Abstract
Background
Intensive care unit (ICU) nurses are at an increased risk of burnout and may have an intention-to-leave their jobs. The COVID-19 pandemic may increase this risk.
Objective
The objective of this study was to describe the prevalence of burnout risk and intention-to-leave the job and nursing profession among ICU nurses and to analyse the relationships between these variables and the work environment after two years of the COVID-19 pandemic.
Design
A national cross-sectional survey of all nurses working in Belgian ICUs was conducted between December 2021 and January 2022 during the 4th and 5th waves of the COVID-19 pandemic in Belgium. The Practice Environment Scale of the Nursing Work Index (PES-NWI) was used to measure the work environment, intention-to-leave the hospital and/or the profession was assessed. The risk of burnout was assessed using the Maslach Burnout Inventory scale including emotional exhaustion, depersonalisation, and reduced personal accomplishment.
Setting
Nurses in 78 out of 123 Belgian hospital sites with an ICU participated in the survey.
Participants
2321 out of 4851 nurses (47.8%) completed the entire online survey.
Results
The median overall risk of burnout per hospital site (high risk in all three subdimensions) was 17.6% [P25: 10.0 - P75: 28.8] and the median proportion of nurses with a high risk in at least one subdimension of burnout in Belgian ICUs was 71.6% [56.7–82.7]. A median of 42.9% [32.1–57.1] of ICU nurses stated that they intended-to-leave the job and 23.8% [15.4–36.8] stated an intent-to-leave the profession. The median overall score of agreement with the presence of positive aspects in the work environment was 49.0% [44.8–55.8]. Overall, nurses working in the top 25% of best-performing hospital sites with regard to work environment had a statistically significant lower risk of burnout and intention-to-leave the job and profession compared to those in the lowest performing 25% of hospital sites. Patient-to-nurse ratio in the worst performing quartile was associated with a higher risk for emotional exhaustion (OR = 1.53, 95% CI:1.04–2.26) and depersonalisation (OR = 1.48, 95% CI:1.03–2.13) and intention-to-leave the job (OR = 1.46, 95% CI:1.03–2.05).
Conclusions
In this study, a high prevalence of burnout risk and intention-to-leave the job and nursing profession was observed after two years of the COVID-19 pandemic. Nevertheless, there was substantial variation across hospital sites which was associated with the quality of the work environment.
Tweetable abstract
“Burnout & intention to leave was high for Belgian ICU nurses after 2 years of COVID, but wellbeing was better with high quality work environments and more favourable patient to nurse ratios”.
Keywords: Burnout, Intensive care units, Nurses, COVID-19, Adults, Workload
What is already known
-
•
The COVID-19 pandemic has had a strong impact on ICU nurses' wellbeing and increases the risk of burnout
-
•
A large proportion of ICU nurses in Belgium are at high risk of burnout
-
•
A better work environment is associated with better quality of care, employee satisfaction, turnover, and average job tenure among ICU nurses
What this paper adds
-
•
Even after two years of the COVID-19 pandemic, ICU nurses working in hospitals with a better working environment had less risk of burnout and intention-to-leave.
-
•
Nurse participation in hospital affairs and staffing, and resource adequacy are the work environment dimensions with the lowest score and require particular attention.
-
•
ICU nurses working in hospitals with a lower patient-to-nurse ratio have a lower risk of emotional exhaustion, depersonalisation, and intention-to-leave the job.
1. Background
Burnout is a syndrome that is conceptualised as chronic workplace stress that has not been successfully managed and has resulted in feelings of emotional exhaustion, depersonalization, and a lack of personal accomplishment (Maslach et al., 1996; Atroszko et al., 2020). Nurses are particularly prone to burnout due to various professional practice circumstances and working conditions that can lead to physical and emotional exhaustion (Aiken et al., 2012, Aiken et al., 2012; Woo et al., 2020). Nurse burnout is associated with reduced safety and quality of care, decreased patient satisfaction, and reduced organisational commitment and productivity of nurses (Jun et al., 2021; Van Gerven et al., 2016). Some studies have reported a high prevalence of burnout among nurses in Belgium compared to other European countries (Woo et al., 2020). One study reported a prevalence of 30% of high risk of emotional exhaustion among nurses working in hospitals in 2012 (Vandenbroeck et al., 2017) while another reported a prevalence of 36% among nurses in general medical and surgical units in 2019 (Van den Heede et al., 2019). One of the main potential explanations for this high prevalence is the high patient-to-nurse ratio in Belgium compared to other countries (Aiken et al., 2012, Aiken et al., 2012), which has been shown to be associated with high risk of burnout (Pérez-Francisco et al., 2020; Welp et al., 2019). Nevertheless, a study published in 2018 reported a lower risk of burnout among intensive care unit (ICU) nurses: 11% had a high risk of emotional exhaustion. This study also showed that 7% of ICU nurses intended to leave the nursing profession (Vermeir et al., 2018).
Since March 2020, Europe has been facing the COVID-19 pandemic, caused by the SARS-CoV-2 virus. In Belgium, the Hospital Emergency Plan was launched on March 13, 2020. Intensive care units in Belgium have been heavily impacted by COVID-19 and mortality has been high (Taccone et al., 2020). As of this time, the country has experienced seven waves, mainly in the autumn and winter of December 2021 (Dellicour et al., 2021; Molenberghs et al., 2020; Natalia et al., 2022). During the COVID-19 pandemic, frontline nurses were exposed to higher levels of stress and traumatic events that could increase the risk of burnout (Guixia and Hui, 2020; Hu et al., 2020; LeClaire et al., 2022; Moradi et al., 2021). A study conducted after the first wave of COVID-19 showed a high risk of emotional exhaustion (38%) among French-speaking ICU nurses in Belgium (Bruyneel et al., 2021b). This high risk of emotional exhaustion was more pronounced in ICU nurses compared to non-ICU nurses (Odds Ratio [OR] = 1.23, 95% Confidence Interval [CI]: 1.07–1.42) (Bruyneel and Smith, 2021). The main risk factors for burnout among ICU nurses during the COVID-19 pandemic were a higher than standard patient-to-nurse ratio, a perceived increase in workload, having symptoms of COVID-19 without being tested, and shortage of COVID-19 protective equipment. Another study in Belgium showed an increase in the risk of burnout and the high risk of emotional exhaustion in French-speaking ICU nurses compared to before the COVID-19 pandemic (Butera et al., 2021). The nurse-to-patient ratio in the ICU in Belgium (about 1:3) is the most unfavourable in Europe, which could explain this high prevalence (Bruyneel et al., 2019; Van Den Heede et al., 2022).
There is a large body of evidence that shows that nurse workload, the quality of the work environment, and patient care demands influence patient outcomes (Cho et al., 2015; Lake et al., 2020; Simonetti et al., 2021). A study in the United States (US) found that interventions that aim to provide better work environment standards (e.g., true collaboration, authentic leadership, collaboration, effective decision making, appropriate staffing, meaningful recognition) are associated with improved employee satisfaction, turnover, and average job tenure among ICU nurses (Kester et al., 2021).
The association between work environment and nurse well-being is very clear in the literature. However, it is unclear whether this association was still valid during a public health crisis that induced a lot of additional stress in healthcare workers: was a better hospital work environment associated with the well-being of ICU nurses during the COVID-19 pandemic? The objectives of this study were to describe the prevalence of high burnout risk, and intention-to-leave the job and the nursing profession among ICU nurses and to analyse the relationships between these variables and the work environment after two years of the COVID-19 pandemic.
