; coefficient = −0.62 [standard error, 0.24]) and patients (n = 32 WFH vs 34 non-WFH; coefficient = −0.18 [0.24]), although the association was not significant for patients (see Table S4, Supplemental Digital Content 1, http://links.lww.com/JOM/B176). Among those with presenteeism >0% time loss, WFH was associated with lower percentage time loss while working in caregivers (n = 64 vs 17; coefficient = −0.24 [0.27]) or patients (n = 37 vs 21; coefficient = −0.49 [0.33]), but the associations were not significant.
By combining the estimates obtained from two-part models, the average marginal effects of WFH on absenteeism and presenteeism were −0.99 (95% CI, −4.68 to 2.48) and 4% (−2% to 10%) for caregivers and −0.03 (−3.84 to 3.66) and 3% (−6% to 13%) for patients, respectively (Table 3). The 95% CI crossed 0 mainly because of the opposite effects of WFH in the two parts observed above: positive association with the probability of having absenteeism or presenteeism and negative association with the time loss from absenteeism and presenteeism among those having absenteeism or presenteeism.
TABLE 3.
Average Marginal Effects of WFH on Overall Absenteeism and Presenteeism
| Caregivers | Patients | |||||
|---|---|---|---|---|---|---|
| Variable | WFH | Non-WFH | Difference | WFH | Non-WFH | Difference |
| Absenteeism in the past 3 mo | ||||||
| Part 1: predicted probability of having absenteeism | 0.49 (0.42 to 0.58) | 0.34 (0.22 to 0.46) | 0.16 (0.02 to 0.31) | 0.38 (0.27 to 0.50) | 0.33 (0.23 to 0.44) | 0.05 (−0.13 to 0.23) |
| Part 2: predicted number of absent workdaysa | 7.11 (5.03 to 17.04) | 13.19 (6.02 to 33.84) | −6.08 (−20.05 to 1.32) | 5.27 (3.26 to 32.20) | 6.31 (2.54 to 45.94) | −1.04 (−23.40 to 9.22) |
| Total number of absent workdays | 3.56 (2.60 to 6.19) | 4.54 (1.83 to 9.04) | −0.99 (−4.68 to 2.48) | 1.68 (1.03 to 6.51) | 1.71 (0.77 to 6.85) | −0.03 (−3.84 to 3.66) |
| Presenteeism in the past 7 d | ||||||
| Part 1: predicted probability of having presenteeism | 0.42 (0.34 to 0.50) | 0.23 (0.13 to 0.35) | 0.19 (0.03 to 0.34) | 0.40 (0.29 to 0.51) | 0.22 (0.12 to 0.33) | 0.18 (−0.00 to 0.35) |
| Part 2: predicted percentage time loss while workingb | 0.31 (0.22 to 0.36) | 0.35 (0.19 to 0.52) | −0.04 (−0.23 to 0.10) | 0.30 (0.21 to 0.48) | 0.39 (0.21 to 0.65) | −0.09 (−0.33 to 0.14) |
| Total percentage time loss while working | 0.12 (0.09 to 0.15) | 0.08 (0.03 to 0.13) | 0.04 (−0.02 to 0.10) | 0.11 (0.07 to 0.18) | 0.08 (0.03 to 0.14) | 0.03 (−0.06 to 0.13) |
95% CI was estimated based on 5000 Bootstrapped replications.
aAmong those having number of absent work days >0.
bAmong those having percentage time loss while working >0.
Because the associations of the confounding variables with absenteeism and presenteeism were not the focus of the study, we highlighted significant associations in the Supplemental Digital Content 1, http://links.lww.com/JOM/B176. Their associations differed by work productivity loss outcome, the probability of absenteeism and presenteeism in the first part model (see Figure S1, Supplemental Digital Content 2, http://links.lww.com/JOM/B177, and Figure S2, Supplemental Digital Content 3, http://links.lww.com/JOM/B178), or the time loss from absenteeism and presenteeism in the second part model (see Table S4, Supplemental Digital Content 1, http://links.lww.com/JOM/B176), as well as by caregivers and patients.
DISCUSSION
To the best of our knowledge, this is the first study assessing the association of WFH with work productivity loss including absenteeism and presenteeism among caregivers and patients during the COVID-19 pandemic. Our findings suggested that WFH was associated with a higher odds of absenteeism or presenteeism among both caregivers and patients. However, when focusing on the relatively smaller subgroups with absenteeism or presenteeism, WFH may be associated with lower work productivity loss. These two opposite associations led to no significant associations of WFH with overall absenteeism and presenteeism among both caregivers and patients.
