Background
Nursing care is essential to overall quality of healthcare experienced by patients and families—especially during childbearing. However, evidence regarding quality of nursing care during labor and birth is lacking, and established nurse-sensitive outcome indicators have limited applicability to maternity care. Nurse-sensitive outcomes need to be established for maternity care, and prior research suggests that the initiation of human milk feeding during childbirth hospitalization is a potentially nurse-sensitive outcome.
Objective
The aim of this study was to determine the relationship between nurse-reported staffing, missed nursing care during labor and birth, and exclusive breast milk feeding during childbirth hospitalization as a nurse-sensitive outcome.
Methods
2018 Joint Commission PC-05 Exclusive Breast Milk Feeding rates were linked to survey data from labor nurses who worked in a selected sample of hospitals with both PC-05 data and valid 2018 American Hospital Association Annual Survey data. Nurse-reported staffing was measured as the perceived compliance with Association of Women’s Health, Obstetric and Neonatal Nurses staffing guidelines by the labor and delivery unit. Data from the nurse survey were aggregated to the hospital level. Bivariate linear regression was used to determine associations between nurse and hospital characteristics and exclusive breast milk feeding rates. Generalized structural equation modeling was used to model relationships between nurse-reported staffing, nurse-reported missed care, and exclusive breast milk feeding at the hospital level.
Results
The sample included 184 hospitals in 29 states and 2,691 labor nurses who worked day, night, or evening shifts. Bivariate analyses demonstrated a positive association between nurse-reported staffing and exclusive breast milk feeding and a negative association between missed nursing care and exclusive breast milk feeding. In structural equation models controlling for covariates, missed skin-to-skin mother–baby care and missed breastfeeding within 1 hour of birth mediated the relationship between nurse-reported staffing and exclusive breast milk feeding rates.
Discussion
This study provides evidence that hospitals’ nurse-reported compliance with Association of Women’s Health, Obstetric and Neonatal Nurses staffing guidelines predicts hospital-exclusive breast milk feeding rates and that the rates are a nurse-sensitive outcome.
Key Words: childbirth, human milk feeding, missed nursing care, nurse-sensitive patient outcomes, nurse staffing
Nursing care is an important component of the overall quality of healthcare experienced by patients and families, especially during the perinatal period. Childbirth is a leading reason for hospital admission in the United States (Agency for Healthcare Research and Quality, 2021). In 2020, there were 3,613,482 U.S. births, 98.7% of which occurred in hospitals (Gregory et al., 2021). Although multiple aspects of nursing care quality have been studied in medical–surgical and intensive care settings, established nurse-sensitive indicators (e.g., hospital-acquired pressure injuries and central line-associated bloodstream infections) have little relevance to maternity settings. Evidence for nursing care quality in maternity settings is limited, and nurse-sensitive maternity indicators need to be established. Prior research with mothers, nurses, and physicians suggests that one such potential indicator is the initiation of human milk feeding during childbirth hospitalization (Lyndon et al., 2017).
Human milk feeding, defined as breastfeeding, chestfeeding, or the feeding of pumped human milk, promotes the health of both mothers and infants. We use gendered and gender-neutral terms in this article to include all persons with the capacity for pregnancy, birth, and lactation. We retain the wording used in the original report when referring to prior research publications. Mothers who breastfeed have a reduced risk of developing breast cancer (World Health Organization [WHO], 2017) as well as ovarian cancer, hypertension, cardiovascular disease, and Type 2 diabetes (American College of Obstetricians and Gynecologists, 2021). Breastfed infants have a reduced risk of sudden infant death and developing respiratory, gastrointestinal and ear infections, allergic diseases such as asthma and eczema, and inflammatory bowel disease (Meek et al., 2022). Exclusive breastfeeding or provision of human milk are recommended to 6 months of age (American College of Obstetricians and Gynecologists, 2021; Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) 2021; Meek et al., 2022; WHO, 2017). Success in breastfeeding or achieving human milk feeding goals has been described as a collective societal responsibility (Rollins et al., 2016), and hospital and healthcare provider practices influence the successful initiation of human milk feeding (Centers for Disease Control and Prevention, 2021; Rollins et al., 2016; WHO, 2017).
In Donabedian’s widely used and adapted structure–process–outcomes model for healthcare quality, structural, environmental, organizational, and patient factors affect the process of care, and in turn, the process of care and patient factors affect outcomes (Donabedian, 1980). Substantial literature supports an empirical relationship between nurse staffing as a structural factor and patient outcomes (Blume et al., 2021). One of the proposed processes through which nurse staffing may affect patient outcomes is missed nursing care (Griffiths et al., 2018), which occurs when nurses must make decisions about how to provide the best possible care in the face of multiple competing demands and resource constraints. Under such circumstances, nurses use knowledge and clinical judgment to engage in a deliberate prioritization process so that essential care is given. In contrast, less critical care may be abbreviated, delayed, or omitted (Kalisch et al., 2009).