2. Methods
2.1. Study design
A national cross-sectional study was conducted between December 2021 and January 2022 during the 4th and 5th waves of the COVID-19 pandemic in Belgium (supplementary material Fig. 1). For the recruitment of hospitals and intensive care units, all general acute hospitals (including university hospitals) were invited to participate (invitation to the Chief Nursing Officer - CNO and the Chief Executive Officer (CEO)/Chief Medical Officer – CMO) via an email invitation sent in the first week of September 2021. After 14 days, a reminder was sent to hospitals that did not respond to the initial invitation. The call to participate was open until 1 October, 2021. All hospitals that wanted to participate were allowed to participate with all the intensive care units of the hospital. The hospital managers could limit the participation to one hospital site if a hospital consisted of multiple sites. Each hospital had to appoint a field manager (e.g., chief nursing officer, middle management, ward manager) to be the single point of contact with the research team. During an information session (virtual or in person), the field manager was given additional explanation about the data collection process or could ask for more details about the study.
The survey target population included all registered staff nurses providing direct care to patients in the participating ICU units. Nurses on leave (sick leave, maternity leave, or holiday), agency nurses, ward managers, healthcare assistants, and other non-nursing staff were excluded. Per participating ICU, the number of eligible nurses (applying the inclusion and exclusion criteria on 21 September, 2021) was used to prepare unique participation IDs (QR code giving access to the online survey). All nurses received an envelope from the field manager with information about the study and an invitation to participate. This invitation included an individualised but anonymized link (QR-code) to an online survey (online platform, Check Market). The QR code allowed (with consent of the respondents) the identification of the nursing unit of the respondent.
2.2. Instruments and measures
The survey was largely based on the RN4CAST survey that was designed to study how features of the work environment and staffing levels (number and qualification) impact nurse retention, burnout among nurses, and patient outcomes (Sermeus et al., 2011). Except for some minor modifications in scoping review and professional nursing organisation (e.g., SIZ Nursing) to better match the ICU site, the same survey that was used during a previous nationwide study conducted on general hospitalisation units in 2009 and 2019 was used. The survey is available in French, Dutch, and German (Van den Heede et al., 2019).
The instrument includes the following measures and questions (Sermeus et al., 2011):
(1) Demographic variables, such as education level, age, gender and years of expertise within the hospital/profession/ICU.
(2) Information on nurse staffing. Each nurse was asked to provide information on their qualification level, and to report the number of nurses and patients present on the nursing ward as well as the number of patients cared for during the last shift or workday. Based on the provided information, patient-to-nurse ratios were calculated overall and per type of shift (Sermeus et al., 2011).
(3) The risk of burnout. The risk of burnout was assessed using the validated Maslach Burnout Inventory (MBI) scale (Dion and Tessier, 1994; Maslach et al., 1986). The 22 items of this scale are scored on a 7-point Likert scale ranging from 0 = Never to 6 = Every day capturing 3 dimensions of burnout: emotional exhaustion (EE), depersonalisation (DP), and reduced personal achievement (PA). The cut-off points for high risk were > 26 for emotional exhaustion, > 9 for depersonalisation, and < 33 for reduced personal achievement (Maslach et al., 1986). To estimate the overall prevalence of burnout, two definitions were used to compare with other studies. The first is the high risk of burnout in at least one of the three dimensions (broad definition) (Bruyneel et al., 2021b; Butera et al., 2021; Embriaco et al., 2007; Shah et al., 2019). The second is a single score according to the method that is most frequently used in the literature: a combination of high emotional exhaustion, high depersonalisation, and low personal achievement (strict definition) (Boutou et al., 2019; Rotenstein et al., 2018).
(4) The intention-to-leave the hospital and/or the profession in the next year was assessed dichotomously (yes or no). For those who answered yes, the type of work sought was requested.
(5) The Practice Environment Scale of the Nursing Work Index (PES-NWI) (Lake, 2002) was used to measure the nursing practice environment as is commonly done (Swiger et al., 2017). It includes 32 items with an ordinal score (from 1 = strongly disagree to 4 = strongly agree) to assess 5 components of the environment: Nurse participation in hospital affairs (1), nursing foundations for quality of care (2), nurse manager ability, leadership, and support of nurses (3), staffing and resource adequacy (4), and collegial nurse-physician relations (5). For each sub-dimension, we calculated the average percentage of nurses at the hospital site answering that they agree or strongly agree with the items of the Practice Environment Scale of the Nursing Work Index (overall score) of the items in the sub-dimension. We also categorised the nurse working environment into quartiles, based on a composite score calculated as the mean of the item scores for each hospital site. Hence, the lowest quartile consists of the 25% of hospital sites with the worst performance in nurse working environment and the highest quartile includes the 25% best performing hospital sites.
2.3. Statistical analyses
Nurses are considered key sources of information for the assessment of performance at the hospital site level. Hospital site descriptive statistics were computed by averaging answers from nurses within the same hospital site. Arbitrarily, at the level of a hospital site, a minimum of 10 respondents or a response rate of 75% was required to include the hospital site in the final sample, being sufficiently representative. Results at the national level were calculated as weighted average percentages by hospital site, the weight being the number of respondents at the hospital site. Median (Mdn) variables and InterQuartile Ranges (p25-p75) were used to describe all variables.
Multiple logistic regression analyses were performed to test the association between the nurse working environment and patient-to-nurse ratio at the hospital site level on the one hand (independent variables), and high risk of burnout and intention-to-leave the profession on the other hand (dependent variables). All analyses included variables for region and type of hospital site, and the sex, age, and qualification of the nurse. Moreover, the clustering of nurses within hospital sites was taken into account using a generalised estimation equation approach. Odds ratios (OR) with 95% confidence intervals (95% CI) and p-values are used to describe the results. A p-value < 0.05 was considered statistically significant.
The statistical analyses were performed using SAS 9.4 and R 4.1.2.
2.4. Ethical considerations
The ethics committee of University Hospital Leuven approved this study (S65994) on 12 November, 2021. The data were processed according to the Belgian law of 30 July, 2018 and with Regulation (EU) 2016/679 of 27 April, 2016, concerning the protection of natural persons in respect of processing activities and to ensure the free flow of personal data.
All nurses were informed via the information letter and electronically signed a Declaration of Consent via the software platform.
3. Results
3.1. Description of the participating hospitals and nurse characteristics
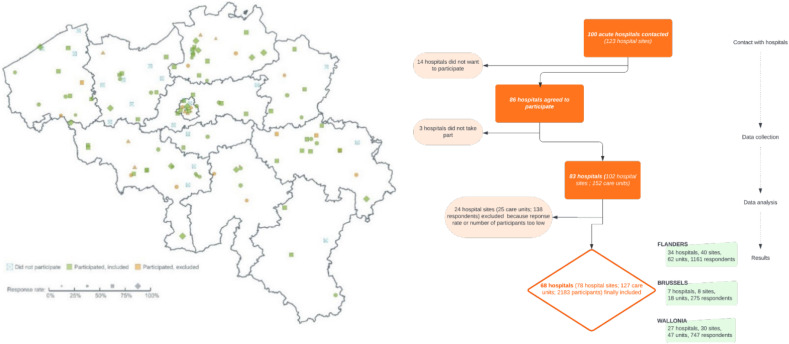
Eighty-six out of 100 Belgian acute hospitals (78 out of 123 hospital sites) with ICUs agreed to participate in the survey. Three hospitals that initially agreed to participate decided not to participate at the time the data collection started due to the extra burden caused by the 4th and 5th waves of the COVID-19 pandemic. The sample, therefore, included 83 hospitals, including six out of seven university hospitals, accounting for 1721 operational beds or 86.4% of the estimated operational ICU beds in Belgium. In total, 2321 of 4851 invited nurses completed the questionnaire, corresponding to a response rate of 47.8% (supplementary material Fig. 2). For the data analysis, 24 hospital sites with 138 respondents (5.9%) were further excluded because they did not reach the minimum of 10 respondents nor a response rate of 75%. Hence, the final sample included 68 hospitals, 78 hospital sites, and 2183 respondents (Fig. 1 ).