Although many studies have investigated the impact of WFH on work productivity during COVID-19, the results varied by population, setting, occupation, and time of measurement.8–18 Only a few studies have measured the impact of WFH on absenteeism and presenteeism due to health problems during the pandemic.28,29 However, their study design and methods to measure presenteeism differed from ours and thus are not comparable. Gerich28 measured the association of WFH with sickness presenteeism propensity among 517 employees in the finance, insurance, and IT sectors of Austria between February and March 2021. Sickness presenteeism propensity was calculated as the number of sickness presence days divided by the sum of sickness presence and absence days in the past 12 months. Presenteeism propensity of employees with and without WFH experience in the past 12 months was found not significantly different, but using WFH for additional work after regular office hours, on weekends or days off, was associated with increased sickness presenteeism propensity. Steidelmüller et al47 found a positive relationship between WFH and sickness presenteeism propensity using the 2015 European Working Conditions Survey. Shimura et al29 measured presenteeism using the short form of Work Limitation Questionnaire (WLQ) in 2019 and 2020 among survey participants at 23 companies from tertiary industries of Japan who had never engaged in remote work in 2019. The WLQ presenteeism score was interpreted as the percentage of productivity loss due to health problems in the past 2 weeks. The 1-year change in presenteeism from 2019 to 2020 was not significantly different across the frequency of remote work (0 days, 1 to 2 days, 3 to 4 days, or 5 days a week). Only remote working 5 days a week was associated with a higher odds of increased presenteeism between 2019 and 2020 compared with no remote working.
Despite different study designs or presenteeism outcomes, our study findings are consistent with those of these three studies that WFH is associated with higher chance of working while ill or presenteeism in patients.28,29,47 We did not find a significant association between WFH and the probability of absenteeism in patients. The findings suggested that WFH, patients are more likely to choose to keep working while ill and thus have productivity loss at work instead of taking sickness absence. Working from home offers less barriers for patients to work despite illness because of the avoided commute to office, convenient home environment for their illness management, and less chance of being noticed by their supervisors or colleagues. Holland and Collins48 distinguished between voluntary and involuntary sickness presenteeism and suggested that although working despite illness is voluntary, it can improve productivity among workers with rheumatoid arthritis. The rapid transition to WFH during COVID-19 allowed people with a chronic condition to much more easily work during their illness voluntarily, thus minimizing their lost productivity. This might partly explain why we found that WFH was not associated with increased overall work productivity loss.
There is limited evidence on the impact of WFH on caregivers' work productivity. Perez et al7 suggested WFH may hinder employees' productivity if they are in dual roles of caring children and working at home. More studies and policies focused on the potential benefits of WFH on improving work-life balance and increasing labor force participation of specific groups such as older workers, women with young children, caregivers, and people with disabilities.2,4 People with chronic conditions and caregivers may have been more likely to stop working during the pandemic given that they are already at higher risk of work stoppage or early retirement due to their health problems or caregiving responsibilities. By focusing on those who had worked, our study could not capture the potential impact of WFH on the labor force participation (eg, work stoppage), which is also one important component of work productivity loss.
Different methods and questionnaires are used to measure absenteeism and presenteeism among caregivers and patients. The questions measuring absenteeism mainly vary by the recall period from 1 week, 1 month, 3 months, to 12 months.49 The questionnaires measuring presenteeism vary by the construct, measurement method, and recall period. The three common measurement methods for presenteeism (work productivity loss while working) include a 0 to 10 scale (eg, the Work Productivity and Activity Impairment questionnaire50 and the World Health Organization Health and Work Performance Questionnaire51), direct hour estimation (eg, the Health and Labour Questionnaire52 and the VOLP), and a multidimensional questionnaire (eg, the WLQ53). The questionnaires using the three different methods gave a wide range of lost time presenteeism estimates.54,55 Thus, using different questionnaires to measure absenteeism and presenteeism might lead to different findings on the impact of WFH.
