Goal:
Downcoding at nonprofit healthcare institutions can account for significant revenue losses that, in turn, can affect the amount and quality of care they provide. Using the inpatient medical note to assess the complexity of care, we wanted to quantify the visit coding distribution at the largest tertiary care center in West Virginia and to improve the documentation and coding if found to be below national benchmarks.
Methods:
We measured the number of encounters and associated documentation of level 1, 2, and 3 visits among hospitalists. We compared our data to national benchmark data. We then implemented a multifaceted, multidisciplinary intervention to improve documentation and coding.
Principal Findings:
We found a significant average increase of level 3 admission history and physical visits of 76% (p < .0001) and 112% (p < .001) for subsequent encounters compared with baseline preintervention visit types. With team-based coding interventions in place, documentation accurately now reflects the complexity of care delivered. Based on Medicare reimbursement rates, this new accuracy has led to an increase in revenue of $233, 988.79 per 10,000 encounters.
Applications to Practice:
Provider knowledge of medical billing and coding guidelines is essential. In particular, large academic institutions typically operate on small margins, so even simple adjustments and quality improvement efforts in billing and coding can help immensely by accurately representing the amount and quality of medical services. An institution can markedly improve revenues by coding notes to reflect the true complexity of care that is delivered.
INTRODUCTION
In healthcare, accurate billing and coding are both essential and problematic. Physician providers, medical institutions, and insurers alike widely recognize upcoding as a detriment to healthcare because it leads to fraud and overbilling (Kesselheim & Brennan, 2005; McKinnon, 2004). On the other hand, downcoding accounts for significant revenue losses, especially at nonprofit institutions that provide complex care for large volumes of patients (Fleishon et al., 2017; Kesselheim & Brennan, 2005; Terry, 2006) when it misrepresents the services rendered (McKinnon, 2004).
The heavy burden of documentation can lead to errors of omission in the medical records, and studies have shown that overly cautious physicians tend to downcode (Powell et al., 2012; Weiner et al., 2020). Downcoding can be related to time constraints, which are associated with less thorough documentation and more errors of omission and commission (Powell et al., 2012; Weiner et al., 2020). This practice has an impact on the amount and quality of care when physicians increase the number of patients seen in a day to meet productivity targets.
In inpatient medicine, the medical note is the primary indicator of decision-making and care complexity of patient encounters. Visit demarcations range from levels 1 (reflecting low-complexity medical decision-making) to 3 (reflecting comprehensive, high-complexity medical decision-making; American Medical Association, 2021; Centers for Medicare & Medicaid Services, 1995, 1997).
Many hospitals use hospitalist teams to provide care for most patients (Wachter et al., 1999). Reimbursement depends on the note type for inpatient medicine for the initial and follow-up visits that hospitalists document during a patient's admission. Academic centers typically encounter patients who are sicker than those at other facilities (Fleishon et al., 2017). Therefore, we evaluated our large academic tertiary care center—the only one in the state—for appropriateness of inpatient note coding. We hypothesized that the billing levels would be on par or higher than averages across the United States, given the country's complex patient population. The objective of our retrospective cohort study was twofold: to quantify the number of encounter types and then to improve their quality if they were below national quality benchmarks.
METHODS
We analyzed data from 26 hospitalists providing care over a 2-year period (see Supplementary Table 1, published as Supplemental Digital Content at http://links.lww.com/JHM/A86). The data included 7,987 admission encounters and 51,583 subsequent encounters; they were obtained using Tableau Analytics, which is used for systems-level accounting at the institution. The analysis was completed in two phases.
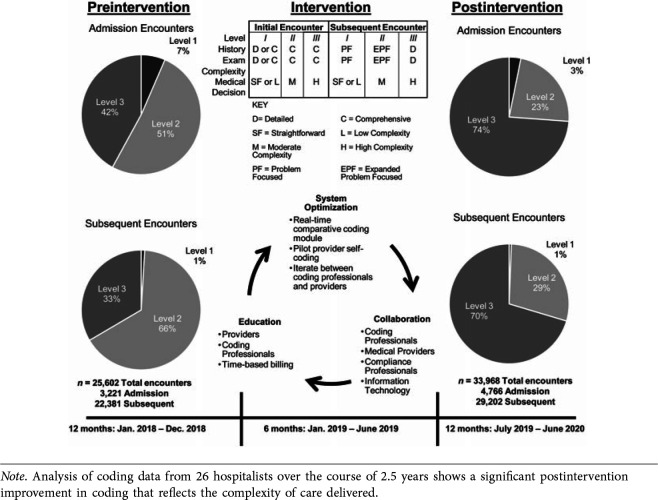
First, we analyzed the total number of visit types for the 26 hospitalists for 1 year. We used statistical models such as the Student t test and analysis of variance to evaluate level 1, 2, and 3 visits (Figure 1). We compared that data to benchmarks provided by the Society of Hospital Medicine (White et al., 2018). We then implemented a multidisciplinary response including education, collaboration, and system optimization, which we based on plan–do–study–act (PDSA) quality improvement principles. After our initial analysis, we iterated small interventions and studied their systemwide effects (Taylor et al., 2014).