Fig. 1.
Hospital sites and respondent selection process.
The median age [p25-p75] of nurses per hospital site was 35 years [28–47] and the proportion of women was 74.5%. A total of 59.8% of the nurses worked full time and 72.2% of the sample were ICU specialist nurses and 10.6% had a university degree with a specialisation. The median patient-to-nurse ratio for the day shift was 2.1 [1.9–2.4] and 2.6 [2.3–2.8] for the night shift. The median ratio of healthcare assistant-to-patient and logistics support assistant-to-patient was 0.21 [0.10–0.43] and 0.43 [0.26–0.69], respectively (Table 1 ).
Table 1.
Description of the participating hospitals and nurse characteristics at the hospital site level.
| Variables | Results |
|---|---|
| Number ICU beds, n | 1721 |
| Number hospital academic, n (%) | 6 (8.8%) |
| Number bed academic, n (%) | 284 (16.5%) |
| Age (year), median [p25-p75] | 35 [28–47] |
| Gender, female, n (%) | 1626 (74.5%) |
| Experience in ICU (years), median [p25-p75] | 11 [4–22] |
| Full-time employed, n (%) | 1305 (59.8%) |
| Diploma, n (%) | |
| Bachelor's degree | 303 (13.9%) |
| Specialised nurses | 1577 (72.2%) |
| University degree | 34 (1.6%) |
| Specialised nurses and university degree | 232 (10.6%) |
| Nurses w/o bachelor's | 37 (1.7%) |
| Patient-to-nurse ratio, median [p25-p75] | |
| Overall ratio | 2.3 [2.0–2.5] |
| Day shifts (morning to evening) | 2.1 [1.9–2.4] |
| Night shift | 2.6 [2.3–2.8] |
| Healthcare assistants-to-patient ratio (all shifts and days), median [p25-p75] | 0.21 [0.10–0.43] |
| Logistic support assistants-to-patient ratio (all shifts and days), median [p25-p75] | 0.42 [0.26–0.69] |
Legend: ICU: Intensive Care Unit.
3.2. Prevalence of high risk of burnout and intention-to-leave the job and profession
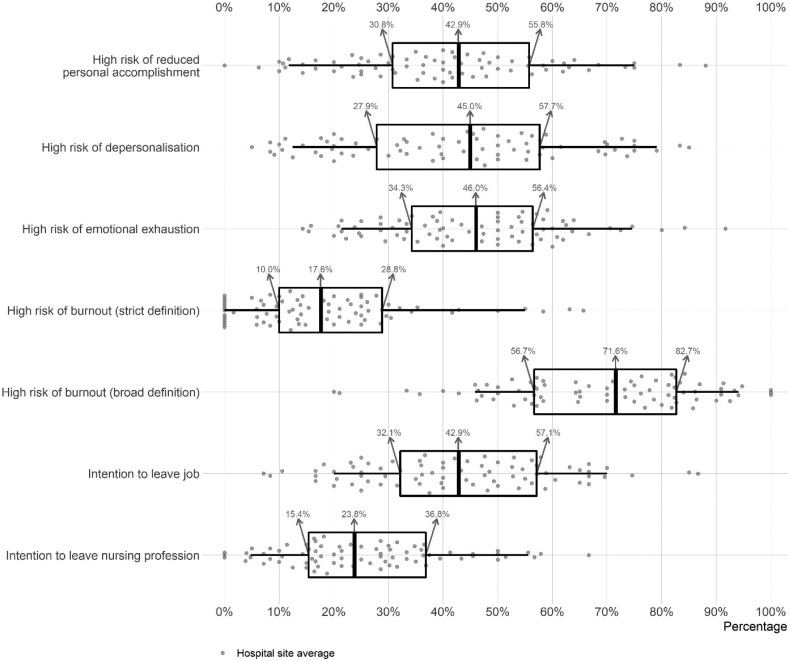
Regarding the high risk of burnout, the median prevalence at the hospital site level was 17.6% [10.0–28.8] using the strict definition and 71.6% [56.7–82.7] using the broad definition. The analysis of high risk of burnout by subdimension showed a median prevalence of 42.9% [30.8–55.8] for reduced personal achievement, 45.0% [27.9–57.7] for depersonalisation, and 46.0% [34.3–56.4] for emotional exhaustion. A median of 42.9% [32.1–57.1] of nurses at a given hospital site indicated an intention-to-leave their job and 23.8% [15.4–36.8] stated an intention-to-leave the nursing profession (Fig. 2 ).
Fig. 2.
Prevalence of risk of burnout and intention-to-leave the job.
3.3. Work environment
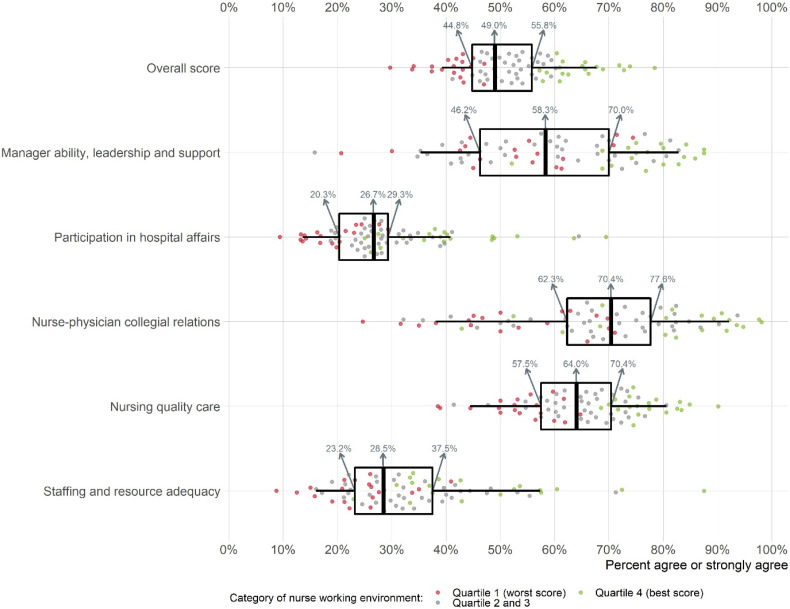
The median percentage of nurses at a given hospital site who agreed or strongly agreed with all Practice Environment Scale of the Nursing Work Index items was 49.0% [44.8–55.8]. There were three subscales with a higher median score (nurse-physician collegial relationship – 70.4% [62.3–77.8]; foundations for nursing quality of care – 64.0% [57.5–70.4]; manager ability, leadership, and support – 58.3% [46.2–70.0]) and two subscales with a lower median score (staffing and resource adequacy – 28.5% [23.2–37.5]; participation in hospital affairs – 26.7% [20.3–29.3]) (Fig. 3 ).
Fig. 3.
General overview of nurses (strongly) agreeing with presence of positive work environment aspects at hospital site.
3.4. Factors correlating burnout risk and intention-to-leave with work environment
In the multivariate analysis, overall, nurses working in hospitals with a better work environment had a statistically significant lower risk of burnout based on both definitions and all three dimensions as well as a lower risk of intention-to-leave the job and the nursing profession when comparing quartile 4 hospitals to quartile 1 (the lowest score). The higher patient-to-nurse ratio in the 4th quartile was associated with a higher risk for emotional exhaustion (OR = 1.53, 95% CI:1.04–2.26) and depersonalisation (OR = 1.48, 95% CI:1.03–2.13) and intention-to-leave the nursing profession (OR = 1.46, 95% CI:1.03–2.05) compared to the first quartile.