In the context of human milk feeding, nurses play a significant role in supporting the initiation of lactation during childbirth hospitalization (Bramson et al., 2010). For example, in the United States, nurses usually manage early skin-to-skin contact and early breastfeeding initiation within the first minutes and hours of newborn life—both of which increase the likelihood of breastfeeding success and duration in a dose–response relationship (WHO, 2017). Structural factors—such as nurse staffing—that affect the nursing care process may limit the overall “dose” of breastfeeding-related nursing care patients receive (Simpson et al., 2016). Prior work suggests care processes can promote successful initiation and continuation of breastfeeding—such as breastfeeding support and aspects of management of newborn transition—which may be missed during labor, birth, and postpartum care when nurses have to prioritize other care components because of inadequate staffing and competing demands (Lyndon et al., 2017; Simpson et al., 2020), and missed nursing care is associated with lower rates of exclusive breastfeeding at hospital discharge (Simpson et al., 2020). This study aimed to determine the relationship between nurse-reported staffing, missed nursing care, and exclusive breast milk feeding during childbirth hospitalization while accounting for other structural factors, including hospital size, teaching intensity, level of obstetric and neonatal services, volume of births, and location.
METHODS
Sample and Procedures
Nurse survey data came from self-reported measures via the LaborRNs Survey, which was distributed through e-mail to 10,620 nurses from 277 labor and birth units in 37 states across the United States from February 2018 through July 2019, as previously described (Lyndon et al., 2022). Hospital data were obtained from the 2018 American Hospital Association (AHA) Annual Survey and the 2018 Joint Commission Health Care Quality Data (http://www.healthcarequalitydata.org/). The institutional review boards at New York University and the University of California San Francisco approved the study. Our study center was responsible for all recruitment and data collection, and participating hospitals were not engaged in human subjects’ activity. However, we also obtained local institutional review board approval at any of the hospitals that required it.
States participating in the LaborRNs Survey were chosen based on state demographics, number of birth hospitals, and availability of state inpatient data. We recruited registered nurses (RNs) working in labor and birth units that reported at least 40 births per year, as indicated in the AHA Annual Survey. The survey achieved a response rate of 35%, yielding 3,676 records. We excluded survey records with incomplete data (≥40% of items and/or >3 scales) and surveys from ineligible respondents (e.g., receptionist and lactation consultant). Only hospitals with ≥4 surveys were included in hospital-level analyses as per prior research (Lake et al., 2017; Simpson et al., 2020). To ensure this exclusion criterion did not eliminate small rural hospitals from the sample, we retained responses from hospitals with fewer than four completed surveys if this represented a response rate equal to or greater than the average hospital response rate of 35% (Lyndon et al., 2022).
Measures
Nurse Survey Data
The LaborRNs Survey measures included the Perinatal Missed Care Survey, a measure of staffing guideline adherence, measures of safety climate, burnout, and intention to leave, and demographic items.
Predictor: Staffing Guideline Adherence
Nurse perception of unit adherence to staffing guidelines for specific aspects of care was measured using a 4-point Likert-type scale for each of the 14 items presenting recommended nurse-to-patient ratios to particular parts of care, as stated in the AWHONN 2010 Guidelines for Professional Registered Nurse Staffing for Perinatal Units (AWHONN, 2010). Response options regarding unit adherence were “rarely,” “occasionally,” “frequently,” “always,” and “not applicable.” A staffing score was created for each respondent by taking the mean of their individual response scores, with higher scores indicating better adherence to staffing guidelines.
Mediator: Perinatal Missed Nursing Care
The Perinatal Missed Care Survey is a valid and reliable adaptation of the MISSCARE Survey to labor and birth (Kalisch & Williams, 2009; Lyndon et al., 2022). Twenty-five items addressing the frequency with which aspects of essential nursing care during labor and birth are missed (delayed, unfinished, or completely missed) on the unit were measured using a 4-point Likert-type scale, with response options rarely, occasionally, frequently, and always, or not applicable” A missed care score was created for each respondent by dichotomizing the responses (rarely = 0, occasionally/frequently/always = 1) and summing the number of items reported missed (Lyndon et al., 2022).
Covariate: Patient Safety Climate
Nurses’ perceptions of their units’ safety climate were measured using seven items from the Safety Climate subscale of the Safety Attitudes Questionnaire (Sexton et al., 2006). The questions included the following: “The culture of this unit makes it easy to learn from the errors of others,” “Medical and nursing errors are handled appropriately on this unit,” “I know the proper channels to direct questions regarding patient safety,” “I am encouraged by my colleagues to report any patient safety concerns that I may have,” “I receive appropriate feedback about my performance,” “I would feel safe being treated here as a patient,” and “In this unit, it is difficult to discuss errors” (reverse scored). Each item was rated on a 5-point Likert scale, ranging from 1 = disagree strongly to 5 = agree strongly. The subscale for each nurse was scored by averaging safety climate items, with scores ranging between 1 and 5 and higher scores indicating a better-perceived safety climate.
Covariates: Nurse Demographics
Nurse demographics, including age, education, years of experience as an RN, years of experience as an RN in labor and birth, years working in their current hospital, and shift usually worked, were included based on prior research on patient safety and nurse-sensitive patient outcomes (Aiken et al., 2011, 2012; Ball et al., 2018; Griffiths et al., 2014). Gender, race, and ethnicity were included following federal requirements for funded research.
Hospital Data
Outcome: Exclusive Breast Milk Feeding Rate
The Joint Commission’s Perinatal Core Measure PC-05, exclusive breast milk feeding (EBMF), is a National Quality Forum voluntary consensus measure expressing the proportion of newborns fed only breast milk from birth through hospital discharge. The EBMF numerator includes newborns fed only breast milk during the birth hospitalization. The EBMF denominator includes live newborns, excluding those admitted to the neonatal intensive care unit (NICU), those with galactosemia or receiving parenteral nutrition, newborns with a length of stay of >120 days, and newborns who died during birth hospitalization (The Joint Commission, 2018). Hospitals participating in the Joint Commission Accreditation Program are expected to report this national quality measure, and we extracted hospital data from the 2018 Joint Commission Health Care Quality Data.