One of our study limitations was the cross-sectional design. The impact of WFH on absenteeism and presenteeism might change over time. Biron et al56 measured sickness absenteeism (number of work hours missed because of a health problem in the last week) and presenteeism (number of days worked while having a health problem in the last week) among workers who were WFH at least 80% of their work hours in the past 7 days in Quebec, Canada, over three waves during the COVID-19 pandemic: the early strict lockdown period (April 2020), the reopen period (end of June 2020), and the second strict lockdown period (end of November and early December 2020). They found presenteeism remained stable, but absenteeism decreased from the first period to the latter two periods.
Again, because of the cross-sectional design, we cannot rule out the reverse causation between absenteeism and presenteeism and WFH and unobserved heterogeneity. Caregivers and patients who had absenteeism and presenteeism might choose WFH to adapt their work to their caregiving or health needs. However, WFH was the only option for most workplaces during the early COVID-19 pandemic, which might mitigate the self-selection of WFH. In our regression models, we also controlled for potential confounders including age, sex, self-rated health, education, occupation, employment status, caregiving characteristics, and job-related characteristics. Despite this, some unobserved variables related to both WFH and work productivity loss outcomes (such as home office environment and technological and workplace support) might still bias the results. Thus, longitudinal studies or even randomized controlled trials57 are needed in the future to measure the impact of WFH on work productivity loss among caregivers and patients.
Another limitation is that our WFH status was determined by asking whether the survey respondents worked from home in the past 7 days. Their WFH status and hours worked from home might change over the past 3 months. The limitation is expected to have a larger impact on our absenteeism outcome in the past 3 months than our presenteeism outcome in the past 7 days. Our data collection time was from May 15 to June 2, 2020, for caregivers, so the past 3 months included 1 month before strict lockdown and 2 months in the strict lockdown period in Canada. The past 3 months for the collection time for patients (July 11 to 17, 2020) included the 1-month strict lockdown period to the 2-month reopening period in Canada. Based on a report by Statistics Canada, about 40% of employees worked most of their hours from home in April 2020, which dropped to about 27% in July 2020.58 Thus, WFH status in the past 7 days might not accurately represent WFH status in the 3-month recall period.
Our findings have important practical implications. Working from home arrangements are expected to continue for many workplaces and occupations even after the pandemic. The survey conducted by Statistics Canada showed that 80% of employees would like to work at least half of their hours from home once the pandemic is over.19 Our study reinforced that WFH is not associated with increased absenteeism and presenteeism among caregivers and patients who already have high work productivity loss.22–27 Working from home could also be offered by organizations to support their employees in adapting their work to their caregiving and health requirements.
CONCLUSION
Working from home was associated with an increased likelihood of absenteeism and presenteeism for caregivers and patients but lower work productivity loss among those with absenteeism and presenteeism. Consequently, WFH was not associated with total absenteeism or total presenteeism among caregivers and patients. The pandemic accelerated the transition to WFH for many people. Our results suggest that this represents an opportunity for increased flexibility and inclusion of people with chronic conditions and caregivers in the workplace without impacting productivity, although further research is needed. Our findings also emphasize the importance of considering sociodemographic differences.
ACKNOWLEDGMENTS
We acknowledge the contribution of Julie Sou in the early stages of questionnaire development as well as Isabel (Annie) Moore for editing the manuscript. Dr Wei Zhang would like to acknowledge the support of the Michael Smith Health Research BC Scholar Program. Dr Richard Sawatzky acknowledges the support of Canada Research Chairs Program–Canadian Institutes of Health Research. Dr Christine Lee acknowledges the grants received to conduct clinical trials from Ferring–Rebiotix, Seres Therapeutics, and Summit Therapeutics, respectively.
Footnotes
Funding: This work was funded by a grant from the BC SUPPORT Unit Methods Cluster Project Award [HESM–206]. The funding body had no role in the design, methods, data collection, analysis, data interpretation, or preparation of the article.
Declaration of Conflicting Interests: None declared.
Ethics Approval and Consent to Participate: This study was approved by the University of British Columbia–Providence Health Care Research Ethics Board (Ethics Certificate No. H19-00329). The online survey participants provided their consent online to continue the survey.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
Contributor Information
Huiying Sun, Email: hsun@hivnet.ubc.ca.
Aaron Gelfand, Email: atgelfan@gmail.com.
Richard Sawatzky, Email: rick.sawatzky@twu.ca.
Alison Pearce, Email: alison.pearce@sydney.edu.au.