The nurses working in Brussels and Wallonia were statistically significant more at risk for the dimensions of burnout, for both definitions of burnout and intention-to-leave job as well as for the nursing profession than nurses working in Flanders. Master-level trained nurses had a higher risk of intention-to-leave the nursing profession (OR = 3.13, 95% CI:1.38–7.12) compared to bachelor-level nurses. Nurses in academic hospitals were more at risk for emotional exhaustion (OR = 1.42, 95% CI:1.11–1.82) and intention-to-leave the job (OR = 1.32, 95% CI:1.00–1.75) than those in non-academic hospitals. With regard to age, overall, older nurses were less likely to experience depersonalisation but more likely to have reduced personal achievement and nurses aged 25–40 were more likely to intend to leave their jobs and the nursing profession than nurses aged under 25 (Table 2 ).
Table 2.
Factors associated with burnout risk, intention-to-leave the profession, and work environment.
| At high risk of emotional exhaustion | At high risk of depersonalization | At high risk of reduced personal accomplishment | At high risk of burnout (strict definition) |
At high risk of burnout (broad definition) |
Intention-to-leave job | Intention-to-leave nursing profession | |
|---|---|---|---|---|---|---|---|
| OR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | OR [95%CI] | |
| Region | |||||||
| Flanders [REF] | – | – | – | – | – | – | – |
| Brussels | 1.74 [1.28–2.37]*** | 2.51 [1.74–3.61]*** | 2.27 [1.57–3.29]*** | 2.20 [1.37–3.52]** | 2.88 [1.61–5.13]*** | 1.79 [1.36–2.35]*** | 1.98 [1.24–3.18]** |
| Wallonia | 1.99 [1.50–2.62]*** | 2.62 [1.93–3.56]*** | 2.42 [1.93–3.04]*** | 2.61 [1.77–3.85]*** | 2.93 [2.16–3.98]*** | 1.71 [1.25–2.34]*** | 2.26 [1.67–3.08]*** |
| Hospital type | |||||||
| General hospital [REF] | – | – | – | – | – | – | – |
| University hospital | 1.42 [1.11–1.82]** | 1.09 [0.76–1.55] | 0.90 [0.64–1.26] | 1.37 [0.83–2.26] | 0.96 [0.64–1.44] | 1.32 [1.00–1.75]* | 1.34 [0.88–2.04] |
| Hospital-level patient-to-nurse ratio | |||||||
| Quartile 1 - lowest/best PTN [REF] | – | – | – | – | – | – | – |
| Quartile 2 | 1.18 [0.93–1.50] | 1.35 [0.93–1.94] | 0.90 [0.67–1.22] | 1.20 [0.78–1.85] | 1.15 [0.77–1.70] | 1.37 [1.07–1.77]* | 1.61 [1.14–2.27]** |
| Quartile 3 | 0.90 [0.67–1.21] | 1.09 [0.75–1.57] | 0.83 [0.62–1.10] | 1.08 [0.67–1.74] | 0.92 [0.64–1.31] | 0.94 [0.65–1.37] | 1.07 [0.72–1.60] |
| Quartile 4 - highest/worst PTN | 1.53 [1.04–2.26]* | 1.48 [1.03–2.13]* | 0.80 [0.56–1.14] | 1.56 [0.83–2.97] | 1.10 [0.71–1.69] | 1.46 [1.03–2.05]* | 1.40 [0.85–2.32] |
| Nurse Working Environment | |||||||
| Quartile 1 - lowest/worst score [REF] | – | – | – | – | – | – | – |
| Quartile 2 | 0.76 [0.54–1.07] | 0.94 [0.67–1.31] | 0.97 [0.75–1.27] | 0.73 [0.46–1.15] | 1.03 [0.73–1.47] | 0.59 [0.43–0.81]** | 0.83 [0.57–1.21] |
| Quartile 3 | 0.53 [0.38–0.73]*** | 0.75 [0.52–1.09] | 0.83 [0.62–1.10] | 0.62 [0.39–0.99]* | 0.71 [0.50–1.01] | 0.56 [0.40–0.79]*** | 0.74 [0.53–1.02] |
| Quartile 4 - highest/best score | 0.28 [0.19–0.42]*** | 0.41 [0.26–0.66]*** | 0.64 [0.43–0.95]* | 0.24 [0.11–0.54]*** | 0.45 [0.30–0.68]*** | 0.33 [0.23–0.46]*** | 0.35 [0.23–0.55]*** |
| Education | |||||||
| Bachelor's degree [REF] | – | – | – | – | – | – | – |
| Specialised nurses | 1.00 [0.81–1.25] | 1.16 [0.88–1.53] | 1.30 [0.99–1.73] | 1.01 [0.69–1.47] | 1.08 [0.85–1.38] | 1.17 [0.91–1.51] | 1.23 [0.92–1.65] |
| University degree | 1.34 [0.61–2.94] | 1.09 [0.56–2.15] | 1.31 [0.56–3.06] | 1.14 [0.43–2.99] | 0.94 [0.39–2.30] | 2.12 [0.99–4.50] | 3.13 [1.38–7.12]** |
| Specialised nurses and university degree | 1.12 [0.75–1.68] | 1.34 [0.96–1.86] | 1.20 [0.86–1.69] | 1.10 [0.71–1.72] | 1.03 [0.71–1.49] | 1.45 [0.99–2.12] | 1.95 [1.29–2.95]** |
| Nurses no bachelor | 1.02 [0.45–2.30] | 1.38 [0.71–2.66] | 1.37 [0.72–2.57] | 0.99 [0.41–2.36] | 1.18 [0.59–2.37] | 1.16 [0.57–2.35] | 0.94 [0.38–2.31] |
| Sex | |||||||
| Female [REF] | – | – | – | – | – | – | – |
| Male | 0.83 [0.69–0.99]* | 1.68 [1.36–2.07]*** | 0.86 [0.69–1.08] | 1.11 [0.85–1.45] | 0.95 [0.77–1.16] | 1.14 [0.97–1.35] | 1.26 [1.04–1.54]* |
| Non-binary | 0.67 [0.14–3.10] | 1.11 [0.38–3.27] | 0.40 [0.10–1.59] | 0.39 [0.07–2.13] | 0.65 [0.21–2.01] | 3.80 [1.52–9.55]** | 2.65 [0.94–7.49] |
| Age | |||||||
| Under 25 [REF] | – | – | – | – | – | – | – |
| 25–29 | 1.24 [0.81–1.90] | 1.27 [0.88–1.82] | 1.63 [1.17–2.29]** | 1.51 [0.95–2.41] | 1.62 [1.09–2.40]* | 2.12 [1.51–2.99]*** | 1.86 [1.18–2.93]** |
| 30–34 | 1.42 [0.94–2.15] | 1.05 [0.68–1.63] | 1.61 [1.07–2.40]* | 1.26 [0.78–2.03] | 1.79 [1.18–2.70]** | 3.31 [2.25–4.85]*** | 3.26 [1.90–5.59]*** |
| 35–39 | 1.14 [0.80–1.63] | 0.94 [0.62–1.44] | 1.82 [1.27–2.62]** | 1.49 [0.98–2.25] | 1.28 [0.80–2.06] | 2.48 [1.68–3.67]*** | 2.91 [1.73–4.88]*** |
| 40–44 | 1.01 [0.69–1.48] | 0.63 [0.40–1.00]* | 1.92 [1.22–3.03]** | 1.48 [0.87–2.51] | 0.99 [0.61–1.61] | 2.21 [1.52–3.21]*** | 2.27 [1.28–4.01]** |
| 45–49 | 1.34 [0.94–1.92] | 0.71 [0.47–1.08] | 1.86 [1.23–2.80]** | 1.34 [0.87–2.09] | 1.43 [0.90–2.28] | 1.56 [1.03–2.35]* | 1.61 [0.89–2.92] |
| 50–54 | 1.28 [0.81–2.01] | 0.62 [0.39–0.97]* | 1.49 [1.04–2.13]* | 1.36 [0.79–2.37] | 1.00 [0.64–1.56] | 1.50 [1.00–2.23]* | 1.56 [0.84–2.91] |
| 55–59 | 0.76 [0.46–1.25] | 0.35 [0.22–0.56]*** | 1.73 [1.12–2.68]* | 0.63 [0.34–1.14] | 0.99 [0.59–1.65] | 1.33 [0.81–2.19] | 1.79 [0.96–3.31] |
| 60 or over | 0.73 [0.46–1.15] | 0.20 [0.10–0.39]*** | 1.20 [0.65–2.22] | 0.30 [0.12–0.76]* | 0.77 [0.38–1.55] | 0.66 [0.36–1.23] | 1.27 [0.70–2.28] |
Legend: * p-value < 0.05, ** p-value < 0.01, *** p-value < 0.001; value in bold is statistically significant; [ref] = reference.