Covariates: Hospital Characteristics
We extracted annual birth volume, AHA categories of obstetric care (uncomplicated cases, most complicated cases, and all serious illnesses) and NICU (yes/no), critical access and sole community provider status, teaching status, and rurality (core-based statistical area; categorized as metro, micro, or rural) from the 2018 AHA Annual Survey.
Data Analysis
Our analyses were conducted with a subset of LaborRNs hospitals that reported their 2018 EBMF rate to The Joint Commission. The outcome of the EBMF rate was collected at the hospital level; therefore, we aggregated all variables of interest (predictors, mediators, and covariates) to the hospital level. Mean nurse age, mean years of experience as a labor and birth RN, summed scores of missed care aspects (1–25), staffing guideline adherence score (1–4), and safety climate (1–5) were aggregated to the hospital level based on the average scores among nurse respondents in each hospital. The proportion of respondents with a baccalaureate degree (BSN/BS) or higher in nursing and proportions of nurses reporting each specific nursing care aspect missed on each unit were calculated at the hospital level.
Descriptive statistics were computed to summarize characteristics of nurse respondents and hospitals, using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. The EBMF rate was tested for normality of distribution across hospitals using the Shapiro–Wilk test. Differences in EBMF rates on categorical hospital characteristics were tested using one-way analysis of variance. Bivariate linear regression models were then used to determine the association between continuous nurse/hospital variables and EBMF rate at the hospital level and to estimate the relationship between staffing guideline adherence and missed nursing care. Variables associated with EBMF rate at an exploratory level of significance (p < .10) in bivariate analyses or deemed essential to the model by experts on maternity nurse staffing were further included in a mediation analysis of staffing guideline adherence, missed nursing care, and EBMF rate. A generalized structural equation model was used to assess the mediating effect of missed nursing care on the association between staffing guideline adherence and EBMF rate. Generalized structural equation models are models that can estimate the linear associations of noncontinuous (e.g., binary, categorical, and count) indicator variables. Maximum likelihood was used to estimate total, direct, and indirect effects. All statistical analyses were conducted using Stata, Release 13 (StataCorp LP, College Station, TX).
RESULTS
The sample included 184 hospitals in 29 states and 2,691 labor nurses. Table 1 presents the characteristics of nurse respondents. The mean age was 40.6 (±11.7) years, and mean years of labor nurse experience was 12.5 (±12.1). Most respondents were female, White, and worked full-time. About half of the respondents worked day shifts, one third worked night shifts, and the remainder worked evenings or rotating shifts; nearly 75% of respondents held a bachelor’s or higher degree. The EBMF rate in sample hospitals ranged from 12.8% to 97.2%, with a mean rate of 55.5% (SD = 16.1%). Hospital-level missed care scores ranged from 4.32–23 out of 25, with a mean of 11.12 (SD = 3.17). Hospital-level nurse staffing guideline adherence scores ranged from 1.75 to 3.89 out of 4, with a mean of 3.05 (SD = 0.49).
TABLE 1.
Demographic Characteristics of Nurse Respondents (N = 2,691)
| Respondent characteristics | N | n | % | Mean | SD |
|---|---|---|---|---|---|
| Age (years) | 2,507 | 40.63 | 11.74 | ||
| 18–24.9 | 102 | 4.1 | |||
| 25–44.9 | 1,500 | 59.9 | |||
| 45–64.9 | 860 | 34.3 | |||
| ≥65 | 42 | 1.7 | |||
| Gender | 2,382 | ||||
| Female | 2,319 | 97.4 | |||
| Male | 12 | 0.5 | |||
| Unknown/decline to report | 51 | 2.1 | |||
| Race | 2,691 | ||||
| American Indian/Alaska Native | 18 | 0.7 | |||
| Asian | 64 | 2.4 | |||
| Black/African American | 62 | 2.3 | |||
| Multiracial | 59 | 2.2 | |||
| Native Hawaiian/other Pacific Islander | 8 | 0.3 | |||
| White | 2,188 | 81.3 | |||
| Decline to report | 292 | 10.9 | |||
| Ethnicity | 2,433 | ||||
| Not Hispanic/Latino | 2,284 | 93.9 | |||
| Hispanic/Latino | 149 | 6.1 | |||
| Shift usually worked | 2,630 | ||||
| Days | 1,436 | 54.6 | |||
| Evenings | 94 | 3.6 | |||
| Nights | 929 | 35.3 | |||
| Rotating | 171 | 6.5 | |||
| Employment status | 2,631 | ||||
| Full-time | 1,962 | 74.6 | |||
| Part-time | 669 | 25.4 | |||
| Role in the unit | 2,649 | ||||
| Staff RN | 1,641 | 61.9 | |||
| Charge RN | 104 | 3.9 | |||
| Staff and charge RN | 705 | 26.6 | |||
| Administrator | 109 | 4.1 | |||
| Clinical nurse specialist or nurse educator | 33 | 1.3 | |||
| Other | 57 | 2.2 | |||
| Highest nursing education | 2,643 | ||||
| Diploma | 62 | 2.4 | |||
| Associate degree | 668 | 25.3 | |||
| Bachelor’s degree | 1,684 | 63.7 | |||
| Master’s degree | 220 | 8.3 | |||
| Doctoral degree | 9 | 0.3 | |||
| Years of experience as an RN | 2,609 | 14.96 | 12.95 | ||
| <5 | 543 | 20.8 | |||
| 5–9.9 | 578 | 22.2 | |||
| 10–19.9 | 667 | 25.6 | |||
| ≥20 | 821 | 31.5 | |||
| Years of experience as an L&B RN | 2,608 | 12.45 | 12.06 | ||
| <5 | 843 | 32.3 | |||
| 5–9.9 | 448 | 17.2 | |||
| 10–19.9 | 681 | 26.1 | |||
| ≥20 | 636 | 24.9 | |||
| Years working in current hospital | 2,589 | 10.44 | 9.73 | ||
| <5 | 1,002 | 38.7 | |||
| 5–9.9 | 483 | 18.7 | |||
| 10–19.9 | 639 | 24.7 | |||
| ≥20 | 465 | 8.0 |
Note. L&B = labor and birth; RN = registered nurse.