Aslam H. Anis, Email: aslam.anis@ubc.ca.
Katrina Prescott, Email: prescott.katrina@gmail.com.
Christine Lee, Email: Christine.Lee@islandhealth.ca.
REFERENCES
- 1.Nilles JM. Traffic reduction by telecommuting: a status review and selected bibliography. Transp Res A. 1988;22:301–317. [Google Scholar]
- 2.Athanasiadou C, Theriou G. Telework: systematic literature review and future research agenda. Heliyon. 2021;7:e08165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels K, Lamond D, Standen P. Teleworking: frameworks for organizational research. J Manag Stud. 2001;38:1151–1185. [Google Scholar]
- 4.Messenger J Vargas Llave O Gschwind L, et al. Working Anytime, Anywhere: The Effects on the World of Work. Geneva: Publications Office of the European Union, Luxembourg, and the International Labour Office. Available at: http://bookshop.europa.eu/uri?target=EUB:NOTICE:TJ0616316:EN:HTML. 2017. Accessed December 13, 2021. [Google Scholar]
- 5.Harker Martin B, MacDonnell R. Is telework effective for organizations? A meta-analysis of empirical research on perceptions of telework and organizational outcomes. Manag Res Rev. 2012;35:602–616. [Google Scholar]
- 6.Dutcher EG. The effects of telecommuting on productivity: an experimental examination. The role of dull and creative tasks. J Econ Behav Org. 2012;84:355–363. [Google Scholar]
- 7.Perez MP, Sánchez AM, de Luis Carnicer MP. Benefits and barriers of telework: perception differences of human resources managers according to company's operations strategy. Technovation. 2002;22:775–783. [Google Scholar]
- 8.Smite D, Tkalich A, Moe NB, Papatheocharous E, Klotins E, Buvik MP. Changes in perceived productivity of software engineers during COVID-19 pandemic: the voice of evidence. J Syst Softw. 2022;186:111197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Awada M, Lucas G, Becerik-Gerber B, Roll S. Working from home during the COVID-19 pandemic: impact on office worker productivity and work experience. Work. 2021;69:1171–1189. [DOI] [PubMed] [Google Scholar]
- 10.Huls SPI, Sajjad A, Kanters TA, Hakkaart-van Roijen L, Brouwer WBF, van Exel J. Productivity of working at home and time allocation between paid work, unpaid work and leisure activities during a pandemic. Pharmacoeconomics. 2022;40:77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guler MA, Guler K, Guneser Gulec M, Ozdoglar E. Working from home during a pandemic: investigation of the impact of COVID-19 on employee health and productivity. J Occup Environ Med. 2021;63:731–741. [DOI] [PubMed] [Google Scholar]
- 12.Kitagawa R, Kuroda S, Okudaira H, Owan H. Working from home and productivity under the COVID-19 pandemic: using survey data of four manufacturing firms. Plos One. 2021;16:e0261761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zürcher A, Galliker S, Jacobshagen N, Lüscher Mathieu P, Eller A, Elfering A. Increased working from home in vocational counseling psychologists during COVID-19: associated change in productivity and job satisfaction. Front Psychol. 2021;12:750127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weitzer J Papantoniou K Seidel S, et al. Working from home, quality of life, and perceived productivity during the first 50-day COVID-19 mitigation measures in Austria: a cross-sectional study. Int Arch Occup Environ Health. 2021;94:1823–1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kusoski C, Polley S, Kennerly-Shah J. Coronavirus 2019 work-from-home productivity of inpatient and infusion pharmacists at a comprehensive cancer center. J Am Pharm Assoc (2003). 2022;62:877–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sher AC, Salman R, Seghers VJ, Desai NK, Sammer MBK. Performance of pediatric neuroradiologists working from home during a pandemic at a quaternary pediatric academic hospital. AJNR Am J Neuroradiol. 2022;43:474–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow JSF, Palamidas D, Marshall S, Loomes W, Snook S, Leon R. Teleworking from home experiences during the COVID-19 pandemic among public health workers (TelEx COVID-19 study). BMC Public Health. 2022;22:674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morikawa M. Work-from-home productivity during the COVID-19 pandemic: Evidence from Japan. Econ Inq. 2022;60:508–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehdi T, Morissette R. Working from home: productivity and preferences. Catalogue no. 45280001; Ottawa: Statistics Canada Available at: https://www150.statcan.gc.ca/n1/pub/36-28-0001/2021005/article/00001-eng.htm. April 1, 2021. Accessed May 17, 2022.