4. Discussion
This study assessed burnout and intention-to-leave the job and the nursing profession and analysed the relationships between these variables and the work environment among ICU nurses. Based on our study findings we can make some important observations.
First, this study confirms that, after two years of the COVID-19 pandemic, the rates of ICU nurses in Belgium at high risk of burnout and with the intention-to-leave the job and the profession are higher compared to similar data dating from before the pandemic (Bruyneel et al., 2021b; Van den Heede et al., 2019). Compared to studies in other countries, our results are also higher for risk of burnout and intention-to-leave the job and profession among ICU nurses (Gualano et al., 2021; Ramírez-Elvira et al., 2021; Xu et al., 2021). The impact of COVID-19 on the risk of burnout and intention-to-leave the job and the profession seems to be increased among ICU nurses compared to before the pandemic and after the first wave (Bruyneel et al., 2021b; Butera et al., 2021; Vermeir et al., 2018). This can be explained by several elements including the lack of personal protective equipment, fear of being contaminated, increased mortality rates compared to normal, successive waves, societal expectations, and accumulation over time (Bruyneel et al., 2021b; Khan et al., 2022; LeClaire et al., 2022; Moradi et al., 2021). Hospitals have implemented, in a variable and heterogeneous way, several internal measures (e.g., psychologists, debriefing, meditation) which may have influenced the results with ICU nurses in Belgium (Paquay et al., 2022; Servotte et al., 2020; Van Den Heede et al., 2022).
Second, hospitals with a better working environment, even in times of pandemic, have better results for the risk of burnout and intention-to-leave the job and profession than hospitals with a worse environment. This association has already been demonstrated in other studies and it seems that hospitals with a better work environment are better able to protect the wellbeing of nurses even in times of high stress (Alharbi et al., 2020; Kester et al., 2021; Lake et al., 2022; Sermeus et al., 2011; Van den Heede et al., 2019; Wei et al., 2018). Given these results by subscale, hospital managers and health-related policies can prioritise their interventions to improve the nursing work environment. Initiatives such as the “Magnet hospital accreditation” concept could be interesting to implement to foster a better working environment that includes factors such as structural empowerment of clinical staff, transformational leadership, exemplary and evidence-based professional practice, new knowledge, innovations and improvements (Lake et al., 2022; Sermeus et al., 2022, Sermeus et al., 2022). This accreditation requires, among other things, flat and decentralised organisational structures, empowerment of the frontline staff in decision-making and transformational leadership (Sermeus et al., 2022, Sermeus et al., 2022). The analysis of the working environment in this study showed that the worst subscales were “participation in hospital affairs” and “adequate staffing and resources”. If we compare the results on the work environment with a study conducted in general hospitalisation units in 2019, the results on the dimension “participation in hospital affairs” were much worse in this study (Van den Heede et al., 2019). It is likely that many factors related to the pandemic are responsible for this, such as the integration of head nurses into care, the difficulties of management present in ICUs, and an expectation of structural changes in the hospital's organisation. The dimension “foundations for quality of care” also decreased compared to 2019, as COVID-19 patients may contribute to a high workload in ICUs (Bruyneel et al., 2021a; Dellicour et al., 2021). In addition, Belgium experienced two initial major waves in COVID-19 hospital admissions to the ICU and high occupancy rates impacted the mortality of COVID-19 and non-COVID-19 patients (Brinkman et al., 2022; Guillon et al., 2021; Payet et al., 2022; Taccone et al., 2020). On the other hand, the results for the dimension “physician-nurse relationships” were better, this can be explained by the close and permanent collaboration in the ICU, especially during the COVID-19 period (Chapman et al., 2021; Yan et al., 2021). The results for the “leadership” and “management” dimensions are somewhat ambiguous with relatively good scores for some items and relatively poor scores on items like “praise” and “recognition”. Lack of praise and recognition from management and supervisors are likely to be priorities for investment in the work environment, alongside the general lack of recognition of their role throughout the pandemic (e.g., from the general public, policy makers, the media) ensuring that people receive recognition in line with their personal definition of meaning, fulfilment, development, and advancement at every stage of their professional career.
Third, concerning the patient-to-nurse ratio, we found an independent association between only emotional exhaustion and depersonalisation with intention-to-leave the job. This observation had already been made for the risk of burnout and the patient-to-nurse ratio (Bruyneel et al., 2021b). In addition, the increased workload due to COVID-19 and the deployment of non-ICU nurses to compensate for it may also have increased the high risk of burnout among ICU nurses (Bruyneel et al., 2021a; Lucchini et al., 2021). A better patient-to-nurse ratio could therefore also influence some of the outcomes of intensive care nurses.
Finally, we found other independent factors for the risk of burnout and the intention-to-leave the job and the nursing profession. Nurses with a university degree had a higher risk of intention-to-leave the nursing profession, which can be explained by other professional opportunities, but will complicate the ability to hire and retain nurse managers who are required to have a university degree in Belgium (Phillips et al., 2021). ICU nurses between 25 and 40 years old had a higher risk of intention-to-leave their job and the nursing profession. Retention seems to be a real challenge in these age categories. Given these results, it seems essential to invest in retention policies to minimise turnover (such as improved job satisfaction and organisational commitments), especially as the expertise required to work in critical care and provide high quality care is scarce and requires a long period of education and on-the-job training (Butera et al., 2021; Lee et al., 2018; Xu et al., 2021). A specific strategy per age group seems to be useful with measures to improve work-life balance (e.g., family-friendly working hours, adapting shifts with childcare needs, more financial incentives), to stimulate younger nurses (e.g., professional development and project work), and to divide and adjust work circumstances to adapt the work to account for generational differences (e.g., less frequency of night shifts, physically demanding work) and paying attention to intergenerational conflicts for older nurses (Clendon and Walker, 2012; Khan et al., 2019; Wieck et al., 2010). In addition, the COVID-19 pandemic certainly worsened the relationships between colleagues and traumatic/stressful experiences in the workplace, important factors for the intention-to-leave the job among ICU nurses (Khan et al., 2019).