Table 2 presents EBMF rates by hospital characteristics. Most hospitals were in metro–urban areas and teaching-affiliated, had NICUs, and had nonprofit ownership. In bivariate analyses, obstetric level was identified as a significant covariate. Though not significant, hospital ownership and NICU status were also included in the model because of their substantive importance—based on the expert clinical judgment of our research team.
TABLE 2.
Distribution of Exclusive Breast Milk Feeding (EBMF) Rate by Hospital Characteristics (N = 184)
| Hospital characteristics | N | n | % | EBMF ratea | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | F | df | p | ||||
| Urban/rural | 184 | 1.19 | [2, 181] | .306 | ||||
| Metro | 152 | 82.6 | 0.56 | 0.15 | ||||
| Micro | 30 | 6.3 | 0.54 | 0.19 | ||||
| Rural | 2 | 1.9 | 0.40 | 0.36 | ||||
| Ownership | 184 | 3.47 | [3, 180] | .017 | ||||
| Government | 22 | 12.0 | 0.54 | 0.16 | ||||
| Church operated | 39 | 21.2 | 0.58 | 0.13 | ||||
| Other nonprofit | 104 | 56.5 | 0.57 | 0.17 | ||||
| Investor owned | 19 | 10.3 | 0.45 | 0.15 | ||||
| Teaching hospital | 184 | 1.98 | [1, 182] | .161 | ||||
| Yes | 114 | 62.0 | 0.54 | 0.16 | ||||
| No | 70 | 38.0 | 0.58 | 0.17 | ||||
| Critical assess hospital | 184 | 1.30 | [1, 182] | .256 | ||||
| Yes | 6 | 3.3 | 0.63 | 0.22 | ||||
| No | 178 | 96.7 | 0.55 | 0.16 | ||||
| Sole community provider | 184 | 0.55 | [1, 182] | .461 | ||||
| Yes | 14 | 7.6 | 0.53 | 0.21 | ||||
| No | 170 | 92.4 | 0.56 | 0.16 | ||||
| Obstetric level | 158 | 2.73 | [2, 155] | .068 | ||||
| Uncomplicated cases | 40 | 25.3 | 0.56 | 0.17 | ||||
| Most complicated cases | 63 | 39.9 | 0.59 | 0.15 | ||||
| All serious illnesses | 55 | 34.8 | 0.53 | 0.15 | ||||
| Neonatal intensive care hospital | 160 | 1.48 | [1, 158] | .226 | ||||
| Yes | 96 | 60.0 | 0.58 | 0.16 | ||||
| No | 64 | 40.0 | 0.55 | 0.16 | ||||
Note. N = 184 hospitals; analyses conducted using one-way analysis of variance.
aAs defined by The Joint Commission Perinatal Core Measure PC-05.
Results of the hospital-level bivariate regressions are shown in Table 3, including selected nurse and structural characteristics. The proportion of nurses with BSN or higher education was positively associated with EBMF rate (p < .10). Although not significantly associated with EBMF rates, years of labor nurse experience were identified as a potential nurse-level confounding variable for inclusion in the mediation models. For hospital environment characteristics, annual birth volume and nurse-perceived safety climate were significantly associated with EBMF rates (p < .10) and controlled in the mediation models.
TABLE 3.
Distribution of Structural Characteristics, Nurse Characteristics, and Nursing Process Indicators and Their Bivariate Associations With Exclusive Breast Milk Feeding (EBMF) Rates
| Variables | Mean | SD | EBMF rate | |||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | SE | p | |||
| Nurse respondent characteristics | ||||||
| Mean age | 41.12 | 5.30 | 0.004 | [−0.001, 0.008] | 0.002 | .101 |
| Mean year of experience as an L&B RN | 12.74 | 4.41 | 0.004 | [−0.002, 0.009] | 0.003 | .170 |
| Proportion of nurses with BSN or above | 0.66 | 0.21 | 0.011 | [−0.01, 0.215] | 0.057 | .076 |
| Structural characteristics | ||||||
| Nurse staffing (1–4) | 3.06 | 0.49 | 0.141 | [0.097, 0.183] | 0.022 | <.001 |
| Safety climate (1–5) | 4.12 | 0.4 | 0.051 | [−0.008, 0.110] | 0.030 | .091 |
| Annual birth volume (/1,000) | 1.94 | 1.91 | −0.014 | [−0.027, −0.002] | 0.006 | .019 |
| Nursing process indicators | ||||||
| Sum missed care score (1–25) | 11.12 | 3.17 | −0.014 | [−0.021, −0.007] | 0.004 | <.001 |
| Missed skin-to-skin mother baby care after birth (0–1) | 0.25 | 0.19 | −0.427 | [−0.534, −0.321] | 0.053 | <.001 |
| Missed breastfeeding within 1 hour after birth (0–1) | 0.38 | 0.23 | −0.307 | [−0.400, −0.213] | 0.047 | <.001 |
| Missed recovery care (0–1) | 0.43 | 0.23 | −0.157 | [−0.257, −0.057] | 0.051 | .002 |
Note. Coefficients, SEs, and p-values reported from bivariate regressions predicting EBMF and for bivariate association between nurse staffing and missed nursing care. Birth volumes in each hospital were divided by 1,000 to calibrate the coefficients and 95% CI better. CI = confidence interval; L&B = labor and birth; RN = registered nurse; BSN = Bachelor of Science in Nursing.