- 20.Centre for Surveillance and Applied Research, Public Health Agency of Canada . Canadian Chronic Disease Indicators (CCDI), 2019 Edition. Available at: https://health-infobase.canada.ca/ccdi/data-tool/?edi=2019&Dom=5&Ind=1&MS=14. 2019. Accessed March 22, 2022.
- 21.Statistics Canada . The experiences and needs of older caregivers in Canada. Available at: https://www150.statcan.gc.ca/n1/pub/75-006-x/2020001/article/00007-eng.htm. 2020. Accessed June 20, 2022.
- 22.Zhang W, McLeod C, Koehoorn M. The relationship between chronic conditions and absenteeism and associated costs in Canada. Scand J Work Environ Health. 2016;42:413–422. [DOI] [PubMed] [Google Scholar]
- 23.Zhang W, Sun H, Li X. The association between chronic conditions and non-agricultural work productivity loss among the middle-aged Chinese population. J Occup Environ Med. 2018;60:832–838. [DOI] [PubMed] [Google Scholar]
- 24.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46:398–412. [DOI] [PubMed] [Google Scholar]
- 25.Kotseva K Gerlier L Sidelnikov E, et al. Patient and caregiver productivity loss and indirect costs associated with cardiovascular events in Europe. Eur J Prev Cardiol. 2019;26:1150–1157. [DOI] [PubMed] [Google Scholar]
- 26.Kahn SA, Lin CW, Ozbay B, Wang A, Chao J, Skup M. Indirect costs and family burden of pediatric Crohn's disease in the United States. Inflamm Bowel Dis. 2017;23:2089–2096. [DOI] [PubMed] [Google Scholar]
- 27.Fujihara S, Inoue A, Kubota K, Yong KFR, Kondo K. Caregiver burden and work productivity among Japanese working family caregivers of people with dementia. Int J Behav Med. 2019;26:125–135. [DOI] [PubMed] [Google Scholar]
- 28.Gerich J. Home-based telework and presenteeism: new lessons learned from the Covid-19 pandemic. J Occup Environ Med. 2022;64:243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shimura A, Yokoi K, Ishibashi Y, Akatsuka Y, Inoue T. Remote work decreases psychological and physical stress responses, but full-remote work increases presenteeism. Front Psychol. 2021;12:730969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sinha M, Statistics Canada, Social and Aboriginal Statistics Division . Portrait of Caregivers, 2012. Ottawa: Statistics Canada. Available at: https://www150.statcan.gc.ca/n1/en/pub/89-652-x/89-652-x2013001-eng.pdf?st=SifrFblD. 2014. Accessed August 3, 2021. [Google Scholar]
- 31.Zhang W, Bansback N, Boonen A, Severens JL, Anis AH. Development of a composite questionnaire, the valuation of lost productivity, to value productivity losses: application in rheumatoid arthritis. Value Health. 2012;15:46–54. [DOI] [PubMed] [Google Scholar]
- 32.Zhang W, Bansback N, Kopec J, Anis AH. Measuring time input loss among patients with rheumatoid arthritis: validity and reliability of the Valuation of Lost Productivity questionnaire. J Occup Environ Med. 2011;53:530–536. [DOI] [PubMed] [Google Scholar]
- 33.Zhang W, Bansback N, Sun H, Pedersen R, Kotak S, Anis AH. Estimating the monetary value of the annual productivity gained in patients with early rheumatoid arthritis receiving etanercept plus methotrexate: interim results from the PRIZE study. RMD Open. 2015;1:e000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang W, Bansback N, Sun H, Pedersen R, Kotak S, Anis AH. Impact of etanercept tapering on work productivity in patients with early rheumatoid arthritis: results from the PRIZE study. RMD Open. 2016;2:e000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sadatsafavi M Rousseau R Chen W, et al. The preventable burden of productivity loss due to suboptimal asthma control: a population-based study. Chest. 2014;145:787–793. [DOI] [PubMed] [Google Scholar]
- 36.McCormick N, Reimer K, Famouri A, Marra CA, Aviña-Zubieta JA. Filling the gaps in SARDs research: collection and linkage of administrative health data and self-reported survey data for a general population-based cohort of individuals with and without diagnoses of systemic autoimmune rheumatic disease (SARDs) from British Columbia, Canada. BMJ Open. 2017;7:e013977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCormick N, Marra CA, Sadatsafavi M, Kopec JA, Aviña-Zubieta JA. Excess productivity costs of systemic lupus erythematosus, systemic sclerosis, and Sjögren's syndrome: a general population-based study. Arthritis Care Res (Hoboken). 2019;71:142–154. [DOI] [PubMed] [Google Scholar]