4.1. Limits and strengths
This study has some limitations. The current study is cross-sectional in nature, which means that it allows us to describe the variation in nurse working environments and nurse outcomes across hospital sites and study the relationships between these concepts but the interpretation of the relationships is limited because many other factors may influence the results. Moreover, the results are self-reported and need to be further explored with additional, more objective measures (e.g., what proportion of nurses that report an intention-to-leave actually leave their job, what is the link between high risk of burnout and clinically-diagnosed burnout, does the nurse-perceived quality of care correspond with objectively measured quality indicators). Although the response rate of 47.8% is relatively good, it is not at the level of similar studies conducted prior to the pandemic (from 40% to 80% depending on the country) (Aiken et al., 2014; Van den Heede et al., 2019). Nevertheless, the response rate (both at the level of the hospitals and the nurses) can, given the specific context (e.g., the COVID crisis had led to increased workload and higher absenteeism among ICU nurses), be considered relatively high. Note that nurses on sick leave were excluded from the analyses, which may have influenced the results. In addition, to allow hospital site-level analyses, we have excluded hospital sites based on arbitrary criteria (i.e., > 75% response rate of ICU nursing staff per hospital site or at least 10 ICU nurses responding). Moreover, it is possible that nurses included in the sample were biased (e.g., more nurses with complaints responded) compared to non-responders. Yet, it is also possible that nurses not included in the survey were absent because of problems such as burnout. The study period was defined by the commissioner of the study (the Belgian Health Care Knowledge Centre) to inform the Belgian Minister of Public Health about the state of wellbeing of ICU nurses after two years of pandemic. After all, ICU nurses were identified as an important bottleneck during the pandemic to ensure sufficient hospital capacity. The timing has an important potential impact on the results. A further follow-up of the study will be required to evaluate how this wellbeing evolved over time (e.g., in periods with lower ICU capacity demands). Finally, other psychological factors (e.g., depression, anxiety) and several internal measures of psychological support that were not analysed in this study could also have influenced the risk of burnout (Fischer et al., 2020).
5. Conclusions
This study found a high prevalence of high burnout risk and intention-to-leave the job and nursing profession after two years of the COVID-19 pandemic. However, there was statistically significant variability in our results by hospital site, which can be largely explained by a better work environment and more favourable patient-to-nurse ratios at some sites. This study highlighted the importance of monitoring the risk of burnout and turnover among ICU nurses during the COVID-19 pandemic or other stressful events and implementing interventions to prevent and manage it, taking into account the risk factors identified in this study.
CRediT authorship contribution statement
Arnaud Bruyneel: Conceptualization, Visualisation, Writing - Review & Editing; Nicolas Bouckaert: Methodology, Software, Data Curation, Formal analysis; Charline Maertens de Noordhout: Validation; Jens Detollenaere: Validation; Laurence Kohn: Validation; Magali Pirson: Validation and Supervision; Walter Sermeus: Validation and Supervision; Koen Van den Heede: Validation, Supervision, Writing- Reviewing and Editing, Project administration.
Data availability statement
The authors prefer not to share the data from our study publicly. However, they are available from the authors.
Funding
This study was funded by the Belgian Health Care Knowledge Centre (KCE). The KCE is a federal institution which is financed by the National Institute for Health and Disability Insurance (NIHDI, RIZIV – INAMI), the Federal Public Service of health, food chain safety and environment, and the Federal Public Service of social security. The development of health services research studies is part of the legal mission of the KCE. Although the development of the studies is paid by the KCE budget, the sole mission of the KCE is providing scientifically valid information.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors acknowledge the contribution of a medical writer, Sandy Field, PhD, in the preparation of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnurstu.2022.104385.
Appendix A. Supplementary data
Supplementary figures
References
- Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M., Bruyneel L., Rafferty A.M., Griffiths P., Moreno-Casbas M.T., Tishelman C., Scott A., Brzostek T., Kinnunen J., Schwendimann R., Heinen M., Zikos D., Sjetne I.S., Smith H.L., Kutney-Lee A. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.H., Sloane D.M., Bruyneel L., Van den Heede K., Griffiths P., Busse R., Diomidous M., Kinnunen J., Kózka M., Lesaffre E., McHugh M.D., Moreno-Casbas M.T., Rafferty A.M., Schwendimann R., Scott P.A., Tishelman C., van Achterberg T., Sermeus W. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383:1824–1830. doi: 10.1016/S0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M., Bruyneel L., Rafferty A.M., Griffiths P., Moreno-Casbas M.T., Tishelman C., Scott A., Brzostek T., Kinnunen J., Schwendimann R., Heinen M., Zikos D., Sjetne I.S., Smith H.L., Kutney-Lee A. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alharbi A.A., Dahinten V.S., MacPhee M. The relationships between nurses’ work environments and emotional exhaustion, job satisfaction, and intent to leave among nurses in Saudi Arabia. J. Adv. Nurs. 2020;76:3026–3038. doi: 10.1111/jan.14512. [DOI] [PubMed] [Google Scholar]
- Atroszko P.A., Demetrovics Z., Griffiths M.D. Work addiction, obsessive-compulsive personality disorder, burn-out, and global burden of disease: implications from the ICD-11. IJERPH. 2020;17:660. doi: 10.3390/ijerph17020660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutou A., Pitsiou G., Sourla E., Kioumis I. Burnout syndrome among emergency medicine physicians: an update on its prevalence and risk factors. Eur. Rev. Med. Pharmacol. Sci. 2019;23:9058–9065. doi: 10.26355/eurrev_201910_19308. [DOI] [PubMed] [Google Scholar]
- Brinkman S., Termorshuizen F., Dongelmans D.A., Bakhshi-Raiez F., Arbous M.S., de Lange D.W., de Keizer N.F., Verbiest D.P., te Velde L.F., van Driel E.M., Rijpstra T., Elbers P.H.J., Houwink A.P.I., Georgieva L., Verweij E., de Jong R.M., van Iersel F.M., Koning T.J.J., Rengers E., Kusadasi N., Erkamp M.L., van den Berg R., Jacobs C.J.M.G., Epker J.L., Rijkeboer A.A., de Bruin M.T., Spronk P., Draisma A., Versluis D.J., van den Berg A.E., Mos M.V., Lens J.A., Pruijsten R.V., Kieft H., Rozendaal J., Nooteboom F., Boer D.P., Janssen I.T.A., van Gulik L., Koetsier M.P., Silderhuis V.M., Schnabel R.M., Drogt I., de Ruijter W., Bosman R.J., Frenzel T., Urlings-Strop L.C., Dijkhuizen A., Hené I.Z., de Meijer A.R., Holtkamp J.W.M., Postma N., Bindels A.J.G.H., Wesselink R.M.J., van Slobbe-Bijlsma E.R., van der Voort P.H.J., Eikemans B.J.W., Mehagnoul-Schipper D.J., Gommers D., Lutisan J.G., Hoeksema M., Barnas M.G.W., Festen-Spanjer B., van Lieshout M., Gritters N.C., van Tellingen M., Brunnekreef G.B., Vandeputte J., Dormans T.P.J., Hoogendoorn M.E., de Graaff M., Moolenaar D., Reidinga A.C., Spijkstra J.J., de Waal R. Comparison of outcome and characteristics between 6343 COVID-19 patients and 2256 other community-acquired viral pneumonia patients admitted to Dutch ICUs. J. Crit. Care. 2022;68:76–82. doi: 10.1016/j.jcrc.2021.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Smith P. Comparison of the prevalence of burnout risk between ICU and non-ICU nurses during the COVID-19 outbreak in French-speaking Belgium. Intensive Crit. Care Nurs. 2021;66 doi: 10.1016/j.iccn.2021.103086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Tack J., Droguet M., Maes J., Wittebole X., Miranda D.R., Pierdomenico L.D. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): a prospective study in 16 hospitals in Belgium. J. Crit. Care. 2019;54:205–211. doi: 10.1016/j.jcrc.2019.08.032. [DOI] [PubMed] [Google Scholar]