In bivariate analyses, staffing guideline adherence and frequency of missed care were both associated with the EBMF rate (Table 3). Staffing guideline adherence was positively associated with EBMF rate (p < .05). Missed care aspects were negatively associated with EBMF rate (p < .05). In addition, three breastfeeding-related items in missed care aspects, including missed skin-to-skin mother–baby care after birth, missed breastfeeding within 1 hour after birth, and missed recovery care, were all negatively associated with EBMF rate (p < .05). In the mediation analysis to assess whether indicators of missed care mediate the association between staffing guideline adherence and EBMF rate, covariates included years of labor nurse experience, proportion of nurses with BSN education or above, safety climate, annual birth volume, hospital ownership, obstetric level, and NICU hospital.
Generalized structural equation modeling (Table 4) showed that overall perinatal missed care (sum of all items) did not significantly mediate the association between staffing guideline adherence and EBMF rate (p > .05). In contrast, two aspects of perinatal missed care related to breastfeeding partially mediated this path. Missed skin-to-skin mother–baby care after birth had a significant indirect effect (β = 0.035), and missed breastfeeding within 1 hour after birth had a significant indirect effect (β = 0.029). The indirect effects for these two elements were significant, yet the direct result between staffing and EBMF rate also remained significant, indicating partial mediation (Figure 1). Missed recovery care in the first 2 hours following birth did not exhibit a significant indirect effect between nurse staffing and EBMF rate (p > .05).
TABLE 4.
Generalized Structural Equation Modeling of Nurse Staffing and Missed Nursing Care on Exclusive Breast Milk Feeding (EBMF) Rate at the Hospital Level (N = 158 Hospitals)
| Effects | Coefficient | 95% CI | p |
|---|---|---|---|
| Nurse staffing → Missed nursing care overall → EBMF rate | |||
| Total effect | 0.136 | [0.081, 0.190] | <.001 |
| Direct effect | 0.123 | [0.064, 0.183] | <.001 |
| Indirect effect | 0.012 | [−0.008, 0.033] | .236 |
| Nurse staffing → Missed skin-to-skin mother–baby care after birth → EBMF rate | |||
| Total effect | 0.133 | [0.080, 0.187] | <.001 |
| Direct effect | 0.098 | [0.047, 0.148] | <.001 |
| Indirect effect | 0.035 | [0.012, 0.059] | .003 |
| Nurse staffing → Missed breastfeeding within 1 hour after birth → EBMF rate | |||
| Total effect | 0.134 | [0.081, 0.188] | <.001 |
| Direct effect | 0.106 | [0.054, 0.157] | <.001 |
| Indirect effect | 0.029 | [0.008, 0.051] | .007 |
| Nurse staffing → Missed recovery care → EBMF rate | |||
| Total effect | 0.138 | [0.083, 0.193] | <.001 |
| Direct effect | 0.136 | [0.079, 0.194] | <.001 |
| Indirect effect | 0.001 | [−0.014, 0.017] | .860 |
Note. Covariates were controlled in mediation models, including safety climate, annual birth volume, hospital ownership, obstetric level, neonatal intensive care hospital, mean years of experience as a labor nurse, and proportion of respondents with BSN degree or above. CI = confidence interval.
FIGURE 1.
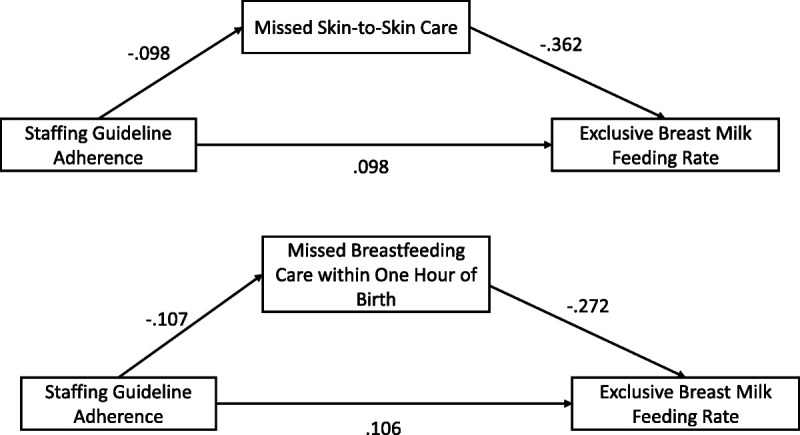
Significant mediation effects of missed care items between nurse-reported staffing guideline adherence and exclusive breast milk feeding rate.