FIGURE 1.
Research Design
Among the interventions was education in the basic tenets of inpatient billing and coding, notably time-based billing. To address department barriers across the organization, we included providers, coders, compliance team members, and information technologists. We had found that coders, for example, hesitated to reach out to providers and confirm that their notes were appropriately coded. To help coders overcome this barrier and clarify diagnoses when necessary, we used the direct chat feature in the electronic health record (EHR) system and electronic messaging to facilitate communication between the coders and providers.
Other challenges complicated efforts to get all professionals on board. For example, the compliance team's main concern was to ensure that notes were not upcoded, which could trigger an audit and the clawback of payments. We addressed this concern by demonstrating through a cost analysis based on our random audit of internal notes that downcoding was far more prevalent and resulted in significant revenue loss. Overall, the cost of downcoding throughout the study period was hundreds of thousands of dollars higher than any penalty incurred from sporadic instances of upcoding. We also promised to monitor coding through internal audits to ensure that no systemic upcoding would occur as a result of our interventions.
For the coding department, the primary concerns were related to the associated culture change. Consistent with the compliance team's concerns, coders often erred to the lower of two levels whenever there was room for discretion in coding notes. This resulted in systemic downcoding, particularly for nonprocedural areas such as inpatient internal medicine. We addressed this concern by establishing collaboration between compliance and coding in which appropriate coding rather than downcoding was seen as the goal when applying discretion to avoid penalties.
Unlike outpatient providers, inpatient providers were not accustomed to coding their own notes. This barrier required a significant amount of effort on our part to explain the nuances of inpatient documentation regarding coding, which we did in a series of weekly lunchtime lectures.
We selected members from all groups (providers, coders, compliance team members, and information technologists) together for a pilot program. We expanded EHR access to include a pilot coding module based on the outpatient EHR coding module, so the providers could self-code. After completing a note, each provider coded it for level 1, 2, or 3 and added ancillary codes (such as “advanced care planning”) from a pop-up menu. The coders then independently reviewed each note and coded it as they normally would. When the coders did not agree with a provider's assessment, they entered a brief description of the discrepancy. We optimized this process by implementing a real-time comparative coding module for providers, so they could see their frequency of coding concurrence and disparity with the coders and the reasons for these differences. We later met with the providers and coders to review notes and discuss areas for improvement. Typically, either the medical reasoning documented by the provider did not capture the services accurately or the professional coders did not fully appreciate the complexity of the medical decision-making described in the note. This intervention spanned about 6 months before changes were made and observed in the health system.
In the second, postintervention phase, we formally studied our PDSA cycle. We followed 26 full-time hospitalists for 12 months after the interventions. The hospitalists worked the same number of pre- and postintervention shifts, and because they were compared to their own data preintervention, we could implement a paired t test to evaluate the difference between the number of encounters of each level pre- and postintervention (see Figure 1 for process flow and timeline of intervention).
The financial analysis was performed using the work relative value units (wRVUs) and percentages of level 1, 2, and 3 visits. We used the following formula for each type of visit:
We multiplied the wRVU total per 10,000 encounters by the $36.09 reimbursement rate determined by Medicare to estimate the cost benefit of the intervention. The reimbursement number is from the study's 2018–2020 time frame.
RESULTS
Preintervention data found 51% of new encounters at level 2, and 42% at level 3. Of repeat encounters, 66% were level 2, and 33% level 3 (Figure 1). Our provider post hoc analysis of these notes showed that 58% of level 2 encounters met level 3 criteria.