- Bruyneel A., Gallani M.-C., Tack J., d’Hondt A., Canipel S., Franck S., Reper P., Pirson M. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit. Care Nurs. 2021;62 doi: 10.1016/j.iccn.2020.102967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Smith P., Tack J., Pirson M. Prevalence of burnout risk and factors associated with burnout risk among ICU nurses during the COVID-19 outbreak in French speaking Belgium. Intensive Crit. Care Nurs. 2021;103059 doi: 10.1016/j.iccn.2021.103059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butera S., Brasseur N., Filion N., Bruyneel A., Smith P. Prevalence and associated factors of burnout risk among intensive care and emergency nurses before and during the coronavirus disease 2019 pandemic: a cross-sectional study in Belgium. J. Emerg. Nurs. 2021;47:879–891. doi: 10.1016/j.jen.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman L.B., Kopp K.E., Petty M.G., Hartwig J.L.A., Pendleton K.M., Langer K., Meiers S.J. Benefits of collaborative patient care rounds in the intensive care unit. Intensive Crit. Care Nurs. 2021;63 doi: 10.1016/j.iccn.2020.102974. [DOI] [PubMed] [Google Scholar]
- Cho E., Sloane D.M., Kim E.-Y., Kim S., Choi M., Yoo I.Y., Lee H.S., Aiken L.H. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int. J. Nurs. Stud. 2015;52:535–542. doi: 10.1016/j.ijnurstu.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clendon J., Walker L. ‘Being young’: a qualitative study of younger nurses’ experiences in the workplace: younger nurses’ experiences in the workplace. Int. Nurs. Rev. 2012;59:555–561. doi: 10.1111/j.1466-7657.2012.01005.x. [DOI] [PubMed] [Google Scholar]
- Dellicour S., Linard C., Van Goethem N., Da Re D., Artois J., Bihin J., Schaus P., Massonnet F., Van Oyen H., Vanwambeke S.O., Speybroeck N., Gilbert M. Investigating the drivers of the spatio-temporal heterogeneity in COVID-19 hospital incidence—Belgium as a study case. Int. J. Health Geogr. 2021;20:29. doi: 10.1186/s12942-021-00281-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dion G., Tessier R. Validation de la traduction de l’Inventaire d’épuisement professionnel de maslach et Jackson. Can. J. Behav. Sci. 1994;26:210–227. doi: 10.1037/0008-400X.26.2.210. [DOI] [Google Scholar]
- Embriaco N., Papazian L., Kentish-Barnes N., Pochard F., Azoulay E. Burnout syndrome among critical care healthcare workers. Curr. Opin. Crit. Care. 2007;13:482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- Fischer R., Mattos P., Teixeira C., Ganzerla D.S., Rosa R.G., Bozza F.A. Association of Burnout with Depression and Anxiety in critical care clinicians in Brazil. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.30898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M.R., Sinigaglia T., Lo Moro G., Rousset S., Cremona A., Bert F., Siliquini R. The burden of burnout among healthcare professionals of intensive care units and emergency departments during the COVID-19 pandemic: a systematic review. IJERPH. 2021;18:8172. doi: 10.3390/ijerph18158172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillon A., Laurent E., Duclos A., Godillon L., Dequin P.-F., Agrinier N., Kimmoun A., Grammatico-Guillon L. Case fatality inequalities of critically ill COVID-19 patients according to patient-, hospital- and region-related factors: a French nationwide study. Ann. Intensive Care. 2021;11:127. doi: 10.1186/s13613-021-00915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guixia L., Hui Z. A study on burnout of nurses in the period of COVID-19. PBS. 2020;9:31. doi: 10.11648/j.pbs.20200903.12. [DOI] [Google Scholar]
- Hu D., Kong Y., Li W., Han Q., Zhang X., Zhu L.X., Wan S.W., Liu Z., Shen Q., Yang J., He H.-G., Zhu J. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. 2020;100424 doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun J., Ojemeni M.M., Kalamani R., Tong J., Crecelius M.L. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int. J. Nurs. Stud. 2021;119 doi: 10.1016/j.ijnurstu.2021.103933. [DOI] [PubMed] [Google Scholar]
- Kester K., Pena H., Shuford C., Hansen C., Stokes J., Brooks K., Bolton T., Ornell A., Parker P., Febre J., Andrews K., Flynn G., Ruiz R., Evans T., Kettle M., Minter J., Granger B. Implementing AACN’s healthy work environment framework in an intensive care unit. Am. J. Crit. Care. 2021;30:426–433. doi: 10.4037/ajcc2021108. [DOI] [PubMed] [Google Scholar]
- Khan N., Jackson D., Stayt L., Walthall H. Factors influencing nurses’ intentions to leave adult critical care settings: what factors influence nurses’ intentions to leave the adult critical care areas? Nurs. Crit. Care. 2019;24:24–32. doi: 10.1111/nicc.12348. [DOI] [PubMed] [Google Scholar]
- Khan Y., Bruyneel A., Smith P. Determinants of the risk of burnout among nurses during the first wave of the COVID-19 pandemic in Belgium: a cross-sectional study. J. Nurs. Manag. 2022;30:1125–1135. doi: 10.1111/jonm.13624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E.T. Development of the practice environment scale of the nursing work index. Res. Nurs. Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lake E.T., Riman K.A., Lee C. The association between hospital nursing resource profiles and nurse and patient outcomes. J. Nurs. Manag. 2022 doi: 10.1111/jonm.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E.T., Riman K.A., Sloane D.M. Improved work environments and staffing lead to less missed nursing care: a panel study. J. Nurs. Manag. 2020;28:2157–2165. doi: 10.1111/jonm.12970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeClaire M., Poplau S., Linzer M., Brown R., Sinsky C. Compromised integrity, burnout, and intent to leave the job in critical care nurses and physicians. Crit. Care Explor. 2022;4 doi: 10.1097/CCE.0000000000000629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.E., Vincent C., Dahinten V.S., Scott L.D., Park C.G., Dunn Lopez K. Effects of individual nurse and hospital characteristics on patient adverse events and quality of care: a multilevel analysis: patient safety quality of care. J. Nurs. Scholarsh. 2018;50:432–440. doi: 10.1111/jnu.12396. [DOI] [PubMed] [Google Scholar]
- Lucchini A., Bambi S., Bruyneel A. Redefining “Critical care”: from where intensive care unit beds are located to patients’ status. Intensive Crit. Care Nurs. 2021;103188 doi: 10.1016/j.iccn.2021.103188. [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P., Schaufeli W., Schwab R. 1986. Maslach Burnout Inventory Manual, General Survey, Human Services Survey, Educators Survey Ad Scoring Guides. Menlo Park, CA Mind Garden. [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P. 1996. Maslach Burnout Inventory Consulting Psychologists Press. [Google Scholar]