DISCUSSION
Nurse-reported compliance with AWHONN staffing guidelines was a significant predictor of hospital EBMF rate in this sample of 184 birth hospitals that participated in the LaborRNs study and reported their 2018 EBMF rate to The Joint Commission. The mean EBMF rate in our sample was consistent with a recent national study of hospital breastfeeding rates (Patterson et al., 2021). Two aspects of basic nursing care partially mediated the relationship between the staffing guideline adherence measure and the EBMF rate that labor nurses provide: skin-to-skin mother–baby care and breastfeeding within 1 hour of birth. These results support the hypothesis that labor and birth patient outcomes are sensitive to nurse staffing. The results specifically support the hypothesis generated by prior qualitative research with mothers, nurses, and physicians that EBMF is a nurse-sensitive outcome (Lyndon et al., 2017). Our findings further support missed nursing care as one pathway through which nurse staffing may affect childbirth outcomes.
A recent umbrella review of 15 systematic reviews on the relationship between nurse staffing and nurse-sensitive patient outcomes found strong evidence for length of stay, patient dissatisfaction, poor-quality nursing care, and readmission as sensitive to nurse staffing and moderate evidence for the relationship of nurse staffing to failure to rescue, medication errors, mortality, pneumonia, and respiratory failure (Blume et al., 2021). Although a few of these outcomes apply to maternity care, most are rare and not reflective of the main issues in maternity nursing care. Several studies have identified nurse-sensitive outcomes for NICU (Hallowell et al., 2016; Tawfik et al., 2020; Tubbs-Cooley et al., 2015). However, our study is one of few that has tested the relationship of any measure of RN staffing during labor, birth, and the immediate postpartum period with patient outcomes, and those who have tested these relationships have had mixed results (Simpson et al., 2020; Turner et al., 2021; Wilson & Butler, 2021). Hence, our results represent a step toward developing nurse-sensitive outcome indicators specific to maternity care.
Likewise, the literature on perinatal missed nursing care is limited. To date, three U.S. studies report the prevalence of missed nursing care during labor and birth (Lake et al., 2020; Lyndon et al., 2022; Simpson et al., 2019). There are also studies examining missed nursing care among midwives in Australia (Blackman et al., 2020) and nurses and midwives in Ethiopia (Haftu et al., 2019) reporting high prevalence of missed nursing care; however, neither of these studies included assessment of care specific to breastfeeding. The relationship between the models of care during labor and birth in these countries and the United States is difficult to determine. There is substantial correspondence between the responsibilities of U.S. labor nurses during labor and birth and those of U.K. midwives (Lyndon et al., 2017), and our U.S.-based results may apply to these other countries.
Strengths and Limitations
This study provides evidence for the role of nursing care during labor on patient outcomes, specifically initiation of human milk feeding. Limitations include the self-reported nature of staffing guideline adherence and missed nursing care, potential self-selection bias among participating hospitals, lack of information about hospitals’ baby-friendly status, and the inability to obtain EBMF rates for all hospitals in the larger sample of participating hospitals. The RN study population had a lower mean age, less racial/ethnic diversity, and greater proportion of females and BSN or higher education than the general U.S. nursing population. National specialty data are not available for comparison to the U.S. population of labor and birth nurses.
Staffing measures are uniquely tricky for labor and birth because of factors affecting care during labor and birth that hours per patient day do not capture (Simpson, 2015; Wilson & Blegen, 2010), and there is no standard objective measure for staffing labor within birth units. We chose to use nurses’ perceptions of their unit’s compliance with AWHONN staffing guidelines, as it is reasonable to assume that nurses can reliably report the number of patients they are typically assigned. Nurses understand the unit’s typical staffing patterns throughout multiple assignments. Although it would be desirable to have an objective measure of missed nursing care, self-report is a standard approach in this type of research (Griffiths et al., 2018; Jones et al., 2015). Objective measures are logistically challenging to obtain at scale.
The nature of our data dictated our analyses. Because the outcome of interest (EBMF) is reported to The Joint Commission at the hospital level, this necessitated aggregating the nurse-level data and conducting the analyses at the hospital level. A limitation is a potential for ascribing the relationships identified at the group level to individuals. Our approach is reasonable in the context of the challenges of obtaining valid individual-level breast milk feeding data across many settings. Finally, given the known disparities in breastfeeding rates across racial groups (Centers for Disease Control and Prevention, 2021), examining racialized aspects of human milk feeding support is vital. Hospital-level data on race and ethnicity were not available at the time of this analysis.
Conclusion
The results of this study provide evidence supporting exclusive breast milk feeding during childbirth hospitalization as a nurse-sensitive outcome. The relationship between nurse staffing, missed nursing care, and exclusive breast milk feeding during childbirth hospitalization is essential because human milk feeding has substantial life course health benefits to birthing people and newborns. Hospitals should facilitate practices that promote successful human milk feeding, including providing adequate staffing and organizational structures to support nurses’ provision of high-quality care, including routine skin-to-skin care at birth and assistance with initiating feeding within the first hour of birth.

ORCID iDs
Audrey Lyndon https://orcid.org/0000-0003-2215-4273
Kathleen Simpson https://orcid.org/0000-0002-9023-8009
Joanne Spetz https://orcid.org/0000-0003-3112-5511
Jie Zhong https://orcid.org/0000-0003-1025-7785
Jason Fletcher https://orcid.org/0000-0002-4760-7200
Caryl Gay https://orcid.org/0000-0002-6865-6335
Gay Landstrom https://orchid.org/0000-0002-7133-9381
Footnotes
This project was supported by the Agency for Healthcare Research and Quality (Grant No. R01HS025715). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The Association for Women’s Health, Obstetric and Neonatal Nursing supported the development of the survey used in this study and provided nonfinancial support for study recruitment.