- 38.Zhang W, Li KH, Gobis B, Zed PJ, Lynd LD. Work productivity losses and associated risk factors among university employees in the CAMMPUS Wellness Program. J Occup Environ Med. 2020;62:25–29. [DOI] [PubMed] [Google Scholar]
- 39.Rodriguez Llorian E Zhang W Khakban A, et al. Productivity loss among people with early multiple sclerosis: a Canadian study. Mult Scler. 2022;28:1414–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gelfand A Sou J Sawatzky R, et al. Valuation of lost productivity in caregivers: a validation study. Front Psychol. 2021;12:727871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Statistics Canada . National Occupational Classification (NOC) 2016 Version 1.1. Available at: https://www.statcan.gc.ca/eng/subjects/standard/noc/2016/indexV1.1. 2018. Accessed August 25, 2018.
- 42.Zhang W, Sun H. How to analyze work productivity loss due to health problems in randomized controlled trials? A simulation study. BMC Med Res Methodol. 2021;21:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kleinman NL Brook RA Patel PA, et al. The impact of gout on work absence and productivity. Value Health. 2007;10:231–237. [DOI] [PubMed] [Google Scholar]
- 44.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. [DOI] [PubMed] [Google Scholar]
- 45.Basu A, Manca A. Regression estimators for generic health-related quality of life and quality-adjusted life years. Med Decis Making. 2012;32:56–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. Hoboken, NJ: John Wiley & Sons, Inc.; 2013. [Google Scholar]
- 47.Steidelmüller C, Meyer SC, Müller G. Home-based telework and presenteeism across Europe. J Occup Environ Med. 2020;62:998–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holland P, Collins AM. “Whenever I can I push myself to go to work”: a qualitative study of experiences of sickness presenteeism among workers with rheumatoid arthritis. Disabil Rehabil. 2018;40:404–413. [DOI] [PubMed] [Google Scholar]
- 49.Zhang W, Tocher P, L’Heureux J, Sou J, Sun H. Measuring, analyzing and presenting work productivity loss in randomized controlled trials: a scoping review. Value Health. 2022; DOI: 10.1016/j.jval.2022.06.015. Open Access: Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 50.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC Ames M Hymel PA, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med. 2004;46:S23–S37. [DOI] [PubMed] [Google Scholar]
- 52.van Roijen L, Essink-Bot ML, Koopmanschap MA, Bonsel G, Rutten FF. Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. Int J Technol Assess Health Care. 1996;12:405–415. [DOI] [PubMed] [Google Scholar]
- 53.Lerner D, Amick BC, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39:72–85. [DOI] [PubMed] [Google Scholar]
- 54.Zhang W Gignac MA Beaton D Tang K Anis AH, Canadian Arthritis Network Work Productivity Group . Productivity loss due to presenteeism among patients with arthritis: estimates from 4 instruments. J Rheumatol. 2010;37:1805–1814. [DOI] [PubMed] [Google Scholar]
- 55.Gardner BT, Dale AM, Buckner-Petty S, Van Dillen L, Amick BC, 3rd, Evanoff B. Comparison of employer productivity metrics to lost productivity estimated by commonly used questionnaires. J Occup Environ Med. 2016;58:170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Biron C, Karanika-Murray M, Ivers H, Salvoni S, Fernet C. Teleworking while sick: a three-wave study of psychosocial safety climate, psychological demands, and presenteeism. Front Psychol. 2021;12:734245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bloom N, Liang J, Roberts J, Ying ZJ. Does working from home work? Evidence from a Chinese experiment. Q J Econ. 2015;130:165–218. [Google Scholar]
- 58.Mehdi T, Morissette R. Working from home in Canada: what have we learned so far? Statistics Canada. Catalogue no. 36-28-0001. Epub ahead of print October 27, 2021. DOI: 10.25318/36280001202101000001-ENG.