- Molenberghs G., Faes C., Verbeeck J., Deboosere P., Abrams S., Willem L., Aerts J., Theeten H., Devleesschauwer B., Sierra N.B., Renard F., Herzog S., Lusyne P., Van der Heyden J., Van Oyen H., Van Damme P., Hens N. Belgian COVID-19 mortality, excess deaths, number of deaths per million, and infection fatality rates (9 March — 28 June 2020) (preprint) Epidemiology. 2020 doi: 10.1101/2020.06.20.20136234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi Y., Baghaei R., Hosseingholipour K., Mollazadeh F. Challenges experienced by ICU nurses throughout the provision of care for COVID-19 patients: a qualitative study. J. Nurs. Manag. 2021;29:1159–1168. doi: 10.1111/jonm.13254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natalia Y.A., Faes C., Neyens T., Molenberghs G. The COVID-19 wave in Belgium during the fall of 2020 and its association with higher education. PLoS ONE. 2022;17 doi: 10.1371/journal.pone.0264516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquay M., Dubois N., Diep A.N., Graas G., Sassel T., Piazza J., Servotte J.-C., Ghuysen A. “Debriefing and organizational lessons learned” (DOLL): a qualitative study to develop a classification framework for reporting clinical debriefing results. Front. Med. 2022;9 doi: 10.3389/fmed.2022.882326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payet C., Polazzi S., Rimmelé T., Duclos A. Mortality among noncoronavirus disease 2019 critically ill patients attributable to the pandemic in France. Crit. Care Med. 2022;50:138–143. doi: 10.1097/CCM.0000000000005215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Francisco D.H., Duarte-Clíments G., del Rosario-Melián J.M., Gómez-Salgado J., Romero-Martín M., Sánchez-Gómez M.B. Influence of workload on primary care nurses’ health and burnout, patients’ safety, and quality of care: integrative review. Healthcare. 2020;8:12. doi: 10.3390/healthcare8010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips J., Palokas M., Christian R., Harris J., Hinton E. Emotional intelligence in nurse managers as it relates to staff nurse job satisfaction and retention: a scoping review. JBI Evid. Synth. 2021;19:3238–3267. doi: 10.11124/JBIES-20-00299. [DOI] [PubMed] [Google Scholar]
- Ramírez-Elvira S., Romero-Béjar J.L., Suleiman-Martos N., Gómez-Urquiza J.L., Monsalve-Reyes C., Cañadas-De la Fuente G.A., Albendín-García L. Prevalence, risk factors and burnout levels in intensive care unit nurses: a systematic review and meta-analysis. IJERPH. 2021;18:11432. doi: 10.3390/ijerph182111432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenstein L.S., Torre M., Ramos M.A., Rosales R.C., Guille C., Sen S., Mata D.A. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sermeus W., Aiken L.H., Ball J., Bridges J., Bruyneel L., Busse R., De Witte H., Dello S., Drennan J., Eriksson L.E., Griffiths P., Kohnen D., Köppen J., Lindqvist R., Maier C.B., McHugh M.D., McKee M., Rafferty A.M., Schaufeli W.B., Sloane D.M., Alenius L.S., Smith H. A workplace organisational intervention to improve hospital nurses’ and physicians’ mental health: study protocol for the Magnet4Europe wait list cluster randomised controlled trial. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-059159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sermeus W., Aiken L.H., Van den Heede K., Rafferty A.M., Griffiths P., Moreno-Casbas M.T., Busse R., Lindqvist R., Scott A.P., Bruyneel L., Brzostek T., Kinnunen J., Schubert M., Schoonhoven L., Zikos D., RN4CAST consortium Nurse forecasting in Europe (RN4CAST): rationale, design and methodology. BMC Nurs. 2011;10(6) doi: 10.1186/1472-6955-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sermeus W., Aiken L.H., Ball J., Bridges J., Bruyneel L., Busse R., De Witte H., Dello S., Drennan J., Eriksson L.E., Griffiths P., Kohnen D., Köppen J., Lindqvist R., Maier C.B., McHugh M.D., McKee M., Rafferty A.M., Schaufeli W.B., Sloane D.M., Alenius L.S., Smith H. A workplace organisational intervention to improve hospital nurses’ and physicians’ mental health: study protocol for the Magnet4Europe wait list cluster randomised controlled trial. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-059159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servotte J.-C., Welch-Horan T.B., Mullan P., Piazza J., Ghuysen A., Szyld D. Development and implementation of an end-of-shift clinical debriefing method for emergency departments during COVID-19. Adv. Simul. 2020;5:32. doi: 10.1186/s41077-020-00150-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A., Wyatt M., Gourneau B., Shih G., De Ruyter M. Emotional exhaustion among anesthesia providers at a tertiary care center assessed using the MBI burnout survey. Psychol. Health Med. 2019;24:620–624. doi: 10.1080/13548506.2018.1546019. [DOI] [PubMed] [Google Scholar]
- Simonetti M., Cerón C., Galiano A., Lake E.T., Aiken L.H. Hospital work environment, nurse staffing and missed care in Chile: a cross-sectional observational study. J. Clin. Nurs. 2021;jocn.16068 doi: 10.1111/jocn.16068. [DOI] [PubMed] [Google Scholar]
- Swiger P.A., Patrician P.A., Raju D., Breckenridge-Sproat S., Loan L.A., Miltner R.S.Susie. The Practice Environment Scale of the Nursing Work Index: an updated review and recommendations for use. Int. J. Nurs. Stud. 2017;74:76–84. doi: 10.1016/j.ijnurstu.2017.06.003. [DOI] [PubMed] [Google Scholar]
- Taccone F.S., Vangoethem N., Depauw R., Wittebole X., Blot K., Vanoyen H., Lernout T., Montourcy M., Meyfroidt G., Vanbeckhoven D. The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium. Lancet Reg. Health Eur. 2020;100019 doi: 10.1016/j.lanepe.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Heede K., Bruyneel L., Beeckmans D., Boon N., Bouckaert N., Cornelis J., Dossche D., Van de Voorde C., Sermeus W. KCE Reports 325, D/2019/10.273/75. Belgian Health Care Knowledge Centre (KCE); Brussels: 2019. Safe nurse staffing levels in acute hospitals. Health Services Research (HSR) [Google Scholar]
- Van den Heede K., Bouckaert N., Detollenaere J., Kohn K., Maertens de Noordhout C., Vanhooreweghe J., Bruyneel A., Sermeus W. (No. KCE Reports 353. D/2022/10.273/24.) Belgian Health Care Knowledge Centre (KCE); Brussels: 2022. Nurse staffing on Belgian intensive care units: the impact of two years of COVID-19 pandemic. Health Services Research (HSR) [Google Scholar]
- Vandenbroeck S., Van Gerven E., De Witte H., Vanhaecht K., Godderis L. Burnout in Belgian physicians and nurses. Occup. Med. 2017;67:546–554. doi: 10.1093/occmed/kqx126. [DOI] [PubMed] [Google Scholar]
- Van Gerven E., Vander Elst T., Vandenbroeck S., Dierickx S., Euwema M., Sermeus W., De Witte H., Godderis L., Vanhaecht K. Increased risk of burnout for physicians and nurses involved in a patient safety incident. Med. Care. 2016;54:937–943. doi: 10.1097/MLR.0000000000000582. [DOI] [PubMed] [Google Scholar]
- Vermeir P., Blot S., Degroote S., Vandijck D., Mariman A., Vanacker T., Peleman R., Verhaeghe R., Vogelaers D. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: a questionnaire study. Intensive Crit. Care Nurs. 2018;48:21–27. doi: 10.1016/j.iccn.2018.07.001. [DOI] [PubMed] [Google Scholar]
- Welp A., Rothen H.U., Massarotto P., Manser T. Teamwork and clinician burnout in Swiss intensive care: the predictive role of workload, and demographic and unit characteristics. Swiss Med. Wkly. 2019 doi: 10.4414/smw.2019.20033. [DOI] [PubMed] [Google Scholar]
- Wei H., Sewell K.A., Woody G., Rose M.A. The state of the science of nurse work environments in the United States: a systematic review. Int. J. Nurs. Sci. 2018;5:287–300. doi: 10.1016/j.ijnss.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieck K.L., Dols J., Landrum P. Retention priorities for the intergenerational nurse workforce. Nurs. Forum. 2010;45:7–17. doi: 10.1111/j.1744-6198.2009.00159.x. [DOI] [PubMed] [Google Scholar]
- Woo T., Ho R., Tang A., Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J. Psychiatr. Res. 2020;123:9–20. doi: 10.1016/j.jpsychires.2019.12.015. [DOI] [PubMed] [Google Scholar]
- Xu G., Zeng X., Wu X. Global prevalence of turnover intention among intensive care nurses: a meta-analysis. Nurs. Crit. Care. 2021;nicc.12679 doi: 10.1111/nicc.12679. [DOI] [PubMed] [Google Scholar]
- Yan C., Zhang X., Gao C., Wilfong E., Casey J., France D., Gong Y., Patel M., Malin B., Chen Y. Collaboration structures in COVID-19 critical care: retrospective network analysis study. JMIR Hum. Factors. 2021;8 doi: 10.2196/25724. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures
Data Availability Statement
The authors prefer not to share the data from our study publicly. However, they are available from the authors.