The authors have no conflicts of interest to report.
Contributor Information
Audrey Lyndon, Email: al6148@nyu.edu.
Kathleen Rice Simpson, Email: krsimpson@prodigy.net.
Joanne Spetz, Email: joanne.spetz@ucsf.edu.
Jie Zhong, Email: jz3750@nyu.edu.
Caryl L. Gay, Email: caryl.gay@ucsf.edu.
Jason Fletcher, Email: jason.fletcher@nyu.edu.
Gay L. Landstrom, Email: gay.landstrom@trinity-health.org.
REFERENCES
- Agency for Healthcare Research and Quality . (2021). HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP). April 2021. Retrieved October 2021, from https://hcup-us.ahrq.gov/faststats/NationalDiagnosesServlet
- Aiken L. H. Cimiotti J. P. Sloane D. M. Smith H. L. Flynn L., & Neff D. F. (2011). Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care, 49, 1047–1053. 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L. H. Sermeus W. Van den Heede K. Sloane D. M. Busse R. McKee M. Bruyneel L. Rafferty A. M. Griffiths P. Moreno-Casbas M. T. Tishelman C. Scott A. Brzostek T. Kinnunen J. Schwendimann R. Heinen M. Zikos D. Sjetne I. S. Smith H. L., & Kutney-Lee A. (2012). Patient safety, satisfaction, and quality of hospital care: Cross-sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ, 344, e1717. 10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists . (2021). Barriers to breastfeeding: Supporting initiation and continuation of breastfeeding: ACOG committee opinion, number 821. Obstetrics and Gynecology, 137, e54–e62. 10.1097/AOG.0000000000004249 [DOI] [PubMed] [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses . (2010). Guidelines for professional registered nurse staffing for perinatal units.
- Association of Women’s Health, Obstetric and Neonatal Nurses . (2021). Breastfeeding and the use of human milk (an official statement). Journal of Obstetric, Gynecologic, & Neonatal Nursing, 50, e1–e5. 10.1016/j.jogn.2021.06.006 [DOI] [PubMed] [Google Scholar]
- Ball J. E. Bruyneel L. Aiken L. H. Sermeus W. Sloane D. M. Rafferty A. M. Lindqvist R. Tishelman C., & Griffiths P. (2018). Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies, 78, 10–15. 10.1016/j.ijnurstu.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackman I. Hadjigeorgiou E., & McNeill L. (2020). Causal links to missed Australian midwifery care: What is the evidence? European Journal of Midwifery, 4, 41. 10.18332/ejm/127769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blume K. S. Dietermann K. Kirchner-Heklau U. Winter V. Fleischer S. Kreidl L. M. Meyer G., & Schreyogg J. (2021). Staffing levels and nursing-sensitive patient outcomes: Umbrella review and qualitative study. Health Services Research, 56, 885–907. 10.1111/1475-6773.13647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramson L. Lee J. W. Moore E. Montgomery S. Neish C. Bahjri K., & Melcher C. L. (2010). Effect of early skin-to-skin mother–infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. Journal of Human Lactation, 26, 130–137. 10.1177/0890334409355779 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2021). Breastfeeding report card United States, 2020. https://www.cdc.gov/breastfeeding/pdf/2020-Breastfeeding-Report-Card-H.pdf
- Donabedian A. (1980). The definition of quality and approaches to its assessment. Health Administration Press. [Google Scholar]
- Gregory E. C. Osterman M. J., & Valenzuela C. P. (2021). NVSR 70-15: Changes in home births by race and Hispanic origin and state of residence of mother: United States, 2018–2019 and 2019–2020. National Vital Statistics Reports, 70. 10.15620/cdc:110853 [DOI] [PubMed] [Google Scholar]
- Griffiths P. Dall’Ora C. Simon M. Ball J. Lindqvist R. Rafferty A.-M. Schoonhoven L. Tishelman C., & Aiken L. H. (2014). Nurses’ shift length and overtime working in 12 European countries: The association with perceived quality of care and patient safety. Medical Care, 52, 975–981. 10.1097/mlr.0000000000000233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P. Recio-Saucedo A. Dall’Ora C. Briggs J. Maruotti A. Meredith P. Smith G. B., & Ball J., Missed Care Study Group . (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74, 1474–1487. 10.1111/jan.13564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haftu M. Girmay A. Gebremeskel M. Aregawi G. Gebregziabher D., & Robles C. (2019). Commonly missed nursing cares in the obstetrics and gynecologic wards of Tigray general hospitals; Northern Ethiopia. PLOS ONE, 14, e0225814. 10.1371/journal.pone.0225814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallowell S. G. Rogowski J. A. Spatz D. L. Hanlon A. L. Kenny M., & Lake E. T. (2016). Factors associated with infant feeding of human milk at discharge from neonatal intensive care: Cross-sectional analysis of nurse survey and infant outcomes data. International Journal of Nursing Studies, 53, 190–203. 10.1016/j.ijnurstu.2015.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones T. L. Hamilton P., & Murry N. (2015). Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52, 1121–1137. 10.1016/j.ijnurstu.2015.02.012 [DOI] [PubMed] [Google Scholar]
- Kalisch B. J. Landstrom G. L., & Hinshaw A. S. (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65, 1509–1517. 10.1111/j.1365-2648.2009.05027.x [DOI] [PubMed] [Google Scholar]