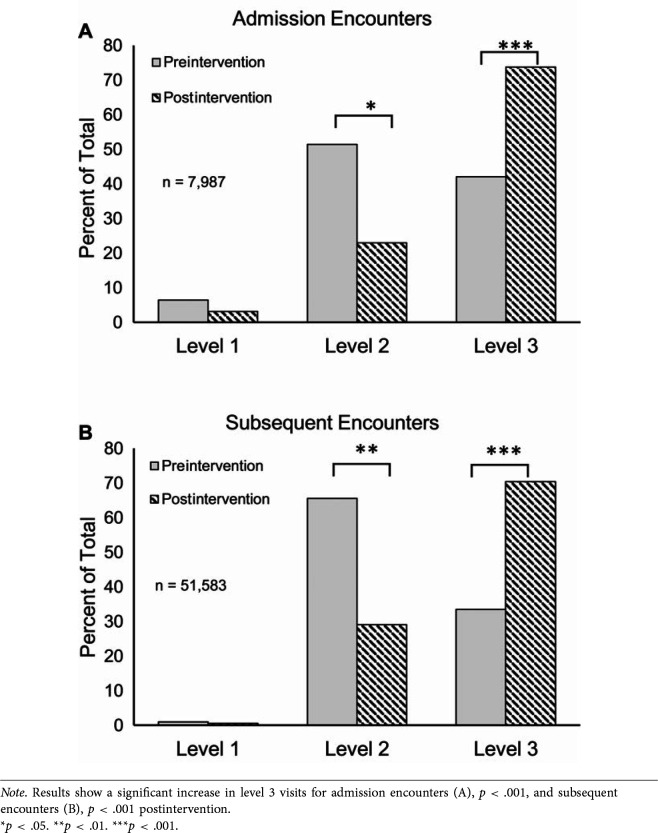
Postintervention inpatient admission encounters averaged 23% level 2 and 74% level 3 (Figure 1; level 2 p < .05, level 3 p < .001), and repeat encounters averaged 29% level 2 and 70% level 3 (level 2 p < .01, level 3 p < .001). Overall, results showed significant average improvement of level 3 admission encounters of 76% (Figure 2A, p < .001) and 112% (Figure 2B, p < .001) for subsequent encounters compared with baseline preintervention visit types. This reflected an improvement of 13.6% wRVUs per new encounter and 14.3% wRVUs per repeat encounter (Table 1). Based on Medicare reimbursement rates, this translated to a conservative estimate of revenue increase of $233,988.79 per 10,000 encounters (Table 1).
FIGURE 2.
Improvement of Level 3 Visits, Postintervention
TABLE 1. Cost Improvement Analysis.
| wRVU Total and Estimated Reimbursement per 10,000 Encounters, 2018–2020 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| wRVU | Admission Encounters | Subsequent Encounters | All Encounters Total |
||||||||
| Level 1 1.92 |
Level 2 2.61 |
Level 3 3.86 |
Total | Estimated Reimbursement |
Level 1 0.76 |
Level 2 1.29 |
Level 3 2 |
Total | Estimated Reimbursement |
||
| Preintervention | 1,246.08 | 13,433.67 | 16227.4 | 30,907.19 | $1,115,440.49 | 72.2 | 9,118.40 | 6,690 | 15,880.60 | $573,130.85 | $1,688,571.34 |
| Postintervention | 604.8 | 6,008.22 | 28502.2 | 35,115.26 | $1,267,309.73 | 44.84 | 4,035.17 | 14,076 | 18,156.01 | $655,250.40 | $1,922,560.13 |
| Total improvement | 13.62% | $151,869.25 | Total improvement | 14.33% | $82,119.55 | ||||||
| Total improvement | $233,988.79 | ||||||||||
| 13.86% | |||||||||||
Note. wRVU = work relative value unit.
DISCUSSION
The results of this study indicate that implementing quality improvement tactics for inpatient note documentation and coding can help a health system generate a significant amount of revenue. The analysis of coding practices resulted in significant improvements to level 3 billing at our hospital, for both initial and follow-up inpatient encounters.
As the primary referral center for West Virginia, the tertiary academic medical center in this study provides the highest level of care. And as such, it should have an inpatient note coding level distribution that is at least near the national average. Prior to our quality improvement project, however, the coding levels were significantly below average—routinely downcoded notes did not accurately capture the complexity of medical care for the many high-acuity patients.
The intervention described here to change documentation and coding practices has led to increased reimbursement because it truly reflects the complexity of care rendered by inpatient providers. This increase in revenue has allowed the expansion of services, which is particularly important for academic centers that care for a disproportionate number of socioeconomically disadvantaged patients.