- Kalisch B. J., & Williams R. A. (2009). Development and psychometric testing of a tool to measure missed nursing care. The Journal of Nursing Administration, 39, 211–219. 10.1097/NNA.0b013e3181a23cf5 [DOI] [PubMed] [Google Scholar]
- Lake E. T. de Cordova P. B. Barton S. Singh S. Agosto P. D. Ely B. Roberts K. E., & Aiken L. H. (2017). Missed nursing care in pediatrics. Hospital Pediatrics, 7, 378–384. 10.1542/hpeds.2016-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E. T. French R. O’Rourke K. Sanders J., & Srinivas S. K. (2020). Linking the work environment to missed nursing care in labour and delivery. Journal of Nursing Management, 28, 1901–1908. 10.1111/jonm.12856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyndon A. Simpson K. R., & Spetz J. (2017). Thematic analysis of US stakeholder views on the influence of labour nurses’ care on birth outcomes. BMJ Quality & Safety, 26, 824–831. 10.1136/bmjqs-2016-005859 [DOI] [PubMed] [Google Scholar]
- Lyndon A. Simpson K. R. Spetz J. Fletcher J. Gay C. L., & Landstrom G. L. (2022). Psychometric properties of the perinatal missed care survey and missed care during labor and birth. Applied Nursing Research, 63, 151516. 10.1016/j.apnr.2021.151516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meek J. Y., & Noble L., Section on Breastfeeding . (2022). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 150, e2022057988. 10.1542/peds.2022-057988 [DOI] [PubMed] [Google Scholar]
- Patterson J. A. Keuler N. S., & Buckingham W. R. (2021). Differences in exclusive breastfeeding rates in US hospitals according to babyfriendly hospital initiative designation and area deprivation index category. Breastfeeding Medicine, 16, 799–806. 10.1089/bfm.2021.0050 [DOI] [PubMed] [Google Scholar]
- Rollins N. C. Bhandari N. Hajeebhoy N. Horton S. Lutter C. K. Martines J. C. Piwoz E. G. Richter L. M., & Victora C. G., Lancet Breastfeeding Series Group . (2016). Why invest, and what it will take to improve breastfeeding practices? Lancet, 387, 491–504. 10.1016/S0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Sexton J. B. Helmreich R. L. Neilands T. B. Rowan K. Vella K. Boyden J. Roberts P. R., & Thomas E. J. (2006). The safety attitudes questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Services Research, 6, 44. 10.1186/1472-6963-6-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson K. R. (2015). Predicting nurse staffing needs for a labor and birth unit in a large-volume perinatal service. Journal of Obstetric, Gynecologic & Neonatal Nursing, 44, 329–338. 10.1111/1552-6909.12549 [DOI] [PubMed] [Google Scholar]
- Simpson K. R. Lyndon A., & Ruhl C. (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and job stress and dissatisfaction. Journal of Obstetric, Gynecologic & Neonatal Nursing, 45, 481–490. 10.1016/j.jogn.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Simpson K. R. Lyndon A. Spetz J. Gay C. L., & Landstrom G. L. (2019). Adaptation of the MISSCARE survey to the maternity care setting. Journal of Obstetric, Gynecologic & Neonatal Nursing, 48, 456–467. 10.1016/j.jogn.2019.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson K. R. Lyndon A. Spetz J. Gay C. L., & Landstrom G. L. (2020). Missed nursing care during labor and birth and exclusive breast milk feeding during hospitalization for childbirth. MCN. The American Journal of Maternal Child Nursing, 45, 280–288. 10.1097/NMC.0000000000000644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tawfik D. S. Profit J. Lake E. T. Liu J. B. Sanders L. M., & Phibbs C. S. (2020). Development and use of an adjusted nurse staffing metric in the neonatal intensive care unit. Health Services Research, 55, 190–200. 10.1111/1475-6773.13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joint Commission . (2018). Specifications manual for Joint Commission national quality measures (v2018A). https://manual.jointcommission.org/releases/TJC2018A/
- Tubbs-Cooley H. L. Pickler R. H., & Meinzen-Derr J. K. (2015). Missed oral feeding opportunities and preterm infants’ time to achieve full oral feedings and neonatal intensive care unit discharge. American Journal of Perinatology, 32, 1–8. 10.1055/s-0034-1372426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner L. Griffiths P., & Kitson-Reynolds E. (2021). Midwifery and nurse staffing of inpatient maternity services—A systematic scoping review of associations with outcomes and quality of care. Midwifery, 103, 103118. 10.1016/j.midw.2021.103118 [DOI] [PubMed] [Google Scholar]
- Wilson B. L., & Blegen M. (2010). Labor and delivery nurse staffing as a cost-effective safety intervention. The Journal of Perinatal & Neonatal Nursing, 24, 312–319. 10.1097/JPN.0b013e3181f32703 [DOI] [PubMed] [Google Scholar]
- Wilson B. L., & Butler R. J. (2021). Identifying optimal labor and delivery nurse staffing: The case of cesarean births and nursing hours. Nursing Outlook, 69, 84–95. 10.1016/j.outlook.2020.07.003 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2017). Guideline: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. https://apps.who.int/iris/bitstream/handle/10665/259386/9789241550086-eng.pdf [PubMed]