Study Limitations
Limitations of our work include the lack of a standard control group, as the billing and coding department in this study is shared across all inpatient hospital services. Any change implemented in the coding department affects the entire hospital. Therefore, we used the control data of pre-intervention hospitalist encounter type. Results across the entire health system may be within a margin of error, as our cohort of hospitalists averaged a similar volume across time. As at many hospitals, total volume of visits was affected by the COVID-19 pandemic and thus total revenues may be affected.
CONCLUSION
Billing and coding may be the parts of medicine that no one likes to discuss. Nevertheless, financing healthcare remains a key issue (Kesselheim & Brennan, 2005; Wachter et al., 1999). By using a multipronged, multidisciplinary approach to improve provider documentation and coding practices, an institution can markedly improve revenues by ensuring that coding notes accurately reflect the complexity of care delivered. Future research could extend this study to evaluate groups outside of the hospitalists' pre- and postintervention and evaluate proceduralists using similar approaches.
Supplementary Material
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's website (www.jhmjournalonline.com).
Contributor Information
Danielle DeCicco, Email: dd0013@mix.wvu.edu, West Virginia University School of Medicine, Morgantown, West Virginia, and J. W. Ruby Memorial Hospital Department of Medicine, Morgantown, West Virginia.
Troy M. Krupica, Email: tkrupica@hsc.wvu.edu, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine and Section of Hospital Medicine.
Ronald Pellegrino, Email: pellegrinor@wvumedicine.org, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine.
Ziad O. Dimachkie, Email: ziad.dimachkie@hsc.wvu.edu, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine and Section of Hospital Medicine.
REFERENCES
- American Medical Association. (2021). CPT evaluation and management (E/M). https://www.ama-assn.org/practice-management/cpt/cpt-evaluation-and-management
- Centers for Medicare & Medicaid Services. (1995). Documentation guidelines for evaluation and management services. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/95docguidelines.pdf
- Centers for Medicare & Medicaid Services. (1997). Documentation guidelines for evaluation and management services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
- Fleishon H. B., Itri J. N., Boland G. W., Duszak R., Jr. (2017). Academic medical centers and community hospitals integration: Trends and strategies. Journal of the American College of Radiology, 14(1), 45–51. 10.1016/j.jacr.2016.07.006 [DOI] [PubMed] [Google Scholar]
- Kesselheim A. S., Brennan T. A. (2005). Overbilling vs. downcoding—the battle between physicians and insurers. New England Journal of Medicine, 352(9), 855–857. 10.1056/nejmp058011 [DOI] [PubMed] [Google Scholar]
- McKinnon P. (2004). Stealth downcoding and what you can do about it. Journal of Medical Practice Management, 20(1), 28–29. https://pubmed.ncbi.nlm.nih.gov/15500019/ [PubMed] [Google Scholar]
- Powell A., Savin S., Savva N. (2012). Physician workload and hospital reimbursement: Overworked physicians generate less revenue per patient. Manufacturing and Service Operations Management, 14(4), 512–528. 10.1287/msom.1120.0384 [DOI] [Google Scholar]
- Taylor M. J., McNicholas C., Nicolay C., Darzi A., Bell D., Reed J. E. (2014). Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Quality and Safety, 23(4), 290–298. 10.1136/bmjqs-2013-001862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry K. (2006). Blending: The new downcoding. Medical Economics, 83(9), 34–38. https://pubmed.ncbi.nlm.nih.gov/16749632/ [PubMed] [Google Scholar]
- Wachter R. M., Whitcomb W. F., Nelson J. R. (1999). Financial implications of implementing a hospitalist program. Healthcare Financial Management, 53(3), 48–51. https://pubmed.ncbi.nlm.nih.gov/10351056/ [PubMed] [Google Scholar]
- Weiner S. J., Wang S., Kelly B., Sharma G., Schwartz A. (2020). How accurate is the medical record? A comparison of the physician's note with a concealed audio recording in unannounced standardized patient encounters. Journal of the American Medical Informatics Association, 27(5), 770–775. 10.1093/jamia/ocaa027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A. W., Anders J. A., Anoff D. A., Creamer J. C., Flores L. F., George R. G., Huang B. H., Kurian L. K., Merchant M. M., Narreddy K. N., Papetti E. P., Sites C. S., Small S. S., Stephan T. S., Trask A. T., Vuong K. V., Siy J. S. (2018, October). 2018 State of Hospital Medicine Report. Society of Hospital Medicine. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.